Abstract
Despite increasing use, the exact prevalence and predictors of peripherally inserted central catheter-associated bloodstream infection (PICC-CLABSI) in hospitalized patients with cancer are not elucidated.
This retrospective cohort study included consecutive patients who underwent peripherally inserted central catheter (PICC) placement in 4 institutions (during 12 months in 3 hospitals and 10 months in 1 hospital). The prevalence of PICC-CLABSI was evaluated. The association between predictors and PICC-CLABSI were analyzed using Cox proportional hazards regression models and Kaplan-Meier survival analysis with log-rank tests.
During the study period, 539 PICCs were inserted in 484 patients for a total of 10,841 catheter days. PICC-CLABSI occurred in 25 (5.2%) patients, with an infection rate of 2.31 per 1000 catheter days. PICC for chemotherapy (hazards ratio [HR] 11.421; 95% confidence interval (CI), 2.434–53.594; P = .019), double lumen catheter [HR 5.466; 95% CI, 1.257–23.773; P = .007], and PICC for antibiotic therapy [HR 2.854; 95% CI, 1.082–7.530; P = .019] were associated with PICC-CLABSI.
PICC for chemotherapy or antibiotics, and number of catheter lumens are associated with increased risk of PICC-CLABSI in cancer patients. Careful assessment of these factors might help prevent PICC-CLABSI and improve cancer patients care.
Keywords: catheterisation, catheter-related infections, central venous, neoplasms
1. Introduction
Utilization of central venous catheter plays a key role in managing hospitalized cancer patients.[1–4] Currently, peripherally inserted central catheter (PICC) is the most common central venous catheter used in inpatient setting.[5,6] However, the growing use of PICCs creates new insights of hospital infection.[7] An often and serious complication of PICC is central line associated bloodstream infection (CLABSI).[8,9] CLABSI is an important and preventable cause of morbidity and mortality in hospitalized patients;[10] it results in increased healthcare cost and duration of patients’ hospital stay.[11] Patients with cancer are particularly susceptible to infection, as they are often immune-compromised and have a high burden of comorbidities.[4]
Historically, PICCs are known to be safer than other central lines regarding infection, possibly due to lower bacterial density and lower temperature of the PICC placement site compared with the placement sites of other central venous catheters which include neck and groin.[12] However, recent data suggest that PICC-associated blood stream infection (PICC-CLABSI) rates vary among different patient groups and are actually similar to or even exceed blood stream infection rates of other central venous catheters.[13] Few studies have investigated PICC-CLABSI predictors in patients with cancer, especially adults.[14,15]
To better understand PICC-related risk in patients with cancer and improve cancer patient's safety, the factors associated with an adverse clinical outcome must be elucidated. Therefore, the purpose of this study was to evaluate the prevalence and predictors of PICC-CLABSI in a large cohort of patients with cancer.
2. Methods
2.1. Study design and data collection
The institutional review boards of 4 institutions approved this study, and informed patient consent was waived. Medical records of consecutive adult hospitalized patients who underwent PICC placement between 1st January and 31st October 2017 in 1 hospital (National Cancer Center of Korea) and between 1st October 2016 and 30th September 2017 in the other hospitals (Hanyang University Guri Hospital, The Catholic University of Korea Incheon St. Mary's Hospital, and the Catholic University of Korea Bucheon St. Mary's Hospital) were collected from the electronic medical record database in each institution. The study period of 1 hospital (National Cancer Center of Korea) differed from that of the other hospitals because active surveillance data for all admitted patients was available in that hospital from 1st January 2017. When an individual patient had more than one PICC placed during the study period, each session was considered as a separate event. Exclusion criteria were: patients transferred or who had indwelling times of PICC less than 2 days, or those who lacked information regarding the insertion or removal date of PICC.
2.2. PICC insertion and management
All the procedures and management followed the Korean Nosocomial Infection Surveillance and Prevention Protocol[16] and United States guidelines for preventing catheter-related infections.[17] Single or double 4 to 5 French (Fr) lumen PICC catheters (PowerPICC, Bard Access Systems Inc.; Turbo-Ject PICC, Cook Medical) were used in this study. All the catheters were inserted by trained interventional radiologists who followed routine protocol, using the smallest caliber of catheters in the largest vein available. The procedures were performed in a dedicated angiography suite. Each catheter placement was performed under ultrasound and fluoroscopy guidance, following maximal evidence-based aseptic protocol of each institution. The opposite side of the dominant upper arm anteromedial surface was the preferred location to insert the catheter unless there were clinical contraindications (eg, previous axillary operation or radiotherapy, arm edema, or arteriovenous fistula for dialysis access). At the end of the procedure, the location of the catheter tip was carefully assessed using fluoroscopy to determine if it was placed properly at the cavo-atrial junction. Regular device checks and insertion-site care entailed weekly changing of the film-covered dressing and a new gauze application every other day in all cases.
2.3. Definition and variables
The National Healthcare Safety Network surveillance definition of PICC-CLABSI was used.[8,18] In brief, PICC-CLABSI is a primary bloodstream infection in a patient who has had a PICC in place for > 2 days and has a recognized pathogen (identified from 1 or more blood specimens by a culture- or non-culture-based microbiologic test. The non-culture-based microbiologic test was defined as causative bacterial detection method using microbial antigen, RNA or DNA, such as immunoassays or nucleic acid amplification test.) that is not related to an infection at another site. The prevalence of PICC-CLABSI was calculated as percentage and rate per catheter day.[3]
PICC-use related covariates were evaluated using a conceptual model of predictors of PICC complications.[19] In brief, conceptual model consists of patient, device, and provider factors that can influence PICC-related complications. Intensive Care Unit (ICU) status was defined as patients who required any ICU care within 1 month prior to or after catheter insertion. The indication for PICC placement was based on the initial indications of catheter insertion, such as poor venous access, parenteral nutrition, administration of antibiotics, or intravenous chemotherapy. The dwell time of a PICC was calculated in days by subtracting the date of a PICC removal from the date of its placement. Three reviewers evaluated these data in consensus to ensure agreement on assignment.
2.4. Statistical analysis
Each PICC-placement was regarded as a separate unit in all the statistical analyses. Predictors of PICC-CLABSI were investigated by univariable Cox proportional hazard tests first, and then by using a full multivariable model with P values < .10 to evaluate hazards ratio (HRs) and 95% confidence interval (CI). Kaplan-Meier survival analysis with log-rank test was performed for candidate predictor derived from the multivariable models. Statistical significance was set at P< .05. SPSS for Windows (v18.0; SPSS Inc.) was used for analysis.
3. Results
3.1. Patient characteristics and clinical outcome
During study period, a total of 539 PICCs inserted in 484 patients for a total of 10,841 catheter days were enrolled (Fig. 1). PICC-CLABSI occurred in 25 (5.2%) patients, with an infection rate of 2.31 per 1000 catheter days. Most of the patients had solid tumor (n = 465; 96.1%) and 19 patients had a hematologic malignancy (3.9%). All the patients with PICC-CLABSI had solid tumors.
Figure 1.
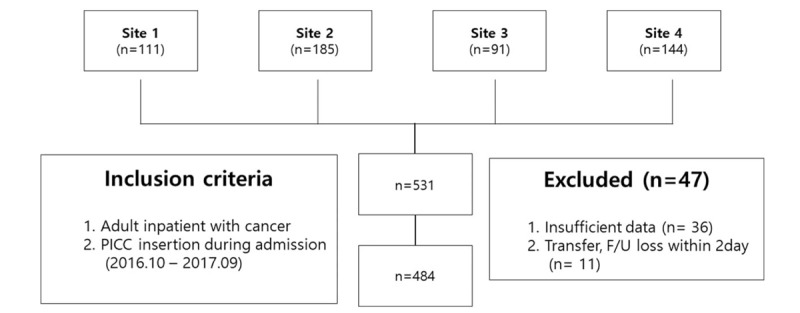
Study flow diagram.
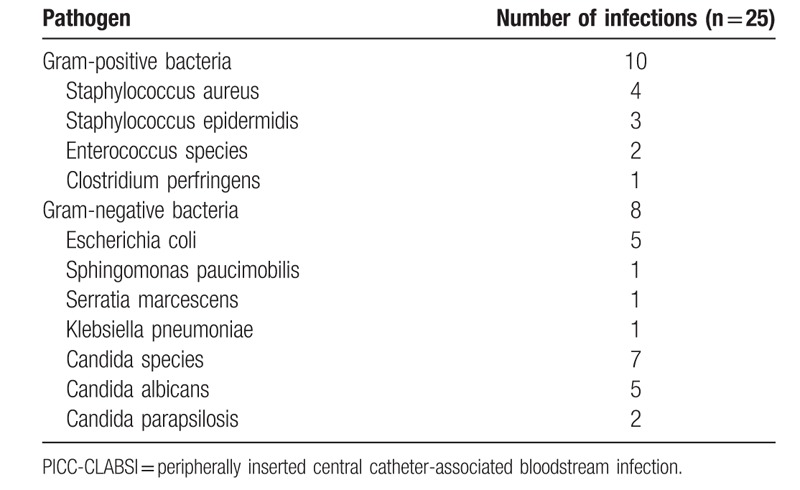
Table 1 demonstrates descriptive statistics for Predictors of PICC-CLABSI according to PICC-CLABSI Status. The mean hospital stays of the non-CLABSI group and CLABSI group were 39.8 days [range 2–575], and 64.4 days [13–210], respectively. Most of the catheters in the CLABSI group were double-lumen devices (92.0%; n = 23). The common causative microorganism of PICC-CLABSI was Candida species (n = 7) and Escherichia coli (n = 5) (Table 2).
Table 1.
Descriptive Statistics for Patient, Device, and Provider Predictors of PICC-CLABSI according to PICC-CLABSI Status.
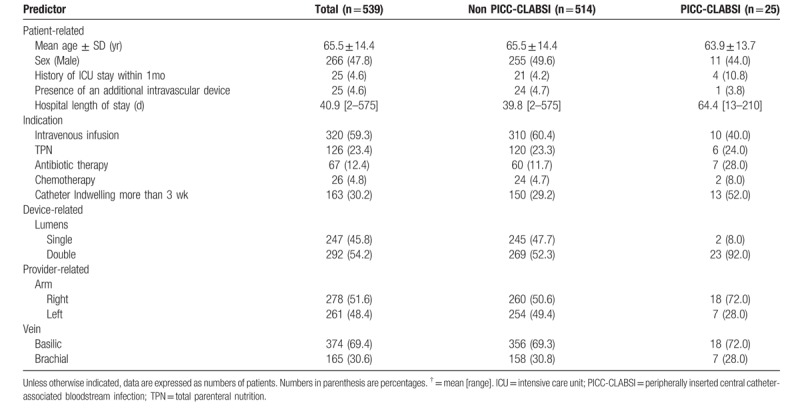
Table 2.
Microbiology of PICC-CLABSI.
3.2. Risk factors of PICC-CLABSI
Table 3 shows univariable and multivariable Cox analysis of predictors of PICC-CLABSI. Multivariable analysis showed that the risk of PICC-CLABSI was significantly associated with indication for chemotherapy (HR 11.421; 95% CI, 2.434–53.594), double lumen catheter (HR 5.466; 95% CI, 1.257–23.773), and indication for antibiotics delivery (HR 2.854; 95% CI, 1.082–7.530). Kaplan-Meier survival analysis for each derived predictor from multivariable model is presented in Figure 2A and B.
Table 3.
Univariable and multivariable Cox proportional hazards regression models of predictors of PICC-CLABSI.
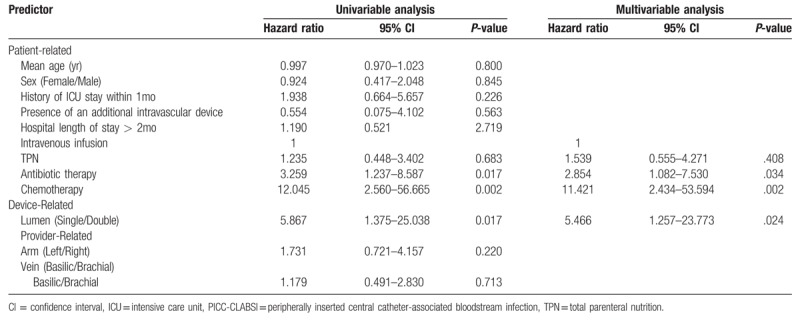
Figure 2.
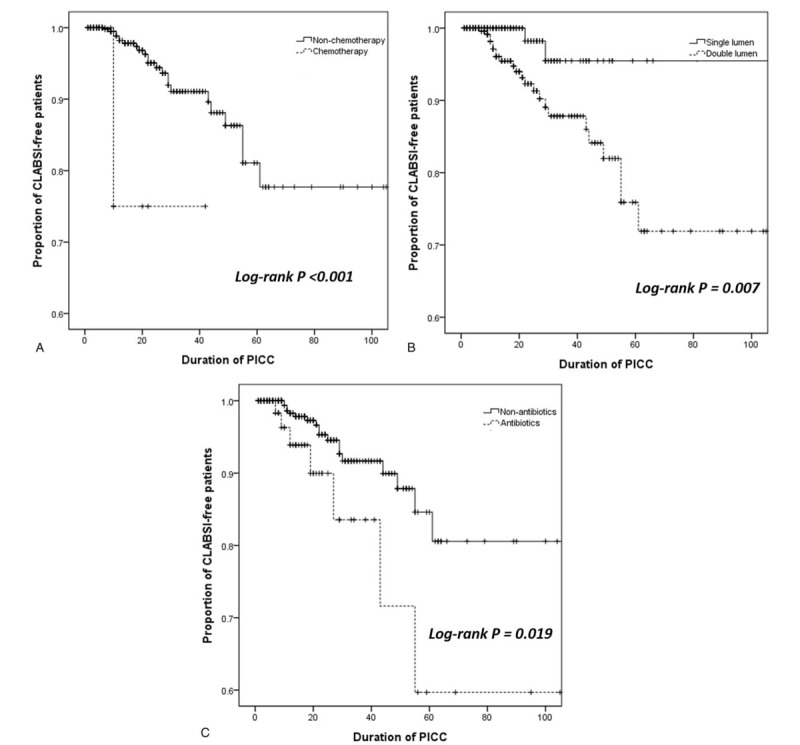
Kaplan-Meier analysis for predictors of PICC-CLABSI. 2-A; cumulative PICC-CLABSI free survival according to indwelling time of chemotherapy versus non-chemotherapy. 2-B; cumulative PICC-CLABSI free survival according to indwelling time of single lumen versus double lumen. 2-C; cumulative PICC-CLABSI free survival according to indwelling time of antibiotics versus non-antibiotics. PICC-CLABSI = peripherally inserted central catheter-associated bloodstream infection.
4. Discussion
The present study investigated rates and risk factors of PICC-CLABSI among patients with cancer. Although PICC has many advantages, mounting evidence suggests that the risk of PICC-CLABSI are not low.[5,13,19] In this study of 539 PICCs in cancer patients in a multicenter hospitalized setting, CLABSI rated 2.31 per 1000 catheter days. This value is higher than the value in the previous literature regarding oncology patients,[2,3,15] comparable to a previous prospective study on cancer patients[14] and hospitalized population.[1,19,20] Even in cancer patients, CLABSI rates vary among different patient settings, as 0.95 per 1000 catheter-days in cancer patients undergoing chemotherapy, 6.61 per 1000- catheter days in hematologic malignancy, and 8 per 1000-catheter day in patients with solid tumor.[2,15,21] Moreover, a recent systematic review and meta-analysis showed that PICC-CLABSI rates were actually identical to that of other central venous catheter in inpatient setting.[13] In this study, most of the patients had solid tumors and very low population had hematologic malignancy. Moreover, relatively low recruitment of ICU patients also partly had a role in our overall CLABSI rate.
Administration of chemotherapy has been described as a significant risk factor for PICC-CLABSI.[3,15] The use of totally implantable venous ports is common practice for cancer patients. In patients with cancer, the risk of totally implantable venous port related infection rates was reported from 0.20 to 0.21 per 1000 catheter-days.[22] In this study, using PICC primarily for chemotherapy showed a much higher infection rate (10.0 per 1000 catheter-days). Moreover, PICC for chemotherapy remained a significant predictor on Cox hazard model (HR 11.421), suggesting earlier time to infection. The higher rate of infection and HR are probably due to immunosuppression by diverse chemotherapeutic agents.[3]
The association between antibiotics use and development of PICC-CLABSI in cancer patients has not been well understood until now. One study regarding patients with bone infection undergoing long-term antibiotics use via PICC reported that PICC-CLABSI rate was up to 6%.[23] In this study, 7 of 67 (10.4%) patients who underwent PICC placement for antibiotics use were diagnosed with PICC-CLABSI. Kaplan-Meier estimates of PICC-CLABSI between the antibiotics-use group and the other patients showed an increase in hazard ratio (Fig. 2-C). It is speculated that during antibiotic therapy, the cause of infection itself that necessitated the antibiotics use and the deterioration of the normal flora could be a source of vulnerability to a systemic infection, such as CLABSI.
A device-related independent risk factor for PICC-CLABSI that emerged from our study is double lumen catheter. Previous studies showed the number of catheter lumen is an independent risk factor for PICC-CLABSI.[5,19,24] Chopra et al demonstrated increasing number of lumens was associated with a greater risk of and an earlier time to infection.[19] Similarly, double lumen catheter was a strong risk factor in multivariable cox hazard model (HR 5.466) in the present study. Careful assessment of necessity of PICC and efforts to use as fewer lumen as possible is mandatory to reduce complications like infection.[5,24]
Our study had several limitations; the first and major 1 is that the retrospective design of our study is subject to selection bias. However, all consecutive patients were evaluated during the study period and a multicenter setting was applied to reflect the heterogeneous patient setting in daily practice. Second, data were collected through review of medical records, therefore, susceptible to reporting bias. However, all the inpatient's data collected were followed up during the study period to minimize the risk of reporting bias. Third, immune status or disease station of each patient are thought to be meaningful in evaluating risk factors of CLABSI. However, we could not investigate each patients’ immune status or degree of disease progression by single objective criteria. However, we did investigate catheter indwelling time for each patient and compare the parameter by PICC-CLABSI status.
5. Conclusion
In conclusion, using PICC for chemotherapy or antibiotic therapy, and number of catheter lumens are associated with increased risk of PICC-CLABSI in cancer patients. Careful assessment of these factors might be helpful to prevent PICC-CLABSI and improve the care for cancer patients.
Author contributions
Conceptualization: Jae Hwan Lee, Min Uk Kim.
Data curation: Jae Hwan Lee, Min Uk Kim, Eung Tae Kim, Dong Jae Shim, Il Jung Kim, Jong Hyun Byeon, Hyun Beom Kim.
Formal analysis: Jae Hwan Lee.
Funding acquisition: Dong Jae Shim.
Investigation: Jae Hwan Lee.
Methodology: Jae Hwan Lee.
Supervision: Min Uk Kim.
Validation: Jae Hwan Lee.
Writing – original draft: Jae Hwan Lee.
Writing – review & editing: Min Uk Kim, Eung Tae Kim, Dong Jae Shim, Il Jung Kim, Jong Hyun Byeon, Hyun Beom Kim.
Min Uk Kim orcid: 0000-0003-0564-5724.
Footnotes
Abbreviations: CI = confidence interval, CLABSI = central line-associated bloodstream infection, HR = hazards ratio, PICC = peripherally inserted central catheter, PICC-CLABSI = peripherally inserted central catheter associated bloodstream infection.
How to cite this article: Lee JH, Kim MU, Kim ET, Shim DJ, Kim IJ, Byeon JH, Kim HB. Prevalence and predictors of peripherally inserted central venous catheter associated bloodstream infections in cancer patients: A multicentre cohort study. Medicine. 2020;99:6(e19056).
This research was supported by a Grant from the Korean Society of Interventional Radiology -Terumo research fund (2018). The funders had no role in this research.
Institutional review board of the 4 hospitals approved this retrospective study (Name of ethical committee, registration number).
Institutional review board of National Cancer center of Korea, NCC2019-0008
Institutional review board of Hanyang university Guri hospital, 2018–05-019-001.
The Institutional Review Board of The Catholic University of Korea Catholic Medical Center (for Incheon St.Mary's Hospital and Bucheon St.Mary's Hospital), XC18REDI0029.
The datasets generated and/or analysed during the current study are not publicly available due to protection from compromise of participant's privacy but are available from the corresponding author on reasonable request.
The authors have no conflicts of interest to disclose.
References
- [1].Ajenjo MC, Morley JC, Russo AJ, et al. Peripherally inserted central venous catheter-associated bloodstream infections in hospitalized adult patients. Infect Control Hosp Epidemiol 2011;32:125–30. [DOI] [PubMed] [Google Scholar]
- [2].Cheong K, Perry D, Karapetis C, et al. High rate of complications associated with peripherally inserted central venous catheters in patients with solid tumours. Intern Med J 2004;34:234–8. [DOI] [PubMed] [Google Scholar]
- [3].Bouzad C, Duron S, Bousquet A, et al. Peripherally inserted central catheter-related infections in a cohort of hospitalized adult patients. Cardiovasc Intervent Radiol 2016;39:385–93. [DOI] [PubMed] [Google Scholar]
- [4].Walshe LJ, Malak SF, Eagan J, et al. Complication rates among cancer patients with peripherally inserted central catheters. J Clin Oncol 2002;20:3276–81. [DOI] [PubMed] [Google Scholar]
- [5].Herc E, Patel P, Washer LL, et al. A model to predict central-line-associated bloodstream infection among patients with peripherally inserted central catheters: the MPC score. Infect Control Hosp Epidemiol 2017;38:1155–66. [DOI] [PubMed] [Google Scholar]
- [6].Parienti JJ, Mongardon N, Megarbane B, et al. Intravascular complications of central venous catheterization by insertion site. N Engl J Med 2015;373:1220–9. [DOI] [PubMed] [Google Scholar]
- [7].Chopra V, O’horo JC, Rogers MA, et al. The risk of bloodstream infection associated with peripherally inserted central catheters compared with central venous catheters in adults: a systematic review and meta-analysis. Infect Control Hosp Epidemiol 2013;34:908–18. [DOI] [PubMed] [Google Scholar]
- [8].Miller DL, O’Grady NP. Society of Interventional R. Guidelines for the prevention of intravascular catheter-related infections: recommendations relevant to interventional radiology for venous catheter placement and maintenance. J Vasc Interv Radiol 2012;23:997–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Mermel LA, Allon M, Bouza E, et al. Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis 2009;49:1–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Maki DG, Kluger DM, Crnich CJ. The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo clinic proceedings. Elsevier 2006;1159–71. [DOI] [PubMed] [Google Scholar]
- [11].Gunst M, Matsushima K, Vanek S, et al. Peripherally inserted central catheters may lower the incidence of catheter-related blood stream infections in patients in surgical intensive care units. Surgical infections 2011;12:279–82. [DOI] [PubMed] [Google Scholar]
- [12].Safdar N, Maki DG. Risk of catheter-related bloodstream infection with peripherally inserted central venous catheters used in hospitalized patients. Chest 2005;128:489–95. [DOI] [PubMed] [Google Scholar]
- [13].Chopra V, O’Horo JC, Rogers MA, et al. The risk of bloodstream infection associated with peripherally inserted central catheters compared with central venous catheters in adults: a systematic review and meta-analysis. Infect Control Hosp Epidemiol 2013;34:908–18. [DOI] [PubMed] [Google Scholar]
- [14].Mollee P, Jones M, Stackelroth J, et al. Catheter-associated bloodstream infection incidence and risk factors in adults with cancer: a prospective cohort study. J Hosp Infect 2011;78:26–30. [DOI] [PubMed] [Google Scholar]
- [15].Bertoglio S, Faccini B, Lalli L, et al. Peripherally inserted central catheters (PICCs) in cancer patients under chemotherapy: a prospective study on the incidence of complications and overall failures. J Surg Oncol 2016;113:708–14. [DOI] [PubMed] [Google Scholar]
- [16].Choi YH. Prospective nationwide healthcare-associated infection surveillance system in South Korea. J Korean Med Sci 2018;61:21–5. [Google Scholar]
- [17].Tacconelli E, Smith G, Hieke K, et al. Epidemiology, medical outcomes and costs of catheter-related bloodstream infections in intensive care units of four European countries: literature- and registry-based estimates. J Hosp Infect 2009;72:97–103. [DOI] [PubMed] [Google Scholar]
- [18].O’Grady NP, Alexander M, Burns LA, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control 2011;39:S1–34. [DOI] [PubMed] [Google Scholar]
- [19].Chopra V, Ratz D, Kuhn L, et al. PICC-associated bloodstream infections: prevalence, patterns, and predictors. Am J Med 2014;127:319–28. [DOI] [PubMed] [Google Scholar]
- [20].Pongruangporn M, Ajenjo MC, Russo AJ, et al. Patient- and device-specific risk factors for peripherally inserted central venous catheter-related bloodstream infections. Infect Control Hosp Epidemiol 2013;34:184–9. [DOI] [PubMed] [Google Scholar]
- [21].Worth LJ, Seymour JF, Slavin MA. Infective and thrombotic complications of central venous catheters in patients with hematological malignancy: prospective evaluation of nontunneled devices. Support Care Cancer 2009;17:811–8. [DOI] [PubMed] [Google Scholar]
- [22].Lebeaux D, Fernandez-Hidalgo N, Chauhan A, et al. Management of infections related to totally implantable venous-access ports: challenges and perspectives. Lancet Infect Dis 2014;14:146–59. [DOI] [PubMed] [Google Scholar]
- [23].Valbousquet Schneider L, Jr, Duron S, Arnaud FX, et al. Evaluation of PICC complications in orthopedic inpatients with bone infection for long-term intravenous antibiotics therapy. J Vasc Access 2015;16:299–308. [DOI] [PubMed] [Google Scholar]
- [24].Bozaan D, Skicki D, Brancaccio A, et al. Less lumens-less risk: a pilot intervention to increase the use of single-lumen peripherally inserted central catheters. J Hosp Med 2018;10.12788/jhm.3097. [DOI] [PubMed] [Google Scholar]


