Abstract
Background
A decision to delay seeking treatment for symptoms of acute coronary syndrome increases the risk of serious complications, disability, and death.
Aims
The purpose of this study was to determine if there was an association between gradual vs abrupt symptom onset and prehospital delay for patients with acute coronary syndrome and to examine the relationship between activities at symptom onset and gradual vs abrupt symptom onset.
Methods
This was a secondary analysis of a large prospective multi-center study. Altogether, 474 patients presenting to the emergency department with symptoms of acute coronary syndrome were included in the study. Symptom characteristics, activity at symptom onset, and prehospital delay were measured with the ACS Patient Questionnaire.
Results
Median prehospital delay time was four hours. Being uninsured (β=0.120, p=0.031) and having a gradual onset of symptoms (β=0.138, p=0.003) were associated with longer delay. A diagnosis of ST-elevation myocardial infarction (β=−0.205, p=0.001) and arrival by ambulance (β=−0.317, p<0.001) were associated with shorter delay. Delay times were shorter for patients who experienced an abrupt vs gradual symptom onset (2.57 h vs 8 h, p<0.001). Among men with an abrupt onset of symptoms and a ST-elevation myocardial infarction diagnosis, 54% reported that symptoms were triggered by exertion (p=0.046).
Conclusion
Patients should be counselled that a gradual onset of symptoms for potential acute coronary syndrome is an emergency and that they should call 911. Men with ischemic heart disease or with multiple risk factors should be cautioned that symptom onset following exertion may represent acute coronary syndrome.
Keywords: Acute coronary syndrome, prehospital delay, symptoms, symptom onset, sex differences, treatment-seeking
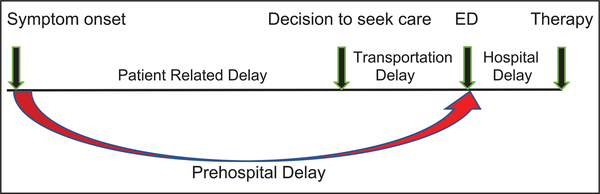
Failure to recognize symptoms of acute coronary syndrome (ACS) and to respond rapidly and appropriately has been implicated in prehospital delay.1 Total prehospital delay time is defined as the time from symptom onset to arrival in the emergency department (ED). Prehospital delay has three phases: (a) symptom recognition to a decision to seek medical care; (b) the decision to seek care to first medical contact; and (c) first medical contact to hospital arrival (“transportation time”) (Figure 1).2 Delay times of more than two hours are still common and continue to pose a threat to the administration of timely and effective treatments.3,4 Studies have shown that the time for individuals to recognize, interpret, and make a decision to seek medical attention (individual’s delay time) is the main cause and the major contributor to prehospital delay. Thus, the best option for reducing total ischemic time, and to preserve myocardium, is to reduce the time from symptom onset to first medical contact.5,6 Total ischemic time has a critical impact on outcomes in patients with ACS.7 The decision to delay seeking treatment considerably increase a person’s risk for serious complications, major disability, and death.8 There is little reduction in mortality for reperfusion if it occurs after six hours, and studies demonstrate that every 30 min delay in flow restoration reduces life expectancy by one year.9,10
Figure 1.
Phases of delay time in patients with acute coronary syndrome (ACS) before reperfusion therapy. ED: emergency department.
The sub-categories of ACS include ST-elevation myocardial infarction (STEMI), non-ST-elevation myocardial infarction (NSTEMI), and unstable angina (UA). STEMI presents with abnormal troponin cardiac enzymes. Revascularization, often percutaneous coronary intervention (PCI), is an emergency. For patients with NSTEMI, positive biomarkers, transient ST elevation, ST depression, or new T wave inversions with continuous cardiac chest pain are diagnostic. An invasive strategy, such as PCI, is often selected in addition to medical therapy. Patients with UA, present with normal initial biomarkers and symptoms at rest and medical therapy is recommended.11,12
Despite decades of research focused on identifying factors associated with patient delay and success in reducing door to balloon times, almost 40% of patients delay longer than six hours, the window needed to salvage myocardial tissue,13,14 indicating that previous attempts to reduce patient delay have been relatively unsuccessful. One reason might be misinterpretation of symptoms.15,16 The timely and accurate identification of symptoms of ACS can be difficult for individuals because such symptoms may be similar to those of other less serious conditions.17 Individuals may attribute their symptoms to non-cardiac causes, and thus not seek care.18 This can lead to decision delay, which consumes the largest proportion of prehospital delay time.6
Characteristics of symptom onset, such as type and timing of symptoms, can affect behaviors that could negatively influence treatment-seeking behavior and increase prehospital delay.15 Some studies have shown that women are more likely to experience longer prehospital delay time than men.19–21 However, other research has suggested that there are no sex differences in prehospital delay time.22,23 Gradual vs abrupt onset of symptoms has been implicated in care-seeking behaviors. In addition, a variety of triggers have been associated with the onset of an acute ischemic episode and may contribute to an individual’s perception of symptoms. Physical activity, behaviors, and emotional upset occurring within 1–2 h of symptom onset have been reported as precursors to ACS.24–26 Whether physical exertion or emotions trigger variations in symptom onset is unknown. Differences in pathophysiology or in risk factors may influence the development and outcomes of symptoms during ACS.27
The need to reduce patient prehospital delay times to speed diagnosis and treatment of ACS has driven efforts to increase knowledge of ACS symptoms among the public and health professionals.28 Prior studies have identified a lack of knowledge of ACS symptoms as an important factor in patients’ delay in seeking medical care.29,30 Additional evidence of how the symptom experience influences care seeking behavior will enable health care providers to target and develop interventions to decrease prehospital delay.31 Therefore, the objectives of this study were to: (a) determine if there was an association between gradual vs abrupt onset and prehospital delay time for women and men with ACS; and (b) examine the relationship between activities at symptom onset and gradual vs abrupt symptom onset.
Methods
Design, sample, and setting
This is a secondary data analysis using data from a large prospective, multicenter study conducted in four regions of the USA (Pacific Northwest, West, Southwest, and Midwest).32 Study sites included four academic medical centers and one large regional referral hospital. Enrollment occurred from January 2011–December 2014. Symptoms were assessed within 15 min of admission to the ED. In-depth methods have been reported elsewhere.33 The sample included 1064 women and men presenting to the ED for symptoms of potential ACS. This secondary data analysis included only patients that went on to be diagnosed with ACS (n=474) because this is the population of high-risk patients who may require urgent reperfusion therapies. Inclusion criteria were: (a) ⩾21 years old, (b) ability to speak and understand English, and (c) arrived by private transportation or emergency medical services (EMS). Exclusion criteria were: (a) exacerbation of heart failure (brain natriuretic peptide >500 pg/ml), (b) transferred from a hemodialysis center, (c) referred for evaluation of a dysrhythmia, and (d) cognitive impairment.32 The study received the approval of Institutional Review Boards at the five data collection sites and the sponsoring institution.
Measures
Symptom characteristics and time from symptom onset to arrival in the ED were assessed with the ACS Patient Information Questionnaire. The questionnaire includes patient-reported information on demographic and symptom variables, including symptom onset and activity at symptom onset. The questionnaire was designed using the standardized reporting guidelines for studies evaluating patients with potential ACS in emergency settings.34 The criteria were established by the Multidisciplinary Standardized Reporting Criteria Task Force and are supported by the Society for Academic Medicine, the American College of Emergency Physicians, the American Heart Association, and the American College of Cardiology.34 Prehospital delay time was the primary outcome. Patients were asked to recall the time that their symptoms began. The time difference between symptom onset and ED arrival constituted “prehospital delay”, measured in hours and minutes. Activity at symptom onset was explored with an open-ended question: “What were you doing during the 48 hours before your symptoms began?” Patients gave 209 different answers to their activity at symptom onset and answers were categorized into five themes: (a) resting (e.g. reclining, reclining and watching TV); (b) sleeping; (c) sitting (e.g. deskwork, driving, eating, reading); (d) exertion (e.g. running, jogging, climbing stairs, pulling, pushing, shoveling, heavy gardening), and (e) emotional stress (e.g. anger, tension, stress).
Procedures
Eligible patients were approached by the research staff for enrollment after they were considered stable by hospital staff and had been transferred to a private examination room. The study was then explained, and once consent was obtained, the ACS Information Questionnaire was completed by research staff. All data was collected directly from the patient in the ED or catheterization laboratory.
Data analysis
Data were examined for their distributional properties, outliers, and presence of missing data. Participants with missing data for prehospital delay times (n=45) or symptom onset (n=6) were excluded from the analyses. Descriptive statistics were used to summarize the demographic and clinical characteristics of the sample. Comparison of means was accomplished using independent sample t tests. Categorical variables were analyzed using the chi-square test and were reported as frequencies and percentages. Prehospital delay time was initially analyzed for conformity to the normal distribution assumptions using the Shapiro-Wilk test and a histogram. Because prehospital delay times were not normally distributed (positive skew), delay times are presented as medians and interquartile ranges (IQRs). Data were log-transformed for regression analyses. The nonparametric Mann-Whitney test was used to compare prehospital delay times between two groups of patients; those with abrupt symptom onset and those with gradual symptom onset. Bivariate regression analyses were initially conducted on prehospital delay time and each sociodemographic and clinical variable. In multiple regression analysis, all variables were entered into the regression model simultaneously. Linktest was used to test for model specification of independent variables after each regression model. The results indicated that the regression model specified variables correctly. The omnibus test, which tests the null hypothesis of no difference across groups,35 conducted after predictors for more than two categories which were significant in the regression model was used to examine differences across the group. Chi-square tests were used to compare differences in activity at symptom onset in women and men. All statistical analyses were run with STATA statistical software (Version 14.2, Release12, StataCorp LP, College Station, Texas, USA). Significance was set at p<0.05 for all statistical tests.
Results
A total of 474 patients with ACS were included in the study. Demographic and clinical characteristics of patients are shown in Table 1. One hundred thirty-one women (27.65%) and 343 men (72.65%), ranging in age from 29–93 years (mean age 61.68±11.94 years) were enrolled. Women were significantly older than men (64.72 years vs 60.52 years; p<0.001).
Table 1.
Demographic and clinical characteristics by sex (n=474).
| Characteristics | Total (n=474) | Women (n=131, 27.65%) | Men (n=343, 72.65%) | p Value |
|---|---|---|---|---|
| Age, mean (SD) | 61.68 (11.94) | 64.72 (13.32) | 60.52 (11.17) | <0.001 |
| Race/ethnicity | 0.532 | |||
| White | 325 (69.1) | 87 (66.92) | 238 (69.79) | |
| Black | 56 (11.9) | 20 (15.38) | 36 (10.56) | |
| Hispanic | 45 (9.5) | 12 (9.23) | 33 (9.68) | |
| Other | 45 (9.5) | 11 (8.46) | 34 (9.97) | |
| Insurance | 0.015 | |||
| Private | 195 (42.12) | 56 (43.41) | 139 (41.62) | |
| Govt./other | 197 (42.55) | 63 48.84) | 134(40.12) | |
| Not insured | 71 (15.33) | 10 (7.75) | 61 (18.26) | |
| Education | 0.317 | |||
| <High school diploma | 60 (12.7) | 23 (17.56) | 37 (10.82) | |
| High school diploma | 112 (23.6) | 32 (14.43) | 80 (23.39) | |
| Some college | 154 (32.5) | 41 (31.30) | 113 (33.04) | |
| College degree/grad work | 89 (18.8) | 22 (16.79) | 67 (19.59) | |
| Graduate degree | 58 (12.2) | 13 (9.92) | 45 (13.16) | |
| Income, n (%) | 0.874 | |||
| <$20,000 | 121 (25.5) | 34 (25.95) | 87 (25.36) | |
| $20,000–$49,999 | 139 (29.3) | 39 (29.77) | 100 (29.15) | |
| $50,000–$99,999 | 103 (22.0) | 26 (19.85) | 77 (22.45) | |
| ⩾$100,000 | 56 (11.8) | 14 (10.69) | 42 (12.24) | |
| Missing | 55 (11.6) | 18 (13.74) | 37 (10.79) | |
| Marital status, n (%) | 0.526 | |||
| Single/separated/divorced/widowed | 202 (42.71) | 59 (45.04) | 143 (41.81) | |
| Married/committed relationship | 271 (57.29) | 72 (54.96) | 199 (58.19) | |
| Recruitment site | 0.345 | |||
| Midwest | 55 (11.6) | 54 (41.22) | 129 (37.61) | |
| Northwest 1 | 85 (18.0) | 16 (12.21) | 39 (11.37) | |
| Northwest 2 | 46 (9.7) | 22 (16.79) | 63 (18.37) | |
| West | 183 (38.6) | 7 (5.34) | 39 (11.37) | |
| Southwest | 105 (22.2) | 32 (24.43) | 73 (21.28) | |
| Obese | 0.193 | |||
| Yes | 184 (39.07) | 45 (34.35) | 139 (40.88) | |
| No | 287 (60.93) | 86 (65.65) | 201 (59.12) | |
| Diagnosis | 0.291 | |||
| Unstable angina | 105 (22.15) | 31 (23.66) | 74 (21.57) | |
| NSTEMI | 251 (52.95) | 74 (57.49) | 177 (52.60) | |
| STEMI | 118 (24.89) | 24 (19.85) | 92 (26.82) | |
| Diabetes | 0.322 | |||
| Yes | 140 (29.98) | 34 (26.56) | 106 (31.27) | |
| No | 327 (70.02) | 94 (73.44) | 233 (68.73) | |
| Hypertension | 0.404 | |||
| Yes | 324 (68.79) | 85 (65.89) | 239 (69.88) | |
| No | 147 (31.21) | 41 (34.11) | 103 (30.12) | |
| Family history heart disease/premature cardiac death | 0.255 | |||
| Yes | 214 (46.52) | 65 (51.78) | 149 (44.88) | |
| No | 246 (53.48) | 63 (49.22) | 183 (55.12) | |
| Current smoker | 0.118 | |||
| Yes | 114 (24.05) | 25 (19.08) | 89 (25.95) | |
| No | 360 (75.95) | 106 (80.92) | 254 (74.05) | |
| Mode of arrival to the ED | 0.319 | |||
| Self-transport | 245 (52.02) | 61 (46.92) | 184 (53.96) | |
| Ambulance/paramedic | 210 (44.59) | 63 (48.46) | 147 (43.11) | |
| Transfer from another facility | 16 (3.40) | 6 (4.62) | 10 (2.93) |
ED: emergency department; Govt.: government; NSTEMI: non-ST elevation myocardial infarction; SD: standard deviation; STEMI: ST-elevation myocardial infarction.
Statistically significant values are bolded.
Abrupt versus gradual symptom onset
Two hundred sixty-one patients (55.77%) reported abrupt symptom onset, and 207 (44.23%) experienced gradual symptom onset. Of note, 115 (24.57%) patients were diagnosed with STEMI. Of these, 65 (56.52%) experienced abrupt symptom onset, and 50 (43.48%) experienced gradual symptom onset. There were no significant differences in demographic and clinical characteristic between patients with ACS who reported an abrupt versus gradual symptom onset in this cohort (Table 2). Women in both the abrupt symptom onset and gradual symptom onset groups were significantly older than men (64.01±13.22 vs 59.73±11.52, p=0.008, and 66.08±13.80 vs 61.39±10.73, p=0.013 respectively; Table 3). In the gradual symptom onset group, men were more likely to have higher education levels than women (p=0.02). For the abrupt symptom onset group, men were more likely to be current smokers compared to women (p=0.04).
Table 2.
Sample characteristics for abrupt and gradual onset of symptom groups (n=468).
| Sample characteristics | Abrupt symptom onset (n=261; 55.77%) | Gradual symptom onset (n=207; 44.23%) | p Value |
|---|---|---|---|
| Age, mean (SD) | 61.03 (12.19) | 62.50 (11.67) | 0.18 |
| Race/ethnicity | 0.363 | ||
| White | 173 (66.80) | 147 (71.36) | |
| Black | 36 (13.90) | 19 (9.22) | |
| Hispanic | 23 (8.88) | 22 (10.68) | |
| Other | 27 (10.42) | 18 (8.74) | |
| Insurance | 0.572 | ||
| Private | 113 (44.14) | 79 (39.30) | |
| Govt./other | 104 (40.63) | 90 (44.78) | |
| Not insured | 39 (15.23) | 32 (15.92) | |
| Education | 0.84 | ||
| Less than high school diploma | 31 (11.88) | 29 (14.08) | |
| High school diploma | 59 (22.61) | 52 (25.24) | |
| Some college | 90 (34.48) | 63 (30.58) | |
| College degree/graduate work | 48 (18.39) | 38 (18.45) | |
| Graduate degree | 33 (12.64) | 24 (11.65) | |
| Income | 0.127 | ||
| <$20,000 | 61 (26.18) | 60 (28.99) | |
| $20,000–$50,000 | 78 (29.89) | 59 (28.50) | |
| $50,000–$100,000 | 61 (23.37) | 41 (19.81) | |
| $100,000+ | 33 (12.64) | 23 (11.11) | |
| Missing | 28 (10.73) | 24 (11.59) | |
| Marital status | |||
| Single/separated/Divorced/widowed | 109 (41.92) | 93 (44.93) | 0.515 |
| Married/committed relationship | 151 (58.08) | 114 (55.07) | |
| Recruitment site | 0.945 | ||
| Midwest | 104 (39.85) | 78 (37.68) | |
| Northwest 1 | 32 (12.26) | 23 (11.11) | |
| Northwest 2 | 46 (17.62) | 37 (17.87) | |
| West | 23 (8.81) | 22 (10.63) | |
| Southwest | 56 (21.46) | 47 (22.71) | |
| Obese | 0.68 | ||
| Yes | 100 (38.31) | 82 (40.20) | |
| No | 161 (61.69) | 122 (59.80) | |
| Diagnosis | 0.91 | ||
| Unstable angina | 55 (21.07) | 47 (22.71) | |
| NSTEMI | 141 (54.02) | 110 (53.14) | |
| STEMI | 65 (24.90) | 50 (24.15) | |
| Diabetes | 0.38 | ||
| Yes | 74 (28.35) | 66 (32.04) | |
| No | 187 (71.65) | 140 (67.96) | |
| Hypertension | 0.45 | ||
| Yes | 175 (67.83) | 147 (71.01) | |
| No | 83 (32.17) | 60 (28.99) | |
| Family history heart disease/premature cardiac death | 0.78 | ||
| Yes | 116 (46.03) | 96 (47.29) | |
| No | 136 (53.97) | 107 (52.71) | |
| Current smoker | 68 (26.05) | 44 (21.26) | 0.22 |
| Yes | 193 (73.95) | 163 (78.74) | |
| No | |||
| Mode of arrival to the ED | 0.52 | ||
| Self-transport | 137 (52.69) | 106 (51.71) | |
| Ambulance/paramedic | 112 (43.08) | 94 (45.85) | |
| Transfer from another facility | 11 (4.23) | 5 (2.44) |
ED: emergency department; Govt.: government; NSTEMI: non-ST elevation myocardial infarction; SD: standard deviation; STEMI: ST-elevation myocardial infarction.
Statistically significant values are bolded.
Table 3.
Sample characteristics for abrupt and gradual symptom onset groups by sex (n=468).
| Sample characteristics | Abrupt symptom onset (n=261, 55.77%) |
p Value | Gradual symptom onset (207, 44.23%) |
p Value | ||
|---|---|---|---|---|---|---|
| Women (n=79, 61.72%) | Men (n=182, 53.53%) | Women (n=49, 38.28%) | Men (n=158, 46.47%) | |||
| Age (mean, SD) | 64.01 (13.22) | 59.73 (11.52) | 0.008 | 66.08 (13.80) | 61.39 (10.73) | 0.013 |
| Marital status | ||||||
| Single/separated/divorced/widowed | 31 (39.24) | 78 (43.09) | 0.56 | 28 (57.14) | 65 (41.14) | 0.051 |
| Married/committed relationship | 48 (60.76) | 103 (56.91) | 21 (42.86) | 93 (58.86) | ||
| Education | 0.98 | 0.02 | ||||
| <High school Diploma | 10 (12.66) | 21 (11.54) | 13 (26.53) | 16 (10.19) | ||
| High school diploma | 16 (20.25) | 43 (23.63) | 15 (30.61) | 37 (23.57) | ||
| Some college | 28 (35.44) | 62 (34.07) | 12 (24.49) | 51 (32.48) | ||
| College degree | 15 (18.99) | 33 (18.13) | 6 (12.24) | 32 (20.38) | ||
| Graduate degree | 10 (12.66) | 23 (12.64) | 3 (6.12) | 21 (13.38) | ||
| Insurance | 0.084 | 0.112 | ||||
| Private | 37 (74.44) | 76 (42.70) | 17 (35.42) | 62 (40.52) | ||
| Govt./other | 35 (44.87) | 69 (38.76) | 27 (56.25) | 63 (41.18) | ||
| Not insured | 6 (7.69) | 33 (18.54) | 4 (8.33) | 28 (18.30) | ||
| Income | 0.94 | 0.50 | ||||
| <$20,000 | 18 (22.78) | 43 (23.62) | 16 (32.65) | 44 (27.85) | ||
| $20,000–$50,000 | 23 (29.11) | 55 (30.22) | 14 (28.57) | 45 (28.48) | ||
| $50,000–$100,000 | 17 (21.52) | 44 (24.18) | 8 (16.33) | 33 (20.89) | ||
| $100,000+ | 11 (13.92) | 22 (12.09) | 3 (6.33) | 20 (12.66) | ||
| Missing | 10 (12.66) | 18 (9.89) | 8 (16.33) | 16 (10.33) | ||
| Obese | 0.53 | 0.21 | ||||
| Yes | 28 (35.44) | 72 (39.56) | 16 (32.65) | 66 (42.58) | ||
| No | 51 (64.56) | 110 (60.44) | 33 (67.35) | 89 (57.42) | ||
| Diagnosis | 0.32 | 0.51 | ||||
| Unstable angina | 19 (24.05) | 36 (19.78) | 11 (22.45) | 36 (22.78) | ||
| NSTEMI | 45 (56.96) | 96 (52.75) | 29 (59.18) | 81 (51.27) | ||
| STEMI | 15 (18.99) | 50 (27.47) | 9 (18.37) | 41 (25.95) | ||
| Diabetes | 0.67 | 0.34 | ||||
| Yes | 21 (26.58) | 53 (29.12) | 13 (26.53) | 53 (33.76) | ||
| No | 58 (73.42) | 129 (70.88) | 36 (73.47) | 104 (66.24) | ||
| Hypertension | 0.6 | 0.17 | ||||
| Yes | 54 (70.13) | 121 (66.85) | 31 (63.27) | 116 (73.42) | ||
| No | 23 (29.87) | 60 (33.15) | 18 (36.73) | 42 (26.58) | ||
| Family history heart disease/premature cardiac death | 0.32 | 0.35 | ||||
| Yes | 39 (50.65) | 77 (44.00) | 26 (53.06) | 70 (45.45) | ||
| No | 38 (49.35) | 98 (56.00) | 23 (46.94) | 84 (54.55) | ||
| Current smoker | 0.04 | 0.57 | ||||
| Yes | 14 (17.72) | 54 (29.67) | 9 (18.37) | 35 (22.15) | ||
| No | 65 (82.28) | 128 (70.33) | 40 (81.63) | 123 (77.85) | ||
| Mode of arrival to ED | 0.23 | 0.93 | ||||
| Self-transport | 36 (45.57) | 101 (55.80) | 24 (50) | 82 (52.23) | ||
| Ambulance/paramedic | 38 (48.10) | 74 (40.88) | 23 (47.92) | 71 (45.22) | ||
| Transfer from another facility | 5 (6.33) | 6 (3.31) | 1 (2.08) | 4 (2.55) | ||
ED: emergency department; Govt.: government; NSTEMI: non-ST elevation myocardial infarction; SD: standard deviation; STEMI: ST-elevation myocardial infarction.
Statistically significant values are bolded.
Prehospital delay in women and men
The median prehospital delay time for the entire sample was four hours; the IQR was 22.72 h. The median prehospital delay time was 3.47 h (IQR=22.7 h) for women and 4.09 h (IQR=23.7 h) for men (p=0.83). Delay times were significantly shorter in both women and men who experienced abrupt symptom onset (2.57 h, IQR=19 h; 8 h, IQR=46.3; p<001). For women who experienced abrupt symptom onset, the median prehospital delay time was 2.4 h (IQR=16 h); for those in the gradual symptom onset group, it was 11.7 h (IQR=45.6 h; p=0.023). Similarly, there was a significant difference between median delay time in men with abrupt symptom onset (2.8 h, IQR=21.5h) compared to gradual symptom onset (7.17 h, IQR=46.65 h; p<001). Differences between women and men were not significant (abrupt symptom onset 2.48 h, IQR=16 h vs 2.85 h, IQR=21.5 h, p=0.98; gradual symptom onset 11.76 h, IQR=45.6 vs 7.17 h, IQR=46.5 h, respectively, p=0.68).
Factors influencing prehospital delay time
Demographic, clinical, and symptom onset variables were examined to determine if there were associations with prehospital delay (Table 4). In bivariate analysis, there were no significant differences in prehospital delay time in association with demographic characteristics and clinical history. The final regression model accounted for 26.2% of the variance in delay time in patients with ACS. Not being insured (β=0.120, p=0.031) and a gradual symptom onset (β=0.138, p=0.003) were associated with longer prehospital delay times; a diagnosis of STEMI (β=−0.205, p=0.001) and arrival by ambulance (β=−0.317, p<0.001) were associated with shorter delay.
Table 4.
Factors influencing prehospital delay time (n=429).
| Characteristics | n (%) | β | p Value |
|---|---|---|---|
| Age, mean (SD) | 61.68 (11.94) | −0.004 | 0.942 |
| Gender | |||
| Female | 131 (27.64) | 0.041 | 0.387 |
| Male | 343 (72.36) | ||
| Marital status | |||
| Married/committed relationship | 271 (57.29) | 0.078 | 0.112 |
| Single/separated/Divorced/widowed | 202 (42.71) | ||
| Insurance | |||
| Private | 195 (42.12) | 0.003 | 0.955 |
| Not insured | 71 (15.33) | 0.120 | 0.031 |
| Govt./other | 197 (42.55) | ||
| Education | |||
| High school diploma | 112 (23.68) | 0.115 | 0.100 |
| Some college | 154 (32.56) | 0.142 | 0.058 |
| College degree/ graduate work | 89 (18.82) | 0.034 | 0.618 |
| Graduate degree | 58 (12.26) | 0.022 | 0.745 |
| <High school diploma | 60 (12.68) | ||
| Income | |||
| $20,000–$50,000 | 139 (33.17) | 0.056 | 0.458 |
| $50,000–$100,000 | 103 (24.58) | −0.005 | 0.940 |
| $100,000+ | 56 (13.37) | 0.011 | 0.877 |
| <$20,000 | 121 (28.88) | −0.0008 | 0.991 |
| Missing | |||
| Diagnosis | |||
| NSTEMI | 251 (23.59) | −0.030 | 0.618 |
| STEMI | 118 (11.09) | −0.205 | 0.001 |
| Unstable angina | 105 (9.87) | ||
| Obese | |||
| Yes | 184 (39.07) | 0.030 | 0.547 |
| No | 287 (60.93) | ||
| Hypercholesterolemia | |||
| Yes | 292 (63.07) | 0.064 | 0.189 |
| No | 171 (36.93) | ||
| Diabetes | |||
| Yes | 142 (30.02) | 0.012 | 0.793 |
| No | 331 (69.98) | ||
| Hypertension | |||
| Yes | 324 (68.79) | 0.070 | 0.167 |
| No | 147 (31.21) | ||
| Family history heart disease/premature cardiac death | |||
| Yes | 214 (46.52) | 0.081 | 0.091 |
| No | 246 (53.48) | ||
| Current smoker | |||
| Yes | 114 (24.05) | −0.015 | 0.762 |
| No | 360 (75.95) | ||
| Mode of arrival to the ED | |||
| Ambulance/paramedic | 210 (44.59) | −0.317 | <0.001 |
| Transfer from another facility | 16 (3.40) | −0.082 | 0.084 |
| Self-transport | 245 (52.02) | ||
| Onset of symptoms | |||
| Gradual | 207 (44.23) | 0.138 | 0.003 |
| Abrupt | 261 (55.77) |
ED: emergency department; Govt.: government; NSTEMI: non-ST elevation myocardial infarction; SD: standard deviation; STEMI: ST-elevation myocardial infarction.
Statistically significant values are bolded.
Activity at symptom onset
Patients with a STEMI diagnosis, who experienced an abrupt onset of symptoms, were more likely to report that symptoms began following exertion (50.79% vs 49.21%) than were those with an NSTEMI (31.06% vs 68.94%) or UA (39.22% vs 60.78%, p=0.028) diagnosis (Table 5). Patients with a gradual onset of symptoms were less likely to report that symptoms were triggered by exertion regardless of diagnosis. There was a relationship between the type of infarction and exertion in men but there was no such relationship for women. Among men with an abrupt onset of symptoms and a STEMI diagnosis, 54% reported symptoms preceded by exertion (Table 6). For women with a gradual onset of symptom, sleeping was the most common activity at symptom onset in those with STEMI and for men with a gradual onset of symptoms exertion was the most common activity at symptom onset in those with UA (Table 7).
Table 5.
Activity at symptom onset by symptom onset group and diagnosis (n=468).
| Activity at symptom onset | UA | Abrupt symptom onset (n=261, 55.77%) |
p Value | UA | Gradual symptom onset (n=207, 44.23%) |
p Value | ||
|---|---|---|---|---|---|---|---|---|
| NSTEMI | STEMI | NSTEMI | STEMI | |||||
| Rest | 0.21 | 0.15 | ||||||
| Yes | 7 (15.91) | 24 (22.64) | 6 (11.54) | 6 (15.00) | 19 (22.62) | 3 (8.33) | ||
| No | 37 (84.09) | 82 (77.36) | 46 (88.46) | 34 (85.00) | 65 (77.38) | 33 (91.67) | ||
| Sleep | 0.63 | 0.18 | ||||||
| Yes | 7 (13.73) | 26 (19.70) | 11 (17.46) | 2 (4.76) | 8 (8.70) | 7 (16.28) | ||
| No | 44 (86.27) | 106 (80.30) | 52 (82.54) | 40 (95.24) | 84 (91.30) | 36 (83.72) | ||
| Sitting | 0.91 | 0.5 | ||||||
| Yes | 13 (25.49) | 31 (23.48) | 14 (22.22) | 6 (14.29) | 32 (34.78) | 12 (27.91) | ||
| No | 38 (74.51) | 101 (76.52) | 49 (77.78) | 36 (85.71) | 60 (65.22) | 31 (72.09) | ||
| Exertion | 0.028 | 0.001 | ||||||
| Yes | 20 (39.22) | 41 (31.06) | 32 (50.79) | 27 (64.29) | 28 (30.43) | 20 (46.51) | ||
| No | 31 (60.78) | 91 (68.94) | 31 (49.21) | 15 (35.71) | 64 (69.57) | 23 (53.49) | ||
| Emotional stress | 0.07 | 0.57 | ||||||
| Yes | 4 (7.84) | 10 (7.58) | 0 (0.0) | 1 (2.38) | 5 (5.43) | 1 (2.33) | ||
| No | 47 (92.16) | 122 (92.42) | 63 (100) | 41 (97.62) | 87 (94.57) | 42 (97.67) | ||
NSTEMI: non-ST elevation myocardial infarction; STEMI: ST-elevation myocardial infarction; UA: unstable angina.
Statistically significant values are bolded.
Table 6.
Activity for abrupt symptom onset group by sex and diagnosis (n=246).
| Activity at symptom onset | UA | Women (n=76) |
p Value | UA | Men (n=170) |
p Value | ||
|---|---|---|---|---|---|---|---|---|
| NSTEMI | STEMI | NSTEMI | STEMI | |||||
| Rest | 0.53 | 0.21 | ||||||
| Yes | 0 (0.00) | 10 (29.41) | 2 (20.00) | 7 (25.00) | 14 (19.44) | 4 (9.52) | ||
| No | 16 (100) | 24 (70.59) | 8 (80.00) | 21 (75.00) | 58 (80.56) | 38 (90.48) | ||
| Sleep | 0.15 | 0.68 | ||||||
| Yes | 1 (5.88) | 10 (22.73) | 5 (33.33) | 6 (17.65) | 16 (18.18) | 6 (12.50) | ||
| No | 16 (94.12) | 34 (77.27) | 10 (66.67) | 28 (82.35) | 72 (81.82) | 42 (87.50) | ||
| Sitting | 0.24 | 0.81 | ||||||
| Yes | 6 (35.29) | 8 (18.18) | 2 (13.33) | 7 (20.59) | 23 (26.14) | 12 (25.00) | ||
| No | 11 (64.71) | 36 (81.82) | 13 (86.67) | 27 (79.41) | 65 (73.86) | 36 (75.00) | ||
| Exertion | 0.30 | 0.046 | ||||||
| Yes | 8 (47.06) | 12 (27.27) | 6 (40.00) | 12 (35.29) | 29 (32.95) | 26 (54.17) | ||
| No | 9 (52.94) | 32 (72.73) | 9 (60.00) | 22 (64.71) | 59 (76.05) | 22 (45.83) | ||
| Emotional stress | 0.42 | 0.187 | ||||||
| Yes | 2 (11.76) | 4 (9.09) | 0 (0.00) | 2 (5.88) | 6 (6.82) | 0 (0.00) | ||
| No | 15 (88.24) | 40 (90.91) | 15 (100.) | 32 (94.12) | 82 (93.18) | 48 (100) | ||
NSTEMI: non-ST elevation myocardial infarction; STEMI: ST-elevation myocardial infarction; UA: unstable angina.
Statistically significant values are bolded.
Table 7.
Activity for gradual symptom onset group by sex and diagnosis (n=177).
| Activity at symptom onset | UA | Women (n=43) |
p Value | UA | Men (n=134) |
p Value | ||
|---|---|---|---|---|---|---|---|---|
| NSTEMI | STEMI | NSTEMI | STEMI | |||||
| Rest | 0.18 | 0.084 | ||||||
| Yes | 0 (0.00) | 7 (26.92) | 2 (40.00) | 6 (18.75) | 12 (20.69) | 1 (3.23) | ||
| No | 8 (100) | 19 (73.08) | 3 (60.00) | 26 (81.25) | 46 (79.31) | 30 (96.77) | ||
| Sleep | 0.006 | 0.32 | ||||||
| Yes | 1 (11.11) | 0 (0.00) | 3 (37.50) | 1 (3.03) | 8 (12.12) | 4 (11.43) | ||
| No | 8 (88.89) | 26 (100.0) | 5 (62.50) | 32 (96.97) | 58 (87.88) | 31 (88.57) | ||
| Sitting | 0.22 | 0.089 | ||||||
| Yes | 2 (22.22) | 11 (42.31) | 1 (12.50) | 4 (12.12) | 21 (31.82) | 11 (31.43) | ||
| No | 7 (77.78) | 15 (57.69) | 7 (87.50) | 29 (87.88) | 45 (68.18) | 24 (68.57) | ||
| Exertion | 0.079 | 0.007 | ||||||
| Yes | 6 (66.67) | 7 (26.92) | 2 (25.00) | 21 (63.64) | 21 (31.82) | 18 (51.43) | ||
| No | 3 (33.33) | 19 (73.08) | 6 (75.00) | 12 (36.36) | 45 (68.18) | 17 (48.57) | ||
| Emotional stress | 0.716 | 0.68 | ||||||
| Yes | 0 (0.00) | 1 (3.85) | 0 (0.00) | 1 (3.03) | 4 (6.06) | 1 (2.86) | ||
| No | 9 (100) | 25 (96.15) | 8 (100) | 32 (96.97) | 62 (93.94) | 34 (97.14) | ||
NSTEMI: non-ST elevation myocardial infarction; STEMI: ST-elevation myocardial infarction; UA: unstable angina.
Statistically significant values are bolded.
Discussion
Prolonged prehospital delay time can postpone treatment and can result in poor outcomes for patients with ACS, a potentially life-threatening condition. We found that four variables were associated with prehospital delay. Gradual symptom onset and not having insurance were significantly related to longer prehospital delay time. A STEMI diagnosis and use of an ambulance were significantly related to shorter prehospital delay times. Other key findings were that median delay times for women (3.5 h) and men (4 h) were not significantly different. These delay times however, were still significantly longer than the American Heart Association (AHA) recommendation of <120 min.36 Despite the implementation of specific public policies, these times have not changed in the last decade.37 Importantly, delay times were significantly shorter for both women and men who experienced abrupt symptom onset. Finally, physical exertion was a significant symptom trigger.
There have been contradictory findings for differences in prehospital delay time between women and men. Some studies concluded that women had longer prehospital delay times,38 whereas other studies found that there was no difference between women and men.39 Bruins Slot et al. found that overall prehospital delay was similar in women and men suspected of ACS.2 Nguyen et al., in a systematic review of the literature from 1960–2008, found that in the majority of studies, which included patients hospitalized with acute myocardial infarction (AMI), women were more likely to arrive at the hospital later than men.19 However, the authors included only patients with AMI; in the present study, we also included patients with UA. We also found that patients with STEMI (a true emergency) had shorter prehospital delay times. These patients require emergency reperfusion, and most fell outside the time for optimum intervention.40
Our study revealed that patients with gradual symptom onset experienced a greater delay time compared to patients with abrupt symptom onset (8 h vs 2.57 h, p<0.001). Our finding is consistent with previous investigations. Prior studies demonstrated that patients who had abrupt and intense symptoms, which are almost immediately recognizable as a potential heart attack, go to the hospital quickly.15 Mild, diffuse, or vague symptoms that begin gradually are associated with prolonged prehospital delay because patients often attribute their symptoms to non-cardiac causes.41 Consistent with prior investigations, we found patients who were not insured had prolonged prehospital delay times compared to patients with private and government insurance. Prior studies indicated that lack of health insurance was associated with delays in seeking emergency care for AMI.42 O’Donnell et al.43 found that patients with private insurance were more likely to experience a shorter prehospital delay.
Patients with a STEMI diagnosis and patients who arrived to the ED by ambulance experienced shorter prehospital delay times. Perkins-Porras and colleagues also showed that patients who had STEMI rather than NSTEMI or UA were more likely to experience shorter prehospital delay times.44 Similar to our findings, previous studies found that initial contact with EMS reduces prehospital delay time.44,45 Unfortunately, only 44.6% of patients in our study called EMS. In addition, EMS transport was used by only 56.3% of STEMI patients. Similar to our study, Mathews et al.46 found that patients transported by EMS with STEMI had significantly shorter delays in symptom-onset to arrival time (median 89 min vs 120 min; p<0.0001), compared with self-transported patients. Sixty percent of STEMI patients in the Mathews et al. study used an ambulance.46
Finally, physical exertion was the only activity related to symptom onset in patients with ACS, and patients with STEMI were more likely to experience abrupt symptom onset with exertion compared to patients with UA and NSTEMI. Similarly, results from prior studies showed that physical exertion was associated with higher risk of myocardial infarction (MI).47 Buckley et al. found that patients with exertion-triggered MI were at higher risk of presenting with an occluded than a non-occluded artery on hospital admission.48 We also found that more men than women with STEMI in our sample had symptoms following physical exertion. This finding is consistent with a recent study that men were more likely to experience coronary occlusion with heavy exertion than were women (17% vs 5%). Exertion is known to be associated with rupture of vulnerable atherosclerotic plaques.48 Our multi-center and heterogeneous sample of the patients allows for generalization of our findings to other cohorts of the American population.
Limitations
This study had limitations. Patients were asked, “When did symptoms responsible for this admission start?” Some patients could not recall accurately when their symptoms began and thus prehospital delay was abstracted from the medical record. Also, admission to the ED for ACS is stressful and makes recall arduous. Exertion-related cardiac events have been defined as symptoms that begin within 1 hour of physical exertion.49 However, there is no general agreement regarding how long before symptom onset an activity can be regarded as a trigger.50 Patients in our study were queried about whether they had single or multiple symptoms in the 48 h prior to admission.
Conclusion
Prehospital delay for symptoms of potential ACS remains excessive for women and men despite the identification of barriers to treatment, such as being insured or gradual onset of symptoms. Patients should be counseled that a gradual, as well as abrupt, onset of symptoms for potential ACS is an emergency and they should call 911. Men with ischemic heart disease or with multiple risk factors should be cautioned that symptom onset following exertion may represent ACS. Patients should be cautioned that a gradual onset of symptoms may signify ACS and that they should seek immediate care.
Implications for practice.
At-risk individual’s and emergency department clinicians should be aware that abrupt onset of symptoms is associated with ST-elevation myocardial infarction and requires emergent reperfusion to preserve myocardium.
Patients should be counselled that a gradual onset of symptoms for potential acute coronary syndrome (ACS) is an emergency and they should call 911.
Men with ischemic heart disease or with multiple risk factors should be cautioned that the symptom onset following exertion may represent ACS.
Prehospital delay for symptoms of potential ACS remains excessive for women and men and is associated with lack of insurance and gradual onset of symptoms.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by a grant to HA DeVon from NINR (National Institute of Nursing Research) (R01NR012012).
Footnotes
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1.Moser DK, Kimble LP, Alberts MJ, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: A scientific statement from the American Heart Association Council on cardiovascular nursing and stroke council. Circulation 2006; 114: 168–182. [DOI] [PubMed] [Google Scholar]
- 2.Bruins Slot MH, Rutten FH, van der Heijden GJ, et al. Gender differences in pre-hospital time delay and symptom presentation in patients suspected of acute coronary syndrome in primary care. Fam Pract 2012; 29: 332–337. [DOI] [PubMed] [Google Scholar]
- 3.McKee G, Mooney M, O’Donnell S, et al. Multivariate analysis of predictors of pre-hospital delay in acute coronary syndrome. Int J Cardiol 2013; 168: 2706–2713. [DOI] [PubMed] [Google Scholar]
- 4.Isaksson RM, Holmgren L, Lundblad D, et al. Time trends in symptoms and prehospital delay time in women vs. men with myocardial infarction over a 15-year period. The Northern Sweden MONICA Study. Eur J Cardiovasc Nurs 2008; 7: 152–158. [DOI] [PubMed] [Google Scholar]
- 5.Ottesen MM, Dixen U, Torp-Pedersen C, et al. Prehospital delay in acute coronary syndrome–an analysis of the components of delay. Int J Cardiol 2004; 96: 97–103. [DOI] [PubMed] [Google Scholar]
- 6.Mooney M, McKee G, Fealy G, et al. A randomized controlled trial to reduce prehospital delay time in patients with acute coronary syndrome (ACS). J Emerg Med 2014; 46: 495–506. [DOI] [PubMed] [Google Scholar]
- 7.Terkelsen CJ, Sorensen JT, Maeng M, et al. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA 2010; 304: 763–771. [DOI] [PubMed] [Google Scholar]
- 8.Wah W, Pek PP, Ho AF, et al. Symptom-to-door delay among patients with ST-segment elevation myocardial infarction in Singapore. Emerg Med Australas 2017; 29: 24–32. [DOI] [PubMed] [Google Scholar]
- 9.Rathore SS, Curtis JP, Chen J, et al. Association of door-to-balloon time and mortality in patients admitted to hospital with ST elevation myocardial infarction: National cohort study. BMJ 2009; 338: b1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gersh BJ and Stone GW. Pharmacological facilitation of coronary intervention in ST-segment elevation myocardial infarction: Time is of the essence. JACC Cardiovasc Interv 2010; 3: 1292–1294. [DOI] [PubMed] [Google Scholar]
- 11.Nakashima T and Tahara Y. Achieving the earliest possible reperfusion in patients with acute coronary syndrome: A current overview. J Intensive Care 2018; 6: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Basit H, Malik A, Huecker MR. Non ST Segment Elevation (NSTEMI) Myocardial Infarction [Updated 2019 May 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 January. Available from: https://europepmc.org/books/NBK513228. [Google Scholar]
- 13.Menees DS, Peterson ED, Wang Y, et al. Door-to-balloon time and mortality among patients undergoing primary PCI. N Engl J Med 2013; 369: 901–909. [DOI] [PubMed] [Google Scholar]
- 14.Goldberg RJ, Steg PG, Sadiq I, et al. Extent of, and factors associated with, delay to hospital presentation in patients with acute coronary disease (the GRACE registry). Am J Cardiol 2002; 89: 791–796. [DOI] [PubMed] [Google Scholar]
- 15.O’Donnell S, McKee G, Mooney M, et al. Slow-onset and fast-onset symptom presentations in acute coronary syndrome (ACS): New perspectives on prehospital delay in patients with ACS. J Emerg Med 2014; 46: 507–515. [DOI] [PubMed] [Google Scholar]
- 16.Thuresson M, Jarlov MB, Lindahl B, et al. Symptoms and type of symptom onset in acute coronary syndrome in relation to ST elevation, sex, age, and a history of diabetes. Am Heart J 2005; 150: 234–242. [DOI] [PubMed] [Google Scholar]
- 17.Moser DK, Kimble LP, Alberts MJ, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: A scientific statement from the American Heart Association Council on Cardiovascular Nursing and Stroke Council. J Cardiovasc Nurs 2007; 22: 326–343. [DOI] [PubMed] [Google Scholar]
- 18.Rosenfeld AG. Treatment-seeking delay among women with acute myocardial infarction: Decision trajectories and their predictors. Nurs Res 2004; 53: 225–236. [DOI] [PubMed] [Google Scholar]
- 19.Nguyen HL, Saczynski JS, Gore JM, et al. Age and sex differences in duration of prehospital delay in patients with acute myocardial infarction: A systematic review. Circ Cardiovasc Qual Outcomes 2010; 3: 82–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lawesson SS, Isaksson RM, Ericsson M, Ängerud K, Thylén I. Gender disparities in first medical contact and delay in ST-elevation myocardial infarction: a prospective multicentre Swedish survey study. BMJ Open 2018; 8: e020211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim HS, Lee KS, Eun SJ, et al. Gender differences in factors related to prehospital delay in patients with ST-segment elevation myocardial infarction. Yonsei Med J 2017; 58: 710–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grace SL, Abbey SE, Bisaillon S, et al. Presentation, delay, and contraindication to thrombolytic treatment in females and males with myocardial infarction. Womens Health Issues 2003; 13: 214–221. [DOI] [PubMed] [Google Scholar]
- 23.Lovlien M, Schei B and Hole T. Prehospital delay, contributing aspects and responses to symptoms among Norwegian women and men with first time acute myocardial infarction. Eur J Cardiovasc Nurs 2007; 6: 308–313. [DOI] [PubMed] [Google Scholar]
- 24.Moller J, Hallqvist J, Diderichsen F, et al. Do episodes of anger trigger myocardial infarction? A case-crossover analysis in the Stockholm Heart Epidemiology Program (SHEEP). Psychosom Med 1999; 61: 842–849. [DOI] [PubMed] [Google Scholar]
- 25.Strike PC and Steptoe A. Behavioral and emotional triggers of acute coronary syndromes: A systematic review and critique. Psychosom Med 2005; 67: 179–186. [DOI] [PubMed] [Google Scholar]
- 26.Selvi Y, Aydin A, Gumrukcuoglu HA, et al. Dream anxiety is an emotional trigger for acute myocardial infarction. Psychosomatics 2011; 52: 544–549. [DOI] [PubMed] [Google Scholar]
- 27.Stewart RA, Robertson MC, Wilkins GT, et al. Association between activity at onset of symptoms and outcome of acute myocardial infarction. J Am Coll Cardiol 1997; 29: 250–253. [DOI] [PubMed] [Google Scholar]
- 28.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics–2015 update: A report from the American Heart Association. Circulation 2015; 131: e29–322. [DOI] [PubMed] [Google Scholar]
- 29.Nielsen CG, Laut KG, Jensen LO, et al. Patient delay in patients with ST-elevation myocardial infarction: Time patterns and predictors for a prolonged delay. Eur Heart J Acute Cardiovasc Care 2017; 6: 583–591. [DOI] [PubMed] [Google Scholar]
- 30.Tummala SR and Farshid A. Patients’ understanding of their heart attack and the impact of exposure to a media campaign on pre-hospital time. Heart Lung Circ 2015; 24: 4–10. [DOI] [PubMed] [Google Scholar]
- 31.Hwang SY, Park EH, Shin ES, et al. Comparison of factors associated with atypical symptoms in younger and older patients with acute coronary syndromes. J Korean Med Sci 2009; 24: 789–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.DeVon HA, Vuckovic K, Burke LA, et al. What’s the risk? Older women report fewer symptoms for suspected acute coronary syndrome than younger women. Biores Open Access 2018; 7: 131–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Devon HA, Rosenfeld A, Steffen AD, et al. Sensitivity, specificity, and sex differences in symptoms reported on the 13-item acute coronary syndrome checklist. J Am Heart Assoc 2014; 3: e000586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hollander JE, Blomkalns AL, Brogan GX, et al. Standardized reporting guidelines for studies evaluating risk stratification of ED patients with potential acute coronary syndromes. Acad Emerg Med 2004; 11: 1331–1340. [DOI] [PubMed] [Google Scholar]
- 35.Chen T, Xu M, Tu J, et al. Relationship between omnibus and post-hoc tests: An investigation of performance of the F test in ANOVA. Shanghai Arch Psychiatry 2018; 30: 60–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013; 61: 485–510. [DOI] [PubMed] [Google Scholar]
- 37.Goldberg RJ, Spencer FA, Fox KA, et al. Prehospital delay in patients with acute coronary syndromes (from the Global Registry of Acute Coronary Events (GRACE)). Am J Cardiol 2009; 103: 598–603. [DOI] [PubMed] [Google Scholar]
- 38.Rivero F, Bastante T, Cuesta J, et al. Factors associated with delays in seeking medical attention in patients With ST-segment elevation acute coronary syndrome. Rev Esp Cardiol (Engl Ed) 2016; 69: 279–285. [DOI] [PubMed] [Google Scholar]
- 39.Farshidi H, Rahimi S, Abdi A, et al. Factors associated with pre-hospital delay in patients with acute myocardial infarction. Iran Red Crescent Med J 2013; 15: 312–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Van de Werf F, Bax J, Betriu A, et al. Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: The Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J 2008; 29: 2909–2945. [DOI] [PubMed] [Google Scholar]
- 41.Noureddine S, Arevian M, Adra M, et al. Response to signs and symptoms of acute coronary syndrome: Differences between Lebanese men and women. Am J Crit Care 2008; 17: 26–35. [PubMed] [Google Scholar]
- 42.Smolderen KG, Spertus JA, Nallamothu BK, et al. Health care insurance, financial concerns in accessing care, and delays to hospital presentation in acute myocardial infarction. JAMA 2010; 303: 1392–1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.O’Donnell S, Condell S, Begley C, et al. Prehospital care pathway delays: Gender and myocardial infarction. J Adv Nurs 2006; 53: 268–276. [DOI] [PubMed] [Google Scholar]
- 44.Perkins-PorraL, WhiteheaL, StrikC, et al. Pre-hospital delay in patients with acute coronary syndrome: Factors associated with patient decision time and home-to-hospital delay. Eur J Cardiovasc Nurs 2009; 8: 26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Johansson I, Stromberg A and Swahn E. Factors related to delay times in patients with suspected acute myocardial infarction. Heart Lung 2004; 33: 291–300. [DOI] [PubMed] [Google Scholar]
- 46.Mathews R, Peterson ED, Li S, et al. Use of emergency medical service transport among patients with ST-segment-elevation myocardial infarction: Findings from the National Cardiovascular Data Registry Acute Coronary Treatment Intervention Outcomes Network Registry–Get With The Guidelines. Circulation 2011; 124: 154–163. [DOI] [PubMed] [Google Scholar]
- 47.Lohsoonthorn V, Rattananupong T, Wynne K, et al. Immediate risk of myocardial infarction following physical exertion, tea, and coffee: A case-crossover study in Thailand. PLoS One 2019; 14: e0210959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Buckley T, Soo Hoo SY, Shaw E, et al. Triggering of acute coronary occlusion by episodes of vigorous physical exertion. Heart Lung Circ 2018. [DOI] [PubMed] [Google Scholar]
- 49.Rai M and Thompson PD. The definition of exertion-related cardiac events. Br J Sports Med 2011; 45: 130–131. [DOI] [PubMed] [Google Scholar]
- 50.Krantz DS and McCeney MK. Effects of psychological and social factors on organic disease: A critical assessment of research on coronary heart disease. Annu Rev Psychol 2002; 53: 341–369. [DOI] [PubMed] [Google Scholar]