Abstract
Recent advances in endoscopic technology allow detailed observation of the gastric mucosa. Today, endoscopy is used in the diagnosis of gastritis to determine the presence/absence of Helicobacter pylori (H. pylori) infection and evaluate gastric cancer risk. In 2013, the Japan Gastroenterological Endoscopy Society advocated the Kyoto classification, a new grading system for endoscopic gastritis. The Kyoto classification organized endoscopic findings related to H. pylori infection. The Kyoto classification score is the sum of scores for five endoscopic findings (atrophy, intestinal metaplasia, enlarged folds, nodularity, and diffuse redness with or without regular arrangement of collecting venules) and ranges from 0 to 8. Atrophy, intestinal metaplasia, enlarged folds, and nodularity contribute to gastric cancer risk. Diffuse redness and regular arrangement of collecting venules are related to H. pylori infection status. In subjects without a history of H. pylori eradication, the infection rates in those with Kyoto scores of 0, 1, and ≥ 2 were 1.5%, 45%, and 82%, respectively. A Kyoto classification score of 0 indicates no H. pylori infection. A Kyoto classification score of 2 or more indicates H. pylori infection. Kyoto classification scores of patients with and without gastric cancer were 4.8 and 3.8, respectively. A Kyoto classification score of 4 or more might indicate gastric cancer risk.
Keywords: Gastric cancer, Helicobacter pylori, Endoscopy, Kyoto classification, Atrophy, Intestinal metaplasia, Enlarged fold, Nodularity, Diffuse redness, Regular arrangement of collecting venules
Core tip: The Kyoto classification organizes endoscopic findings based on Helicobacter pylori (H. pylori) infection. The score of the Kyoto classification is the sum of scores of five endoscopic findings (atrophy, intestinal metaplasia, enlarged folds, nodularity, and diffuse redness with or without regular arrangement of collecting venules) and ranges from 0 to 8. A high score is believed to reflect a higher risk of current H. pylori infection and gastric cancer. A Kyoto classification score of 0 indicates no H. pylori infection. A Kyoto classification score of ≥ 2 indicates current H. pylori infection. A Kyoto classification score of ≥ 4 might indicate gastric cancer risk.
INTRODUCTION
Gastric cancer is the third most common cancer in the world and is the cancer with the third greatest number of mortalities. If gastric cancer is detected at an early stage, it can be cured via endoscopic submucosal dissection[1,2]. Although periodic endoscopic examination is important for detecting early gastric cancer, efficient surveillance requires identification of high-risk populations[3-7]. The genetic risks of gastric cancer have been reported to include hereditary cancer syndrome, single nucleotide polymorphisms, and family history[8-12]. Environmental risks include Helicobacter pylori infection, smoking, excessive salt consumption, and lack of vegetable. Among them, the association between H. pylori infection and the development of gastric cancer is well established, and H. pylori virulence factors (cagA, vacA, iceA, and dupA) are known[13-16]. The International Agency for Research on Cancer categorized H. pylori infection as a type I carcinogen and it is considered the primary cause of gastric cancer. On the other hand, H. pylori eradication reduces gastric cancer risk[17-20]. Therefore, the accurate assessment of H. pylori infection status is important. Nowadays, endoscopic examination is required to diagnose H. pylori infection status. In 2013, the Japan Gastroenterological Endoscopy Society advocated the Kyoto classification, a new grading system for endoscopic gastritis. In this review, we focus on up-to-date reports regarding the Kyoto classification to help improve endoscopic practice.
DEFINITION OF KYOTO CLASSIFICATION OF GASTRITIS
Thanks to advances in endoscopic technology, it is now possible to observe the gastric mucosa in minute detail. Today, endoscopy is used in the diagnosis of gastritis to determine the presence/absence of H. pylori infection and evaluate the risks of gastric cancer. The Kyoto classification of endoscopic findings was advocated when the 85th Congress of the Japan Gastroenterological Endoscopy Society was held in Kyoto in 2013. The purpose of the Kyoto classification was to evaluate the gastric mucosa, as this presents a potential risk of developing gastric cancer[21,22]. In this classification, 19 endoscopic findings related to gastritis, including atrophy, intestinal metaplasia, enlarged folds (tortuous folds), nodularity, diffuse redness, regular arrangement of collecting venules (RAC), map-like redness, foveolar-hyperplastic polyp, xanthoma, mucosal swelling, patchy redness, depressed erosion, sticky mucus, hematin, red streak, spotty redness, multiple white and flat elevated lesions, fundic gland polyp, and raised erosion, are characterized. Among them, atrophy, intestinal metaplasia, enlarged folds, and nodularity, which may be related to gastric cancer risk, and diffuse redness with or without RAC, which is related to H. pylori infection status, are accounted for in the Kyoto classification score (Table 1)[22].
Table 1.
Kyoto classification score
| Kyoto classification | Score |
| Atrophy | |
| None, C1 | 0 |
| C2 and C3 | 1 |
| O1-O3 | 2 |
| Intestinal metaplasia | |
| None | 0 |
| Antrum | 1 |
| Corpus and antrum | 2 |
| Enlarged folds | |
| Absence | 0 |
| Presence | 1 |
| Nodularity | |
| Absence | 0 |
| Presence | 1 |
| Diffuse redness | |
| None | 0 |
| Mild (with RAC) | 1 |
| Severe | 2 |
| Kyoto score | 0-8 |
RAC: Regular arrangement of collecting venules.
Endoscopic atrophy (Kimura-Takemoto classification)
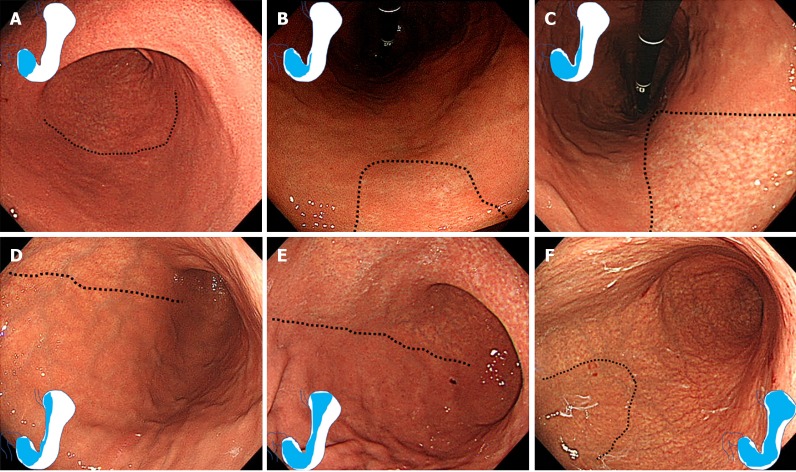
Atrophy includes “pathological” atrophy and “endoscopic” atrophy. Atrophy is pathologically defined as a loss of glandular tissue[23]. The Kyoto classification adopted Kimura-Takemoto classification of endoscopic atrophy[24]. Kimura et al[24] defined a visible capillary network, low niveau, and yellowish pale in color as atrophic features, while diffuse redness with high mucosal height as characteristics of non-atrophy. We show endoscopic images and a schematic diagram in Figure 1. “Endoscopic” atrophy has been reported to correlate well with “pathological” atrophy[25-29]. In the Kyoto classification score, non-atrophy (C0) and C1 were scored as Atrophy score 0, C2 and C3 as Atrophy score 1, and O1 to O3 as Atrophy score 2.
Figure 1.
Kimura-Takemoto classification of endoscopic atrophy. Atrophic borders are indicated by a dotted line. A: C1 (Atrophy is limited to the antrum); B: C2 (Atrophy is limited to the minor area of the lesser curvature of the body); C: C3 (Atrophy exists in the major area of the lesser curvature of the body but does not extend beyond the cardia); D: O1 (Atrophy extends to the fundus over the cardia. Atrophic border of the body lies between the lesser curvature and anterior wall); E: O2 (Atrophic border of the body lies on the anterior wall); F: O3 (Atrophy is widespread with the border between the anterior wall and greater curvature).
Endoscopic intestinal metaplasia
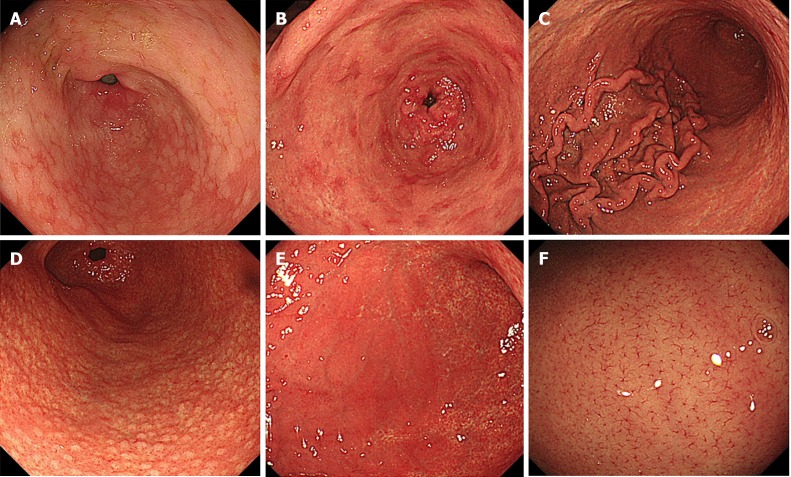
Intestinal metaplasia typically appears grayish-white and slightly elevated plaques surrounded by mixed patchy pink and pale areas of mucosa, forming an irregular uneven surface (Figure 2A). A villous appearance, whitish mucosa, and rough mucosal surface are useful indicators for endoscopic diagnosis of intestinal metaplasia[30]. Image-enhanced endoscopy, including narrow-band imaging (NBI), blue laser imaging, and linked color imaging, has improved the visibility of endoscopic findings and accuracy of endoscopic diagnosis of intestinal metaplasia[31-39]. A white opaque substance on the surface epithelium and light blue crest on the mucosal epithelial rim visualized using magnified NBI are associated with intestinal metaplasia[40-42].
Figure 2.
Endoscopic findings of Kyoto classification. A: Intestinal metaplasia; B: Map-like redness; C: Enlarged folds; D: Nodularity; E: Diffuse redness; F: Regular arrangement of collecting venules in weakly magnified image.
In the Kyoto classification score, the absence of intestinal metaplasia was scored as Intestinal metaplasia score 0, the presence of intestinal metaplasia within the antrum as Intestinal metaplasia score 1, and intestinal metaplasia extending into the corpus as Intestinal metaplasia score 2. The Intestinal metaplasia score is diagnosed by using white light imaging. Intestinal metaplasia diagnosis based on image-enhanced endoscopy using NBI, blue laser imaging, linked color imaging, and chromo-endoscopy is not included in the Kyoto score.
Map-like redness (synonymous with mottled patchy erythema) is defined as multiple flat or slightly depressed erythematous lesions that have various shapes, sizes, and red densities (Figure 2B)[6,43]. When using biopsy specimens of map-like redness, intestinal metaplasia is frequently observed (87.3%)[43]. The mechanism of the appearance of map-like redness is thought to be strengthening of the contrast between non-atrophic mucosa and atrophic mucosa after diffuse redness has disappeared following successful eradication[21]. Map-like redness is not always found following eradication. However, when it is observed, there is virtually no doubt that it is indicative of post-eradication gastric mucosa[22].
Enlarged folds
An enlarged fold is defined as a fold with a width of 5 mm or more that is not flattened or is only partially flattened by insufflation of the stomach (Figure 2C). Rugal hyperplasia is a synonym for enlarged folds.
In the Kyoto classification score, the absence and presence of enlarged folds was scored as Enlarged folds score 0 and 1, respectively.
Nodularity
Nodular gastritis is characterized by a miliary pattern resembling “goose flesh” mainly located in the antrum (Figure 2D). Nodularity can be more clearly seen following the use of indigo carmine spray. Lymphoid follicles and/or intense inflammatory cell infiltration are observed in biopsy specimens of nodularity[44]. Nodular gastritis displays a female predominance and improves gradually with age. A high serum H. pylori antibody titer is correlated to nodularity[45-49].
In the Kyoto classification score, the absence and presence of nodularity was scored as Nodularity score 0 and 1, respectively.
Diffuse redness
Diffuse redness refers to uniform redness with continuous expansion observed in non-atrophic mucosa mainly in the corpus (Figure 2E) and is typical of endoscopic superficial gastritis[22,24]. Congestion and dilation of the subepithelial capillary network in the gastric mucosa with inflammatory change of the mucosal surface color to red[50]. Since the assessment of the severity of diffuse redness is affected by the setting of the endoscope and monitor, objective assessment may be difficult.
On the other hand, RAC is a condition in which the collecting venules are arranged in the corpus. From a distance, it appears like numerous dots. From up close, it has the appearance of a regular pattern of starfish-like shapes (Figure 2F).
In the Kyoto classification score, the absence of diffuse redness was scored as Diffuse redness score 0, mild diffuse redness or diffuse redness with RAC as Diffuse redness score 1, and severe diffuse redness or diffuse redness without RAC as Diffuse redness score 2.
Kyoto classification score
The Kyoto classification score for gastritis is based on the sum of scores of the five endoscopic findings and ranges from 0 to 8 (Table 1). A high score is believed to reflect increased risk of H. pylori infection and gastric cancer. In a study that evaluated the usefulness and convenience of the Kyoto classification, a mini-lecture improved the accuracy of endoscopic diagnosis[51].
DIAGNOSIS OF HELICOBACTER PYLORI INFECTION BY ENDOSCOPIC FINDINGS
There are several reports to investigate the relationship between endoscopic findings and H. pylori infection[52-56]. Table 2 shows the diagnostic values of the Kyoto classification for H. pylori infection[57-62]. Enlarged folds had a relatively good positive predictive value (56.2–86.0%). Although nodularity had a low sensitivity (6.4%–32.1%) for H. pylori infection, it had excellent specificity for a current infection (95.8%–98.8%). Diffuse redness had a good positive predictive value (65.6%–91.5%). RAC had a high sensitivity for non-infection (86.7%–100%).
Table 2.
Diagnostic value of Kyoto classification for Helicobacter pylori infection
| Endoscopic findings | Ref. | Year | No. of subjects | Sensitivity | Specificity | PPV | NPV |
| Diagnosis for current H. pylori infection | |||||||
| Enlarged folds | Kato et al[59] | 2013 | 275 | 58.5 | 79.5 | 76.9 | 62.2 |
| Enlarged folds | Mao et al[60] | 2016 | 256 | 60.2 | 92.3 | 86.0 | 74.6 |
| Enlarged folds | Yoshii et al[61] | 2019 | 498 | 23.1 | 96.6 | 56.2 | 87.0 |
| Nodularity | Laine et al[57] | 1995 | 52 | 32.1 | 95.8 | 90.0 | 54.8 |
| Nodularity | Kato et al[59] | 2013 | 275 | 5.3 | 98.8 | 75.0 | 59.4 |
| Nodularity | Yoshii et al[61] | 2019 | 498 | 6.4 | 98.3 | 41.7 | 84.9 |
| Diffuse redness | Kato et al[59] | 2013 | 275 | 83.4 | 66.9 | 73.8 | 78.4 |
| Diffuse redness | Mao et al[60] | 2016 | 256 | 57.5 | 95.8 | 91.5 | 74.7 |
| Diffuse redness | Yoshii et al[61] | 2019 | 498 | 60.0 | 94.7 | 65.6 | 93.3 |
| Diagnosis for negative H. pylori infection | |||||||
| RAC | Yagi et al[58] | 2002 | 557 | 91.1 | 97.9 | 95.0 | 96.2 |
| RAC | Kato et al[59] | 2013 | 275 | 93.6 | 48.0 | 87.0 | 66.8 |
| RAC | Mao et al[60] | 2016 | 256 | 86.7 | 90.2 | 87.5 | 89.6 |
| RAC | Garcés-Durán et al[62] | 2019 | 140 | 100.0 | 49.0 | 47.3 | 100.0 |
PPV: Positive predictive value; NPV: Negative predictive value; RAC: Regular arrangement of collecting venules; H. pylori: Helicobacter pylori.
Yoshii et al[61] reported that endoscopic atrophy has a specificity of 75.5% for the diagnosis of past H. pylori infection. Furthermore, intestinal metaplasia and map-like redness also have a higher specificity (92.6% and 98.0%, respectively) for the diagnosis of past H. pylori infection.
Diagnosis of H. pylori infection based on Kyoto classification score
Several studies investigated the relationship between the total Kyoto classification score and H. pylori infection. We reported an association between total Kyoto classification score and serum H. pylori antibody titer[48]. Kyoto scores were 0.1, 0.4, 1.9, and 2.3 for negative-low, negative-high, positive-low, and positive-high titers of H. pylori antibody, respectively. Kyoto scores increased in line with the H. pylori antibody titer. In subjects with a negative-high H. pylori antibody titer, the Kyoto classification had an excellent area under the receiver operating characteristics curve (0.886) for predicting H. pylori infection with a cutoff value of 2. A Kyoto score of ≥ 2 could predict H. pylori infection with an accuracy of 90%[63]. In 870 subjects with no history of H. pylori eradication therapy, H. pylori infection rates in those with Kyoto classification scores of 0, 1, and ≥ 2 were 1.5%, 45%, and 82%, respectively[64].
High Kyoto scores do not always correspond to an active H. pylori infection. False diagnosis can occur due to either a spontaneous negative conversion or an unintentional eradication. In cases of spontaneous negative conversion, the harsh environment of the intestinal metaplasia removes the H. pylori infection spontaneously. In cases of unintentional eradication, the H. pylori infection is eradicated after the treatment of other infectious diseases with antibiotics.
Essentially, a Kyoto classification score of ≥ 2 indicates H. pylori infection. On the other hand, a Kyoto classification score of 0 indicates no H. pylori infection.
GASTRIC CANCER RISK ASSESSED BASED ON ENDOSCOPIC FINDINGS OF KYOTO CLASSIFICATION
There are several reports of gastric cancer risk assessed based on endoscopic findings[65-69]. Three Japanese cohort studies revealed the association of endoscopic atrophy with gastric cancer incidence (Table 3). They showed that the gastric cancer incidence of mild, moderate, and severe atrophy is 0.04%–0.10%/year, 0.12%–0.34%/year, and 0.31%–1.60%/year, respectively[70-72]. Shichijo et al[71] reported that cancer incidence was extremely high, affecting 16.0% of patients with severe atrophy over 10-year periods. Gastric cancer risk increases according to the extent of the gastric atrophy.
Table 3.
Gastric cancer incidence according to endoscopic atrophy
| Ref. | Population | No. of subjects | No. of cancers | Duration, yr |
Gastric cancer incidence, %/yr |
||
| Mild | Moderate | Severe | |||||
| Take et al[70], 2011 | Post eradication with peptic ulcer | 1674 | 28 | 5.6 | 0.04 | 0.28 | 0.62 |
| Shichijo et al[71], 2016 | Post eradication | 573 | 21 | 6.2 | 0.071 | 0.341 | 1.601 |
| Kaji et al[72], 2019 | Medical examination | 12941 | 63 | 3.7 | 0.10 | 0.16 | 0.31 |
| Post eradication | 2571 | 20 | 3.7 | 0.06 | 0.12 | 0.42 | |
Incidence was calculated by dividing the incidence per 10 years by 10.
Table 4 shows the odds ratio of gastric cancer depending on the presence or absence of the endoscopic findings of the Kyoto classification[49,73-75]. Gastric atrophy (open-type) was associated with gastric cancer with an odds ratio of 7.2–14.2[76,77].
Table 4.
Odds ratios of endoscopic findings for gastric cancer
| Endoscopic findings | Ref. | Population | No. of subjects | Odds ratio |
| Atrophy | Masuyama et al[76], 2015 | Without eradication | 27777 | 14.21 |
| Atrophy | Sekikawa et al[77], 2016 | Screening | 1823 | 7.21 |
| Intestinal metaplasia | Sugimoto et al[74], 2017 | Endoscopic gastritis | 1200 | 5.0 |
| Enlarged folds | Nishibayashi et al[73], 2003 | H. pylori positive | 276 | 5.0 |
| Nodularity | Nishikawa et al[49], 2018 | H. pylori positive | 674 | 13.9 |
| RAC | Majima et al[75], 2019 | Post eradication | 194 | 0.4 |
Odds ratio for open-type atrophy calculated with closed-type atrophy as a reference. RAC: Regular arrangement of collecting venules; H. pylori: Helicobacter pylori.
Sugimoto et al[74] have reported that endoscopic intestinal metaplasia was associated with early gastric cancer with an odds ratio of 5.0. Intestinal metaplasia is reported to be associated with intestinal-type cancer[78].
A cross-sectional study reported an odds ratio of 5.0 for enlarged folds of 5 mm or more for gastric cancer patient with H. pylori-infected controls as a reference[73]. It also indicated an upward shift in the distribution of gastric fold widths in H. pylori-positive patients with gastric cancer to an odds ratio of 35.5 in those with a fold width of 7 mm. Inflammation-induced DNA methylation of various genes is involved in the development of gastric cancer in gastritis with enlarged folds[50,73,79-85]. Enlarged folds are reported to be associated with diffuse-type gastric cancer[73,86].
Nishikawa et al[49] reported an odds ratio of 13.9 for gastric cancer in H. pylori-positive patients with nodularity. In a study involving H. pylori-positive patients under the age of 29, nodularity provided an odds ratio of 64.2 for gastric cancer. Nodularity is reported to be associated with diffuse-type cancer[49,87].
RAC was reported to be negatively associated with gastric cancer (odds ratio: 0.4)[75].
Gastric cancer risk assessed using the Kyoto classification score
Sugimoto et al[74] presented the relationship between total Kyoto classification score and gastric cancer risk. In their cross-sectional study, the total Kyoto classifications scores of patients with and without gastric cancer were 4.8 and 3.8, respectively. This study suggests that a Kyoto classification score of ≥ 4 might indicate gastric cancer risk.
CONCLUSION
The Kyoto classification organized endoscopic findings related to H. pylori infection. A Kyoto classification score ≥ 2 indicates H. pylori infection. An H. pylori test is essential for such cases with no history of H. pylori eradication.
A Kyoto classification score ≥ 4 might indicate gastric cancer risk. Such cases need careful follow-up. However, research related to the Kyoto score is still scarce and further study is needed.
Footnotes
Conflict-of-interest statement: Authors declare no conflict of interests for this article.
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: Japan Gastroenterological Endoscopy Society, No. 36450775; The Japanese Society of Gastroenterology, No. 037068; The Japanese Society of Internal Medicine, No. 24993; European Society of Gastrointestinal Endoscopy, No. 11413; American Society for Gastrointestinal Endoscopy, No. 154418; Japan Surgical Society, No. 0416990; The Japanese Society for Helicobacter Research, No. 773815.
Peer-review started: December 30, 2019
First decision: January 11, 2020
Article in press: January 19, 2020
Specialty type: Gastroenterology and Hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ahmed M, Durazzo M, Lieto E S-Editor: Zhang L L-Editor: A E-Editor: Ma YJ
Contributor Information
Osamu Toyoshima, Department of Gastroenterology, Toyoshima Endoscopy Clinic, Tokyo 157-0066, Japan; Department of Gastroenterology, Graduate School of Medicine, The University of Tokyo, Tokyo 113-8655, Japan.
Toshihiro Nishizawa, Department of Gastroenterology, Toyoshima Endoscopy Clinic, Tokyo 157-0066, Japan; Department of Gastroenterology and Hepatology, International University of Health and Welfare, Mita Hospital, Tokyo 108-8329, Japan.
Kazuhiko Koike, Department of Gastroenterology, Graduate School of Medicine, The University of Tokyo, Tokyo 113-8655, Japan.
References
- 1.Nishizawa T, Yahagi N. Long-Term Outcomes of Using Endoscopic Submucosal Dissection to Treat Early Gastric Cancer. Gut Liver. 2018;12:119–124. doi: 10.5009/gnl17095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Draganov PV, Wang AY, Othman MO, Fukami N. AGA Institute Clinical Practice Update: Endoscopic Submucosal Dissection in the United States. Clin Gastroenterol Hepatol. 2019;17:16–25.e1. doi: 10.1016/j.cgh.2018.07.041. [DOI] [PubMed] [Google Scholar]
- 3.Nishizawa T, Suzuki H, Arano T, Yoshida S, Yamashita H, Hata K, Kanai T, Yahagi N, Toyoshima O. Characteristics of gastric cancer detected within 1 year after successful eradication of Helicobacter pylori. J Clin Biochem Nutr. 2016;59:226–230. doi: 10.3164/jcbn.16-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malfertheiner P, Megraud F, O'Morain CA, Gisbert JP, Kuipers EJ, Axon AT, Bazzoli F, Gasbarrini A, Atherton J, Graham DY, Hunt R, Moayyedi P, Rokkas T, Rugge M, Selgrad M, Suerbaum S, Sugano K, El-Omar EM European Helicobacter and Microbiota Study Group and Consensus panel. Management of Helicobacter pylori infection-the Maastricht V/Florence Consensus Report. Gut. 2017;66:6–30. doi: 10.1136/gutjnl-2016-312288. [DOI] [PubMed] [Google Scholar]
- 5.Sakitani K, Nishizawa T, Arita M, Yoshida S, Kataoka Y, Ohki D, Yamashita H, Isomura Y, Toyoshima A, Watanabe H, Iizuka T, Saito Y, Fujisaki J, Yahagi N, Koike K, Toyoshima O. Early detection of gastric cancer after Helicobacter pylori eradication due to endoscopic surveillance. Helicobacter. 2018;23:e12503. doi: 10.1111/hel.12503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Banks M, Graham D, Jansen M, Gotoda T, Coda S, di Pietro M, Uedo N, Bhandari P, Pritchard DM, Kuipers EJ, Rodriguez-Justo M, Novelli MR, Ragunath K, Shepherd N, Dinis-Ribeiro M. British Society of Gastroenterology guidelines on the diagnosis and management of patients at risk of gastric adenocarcinoma. Gut. 2019;68:1545–1575. doi: 10.1136/gutjnl-2018-318126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pimentel-Nunes P, Libânio D, Marcos-Pinto R, Areia M, Leja M, Esposito G, Garrido M, Kikuste I, Megraud F, Matysiak-Budnik T, Annibale B, Dumonceau JM, Barros R, Fléjou JF, Carneiro F, van Hooft JE, Kuipers EJ, Dinis-Ribeiro M. Management of epithelial precancerous conditions and lesions in the stomach (MAPS II): European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter and Microbiota Study Group (EHMSG), European Society of Pathology (ESP), and Sociedade Portuguesa de Endoscopia Digestiva (SPED) guideline update 2019. Endoscopy. 2019;51:365–388. doi: 10.1055/a-0859-1883. [DOI] [PubMed] [Google Scholar]
- 8.Study Group of Millennium Genome Project for Cancer. Sakamoto H, Yoshimura K, Saeki N, Katai H, Shimoda T, Matsuno Y, Saito D, Sugimura H, Tanioka F, Kato S, Matsukura N, Matsuda N, Nakamura T, Hyodo I, Nishina T, Yasui W, Hirose H, Hayashi M, Toshiro E, Ohnami S, Sekine A, Sato Y, Totsuka H, Ando M, Takemura R, Takahashi Y, Ohdaira M, Aoki K, Honmyo I, Chiku S, Aoyagi K, Sasaki H, Ohnami S, Yanagihara K, Yoon KA, Kook MC, Lee YS, Park SR, Kim CG, Choi IJ, Yoshida T, Nakamura Y, Hirohashi S. Genetic variation in PSCA is associated with susceptibility to diffuse-type gastric cancer. Nat Genet. 2008;40:730–740. doi: 10.1038/ng.152. [DOI] [PubMed] [Google Scholar]
- 9.Tanikawa C, Urabe Y, Matsuo K, Kubo M, Takahashi A, Ito H, Tajima K, Kamatani N, Nakamura Y, Matsuda K. A genome-wide association study identifies two susceptibility loci for duodenal ulcer in the Japanese population. Nat Genet. 2012;44:430–434, S1-S2. doi: 10.1038/ng.1109. [DOI] [PubMed] [Google Scholar]
- 10.Han MA, Oh MG, Choi IJ, Park SR, Ryu KW, Nam BH, Cho SJ, Kim CG, Lee JH, Kim YW. Association of family history with cancer recurrence and survival in patients with gastric cancer. J Clin Oncol. 2012;30:701–708. doi: 10.1200/JCO.2011.35.3078. [DOI] [PubMed] [Google Scholar]
- 11.Nishizawa T, Suzuki H, Sakitani K, Yamashita H, Yoshida S, Hata K, Kanazawa T, Fujiwara N, Kanai T, Yahagi N, Toyoshima O. Family history is an independent risk factor for the progression of gastric atrophy among patients with Helicobacter pylori infection. United European Gastroenterol J. 2017;5:32–36. doi: 10.1177/2050640616642341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Toyoshima O, Tanikawa C, Yamamoto R, Watanabe H, Yamashita H, Sakitani K, Yoshida S, Kubo M, Matsuo K, Ito H, Koike K, Seto Y, Matsuda K. Decrease in PSCA expression caused by Helicobacter pylori infection may promote progression to severe gastritis. Oncotarget. 2018;9:3936–3945. doi: 10.18632/oncotarget.23278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yamaoka Y. Mechanisms of disease: Helicobacter pylori virulence factors. Nat Rev Gastroenterol Hepatol. 2010;7:629–641. doi: 10.1038/nrgastro.2010.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hatakeyama M. Helicobacter pylori CagA and gastric cancer: a paradigm for hit-and-run carcinogenesis. Cell Host Microbe. 2014;15:306–316. doi: 10.1016/j.chom.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 15.Talebi Bezmin Abadi A, Perez-Perez G. Role of dupA in virulence of Helicobacter pylori. World J Gastroenterol. 2016;22:10118–10123. doi: 10.3748/wjg.v22.i46.10118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Imkamp F, Lauener FN, Pohl D, Lehours P, Vale FF, Jehanne Q, Zbinden R, Keller PM, Wagner K. Rapid Characterization of Virulence Determinants in Helicobacter pylori Isolated from Non-Atrophic Gastritis Patients by Next-Generation Sequencing. J Clin Med. 2019:8. doi: 10.3390/jcm8071030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nishizawa T, Suzuki H, Maekawa T, Harada N, Toyokawa T, Kuwai T, Ohara M, Suzuki T, Kawanishi M, Noguchi K, Yoshio T, Katsushima S, Tsuruta H, Masuda E, Tanaka M, Katayama S, Kawamura N, Nishizawa Y, Hibi T, Takahashi M. Dual therapy for third-line Helicobacter pylori eradication and urea breath test prediction. World J Gastroenterol. 2012;18:2735–2738. doi: 10.3748/wjg.v18.i21.2735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nishizawa T, Suzuki H. Gastric Carcinogenesis and Underlying Molecular Mechanisms: Helicobacter pylori and Novel Targeted Therapy. Biomed Res Int. 2015;2015:794378. doi: 10.1155/2015/794378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee YC, Chiang TH, Chou CK, Tu YK, Liao WC, Wu MS, Graham DY. Association Between Helicobacter pylori Eradication and Gastric Cancer Incidence: A Systematic Review and Meta-analysis. Gastroenterology. 2016;150:1113–1124.e5. doi: 10.1053/j.gastro.2016.01.028. [DOI] [PubMed] [Google Scholar]
- 20.Kishikawa H, Ojiro K, Nakamura K, Katayama T, Arahata K, Takarabe S, Miura S, Kanai T, Nishida J. Previous Helicobacter pylori infection-induced atrophic gastritis: A distinct disease entity in an understudied population without a history of eradication. Helicobacter. 2020;25:e12669. doi: 10.1111/hel.12669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kato M. Endoscopic Findings of H. pylori Infection. In: Suzuki H, Warren R, Marshall B, editors. Helicobacter pylori. Tokyo: Springer Japan; 2016. pp. 157–167. Available from: https://link.springer.com/chapter/10.1007/978-4-431-55705-0_10. [Google Scholar]
- 22.Haruma K, Kato M, Inoue K, Murakami K, Kamada T. Kyoto Classification of Gastritis. 1st ed. Tokyo Japan: Nihon Medical Center, 2017. [Google Scholar]
- 23.Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol. 1996;20:1161–1181. doi: 10.1097/00000478-199610000-00001. [DOI] [PubMed] [Google Scholar]
- 24.Kimura K, Takemoto T. An endoscopic recognition of the atrophic border and its significance in chronic gastritis. Endoscopy. 1969;3:87–97. [Google Scholar]
- 25.Mihara M, Haruma K, Kamada T, Komoto K, Yoshihara M, Sumii K, Kajiyama G. The role of endoscopic findings for the diagnosis of Helicobacter pylori infection: evaluation in a country with high prevalence of atrophic gastritis. Helicobacter. 1999;4:40–48. doi: 10.1046/j.1523-5378.1999.09016.x. [DOI] [PubMed] [Google Scholar]
- 26.Naylor GM, Gotoda T, Dixon M, Shimoda T, Gatta L, Owen R, Tompkins D, Axon A. Why does Japan have a high incidence of gastric cancer? Comparison of gastritis between UK and Japanese patients. Gut. 2006;55:1545–1552. doi: 10.1136/gut.2005.080358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Quach DT, Le HM, Nguyen OT, Nguyen TS, Uemura N. The severity of endoscopic gastric atrophy could help to predict Operative Link on Gastritis Assessment gastritis stage. J Gastroenterol Hepatol. 2011;26:281–285. doi: 10.1111/j.1440-1746.2010.06474.x. [DOI] [PubMed] [Google Scholar]
- 28.Quach DT, Le HM, Hiyama T, Nguyen OT, Nguyen TS, Uemura N. Relationship between endoscopic and histologic gastric atrophy and intestinal metaplasia. Helicobacter. 2013;18:151–157. doi: 10.1111/hel.12027. [DOI] [PubMed] [Google Scholar]
- 29.Kono S, Gotoda T, Yoshida S, Oda I, Kondo H, Gatta L, Naylor G, Dixon M, Moriyasu F, Axon A. Can endoscopic atrophy predict histological atrophy? Historical study in United Kingdom and Japan. World J Gastroenterol. 2015;21:13113–13123. doi: 10.3748/wjg.v21.i46.13113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fukuta N, Ida K, Kato T, Uedo N, Ando T, Watanabe H, Shimbo T Study Group for Investigating Endoscopic Diagnosis of Gastric Intestinal Metaplasia. Endoscopic diagnosis of gastric intestinal metaplasia: a prospective multicenter study. Dig Endosc. 2013;25:526–534. doi: 10.1111/den.12032. [DOI] [PubMed] [Google Scholar]
- 31.Ang TL, Pittayanon R, Lau JY, Rerknimitr R, Ho SH, Singh R, Kwek AB, Ang DS, Chiu PW, Luk S, Goh KL, Ong JP, Tan JY, Teo EK, Fock KM. A multicenter randomized comparison between high-definition white light endoscopy and narrow band imaging for detection of gastric lesions. Eur J Gastroenterol Hepatol. 2015;27:1473–1478. doi: 10.1097/MEG.0000000000000478. [DOI] [PubMed] [Google Scholar]
- 32.Saka A, Yagi K, Nimura S. OLGA- and OLGIM-based staging of gastritis using narrow-band imaging magnifying endoscopy. Dig Endosc. 2015;27:734–741. doi: 10.1111/den.12483. [DOI] [PubMed] [Google Scholar]
- 33.Pimentel-Nunes P, Libânio D, Lage J, Abrantes D, Coimbra M, Esposito G, Hormozdi D, Pepper M, Drasovean S, White JR, Dobru D, Buxbaum J, Ragunath K, Annibale B, Dinis-Ribeiro M. A multicenter prospective study of the real-time use of narrow-band imaging in the diagnosis of premalignant gastric conditions and lesions. Endoscopy. 2016;48:723–730. doi: 10.1055/s-0042-108435. [DOI] [PubMed] [Google Scholar]
- 34.Sha J, Wang P, Zhu B, Zhu M, Li X, Gao F. Acetic Acid Enhanced Narrow Band Imaging for the Diagnosis of Gastric Intestinal Metaplasia. PLoS One. 2017;12:e0170957. doi: 10.1371/journal.pone.0170957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ono S, Kato M, Tsuda M, Miyamoto S, Abiko S, Shimizu Y, Sakamoto N. Lavender Color in Linked Color Imaging Enables Noninvasive Detection of Gastric Intestinal Metaplasia. Digestion. 2018;98:222–230. doi: 10.1159/000489454. [DOI] [PubMed] [Google Scholar]
- 36.Takeda T, Asaoka D, Nojiri S, Nishiyama M, Ikeda A, Yatagai N, Ishizuka K, Hiromoto T, Okubo S, Suzuki M, Nakajima A, Nakatsu Y, Komori H, Akazawa Y, Nakagawa Y, Izumi K, Matsumoto K, Ueyama H, Sasaki H, Shimada Y, Matsumoto K, Osada T, Hojo M, Kato M, Nagahara A. Linked Color Imaging and the Kyoto Classification of Gastritis: Evaluation of Visibility and Inter-Rater Reliability. Digestion. 2019:1–10. doi: 10.1159/000501534. [DOI] [PubMed] [Google Scholar]
- 37.Esposito G, Pimentel-Nunes P, Angeletti S, Castro R, Libânio D, Galli G, Lahner E, Di Giulio E, Annibale B, Dinis-Ribeiro M. Endoscopic grading of gastric intestinal metaplasia (EGGIM): a multicenter validation study. Endoscopy. 2019;51:515–521. doi: 10.1055/a-0808-3186. [DOI] [PubMed] [Google Scholar]
- 38.Dohi O, Majima A, Naito Y, Yoshida T, Ishida T, Azuma Y, Kitae H, Matsumura S, Mizuno N, Yoshida N, Kamada K, Itoh Y. Can image-enhanced endoscopy improve the diagnosis of Kyoto classification of gastritis in the clinical setting? Dig Endosc. 2019 doi: 10.1111/den.13540. [DOI] [PubMed] [Google Scholar]
- 39.Chiu PWY, Uedo N, Singh R, Gotoda T, Ng EKW, Yao K, Ang TL, Ho SH, Kikuchi D, Yao F, Pittayanon R, Goda K, Lau JYW, Tajiri H, Inoue H. An Asian consensus on standards of diagnostic upper endoscopy for neoplasia. Gut. 2019;68:186–197. doi: 10.1136/gutjnl-2018-317111. [DOI] [PubMed] [Google Scholar]
- 40.Uedo N, Ishihara R, Iishi H, Yamamoto S, Yamamoto S, Yamada T, Imanaka K, Takeuchi Y, Higashino K, Ishiguro S, Tatsuta M. A new method of diagnosing gastric intestinal metaplasia: narrow-band imaging with magnifying endoscopy. Endoscopy. 2006;38:819–824. doi: 10.1055/s-2006-944632. [DOI] [PubMed] [Google Scholar]
- 41.Kanemitsu T, Yao K, Nagahama T, Imamura K, Fujiwara S, Ueki T, Chuman K, Tanabe H, Atsuko O, Iwashita A, Shimokawa T, Uchita K, Kanesaka T. Extending magnifying NBI diagnosis of intestinal metaplasia in the stomach: the white opaque substance marker. Endoscopy. 2017;49:529–535. doi: 10.1055/s-0043-103409. [DOI] [PubMed] [Google Scholar]
- 42.Togo K, Ueo T, Yao K, Wada K, Honda H, Inoue S, Fukuda M, Yanai Y, Yonemasu H, Murakami K. White opaque substance visualized by magnifying narrow-band imaging is associated with intragastric acid conditions. Endosc Int Open. 2018;6:E830–E837. doi: 10.1055/a-0611-4825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nagata N, Shimbo T, Akiyama J, Nakashima R, Kim HH, Yoshida T, Hoshimoto K, Uemura N. Predictability of Gastric Intestinal Metaplasia by Mottled Patchy Erythema Seen on Endoscopy. Gastroenterology Res. 2011;4:203–209. doi: 10.4021/gr357w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Achyut BR, Moorchung N, Srivastava AN, Gupta NK, Mittal B. Risk of lymphoid follicle development in patients with chronic antral gastritis: role of endoscopic features, histopathological parameters, CagA status and interleukin-1 gene polymorphisms. Inflamm Res. 2008;57:51–56. doi: 10.1007/s00011-007-7033-2. [DOI] [PubMed] [Google Scholar]
- 45.Miyamoto M, Haruma K, Yoshihara M, Hiyama T, Sumioka M, Nishisaka T, Tanaka S, Chayama K. Nodular gastritis in adults is caused by Helicobacter pylori infection. Dig Dis Sci. 2003;48:968–975. doi: 10.1023/a:1023016000096. [DOI] [PubMed] [Google Scholar]
- 46.Chen MJ, Wang TE, Chang WH, Liao TC, Lin CC, Shih SC. Nodular gastritis: an endoscopic indicator of Helicobacter Pylori infection. Dig Dis Sci. 2007;52:2662–2666. doi: 10.1007/s10620-006-9281-3. [DOI] [PubMed] [Google Scholar]
- 47.Nomura S, Terao S, Adachi K, Kato T, Ida K, Watanabe H, Shimbo T Research Group for Establishment of Endoscopic Diagnosis of Chronic Gastritis. Endoscopic diagnosis of gastric mucosal activity and inflammation. Dig Endosc. 2013;25:136–146. doi: 10.1111/j.1443-1661.2012.01357.x. [DOI] [PubMed] [Google Scholar]
- 48.Toyoshima O, Nishizawa T, Sakitani K, Yamakawa T, Takahashi Y, Yamamichi N, Hata K, Seto Y, Koike K, Watanabe H, Suzuki H. Serum anti-Helicobacter pylori antibody titer and its association with gastric nodularity, atrophy, and age: A cross-sectional study. World J Gastroenterol. 2018;24:4061–4068. doi: 10.3748/wjg.v24.i35.4061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nishikawa I, Kato J, Terasoma S, Matsutani H, Tamaki H, Tamaki T, Kuwashima F, Nakata H, Tomeki T, Matsunaka H, Ibata Y, Yamashita Y, Maekita T, Higashi K, Ichinose M. Nodular gastritis in association with gastric cancer development before and after Helicobacter pylori eradication. JGH Open. 2018;2:80–86. doi: 10.1002/jgh3.12049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Uchiyama K, Ida K, Okuda J, Asai Y, Ohyama Y, Kuroda M, Matsumoto N, Takami T, Ogawa T, Takaori K. Correlations of hemoglobin index (IHb) of gastric mucosa with Helicobacter pylori (H. pylori) infection and inflammation of gastric mucosa. Scand J Gastroenterol. 2004;39:1054–1060. doi: 10.1080/00365520410009645. [DOI] [PubMed] [Google Scholar]
- 51.Sakae H, Iwamuro M, Okamoto Y, Obayashi Y, Baba Y, Hamada K, Gotoda T, Abe M, Kono Y, Kanzaki H, Kawano S, Kawahara Y, Tanaka T, Yanai H, Okada H. Evaluation of the Usefulness and Convenience of the Kyoto Classification of Gastritis in the Endoscopic Diagnosis of the Helicobacter pylori Infection Status. Digestion. 2019:1–8. doi: 10.1159/000502573. [DOI] [PubMed] [Google Scholar]
- 52.Zullo A, Hassan C, Romiti A, Giusto M, Guerriero C, Lorenzetti R, Campo SM, Tomao S. Follow-up of intestinal metaplasia in the stomach: When, how and why. World J Gastrointest Oncol. 2012;4:30–36. doi: 10.4251/wjgo.v4.i3.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Watanabe K, Nagata N, Nakashima R, Furuhata E, Shimbo T, Kobayakawa M, Sakurai T, Imbe K, Niikura R, Yokoi C, Akiyama J, Uemura N. Predictive findings for Helicobacter pylori-uninfected, -infected and -eradicated gastric mucosa: validation study. World J Gastroenterol. 2013;19:4374–4379. doi: 10.3748/wjg.v19.i27.4374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Song H, Ekheden IG, Zheng Z, Ericsson J, Nyrén O, Ye W. Incidence of gastric cancer among patients with gastric precancerous lesions: observational cohort study in a low risk Western population. BMJ. 2015;351:h3867. doi: 10.1136/bmj.h3867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Olmez S, Aslan M, Erten R, Sayar S, Bayram I. The Prevalence of Gastric Intestinal Metaplasia and Distribution of Helicobacter pylori Infection, Atrophy, Dysplasia, and Cancer in Its Subtypes. Gastroenterol Res Pract. 2015;2015:434039. doi: 10.1155/2015/434039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Genta RM, Sonnenberg A. Helicobacter-negative gastritis: a distinct entity unrelated to Helicobacter pylori infection. Aliment Pharmacol Ther. 2015;41:218–226. doi: 10.1111/apt.13007. [DOI] [PubMed] [Google Scholar]
- 57.Laine L, Cohen H, Sloane R, Marin-Sorensen M, Weinstein WM. Interobserver agreement and predictive value of endoscopic findings for H. pylori and gastritis in normal volunteers. Gastrointest Endosc. 1995;42:420–423. doi: 10.1016/s0016-5107(95)70043-9. [DOI] [PubMed] [Google Scholar]
- 58.Yagi K, Nakamura A, Sekine A. Characteristic endoscopic and magnified endoscopic findings in the normal stomach without Helicobacter pylori infection. J Gastroenterol Hepatol. 2002;17:39–45. doi: 10.1046/j.1440-1746.2002.02665.x. [DOI] [PubMed] [Google Scholar]
- 59.Kato T, Yagi N, Kamada T, Shimbo T, Watanabe H, Ida K Study Group for Establishing Endoscopic Diagnosis of Chronic Gastritis. Diagnosis of Helicobacter pylori infection in gastric mucosa by endoscopic features: a multicenter prospective study. Dig Endosc. 2013;25:508–518. doi: 10.1111/den.12031. [DOI] [PubMed] [Google Scholar]
- 60.Mao T, Wang Y, Yin F, Zhao Q, Yang L, Ding X, Tian Z. Association of Endoscopic Features of Gastric Mucosa with Helicobacter pylori Infection in Chinese Patients. Gastroenterol Res Pract. 2016;2016:6539639. doi: 10.1155/2016/6539639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yoshii S, Mabe K, Watano K, Ohno M, Matsumoto M, Ono S, Kudo T, Nojima M, Kato M, Sakamoto N. Validity of endoscopic features for the diagnosis of Helicobacter pylori infection status based on the Kyoto classification of gastritis. Dig Endosc. 2020;32:74–83. doi: 10.1111/den.13486. [DOI] [PubMed] [Google Scholar]
- 62.Garcés-Durán R, García-Rodríguez A, Córdova H, Cuatrecasas M, Ginès À, González-Suárez B, Araujo I, Llach J, Fernández-Esparrach G. Association between a regular arrangement of collecting venules and absence of Helicobacter pylori infection in a European population. Gastrointest Endosc. 2019;90:461–466. doi: 10.1016/j.gie.2019.05.027. [DOI] [PubMed] [Google Scholar]
- 63.Toyoshima O, Nishizawa T, Arita M, Kataoka Y, Sakitani K, Yoshida S, Yamashita H, Hata K, Watanabe H, Suzuki H. Helicobacter pylori infection in subjects negative for high titer serum antibody. World J Gastroenterol. 2018;24:1419–1428. doi: 10.3748/wjg.v24.i13.1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nishizawa T, Sakitani K, Suzuki H, Yamakawa T, Takahashi Y, Yamamichi N, Watanabe H, Seto Y, Koike K, Toyoshima O. A combination of serum anti-Helicobacter pylori antibody titer and Kyoto classification score could provide a more accurate diagnosis of H pylori. United European Gastroenterol J. 2019;7:343–348. doi: 10.1177/2050640619825947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Uemura N, Okamoto S, Yamamoto S, Matsumura N, Yamaguchi S, Yamakido M, Taniyama K, Sasaki N, Schlemper RJ. Helicobacter pylori infection and the development of gastric cancer. N Engl J Med. 2001;345:784–789. doi: 10.1056/NEJMoa001999. [DOI] [PubMed] [Google Scholar]
- 66.Take S, Mizuno M, Ishiki K, Hamada F, Yoshida T, Yokota K, Okada H, Yamamoto K. Seventeen-year effects of eradicating Helicobacter pylori on the prevention of gastric cancer in patients with peptic ulcer; a prospective cohort study. J Gastroenterol. 2015;50:638–644. doi: 10.1007/s00535-014-1004-5. [DOI] [PubMed] [Google Scholar]
- 67.Sakitani K, Hirata Y, Suzuki N, Shichijo S, Yanai A, Serizawa T, Sakamoto K, Akanuma M, Maeda S, Yamaji Y, Iwamoto Y, Kawazu S, Koike K. Gastric cancer diagnosed after Helicobacter pylori eradication in diabetes mellitus patients. BMC Gastroenterol. 2015;15:143. doi: 10.1186/s12876-015-0377-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Toyoshima O, Yamaji Y, Yoshida S, Matsumoto S, Yamashita H, Kanazawa T, Hata K. Endoscopic gastric atrophy is strongly associated with gastric cancer development after Helicobacter pylori eradication. Surg Endosc. 2017;31:2140–2148. doi: 10.1007/s00464-016-5211-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shichijo S, Hirata Y, Niikura R, Hayakawa Y, Yamada A, Koike K. Association between gastric cancer and the Kyoto classification of gastritis. J Gastroenterol Hepatol. 2017;32:1581–1586. doi: 10.1111/jgh.13764. [DOI] [PubMed] [Google Scholar]
- 70.Take S, Mizuno M, Ishiki K, Yoshida T, Ohara N, Yokota K, Oguma K, Okada H, Yamamoto K. The long-term risk of gastric cancer after the successful eradication of Helicobacter pylori. J Gastroenterol. 2011;46:318–324. doi: 10.1007/s00535-010-0347-9. [DOI] [PubMed] [Google Scholar]
- 71.Shichijo S, Hirata Y, Niikura R, Hayakawa Y, Yamada A, Ushiku T, Fukayama M, Koike K. Histologic intestinal metaplasia and endoscopic atrophy are predictors of gastric cancer development after Helicobacter pylori eradication. Gastrointest Endosc. 2016;84:618–624. doi: 10.1016/j.gie.2016.03.791. [DOI] [PubMed] [Google Scholar]
- 72.Kaji K, Hashiba A, Uotani C, Yamaguchi Y, Ueno T, Ohno K, Takabatake I, Wakabayashi T, Doyama H, Ninomiya I, Kiriyama M, Ohyama S, Yoneshima M, Koyama N, Takeda Y, Yasuda K. Grading of Atrophic Gastritis is Useful for Risk Stratification in Endoscopic Screening for Gastric Cancer. Am J Gastroenterol. 2019;114:71–79. doi: 10.1038/s41395-018-0259-5. [DOI] [PubMed] [Google Scholar]
- 73.Nishibayashi H, Kanayama S, Kiyohara T, Yamamoto K, Miyazaki Y, Yasunaga Y, Shinomura Y, Takeshita T, Takeuchi T, Morimoto K, Matsuzawa Y. Helicobacter pylori-induced enlarged-fold gastritis is associated with increased mutagenicity of gastric juice, increased oxidative DNA damage, and an increased risk of gastric carcinoma. J Gastroenterol Hepatol. 2003;18:1384–1391. doi: 10.1046/j.1440-1746.2003.03192.x. [DOI] [PubMed] [Google Scholar]
- 74.Sugimoto M, Ban H, Ichikawa H, Sahara S, Otsuka T, Inatomi O, Bamba S, Furuta T, Andoh A. Efficacy of the Kyoto Classification of Gastritis in Identifying Patients at High Risk for Gastric Cancer. Intern Med. 2017;56:579–586. doi: 10.2169/internalmedicine.56.7775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Majima A, Dohi O, Takayama S, Hirose R, Inoue K, Yoshida N, Kamada K, Uchiyama K, Ishikawa T, Takagi T, Handa O, Konishi H, Naito Y, Itoh Y. Linked color imaging identifies important risk factors associated with gastric cancer after successful eradication of Helicobacter pylori. Gastrointest Endosc. 2019;90:763–769. doi: 10.1016/j.gie.2019.06.043. [DOI] [PubMed] [Google Scholar]
- 76.Masuyama H, Yoshitake N, Sasai T, Nakamura T, Masuyama A, Zuiki T, Kurashina K, Mieda M, Sunada K, Yamamoto H, Togashi K, Terano A, Hiraishi H. Relationship between the degree of endoscopic atrophy of the gastric mucosa and carcinogenic risk. Digestion. 2015;91:30–36. doi: 10.1159/000368807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sekikawa A, Fukui H, Sada R, Fukuhara M, Marui S, Tanke G, Endo M, Ohara Y, Matsuda F, Nakajima J, Henmi S, Saito S, Tsumura T, Maruo T, Kimura T, Osaki Y. Gastric atrophy and xanthelasma are markers for predicting the development of early gastric cancer. J Gastroenterol. 2016;51:35–42. doi: 10.1007/s00535-015-1081-0. [DOI] [PubMed] [Google Scholar]
- 78.Chung SJ, Park MJ, Kang SJ, Kang HY, Chung GE, Kim SG, Jung HC. Effect of annual endoscopic screening on clinicopathologic characteristics and treatment modality of gastric cancer in a high-incidence region of Korea. Int J Cancer. 2012;131:2376–2384. doi: 10.1002/ijc.27501. [DOI] [PubMed] [Google Scholar]
- 79.Yasunaga Y, Shinomura Y, Kanayama S, Higashimoto Y, Yabu M, Miyazaki Y, Kondo S, Murayama Y, Nishibayashi H, Kitamura S, Matsuzawa Y. Increased production of interleukin 1 beta and hepatocyte growth factor may contribute to foveolar hyperplasia in enlarged fold gastritis. Gut. 1996;39:787–794. doi: 10.1136/gut.39.6.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Yasunaga Y, Shinomura Y, Kanayama S, Higashimoto Y, Yabu M, Miyazaki Y, Murayama Y, Nishibayashi H, Kitamura S, Matsuzawa Y. Mucosal interleukin-1 beta production and acid secretion in enlarged fold gastritis. Aliment Pharmacol Ther. 1997;11:801–809. doi: 10.1046/j.1365-2036.1997.00200.x. [DOI] [PubMed] [Google Scholar]
- 81.Miyazaki T, Murayama Y, Shinomura Y, Yamamoto T, Watabe K, Tsutsui S, Kiyohara T, Tamura S, Hayashi N. E-cadherin gene promoter hypermethylation in H. pylori-induced enlarged fold gastritis. Helicobacter. 2007;12:523–531. doi: 10.1111/j.1523-5378.2007.00519.x. [DOI] [PubMed] [Google Scholar]
- 82.Yamamoto E, Toyota M, Suzuki H, Kondo Y, Sanomura T, Murayama Y, Ohe-Toyota M, Maruyama R, Nojima M, Ashida M, Fujii K, Sasaki Y, Hayashi N, Mori M, Imai K, Tokino T, Shinomura Y. LINE-1 hypomethylation is associated with increased CpG island methylation in Helicobacter pylori-related enlarged-fold gastritis. Cancer Epidemiol Biomarkers Prev. 2008;17:2555–2564. doi: 10.1158/1055-9965.EPI-08-0112. [DOI] [PubMed] [Google Scholar]
- 83.Suzuki M, Suzuki H, Minegishi Y, Ito K, Nishizawa T, Hibi T. H. Pylori-Eradication Therapy Increases RUNX3 Expression in the Glandular Epithelial Cells in Enlarged-Fold Gastritis. J Clin Biochem Nutr. 2010;46:259–264. doi: 10.3164/jcbn.09-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yamamoto E, Suzuki H, Takamaru H, Yamamoto H, Toyota M, Shinomura Y. Role of DNA methylation in the development of diffuse-type gastric cancer. Digestion. 2011;83:241–249. doi: 10.1159/000320453. [DOI] [PubMed] [Google Scholar]
- 85.Tahara T, Tahara S, Horiguchi N, Kato T, Shinkai Y, Okubo M, Terada T, Yoshida D, Funasaka K, Nagasaka M, Nakagawa Y, Kurahashi H, Shibata T, Tsukamoto T, Ohmiya N. Prostate Stem Cell Antigen Gene Polymorphism Is Associated with H. pylori-related Promoter DNA Methylation in Nonneoplastic Gastric Epithelium. Cancer Prev Res (Phila) 2019;12:579–584. doi: 10.1158/1940-6207.CAPR-19-0035. [DOI] [PubMed] [Google Scholar]
- 86.Watanabe M, Kato J, Inoue I, Yoshimura N, Yoshida T, Mukoubayashi C, Deguchi H, Enomoto S, Ueda K, Maekita T, Iguchi M, Tamai H, Utsunomiya H, Yamamichi N, Fujishiro M, Iwane M, Tekeshita T, Mohara O, Ushijima T, Ichinose M. Development of gastric cancer in nonatrophic stomach with highly active inflammation identified by serum levels of pepsinogen and Helicobacter pylori antibody together with endoscopic rugal hyperplastic gastritis. Int J Cancer. 2012;131:2632–2642. doi: 10.1002/ijc.27514. [DOI] [PubMed] [Google Scholar]
- 87.Kamada T, Tanaka A, Yamanaka Y, Manabe N, Kusunoki H, Miyamoto M, Tanaka S, Hata J, Chayama K, Haruma K. Nodular gastritis with helicobacter pylori infection is strongly associated with diffuse-type gastric cancer in young patients. Digestive Endoscopy. 2007;19:180–184. [Google Scholar]