Abstract
Background:
Nail bed and fingertip injuries are the commonest hand injuries in children and can lead to profound functional and cosmetic impairments if not appropriately managed. Fingertip injuries can present with subungual hematomas, simple or stellate lacerations, crush, or avulsion injuries, often with associated fractures or tip amputations. The fundamentals of managing nail bed injuries concern restoring the form and function of a painless fingertip. However, there are controversies surrounding the optimal management of each of these injuries, which has led to nonuniformity of clinical practice.
Methods:
The PubMed database was searched from March 2001 to March 2019, using a combination of MeSH terms and keywords. Studies evaluating children (<18 years of age) and the fingertip (defined as distal to the distal interphalangeal joint) were included following screening by the authors.
Results and Conclusion:
The evidence base for the diverse clinical management strategies currently employed for fingertip injuries in the pediatric population is limited. Further studies yielding level I data in this field are warranted.
INTRODUCTION
The fingertip is a highly sensate structure, with exquisite mobility and stability. However, fine dexterity comes at the expense of vulnerability to injury.
Fingertip and nail bed injuries account for over two-thirds of all pediatric hand injuries.1 They can be caused by sharp injuries, resulting in clean lacerations, or more commonly blunt trauma. Nail bed injuries include subungual hematomas, simple or stellate lacerations, crush injuries, and avulsions (Fig. 1),2 and the trauma is often underestimated.3 The commonest mechanism is via a crush injury of the middle finger in a closing door in the home environment,4 despite the presence of adults.5
Fig. 1.
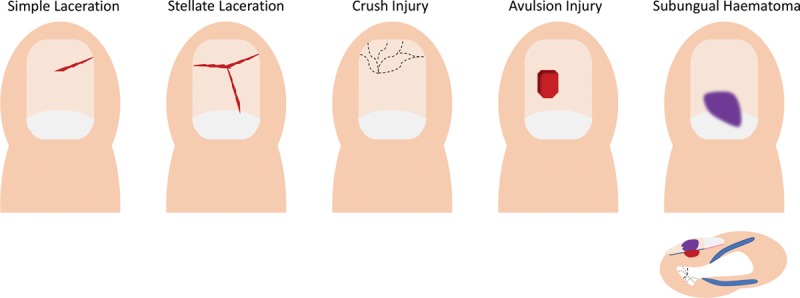
Schematic of the different presentations of distal tip injuries, demonstrating simple laceration, stellate laceration, crush injury, avulsion injury, and subungual haematoma (with associated lateral view).
Suboptimal management of pediatric fingertip injuries can lead to lasting functional, cosmetic, psychological, and economic consequences.6 A recent Cochrane review highlighted that high-level evidence in management is lacking7 and nonuniformity is accordingly reported between care providers.8 Herein, the need for level I data and preventative measures is recognized.
METHODOLOGY
The PubMed database was searched from March 2001 to March 2019, using a combination of MeSH terms and keywords. Studies evaluating children (<18 years of age) and the fingertip (distal to the distal interphalangeal joint [DIPJ]) were included following independent screening by the authors. The literature search was conducted using the PRISMA guidelines, and the search strategy is included (Fig. 2). GRADE assessment9 was used to assess the quality of evidence.
Fig. 2.
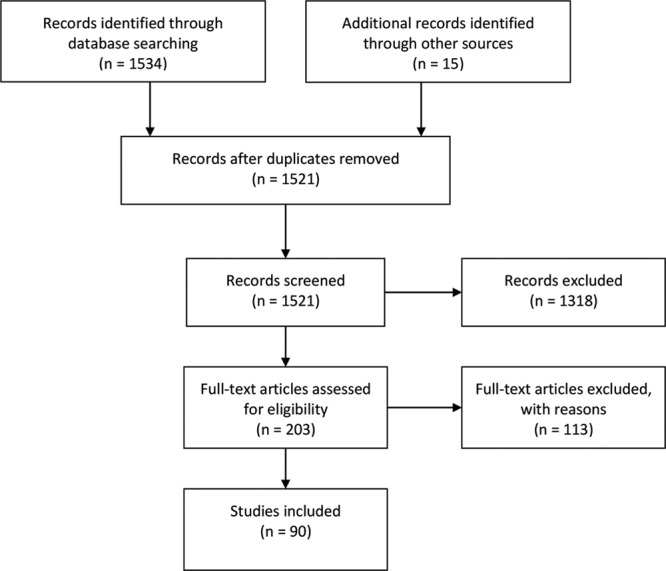
PRISMA diagram and search strategy used:“Infant”[Mesh] OR “Child”[Mesh] OR “Adolescent”[Mesh] AND “Nails/injuries”[Mesh] OR “Nails/surgery”[Mesh] OR “Finger Injuries”[Mesh] OR “Nail Diseases/surgery”[Mesh] OR “Nail Diseases/therapy”[Mesh]
EPIDEMIOLOGY
Fingertip injuries in children are the most common hand injury to present in the emergency departments (EDs).2 In the United States, almost 700,000 children are treated annually for door-related distal tip injuries alone.10 Children (particularly males) under 5 years old underwent the highest annual rate of finger amputations (18.8/100,000 population).11 A large retrospective study highlighted that crush, nail bed, and middle finger were the most common mechanism, type, and digit injured, respectively.12
ANATOMY OF THE DISTAL TIP AND NAIL BED
The fingertip encompasses the structures of the finger distal to the DIPJ.13 These include the nail plate and the perionychium, which comprises the nail bed, eponychium, paronychium, and hyponychium (Fig. 3).2 These specializations confer exquisite 2-point discrimination, pincer grip, and regulation of peripheral circulation.
Fig. 3.

Schematic of the nail apparatus.
MECHANISMS AND CLASSIFICATIONS OF DISTAL TIP INJURIES
Nail bed injuries are diverse in both mechanism and presentation. Ashbell et al (1967) classified subungual hematoma, simple lacerations, stellate lacerations, severe crush, and avulsion,14 though amputations are also common.
Subungual hematomas present after bleeding under the nail plate following blunt trauma to the nail bed. Clinically, the Van Beek classification system denominates 5 principal nail bed injuries (Table 1), subclassified by location within the nailbed (involving either the sterile and/or germinal matrix, respectively) and the extent of injury.15
Table 1.
Van Beek Classification of Nail Bed Injuries
| Type | Description |
|---|---|
| SI | Small (<25%) subungual hematoma |
| SII | Sterile matrix laceration with large (>50%) subungual hematoma |
| SIII | Sterile matrix laceration associated with fracture of the distal phalanx |
| SIV | Sterile matrix fragmentation |
| SV | Sterile matrix avulsion |
| GI | Small (<25%) subungual hematoma, proximal nail |
| GII | Germinal matrix laceration with large (>50%) subungual hematoma |
| GIII | Germinal matrix laceration associated with fracture of the distal phalanx |
| GIV | Germinal matrix fragmentation |
| GV | Germinal matrix avulsion |
Amputations are described in relation to the zone and plane of injury. The recent pulp, nail, bone classification has shown low interobserver concordance (< 60%),16 undermining overly precise, unreproducible classification systems. A simpler binary classification of fingertip amputations17 is frequently used: zone I—distal to the lunula; zone II—between the DIPJ and the lunula.
Fractures of the distal phalanx constitute almost 50% of all hand fractures, and 50% are associated with injuries to the nail bed.18 Fractures can be classified by type (transverse, longitudinal split, or comminuted) or anatomy (extra-articular or intra-articular). Distal tuft fractures account for 80% of hand fractures in children under 4 years old, commonly arising from crush injuries. Distal phalangeal shaft fractures are typically longitudinal or transverse and are minimally displaced.
Distal phalangeal base fractures are unstable and can lead to volar angulation. In children, these fractures may lead to physeal injuries, which are categorized by the Salter–Harris classification (Table 2), with type II being the most common.19
Table 2.
Salter–Harris Classification of Fractures in Children
| Type | Description |
|---|---|
| I | Transverse fracture through the physis only |
| II | Fracture line through the physis and extending to include a portion of the metaphysis |
| III | Fracture line through the physis and exiting through the epiphysis into a joint |
| IV | Vertical fracture line through the epiphysis, physis, and metaphysis |
| V | Crush injury to the physis |
Seymour fractures are open physeal fractures of the distal phalanx that occur from hyperflexion injury (Fig. 4). These fractures are often misdiagnosed, undertreated and complicated by infection and growth arrest.20
Fig. 4.
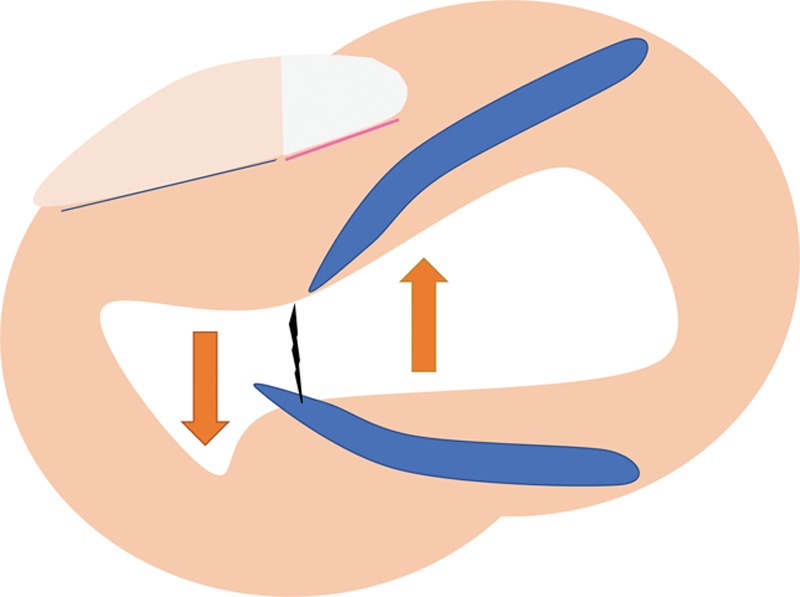
Schematic of a Seymour fracture. Since the extensor tendon inserts into the epiphysis, which is proximal to the insertion of the flexor digitorum profundus (FDP), fractures at the metaphysis cause net extension of the proximal fragment (up arrow) and unopposed flexion of the distal fragment of the distal phalanx (down arrow).
Intra-articular distal phalangeal fractures occur as avulsion fractures. The mallet finger describes a flexion deformity resulting from impaired extension of the DIPJ, commonly due to forced flexion of an actively extended finger. The extensor tendon can avulse an epiphyseal fragment, resulting in an intra-articular fracture. Mallet deformities are Salter–Harris Type III or Type IV fractures, classified as: type I – only the tendon ruptures, type II—small avulsion fracture, and type III—involves > 25% of the articular surface. If left untreated, “swan neck” deformities can manifest, wherein the proximal interphalangeal joint extends due to volar displacement of lateral bands.
Lastly, “Jersey” fingers refer to sudden hyperextension of an actively flexed finger with fracture at the distal phalangeal base of the volar distal phalanx due to the avulsed flexor digitorum profundus tendon. These classically occur in contact sports such as rugby or American football. Leddy and Packer (Table 3)21 categorize these injuries based on location, degree of tendon retraction, and presence of an osseous fragment.
Table 3.
Leddy and Packer Classification of Flexor Digitorum Profundus (FDP) Tendon Avulsion
| Type | Description |
|---|---|
| I | FDP tendon retracted to palm. Leads to disruption of the vascular supply |
| II | FDP retracts to level of PIP joint |
| III | Large avulsion fracture limits retraction to the level of the DIP joint |
| IV | Osseous fragment and simultaneous avulsion of the tendon from the fracture fragment (“Double avulsion” with subsequent retraction of the tendon usually into palm) |
| V | Ruptured tendon with bone avulsion with bony comminution of the remaining distal phalanx (Va, extraarticular; Vb, intra-articular) |
EVIDENCE BASE FOR MANAGEMENT STRATEGIES
The objective of management is to restore the form and function of a durable, pain-free yet sensate fingertip. A thorough history and examination should elicit age, sex, hand dominance, professional goals, hobbies, comorbidities, and the status of the defect and remaining soft tissue. Since older children may anatomically resemble adults in terms of physeal closure, the principles discussed herein may be broadly applicable.
Subungual Hematomas—Remove and Repair or Trephinate and Drain?
Subungual hematomas often result from compression injuries to the nail. Currently, level III evidence supports removing the nail plate to permit nail bed exploration and repair if there is a displaced tuft fracture.2 However, if the nail fold edges are intact and (if present) the fracture is not displaced, then optimal management is controversial. Traditionally, treatment was based on the relative size of the hematoma22: the nail plate was removed for hematomas > 50% of the nail, or 25% if in the presence of a fracture. Simple nail plate trephination to evacuate subungual hematomas arising from door crush or blunt nail bed injuries in children with intact nail folds and nail margins has produced same or superior results, when compared to nail removal and formal nail bed reconstruction.18,23 Moreover, trephination23 or expectant management alone24 has demonstrated similar cosmetic outcomes and complication rates, irrespective of the size of hematoma or presence of a nondisplaced fracture.25
Decontamination of the skin before incision is part of the standard of surgical care. Of the commonly used surgical skin preparations, a prospective randomized trial found that DuraPrep (Iodine Povacrylex and Isopropyl Alcohol; 3MHealthcare, Minnesota) and Betadine solution (10% povidone-iodine; Purdue Pharma LLP, Connecticut) were superior to ChloraPrep (2% chlorhexidine gluconate and 70% isopropyl alcohol; Texas) for preoperative decontamination in clean elective soft tissue hand surgery.26 Further study of the efficacy of skin preparations in the surgery of contaminated hand wounds is warranted. Subungual hematoma drainage involves trephination, in which the hematoma is evacuated through a sufficiently large hole in the nail plate created by a blade or electrocautery with a needle point (eg, Colorado tip).
Nail Bed Injury—Sutures or Adhesives?
Nail bed lacerations include simple lacerations, stellate lacerations, or crush injuries. The latter two often involve fragmentation of the nail plate. The success of nail bed repair diminishes with delay following injury, with recommended intervention within 2–3 days, but ideally sooner. Repair of stellate lacerations can have good outcomes whilst crush injuries have a poorer prognosis due to additional nail bed contusion.27
Though examples of protocols have been described,28 operative technique is widely debated. Absorbable sutures are helpful as they need not be removed. In a survey, hand surgeons preferred an interrupted suture technique (85.1%) using polyglactin 910 (Vicryl-Rapide) (83.3%) material.8
Medical adhesives are an alternative to primary repair with sutures for nail bed injuries.29 2-Octylcyanoacrylate (Dermabond) can bond disrupted nail plate fragments and appose wound margins. Preliminary research suggested that adhesives achieved acceptable cosmetic appearance,30 but were limited in their comparisons with standard suturing, the objectivity of their outcome measures, and their small sample sizes. Later studies highlighted the efficacy of Dermabond relative to suturing, such as similar breaking strength,31 and lower mean tourniquet time required.32 Even though a speedier approach limits operative distress,29 surgeons prefer a figure-of-eight suture (45.1%) to secure the nail plate back under the nail fold over adhesives (20.7%).8 This may reflect how medical adhesives risk chronic infection, granuloma formation and foreign body reaction, and tattooing of the tissue. Widespread adoption therefore demands a stronger evidence base.
Nail Bed Avulsion/Defects—Suture or Graft?
Nail bed avulsions present with the avulsed nail bed attached to the undersurface of the nail plate, which can be sutured in place.33 Small defects < 2mm heal by secondary intention, with the replaced nail plate acting as a cover and a splint. A substitute introduced into the gap (if > 2 mm) can prevent scar formation, particularly for full-thickness germinal matrix injuries. Options include a dermal replacement template (eg, Integra or Matriderm),34 split-thickness skin graft, split-thickness nail bed graft,35 and full-thickness nail bed graft—the latter two are preferred but may cause a donor site deformity.36 The graft can be harvested either from uninjured areas of the involved finger or from other intact digits for larger defects.33 For pediatric nail bed defects beyond 3 × 3 mm, split thickness nail bed grafts harvested from the injured finger or a great toe is recommended,35 though objective functional assessments were lacking in this study.
Distal Phalanx Fracture—Repair and Fixate or Suture?
Over 50% of all nail bed injuries have an associated distal phalanx fracture.6 Traditionally, distal tuft fractures and nondisplaced distal phalanx fractures were managed with nail bed repair and nail plate replacement. Displaced fractures and fractures proximal to the nail fold have been treated with operative fixation utilizing two 0.028-inch Kirschner wires. For open Seymour fractures, the principles of open fracture management are recommended,37 along with antibiotics due to frequent infective complications.20 For nail bed disruptions associated with distal phalangeal fractures, a group from India advocate vertical figure-of-eight tension band sutures without formal nail bed repair or fracture stabilization (held in place for 6 weeks) as a simple, minimally traumatic, and similarly efficacious option.38
Comminuted fractures often have small bony fragments adherent to the nail bed. Repair of the nail bed injury allows approximation of the bony fragments. Nail plate replacement has been often used as a splint for fracture healing, though synthetic alternatives are present if the nail is unavailable.39
Distal Tip Amputations—Revision Amputation, Flaps, or Replantation?
Management of distal tip amputations depends on level of injury and integrity of the remaining structures. The modified Ishikawa classification (Table 4) describes levels of transverse fingertip amputations.40 Oblique amputations are incorporated in more recent classifications.41 Reconstruction may require shortening of exposed bone, skin and nail bed graft placement, and local flap reconstruction or replantation. Lipofilling, proposed by a group in Germany, may improve volume defects and also remediate hypoesthesia by stimulating distal nerve regeneration. This study however had a small sample size and used subjective tools, like visual analogue scale (VAS), to assess outcomes.42
Table 4.
Modified Ishikawa Classification of Fingertip Amputation
| Type | Amputation Level |
|---|---|
| I | Distal to midnail (Ia—beyond the distal edge of the nail; and Ib—between the midnail and distal edge of the nail) |
| II | Between midnail and nail base (eponychium) |
| III | Midway between eponychium and DIPJ |
| IV | Between II and DIPJ |
If the injury exposes the distal phalanx, bone shortening and suturing the remaining skin as local flaps over the distal phalanx is a standard reconstructive technique (eg, Ref 43). Local flap mobilization and advancement is a useful option, and selection of the flap modality is guided by the orientation and configuration of the wound. For instance, volar V-Y advancement flaps are appropriate for injuries occurring in the dorsal oblique and transverse planes.44 Suturing of the skin to the nail bed edge should be tension-free to prevent a hook nail deformity.
Small distal amputations of digits survive as reattached composite grafts in children, with more successful outcomes than in adults.45 The amputated tip is sutured back to the stump without formal microvascular repair, the nail bed is repaired carefully, and any fractures reduced and stabilized, for example, with Kirschner wires or a 23 or 21-gauge needle.46 The most likely outcome of the composite grafts is partial survival; graft success is unlikely in those over 4 years of age47 and those suffering from crush injuries.40 In older children, tip amputations can be defatted and replaced as a “cap” graft, with better success.48 Thus, parents should be cautioned regarding these limitations.
Should the Nail Plate Be Replaced or Discarded?
Having repaired the nail bed, 96% of surgeons replace the nail plate whilst 4% prefer to discard it.8 Nail replacement has been argued to confer key advantages.33 First, it acts as a mold to maintain the normal anatomy for new nail growth and can splint any associated distal fracture. Furthermore, replacing the proximal portion of the nail plate prevents scar formation between the proximal nail fold and the germinal matrix, leading to a permanently split nail.49 Consequently, splinting of the proximal nail fold with a replaced nail plate was recommended for 2–3 weeks.
This surgical dogma has been challenged by evidence of higher morbidity accompanying nail plate replacement. Replacing the nail plate has a higher complication rate (17.6%) than discarding the nail plate and applying a nonadherent (Mepitel) dressing (5%).50 Such complications included postoperative infection, persistent pain, delayed wound healing, and overgranulation. It is argued that small nails (in children) or nail fragments might be harder to clean, effectively acting as a foreign body.51 Prophylactic antibiotics have not significantly influenced infection rates.52 The method of nail plate fixation may provoke inflammation and edema, leading to postoperative nail fold lacerations at the sites of, for example, tight sutures.53 These studies suggest that replacing the nail plate might not be solely accountable for complications and increased morbidity.
This highlights a need for high-quality studies to establish definitive indications and management strategies.7 An ongoing multicenter randomized controlled trial (Nail bed INJury Analysis [NINJA] trial) aims to address whether the nail plate should be replaced following nail bed repair in children.54 Their preliminary study agreed with an earlier study50 that showed that nail plate replacement was associated with greater incidence of infection, complications, and postoperative pain, but did not reach statistical significance, likely due to a small sample size. It is hoped that the definitive trial will better inform the most appropriate management. Ultimately, the objective is to minimize morbidity, exposure to multiple operations, and number of follow-ups needed,50 whilst optimizing outcomes.
PATIENT-REPORTED OUTCOME MEASURES
Healthcare systems endeavor to optimize outcomes. To accurately evaluate the efficacy of any intervention, appropriate outcome measures are essential. Traditional objective clinical assessments (eg, grip strength and range of motion) do not consider the patient’s ability to resume normal activities of daily living or persistent pain. Consequently, the focus has shifted toward longitudinal assessment of patient-reported outcome measures (PROMs). However, convention holds that children’s self-reported health information is unreliable, which has limited the attention and utilization of pediatric PROMs despite evidence suggesting that children (beyond 8 years of age) can accurately report their health status.55
Adopting an appropriate PROM for functional hand outcomes in children has proven challenging. An established PROM for functional hand outcomes in adults is the Michigan Hand Outcomes Questionnaire but is not validated for direct use in children. Two studies adopted this method in a pediatric sample56 by modifying the questionnaire to allow evaluation of the child’s outcome by proxy. Another popular adult PROM is the Disabilities of the Arm, Shoulder, and Hand (DASH) or its abbreviated counterpart, QuickDASH. Whilst the QuickDASH has shown evidence of internal reliability in patients aged 8–18 years, several limitations were identified in younger patients.57 Thus, utilizing PROMs developed for adults in children likely has limited reliability, content validity, or applicability.
This highlights a need for pediatric-specific hand outcome measures. For instance, the Wong-Baker FACES Pain Rating Scale has been successfully validated in children presenting at the ED,58 and has aided the scoring of acute pain associated with removing a wound dressing.
The hand is an important tool in our social lives, thus good cosmetic outcomes are highly desirable, and lasting deformities may impact self-esteem. Affected children and their parents may rate the appearance of the fingernail using a VAS. For surgeons, the Zook classification tool (Table 5) of nailbed appearance59 is a validated method of categorizing outcomes based on several variables that are compared to the uninjured equivalent contralateral finger nail. These include incomplete nail plate adherence, nail ridging, split nails, or eponychial deformity. Surgeons have cited the most important outcome measure as cosmetic appearance (33%), followed by nail regrowth (28%) and parent satisfaction (14%).8 Other important pragmatic factors are operative time, total time spent in the hospital, and postoperative complication rates.
Table 5.
Zook’s Classification of Fingernail Appearance
| Criterion | Description |
|---|---|
| Nail shape | Identical to opposite |
| Shorter | |
| Narrower | |
| Longitudinal curve | |
| Transverse curve | |
| Nail adherence | Complete |
| 2/3 to complete | |
| 1/3 to 2/3 | |
| <1/3 | |
| Eponychium | Identical to opposite |
| Notched | |
| Synechia | |
| Nail surface | Identical to opposite |
| Slightly rough | |
| Very rough | |
| Longitudinal ribs | |
| Transverse grooves | |
| Split nail | Absent |
| Present |
PREVENTION
Education of the patient, parent, and general public of prevention of digit injuries should be reinforced. Since most digit injuries occur at home or school despite adult supervision,5 preventative measures are needed. These include installing finger-shield door hinge safeguards or door stoppers to limit the impact of door closing on fingers. For other risky recreational activities/sports, use of safety gloves or warning signs should be encouraged. Widespread adoption can be disseminated through use of safety checklists and awareness programs. Since a single ED can charge over $300,000 per year12 for fingertip injuries alone, introducing targeted prevention strategies is important.
CONCLUSIONS
Pediatric distal tip injuries pose a significant healthcare challenge, particularly if not managed appropriately. High-quality level I evidence is currently lacking. Randomized studies (eg, NINJA trial) are crucial to guide best practice. Optimum care provision requires matching of the different indications for treatment with appropriate management strategies, with adoption of pediatric-specific PROMs. These should be promoted alongside targeted prevention mechanisms, to reduce the burden of these common injuries.
Footnotes
Published online 20 January 2020.
Disclosures: Aina Greig is the Co-Chief Investigator and Principal Investigator for the Lead Site of the Nailbed INJury Analysis (NINJA) multicentre, pragmatic randomised controlled trial. The other authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Saraf S, Tiwari V. Fingertip injuries. Indian J Orthop. 2007;41:163–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel L. Management of simple nail bed lacerations and subungual hematomas in the emergency department. Pediatr Emerg Care. 2014;30:742–745; quiz 746. [DOI] [PubMed] [Google Scholar]
- 3.Nanninga GL, de Leur K, van den Boom AL, et al. Case report of nail bed injury after blunt trauma; what lies beneath the nail? Int J Surg Case Rep. 2015;15:133–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Qadhi S, Chan KJ, Fong G, et al. Management of uncomplicated nail bed lacerations presenting to a children’s emergency department. Pediatr Emerg Care. 2011;27:379–383. [DOI] [PubMed] [Google Scholar]
- 5.Liu WH, Lok J, Lau MS, et al. Mechanism and epidemiology of paediatric finger injuries at prince of wales hospital in hong kong. Hong Kong Med J. 2015;21:237–242. [DOI] [PubMed] [Google Scholar]
- 6.George A, Alexander R, Manju C. Management of nail bed injuries associated with fingertip injuries. Indian J Orthop. 2017;51:709–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Capstick R, Giele H. Interventions for treating fingertip entrapment injuries in children. Cochrane Database Syst Rev. 2014 Apr 30;(4)CD009808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sierakowski A, Gardiner MD, Jain A, et al. ; Nail bed INJury Analysis (NINJA) Collaborative Group. Surgical treatment of paediatric nail bed injuries in the united kingdom: surgeon and patient priorities for future research. J Plast Reconstr Aesthet Surg. 2016;69:286–288. [DOI] [PubMed] [Google Scholar]
- 9.Dijkers M. Introducing GRADE: a systematic approach to rating evidence in systematic reviews and to guideline development. KT Update. 2013. Available at https://ktdrr.org/products/update/v1n5/ [Google Scholar]
- 10.Algaze I, Snyder AJ, Hodges NL, et al. Children treated in united states emergency departments for door-related injuries, 1999-2008. Clin Pediatr (Phila). 2012;51:226–232. [DOI] [PubMed] [Google Scholar]
- 11.Reid DBC, Shah KN, Eltorai AEM, et al. Epidemiology of finger amputations in the united states from 1997 to 2016 . J Hand Surg Glob Online. 2019;1:45–51. [Google Scholar]
- 12.Yorlets RR, Busa K, Eberlin KR, et al. Fingertip injuries in children: epidemiology, financial burden, and implications for prevention. Hand (N Y). 2017;12:342–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tang JB, Elliot D, Adani R, et al. Repair and reconstruction of thumb and finger tip injuries: a global view. Clin Plast Surg. 2014;41:325–359. [DOI] [PubMed] [Google Scholar]
- 14.Ashbell TS, Kleinert HE, Putcha SM, et al. The deformed finger nail, a frequent result of failure to repair nail bed injuries. J Trauma. 1967;7:177–190. [DOI] [PubMed] [Google Scholar]
- 15.Van Beek AL, Kassan MA, Adson MH, et al. Management of acute fingernail injuries. Hand Clin. 1990;6:23–35; discussion 37. [PubMed] [Google Scholar]
- 16.Pinsolle V, Salmi LR, Evans DM, et al. Reliability of the pulp nail bone (PNB) classification for fingertip injuries. J Hand Surg Eur Vol. 2007;32:188–192. [DOI] [PubMed] [Google Scholar]
- 17.Tamai S. Twenty years’ experience of limb replantation–review of 293 upper extremity replants. J Hand Surg Am. 1982;7:549–556. [DOI] [PubMed] [Google Scholar]
- 18.Gellman H. Fingertip-nail bed injuries in children: current concepts and controversies of treatment. J Craniofac Surg. 2009;20:1033–1035. [DOI] [PubMed] [Google Scholar]
- 19.Carson S, Woolridge DP, Colletti J, et al. Pediatric upper extremity injuries. Pediatr Clin North Am. 2006;53:41–67, v. [DOI] [PubMed] [Google Scholar]
- 20.Reyes BA, Ho CA. The high risk of infection with delayed treatment of open seymour fractures: salter-harris I/II or juxta-epiphyseal fractures of the distal phalanx with associated nailbed laceration. J Pediatr Orthop. 2017;37:247–253. [DOI] [PubMed] [Google Scholar]
- 21.Leddy JP, Packer JW. Avulsion of the profundus tendon insertion in athletes. J Hand Surg Am. 1977;2:66–69. [DOI] [PubMed] [Google Scholar]
- 22.Simon RR, Wolgin M. Subungual hematoma: association with occult laceration requiring repair. Am J Emerg Med. 1987;5:302–304. [DOI] [PubMed] [Google Scholar]
- 23.Roser SE, Gellman H. Comparison of nail bed repair versus nail trephination for subungual hematomas in children. J Hand Surg Am. 1999;24:1166–1170. [DOI] [PubMed] [Google Scholar]
- 24.Seaberg DC, Angelos WJ, Paris PM. Treatment of subungual hematomas with nail trephination: a prospective study. Am J Emerg Med. 1991;9:209–210. [DOI] [PubMed] [Google Scholar]
- 25.Dean B, Becker G, Little C. The management of the acute traumatic subungual haematoma: a systematic review. Hand Surg. 2012;17:151–154. [DOI] [PubMed] [Google Scholar]
- 26.Xu PZ, Fowler JR, Goitz RJ. Prospective randomized trial comparing the efficacy of surgical preparation solutions in hand surgery. Hand (N Y). 2017;12:258–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee KH, Kang DH. Analysis of Nail bed injuries: causes, treatment, results, and prognosis. Hand (New York, N,Y). 2016;111 suppl58S–59S. [Google Scholar]
- 28.Rubin AI, Jellinek NJ, Daniel CR, III, et al. Scher and Daniel’s Nails Diagnosis, Surgery, Therapy. 2018Philadelphia, PA: Springer. [Google Scholar]
- 29.Edwards S, Parkinson L. Is fixing pediatric nail bed injuries with medical adhesives as effective as suturing?: a review of the literature. Pediatr Emerg Care. 2019;35:75–77. [DOI] [PubMed] [Google Scholar]
- 30.Richards AM, Crick A, Cole RP. A novel method of securing the nail following nail bed repair. Plast Reconstr Surg. 1999;103:1983–1985. [DOI] [PubMed] [Google Scholar]
- 31.Hallock GG, Lutz DA. Octyl-2-cyanoacrylate adhesive for rapid nail plate restoration. J Hand Surg Am. 2000;25:979–981. [DOI] [PubMed] [Google Scholar]
- 32.Strauss EJ, Weil WM, Jordan C, et al. A prospective, randomized, controlled trial of 2-octylcyanoacrylate versus suture repair for nail bed injuries. J Hand Surg Am. 2008;33:250–253. [DOI] [PubMed] [Google Scholar]
- 33.Tos P, Titolo P, Chirila NL, et al. Surgical treatment of acute fingernail injuries. J Orthop Traumatol. 2012;13:57–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fiedler DK, Barrett JE, Lourie GM. Nail bed reconstruction using single-layer bovine acellular dermal matrix. J Hand Surg Am. 2017;42:e67–e74. [DOI] [PubMed] [Google Scholar]
- 35.Rohard I, Subotic U, Weber DM. Primary reconstruction of fingernail injuries in children with split-thickness nail bed grafts. Eur J Pediatr Surg. 2012;22:283–288. [DOI] [PubMed] [Google Scholar]
- 36.Gunasagaran J, Sian KS, Ahmad TS. Nail bed and flap reconstructions for acute fingertip injuries - A case review and report of a chemical burn injury. J Orthop Surg (Hong Kong). 2019;27:2309499019839278. [DOI] [PubMed] [Google Scholar]
- 37.Krusche-Mandl I, Köttstorfer J, Thalhammer G, et al. Seymour fractures: retrospective analysis and therapeutic considerations. J Hand Surg Am. 2013;38:258–264. [DOI] [PubMed] [Google Scholar]
- 38.Memon FW. Results of vertical figure-of-eight tension band suture for finger nail disruptions with fractures of distal phalanx. Indian J Orthop. 2012;46:346–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Suitjino D, Silverberg MA. Nailbed injuries treatment & management: emergency department care, consultations, medical care. Medscape:2017.
- 40.Borrelli MR, Dupré S, Mediratta S, et al. Composite grafts for pediatric fingertip amputations: a retrospective case series of 100 patients. Plast Reconstr Surg Glob Open. 2018;6:e1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Champagne L, Hustedt JW, Walker R, et al. Digital tip amputations from the perspective of the nail. Adv Orthop. 2016;2016:1967192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cerny MK, Moog P, Bauer AT, et al. Lipofilling of fingertips for volume defects after fingertip injuries. Ann Plast Surg. 2018;81:653–656. [DOI] [PubMed] [Google Scholar]
- 43.Abzug JM, Kozin SH. Pediatric replantation. J Hand Surg Am. 2014;39:143–145. [DOI] [PubMed] [Google Scholar]
- 44.Atasoy E, Ioakimidis E, Kasdan ML, et al. Reconstruction of the amputated finger tip with a triangular volar flap. A new surgical procedure. J Bone Joint Surg Am. 1970;52:921–926. [PubMed] [Google Scholar]
- 45.Heistein JB, Cook PA. Factors affecting composite graft survival in digital tip amputations. Ann Plast Surg. 2003;50:299–303. [DOI] [PubMed] [Google Scholar]
- 46.Lee DH, Mignemi ME, Crosby SN. Fingertip injuries: an update on management. J Am Acad Orthop Surg. 2013;21:756–766. [DOI] [PubMed] [Google Scholar]
- 47.Butler DP, Murugesan L, Ruston J, et al. The outcomes of digital tip amputation replacement as a composite graft in a paediatric population. J Hand Surg Eur Vol. 2016;41:164–170. [DOI] [PubMed] [Google Scholar]
- 48.Kandel W. Cap-plasty reattachment for unreplantable fingertip amputations. Egypt Orthop J. 2014;49:277–280. [Google Scholar]
- 49.Bharathi RR, Bajantri B. Nail bed injuries and deformities of nail. Indian J Plast Surg. 2011;44:197–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Miranda BH, Vokshi I, Milroy CJ. Pediatric nailbed repair study: nail replacement increases morbidity. Plast Reconstr Surg. 2012;129:394e–396e. [DOI] [PubMed] [Google Scholar]
- 51.Jain A, Sierakowski A, Gardiner MD, et al. Nail bed injury assessment pilot (NINJA-P) study: should the nail plate be replaced or discarded after nail bed repair in children? Study protocol for a pilot randomised controlled trial. Pilot Feasibility Stud. 2015;1:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Altergott C, Garcia FJ, Nager AL. Pediatric fingertip injuries: do prophylactic antibiotics alter infection rates? Pediatr Emerg Care. 2008;24:148–152. [DOI] [PubMed] [Google Scholar]
- 53.Miranda BH, Vokshi I, Milroy CJ. Pediatric nail-bed repair study: part 2. Fact or fixation? Plast Reconstr Surg. 2015;136:717e–719e. [DOI] [PubMed] [Google Scholar]
- 54.Greig A, Gardiner MD, Sierakowski A, et al. ; NINJA Pilot Collaborative. Randomized feasibility trial of replacing or discarding the nail plate after nail-bed repair in children. Br J Surg. 2017;104:1634–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Riley AW. Evidence that school-age children can self-report on their health. Ambul Pediatr. 2004;44 suppl371–376. [DOI] [PubMed] [Google Scholar]
- 56.Shauver MJ, Chung KC. The michigan hand outcomes questionnaire after 15 years of field trial. Plast Reconstr Surg. 2013;131:779e–787e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Quatman-Yates CC, Gupta R, Paterno MV, et al. Internal consistency and validity of the quickdash instrument for upper extremity injuries in older children. J Pediatr Orthop. 2013;33:838–842. [DOI] [PubMed] [Google Scholar]
- 58.Garra G, Singer AJ, Taira BR, et al. Validation of the wong-baker FACES pain rating scale in pediatric emergency department patients. Acad Emerg Med. 2010;17:50–54. [DOI] [PubMed] [Google Scholar]
- 59.Zook EG, Guy RJ, Russell RC. A study of nail bed injuries: causes, treatment, and prognosis. J Hand Surg Am. 1984;9:247–252. [DOI] [PubMed] [Google Scholar]


