Abstract
This study assesses the effects of self-dousing and foot immersion on heart rate, core temperature, and thermal discomfort of healthy volunteers randomized to simulated hot and humid vs nonhumid conditions.
Air conditioning1 and electric fans2 are used to mitigate physiological strain during extreme heat exposure but may not always be available.3 Drinking water is commonly recommended4; however, when applied externally, water also can reduce body heat via evaporation from the skin or conduction when body parts with high surface-area-to-mass ratio are submerged. We assessed whether a self-dousing or a foot immersion intervention mitigated increases in cardiovascular (heart rate) and thermal (core temperature) strain and dehydration during conditions simulating hot, humid and very hot, dry heat waves.
Methods
After University of Sydney ethics approval, written consent was obtained from student volunteers. Three interventions were tested. For the control intervention, participants consumed 0.25 L of 22°C (72°F) water every 30 minutes. Additional interventions were (1) foot immersion: water consumption plus submersion of lower legs to mid-calf into 40 L of water maintained at 22°C (72°F) for 20 minutes, followed by 10 minutes out, then repeated or (2) self-dousing: external application of water maintained at 22°C (72°F) across the chest, arms, back, legs, and face with a sponge following the instructions “wet your skin whenever you start feeling warm.” Each intervention lasted 120 minutes and was conducted in a climate chamber under either hot, humid (40°C [104°F], 50% relative humidity) or very hot, dry (47°C [117°F], 10% relative humidity) conditions. Interventions were separated by more than 48 hours. Within each environmental condition, the order of the interventions was randomized.
Outcomes were core (rectal) temperature and heart rate (3-lead electrocardiography) measured continuously, whole-body sweat rate (determined using preintervention to postintervention changes in body mass measured on a platform scale), and whole-body thermal discomfort (assessed every 15 minutes using a visual analog scale with anchors at 0 mm [not uncomfortable], 40 mm [slightly uncomfortable], 80 mm [uncomfortable], and 120 mm [very uncomfortable]). The mean of each outcome variable during the last hour of exposure was analyzed within environmental conditions using 1-way repeated analysis of variance with Sidak post hoc testing. The significance threshold used was P = .05. Version 26 of SPSS software (IBM) was used for all analyses. Clinical significance was defined using a difference in heart rate of 5/min, which can detect variations in heart failure outcomes, and a difference of 125 g/h in whole-body sweat rate, which is used to determine fluid requirements for soldiers.
Results
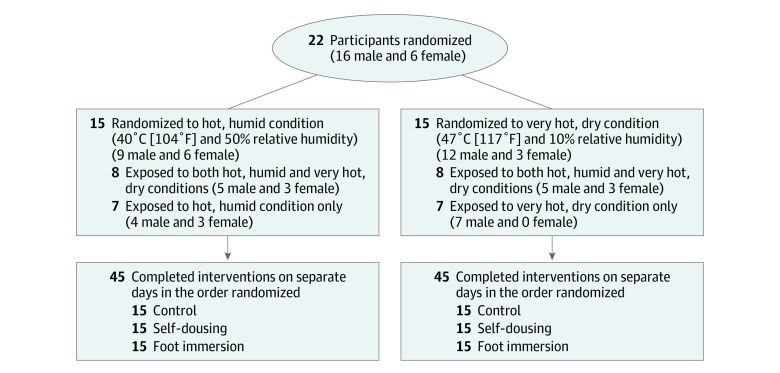
Of 22 volunteers, 8 participated in both environmental exposure conditions and 14 in 1 environmental condition. There were 15 participants for each environmental condition (mean age, 28 [SD, 5] years; exposure to hot, humid conditions: 40% female and mean body mass index [BMI; calculated as weight in kilograms divided by height in meters squared], 24.0 [SD, 2.5]; exposure to very hot, dry conditions: 20% female and mean BMI, 25.5 [SD, 3.1]; Figure). No significant differences in outcome variables were observed at rest.
Figure. Flow of Participants Through the Study.
In the comparison of the foot immersion vs control interventions during exposure to hot, humid conditions, the whole-body sweat rate was significantly lower (114 g/h vs 179 g/h, respectively; difference, −66 g/h [95% CI, −109 to −23 g/h]; P = .003) and the thermal discomfort level was lower (45 mm vs 66 mm; difference, −21 mm [95% CI, −39 to −3 mm]; P = .02); however, heart rate was not (75/min vs 80/min; difference, −5/min [95% CI, −11/min to 1/min]; P = .14). The findings for whole-body sweat rate and heart rate were similar under very hot, dry conditions, but thermal discomfort was not significant (Table).
Table. Outcome Variables at Baseline and During the Last Hour of Simulated Heat Wave Exposure and Comparisons Between the Interventions.
| Type of Simulated Heat Wave Exposure | ||||||
|---|---|---|---|---|---|---|
| Hot, Humid Conditions (40°C [104°F] and 50% Relative Humidity) | Very Hot, Dry Conditions (47°C [117°F] and 10% Relative Humidity) | |||||
| Control | Foot Immersion | Self-Dousing | Control | Foot Immersion | Self-Dousing | |
| Outcome Variables at Baseline, Mean (SD) | ||||||
| Rectal temperature, °C | 37.2 (0.4) | 37.2 (0.3) | 37.2 (0.3) | 37.0 (0.3) | 37.1 (0.4) | 37.1 (0.4) |
| Heart rate, /min | 69 (13) | 70 (10) | 69 (9) | 66 (13) | 65 (11) | 65 (9) |
| Whole-body thermal discomfort, mm | 6 (9) | 14 (16) | 4 (7) | 3 (10) | 1 (3) | 5 (19) |
| Outcome Variables During Last Hour of Exposure, Mean (SD) | ||||||
| Rectal temperature, °C | 37.4 (0.2) | 37.3 (0.2) | 37.3 (0.2) | 37.3 (0.3) | 37.4 (0.4) | 37.4 (0.4) |
| Heart rate, /min | 80 (11) | 75 (10) | 75 (9) | 78 (13) | 76 (12) | 74 (12) |
| Whole-body thermal discomfort, mm | 66 (33) | 45 (24) | 38 (30) | 58 (27) | 44 (27) | 33 (27) |
| Whole-body sweat rate, g/h | 179 (53) | 114 (40) | 93 (46) | 330 (43) | 257 (44) | 119 (56) |
| Between-Group Differences in Outcomes During Last Hour of Exposure (95% CI) | ||||||
|
Self-Dousing
Minus Foot Immersion |
Foot
Immersion Minus Control |
Self-Dousing
Minus Control |
Self-Dousing
Minus Foot Immersion |
Foot
Immersion Minus Control |
Self-Dousing
Minus Control |
|
| Rectal temperature, °C | 0 (−0.2 to 0.2) | 0 (−0.2 to 0.1) | 0 (−0.2 to 0.1) | 0 (−0.2 to 0.2) | 0.1 (−0.1 to 0.3) | 0.1 (−0.1 to 0.2) |
| P value | >.99 | .94 | .94 | >.99 | .57 | .49 |
| Heart rate, /min | 0 (−5 to 4) | −5 (−11 to 1) | −5 (−10 to 0) | −2 (−6 to 2) | −2 (−5 to 1) | −4 (−8 to −1) |
| P value | >.99 | .14 | .04 | .41 | .26 | .02 |
| Whole-body thermal discomfort, mm | −6 (−24 to 11) | −21 (−39 to −3) | −27 (−49 to −6) | −10 (−21 to 0) | −14 (−31 to 3) | −24 (−40 to −9) |
| P value | .70 | .02 | .01 | .05 | .13 | .003 |
| Whole-body sweat rate, g/h | −21 (−72 to 31) | −66 (−109 to −23) | −87 (−144 to −29) | −137 (−179 to −96) | −73 (−99 to −47) | −210 (−256 to −165) |
| P value | .64 | .003 | .004 | <.001 | <.001 | <.001 |
In the comparison of the self-dousing vs control interventions during exposure to hot, humid conditions, heart rate was significantly lower (75/min vs 80/min, respectively; difference, −5/min [95% CI, −10/min to 0/min]; P = .04) as well as the whole-body sweat rate (93 g/h vs 179 g/h; difference, −87 g/h [95% CI, −144 to −29 g/h]; P = .004) and thermal discomfort level (38 mm vs 66 mm; difference, −27 mm [95% CI, −49 to −6 mm]; P = .01). Results were similar under very hot, dry conditions.
In the comparison of the self-dousing vs foot immersion intervention during exposure to very hot, dry conditions, the whole-body sweat rate and thermal discomfort level were lower with self-dousing; however, no differences between interventions were observed under hot, humid conditions. No differences in core temperature or effects of intervention order for any outcome were found.
The reductions in heart rate with the foot immersion and self-dousing interventions attained clinical significance in hot, humid conditions as did the reductions in whole-body sweat rate with self-dousing in very hot, dry conditions.
Discussion
In this preliminary study, foot immersion lowered sweating during exposure to both environmental conditions and lowered thermal discomfort only in hot, humid conditions. The self-dousing intervention lowered heart rate, sweating, and thermal discomfort under both environmental conditions and was more effective than the foot immersion intervention at reducing sweating and thermal discomfort in very hot, dry conditions. Core temperature was unaltered. However, morbidity and mortality from dehydration and cardiovascular failure during heat waves typically surpass those from hyperthermia alone.5 Limitations include testing of only a small number of healthy volunteers. Responses must be evaluated among older adults and among those who have health conditions, are taking medications, or both, which could potentially disrupt thermoregulation.6
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.Friedrich MJ. Tracking progress on mitigating health effects of climate change. JAMA. 2019;321(3):238. doi: 10.1001/jama.2018.21621 [DOI] [PubMed] [Google Scholar]
- 2.Ravanelli NM, Hodder SG, Havenith G, Jay O. Heart rate and body temperature responses to extreme heat and humidity with and without electric fans. JAMA. 2015;313(7):724-725. doi: 10.1001/jama.2015.153 [DOI] [PubMed] [Google Scholar]
- 3.Anderson GB, Bell ML. Lights out: impact of the August 2003 power outage on mortality in New York, NY. Epidemiology. 2012;23(2):189-193. doi: 10.1097/EDE.0b013e318245c61c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wellenius GA, Eliot MN, Bush KF, et al. Heat-related morbidity and mortality in New England: evidence for local policy. Environ Res. 2017;156:845-853. doi: 10.1016/j.envres.2017.02.005 [DOI] [PubMed] [Google Scholar]
- 5.Fouillet A, Rey G, Laurent F, et al. Excess mortality related to the August 2003 heat wave in France. Int Arch Occup Environ Health. 2006;80(1):16-24. doi: 10.1007/s00420-006-0089-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Semenza JC, McCullough JE, Flanders WD, McGeehin MA, Lumpkin JR. Excess hospital admissions during the July 1995 heat wave in Chicago. Am J Prev Med. 1999;16(4):269-277. doi: 10.1016/S0749-3797(99)00025-2 [DOI] [PubMed] [Google Scholar]