The proteins of the mammalian blood coagulation system, a group of proteins and regulators whose major job is to stop bleeding, exist in the plasma vascular compartment and have opportunity to interact with multiple other proteins. The article by Tang et al. presents the novel observation that transferrin, an iron transport protein that exists in plasma in concentration excess to all the blood coagulation proteins, promotes blood coagulation by increasing thrombin and factor XIIa activities and inhibiting antithrombin.
The blood coagulation system whose major function is to control bleeding, i.e., hemostasis, consists of a core group of proenzymes (factor XII, prekallikrein, factor XI, factor IX, factor VII, factor X, prothrombin), cofactors and substrates (high molecular weight kininogen, factor VIII, tissue factor, factor V, protein S, and fibrinogen), clot lysing (fibrinolytic) agents (plasminogen, tissue and urokinase plasminogen activators), and regulators (antithrombin (AT), C1 inhibitor, α-2-antiplasmin, protein C, plasminogen activator inhibitor, and tissue factor pathway inhibitor) (Fig. 1). Deficiencies or defects in these proteins lead to bleeding or influence thrombosis risk. Most think of the process as an isolated system whose activation proceeds through two pathways (tissue factor-factor VIIa or contact activation) in a linear cascade. However, this system exists in the intravascular compartment in blood plasma, a proteinaceous fluid filled with the secreted protein products of the liver and other cells. It has been recognized that the plasma proteins vitronectin, histidine-rich glycoprotein, myeloid-related protein 8–14, amyloid precursor protein, C-reactive protein, and β-2-glycoprotein 1, influence thrombosis risk without effect on hemostasis. Modifiers of hemostasis are less recognized.
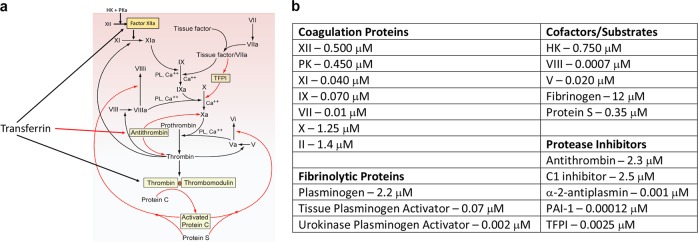
Fig. 1. Transferrin regulates systemic blood coagulation.
a The hemostatic and inhibitor systems in plasma. Lines in black represent activation pathways; lines in red represent inhibitory pathways. The blood coagulation system is activated in two ways: factor XIIa (XIIa) activates factor XI (XI) or tissue factor and factor VIIa (VIIa) activates factor IX (IX). High molecular weight kininogen (HK) and plasma kallikrein (PKa) activate factor XII (XII) to activated factor XII (XIIa). Both pathways lead to factor X activation (Xa). Xa along with factor V (V) catalyzes prothrombin (II) activation to thrombin (IIa), the main blood coagulation enzyme. Thrombin formation is regulated by three systems: (1) the tissue factor pathway inhibitor (TFPI) that regulates VII’s and tissue factor’s direct activation of X; (2) antithrombin that inhibits Xa, IIa, and every other blood coagulation enzyme (not shown); (3) activated protein C (APC) along with its cofactor, protein S, that inactivates VIIIa and Va forms of these cofactors to serve as cofactors for X and II activation, respectively. The present paper introduces another regulator to the blood coagulation system. Transferrin increases activity of factor XIIa (XIIa) and thrombin (IIa) by opening their catalytic sites. It also inhibits antithrombin by binding to its reactive center loop. b The major proteins of the blood coagulation system. Coagulation proteins: factor XII (XII), prekallikrein (PK), factor XI (XI), factor IX (IX), factor VII (VII), factor X (X), and prothrombin (II). Coagulation cofactors and substrates: high molecular weight kininogen (HK), factor VIII (VIII), factor V (V), fibrinogen, and protein S. Tissue factor was not included in this table. Fibrinolytic proteins: plasminogen, tissue plasminogen activator, urokinase plasminogen activator. Protease inhibitors: antithrombin, C1 inhibitor (inhibitor of factor XIIa, plasma kallikrein, factor XIa), α-2-antiplasmin, plasminogen activator inhibitor (PAI-1), and TFPI. The plasma concentration of transferrin is greater than the sum of all coagulation, cofactor/substrate, fibrinolytic, and protease inhibitors combined.
Transferrin is an 80 kDa iron transport protein that exists in plasma at a concentration of 25–45 μM, a value in excess of the sum of all the coagulation proteins and inhibitors.1 Transferrin is produced in the liver, semen, and cerebrospinal fluid. Although transferrin-bound iron accounts for <1% of total iron in the body, transferrin is the most vital protein involved in iron metabolism. Transferrin-bound iron is a pool of iron with the daily highest turnover, 25 mg/24 h. Free transferrin (apotransferrin) binds with high affinity 2 insoluble ferric3+ atoms for soluble transport; low pH (5.6) reduces affinity allowing for iron release to its receptor. High transferrin levels occur with iron deficiency, pregnancy, and oral contraceptives, indicating the need to bind more iron. Alternatively, in chronic inflammatory states, transferrin levels fall. Transferrin is a member of the innate immune system; it impedes bacterial survival upon binding iron. Non-transferrin-bound iron (NTBI) in serum is associated with vascular inflammation characterized by low-density lipoprotein oxidation, increased vascular reactive oxygen species, permeabilization, sustained endothelial cell activation, reduced NO production with impaired vasodilation, vascular calcification, proliferation and apoptosis, and macrophage and platelet activation in mice.2,3 In patients with genetic hemochromatosis, phlebotomy reduces inflammation and lipid peroxidation.2
The paper by Tang et al. reports a novel, expanding role for transferrin in blood coagulation.4 Transferrin is observed to accelerate blood coagulation. Transferrin binds thrombin, factor XII, fibrinogen, and AT with a Kd of 7.7, 13.9, 29, and 524 nM, respectively. Transferrin binds to the exosite I region of thrombin and an analogous region on factor XII, producing a slight shift in the position of the catalytic triad to increase the protease’s activity. This effect is similar both for apotransferrin (iron free) and holotransferrin (iron bound). At concentrations from 0.2 to 5 μM, transferrin enhanced the enzymatic activity of thrombin and factor XIIa by 0.2–1.8-fold and 0.8–2.7-fold, respectively. As revealed by immunoprecipitation, transferrin complexes with prothrombin and factor XII. Moreover, transferrin also blocks AT activity. Inactivation of thrombin or factor Xa by 2 μM AT is completely blocked by 10 μM transferrin. Transferrin binds near the reactive center loop of AT. The interference of thrombin inactivation also augments platelet aggregation induced by thrombin.
The investigators corroborated the above in vitro studies with in vivo murine models. In transferrin-overexpressing Apoe−/− mice (PLP-Tf), versus Apoe−/− controls, both fed a high fat diet (HFD), the plasmas of the transfected mice have shorter activated thromboplastin time (aPTT), prothrombin time (PT) and tail bleeding time. In contrast, when transferrin is knocked down in HFD-fed Apoe−/− mice (RNP-Tf), thrombin and factor XIIa activities are reduced and the aPTT, PT, and tail bleeding times are prolonged. Times of carotid artery thrombosis induced by ferric chloride are shorter in the PLP-Tf mice and prolonged in RNP-Tf mice.
Tang et al. further translated these findings to atherosclerosis.4 The average transferrin level is 4.3 mg/mL in patients with coronary artery disease (n = 120 patients) versus 2.8 mg/mL in healthy individuals (n = 120 subjects). After 6 weeks of treatment with an anti-transferrin antibody, the plasma transferrin levels of HFD-treated Apoe−/− mice dropped, with a prolongation of the aPTT, PT, and tail bleeding time and a decrease in thrombin enzymatic activity. Furthermore, 6 weeks of anti-transferrin antibody treatment or 3 weeks of treatment with either of two peptides that block transferrin’s interaction with thrombin led to reduced atherosclerotic plaque. Neither of these treatments have influence on iron metabolism. In contrast, transferrin overexpression is associated with accelerated atherosclerosis, where coagulation system is activated mainly through potentiating thrombin and factor XIIa and reducing AT’s inhibition of thrombin and factor Xa.
This study expands our notion of modifiers of the blood coagulation system. The hemostatic and thrombotic system is a subset of the inflammatory system. There are several important implications of the present study. Iron deficiency in a healthy individual will lead to increase of transferrin to carry more iron. In the absence of iron, the elevated transferrin may increase thrombin formation to balance lost hemostasis associated with worsening anemia. This kind of mechanism may cause a negative effect in polycythemia where phlebotomy therapy and secondary iron deficiency may contribute to the disease’s prothrombotic state. In chronic inflammatory states where transferrin levels fall, there may be a relaxation of thrombin activation as a counterbalance to the inflammatory state that the individual is experiencing. As ably shown by the authors, these kinds of events have potential to modify atherosclerosis. In conclusion, this important study represents the broader aspects of hemostatic and thrombotic disease, i.e., they usually mirror large disease states taking place in the subject.
References
- 1.Ogun, A. S. & Adeyinka, A. StatPearls (StatPearls Publishing, Treasure Island, FL, 2019).
- 2.Vinchi, F. et al. Eur. Heart J. 10.1093/eurheartj/ehz112 (2019).
- 3.Xu S. Trends Mol. Med. 2019;25:659–661. doi: 10.1016/j.molmed.2019.05.012. [DOI] [PubMed] [Google Scholar]
- 4.Tang, X. et al. Cell Res.10.1038/s41422-019-0260-6 (2019).