Summary:
Neuromas are a debilitating peripheral nerve problem due to aberrant axon sprouting and inflammation after nerve injury. The surgical management of neuromas has for a long time been up for debate, largely due to lack of consistent, reliable outcomes with any one technique. We have found success utilizing targeted muscle reinnervation, a technique originally described in amputees that re-routes the proximal ends of cut sensory nerve stumps into the distal ends of motor nerves to nearby muscles. In doing so, the sensory nerve ending can regenerate along the length of the motor nerve, giving it a place to go and something to do. In this report, we describe our technique specifically for targeted muscle reinnervation of sural nerve neuromas that is applicable to both amputees and to patients with intact limbs. Sural nerve neuromas can occur after sural nerve harvest for reconstructive procedures and particularly after lateral malleolar incisions for orthopedic access to the calcaneus. By re-routing the sural nerve into a motor nerve of the lateral gastrocnemius muscle, we are able to manage a variety of sural nerve neuromas presenting anywhere along the course of the sural nerve and in a variety of clinical settings.
INTRODUCTION
Neuromas are a frustrating clinical problem causing chronic local pain that radiates in the distribution of the specific nerve from pressure, manipulation, or temperature change.1,2 Neuromas occur after numerous types of soft tissue injury, including surgical interventions.3 Amputations are associated with numerous cut nerve endings, causing both local pain and phantom sensations. A multitude of treatments for neuroma have been trialed, attesting to the lack of consistent, reliable outcomes with any one treatment.4–12
Targeted muscle reinnervation (TMR) is a surgical technique in which proximal stumps of cut nerves are coapted to distal motor nerves of adjacent muscles.13–16 TMR reduces both neuroma and phantom limb pain in amputees and is superior to excision and muscle burying.17–19 Here, we describe the clinical application of TMR in the treatment of sural neuromas, specifically with transfer to a motor branch to the lateral gastrocnemius—one of the most common nerve transfers performed for painful neuromas in the leg at our institution.
SURAL NERVE ANATOMY
The sural nerve is a unique sensory nerve in that it often (though not always) forms distally from a combination of 2 peripheral sensory nerves—the medial and lateral sural nerves.20 The medial sural nerve arises from the tibial nerve in the popliteal fossa (around 6 cm proximal to the fibular head) while the lateral sural nerve arises from the common peroneal nerve (around 7 cm proximal to the fibular head).21 Most commonly, the medial and lateral sural nerves join in the distal third of the calf (84% based on a cadaveric study) via a peroneal communicating branch.21 Less often, these nerves join together in the popliteal fossa (12% of cadavers). Even less often, either the medial or lateral sural nerve alone represents the sural nerve proper.
OPERATIVE TECHNIQUE
In the preoperative area, the Tinel sign over the sural nerve is marked. In the operating room, the patient is prepped and draped prone. A longitudinal incision is made over the previously marked Tinel sign. Subcutaneous dissection is performed to identify the sural nerve neuroma bulb. We do not believe neuroma bulb excision is a necessary treatment component given transection and transfer of the more proximal sural nerve will cut the neuroma signal to the brain and result in Wallerian degeneration of distal axons. However, in this situation, there is a need to start distally at the neuroma site to find and dissect both the peroneal and tibial components of the sural nerve neuroma. Starting distally and moving proximally ensures both nerves are identified and the nerve fibers in continuity with the neuroma are definitively treated via TMR. A series of stair-step incisions are then performed in the same fashion as if a sural nerve graft were being harvested (Fig. 1). Gentle traction on the nerve helps identify the subcutaneous course for making stair-step incisions and also helps identify anatomic variants in the medial and lateral sural nerve branches. Once the proximal calf is reached, another longitudinal incision is made in the midline inferior to the popliteal crease. The crural fascia over the 2 heads of the gastrocnemius is opened. A nerve stimulator is used to identify motor branches to the lateral head of the gastrocnemius. These motor branches are transected proximally while maintaining a safe distance from the tibial nerve. The medial and lateral sural cutaneous nerves are brought into the field and transected distally to allow a tension-free coaptation. Each sural nerve branch (medial and lateral) is coapted to a separate gastrocnemius motor branch using 7-0 polypropylene sutures under loupe magnification. The incisions are then closed and a posterior mold splint including the ankle is placed for 1 week. Full ambulation resumes as tolerated.
Fig. 1.

This demonstrates the incisions that are made to trace both medial and lateral sural nerve proximally. Dissection always begins distally and proceeds proximally to ensure both medial and lateral nerve fibers are captured.
CASE EXAMPLE
A 32-year-old man status post cerebellopontine angle meningioma resection developed left facial paralysis. He underwent a facial reanimation surgeries including cross-facial sural nerve graft, unfortunately resulting in significant neuropathic right lower extremity pain. On physical examination, he had a Tinel sign over sural nerve harvest incision. Symptoms improved with lidocaine injection in the outpatient setting. The nerve gap was over 6 cm and too long for nerve graft reconstruction, so he underwent TMR with sural neuroma excision and transfer to motor nerve of lateral gastrocnemius muscle (Fig. 2). At 6 month follow-up, the patient reported no pain and normal ambulation, even with manipulation of the nerve coaptation site.
Fig. 2.
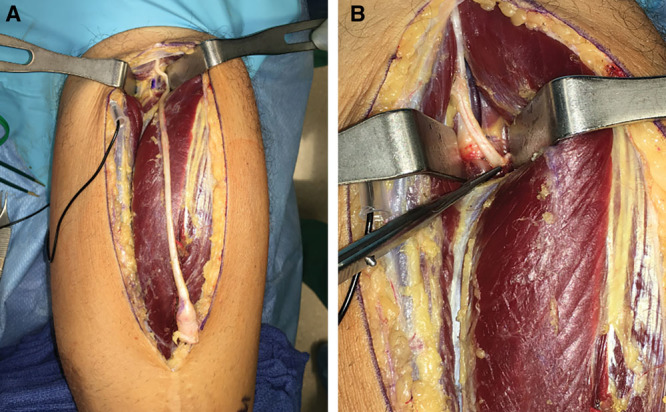
Treatment of sural nerve neuroma in a 32-year-old man who previously had sural nerve grafting for facial reanimation. A, Harvest of sural nerve with neuroma encased in scar tissue distally. B, Coaptation of proximal sural nerve to a motor branch to the lateral gastrocnemius. This patient had only a medial sural nerve component.
DISCUSSION
By providing a distal target, TMR allows for coordinated nerve axon sprouting to provide nerve regeneration rather than neuroma formation.22,23 The goal of the procedure is to give the nerve “somewhere to go and something to do.” TMR results in decreased neuroma formation histologically, in addition to decreased residual limb pain and phantom pain for amputees.19,22 Loss of the lateral gastrocnemius motor function has been well tolerated.
In performing sural nerve TMR, it is important to note the unique anatomy. Unlike other peripheral nerves, which branch distally, the sural nerve is actually the fusion of the medial and lateral sural cutaneous nerves. Because of this dual fiber contribution and because of variable anatomy, it is important to start dissection distally and trace the nerve proximally to capture both components, if present. Thus, some instances of sural nerve transfer will require identification of 2 motor nerve targets—1 for tibial component fibers and 1 for common peroneal fibers—while others may only require a single motor nerve target. Often a bifurcation of the lateral gastrocnemius motor nerve permits 2 separate nerve coaptations. The mismatch in nerve sizes at the coaptation site is in theory problematic, but clinically is not a problem.
TMR is 1 of 3 procedures in our treatment of sural nerve neuromas. We prefer to reconstruct short nerve gaps with nerve allograft as this has been shown to result in improved pain.24 In instances with nerve gaps between 3 and 6 cm where the patient insists on trying to reestablish sensation, we will use the motor nerve to the vastus lateralis as a nerve graft to avoid damage to an alternate sensory nerve and potential for sensory neuromas elsewhere. If nerve allografts are unsuccessful, or in nerve gaps >6 cm that are deemed unreconstructable, we opt for TMR.
CONCLUSION
Our technique for sural nerve TMR with transfer to motor branches of the lateral gastrocnemius is an option for treating sural neuromas while addressing potential variations between patients in sural nerve anatomy.
Footnotes
Published online 17 January 2020.
Disclosure: G.A.D. has received compensation from Axogen as a speaker on several occasions, and has intellectual property and ownership in the Advanced Suture Co. and the Mesh Suture Co. Both J.H.K. and G.A.D. are on the Scientific Advisory Board of Checkpoint. The other authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Pierce RO, Jr, Kernek CB, Ambrose TA., II. The plight of the traumatic amputee. Orthopedics. 1993;16:793–797. [DOI] [PubMed] [Google Scholar]
- 2.Hanley MA, Ehde DM, Jensen M, et al. Chronic pain associated with upper-limb loss. Am J Phys Med Rehabil. 2009;88:742–51; quiz 752, 779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rajput K, Reddy S, Shankar H. Painful neuromas. Clin J Pain. 2012;28:639–645. [DOI] [PubMed] [Google Scholar]
- 4.Thomson CE, Beggs I, Martin DJ, et al. Methylprednisolone injections for the treatment of morton neuroma: a patient-blinded randomized trial. J Bone Joint Surg Am. 2013;95:790–798. [DOI] [PubMed] [Google Scholar]
- 5.Climent JM, Mondéjar-Gómez F, Rodríguez-Ruiz C, et al. Treatment of morton neuroma with botulinum toxin a: a pilot study. Clin Drug Investig. 2013;33:497–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ulrich D, van Doorn L, Hovius S. Fat injection for treatment of painful neuroma after episiotomy. Int J Gynaecol Obstet. 2011;115:290–291. [DOI] [PubMed] [Google Scholar]
- 7.Pet MA, Ko JH, Friedly JL, et al. Traction neurectomy for treatment of painful residual limb neuroma in lower extremity amputees. J Orthop Trauma. 2015;29:e321–e325. [DOI] [PubMed] [Google Scholar]
- 8.Woo SL, Kung TA, Brown DL, et al. Regenerative peripheral nerve interfaces for the treatment of postamputation neuroma pain: a pilot study. Plast Reconstr Surg Glob Open. 2016;4:e1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Souza JM, Purnell CA, Cheesborough JE, et al. Treatment of foot and ankle neuroma pain with processed nerve allografts. Foot Ankle Int. 2016;37:1098–1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koch H, Haas F, Hubmer M, et al. Treatment of painful neuroma by resection and nerve stump transplantation into a vein. Ann Plast Surg. 2003;51:45–50. [DOI] [PubMed] [Google Scholar]
- 11.Dellon AL, Mackinnon SE. Treatment of the painful neuroma by neuroma resection and muscle implantation. Plast Reconstr Surg. 1986;77:427–438. [DOI] [PubMed] [Google Scholar]
- 12.Poppler LH, Parikh RP, Bichanich MJ, et al. Surgical interventions for the treatment of painful neuroma: a comparative meta-analysis. Pain. 2018;159:214–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheesborough JE, Souza JM, Dumanian GA, et al. Targeted muscle reinnervation in the initial management of traumatic upper extremity amputation injury. Hand (N Y). 2014;9:253–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gart MS, Souza JM, Dumanian GA. Targeted muscle reinnervation in the upper extremity amputee: a technical roadmap. J Hand Surg Am. 2015;40:1877–1888. [DOI] [PubMed] [Google Scholar]
- 15.Morgan EN, Kyle Potter B, Souza JM, et al. Targeted muscle reinnervation for transradial amputation: description of operative technique. Tech Hand Up Extrem Surg. 2016;20:166–171. [DOI] [PubMed] [Google Scholar]
- 16.Fracol ME, Janes LE, Ko JH, et al. Targeted muscle reinnervation in the lower leg: an anatomical study. Plast Reconstr Surg. 2018;142:541e–550e. [DOI] [PubMed] [Google Scholar]
- 17.JM. DGaS. Targeted muscle reinnervation for prosthetic control and treatment of neuroma pain. In Atlas of Amputations and Limb Deficiencies. 2016:4th ed Rosemont, IL: American Academy of Orthopaedic Surgeons; 329–337. [Google Scholar]
- 18.Souza JM, Cheesborough JE, Ko JH, et al. Targeted muscle reinnervation: a novel approach to postamputation neuroma pain. Clin Orthop Relat Res. 2014;472:2984–2990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dumanian GA, Potter BK, Mioton LM, et al. Targeted muscle reinnervation treats neuroma and phantom pain in major limb amputees: a randomized clinical trial. Ann Surg. 2019;270:238–246. [DOI] [PubMed] [Google Scholar]
- 20.Riedl O, Frey M. Anatomy of the sural nerve: cadaver study and literature review. Plast Reconstr Surg. 2013;131:802–810. [DOI] [PubMed] [Google Scholar]
- 21.Coert JH, Dellon AL. Clinical implications of the surgical anatomy of the sural nerve. Plast Reconstr Surg. 1994;94:850–855. [DOI] [PubMed] [Google Scholar]
- 22.Kim PS, Ko JH, O’Shaughnessy KK, et al. The effects of targeted muscle reinnervation on neuromas in a rabbit rectus abdominis flap model. J Hand Surg Am. 2012;37:1609–1616. [DOI] [PubMed] [Google Scholar]
- 23.Ko JH, Kim PS, O’Shaughnessy KD, et al. A quantitative evaluation of gross versus histologic neuroma formation in a rabbit forelimb amputation model: potential implications for the operative treatment and study of neuromas. J Brachial Plex Peripher Nerve Inj. 2011;6:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guse DM, Moran SL. Outcomes of the surgical treatment of peripheral neuromas of the hand and forearm: a 25-year comparative outcome study. Ann Plast Surg. 2013;71:654–658. [DOI] [PubMed] [Google Scholar]


