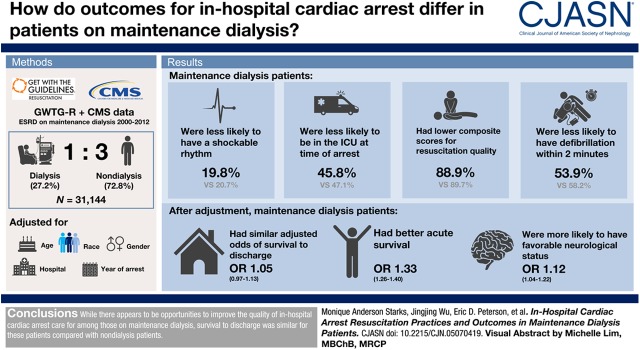
Visual Abstract
Keywords: Dialysis, cardiovascular disease, Epidemiology and outcomes, humans, United States, renal dialysis, Medicaid, logistical models, Centers for Medicare and Medicaid Services (U.S.), heart arrest, chronic kidney failure, Medicare, registries, intensive care units
Abstract
Background and objectives
Patients on maintenance dialysis with in-hospital cardiac arrest have been reported to have worse outcomes relative to those not on dialysis; however, it is unknown if poor outcomes are related to the quality of resuscitation. Using the Get With The Guidelines-Resuscitation (GWTG-R) registry, we examined processes of care and outcomes of in-hospital cardiac arrest for patients on maintenance dialysis compared with nondialysis patients.
Design, setting, participants, & measurements
We used GWTG-R data linked to Centers for Medicare and Medicaid data to identify patients with ESKD receiving maintenance dialysis from 2000 to 2012. We then case-matched adult patients on maintenance dialysis to nondialysis patients in a 1:3 ratio on the basis of age, sex, race, hospital, and year of arrest. Logistic regression models with generalized estimating equations were used to assess the association of in-hospital cardiac arrest and outcomes by dialysis status.
Results
After matching, there were a total of 31,144 GWTG-R patients from 372 sites, of which 8498 (27%) were on maintenance dialysis. Patients on maintenance dialysis were less likely to have a shockable initial rhythm (20% versus 21%) and less likely to be within the intensive care unit at the time of arrest (46% versus 47%) compared with nondialysis patients; they also had lower composite scores for resuscitation quality (89% versus 90%) and were less likely to have defibrillation within 2 minutes (54% versus 58%). After adjustment, patients on maintenance dialysis had similar adjusted odds of survival to discharge (odds ratio [OR], 1.05; 95% confidence interval [95% CI], 0.97 to 1.13), better acute survival (OR, 1.33; 95% CI, 1.26 to 1.40), and were more likely to have favorable neurologic status (OR, 1.12; 95% CI, 1.04 to 1.22) compared with nondialysis patients.
Conclusions
Although there appears to be opportunities to improve the quality of in-hospital cardiac arrest care for among those on maintenance dialysis, survival to discharge was similar for these patients compared with nondialysis patients.
Introduction
More than 200,000 Americans experience in-hospital cardiac arrest annually and survival remains low at approximately 22% (1). Patients with ESKD who are maintained on dialysis are known to be one of the highest risk groups for sudden cardiac death (2–4). Few studies have examined the incidence and outcomes of hospitalized patients on dialysis with a cardiac arrest; prior studies have suggested that cardiac arrests among patients on dialysis accounts for more than 17% of all in-hospital cardiac arrest, occurs 20 times more frequently, and is associated with lower survival compared with the general population (5,6). It has been suggested that the lower survival for patients on maintenance dialysis with in-hospital cardiac arrest may be because of differences in cardiac arrest mechanisms or less optimal resuscitation care, given the unique features of these patients (7).
Because prior large studies utilized only administrative data to characterize cardiac arrest events and outcomes, no study has examined detailed data on the clinical characteristics of cardiac arrest and specific processes of resuscitation care for patients on dialysis with in-hospital cardiac arrest. Therefore, using a comprehensive registry of in-hospital cardiac arrest with consecutive data capture, we sought to understand whether initial rhythm, resuscitation care, and outcomes for cardiac arrest differ for patients on maintenance dialysis compared with nondialysis patients. Our a priori hypotheses were that patients on maintenance dialysis would experience lower-quality resuscitation care and lower survival after in-hospital cardiac arrest compared with nondialysis patients.
Materials and Methods
Data Sources and Linkage
The American Heart Association’s (AHA) Get With the Guidelines-Resuscitation (GWTG-R) program is an ongoing, prospective, hospital-based clinical registry and quality improvement program for patients with in-hospital cardiac arrest. The design of GWTG-R has been previously described in detail (8). Briefly, all full-code patients with a confirmed in-hospital cardiac arrest who received cardiopulmonary resuscitation (CPR) are identified and enrolled by dedicated staff at participating hospitals. Cases are recognized by centralized collection of cardiac arrest flow sheets, review of hospital paging-system logs, routine checks of code carts, pharmacy tracer drug records, and hospital billing charges for code-cart charges. GWTG-R uses standardized “Utstein-Style” definitions for clinical variables and outcomes (9). Registry data completeness and accuracy are ensured by training, certification of hospital staff, and the use of standardized software with internal data checks (9). A prior report shows an error rate in data abstraction of 2% (8).
In this analysis, we sought to include only patients with ESKD receiving maintenance dialysis and exclude patients receiving dialysis for AKI. GWTG-R collects information on exposure to dialysis treatment before cardiac arrest, but the variable does not differentiate the indication for dialysis treatment (AKI versus ESKD). To identify patients with ESKD, we linked GWTG-R to Centers for Medicare and Medicaid (CMS) beneficiary and claims files. CMS files specifically identify all beneficiaries with ESKD, including the date of onset of ESKD. Because ESKD is a qualifying condition for Medicare coverage regardless of age, the ESKD flag variable is specifically tracked and continuously updated by CMS. To exclude patients with ESKD who underwent kidney transplantation, we excluded all patients with diagnosis codes for kidney transplantation (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9] code V42.0). This linkage method enabled us to identify patients with ESKD who were receiving maintenance dialysis before in-hospital cardiac arrest admission.
Because personally identifiable information is removed in GWTG-R, linkage of GWTG-R and CMS data sources was on the basis of six identifiers: the dates of hospital admission and discharge, the patient’s age and sex, the admitting hospital (deidentified), and use of ICD-9 diagnosis and procedure codes (10). ICD-9 codes used for linkage included cardiac arrest (427.5), ventricular fibrillation (427.41), or ventricular flutter (427.42), or a procedure code for CPR (99.60), defibrillation (99.62), defibrillator implantation (00.51 and 37.94), or closed chest message (99.63). We also selected records that included a diagnosis code for acute respiratory failure (518.81) or shock (785.5×) to identify patients who did not have a diagnosis of cardiac arrest in the Medicare claims data but otherwise were uniquely matched on all other identifiers, including hospital (11). A total of 63% of GWTG-R records were successfully linked to CMS files using this methodology.
IQVIA serves as the data collection (through their Patient Management Tool) and coordination center for GWTG. The University of Pennsylvania serves as the data analytic center and has an agreement to prepare the data for research purposes. All participating institutions were required to comply with local regulatory and privacy guidelines and, if required, to secure institutional review board approval. Because data were used primarily at the local site for quality improvement, sites were granted a waiver of informed consent under the common rule.
This study was approved by the Duke University Institutional Review Board (Pro00075032).
Study Population
Our starting cohort (180,655 patients from 667 sites) included all GWTG-R patients aged >18 years old between January 1, 2000 and December 31, 2012 (Figure 1). To avoid inflation in variance because of small numbers, patients were excluded if they were enrolled at sites with fewer than 20 patients with in-hospital cardiac arrest, averaged fewer than five cardiac arrests per year, or had participated in GWTG-R for less than a year. Patients at sites with missing hospital characteristics were also excluded. A total of 73,453 GWTG-R patients were linked to CMS claims records. Within this cohort, we identified 9401 patients with ESKD at the time of in-hospital cardiac arrest hospital admission, using the CMS ESKD indicator variable.
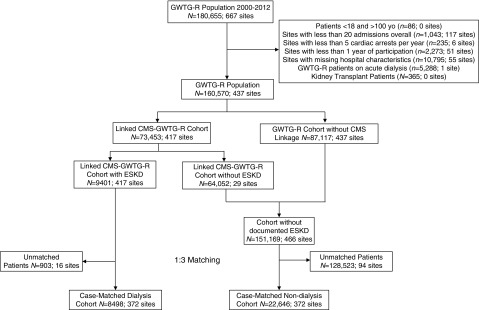
Figure 1.
Flow diagram of patient population. The maintenance dialysis cohort was derived from the GWTG-R cohort linked to CMS files to determine patients with documented ESKD. The nondialysis cohort was derived from GWTG-R patients who were not Medicare beneficiaries (no CMS linkage) as well as CMS-linked patients without the ESKD beneficiary flag. A 1:3 caliper match was used to match cohorts by age, sex, race, and year of cardiac arrest. CMS, Centers for Medicare and Medicaid; GWTG-R, Get With The Guidelines-Resuscitation.
To select a comparison cohort, we excluded patients who acutely received dialysis during in-hospital cardiac arrest admission as identified in GWTG-R, but were not patients on maintenance dialysis as identified by the linked CMS-GWTG-R cohort (n=5288). We also excluded any patients with ESKD who had undergone kidney transplant (n=365). Only index in-hospital cardiac arrest events were included and recurrent events were excluded. Next, to reduce bias, we selected a comparison cohort using a 1:3 caliper matching algorithm to case-match CMS-GWTG-R patients on maintenance dialysis to nondialysis GWTG-R patients on the basis of age, sex, race, hospital, and year of cardiac arrest. For the matching, we used a caliper width that required exact matching for sex and race. For age, we allowed matching up to ±3 years and matching up to ±1 year of cardiac arrest. As a result, our matching algorithm produced a 1:2.665 match. For the matching variables, we compared baseline distributions using absolute standardized differences between cohorts. A standardized difference >10% represents an imbalance between groups (12). Our final analytic dataset included 8498 CMS-GWTG-R patients on maintenance dialysis successfully matched to 22,646 nondialysis GWTG-R in-hospital cardiac arrest patients. Our total final study population was 31,144 patients from 372 hospitals (Figure 1).
Statistical Analyses
Acute resuscitation process quality was measured by five American College of Cardiology/American Heart Association guideline-recommended acute resuscitation measures and a composite performance score as previously defined (13). Briefly, the five ACLS resuscitation process measures were (1) device confirmation of correct endotracheal tube placement (14), (2) a monitored or witnessed cardiac arrest event (15), (3) time to first chest compression ≤1 minute, (4) time to first defibrillation delivered in ≤2 minutes for ventricular tachycardia/ventricular fibrillation (16), and (5) administration of epinephrine or vasopressin for pulseless events within 5 minutes. These five measures were chosen on the basis of standard guideline recommendations, evidence showing association of individual measure with outcome (14–16), and completeness of data (17). A performance score comprising these five resuscitation measures was then calculated for patients on maintenance dialysis versus nondialysis patients, using opportunity-based scoring. Opportunity scoring is defined as the sum of correct care divided by total care opportunities (18). Each patient, depending on the initial rhythm, could contribute either a maximum of four (nonshockable) or five (shockable) opportunities to the model. Duration of resuscitation, defined as the time from onset of cardiac arrest to termination of resuscitation efforts or declaration of the patient’s death, was also calculated for each group and reported.
Our primary exposure variable was ESKD receiving maintenance dialysis. Demographic, clinical, cardiac arrest event, and hospital characteristics were described overall and compared between patients on maintenance dialysis and nondialysis patients. Detailed definitions of the clinical characteristic variables are provided in Supplemental Table 1. Process variables and the composite performance scores were also compared overall and between the two groups. Chi-squared tests compared categorical variables; the Wilcoxon rank-sum test compared continuous variables across hospital performance quartiles. Categorical variables were presented as percentages, and continuous variables were presented as medians and interquartile ranges.
Our primary outcome was survival to discharge. Secondary outcomes were return of spontaneous circulation (acute survival) and favorable neurologic status (as defined by cerebral performance score of 1 or 2). Cerebral performance categories are defined as follows: 1, good cerebral performance; 2, moderate disability; 3, severe disability; 4, coma or vegetative state; and 5, brain death. Patients who died during the hospitalization were assigned a cerebral performance category score of 5 (brain death). Our resulting missing rate for cerebral performance category score was 5%; as a result of our small missingness and the likelihood that the outcome was not missing at random, we did not impute remaining scores.
Differences between unadjusted outcomes for each group was assessed by chi-squared tests for all outcomes. For each outcome, logistic regression models with generalized estimating equations were used to assess the association of outcomes after cardiac arrest and dialysis status. Generalized estimating equations accounts for clustering of patients within hospitals as patients in a given hospital share some commonalities related to their hospital or their environment compared with patients in a different hospital. Given that we utilized caliper matching, which improves the efficiency of variances, we elected not to use traditional conditional logistic regression techniques to account for matching. For adjustment, we sequentially added covariates to the model in three stages to assess effect of specific confounders. Demographic variables and clinical variables were added first, then hospital-level variables, and finally composite performance score. Demographic confounder variables included age, sex, and race, and clinical variables included initial cardiac arrest rhythm, location of cardiac arrest, and time and day of the event. Predictor variables included illness category and preexisting comorbid conditions. Hospital predictor variables included hospital type, hospital bed size, nurse-to-bed ratio, percentage of intensive care unit beds, geographic region, hospital location, and type of hospital ownership. Calendar year of cardiac arrest was included in the model at each sequential stage as a potential confounding variable, given calendar year association with improvement in outcome. All P values were two-sided and significant at P<0.05.
Results
Of 31,144 GWTG-R patients in the matched cohort, 8498 (27%) were on maintenance dialysis. After matching, the absolute percent standardized differences for age, sex, race, and year of cardiac arrest between cohorts were all <10%, indicating no evidence of imbalance between groups for these matching variables. Patients on dialysis had a higher prevalence of diabetes (52% versus 32%), congestive heart failure, prior myocardial infarction, septicemia, and metabolic or electrolyte abnormalities (20% versus 16%) Among the nondialysis cohort, 30% were reported as having some degree of kidney insufficiency. Compared with nondialysis patients, patients on maintenance dialysis were less likely to have malignancy, pneumonia, or respiratory insufficiency.
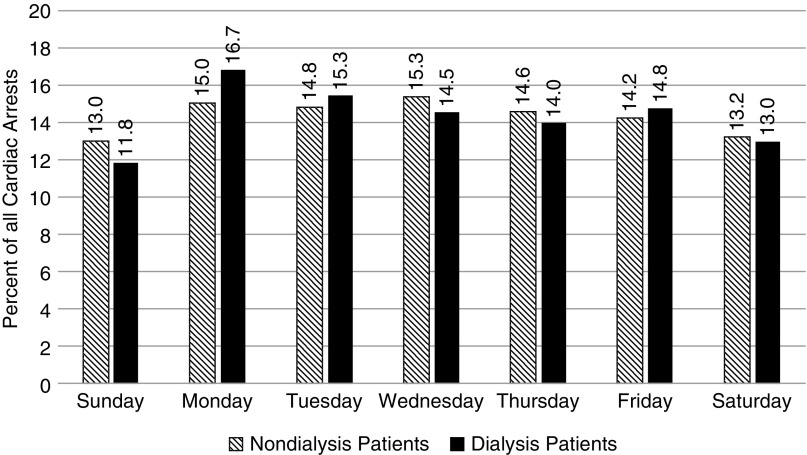
Regarding cardiac arrest characteristics, patients on maintenance dialysis were slightly less likely to have an initial shockable initial rhythm (20% versus 21%) and were less likely to be in the intensive care unit (46% versus 47%) at the time of arrest (Table 1). Because previous studies have reported an increased incidence of cardiac arrest in patients on hemodialysis on the first day of week after the 2-day dialysis-free weekend interval (19), we examined the same day of arrest patterns for in-hospital cardiac arrest, and found a similar pattern of higher rates of cardiac arrest on Monday (17% versus 15%) and Tuesday (15.3% versus 14.8%) for patients on maintenance dialysis compared with nondialysis patients (chi-squared P<0.001) (Figure 2, Supplemental Table 2). Approximately 19% of cardiac arrests in patients on maintenance dialysis were recorded as receiving hemodialysis treatment at the time of arrest. Compared with nondialysis patients, patients on dialysis were more likely to be at a teaching hospital with trauma and cardiac surgery capabilities (Table 2).
Table 1.
Characteristics of patients on dialysis and matched nondialysis controls
| Characteristic | Patients on Dialysis | Nondialysis Patients |
|---|---|---|
| (n=8498) | (n=22,646) | |
| Demographics | ||
| Age, yr, median (IQR) | 66 (5674) | 67 (5775) |
| Male | 4770 (56) | 12,925 (57) |
| Race | ||
| White | 4354 (51) | 12,851 (57) |
| Black | 3217 (38) | 7929 (35) |
| Asian/Pacific Islander | 55 (0.6) | 87 (0.4) |
| American Indian/Eskimo | 27 (0.3) | 41 (0.2) |
| Hispanic | 508 (6) | 846 (4) |
| Other | 323 (4) | 842 (4) |
| Cardiac arrest characteristics | ||
| Initial rhythm | ||
| Ventricular fibrillation/pulseless ventricular tachycardia | 1533 (20) | 4298 (21) |
| Asystole/PEA | 6226 (80) | 16,461 (79) |
| Location of arrest | ||
| Intensive care unit | 3889 (46) | 10,657 (47) |
| Monitored unit | 1517 (18) | 3767 (17) |
| Nonmonitored unit | 1602 (19) | 3847 (17) |
| Arrest at night (11pm–7am) | 2792 (36) | 7315 (36) |
| Arrest on weekend or holiday | 2593 (31) | 7199 (32) |
| Arrest on weekend | 2453 (29) | 6849 (30) |
| Illness category | ||
| Medical, cardiac | 2591 (31) | 7804 (345) |
| Medical, noncardiac | 4363 (51) | 10,056 (44) |
| Surgical, cardiac | 446 (5) | 1610 (7) |
| Surgical, noncardiac | 1041 (12) | 2572 (11) |
| Preexisting conditions | ||
| Myocardial infarction (this admission) | 1175 (14) | 3847 (17) |
| Myocardial infarction (prior admission) | 1661 (20) | 3635 (16) |
| Arrhythmia | ||
| Congestive heart failure (this admission) | 1570 (19) | 3946 (17) |
| Congestive heart failure (prior admission) | 2417 (29) | 4791 (21) |
| Diabetes mellitus | 4404 (52) | 7179 (32) |
| Malignancy | 497 (6) | 3043 (13) |
| Stroke | 352 (4) | 961 (4) |
| Respiratory insufficiency | 3117 (37) | 9757 (43) |
| Pneumonia | 906 (11) | 3033 (13) |
| Hepatic insufficiency | 533 (6) | 1644 (7) |
| Septicemia | 1933 (23) | 3542 (16) |
| Metabolic/electrolyte abnormality | 1705 (20) | 3558 (16) |
| Interventions in place at the time of event | ||
| Vascular access | 4123 (92) | 11,150 (92) |
| Arterial catheter | 669 (8) | 2306 (10) |
| Vasodilators | 2022 (24) | 5761 (25) |
| Hemodialysis | 1582 (19) | N/A |
| Invasive airway | 1923 (3) | 6794 (30) |
Data displayed as N (%) unless specified otherwise.
IQR, interquartile range; PEA, pulseless electrical activity; N/A, not applicable.
Figure 2.
Percent of patients with in-hospital cardiac arrest by day of the week, nondialysis versus patients on dialysis. A higher incidence of cardiac arrests on Mondays and Tuesdays was observed among patients on dialysis (P<0.001).
Table 2.
Hospital characteristics of patients on dialysis and matched nondialysis controls
| Hospital Characteristic | Patients on Dialysis | Nondialysis Patients |
|---|---|---|
| (n=8498) | (n=22,646) | |
| Hospital type | ||
| Teaching (major or minor) | 5771 (68) | 15,699 (69) |
| Trauma services (level 1, 2) | 4394 (54) | 12,023 (55) |
| Cardiac surgery capabilities | 7112 (87) | 19,183 (88) |
| Hospital bed size | ||
| Small (<250 beds) | 1382 (16) | 3457 (15) |
| Medium (250–499 beds) | 3534 (42) | 9365 (41) |
| Large (≥500 beds) | 3582 (42) | 9824 (43) |
| Nurse-to-bed ratio | ||
| <1 | 319 (4) | 791 (4) |
| ≥1, <1.5 | 1910 (23) | 4989 (22) |
| ≥1.5, <2 | 2898 (34) | 7692 (34) |
| ≥2, <2.5 | 2441 (29) | 6670 (30) |
| ≥2.5, <3 | 571 (7) | 1531 (7) |
| ≥3 | 359 (4) | 973 (4) |
| Percentage of intensive care unit beds | ||
| Low (<5%) | 1474 (17) | 3927 (17) |
| Medium (5%–10%) | 6104 (72) | 16,326 (72) |
| High (>10%) | 411 (5) | 1052 (5) |
| United States geographic region | ||
| Northeast | 1043 (12) | 2869 (13) |
| South | 4563 (54) | 12,042 (53) |
| Midwest | 2020 (24) | 5449 (24) |
| West | 872 (10) | 2286 (10) |
| Location | ||
| Urban | 8101 (95) | 21,631 (96) |
| Rural | 397 (5) | 1015 (5) |
| Ownership | ||
| Private | 873 (10) | 2319 (10) |
| Government | 1205 (14) | 3235 (14) |
| Nonprofit | 6420 (76) | 17,092 (6) |
Data displayed as N (%) unless specified otherwise.
Table 3 examines the resuscitation processes of care and outcomes for the two groups. Composite resuscitation quality was slightly lower for patients on maintenance dialysis (89% versus 90%; P<0.001) compared with nondialysis patients at GWTG-R hospitals. However, for most individual processes of care, there were no significant differences between patients on maintenance dialysis and nondialysis patients. However, compared with nondialysis patients, patients on maintenance dialysis were significantly less likely to receive a first shock in ≤2 minutes for ventricular tachycardia/ventricular fibrillation (54% versus 58%; P=0.005) and were slightly less likely to have their cardiac arrest witnessed or monitored (90% versus 91%; P<0.001). There was no difference in median duration of resuscitation for the two groups.
Table 3.
Resuscitation processes of care and outcomes of patients on dialysis and matched nondialysis controls
| Outcome | Patients on Dialysis | Nondialysis Patients | P Value |
|---|---|---|---|
| n=8498 | n=22,646 | ||
| Processes of care | |||
| Device confirmation of correct endotracheal tube placement | |||
| Eligible patients | 5164 (61) | 11,818 (52) | <0.001 |
| Received measure among eligible patients | 4671 (91) | 10,708 (91) | 0.75 |
| Percent pulseless cardiac events monitored or witnessed | |||
| Eligible patients | 7675 (90) | 20,562 (90) | 0.19 |
| Received measure among eligible patients | 6936 (90) | 18,893 (92) | <0.001 |
| Time to first chest compressions ≤1 min | |||
| Eligible patients | 7490 (88) | 19,696 (87) | 0.006 |
| Received measure among eligible patients | 7011 (94) | 18,467 (94) | 0.64 |
| Time to first shock ≤2 mins for ventricular fibrillation/ventricular tachycardia | |||
| Eligible patients | 1412 (17) | 3950 (17) | 0.09 |
| Received measure among eligible patients | 761 (54) | 2299 (58) | 0.005 |
| Time to IV/IO epinephrine/vasopressin bolus administered to pulseless adults ≤5 mins | |||
| Eligible patients | 5041 (59) | 13,220 (58) | 0.13 |
| Received measure among eligible patients | 4159 (83) | 11,061 (84) | 0.06 |
| Processes of care composite measure (Mean±SD) | 88.9±19.0 | 89.7±18.6 | <0.001 |
| Duration of resuscitation, min, median (IQR) | 16 (8–26) | 16 (8–27) | 0.55 |
| Unadjusted outcomes | |||
| Acute survival (return of spontaneous circulation), % | 5820 (69) | 14,054 (62) | <0.001 |
| Survival to discharge, % | 1958 (23) | 5077 (22) | 0.24 |
| Favorable neurologic status (cerebral performance category 1 or 2), % | 1344 (17) | 3394 (16) | 0.07 |
IV/IO, intravenous/intraosseous; IQR, interquartile range.
Compared with nondialysis patients, patients on dialysis had higher unadjusted acute survival rates (69% versus 62%; P<0.001) but similar survival to discharge (23% versus 22%; P=0.24) and favorable neurologic survival (17% versus 16%; P=0.07). Table 4 compares outcomes for patients on maintenance dialysis with nondialysis patients after adjustment for potential confounders. After adjustment for patient characteristics, comorbidities, and cardiac arrest characteristics, patients on dialysis had similar odds of survival to discharge (odds ratio [OR], 1.05; 95% confidence interval [95% CI], 0.97 to 1.12) compared with nondialysis patients. However, patients on dialysis had significantly higher odds of acute survival (return of spontaneous circulation) (OR, 1.33; 95% CI, 1.26 to 1.40) and favorable neurologic status on discharge (OR, 1.12; 95% CI, 1.04 to 1.22) compared with nondialysis patients. Further adjustment for hospital characteristics and CPR process measures did not significantly alter associations with outcomes.
Table 4.
Unadjusted and adjusted outcomes after in-hospital cardiac arrest for patients on dialysis compared with nondialysis patients
| Odds Ratio (95% CI) | P Value | |
|---|---|---|
| Survival to discharge | ||
| Unadjusted | 1.04 (0.97 to 1.12) | 0.27 |
| Adjusted for demographic + comorbidities + cardiac arrest characteristics | 1.04 (0.97 to 1.12) | 0.29 |
| + Hospital characteristics | 1.05 (0.97 to 1.12) | 0.31 |
| + CPR process measures | 1.05 (0.97 to 1.13) | 0.25 |
| Acute survival (return of spontaneous circulation) | ||
| Unadjusted | 1.34 (1.27 to 1.41) | <0.001 |
| Adjusted for demographic + comorbidities + cardiac arrest characteristics | 1.32 (1.25 to 1.39) | <0.001 |
| + Hospital characteristics | 1.32 (1.25 to 1.40) | <0.001 |
| + CPR process measures | 1.33 (1.26 to 1.40) | <0.001 |
| Good neurologic status on hospital discharge | ||
| Unadjusted | 1.07 (1.00 to 1.16) | 0.06 |
| Adjusted for demographic + comorbidities + cardiac arrest characteristics | 1.12 (1.03 to 1.21) | 0.01 |
| + Hospital characteristics | 1.12 (1.03 to 1.21) | 0.01 |
| + CPR process measures | 1.12 (1.04 to 1.22) | 0.01 |
95% CI, 95% confidence interval; CPR, cardiopulmonary resuscitation.
Additional sensitivity analyses including kidney insufficiency as a covariate in the adjusted models did not significantly alter relationships with the outcomes, with the exception of survival to hospital discharge; the association between status of patients on maintenance dialysis and survival was strengthened (OR, 1.20; 95% CI, 1.10 to 1.31).
Discussion
In our study, we found that patients on maintenance dialysis and nondialysis patients experiencing in-hospital cardiac arrest had similar resuscitation quality for several individual process measures including endotracheal tube confirmation, time to first chest compressions, and timely administration of epinephrine/vasopressin. However, some quality measures warrant further attention. Patients on dialysis were less likely to receive a timely first defibrillation for a shockable rhythm compared with case-matched nondialysis patients. Patients on dialysis were also slightly less likely to have a witnessed or monitored event. Despite of these gaps in quality, patients on maintenance dialysis had similar to improved survival outcomes compared with nondialysis patients after accounting for differences in clinical comorbidities, demographics, and cardiac arrest characteristics.
Prior studies have examined incidence rates of in-hospital cardiac arrest among patients on dialysis and have compared outcomes with nondialysis patients (5,6). For this analysis, we utilized the AHA’s GWTG-R registry, which captures consecutive data on in-hospital cardiac arrest for approximately 6% of the nation’s hospitals. Other studies have used Medicare billing claims data to examine incidence and outcomes of CPR in hospitals, but have not examined any differences in resuscitation care (5,6). In addition, these previous studies depended on ICD-9 CPR diagnosis and procedure billing codes to identify in-hospital cardiac arrest, which have been shown to have low reliability and low sensitivity. A recent study found that 60% of confirmed in-hospital cardiac arrest events had no associated CPR procedure billing code, and one third of events had no procedure code or diagnosis code for CPR (20). Additionally, the presence or absence of CPR billing codes had a significant confounding effect on survival; survival outcomes were different among patients with submitted CPR diagnosis (28%) or procedure codes (16%) compared with those without (12%), suggesting underreporting of CPR events with poor outcomes (20).
Despite a higher level of overall comorbidity, we found that adjusted survival to discharge was not worse among patients on dialysis compared with nondialysis patients, and secondary outcomes were significantly better after accounting for clinical comorbidities and cardiac arrest characteristics. Although the overall survival to discharge rate in our study (23%) is in line with overall in-hospital cardiac arrest survival rates reported by previous studies (21%–25%) (5,6), the finding of similar survival outcomes is surprising given a prior study demonstrating worse in-hospital mortality after in-hospital cardiac arrest for patients on maintenance dialysis compared with unmatched nondialysis patients (5). The prior study used administrative billing data (ICD-9 diagnosis and procedure codes) from the National Inpatient Sample to identify patients with ESKD and all patients undergoing CPR during a hospitalization. Our analysis results may differ because (1) we utilized Medicare beneficiary files to verify that patients were ESKD patients (as opposed to patients with AKI) on maintenance dialysis before in-hospital cardiac arrest admission; (2) we did not restrict our analysis to events identified by CPR procedure billing codes, which has been shown to be associated with significantly higher survival (20); and (3) we case-matched on several characteristics, including year of in-hospital cardiac arrest and hospital, to reduce important sources of confounding not addressed by prior studies. Our observation of improved survival outcomes in patients on dialysis may relate to the increased frequency of electrolyte and fluid balance disturbances implicated in cardiac arrest among patients on dialysis (4), which are inciting factors that may be more readily reversible compared with factors leading to in-hospital cardiac arrest in nondialysis patients.
To our knowledge, our study offers the first in-depth examination of granular resuscitation practices and quality for patients on maintenance dialysis after in-hospital cardiac arrest. A recent analysis demonstrated the association between improved resuscitation quality and survival to discharge. For every 10% point increase in a hospital’s composite resuscitation performance, there was a 22% higher adjusted odds of risk standardized survival (13). In our analysis, we found that patients on dialysis had slightly lower overall resuscitation quality compared with case-matched nondialysis patients treated at the same hospital. Although we found that patients on dialysis were slightly less likely to be monitored or witnessed at the time of arrest (90% versus 92% among nondialysis patients), the clinical significance of this finding is uncertain. It is possible that efforts to provide focused monitoring during periods of elevated risk in this population may have value. Similar to previous studies of out-of-hospital cardiac arrest (21), we identified high-risk periods of in-hospital cardiac arrest occurring during dialysis treatment (nearly 20% of all in-hospital cardiac arrest occurred during dialysis treatment) and on the first dialysis treatment days of the week (Mondays and Tuesdays) after the long dialysis-free weekend. Further research is needed to determine whether of enhanced monitoring with cardiac telemetry during the peri- and intradialytic period could help bridge the gap in resuscitation quality between patients on dialysis and nondialysis patients.
Of clinical and statistical significance, we found that patients on dialysis were less likely to receive a timely defibrillation compared with nondialysis patients. The identified delays in defibrillation in patients on dialysis are problematic given the strong association between timely defibrillation and survival. Chan et al. (16) found a 50% reduction in survival to discharge for patients with defibrillation delays beyond 2 minutes and more than 23% of the study cohort had >4 minutes defibrillation delays. Although the predominance of non-ventricular arrhythmias in patients on dialysis observed in our study and confirmed by other studies (22–25) may blunt the effect of improving defibrillation response times, addressing these resuscitation quality gaps could result in a greater improvement in survival for patients on dialysis.
A prior study examining the effect of duration of resuscitation found a higher survival within hospitals with longer durations of resuscitation compared with hospitals with the shorter duration of resuscitation (26). In our analysis, the mean duration of resuscitation was similar for patients on dialysis versus nondialysis patients. This finding is reassuring, given concerns that prior reports of lower survival after in-hospital cardiac arrest could have been accompanied by decreased efforts to provide appropriate therapeutic interventions owing to concerns for futility or harm, a common phenomenon among patients with kidney disease described as “renalism” (5,6,27).
Our study has several limitations. First, our study is observational and therefore cannot prove causation. Second, although GWTG-R reported on multiple comorbidities, other unmeasured factors such as baseline cardiac function and the occurrence of other cardiac events during hospitalization were not reported in GWTG-R and could have confounded the results. Third, participating hospitals in GWTG-R represents approximately 6% of hospitals in the United States and thus may not reflect standard resuscitation practice at all United States hospitals. Further, GWTG-R participating hospitals may be more interested in quality improvement than nonparticipating hospitals, and our results may not be generalizable to nonregistry hospitals. Fourth, we excluded GWTG-R patients who were identified as acute dialysis but were not captured in the Medicare database. It is possible that a small number of patients on maintenance dialysis were excluded if not yet identified in Medicare. Fifth, the linkage rate for GWTG-R and Medicare data were 63%. As a result, some patients on dialysis could have been falsely labeled as nondialysis patients. If this were the case, our observed unadjusted survival differences between the two groups would be expected to be blunted. Sixth, although we found an increase in in-hospital cardiac arrest frequency on Monday and Tuesday, we did not have granular registry information on maintenance dialysis schedule for each patient, so we cannot confirm that increased event frequency on these days was related to a longer antecedent interdialytic interval. Finally, this study did not examine long-term outcomes or quality of life. Additional studies are needed to examine these important outcomes, which would help fully inform decision-making regarding resuscitation preferences.
In conclusion, in a large national registry of in-hospital cardiac arrest, we found that survival outcomes for patients on dialysis after in-hospital cardiac arrest were similar to nondialysis patients. Although many factors should be considered in provider-patient discussions about advanced directives, our study suggests that CPR is not a futile intervention in patients on dialysis with in-hospital cardiac arrest. Our findings also present the opportunity to further improve resuscitation outcomes in patients on maintenance dialysis by improving patient monitoring and resuscitation response times during period of increased risk.
Disclosures
Dr. Chan reports receiving consulting fees from Optum Rx outside of the submitted work. Dr. Peterson reports receiving grants from Abiomed, Amgen, AstraZeneca, Bayer AG, Genentech, Janssen Pharmaceutica Products, LP, Merck and Co., Novartis, Regeneron Pharmaceuticals, Inc, Sanofi-Aventis, and the Society of Thoracic Surgeons, outside of the submitted work. Dr. Pun reports receiving consulting fees from Relypsa, Inc. outside of the submitted work. Dr. Starks is cochair of the American Heart Association GWTG-R Adult Research Task Force and reports that she receives no financial compensation for her leadership role with this task force. Dr. Boulware, Dr. Matsouaka, Dr. Stafford, Dr. Svetkey, and Dr. Wu have nothing to disclose.
Funding
Dr. Pun is supported by National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) grant 5R03DK113324. Dr. Peterson, Dr. Pun, Dr. Stafford, Dr. Svetkey, and Dr. Wu are supported by NIDDK grant P30DK096493. This work was also funded, in part, internally by the Duke Clinical Research Institute, Durham, NC.
Supplementary Material
Acknowledgments
The authors would like to thank Barbara Lytle, MS, for her project leadership. Ms. Lytle has not received compensation for her contributions, apart from their employment at the institution where this study was conducted.
All authors have been involved in the study design, analysis, and manuscript revision. All authors read and approved the final manuscript. Dr. Starks is the guarantor who accepts full responsibility for the work and the conduct of the study, had access to the data, and controlled the decision to publish.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “Reconciling Short- and Long-Term Outcomes of In-Hospital Cardiac Arrest in Patients undergoing Maintenance Dialysis,” on pages 165–167.
Supplemental Material
This article contains the following supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.05070419/-/DCSupplemental.
Supplemental Table 1. Variable definitions for clinical characteristics full listing of Get With The Guidelines-Resuscitation investigators.
Supplemental Table 2. Information on cardiac arrest by days of the week between patients on dialysis and nondialysis patients.
References
- 1.Merchant RM, Yang L, Becker LB, Berg RA, Nadkarni V, Nichol G, Carr BG, Mitra N, Bradley SM, Abella BS, Groeneveld PW; American Heart Association Get With The Guidelines-Resuscitation Investigators : Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med 39: 2401–2406, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Di Lullo L, Rivera R, Barbera V, Bellasi A, Cozzolino M, Russo D, De Pascalis A, Banerjee D, Floccari F, Ronco C: Sudden cardiac death and chronic kidney disease: From pathophysiology to treatment strategies. Int J Cardiol 217: 16–27, 2016 [DOI] [PubMed] [Google Scholar]
- 3.Eckardt KU, Gillespie IA, Kronenberg F, Richards S, Stenvinkel P, Anker SD, Wheeler DC, de Francisco AL, Marcelli D, Froissart M, Floege J; ARO Steering Committee : High cardiovascular event rates occur within the first weeks of starting hemodialysis. Kidney Int 88: 1117–1125, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Makar MS, Pun PH: Sudden cardiac death among hemodialysis patients. Am J Kidney Dis 69: 684–695, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saeed F, Adil MM, Malik AA, Schold JD, Holley JL: Outcomes of in-hospital cardiopulmonary resuscitation in maintenance dialysis patients. J Am Soc Nephrol 26: 3093–3101, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong SP, Kreuter W, Curtis JR, Hall YN, O’Hare AM: Trends in in-hospital cardiopulmonary resuscitation and survival in adults receiving maintenance dialysis. JAMA Intern Med 175: 1028–1035, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alfonzo AV, Simpson K, Deighan C, Campbell S, Fox J: Modifications to advanced life support in renal failure. Resuscitation 73: 12–28, 2007 [DOI] [PubMed] [Google Scholar]
- 8.Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, Berg RA, Nichol G, Lane-Trultt T: Cardiopulmonary resuscitation of adults in the hospital: A report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation 58: 297–308, 2003 [DOI] [PubMed] [Google Scholar]
- 9.Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D, Bossaert LL, Brett SJ, Chamberlain D, de Caen AR, Deakin CD, Finn JC, Gräsner JT, Hazinski MF, Iwami T, Koster RW, Lim SH, Huei-Ming Ma M, McNally BF, Morley PT, Morrison LJ, Monsieurs KG, Montgomery W, Nichol G, Okada K, Eng Hock Ong M, Travers AH, Nolan JP, Utstein C; Utstein Collaborators : Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update of the utstein resuscitation registry templates for out-of-hospital cardiac arrest: A statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American heart association, European resuscitation council, Australian and New Zealand council on resuscitation, heart and stroke foundation of Canada, InterAmerican heart foundation, resuscitation council of Southern Africa, resuscitation council of Asia); and the American heart association emergency cardiovascular care committee and the council on cardiopulmonary, critical care, perioperative and resuscitation. Circulation 132: 1286–1300, 2015 [DOI] [PubMed] [Google Scholar]
- 10.US Public Health Service, US Health Care Financing Administration, US National Center for Health Statistics: ICD-9-CM International Classification of Diseases, Ninth Revision, Clinical Modification, 6th Ed., Official ed., Washington, DC, US Department of Health and Human Services, Public Health Service, Health Care Financing Administration, 1996, pp 1. NCHS CD-ROM 1996, no 1. computer laser optical disc 4 3/4 in. + 1 booklet [Google Scholar]
- 11.Chan PS, Nallamothu BK, Krumholz HM, Spertus JA, Li Y, Hammill BG, Curtis LH; American Heart Association Get with the Guidelines–Resuscitation Investigators : Long-term outcomes in elderly survivors of in-hospital cardiac arrest. N Engl J Med 368: 1019–1026, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Austin PC: Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput 38: 1228–1234, 2009 [Google Scholar]
- 13.Anderson ML, Nichol G, Dai D, Chan PS, Thomas L, Al-Khatib SM, Berg RA, Bradley SM, Peterson ED; American Heart Association’s Get With the Guidelines–Resuscitation Investigators : Association between hospital process composite performance and patient outcomes after in-hospital cardiac arrest care. JAMA Cardiol 1: 37–45, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Phelan MP, Ornato JP, Peberdy MA, Hustey FM; American Heart Association’s Get With The Guidelines-Resuscitation Investigators : Appropriate documentation of confirmation of endotracheal tube position and relationship to patient outcome from in-hospital cardiac arrest. Resuscitation 84: 31–36, 2013 [DOI] [PubMed] [Google Scholar]
- 15.Brady WJ, Gurka KK, Mehring B, Peberdy MA, O’Connor RE; American Heart Association’s Get with the Guidelines (formerly, NRCPR) Investigators : In-hospital cardiac arrest: Impact of monitoring and witnessed event on patient survival and neurologic status at hospital discharge. Resuscitation 82: 845–852, 2011 [DOI] [PubMed] [Google Scholar]
- 16.Chan PS, Krumholz HM, Nichol G, Nallamothu BK; American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators : Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med 358: 9–17, 2008 [DOI] [PubMed] [Google Scholar]
- 17.Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, Neumar RW, O’Neil BJ, Paxton JH, Silvers SM, White RD, Yannopoulos D, Donnino MW: Part 7: Adult advanced cardiovascular life support: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 132[Suppl 2]: S444–S464, 2015 [DOI] [PubMed] [Google Scholar]
- 18.Peterson ED, DeLong ER, Masoudi FA, O’Brien SM, Peterson PN, Rumsfeld JS, Shahian DM, Shaw RE: ACCF/AHA 2010 position statement on composite measures for healthcare performance assessment: A report of American College of Cardiology foundation/American heart association task force on performance measures (writing committee to develop a position statement on composite measures). J Am Coll Cardiol 55: 1755–1766, 2010 [DOI] [PubMed] [Google Scholar]
- 19.Foley RN, Gilbertson DT, Murray T, Collins AJ: Long interdialytic interval and mortality among patients receiving hemodialysis. N Engl J Med 365: 1099–1107, 2011 [DOI] [PubMed] [Google Scholar]
- 20.Khera R, Spertus JA, Starks MA, Tang Y, Bradley SM, Girotra S, Chan PS: Administrative codes for capturing in-hospital cardiac arrest. JAMA Cardiol 2: 1275–1277, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bleyer AJ, Hartman J, Brannon PC, Reeves-Daniel A, Satko SG, Russell G: Characteristics of sudden death in hemodialysis patients. Kidney Int 69: 2268–2273, 2006 [DOI] [PubMed] [Google Scholar]
- 22.Lafrance JP, Nolin L, Senécal L, Leblanc M: Predictors and outcome of cardiopulmonary resuscitation (CPR) calls in a large haemodialysis unit over a seven-year period. Nephrol Dial Transplant 21: 1006–1012, 2006 [DOI] [PubMed] [Google Scholar]
- 23.Wong MC, Kalman JM, Pedagogos E, Toussaint N, Vohra JK, Sparks PB, Sanders P, Kistler PM, Halloran K, Lee G, Joseph SA, Morton JB: Temporal distribution of arrhythmic events in chronic kidney disease: Highest incidence in the long interdialytic period. Heart Rhythm 12: 2047–2055, 2015 [DOI] [PubMed] [Google Scholar]
- 24.Roberts PR, Zachariah D, Morgan JM, Yue AM, Greenwood EF, Phillips PC, Kalra PA, Green D, Lewis RJ, Kalra PR: Monitoring of arrhythmia and sudden death in a hemodialysis population: The CRASH-ILR Study. PLoS One 12: e0188713, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roy-Chaudhury P, Tumlin JA, Koplan BA, Costea AI, Kher V, Williamson D, Pokhariyal S, Charytan DM; MiD investigators and committees : Primary outcomes of the Monitoring in Dialysis Study indicate that clinically significant arrhythmias are common in hemodialysis patients and related to dialytic cycle. Kidney Int 93: 941–951, 2018 [DOI] [PubMed] [Google Scholar]
- 26.Goldberger ZD, Chan PS, Berg RA, Kronick SL, Cooke CR, Lu M, Banerjee M, Hayward RA, Krumholz HM, Nallamothu BK; American Heart Association Get With The Guidelines—Resuscitation (formerly National Registry of Cardiopulmonary Resuscitation) Investigators : Duration of resuscitation efforts and survival after in-hospital cardiac arrest: An observational study. Lancet 380: 1473–1481, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chertow GM, Normand SL, McNeil BJ: “Renalism”: Inappropriately low rates of coronary angiography in elderly individuals with renal insufficiency. J Am Soc Nephrol 15: 2462–2468, 2004 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.