Summary
Background
Although many meta-analyses have examined the association between childhood sexual abuse and subsequent outcomes, the scope, validity, and quality of this evidence has not been comprehensively assessed. We aimed to systematically review existing meta-analyses on a wide range of long-term psychiatric, psychosocial, and physical health outcomes of childhood sexual abuse, and evaluate the quality of the literature.
Methods
In this umbrella review, we searched four databases (PsycINFO, PubMed, Cumulative Index to Nursing and Allied Health Literature, and Global Health) from inception to Dec 31, 2018, to identify meta-analyses of observational studies that examined the association between childhood sexual abuse (before 18 years of age) and long-term consequences (after 18 years). We compared odds ratios (ORs) across different outcomes. We also examined measures of quality, including heterogeneity between studies and evidence for publication bias. This study is registered with PROSPERO, CRD42016049701.
Findings
We identified 19 meta-analyses that included 559 primary studies, covering 28 outcomes in 4 089 547 participants. Childhood sexual abuse was associated with 26 of 28 specific outcomes: specifically, six of eight adult psychiatric diagnoses (ORs ranged from 2·2 [95% CI 1·8–2·8] to 3·3 [2·2–4·8]), all studied negative psychosocial outcomes (ORs ranged from 1·2 [1·1–1·4] to 3·4 [2·3–4·8]), and all physical health conditions (ORs ranged from 1·4 [1·3–1·6] to 1·9 [1·4–2·8]). Strongest psychiatric associations with childhood sexual abuse were reported for conversion disorder (OR 3·3 [95% CI 2·2–4·8]), borderline personality disorder (2·9 [2·5–3·3]), anxiety (2·7 [2·5–2·8]), and depression (2·7 [2·4–3·0]). The systematic reviews for two psychiatric outcomes (post-traumatic stress disorder and schizophrenia) and one psychosocial outcome (substance misuse) met high quality standards. Quality was low for meta-analyses on borderline personality disorder and anxiety, and moderate for conversion disorder. Assuming causality, population attributable risk fractions for outcomes ranged from 1·7% (95% CI 0·7–3·3) for unprotected sexual intercourse to 14·4% (8·8–19·9) for conversion disorder.
Interpretation
Although childhood sexual abuse was associated with a wide range of psychosocial and health outcomes, systematic reviews on only two psychiatric disorders (post-traumatic stress disorder and schizophrenia) and one psychosocial outcome (substance misuse) were of a high quality. Whether services should prioritise interventions that mitigate developing certain psychiatric disorders following childhood abuse requires further review. Higher-quality meta-analyses for specific outcomes and more empirical studies on the developmental pathways from childhood sexual abuse to later outcomes are necessary.
Funding
Wellcome Trust.
Introduction
Child sexual abuse is a global public health concern and is associated with a wide range of adverse outcomes. A meta-analysis of 217 publications has reported a global prevalence of 12% on the basis of 331 independent samples comprising about 10 million individuals.1 Studies have reported associations between childhood sexual abuse and many psychosocial and health-related outcomes, including psychosocial problems,2,3 self-harm,4 psychiatric disorders,5–7 and physical health diagnoses such as HIV8 and obesity.9 These reports have raised important questions about the extent of association between childhood sexual abuse and long-term outcomes in adulthood, the relative effects of childhood sexual abuse on different outcomes, and the quality of the current research base. For example, the long-term effects of sexual abuse on psychiatric outcomes might be stronger than that on physical health ones because of possible over-reporting of symptoms in individuals with psychiatric disorders.10,11
Previous attempts to synthesise the large number of meta-analytical reviews in the field have mostly considered solely mental health outcomes or a single outcome, such as depression, anxiety disorders, suicide and self-injury, or substance misuse.12–15 These reviews have been difficult to compare because their definitions of childhood sexual abuse have differed, they have included different types of study design, and the outcomes vary from diagnoses to self-report markers of morbidity. Furthermore, it has not been possible to identify research gaps in the field, and determine outcomes that are not synthesised or whether there are differential effects of childhood sexual abuse on outcomes. In addition, these reviews have usually been based on small sample sizes and searched literature that is typically more than a decade old, and lack quantitative synthesis and quality assessment.12–17 We aimed to address these limitations and provide an overview of the breadth and validity of the associations of childhood sexual abuse with a diverse range of long-term important psychosocial, psychiatric, and physical health outcomes. Our goal was to provide a comprehensive synthesis of the effects of childhood sexual abuse on morbidity and disability in adulthood, which could help to identify targets for clinical and policy interventions.
Methods
Search strategy and eligibility criteria
We did an umbrella review, in which information from existing meta-analyses of studies on outcomes of childhood sexual abuse was systematically collected and evaluated. We did a keyword search of titles and abstracts in four major digital databases, PsycINFO, PubMed, Cumulative Index to Nursing and Allied Health Literature, and Global Health, for papers published from database inception to Dec 31, 2018, with no language restriction. These databases included dissertation abstracts, and our search included unpublished grey studies. The same keywords were used for each database search for sexual abuse (“sexual abuse” OR “sexual assault” OR “sexual trauma” OR “sexual crime” OR “rape” OR “incest” OR “molestation” OR “victim*” OR “maltreatment”), childhood (“child*” OR “youth” OR “adolescent” OR “young” OR “teen*”), and meta-analysis (“meta-analy*” OR “meta-regression” OR “meta-synthesis”). To include a maximum number of eligible studies that examined long-term outcomes of childhood sexual abuse, we did not set any limit on the outcome in the primary systematic search. We did a secondary search in PsycINFO for the top ten global disability-adjusted life-year (DALY) risks,18 as well as for the top ten global mental and behavioural health DALYs (appendix p 1).19 The references of other umbrella reviews on outcomes of childhood sexual abuse were manually searched.12–17 We also used forward and backward citation chaining to supplement our search.
Inclusion criteria were meta-analyses that reported outcome data for childhood sexual abuse, disaggregated from other forms of abuse; in which the majority of outcomes were in adults (defined as average participant age at time of outcome measurement was older than 18 years for more than 70% of the included primary studies); in which the majority of participants were children at the time of abuse (defined as average participant age at time of abuse being younger than 18 years for more than 70% of the included primary studies); and that provided aggregate quantitative effect sizes for health or psychosocial outcomes (eg, odds ratio, Pearson’s r, or Cohen’s d).
When more than one meta-analysis reported data for the same outcome, the most recent review that met our inclusion criteria was selected, and older meta-analyses were excluded to avoid duplication of samples. When two or more meta-analyses reported data for the same outcome and were published within the same year, the meta-analysis including the greatest number of primary studies was selected, and the others were excluded.20–27 One study was unavailable (and author not contactable).28 In addition, we excluded studies only reporting prevalence of childhood sexual abuse in a selected sample with a certain outcome (eg, homelessness).29
Because data collection resulted in effect size statistics for nearly 100 different outcomes, they were systematically narrowed down using the following criteria: for health outcomes, specific diagnoses (eg, schizophrenia and fibromyalgia) and related symptoms (eg, psychosis and pain) were included, but subcategories of diagnosis (eg, social phobia as a subcategory of anxiety and anorexia nervosa as a subtype of eating disorder) and other symptoms (eg, cardiopulmonary symptoms and chronic pelvic pain) were excluded (appendix pp 2–3). Of psychosocial outcomes, the ten outcomes including the largest number of primary studies, ranging from seven to 45 primary studies, were included (eg, adult sexual revictimisation and substance misuse), whereas outcomes including fewer primary studies, ranging from two to six primary studies, were excluded (eg, recent unprotected anal intercourse, online sexual offending compared with offline sexual offending, self-esteem, and hostility). There was some duplication of participants between anxiety and anxiety symptomatology, and depression and depressive symptomatology. Therefore, the actual sample sizes might be slightly smaller. Because the odds ratio (OR) for sleep disorders (16·2 [95% CI 2·1–126·8]) was derived from a single primary study and had a large 95% CI, these data were excluded as an outlier. The minimum number of primary studies in the eligible meta-analytical reviews was three.
Data extraction was conducted following a predetermined data extraction form (appendix pp 4–5). Effect sizes were extracted from the most parsimonious model because not all studies provided adjusted effect sizes. Sources of heterogeneity, if examined, were reported. The initial screening for inclusion and exclusion of studies was conducted by HPH. A second extractor (SG) was involved in the extraction of effect sizes. In the case of any uncertainty in inclusion and exclusion of studies and data extraction, RY and SF were consulted and any conflicts were resolved through discussion between HPH, RY, and SF. A study protocol was registered with PROSPERO.30
Data analysis
All effect sizes and CIs were converted into ORs to enable comparison across outcomes.31,32 That is, estimates of effects from each meta-review were converted into a common metric, ORs, representing the odds that an outcome (eg, suicide) would occur given a particular exposure (childhood sexual abuse) compared with the odds of the outcome occurring in the absence of that exposure. We calculated population attributable fractions for each outcome on the basis of the relative risk due to childhood sexual abuse and the proportion of the population exposed to childhood sexual abuse, assuming causality between exposure and outcomes.33 No confounder-adjusted effect size data were reported for outcomes, so we calculated population attributable fractions using the confounder-unadjusted attributable risk formula and the conservative 10% prevalence estimate of childhood sexual abuse.34–36
The AMSTAR (a measurement tool to assess systematic reviews) checklist was used to assess the methodological quality of the included systematic reviews,37 and some items were modified for this umbrella review (appendix pp 6–7). For all studies, one point was awarded for each of the eleven criteria met. Scores of 0–3 were considered low, scores of 4–7 were considered medium, and scores of 8–11 were considered high quality.37 HPH and RY did the quality assessment.
Quality was further assessed in the following ways. First, we measured heterogeneity, the relative inconsistency of studies pooled in a particular meta-analysis, using the I2 statistic.38 I2 is reported as a percentage, where scores of less than 50% were considered low heterogeneity.39 Second, we applied the excess significance test, a measure of publication bias that compares the expected versus the observed significance in a meta-analysis.40 Excess significance was calculated as a ratio of the overall OR of each meta-analysis to the OR of the largest primary study included in that meta-analysis, with a ratio greater than 1 indicating bias for publication of an excess number of significant results in the literature.41 To supplement the evaluation of excess significance, we also collected information on another marker of publication bias, small study effects, from the individual meta-analysis included. Third, when data on τ2 estimated heterogeneity and SE (standard error of the effect sizes) were available, prediction intervals were calculated. A 95% prediction interval gives a range of scores in which a future sample statistic can be said to fall with 95% certainty. If the prediction interval includes the null OR of 1, future studies might find that the exposure produced no effect or the opposite effect on the outcome.42
We created an overall quality assessment. Each outcome was assigned a score of 0 or 1 for the five categories of heterogeneity between studies (I2), publication bias (excess statistical significance and small study effects), prediction intervals, and AMSTAR quality measurement scores, with 0 representing low quality and 1 representing high. The five quality analysis scores were then summed to determine an aggregate quality score within the range of 0–5, with 0 designating the lowest overall quality and 5 designating the highest. Because this study is an umbrella review of systematic reviews, we did not assess the quality of individual studies included in each systematic review. ORs were presented in a forest plot using STATA, version 14.
This study is registered with PROSPERO, CRD42016049701.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. HPH had full access to all the data in the study, and all authors had final responsibility for the decision to submit for publication.
Results
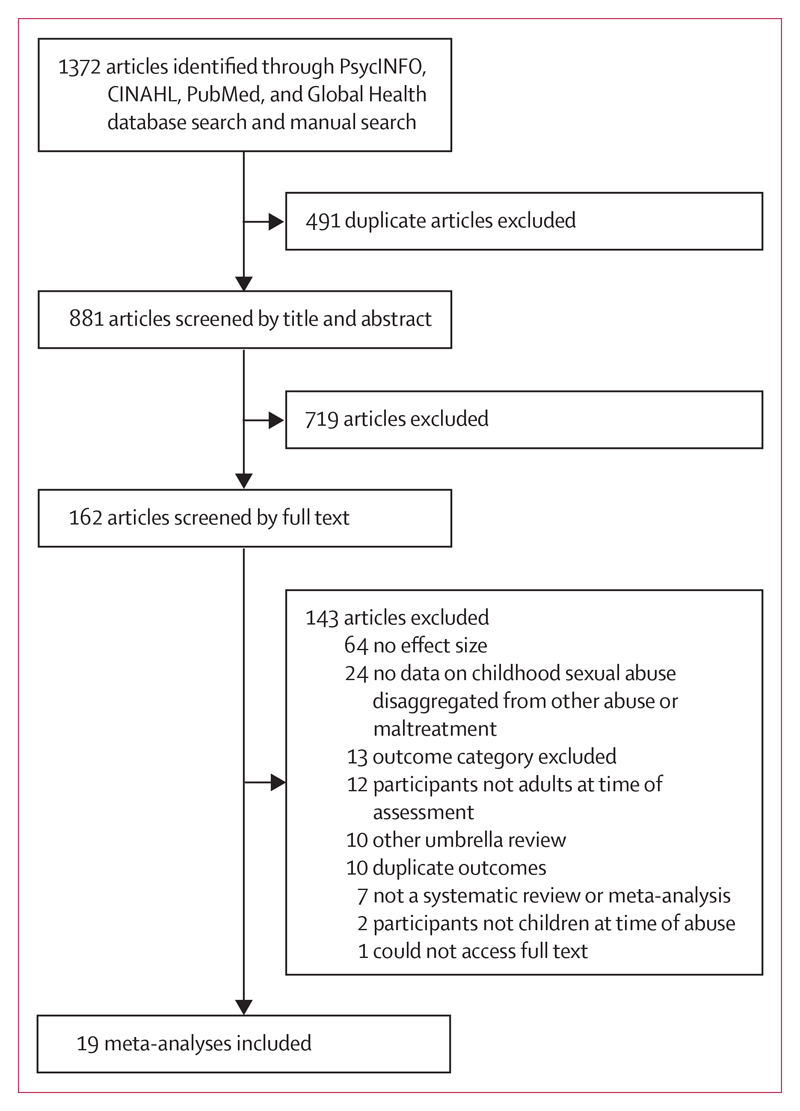
The initial database and manual search yielded 1372 articles (figure 1). We identified 19 eligible meta-analyses with 4 089 547 participants across 28 outcomes and 559 primary studies (table 1).2,3,5–9,43–54 All meta-analyses were published between 1996 and 2018, and the primary studies included in these meta-analyses were reported from 1971 to 2017. The number of primary studies in each meta-analysis ranged from three to 62, and the number of participants ranged from 140 to more than 3 million.6 Outcomes included in the eligible meta-analyses were divided into psychosocial, psychiatric, and physical health outcomes, and childhood sexual abuse was associated with 26 of 28 specific outcomes.
Figure 1. Study selection.
CINAHL=Cumulative Index to Nursing and Allied Health Literature.
Table 1. Characteristics of meta-analyses included in this umbrella review of outcomes following childhood sexual abuse.
| Number of databases searched | Outcome | Number of primary studies | Sample size | Review (year range) | Country | |
|---|---|---|---|---|---|---|
| Amado et al (2015)5 | 4 | Anxiety disorder | 62 | 93 075 | 1995–2014 | Spain |
| Amado et al (2015)5 | 4 | Anxiety symptoms | 41 | 24 270 | 1995–2014 | Spain |
| Amado et al (2015)5 | 4 | Depressive symptoms | 59 | 33 293 | 1988–2014 | Spain |
| Arriola et al (2005)2 | 4 | Adult sexual revictimisation | 21 | 20 956 | 1975–2001 | USA |
| Arriola et al (2005)2 | 4 | Sex work | 23 | 14 996 | 1975–2001 | USA |
| Arriola et al (2005)2 | 4 | Sex with multiple partners | 23 | 16 560 | 1975–2001 | USA |
| Arriola et al (2005)2 | 4 | Unprotected sexual intercourse | 16 | 11 770 | 1991–2001 | USA |
| Chen et al (2010)6 | 9 | Post-traumatic stress disorder | 3 | 788 | 1999–2006 | USA |
| Chen et al (2010)6 | 9 | Schizophrenia | 3 | 3 131 503 | 1997–2004 | USA |
| Chen et al (2010)6 | 9 | Sleep disorders | 1 | 140 | 1988 | USA |
| Chen et al (2010)6 | 9 | Somatoform disorders | 3 | 308 | 1997–2008 | USA |
| Danese et al (2014)9 | 3 | Obesity | 26 | 161 195 | NA | UK |
| Fossati et al (1999)50 | 2 | Borderline personality disorder | 21 | 2479 | 1987–1994 | Italy |
| Halpern et al (2018)51 | 3 | Substance misuse | 7 | 22 527 | 1996–2017 | Brazil |
| Hauser et al (2011)52 | 4 | Fibromyalgia | 10 | 1487 | 1995–2010 | Germany |
| Irish et al (2010)53 | 3 | Pain (continuous) | 9 | 4934 | 1992–2007 | USA |
| Irish et al (2010)53 | 3 | Pain (categorical) | 12 | 222 893 | 1992–2007 | USA |
| Jespersen et al (2009)3 | 3 | Sexual offending against children vs adults* | 15 | 2296 | 1979–2003 | Canada |
| Jespersen et al (2009)3 | 3 | Sexual offending vs non-sexual offending | 17 | 2798 | 1987–2003 | Canada |
| Klonsky et al (2008)54 | 3 | Non-suicidal self-injury | 43 | 13 687 | 1980–2006 | USA |
| Lloyd et al (2012)8 | 6 | HIV | 5 | 7796 | 1995–2009 | USA |
| Ludwig et al (2018)43 | 2 | Conversion disorder | 15 | 2083 | 1971–2016 | Germany |
| Molendijk et al (2017)44 | 3 | Eating disorders | 49 | 15 006 | 1985–2015 | Netherlands |
| Nelson et al (2016)45 | 3 | Depression | 57 | 74 461 | NA | Germany |
| Neumann et al (1996)46 | 1 | Traumatic stress responses | 4 | NA | NA | USA |
| Ng et al (2018)47 | 5 | Suicide attempts | 47 | 151 476 | 1993–2017 | Singapore |
| Quinones-Munoz (2001)48 | 3 | Psychological symptoms | 5 | 3720 | 1992–98 | USA |
| Ulrich et al (2005)49 | 5 | Somatisation | 11 | NA | NA | USA |
| Varese et al (2012)7 | 4 | Psychosis | 20 | 53 050 | 1984–2011 | UK |
NA=not available.
Originally reported as “sexual offending against adults versus children”, so the effect size data included in the following analysis are the reciprocal of the data reported in the original meta-analysis.
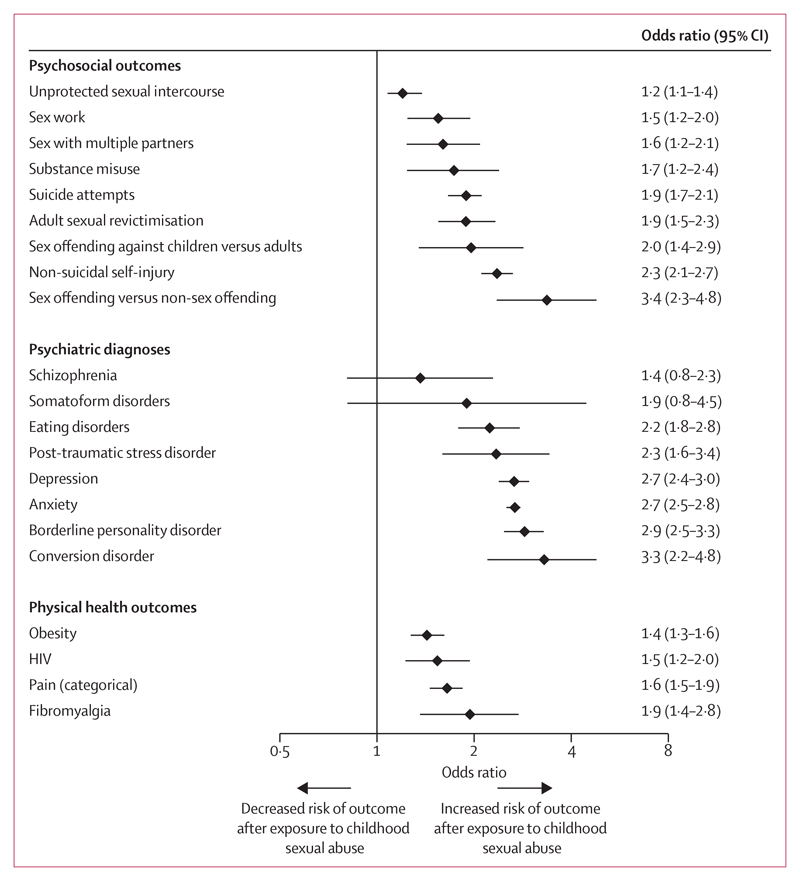
The ORs mostly ranged from 2·2 (95% CI 1·8–2·8) to 3·3 (2·2–4·8) for psychiatric outcomes, from 1·2 (1·1–1·4) to 3·4 (2·3–4·8) for psychosocial outcomes, and from 1·4 (1·3–1·6) to 1·9 (1·4–2·8) for physical health outcomes (figure 2).
Figure 2. Risk estimates of long-term outcomes following childhood sexual abuse.
On the basis of thresholds for small, medium, and large effect sizes,55 childhood sexual abuse was associated with a small increased odds ratio (ie, less than 1·7) for seven outcomes and a medium odds ratio (ie, 1·7–3·5) for 21 outcomes, and was not associated with a large odds ratio (ie, more than 3·5) for any outcome (table 2). Outcomes with the strongest associations with childhood sexual abuse were sexual versus non-sexual offending (OR 3·4 [95% CI 2·3–4·8]), conversion disorder (3·3 [2·2–4·8]), borderline personality disorder (2·9 [2·5–3·3]), anxiety (2·7 [2·5–2·8]), and depression (2·7 [2·4–3·0]).
Table 2. Effect of childhood sexual abuse on long-term outcomes, quality measurements, and population attributable fractions.
| Odds ratio | 95% CI | 95% prediction interval | I2 (%) | 95% CI for I2 | Excess statistical significance ratio | Population attributable fraction (%) | 95% CI for population attributable fraction | |
|---|---|---|---|---|---|---|---|---|
| Sexual offending vs non-sexual offending | 3·4 | 2·3–4·8 | 1·1–10·3 | 54% | 21–74 | ·· | 14·7% | 9·6–19·9 |
| Conversion disorder | 3·3 | 2·2–4·8 | ·· | 41% | 0–68 | ·· | 14·4% | 8·8–19·9 |
| Borderline personality disorder | 2·9 | 2·5–3·3 | ·· | 30% | 0–59 | ·· | 12·4% | 10·4–14·4 |
| Anxiety | 2·7 | 2·5–2·8 | ·· | ·· | ·· | 0·5 | 11·7% | 7·8–15·8 |
| Depression | 2·7 | 2·4–3·0 | ·· | 65% | 54–74 | ·· | 11·4% | 9·8–12·9 |
| Post-traumatic stress responses | 2·6 | 2·2–2·9 | ·· | ·· | ·· | ·· | 10·9% | 9·9–12·7 |
| Psychosis | 2·4 | 2·0–2·9 | ·· | 45% | 7–67 | 1·4 | 9·8% | 7·4–12·4 |
| Non-suicidal self-injury | 2·3 | 2·1–2·7 | ·· | 51% | 32–66 | 1·4 | 9·7% | 8·2–11·4 |
| Post-traumatic stress disorder | 2·3 | 1·6–3·4 | 1·0–5·4 | 0% | 0–0 | 1·0 | 9·6% | 4·8–15·0 |
| Eating disorders | 2·2 | 1·8–2·8 | ·· | 64% | 51–73 | ·· | 9·0% | 6·2–12·0 |
| Anxiety symptomatology | 2·0 | 1·9–2·0 | ·· | ·· | ·· | 1·5 | 7·3% | 6·9–7·8 |
| Depressive symptomatology | 2·0 | 1·9–2·0 | ·· | - | - | 1·5 | 7·3% | 6·9–7·8 |
| Pain (continuous) | 2·0 | 1·3–3·0 | ·· | ·· | ·· | 0·9 | 7·8% | 2·6–13·1 |
| Sexual offending against children vs adults | 2·0 | 1·4–2·9 | 0·5–7·1 | 70% | 50–83 | 1·7 | 7·3% | 3·0–12·4 |
| Fibromyalgia | 1·9 | 1·4–2·8 | 1·0–3·8 | 20% | 0–61 | 1·7 | 7·2% | 3·0–11·8 |
| Adult sexual revictimisation | 1·9 | 1·5–2·3 | ·· | 94% | 92–95 | 1·4 | 6·9% | 4·5–9·7 |
| Somatoform disorders | 1·9 | 0·8–4·5 | 0·3–14·1 | 4% | 0–26 | 1·9 | 6·9% | 1·8–18·8 |
| Suicide attempts | 1·9 | 1·7–2·1 | 1·7–2·2 | 84% | 80–88 | 0·9 | 6·9% | 5·3–8·3 |
| Psychological symptoms | 1·7 | 1·5–2·0 | 0·7–4·3 | 77% | 45–91 | 1·1 | 5·7% | 4·0–7·8 |
| Substance misuse | 1·7 | 1·2–2·4 | 1·1–2·6 | 42% | 0–75 | 0·9 | 5·8% | 2·1–10·0 |
| Pain (categorical) | 1·6 | 1·5–1·9 | ·· | ·· | ·· | 1·3 | 5·2% | 3·8–6·7 |
| Sex with multiple partners | 1·6 | 1·2–2·1 | ·· | 92% | 90–94 | 1·4 | 4·8% | 2·1–8·2 |
| Somatisation | 1·6 | 1·3–1·9 | ·· | 40% | 0–7 | ·· | 4·5% | 2·5–6·6 |
| Sex work | 1·5 | 1·2–2·0 | ·· | 76% | 65–84 | 0·9 | 4·5% | 2·1–7·3 |
| HIV | 1·5 | 1·2–2·0 | 0·9–2·8 | 50% | 0–82 | 1·1 | 4·4% | 1·9–7·2 |
| Obesity | 1·4 | 1·3–1·6 | ·· | 87% | 82–91 | 1·1 | 3·6% | 2·3–5·0 |
| Schizophrenia | 1·4 | 0·8–2·3 | 0·4–4·3 | 0% | 0–0 | 0·9 | 3·0% | 1·8–9·4 |
| Unprotected sexual intercourse | 1·2 | 1·1–1·4 | ·· | 51% | 14–73 | 1·0 | 1·7% | 0·7–3·3 |
Outcomes are ranked by descending effect size.
Population attributable fractions ranged from 1·7% (95% CI 0·7–3·3) for unprotected sexual intercourse to 14·4% (8·8–19·9) for conversion disorder. The highest population attributable fraction was 14·7% (9·6–19·9) for sexual offending versus non-sexual offending (table 2). However, these figures will likely be overestimated because the population attributable fractions were calculated using data without adjustment for confounders.
In studies with sufficient data, half of the studies had 95% prediction intervals that included the null OR of 1, more than half demonstrated evidence of excess significance, more than a fifth had small study effects, and more than a third had high heterogeneity (appendix pp 8–11).
In addition, systematic reviews of 15 of the 28 outcomes had low AMSTAR scores (appendix pp 6–9, 12). Systematic reviews of two outcomes (post-traumatic stress disorder and substance misuse) had high quality scores of 5 (out of 5), and another one (schizophrenia) received a score of 4 (appendix p 8). Quality was low for meta-analyses on both borderline personality disorder and anxiety (scoring 1 out of 5), and moderate (3 out of 5) for conversion disorder and sexual versus non-sexual offending.
For outcomes with high quality scores, we examined absolute rates reported in primary studies. Specifically, longitudinal cohort studies reported that among individuals who experienced childhood sexual abuse, 503 (28%) of 1809 developed substance misuse56 and 36 (38%) of 96 developed post-traumatic stress disorder.57
Among the included systematic reviews, a small number of studies explored sources of heterogeneity among primary studies. No differences were found on the effect of childhood sexual abuse by age on conversion disorders, fibromyalgia, and borderline personality disorders,46,48,51 by gender on depression,53 by study design on obesity and psychosis,7,9 and by adjustment for confounders such as psychiatric comorbidity on obesity and eating disorders.9,52 However, the risk of HIV was higher when individuals experienced sexual abuse in late than in early adolescence.8 In addition, the effects of childhood sexual abuse on obesity attenuated after adjustment for current depression,9 and the risk of anxiety after childhood sexual abuse was higher in females than in males.5
Discussion
In this umbrella review of 28 long-term outcomes of childhood sexual abuse, we summarised the evidence from 19 meta-analyses, including more than 4 million participants from more than 500 primary studies. Childhood sexual abuse was associated with 26 of 28 examined outcomes, including a wide range of psychosocial, psychiatric, and physical health outcomes. Among the 26 outcomes that were significantly associated with childhood sexual abuse, only two were based on systematic reviews with high quality assessment scores: substance misuse and post-traumatic stress disorder.
Our findings underscore the need to better understand the mechanisms underlying the association between childhood sexual abuse and long-term outcomes. Some existing research points to biological mechanisms through which childhood abuse increases the risk of psychopathology and physical illness, such as through the hypothalamic–pituitary–adrenal axis or inflammation.58,59 Some outcomes might also be explained by psychosocial mechanisms, such as risky sexual behaviour and distorted body image.60 For example, childhood sexual abuse is associated with risky sexual behaviours,61,62 which could lead to HIV.63 The association between childhood sexual abuse and physical health problems might also be partially explained by mediating psychiatric factors. For example, the effect of childhood sexual abuse on obesity might be due to depression or certain eating disorders. Childhood sexual abuse is an important predictor of depression over the life course and depression is prospectively linked to obesity; however, it is also possible that effects of childhood sexual abuse on depression and eating disorders are triggered by obesity.64–69
Our review has highlighted research gaps. Primary work should capitalise on prospectively collected measures of childhood sexual abuse to minimise misclassification and recall bias. Future research should also adopt more comprehensive models to account for confounds (eg, other forms of abuse), use stronger designs and analysis (eg, prospective studies) to examine causal inference, and explore source of heterogeneity to identify protective and risk factors. Meta-analyses should ensure more accurate and systematic presentation of data and follow consensus guidelines to facilitate replicability. In addition, we found no meta-analyses on bipolar disorder, which has shown worse clinical outcomes when it occurs in combination with childhood maltreatment,70 obsessive compulsive disorder, or homelessness.
Our results underscore the need for effective interventions. So far, research on the primary prevention of childhood sexual abuse has focused primarily on school-based interventions and home-based parenting interventions. There is some evidence that school-based programmes aimed at helping children to recognise and report sexual abuse improve children’s knowledge and protective behaviours,71 although they are not developed to prevent adverse outcomes after sexual abuse. A growing body of research also suggests that early childhood home visit and parent education programmes promoting recognition of childhood sexual abuse and early symptoms of adverse outcome might prevent or reduce the risk of child maltreatment overall.72–75 In addition, physicians might play a part in screening for childhood sexual abuse, determining the need to report sexual abuse to appropriate safeguarding authorities, and coordinating care with other health professionals to prevent long-term poor outcomes.76
Research has indicated the effectiveness of interventions for post-traumatic stress disorder in individuals who have experienced childhood sexual abuse77,78 as well as depression.78 More specifically, research on various treatment modalities for individuals who have experienced childhood sexual abuse provides some support for cognitive behavioural interventions, particularly the efficacy of trauma-focused cognitive behavioural therapy for young people with post-traumatic stress disorder, anxiety, or depressive symptoms who have been sexually abused.79–82 However, research on treatments for some of the other important outcomes reported, particularly substance misuse and sexual revictimisation, in individuals who have been sexually abused is required. Another area for research is to improve translation of effective interventions into policy and practice, such as establishing community programmes to respond to sexual abuse. Furthermore, to prevent psychopathologies and other outcomes after sexual abuse, more research on the developmental mechanisms is necessary.
The sexual versus non-sexual offending finding does not mean an increased risk of offending in this population—rather, that if an individual has committed a crime, then there is an increased likelihood of being a sexual offender. By contrast, indicative absolute rates on two psychiatric outcomes with high quality scores were high, 28% for substance misuse and 38% for post-traumatic stress disorder, suggesting that interventions for these outcomes should be prioritised.
Strengths of this umbrella review include testing quantitative measures of research and outcome quality, allowing for the comparison of findings across outcomes, and the discrimination between higher and lower quality research findings. Another strength is the inclusion of a wide range of psychosocial, psychiatric, and physical health outcomes, given that many previous meta-analyses and umbrella reviews have focused on either a single or narrow subset of outcomes.12–15 Moreover, temporal ordering between the predictor and outcome of interest (ie, childhood sexual abuse occurring before 18 years of age and outcome measurement occurring after 18 years of age) was part of inclusion criteria, reducing the risk of conflating short-term effects of childhood abuse with adult consequences.
Several limitations should be noted. First, only a small number of the included systematic reviews explored sources of heterogeneity among primary studies by age,46,48,51 and study design.7,9 Other factors, including familial features (protective factors such as stable family environment and supportive relationships), characteristics of abuse, or overlap with other types of child abuse, are likely to moderate or mediate the association between sexual abuse and later outcomes, so not accounting for them might lead to overestimation of effect sizes.83,84 Future studies addressing these confounding factors are necessary for a more precise estimate of the link between child sexual abuse and later outcomes, including using family-based designs. In addition, collection of more detailed information about the nature of the abuse could help to disentangle the effects of different types of abuse. Second, the primary studies included in the meta-analyses were often based on retrospective recall of childhood sexual abuse by adults, and retrospective reports are suboptimal proxies for prospectively collected measures of childhood sexual abuse.11 Thus, future research with prospective designs is necessary. Apart from repeated measures of individuals at different timepoints with questionnaires,85 one other possibility could be using linked register-based datasets in which sexual abuse victimisation and physical and mental health outcomes are longitudinally recorded.86,87 Official register data would reduce report bias of sexual abuse and allow prospective studies of its links to later outcomes. Third, there is a high co-occurrence of childhood sexual abuse with other forms of child abuse, which is associated with poorer psychosocial and health outcomes.88–90 However, as a result of insufficient data, we were not able to take into account effects of other forms of child abuse in this umbrella review. Finally, our analyses showed that current evidence of the association between sexual abuse and health outcomes is inconsistent and studies with significant results were more likely to be published than those with non-significant findings. Future research is necessary to identify contributing factors and to decrease publication bias against studies with non-significant findings.
This umbrella review found that childhood sexual abuse is associated with elevated risks of long-term psychosocial, psychiatric, and physical health outcomes. In particular, there is high-quality evidence for associations between childhood sexual abuse and two psychiatric disorders (schizophrenia and post-traumatic stress disorder) and one psychosocial outcome (substance misuse). Because both relative risks and absolute rates for certain outcomes following childhood sexual abuse have been shown to be increased, this review suggests prioritising interventions that reduce the development of those outcomes that have a high-quality evidence base. Notable gaps include the need for further meta-analyses assessing outcomes for which the current review literature is low quality, and reviews on outcomes (bipolar disorder, obsessive-compulsive disorder, and homelessness) that currently lack systematic reviews. In addition, more empirical studies are necessary to clarify developmental pathways from sexual abuse to health-related and psychosocial outcomes, as well as treatment outcome research in individuals who have experienced childhood sexual abuse.
Supplementary Material
Research in context.
Evidence before this study
We searched PsycINFO, PubMed, Cumulative Index to Nursing and Allied Health Literature, and Global Health for papers published from database inception to Dec 31, 2018, with no language restrictions. We used the search terms (“sexual abuse” OR “sexual assault” OR “sexual trauma” OR “sexual crime” OR “rape” OR “incest” OR “molestation” OR “victim*” OR “maltreatment”), AND (“child*” OR “youth” OR “adolescent” OR “young” OR “teen*”), AND (“meta-analy*” OR “meta-regression” OR “meta-synthesis”). We identified six umbrella reviews that primarily considered mental health outcomes (such as anxiety or depression) or a single outcome (such as suicide), which were published more than 5 years ago, lacked quantitative synthesis and quality assessment, and were mostly based on small sample sizes.
Added value of this study
This umbrella review synthesised meta-analytical evidence on the association between childhood sexual abuse and a wide range of different outcomes. We found that childhood sexual abuse was associated with a wide range of adulthood psychiatric diagnoses, negative psychosocial outcomes, and physical health outcomes.
Implications of all the available evidence
Although there were consistently strong links between childhood sexual abuse and many long-term health and psychosocial outcomes, the quality of the underlying research was limited by small study effects, excess significance, and high heterogeneity between studies. However, two psychiatric disorders (post-traumatic stress disorder and schizophrenia) and one psychosocial outcome (substance misuse) had a high-quality evidence base, and the available evidence suggests that interventions mitigating later substance misuse and post-traumatic stress disorder should be prioritised. Notable gaps in the review literature included links between childhood sexual abuse and bipolar disorder, obsessive-compulsive disorder, and homelessness.
Acknowledgments
RY is supported by a Rubicon Research Fellowship from the Netherlands Organisation for Scientific Research (grant number 446-15-002). AD is funded by the UK National Institute for Health Research Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London (UK), the UK Medical Research Council (grant number P005918), the UK Economic and Social Research Council, and the UK National Society for Prevention of Cruelty to Children (NSPCC). SF is funded by a Wellcome Trust Senior Research Fellowship (grant number 202836/Z/16/Z). We thank Sharon Gil for acting as the second extractor of the effect sizes data. We thank Shaoling Zhong for screening of articles resulted from our updated search for inclusion and exclusion. We thank the following authors for sharing copies of their articles or data with us: Cesare Maffei (Vita-Salute San Raffaele University, Italy), Shane Lloyd, (Brown University, USA), Carlo Faravelli (Universita di Firenze, Italy), Valdo Ricca (Universita di Firenze, Italy), Brenda Miller (Pacific Institute for Research and Evaluation, USA), Yue Wang (Liaoning Cancer Hospital and Institute, China), David Klonsky (University of British Columbia, Canada), Kimberly Arriola (Emory University, USA), and Winfried Hauser (Technical University Munich, Germany).
Footnotes
Contributors
SF and HPH conceived this study; HPH extracted the data and conducted statistical analysis; RY contributed to the data extraction and interpretation; HPH and RY drafted the manuscript; HPH, SF, RY, and AD contributed to the revision of the manuscript; and SF provided overall supervision.
Declaration of interests
We declare no competing interests.
Contributor Information
Prof Andrea Danese, Medical Research Council Social, Genetic and Developmental Psychiatry Centre and Department of Child and Adolescent Psychiatry, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, UK; National and Specialist CAMHS Trauma and Anxiety Clinic, South London and Maudsley NHS Foundation Trust, London, UK.
Prof Seena Fazel, Department of Psychiatry, University of Oxford, Oxford, UK.
References
- 1.Stoltenborgh M, van Ijzendoorn MH, Euser EM, Bakermans-Kranenburg MJ. A global perspective on child sexual abuse: meta-analysis of prevalence around the world. Child Maltreat. 2011;16:79–101. doi: 10.1177/1077559511403920. [DOI] [PubMed] [Google Scholar]
- 2.Arriola KR, Louden T, Doldren MA, Fortenberry RM. A meta-analysis of the relationship of child sexual abuse to HIV risk behavior among women. Child Abuse Negl. 2005;29:725–46. doi: 10.1016/j.chiabu.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 3.Jespersen AF, Lalumiere ML, Seto MC. Sexual abuse history among adult sex offenders and non-sex offenders: a meta-analysis. Child Abuse Negl. 2009;33:179–92. doi: 10.1016/j.chiabu.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 4.Liu RT. Childhood maltreatment and impulsivity: a meta-analysis and recommendations for future study. J Abnorm Child Psychol. 2018 doi: 10.1007/s10802-018-0445-3. published online May 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Amado BG, Arce R, Herraiz A. Psychological injury in victims of child sexual abuse: a meta-analytic review. Psychosoc Interv. 2015;24:49–62. [Google Scholar]
- 6.Chen LP, Murad MH, Paras ML, et al. Sexual abuse and lifetime diagnosis of psychiatric disorders: systematic review and meta-analysis. Mayo Clin Proc. 2010;85:618–29. doi: 10.4065/mcp.2009.0583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38:661–71. doi: 10.1093/schbul/sbs050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lloyd S, Operario D. HIV risk among men who have sex with men who have experienced childhood sexual abuse: systematic review and meta-analysis. AIDS Educ Prev. 2012;24:228–41. doi: 10.1521/aeap.2012.24.3.228. [DOI] [PubMed] [Google Scholar]
- 9.Danese A, Tan M. Childhood maltreatment and obesity: systematic review and meta-analysis. Mol Psychiatry. 2014;19:544–54. doi: 10.1038/mp.2013.54. [DOI] [PubMed] [Google Scholar]
- 10.Newbury JB, Arseneault L, Moffitt TE, et al. Measuring childhood maltreatment to predict early-adult psychopathology: comparison of prospective informant-reports and retrospective self-reports. J Psychiatr Res. 2018;96:57–64. doi: 10.1016/j.jpsychires.2017.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reuben A, Moffitt TE, Caspi A, et al. Lest we forget: comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. J Child Psychol Psychiatry. 2016;57:1103–12. doi: 10.1111/jcpp.12621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maniglio R. Child sexual abuse in the etiology of depression: a systematic review of reviews. Depress Anxiety. 2010;27:631–42. doi: 10.1002/da.20687. [DOI] [PubMed] [Google Scholar]
- 13.Maniglio R. Child sexual abuse in the etiology of anxiety disorders: a systematic review of reviews. Trauma Violence Abuse. 2013;14:96–112. doi: 10.1177/1524838012470032. [DOI] [PubMed] [Google Scholar]
- 14.Maniglio R. The role of child sexual abuse in the etiology of suicide and non-suicidal self-injury. Acta Psychiatr Scand. 2011;124:30–41. doi: 10.1111/j.1600-0447.2010.01612.x. [DOI] [PubMed] [Google Scholar]
- 15.Maniglio R. The role of child sexual abuse in the etiology of substance-related disorders. J Addict Dis. 2011;30:216–28. doi: 10.1080/10550887.2011.581987. [DOI] [PubMed] [Google Scholar]
- 16.Hillberg T, Hamilton-Giachritsis C, Dixon L. Review of meta-analyses on the association between child sexual abuse and adult mental health difficulties: a systematic approach. Trauma Violence Abuse. 2011;12:38–49. doi: 10.1177/1524838010386812. [DOI] [PubMed] [Google Scholar]
- 17.Maniglio R. The impact of child sexual abuse on health: a systematic review of reviews. Clin Psychol Rev. 2009;29:647–57. doi: 10.1016/j.cpr.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 18.WHO. Global health estimates 2014 summary tables. Geneva: World Health Organization; 2014. [Google Scholar]
- 19.US National Institute of Mental Health. Global DALYs contributed by mental and behavioral disorders. [accessed Nov 1, 2016];2010 https://www.nimh.nih.gov/health/statistics/global/global-dalys-contributed-by-mental-and-behavioral-disorders.shtml.
- 20.Hemmingsson E, Johansson K, Reynisdottir S. Effects of childhood abuse on adult obesity: a systematic review and meta-analysis. Obes Rev. 2014;15:882–93. doi: 10.1111/obr.12216. [DOI] [PubMed] [Google Scholar]
- 21.Jumper SA. A meta-analysis of the relationship of child sexual abuse to adult psychological adjustment. Child Abuse Negl. 1995;19:715–28. doi: 10.1016/0145-2134(95)00029-8. [DOI] [PubMed] [Google Scholar]
- 22.Li M, D’Arcy C, Meng X. Maltreatment in childhood substantially increases the risk of adult depression and anxiety in prospective cohort studies: systematic review, meta-analysis, and proportional attributable fractions. Psychol Med. 2016;46:717–30. doi: 10.1017/S0033291715002743. [DOI] [PubMed] [Google Scholar]
- 23.Lindert J, von Ehrenstein OS, Grashow R, Gal G, Braehler E, Weisskopf MG. Sexual and physical abuse in childhood is associated with depression and anxiety over the life course: systematic review and meta-analysis. Int J Public Health. 2014;59:359–72. doi: 10.1007/s00038-013-0519-5. [DOI] [PubMed] [Google Scholar]
- 24.Mandelli L, Petrelli C, Serretti A. The role of specific early trauma in adult depression: a meta-analysis of published literature. Childhood trauma and adult depression. Eur Psychiatry. 2015;30:665–80. doi: 10.1016/j.eurpsy.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 25.Roodman AA, Clum GA. Revictimization rates and method variance: a meta-analysis. Clin Psychol Rev. 2001;21:183–204. doi: 10.1016/s0272-7358(99)00045-8. [DOI] [PubMed] [Google Scholar]
- 26.Smolak L, Murnen SK. A meta-analytic examination of the relationship between child sexual abuse and eating disorders. Int J Eat Disord. 2002;31:136–50. doi: 10.1002/eat.10008. [DOI] [PubMed] [Google Scholar]
- 27.Wang Y, Wu B, Yang H, Song X. The effect of childhood abuse on the risk of adult obesity. Ann Clin Psychiatry. 2015;27:175–84. [PubMed] [Google Scholar]
- 28.Dagang SA. A meta-analytic review of studies examining the effects of childhood sexual abuse in women. Diss Abstr Int Sect B Sci Eng. 1997;57:4701. [Google Scholar]
- 29.Sundin EC, Baguley T. Prevalence of childhood abuse among people who are homeless in Western countries: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2015;50:183–94. doi: 10.1007/s00127-014-0937-6. [DOI] [PubMed] [Google Scholar]
- 30.Hailes HP, Fazel S, Yu R. Longterm outcomes of childhood sexual abuse: an umbrella review. PROSPERO Int Prospect Regist Syst Rev. 2016 CRD42016049701. [Google Scholar]
- 31.Borenstein M. Effect sizes for continuous data. In: Cooper H, Hedges LV, Valentine JC, editors. The handbook of research synthesis and meta-analysis. 2nd edn. New York, NY: Russell Sage Foundation; 2009. pp. 221–36. [Google Scholar]
- 32.Polanin JR, Tanner-Smith EE, Hennessy EA. Estimating the difference between published and unpublished effect sizes: a meta-review. Rev Educ Res. 2016;86:207–36. [Google Scholar]
- 33.Zhang J, Yu KF. What’s the relative risk?: A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–91. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 34.Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health. 1998;88:15–19. doi: 10.2105/ajph.88.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barth J, Bermetz L, Heim E, Trelle S, Tonia T. The current prevalence of child sexual abuse worldwide: a systematic review and meta-analysis. Int J Public Health. 2013;58:469–83. doi: 10.1007/s00038-012-0426-1. [DOI] [PubMed] [Google Scholar]
- 36.von Ins FR, Mikton C, Finkelhor D, et al. Promoting research to prevent child maltreatment; XIXth ISPCAN International Congress on Child Abuse and Neglect; Istanbul, Turkey: 2012. Sep 9–12, [Google Scholar]
- 37.Shea BJ, Grimshaw JM, Wells GA, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10. doi: 10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ioannidis JPA, Patsopoulos NA, Evangelou E. Uncertainty in heterogeneity estimates in meta-analyses. BMJ. 2007;335:914–16. doi: 10.1136/bmj.39343.408449.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions, version 5. Chichester: The Cochrane Collaboration; 2011. [Google Scholar]
- 40.Ioannidis JPA, Trikalinos TA. An exploratory test for an excess of significant findings. Clin Trials. 2007;4:245–53. doi: 10.1177/1740774507079441. [DOI] [PubMed] [Google Scholar]
- 41.Kavvoura F, McQueen M, Khoury M, Tanzi R, Bertram L, Ioannidis J. Evaluation of the potential excess of statistically significant findings in public genetic association studies: application to Alzheimer’s disease. Am J Epidemiol. 2008;168:855–65. doi: 10.1093/aje/kwn206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Inthout J, Ioannidis J, Rovers MM, Goeman J. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open. 2016;6:e010247. doi: 10.1136/bmjopen-2015-010247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ludwig L, Pasman JA, Nicholson T, et al. Stressful life events and maltreatment in conversion (functional neurological) disorder: systematic review and meta-analysis of case-control studies. Lancet Psychiatry. 2018;5:307–20. doi: 10.1016/S2215-0366(18)30051-8. [DOI] [PubMed] [Google Scholar]
- 44.Molendijk ML, Hoek HW, Brewerton TD, Elzinga BM. Childhood maltreatment and eating disorder pathology: a systematic review and dose–response meta-analysis. Psychol Med. 2017;47:1402–16. doi: 10.1017/S0033291716003561. [DOI] [PubMed] [Google Scholar]
- 45.Nelson J, Klumparendt A, Doebler P, Ehring T. Childhood maltreatment and characteristics of adult depression: meta-analysis. Br J Psychiatry. 2016;209:96–104. doi: 10.1192/bjp.bp.115.180752. [DOI] [PubMed] [Google Scholar]
- 46.Neumann DA, Houskamp BM, Pollock VE, Briere J. The long-term sequelae of childhood sexual abuse in women: a meta-analytic review. Child Maltreat. 1996;1:6–16. [Google Scholar]
- 47.Ng QX, Yong BZJ, Ho CYX, Lim DY, Yeo W-S. Early life sexual abuse is associated with increased suicide attempts: an update meta-analysis. J Psychiatr Res. 2018;99:129–41. doi: 10.1016/j.jpsychires.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 48.Quinones-Munoz SL. Psychological effects of childhood sexual abuse in adult males. Diss Abstr Int Sect B Sci Eng. 2001;62:2074. [Google Scholar]
- 49.Ulrich H, Randolph M, Acheson S. Child sexual abuse: a replication of the meta-analytic examination of child sexual abuse by Rind, Tromovitch, and Bauserman (1998) Sci Rev Ment Health Pract. 2005;4:37–51. [Google Scholar]
- 50.Fossati A, Madeddu F, Maffei C. Borderline personality disorder and childhood sexual abuse: a meta-analytic study. J Pers Disord. 1999;13:268–80. doi: 10.1521/pedi.1999.13.3.268. [DOI] [PubMed] [Google Scholar]
- 51.Halpern SC, Schuch FB, Scherer JN, et al. Child maltreatment and illicit substance abuse: a systematic review and meta-analysis of longitudinal studies. Child Abuse Rev. 2018;27:344–60. [Google Scholar]
- 52.Hauser W, Kosseva M, Uceyler N, Klose P, Sommer C. Emotional, physical, and sexual abuse in fibromyalgia syndrome: a systematic review with meta-analysis. Arthritis Care Res. 2011;63:808–20. doi: 10.1002/acr.20328. [DOI] [PubMed] [Google Scholar]
- 53.Irish L, Kobayashi I, Delahanty DL. Long-term physical health consequences of childhood sexual abuse: a meta-analytic review. J Pediatr Psychol. 2010;35:450–61. doi: 10.1093/jpepsy/jsp118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Klonsky E, Moyer A. Childhood sexual abuse and non-suicidal self-injury: meta analysis. Br J Psychiatry. 2008;192:166–70. doi: 10.1192/bjp.bp.106.030650. [DOI] [PubMed] [Google Scholar]
- 55.Chen H, Cohen P, Chen S. How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Commun Stat Simul Comput. 2010;39:860–64. [Google Scholar]
- 56.Silverman AB, Reinherz HZ, Giaconia RM. The long-term sequelae of child and adolescent abuse: a longitudinal community study. Child Abuse Negl. 1996;20:709–23. doi: 10.1016/0145-2134(96)00059-2. [DOI] [PubMed] [Google Scholar]
- 57.Dube SR, Anda RF, Felitti VJ, Chapman DP, Giles WH. Childhood abuse, neglect and household dysfunction and the risk of illicit drug use: the Adverse Childhood Experience Study. Pediatrics. 2003;111:564–72. doi: 10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- 58.Nemeroff CB, Binder E. The preeminent role of childhood abuse and neglect in vulnerability to major psychiatric disorders: toward elucidating the underlying neurobiological mechanisms. J Am Acad Child Adolesc Psychiatry. 2018;53:395–97. doi: 10.1016/j.jaac.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 59.Danese A, Baldwin JR. Hidden wounds? Inflammatory links between childhood trauma and psychopathology. Annu Rev Psychol. 2017;68:517–44. doi: 10.1146/annurev-psych-010416-044208. [DOI] [PubMed] [Google Scholar]
- 60.Kilimnik CD, Meston CM. Role of body esteem in the sexual excitation and inhibition responses of women with and without a history of childhood sexual abuse. J Sex Med. 2016;13:1718–28. doi: 10.1016/j.jsxm.2016.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373:68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- 62.Homma Y, Wang N, Saewyc E, Kishor N. The relationship between sexual abuse and risky sexual behavior among adolescent boys: a meta-analysis. J Adolesc Health. 2012;51:18–24. doi: 10.1016/j.jadohealth.2011.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tiruneh K, Wasie B, Gonzalez H. Sexual behavior and vulnerability to HIV infection among seasonal migrant laborers in Metema district, northwest Ethiopia: a cross-sectional study. BMC Public Health. 2015;15:122. doi: 10.1186/s12889-015-1468-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis. Am J Psychiatry. 2012;169:141–51. doi: 10.1176/appi.ajp.2011.11020335. [DOI] [PubMed] [Google Scholar]
- 65.Luppino F, de Wit L, Bouvy P, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67:220–29. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 66.Stunkard AJ, Faith MS, Allison KC. Depression and obesity. Biol Psychiatry. 2018;54:330–37. doi: 10.1016/s0006-3223(03)00608-5. [DOI] [PubMed] [Google Scholar]
- 67.de Zwaan M. Binge eating disorder and obesity. Int J Obes Relat Metab Disord. 2001;25(suppl 1):S51–55. doi: 10.1038/sj.ijo.0801699. [DOI] [PubMed] [Google Scholar]
- 68.Hudson J, Lalonde J, Berry J, et al. Binge-eating disorder as a distinct familial phenotype in obese individuals. Arch Gen Psychiatry. 2006;63:313–19. doi: 10.1001/archpsyc.63.3.313. [DOI] [PubMed] [Google Scholar]
- 69.Yanovski SZ. Binge eating disorder and obesity in 2003: could treating an eating disorder have a positive effect on the obesity epidemic? Int J Eat Disord. 2003;34:S117–20. doi: 10.1002/eat.10211. [DOI] [PubMed] [Google Scholar]
- 70.Agnew-Blais J, Danese A. Childhood maltreatment and unfavourable clinical outcomes in bipolar disorder: a systematic review and meta-analysis. Lancet Psychiatry. 2016;3:342–49. doi: 10.1016/S2215-0366(15)00544-1. [DOI] [PubMed] [Google Scholar]
- 71.Walsh K, Zwi K, Woolfenden S, Shlonsky A. School-based education programs for the prevention of child sexual abuse: a Cochrane systematic review and meta-analysis. Res Soc Work Pract. 2018;28:33–55. [Google Scholar]
- 72.Mikton C, Butchart A. Child maltreatment prevention: a systematic review of reviews. Bull World Health Organ. 2009;87:353–61. doi: 10.2471/BLT.08.057075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chen M, Chan KL. Effects of parenting programs on child maltreatment prevention: a meta-analysis. Trauma Violence Abuse. 2016;17:88–104. doi: 10.1177/1524838014566718. [DOI] [PubMed] [Google Scholar]
- 74.Liel C. Parenting programs for mothers who are at risk or indicated for child abuse and neglect—a systematic review of the international research literature. Psychol Erziehung und Unterr. 2013;60:11–25. [Google Scholar]
- 75.Euser S, Alink LRA, Stoltenborgh M, Bakermans-Kranenburg MJ, van Ijzendoorn MH. A gloomy picture: a meta-analysis of randomized controlled trials reveals disappointing effectiveness of programs aiming at preventing child maltreatment. BMC Public Health. 2015;15:1068. doi: 10.1186/s12889-015-2387-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kellogg N. The evaluation of sexual abuse in children. Pediatrics. 2005;116:506–12. doi: 10.1542/peds.2005-1336. [DOI] [PubMed] [Google Scholar]
- 77.Ehring T, Welboren R, Morina N, Wicherts JM, Freitag J, Emmelkamp PMG. Meta-analysis of psychological treatments for posttraumatic stress disorder in adult survivors of childhood abuse. Clin Psychol Rev. 2014;34:645–57. doi: 10.1016/j.cpr.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 78.Trask EV, Walsh K, DiLillo D. Treatment effects for common outcomes of child sexual abuse: a current meta-analysis. Aggress Violent Behav. 2011;16:6–19. doi: 10.1016/j.avb.2010.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ramchandani P, Jones DPH. Treating psychological symptoms in sexually abused children: from research findings to service provision. Br J Psychiatry. 2003;183:484–90. doi: 10.1192/bjp.183.6.484. [DOI] [PubMed] [Google Scholar]
- 80.Benuto LT. Trauma-focused cognitive behavioral therapy for juvenile victims of sexual abuse. In: Daniel S, Bromberg DS, O’Donohue WT, editors. Toolkit for working with juvenile sex offenders. San Diego, CA: Academic Press; 2014. pp. 291–312. [Google Scholar]
- 81.Rull J, Pereda N. Psychological intervention with adults sexually abused as children: a systematic review. Anu Psicol. 2011;41:81–105. [Google Scholar]
- 82.Macdonald G, Higgins JP, Ramchandani P, et al. Cognitive-behavioural interventions for children who have been sexually abused. Cochrane Database Syst Rev. 2012;16 doi: 10.1002/14651858.CD001930.pub3. CD001930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Afifi TO, MacMillan HL. Resilience following child maltreatment: a review of protective factors. Can J Psychiatry. 2011;56:266–72. doi: 10.1177/070674371105600505. [DOI] [PubMed] [Google Scholar]
- 84.Domhardt M, Munzer A, Fegert JM, Goldbeck L. Resilience in survivors of child sexual abuse: a systematic review of the literature. Trauma Violence Abuse. 2015;16:476–93. doi: 10.1177/1524838014557288. [DOI] [PubMed] [Google Scholar]
- 85.Noll JG, Zeller MH, Trickett PK, Putnam FW. Obesity risk for female victims of childhood sexual abuse: a prospective study. Pediatrics. 2007;120:e61–67. doi: 10.1542/peds.2006-3058. [DOI] [PubMed] [Google Scholar]
- 86.Elklit A, Shevlin M. Female sexual victimization predicts psychosis: a case-control study based on the Danish registry system. Schizophr Bull. 2010;37:1305–10. doi: 10.1093/schbul/sbq048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Spataro J, Mullen PE, Burgess PM, Wells DL, Moss SA. Impact of child sexual abuse on mental health: prospective study in males and females. Br J Psychiatry. 2004;184:416–21. doi: 10.1192/bjp.184.5.416. [DOI] [PubMed] [Google Scholar]
- 88.Fazel S, Smith EN, Chang Z, Geddes JR. Risk factors for interpersonal violence: an umbrella review of meta-analyses. Br J Psychiatry. 2018;213:609–14. doi: 10.1192/bjp.2018.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Fitton L, Yu R, Fazel S. Childhood maltreatment and violent outcomes: a systematic review and meta-analysis of prospective studies. Trauma Violence Abuse. 2018 doi: 10.1177/1524838018795269. published online Aug 20. [DOI] [PubMed] [Google Scholar]
- 90.Lereya ST, Copeland WE, Costello EJ, Wolke D. Adult mental health consequences of peer bullying and maltreatment in childhood: two cohorts in two countries. Lancet Psychiatry. 2015;2:524–31. doi: 10.1016/S2215-0366(15)00165-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.