Abstract
Background:
Endoscopic tonsillectomy is associated with postoperative pain. Postoperative pain management remains to be improved in children. We aimed to investigate oxycodone preemptive analgesia in children undergoing endoscopic plasma total adenotonsillectomy.
Methods:
166 children with adenotonsillar hypertrophy were recruited at Wuhan Children's Hospital between 08/2016 and 03/2017. They were randomly assigned to receive SPOA (postoperative sufentanil), SPEA+SPOA (preemptive sufentanil and postoperative sufentanil), and OPEA+SPOA (preemptive oxycodone and postoperative sufentanil). The primary endpoint was serum c-fos levels. The secondary endpoints were the response entropy (RE) value, Pediatric Anesthesia Emergence Delirium (PAED) score, FLACC score, and adverse events.
Results:
c-fos mRNA levels were increased significantly after surgery in the SPOA and SPEA+SPOA groups (P < .05). Postoperatively, c-fos mRNA levels were higher in the SPOA group compared with the OPEA+SPOA group (P = .044). The RE values increased in all groups after surgery (P < .05). At extubation, RE values were higher in the SPOA group compared with the SPEA+SPOA and OPEA+SPOA groups (P < .05). The PAED scores were higher in the SPOA group compared with the OPEA+SPOA group (P = .045). In the SPOA group, the FLACC scores were decreased at 24 h after surgery vs 4 hours (P = .044). Prediction probability (Pk) values indicated that RE and c-fos mRNA levels were quantitative predictors for early postoperative stress reaction after surgery.
Conclusions:
The subanalgesic dose of oxycodone (0.1 mg/kg) as preemptive analgesia could improve pain after endoscopic plasma total adenotonsillectomy in children.
Keywords: children, endoscopic plasma total adenotonsillectomy, oxycodone, postoperative pain, preemptive analgesia, reaction entropy, serum c-fos mRNA
1. Introduction
Sleep-disordered breathing (SDB) is a common health issue in China, with a prevalence of 10.1% to 17.2% for occasional SDB and 5.6% to 8.9% for regular SDB. SDB leads to symptoms like daytime sleepiness that can affect school performance and behavioral/cognitive development.[1] Adenotonsillectomy is one of the main surgical methods to manage severe cases.[2] Postoperative pain is common after endoscopic tonsillectomy in children,[3] especially after the termination of total intravenous anesthesia (TIVA) using propofol and remifentanil.[4] Sufentanil is a synthetic opioid analgesic and is commonly used for intraoperative anesthesia and postoperative intravenous analgesia.[5] Oxycodone hydrochloride is a semi-synthetic derivative of opioid alkaloid; it is a dual agonist for both μ and κ opioid receptors.[6]
The entropy value of electroencephalogram (EEG) data can be used to determine the level of sedation.[7] EEG provides two values: state entropy (SE) and response entropy (RE). SE measures the depth of hypnosis, while RE measures the depth of analgesia; therefore, RE can be considered as an indirect measure of pain.[8] The Pediatric Anesthesia Emergence Delirium (PAED) scale assesses the degree of emergence delirium.[9] The face, legs, activity, cry, and consolability (FLACC) scale is used to assess pain in children.[10] The FOS protein leads to the expression of dynorphin and is involved in postoperative pain.[11] Measuring the serum mRNA levels of c-fos (encoding FOS) can be used to evaluate pain development.[11]
Therefore, in the present randomized trial, preemptive analgesia was conducted to proactively prevent and inhibit central and peripheral postoperative pain[12] in order to manage the pain caused by tonsillectomy in patients with adenotonsillar hypertrophy. Entropy index (including preoperative and postoperative RE), PAED score, FLACC score, and serum mRNA c-fos levels were used to evaluate the efficacy of preemptive analgesia using oxycodone or sufentanil.
2. Materials and methods
2.1. Study design and patients
This manuscript adheres to the applicable CONSORT guidelines. This was a randomized controlled clinical trial, registered at www.chictr.org.cn (ChiCTR-INR-16009116, August 29, 2016). Patients with adenotonsillar hypertrophy were recruited at the Department of Otorhinolaryngology of the Wuhan Children's Hospital between August 2016 and March 2017. The study was approved by the Institutional Review Board (IRB) of the Wuhan Maternal and Child Healthcare Hospital. Written informed consent was obtained from the parents or legal guardians for minor subjects.
The inclusion criteria were:
-
1)
to 9 years of age;
-
2)
diagnosed with obstructive sleep apnea-hypopnea syndrome (moderate or less: 1≤ apnea-hypopnea index [AHI] ≤10) with or without hypoxemia (moderate or less: 75%≤ blood oxygen saturation [SpO2] ≤92%);[3]
-
3)
tonsil hypertrophy; and
-
4)
met the sleep-disordered breathing surgical criteria for adenotonsillectomy.
The exclusion criteria were:
-
1)
participated in another clinical trial within 4 weeks before enrollment;
-
2)
history of long-term narcotic or opioid use;
-
3)
allergy to opioids;
-
4)
heart diseases (degree II or more with cardiac functional insufficiency);
-
5)
with severe hypertension;[13]
-
6)
with mild to moderate hypertension, but blood pressure (BP) higher than 140/90 mmHg before medication;[13]
-
7)
hepatic or renal indexes higher than two folds of the upper limit of normal);
-
8)
drug dependency history;
-
9)
dehydration (decreased peripheral perfusion, deep breathing, decreased skin turgor, high urea, low pH, and/or large base deficit);[3] or
-
10)
developmental retardation. (Fig. 1)
Figure 1.
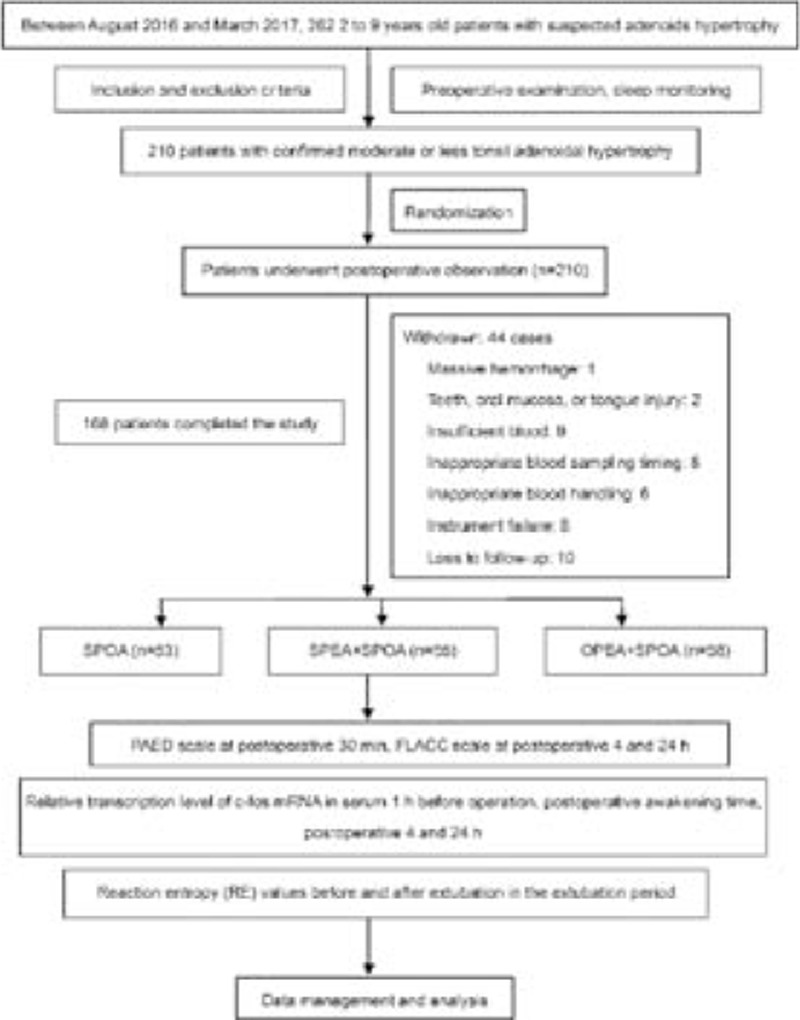
Study flowchart.
2.2. Randomization and grouping
The patients were randomized using sequential sealed envelopes. When one child was entered into the study, the envelope was opened by a designated supervisor, and the child was randomized (1:1:1) to one of 3 groups. The children were given a random ID number. Only the ID number was used in all study paperwork and database. The 3 groups were:
-
1)
sufentanil postoperative analgesia (SPOA group);
-
2)
sufentanil preemptive analgesia (SPEA+SPOA group); and
-
3)
oxycodone preemptive analgesia (OPEA+SPOA group).
Sufentanil was used for postoperative continuous analgesia in the 3 groups. Sufentanil and oxycodone were used as preemptive analgesia before tonsillectomy in the SPEA+SPOA and OPEA+SPOA groups, respectively. Assessors, statisticians, patients, and their parents were blind to grouping.
2.3. Anesthesia protocol
Atropine was intramuscularly injected at 0.02 mg/kg 30 minutes before operation for all patients, followed by oxygen inhalation and intravenous induction. Remifentanil 1 μg/kg and propofol 4 mg/kg were intravenously injected 3 to 5 minutes before operation, with or without sufentanil 0.1 μg/kg or oxycodone 0.1 mg/kg. Cisatracurium (0.05 mg/kg) was injected intravenously, and tracheal intubation was conducted after assisted respiration for 3 min. Propofol 4–12 mg/kg/h and remifentanil 0.05 to 0.1 μg/kg/h were infused continuously to sustain anesthesia. Hydroxyethyl starch was injected at 10 mL/kg/h to sustain circulation stability. All operations were performed by an experienced attending otolaryngologist. Mechanical ventilation was used, and the tracheal tube was removed under vacuum during the recovery period, followed with immediate clearing of secretions and residual blood in the oropharynx. No perioperative steroids were used.
The patients were observed for 15 to 30 minutes before sufentanil at 0.6 μg/kg/d using a BCDB-100 electronic analgesia pump (Shanghai Bochuang Medical Equipment Co., Ltd, China). The drug was diluted in normal saline to 100 mL and continuously injected at 4 mL/h for 24 hours.
2.4. Observation parameters
RE and SE were recorded using a Datex-Ohmeda S/5 monitor (Datex Ohmeda, Helsinki, Finland). BP, electrocardiogram (ECG), heart rate (HR), and SpO2 were monitored. The FLACC scores were determined. FLACC varies from 0 to 10, and ≤5 is considered as satisfying analgesia.[10] PAED scores were determined as previously reported.[14] The degree of emergence delirium increases directly with the total score.[9] The Steward recovery scale was used to evaluate the degree of awakening in the anesthesia recovery room.[15] The FLACC score, PAED score, and Steward recovery scale were assessed by a single anesthetist who did not participate in the operations and was blind to grouping.
2.5. Quantitative real-time PCR
The relative transcription levels of c-fos mRNA and β-actin were determined by fluorescence quantitative RT-PCR before surgery and 15 to 30 minutes after surgery using peripheral blood serum. Total RNA was extracted using Trizol (Invitrogen Inc., Carlsbad, CA)[16] and assessed by electrophoresis. The amount and purity were determined by ultraviolet spectrophotometry. Total RNA (1.0 μg) was denatured at 65°C for 5 minutes and cooled, and the M-Mulv reverse transcriptase was added. The total reaction volume was 20 μL. The mixture was incubated at 42°C for 60 minutes before inactivation at 85°C for 5 minutes. The conditions for RT-PCR were:
-
1)
denaturation at 95°C for 30 seconds;
-
2)
40 cycles of denaturation at 95°C for 15 seconds and extension at 58°C for 20 seconds; and
-
3)
72°C for 90 seconds.
The relative amount of PCR products was calculated by the 2-ΔΔCt method. The primers were: c-fos, forward 3’-AGTTCATCCTGGCAGCTCAC-5’ and reverse 3’-TGCTGCTGATGCTCTTGACA-5’ (204 bp); and β-actin, forward 3’-GTCACCAACTGGGACGACAT-5’ and reverse 3’-GAGGCGTACAGGGATAGCAC-5’ (209 bp).
2.6. Endpoints and follow-up
The primary endpoint was the relative transcription levels of c-fos. The secondary endpoints were the RE value, PAED score, FLACC score, and adverse events.
The patients were monitored for 30 minutes after operation in the anesthesia recovery room, and they were evaluated at 4 and 24 hours after operation. The adverse events were recorded by inquiring the patients and their parents, and by physical examinations. The awakening time was defined as from the start of extubation to when the Steward score reached 6 in the anesthesia recovery room.
2.7. Statistical analysis
The sample size was calculated by multiple populations mean sample size estimation with two-sided α of 0.05, power of 90%, and mean reduction of pain intensity (visual analog scale) after treatment of 4 ± 3 in the SPOA group, 8 ± 4 in the SPEA+SPOA group, and 6.5 ± 3 in the OPEA+SPOA group. The estimated sample size was at least 53 patients for each group. Assuming a drop-out rate of 20%, 66 patients were needed for each group.
SPSS 17.0 (IBM, Armonk, NY) was used for statistical analysis. Continuous data in accordance with the normal distribution (tested with the Kolmogorov-Smirnov test) were presented as mean ± standard deviation (SD). Intergroup comparisons were performed using analysis of variance (ANOVA) and Tukey's post hoc test. Intragroup comparisons were performed using the paired t-test and repeated measures ANOVA. Categorical data were presented as frequency (percentage) and were analyzed using the chi-square test. The correlations were analyzed using the Pearson method. The prediction probability (Pk) of RE values and c-fos mRNA levels to the FLACC score was calculated using the Pk MACRO software.[17] Two-sided P values < .05 were considered statistically significant.
3. Results
3.1. Patients
A total of 262 patients were identified for possible inclusion from August 2016 to March 2017. Among them, 52 patients were excluded (15 for severe sleep apnea-hypopnea syndrome, 24 for mild symptoms and no need for surgery, 2 for mental development disorder, one for participation in another clinical trial, 4 for hepatic or renal dysfunction, and 6 for other reasons); 210 patients with confirmed moderate or less adenotonsillar hypertrophy were randomized. Forty-four patients were withdrawn: massive hemorrhage (n = 1), teeth, oral mucosa, or tongue injury (n = 2), insufficient blood sampling for c-fos measurement (n = 9), inappropriate timing of blood sampling (n = 8), inappropriate handling of blood (n = 6), RT-PCR technical failure (n = 8), and loss to follow-up (n = 10). Eventually, 166 patients completed the study and were included in the final analysis. There were no significant differences among the 3 groups regarding baseline characteristics, HR, BP, and SpO2 before and after anesthesia (Tables 1 and 2). There were no differences in the operative time and awakening time among the three groups (Table 3).
Table 1.
Baseline characteristics of the 3 groups before analgesia.
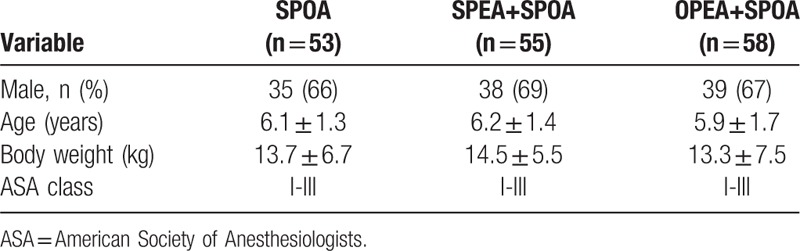
Table 2.
HR, BP, and SpO2 comparison among the three groups before and after extubation.
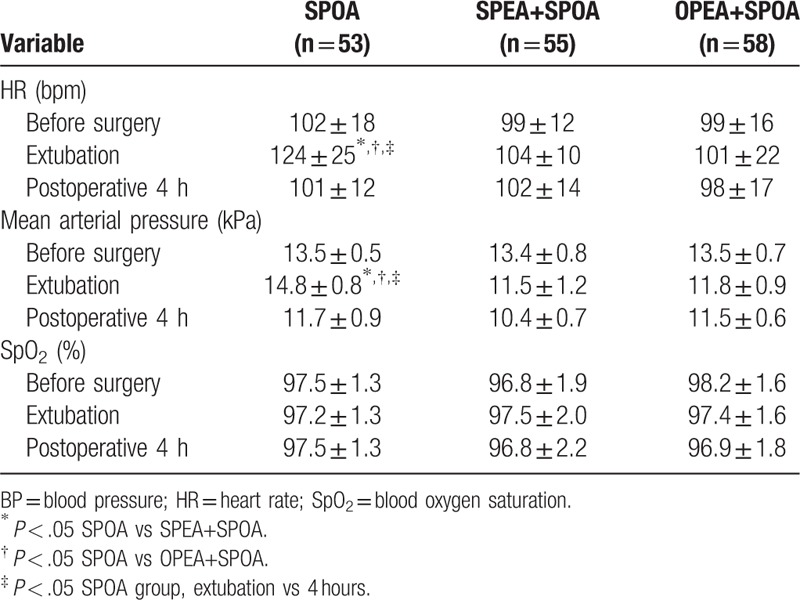
Table 3.
Comparison of the relative serum c-fos mRNA levels, RE values, PAED score, FLACC score, operative time and awakening time among the 3 groups.
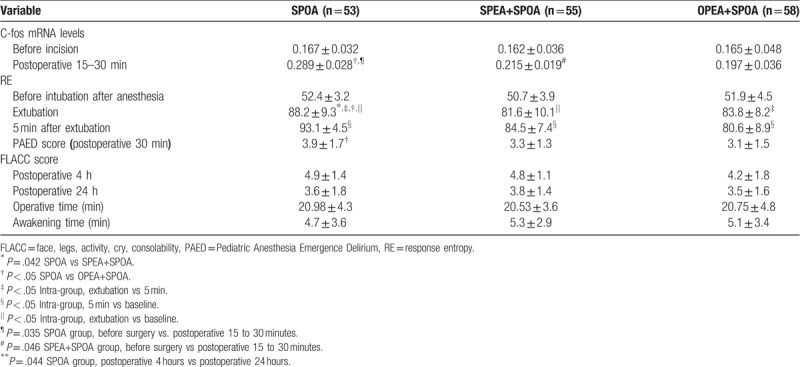
3.2. C-fos mRNA levels
C-fos mRNA levels significantly increased after surgery in the SPOA and SPEA+SPOA groups (P < .05) (Table 3). Postoperatively, c-fos mRNA levels were higher in the SPOA group compared with the OPEA+SPOA group (P = .044).
3.3. RE values, PAED score, and FLACC score
The RE values increased in all 3 groups after surgery (P < .05) (Table 3). At extubation, the RE values were higher in the SPOA group compared with the SPEA+SPOA and OPEA+SPOA groups (P < .05). The PAED scores were higher in the SPOA group compared with the OPEA+SPOA group (P = .045). In the SPOA group, the FLACC scores were decreased at 24 hours after surgery compared with 4 hours (P = .044).
3.4. Correlations and Pk values
Correlations were observed between PAED scores (at 30 minutes) and RE (at 5 minutes) after extubation and c-fos mRNA levels (Table 4). Significant correlations were observed between postoperative FLACC scores (at 4 hours) and RE (at 5 minutes) after extubation and c-fos mRNA levels. Although there were no significant differences of Pk among the three groups, Pk values were greater than 0.5, indicating that the RE value and c-fos mRNA levels were quantitative predictors for early postoperative stress reaction after surgery.
Table 4.
Correlations and Pk values.

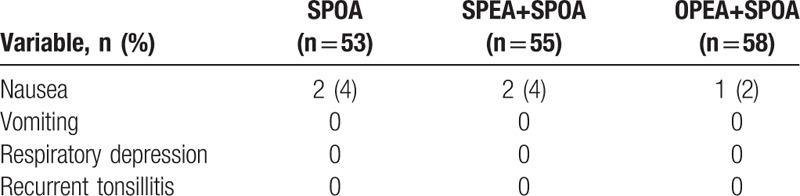
3.5. Adverse events
There was no significant difference among the 3 groups regarding nausea (Table 5). No vomiting, respiratory depression, or recurrent tonsillitis occurred. No postoperative agitation was observed.
Table 5.
Adverse events.
4. Discussion
Remifentanil is indicated for simple procedures that generally do not induce intense pains, unlike major surgeries. Nevertheless, tonsil surgery is associated with pain, especially when it is performed on young, growing patients.[3,4] Remifentanil shows more frequent and severe hyperalgesia than other opioid drugs because of its unique pharmacokinetics.[4,18] Therefore, in children undergoing tonsillectomy, remifentanil-based intravenous anesthesia could result in postoperative pain.[18,19] Remifentanil primarily stimulates the μ receptors, followed with Gi stimulation to produce analgesia, but the constant administration of remifentanil could switch protein G and alter the functionality of the μ receptor, inducing the conversion of the Gi-coupled opioid receptor to Gs-coupled opioid receptor, inducing pain.[20]
Combined intravenous analgesia could reduce the injury stimulation from the tonsil branch of the glossopharyngeal nerve to each level of the central nerve and induce effective analgesia. Oxycodone or sufentanil preemptive analgesia and sufentanil postoperative intravenous analgesia have been reported, but the analgesic effect was not satisfying.[21] Oxycodone is an opioid receptor agonist, stimulating both μ and κ receptor in the central nervous system, but mainly the κ receptor.[22] Oxycodone has the advantages of high bioavailability, stable hemodynamics, and few adverse effects. Oxycodone can be intravenously injected at 0.1 mg/kg after anesthesia induction for the treatment of pain in children undergoing thoracotomy or to alleviate pain due to orthopedic injury.[19] In the present study, oxycodone 0.1 mg/kg and sufentanil were used for preemptive analgesia to reduce postoperative pain for children undergoing tonsillectomy. Postoperative 24-hour FLACC scores of the OPEA+SPOA group were lower than that of the SPOA group. In addition, the tolerance to injury stimulation of the OPEA+SPOA group was elevated, as indicated by the transcription levels of c-fos mRNA. Oxycodone injection 5 minutes before surgery could reduce postoperative pain at the early stage and facilitate the subsequent postoperative analgesia. The tolerance to injury stimulation of the SPEA+SPOA group was also elevated. The FLACC scores indicated that postoperative pain caused by remifentanil could attenuate the postoperative analgesia induced by sufentanil. The PAED score was higher in the SPOA group, in which neither sufentanil nor oxycodone was used, compared with the OPEA+SPOA groups, in which oxycodone was used. Oxycodone 0.1 mg/kg preemptive analgesia in combination with sufentanil postoperative analgesia was demonstrated to be effective for children, and their recovery was uneventful. The possible reason might be that central sensitization induced by the surgical injury could arouse an excitatory state of the central nervous system, which could be eliminated by preoperative analgesia; both peripheral and central sensitization could be suppressed to facilitate postoperative analgesia. Those results are supported by a previous study that showed that sufentanil reduced emergence agitation in children receiving sevoflurane anesthesia for adenotonsillectomy, compared with fentanyl,[23] and by a review that suggests that oxycodone is an adequate alternative for pain management because it is not metabolized by CYP2D6.[24]
The FOS protein is an immediate stress response protein that shows elevated plasma levels as early as 30 to 60 minutes after stimuli and returns to normal by 90 minutes.[25] Even though the relative transcription levels of the c-fos mRNA in the serum is not a direct measurement of pain, it may sensitively and quantitatively reflect stress levels, which include pain, but also nausea, vomiting, and restlessness after injury stimulation.[16] In this regard, c-fos levels have been shown to have good sensitivity, but low specificity.[26] Since intravenous analgesia aims to decrease pain and to alleviate negative experiences like nausea, vomiting, and restlessness, c-fos mRNA levels should be decreased by successful analgesia.[25] In the present study, the relative transcription levels of the c-fos mRNA in serum were increased along with the severity of pain, as supported by previous studies.[27] Since the anesthesia protocol was the same for the three groups, anesthesia should not be a bias on the differences in the c-fos levels among the three groups. In addition, no child showed agitation, nausea, or vomiting in the three groups, which again should not have biased the results. Finally, c-fos levels correlated with RE, supporting its use as a marker of stress.
RE values are calculated from the frequency spectrum of 0.8 to 47 Hz (including EEG and facial electrical components), reflecting the facial muscles’ response to waking pain, and RE can detect this alteration very quickly.[28] Therefore, RE value can quantify the stress pain caused by painful operations such as vacuum aspiration of oropharynx and larynx, and endotracheal intubation.[29]
In the present study, both the c-fos mRNA levels and RE value strongly suggested that oxycodone could reduce central sensitization. RE value (reflecting injury stimulation) was increased substantially when oxycodone and sufentanil were not used, and RE values were maintained at high levels. Though sufentanil was used for postoperative analgesia, the dose was relatively low to avoid any disturbance on circulation and respiration, so that severe postoperative pain was felt by some children. RE value was initially increased when oxycodone was used at 0.1 mg/kg and then gradually decreased, indicating that oxycodone could improve postoperative pain. Moreover, the FLACC score indicated that oxycodone could cooperate with sufentanil for postoperative analgesia.
Though nausea and vomiting could be caused by surgery, it could be associated with extubation as well. Nevertheless, there were no significant differences among the three groups regarding nausea and vomiting.
The present study is not without limitations. The study was a single-center trial with a limited sample size. In addition, there was a lack of long-term follow-up to assess the surgical outcomes or to examine long-term adverse events. Only fixed doses were tested, and additional combinations could be tested. Although only children of 2 to 9 years of age were enrolled, there are important differences in cognition and pain thresholds between children of 2 and 9 years of age. In addition, there might be interindividual variations regarding the response to analgesia, and those differences were not assessed. Finally, although the evaluation indexes used in the study are well-known indicators of pain, they must be considered as surrogates at best and can be influenced by a number of factors.
In conclusion, oxycodone preemptive analgesia (0.1 mg/kg), in combination with sufentanil postoperative analgesia, has an analgesic effect in children undergoing endoscopic plasma adenotonsillectomy. This approach is superior to sufentanil postoperative analgesia and sufentanil preemptive analgesia in combination with sufentanil postoperative analgesia.
Acknowledgments
The authors acknowledge the support of Prof. Zhongfang Xia and former Prof. Zhinan Wang of the Department of Otorhinolaryngology of the Wuhan Children's Hospital, Tongji Medical College, Huazhong University of Science & Technology.
Author contributions
Conceptualization: Jiang Wu, Liang Zhong.
Data curation: Qi Gui, Feng Liu.
Formal analysis: Qi Gui, Shufen Wang, Feng Liu, Fanli Kong.
Funding acquisition: Fanli Kong.
Investigation: Qi Gui, Shufen Wang.
Methodology: Jiang Wu, Qi Gui, Jinlin Wang, Jingjing Ye, Zhongfang Xia, Shufen Wang.
Project administration: Jinlin Wang, Jingjing Ye, Zhongfang Xia.
Resources: Jinlin Wang, Jingjing Ye, Zhongfang Xia.
Software: Zhongfang Xia.
Writing – original draft: Jiang Wu, Liang Zhong.
Writing – review & editing: Jiang Wu, Qi Gui, Jinlin Wang, Jingjing Ye, Zhongfang Xia, Shufen Wang, Feng Liu, Fanli Kong, Liang Zhong.
Footnotes
Abbreviations: ANOVA = analyzed using analysis of variance, BP = blood pressure, ECG = electrocardiogram, EEG = electroencephalogram, FLACC = face, legs, activity, cry, and consolability, IRB = Institutional Review Board, OPEA = preemptive oxycodone, PAED = pediatric anesthesia emergence delirium , Pk = prediction probability, RE = response entropy, RE = response entropy, SD = standard deviation, SE = state entropy, SPEA = preemptive sufentanil, SPOA = postoperative sufentanil, TIVA = total intravenous anesthesia.
How to cite this article: Wu J, Gui Q, Wang J, Ye J, Xia Z, Wang S, Liu F, Kong F, Zhong L. Oxycodone preemptive analgesia after endoscopic plasma total adenotonsillectomy in children: A randomized controlled trial. Medicine. 2020;99:6(e19004).
The authors have no funding and conflicts of interest to disclose.
References
- [1].Liu J, Liu X, Ji X, et al. Sleep disordered breathing symptoms and daytime sleepiness are associated with emotional problems and poor school performance in children. Psychiatry Res 2016;242:218–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Ahn YM. Treatment of obstructive sleep apnea in children. Korean J Pediatr 2010;53:872–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Arbin L, Enlund M, Knutsson J. Post-tonsillectomy pain after using bipolar diathermy scissors or the harmonic scalpel: a randomised blinded study. Eur Arch Otorhinolaryngol 2017;274:2281–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Somaini M, Engelhardt T, Fumagalli R, et al. Emergence delirium or pain after anaesthesia--how to distinguish between the two in young children: a retrospective analysis of observational studies. Br J Anaesth 2016;116:377–83. [DOI] [PubMed] [Google Scholar]
- [5].Savoia G, Loreto M, Gravino E. Sufentanil: an overview of its use for acute pain management. Minerva Anestesiol 2001;67: 9 Suppl 1: 206–16. [PubMed] [Google Scholar]
- [6].Kalso E. Oxycodone. J Pain Symp Manag 2005;29: 5 Suppl: S47–56. [DOI] [PubMed] [Google Scholar]
- [7].Balci C, Karabekir HS, Kahraman F, et al. Comparison of entropy and bispectral index during propofol and fentanyl sedation in monitored anaesthesia care. J Int Med Res 2009;37:1336–42. [DOI] [PubMed] [Google Scholar]
- [8].Mathews DM, Cirullo PM, Struys MM, et al. Feasibility study for the administration of remifentanil based on the difference between response entropy and state entropy. Br J Anaesth 2007;98:785–91. [DOI] [PubMed] [Google Scholar]
- [9].Luo K, Xu JM, Cao L, et al. Effect of dexmedetomidine combined with sufentanil on preventing emergence agitation in children receiving sevoflurane anesthesia for cleft palate repair surgery. Exp Ther Med 2017;14:1775–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Voepel-Lewis T, Zanotti J, Dammeyer JA, et al. Reliability and validity of the face, legs, activity, cry, consolability behavioral tool in assessing acute pain in critically ill patients. Am J Crit Care 2010;19:55–61. [DOI] [PubMed] [Google Scholar]
- [11].Ahmad AH, Ismail Z. c-fos and its Consequences in Pain. The Malaysian journal of medical sciences. MJMS 2002;9:3–8. [PMC free article] [PubMed] [Google Scholar]
- [12].Pogatzki-Zahn EM, Zahn PK. From preemptive to preventive analgesia. Curr Opin Anaesthesiol 2006;19:551–5. [DOI] [PubMed] [Google Scholar]
- [13].Portman RJ, McNiece KL, Swinford RD, et al. Pediatric hypertension: diagnosis, evaluation, management, and treatment for the primary care physician. Curr Probl Pediatr Adolesc Health Care 2005;35:262–94. [DOI] [PubMed] [Google Scholar]
- [14].Bajwa SA, Costi D, Cyna AM. A comparison of emergence delirium scales following general anesthesia in children. Paediatr Anaesth 2010;20:704–11. [DOI] [PubMed] [Google Scholar]
- [15].Mason KP. Pediatric Sedation Outside of the Operating Room: A Multispecialty Collaboration (Second Edition). New York: Springer; 2015. [Google Scholar]
- [16].Yu EH, Tran DH, Lam SW, et al. Remifentanil tolerance and hyperalgesia: short-term gain, long-term pain? Anaesthesia 2016;71:1347–62. [DOI] [PubMed] [Google Scholar]
- [17].Jordan D, Steiner M, Kochs EF, et al. A program for computing the prediction probability and the related receiver operating characteristic graph. Anesth Analg 2010;111:1416–21. [DOI] [PubMed] [Google Scholar]
- [18].Santonocito C, Noto A, Crimi C, et al. Remifentanil-induced postoperative hyperalgesia: current perspectives on mechanisms and therapeutic strategies. Local Reg Anesth 2018;11:15–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Kim SH, Stoicea N, Soghomonyan S, et al. Intraoperative use of remifentanil and opioid induced hyperalgesia/acute opioid tolerance: systematic review. Front Pharmacol 2014;5:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Brum IS, Morsch DM, Pozzobon A, et al. Androgen-dependent expression of c-jun and c-fos in human non-transformed epithelial prostatic cells: association with cell proliferation. Horm Res 2003;60:209–14. [DOI] [PubMed] [Google Scholar]
- [21].Grape S, Tramer MR. Do we need preemptive analgesia for the treatment of postoperative pain? Best Pract Res Clin Anaesthesiol 2007;21:51–63. [DOI] [PubMed] [Google Scholar]
- [22].Bao L, Jin SX, Zhang C, et al. Activation of delta opioid receptors induces receptor insertion and neuropeptide secretion. Neuron 2003;37:121–33. [DOI] [PubMed] [Google Scholar]
- [23].Li J, Huang ZL, Zhang XT, et al. Sufentanil reduces emergence agitation in children receiving sevoflurane anesthesia for adenotonsillectomy compared with fentanyl. Chin Med J 2011;124:3682–5. [PubMed] [Google Scholar]
- [24].Chidambaran V, Sadhasivam S, Mahmoud M. Codeine and opioid metabolism: implications and alternatives for pediatric pain management. Curr Opin Anaesthesiol 2017;30:349–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Bahrami S, Drablos F. Gene regulation in the immediate-early response process. Adv Biol Regu 2016;62:37–49. [DOI] [PubMed] [Google Scholar]
- [26].Kidambi S, Yarmush J, Berdichevsky Y, et al. Propofol induces MAPK/ERK cascade dependant expression of cFos and Egr-1 in rat hippocampal slices. BMC Res Notes 2010;3:201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Ahn SN, Guu JJ, Tobin AJ, et al. Use of c-fos to identify activity-dependent spinal neurons after stepping in intact adult rats. Spinal Cord 2006;44:547–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Paloheimo M. Quantitative surface electromyography (qEMG): applications in anaesthesiology and critical care. Acta Anaesthesiol Scand Suppl 1990;93:1–83. [PubMed] [Google Scholar]
- [29].Aho AJ, Yli-Hankala A, Lyytikainen LP, et al. Facial muscle activity, Response Entropy, and State Entropy indices during noxious stimuli in propofol-nitrous oxide or propofol-nitrous oxide-remifentanil anaesthesia without neuromuscular block. Br J Anaesth 2009;102:227–33. [DOI] [PMC free article] [PubMed] [Google Scholar]


