Abstract
Background:
Peripheral arterial disease is an important vascular complication of diabetes that may lead to lower-extremity amputation. We aimed to compare the treatment and complications of peripheral arterial disease between First Nations people and other people in Ontario with diabetes.
Methods:
Using health care administrative databases, we identified annual cohorts, from 1995/96 to 2014/15, of all people aged 20–105 years in Ontario with a diagnosis of diabetes. We used the Indian Register to identify those who were First Nations people and compared them to all other people in Ontario. We identified revascularization procedures (angioplasty or bypass surgery) and lower-extremity amputation procedures in the 2 populations and determined the mortality rate among those who had had lower-extremity amputation.
Results:
First Nations people received revascularization procedures at a rate comparable to that for other people in Ontario. However, they had lower-extremity amputation procedures at 3–5 times the frequency for other Ontario residents. First Nations people had higher mortality than other people in Ontario after lower-extremity amputation (adjusted hazard ratio 1.15, 95% confidence interval 1.05–1.26), with median survival of 3.5 years versus 4.1 years.
Interpretation:
First Nations people in Ontario had a markedly increased risk for lower-extremity amputation compared to other people in Ontario, and their mortality rate after amputation was 15% higher. Future research is needed to understand what barriers First Nations people face to receive adequate peripheral arterial disease care and what interventions are necessary to achieve equitable outcomes of peripheral arterial disease for First Nations people in Ontario.
Peripheral arterial disease is an important vascular complication of diabetes. More than 1 in 5 people with symptomatic peripheral arterial disease have diabetes.1 The most common symptom of peripheral arterial disease is intermittent claudication, but over half of patients have other, atypical symptoms, with reduced activity and impaired quality of life.2 Peripheral arterial disease can progress to critical limb ischemia, which is characterized by rest pain, tissue loss or gangrene. In addition, distal sensory polyneuropathy, as a microvascular complication of diabetes, can augment the risk of lower extremity injury and infection. As a result, peripheral arterial disease can lead to lower-extremity amputation, which is one of the most feared complications of diabetes and affects quality of life substantially.3,4 More than 80% of lower-extremity amputation procedures in Canada occur in patients with diabetes.5 As a marker for generalized atherosclerosis, peripheral arterial disease also portends other cardiovascular disease, such as myocardial infarction or stroke.
First Nations people in Ontario have a high and growing prevalence of diabetes that exceeds that of other people in the province.6 Previous research has also suggested that First Nations people have a disproportionate burden of peripheral arterial disease.7 For example, a physical examination screening study in a northern Manitoba First Nations community showed a prevalence of impaired pulse of 41% and a prevalence of foot ulcer history of 15%.8 The objective of the present study was to compare the treatment and complications of peripheral arterial disease between First Nations people and other people in Ontario with diabetes.
Methods
Setting and population
In Ontario, ICES maintains comprehensive linked administrative data sets related to the province’s single-payer publicly funded health care system. The general approach to cohort creation, description of the major data sets used and a description of the characteristics of the study cohorts are described in detail elsewhere.9 In brief, we examined annual cohorts of all people aged 20–105 years with diagnosed diabetes in Ontario. We identified First Nations people using the Indian Register, which includes information for all people registered as Status First Nations people under the Indian Act. All other residents were classified as “other people in Ontario.”
Outcome measures and analyses
Using the Canadian Institute for Health Information Discharge Abstract Database, which captures administrative, clinical and demographic information on hospital discharges in Ontario, we determined the proportion of patients in each annual cohort between 2002/03 and 2014/15 who had a revascularization procedure (angioplasty or bypass surgery) to treat peripheral arterial disease in that fiscal year. We then determined the proportion of patients who had a lower-extremity amputation in each annual cohort between 1995/96 and 2014/15. (Amputation procedures could more readily be ascertained in the database before 2002 than revascularization procedures, so we used a longer period for this outcome.) Procedures were classified as minor (toe or foot) or major (at the ankle, below the knee or above the knee). We excluded any procedures where the diagnosis recorded during the same hospital stay was for malignant or benign lower-extremity tumours, trauma, frostbite or burns. Event rates were age-and sex-standardized to the overall 2001 Ontario population, and γ-distributed confidence intervals were calculated. We also examined age-adjusted rates for men and women separately, sex-adjusted rates by age, and age- and sex-adjusted rates by location, in 2014/15 only. We defined location by the Rurality Index of Ontario score for each person’s community of residence, as defined from their home address postal code, and classified it as urban, semiurban or rural based on community characteristics.10 Communities that did not have a Rurality Index of Ontario score were classified as remote.
We then analyzed the data for all people who had major lower-extremity amputation procedures between 2002/03 and 2014/15, and followed them forward until March 2018 for the outcome of all-cause mortality. For people who had more than 1 lower-extremity amputation procedure during this period, we counted the first procedure. We compared First Nations people to other people in Ontario using a Cox proportional hazards model, adjusting for age and sex, with censoring on loss of Ontario health care coverage. The adjusted survival curve was plotted. Analyses were conducted with SAS Enterprise Guide version 7.1 (SAS Institute).
Ethics approval
The project was approved by the Chiefs of Ontario Data Governance Committee. The study also received research ethics review from Queen’s University and Laurentian University.
Results
The demographic characteristics of the population under study are described elsewhere.6 Table 1 shows the characteristics of the annual cohorts from 2002/03 and 2014/15. Compared to other people in Ontario with diabetes, the cohort of First Nations people with diabetes had a greater proportion of women, were younger and were more likely to live in rural areas.
Table 1:
Demographic characteristics of First Nations people and other people in Ontario with diabetes, 2002/03 and 2014/15
| Characteristic | 2002/03; no. (%) of people | 2014/15; no. (%) of people | ||
|---|---|---|---|---|
|
|
|
|||
| First Nations people n = 13 573 |
Other people in Ontario n = 680 880 |
First Nations people n = 23 011 |
Other people in Ontario n = 1 364 136 |
|
| Sex | ||||
|
| ||||
| Male | 6074 (44.8) | 354 541 (52.1) | 10 687 (46.4) | 709 016 (52.0) |
|
| ||||
| Female | 7499 (55.2) | 326 339 (47.9) | 12 324 (53.6) | 655 120 (48.0) |
|
| ||||
| Age, yr | ||||
|
| ||||
| ≤ 19 | 175 (1.3) | 7517 (1.1) | 289 (1.3) | 11 558 (0.8) |
|
| ||||
| 20–34 | 1396 (10.3) | 29 581 (4.3) | 1615 (7.0) | 42 553 (3.1) |
|
| ||||
| 35–49 | 4222 (31.1) | 118 063 (17.3) | 5654 (24.6) | 190 112 (13.9) |
|
| ||||
| 50–64 | 5056 (37.2) | 225 880 (33.2) | 9238 (40.1) | 472 026 (34.6) |
|
| ||||
| 65–74 | 1908 (14.1) | 164 265 (24.1) | 4108 (17.8) | 337 358 (24.7) |
|
| ||||
| 75–105 | 816 (6.0) | 135 574 (19.9) | 2107 (9.2) | 310 529 (22.8) |
|
| ||||
| Location | ||||
|
| ||||
| Urban | 3228 (23.8) | 480 927 (70.6) | 6277 (27.3) | 989 684 (72.6) |
|
| ||||
| Semiurban | 2780 (20.5) | 134 164 (19.7) | 4587 (19.9) | 262 062 (19.2) |
|
| ||||
| Rural | 2526 (18.6) | 59 893 (8.8) | 3865 (16.8) | 103 246 (7.6) |
|
| ||||
| Remote/missing | 5039 (37.1) | 5896 (0.9) | 8282 (36.0) | 9144 (0.7) |
|
| ||||
| Comorbidity* | ||||
|
| ||||
| Low | 3122 (23.0) | 119 756 (17.6) | 5075 (22.1) | 256 192 (18.8) |
|
| ||||
| Medium | 5526 (40.7) | 295 761 (43.4) | 8850 (38.5) | 576 794 (42.3) |
|
| ||||
| High | 4925 (36.3) | 265 363 (39.0) | 9086 (39.5) | 531 150 (38.9) |
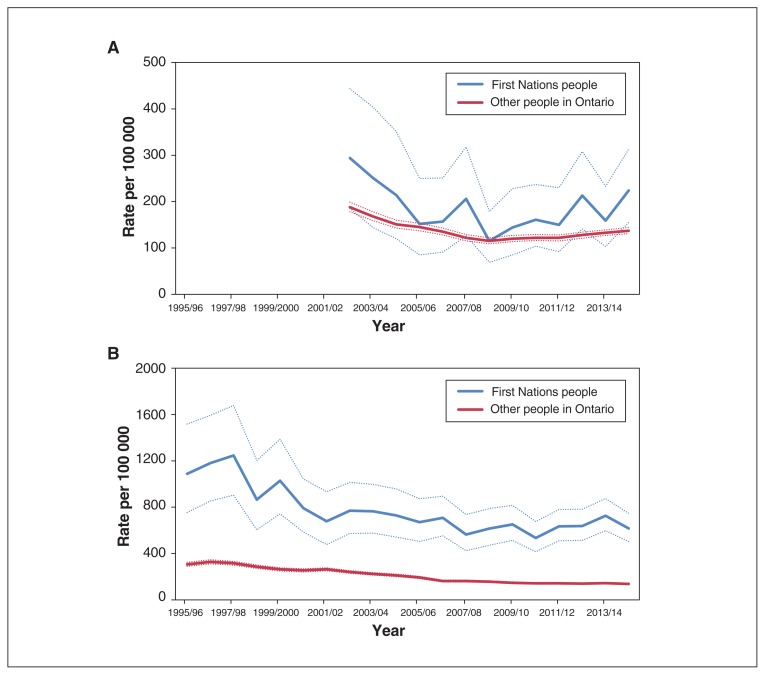
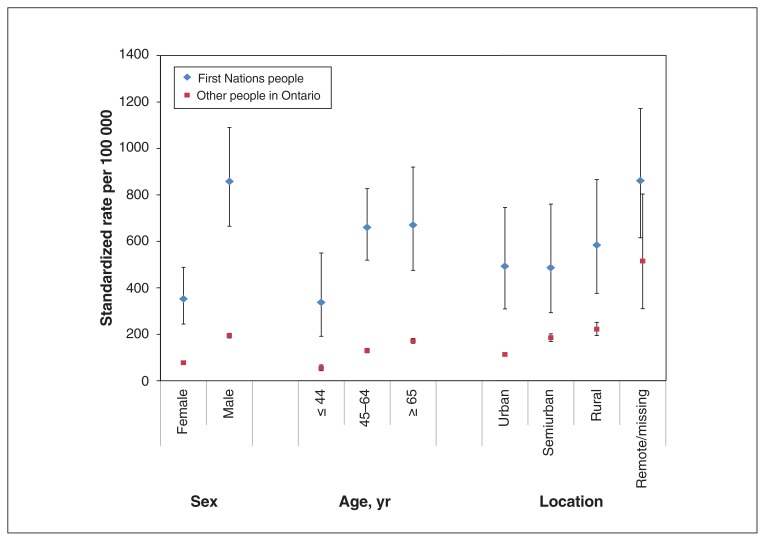
The age- and sex-adjusted rates of revascularization procedures and lower-extremity amputation for First Nations people and other people in Ontario over time are shown in Figure 1. In both populations and across time, about half of all lower-extremity amputation procedures were minor, and half were major.12 Figure 2 shows the lower-extremity amputation rates by age, sex and location for 2014/15 only. First Nations people had a markedly higher rate of amputation than other people in Ontario across all age, sex and location strata. The rates were higher for men than for women among both First Nations people and other people in Ontario. The rates increased with increasing age and increasing rurality in both populations. Those living in remote communities were at particularly increased risk.
Figure 1:
Age- and sex-adjusted rates and 95% confidence intervals of A) revascularization procedures (angioplasty or bypass surgery) (2002/03 to 2014/15) and B) lower-extremity amputation (1995/96 to 2014/15) per 100 000 people with diabetes among First Nations people and other people in Ontario.
Figure 2:
Age-adjusted rates by sex, sex-adjusted rates by age, and age- and sex-adjusted rates by location of lower-extremity amputation among First Nations people and other people in Ontario, 2014/15. Error bars represent 95% confidence intervals.
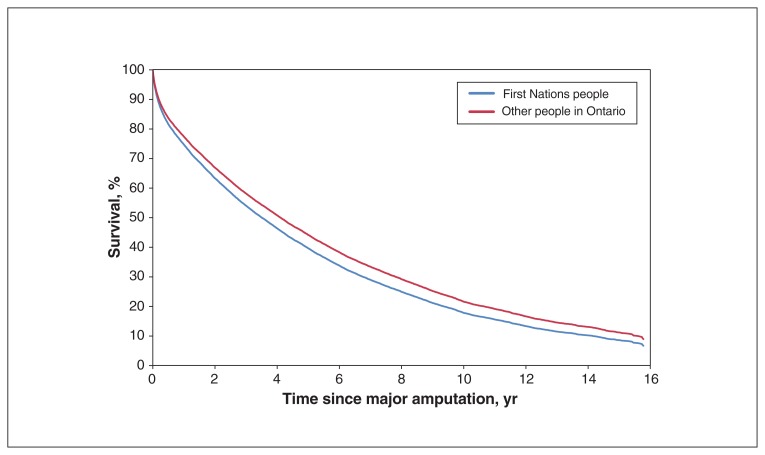
Figure 3 shows survival for the 12 847 people who had a major lower-extremity amputation between 2002/03 and 2014/15. The risk of death after lower-extremity amputation was very high, with a median survival of 3.5 years among First Nations people and 4.1 years among other people in Ontario. The age- and sex-adjusted hazard ratio for mortality among First Nations people was 1.15 (95% confidence interval 1.05–1.26) compared to other Ontarians.
Figure 3:
Adjusted survival curve after major lower-extremity amputation for First Nations people and other people in Ontario.
Interpretation
First Nations people with diabetes underwent revascularization procedures to treat peripheral arterial disease at rates comparable to those for other people in Ontario. However, their rate of lower-extremity amputation was 3–5 times higher than that for other people in Ontario. Since revascularization occurs earlier in the course of disease than amputation, these discordant findings suggest that peripheral arterial disease may be underdiagnosed or undertreated among First Nations people with diabetes, so many patients may not come to medical attention until irreversible complications have already occurred, necessitating amputation. Lower-extremity amputation rates were higher for men than for women among both First Nations people and other people in Ontario. Regarding age, the greatest disparity in rates between the 2 populations was in the youngest age group (≤ 44 yr), with lower-extremity amputation occurring more than 6 times as frequently in First Nations people than in people in Ontario. This increased risk attenuated by age 65 years or more but was still nearly fourfold. Among both First Nations people and other people in Ontario, the risk of lower-extremity amputation increased with increasing rurality. Lower-extremity amputation was strongly predictive of death, with a median survival of only 3.5 years after amputation among First Nations people, 0.6 years less than among other people in Ontario.
This high burden of lower-extremity amputation may have been driven in part by the high prevalence of many of the risk factors for peripheral arterial disease, including smoking and hypertension.12 Yet the magnitude of incremental risk for other macrovascular complications of diabetes, including coronary artery disease and stroke,12,13 faced by First Nations people is not nearly as dramatic as it is for lower-extremity amputation. Therefore, there are likely other factors contributing to this risk. For example, First Nations people may face barriers to screening for milder degrees of peripheral arterial disease, which results in missed opportunities for early intervention and presentation with more advanced disease. A previous study showed that the lower-extremity amputation rates for First Nations people in Manitoba varied by specialist consultation rate and by tribal council, which suggests that health care access may be an important factor.14 In addition, First Nations people may have an increased risk for distal polyneuropathy as a microvascular complication of diabetes, which would increase the risk of foot ulcers that could eventually necessitate lower-extremity amputation. However, this was not an outcome that could be ascertained with our data. Living in remote communities was a risk factor for lower-extremity amputation for both First Nations people and other people in Ontario. This disparity is likely driven in part by poor access to health care, particularly specialized services for wound care and rehabilitation, in these areas. Since more than a third of First Nations people live in remote communities (Table 1), these health care barriers will particularly affect them.
Our results corroborate previous research from Alberta, which showed an approximately threefold increased risk of lower-extremity amputation for First Nations people compared to non–First-Nations people.15 Previous research has shown that lower socioeconomic status is an important independent predictor of lower-extremity amputation in people with diabetes in Ontario,16 and First Nations people have marked disparities in socioeconomic measures.17,18 However, a Manitoba study of First Nations people showed that average income at the tribal council level was not associated with lower-extremity amputation rates.14 A Manitoba study showed that Indigenous people were more likely than non-Indigenous people to require lower-extremity amputation for an emergent indication (such as gangrene or nonhealing foot ulcer), but there was no difference between the 2 groups in perioperative morbidity or long-term mortality.19 In another Manitoba study, the investigators compared outcomes of lower-extremity amputation between First Nations/Métis people and non-Indigenous people.20 Rehabilitation use and duration were similar, but First Nations and Métis people were less likely than non-Indigenous people to experience phantom pain after amputation. We were not able to examine rehabilitation use in our study.
Strengths and limitations
This study has important strengths. It was a participatory research collaboration between academics and representatives of First Nations communities, who were involved throughout the study. In addition, we conducted a population-based study of all people across Ontario and used provincial health care administrative databases that capture all outcome events. Thus, the study had sufficient sample size to be adequately powered to examine rare events such as lower-extremity amputation. However, there are important limitations to highlight. We could identify only major surgical procedures for peripheral arterial disease: revascularization and lower-extremity amputation. Less severe manifestations of peripheral arterial disease, such as symptoms of impaired circulation, foot ulcers or arterial blockages not suitable for intervention, could not be ascertained. As the study relied on secondary data not collected prospectively for research purposes, procedures may have been miscoded, which would have led to misclassification of outcomes. In addition, procedures for Ontarians living in the northwest of the province, where patients requiring specialist services may be referred to Winnipeg, may have been undercounted in our data. As a result, we may have underestimated event rates among those living in this area, which includes a large population of First Nations people. Third, the Ontario Diabetes Database does not distinguish between types of diabetes; however, the vast majority of people with diabetes in the population have type 2. As noted elsewhere in this series,9 the use of neighbourhood-level household income as a proxy for individual-level socioeconomic status is inaccurate among First Nations people, so we were unable to account for socioeconomic status in these analyses. Finally, First Nations people who are not registered with the Indian Register, including members of First Nations not recognized by the federal government, will not have been captured in the First Nations population of this study.
Conclusion
Although First Nations people with diabetes had rates of revascularization procedures to treat peripheral arterial disease comparable to those for other people with diabetes in Ontario, they had an increased risk of lower-extremity amputation, particularly younger people. These results suggest that peripheral arterial disease may be underdiagnosed or undertreated among First Nations people in Ontario. Lower-extremity amputation markedly affects quality of life and is associated with a high mortality rate, which, in the current study, was 15% higher for First Nations people than for other people in Ontario. These results show the health inequities faced by First Nations people and the impact of social, economic and cultural determinants of health.17 Future research is needed to understand what barriers First Nations people face to receive adequate peripheral arterial disease care and what interventions are necessary to achieve equitable outcomes of peripheral arterial disease for First Nations people in Ontario.
Supplementary Material
Acknowledgements
The authors’ partner through the early design, implementation and final dissemination of this project is the Chiefs of Ontario. Their many member contributions were key to the content and quality of the project. The authors also acknowledge the members of the Patient Advisory Committee for providing insightful and thoughtful input; their advice made a significant contribution in shaping the work. For a complete listing of the specific members of the Committee, see Green and colleagues.12 The authors also acknowledge the First Nations people from Big Grassy River First Nation, Alderville First Nation, Caldwell First Nation, Six Nations of the Grand River and Moose Cree First Nation with diabetes who shared their personal experiences. They also thank Susan Schultz for developing the methodology to identify where First Nations people live and Rahim Moineddin for his guidance on statistical analyses.
See related research article at www.cmajopen.ca/lookup/doi/10.9778/cmajo.20190096
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
Contributors: Shahriar Khan analyzed the data. Baiju Shah drafted the manuscript. All of the authors contributed to the conception and design of the study and to data interpretation, revised the manuscript critically for important intellectual content, approved the final version to be published and agreed to be accountable for all aspects of the work.
Funding: This study was supported by an Ontario SPOR SUPPORT Unit IMPACT Award. Additional support was provided to Michael Green through the Brian Hennen Chair in Family Medicine, Queen’s University, to Jennifer Walker through a Tier 2 Canada Research Chair in Indigenous Health and by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care.
Disclaimer: Parts of this material are based on data and information compiled and provided by the Ontario Ministry of Health and Long-Term Care (MOHLTC), Cancer Care Ontario and the Canadian Institute for Health Information. This study was supported by ICES, which is funded by an annual grant from the MOHLTC. The analyses, conclusions, opinions and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
Supplemental information: For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/7/4/E700/suppl/DC1.
References
- 1.Murabito JM, D’Agostino RB, Silbershatz H, et al. Intermittent claudication: a risk profile from the Framingham Heart Study. Circulation. 1997;96:44–9. doi: 10.1161/01.cir.96.1.44. [DOI] [PubMed] [Google Scholar]
- 2.Hiatt WR. Medical treatment of peripheral arterial disease and claudication. N Engl J Med. 2001;344:1608–21. doi: 10.1056/NEJM200105243442108. [DOI] [PubMed] [Google Scholar]
- 3.Zhang P, Brown MB, Bilik D, et al. Health utility scores for people with type 2 diabetes in U.S. managed care health plans: results from Translating Research Into Action for Diabetes (TRIAD) Diabetes Care. 2012;35:2250–6. doi: 10.2337/dc11-2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Reilly DJ, Xie F, Pullenayegum E, et al. Estimation of the impact of diabetes-related complications on health utilities for patients with type 2 diabetes in Ontario, Canada. Qual Life Res. 2011;20:939–43. doi: 10.1007/s11136-010-9828-9. [DOI] [PubMed] [Google Scholar]
- 5.Kayssi A, de Mestral C, Forbes TL, et al. A Canadian population-based description of the indications for lower-extermity amputations and outcomes. Can J Surg. 2016;59:99–106. doi: 10.1503/cjs.013115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Walker JD, Slater M, Jones CR, et al. Diabetes prevalence and incidence in First Nations people in Ontario: a cohort study using linked administrative data. CMAJ. 2019 doi: 10.1503/cmaj.190836. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bonneau C, Caron NR, Hussain MA, et al. Peripheral artery disease among Indigenous Canadians: What do we know? Can J Surg. 2018;61:305–10. doi: 10.1503/cjs.013917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reid KS, Martin BD, Duerksen F, et al. Diabetic foot complications in a northern Canadian Aboriginal community. Foot Ankle Int. 2006;27:1065–73. doi: 10.1177/107110070602701212. [DOI] [PubMed] [Google Scholar]
- 9.Slater M, Green ME, Shah B, et al. First Nations people with diabetes in Ontario: methods for a longitudinal population-based cohort study. CMAJ Open. 2019;7:E680–8. doi: 10.9778/cmajo.20190096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kralj B. Measuring “rurality” for purposes of health-care planning: an empirical measure for Ontario. Ont Med Rev. 2000;67:33–52. [Google Scholar]
- 11.The Johns Hopkins ACG Case-Mix System reference manual version 7.0. Baltimore: Johns Hopkins Bloomberg School of Public Health; 2005. [Google Scholar]
- 12.Green ME, Jones C, Walker JD, et al., editors. First Nations and diabetes in Ontario. Toronto: ICES; 2019. [Google Scholar]
- 13.Chu A. Trends in cardiovascular care and event rates among First Nations and other people with diabetes in Ontario, Canada, 1996–2015. CMAJ. 2019;191:E1291–8. doi: 10.1503/cmaj.190899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martens PJ, Martin BD, O’Neil JD, et al. Diabetes and adverse outcomes in a First Nations population: associations with healthcare access, and socioeconomic and geographical factors. Can J Diabetes. 2007;31:223–32. [Google Scholar]
- 15.First Nations — health trends Alberta. Analytics and Performance Reporting Branch, Health Standards, Quality and Performance Division, Alberta Health; 2017. Mar 7, [accessed 2019 July 9]. Lower leg amputations among Albertans with diabetes. Available: www.afnigc.ca/main/includes/media/pdf/fnhta/HTAFN-2017-03-07-Diabetes_Amputations.pdf. [Google Scholar]
- 16.Amin L, Shah BR, Bierman AS, et al. Gender differences in the impact of poverty on health: disparities in risk of diabetes-related amputation. Diabet Med. 2014;31:1410–7. doi: 10.1111/dme.12507. [DOI] [PubMed] [Google Scholar]
- 17.King M, Smith A, Gracey M. Indigenous health part 2: the underlying causes of the health gap. Lancet. 2009;374:76–85. doi: 10.1016/S0140-6736(09)60827-8. [DOI] [PubMed] [Google Scholar]
- 18.Anand SS, Yusuf S, Jacobs R, et al. Risk factors, atherosclerosis, and cardiovascular disease among Aboriginal people in Canada: the Study of Health Assessment and Risk Evaluation in Aboriginal Peoples (SHARE-AP) Lancet. 2001;358:1147–53. doi: 10.1016/s0140-6736(01)06255-9. [DOI] [PubMed] [Google Scholar]
- 19.Goulet S, Trepman E, Cheang M, et al. Revascularization for peripheral vascular disease in Aboriginal and non-Aboriginal patients. J Vasc Surg. 2006;43:735–41. doi: 10.1016/j.jvs.2005.11.058. [DOI] [PubMed] [Google Scholar]
- 20.Meatherall BL, Garrett MR, Kaufert J, et al. Disability and quality of life in Canadian Aboriginal and non-Aboriginal diabetic lower-extremity amputees. Arch Phys Med Rehabil. 2005;86:1594–602. doi: 10.1016/j.apmr.2004.11.026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.