Abstract
Objective
To estimate the hospital costs of managing anterior epistaxis in the Emergency Department at a Tertiary Care centre in Canada.
Material and methods
A cost analysis was conducted based on a retrospective review of Emergency Department visits from January 2012 to May 2014. A consecutive sample of adult patients with a diagnosis of anterior epistaxis was included. Anterior epistaxis was managed via one of: Nasal clip, Merocel®, Silver Nitrate cautery, Vaseline packing, other treatment or no treatment. Both the direct and indirect hospital costs ($CDN) for anterior epistaxis treatment were calculated from the hospital's perspective. Generalized linear models were used to assess the association between treatment modalities and total hospital costs while controlling for potential confounding factors.
Results
Three hundred and fifty-three patients (49% female) with a mean age of (69.9 ± 18.5) years were included in the analysis. The median (interquartile ranges) costs of treatment ranged from C$227.83 (C$167.96, C$328.69) for observation to C$763.98 (C$632.25,C$830.23) for Merocel®. The overall median total hospital costs incurred across all modalities was C$566.24 (C$459.61, C$753.46) for the management of anterior epistaxis. Silver Nitrate, nasal clip, and observation were statistically associated with a lower cost when compared to Merocel® (P < 0.001) even after potential confounding factors were controlled.
Conclusions
Our results show wide difference in the hospital cost of epistaxis across treatment modalities. These cost estimates can help inform future economic evaluation studies aiming to guide the allocation of health care resources for patients with epistaxis.
Keywords: Anterior epistaxis, Nasal packing, Cautery, Silver nitrate, Hospital costs
Introduction
Epistaxis is a common clinical problem often encountered in the emergency department.1 It is estimated that up to 60% of the general population will experience an episode of epistaxis during their lifetime, but only 6%–10% of affected patients will require specialized treatment.2,3 The majority of epistaxis episodes occur anteriorly, originating from Kiesselbach's plexus of the nasal septum, often referred to as Little's area or that portion of the anterior septum demarcated by the anterior limit of the inferior turbinate.4 Individuals under 10 years of age and over the age of 40 years are the most commonly affected age groups.5
The treatment approach to anterior epistaxis often begins with local pressure, followed by more invasive procedures if that fails.6 These other procedures include chemical cautery,7 anterior packing as well as other hemostatic substances.8,9 Unfortunately, the literature is deplete for the assessment of efficacy of these treatment modalities in the emergency department (ED), and currently treatment selection is largely based on ED physician preference.10 Previous studies have compared the clinical outcomes of the anterior epistaxis management options. Newton et al10 found that the management of anterior epistaxis is quite variable in the ED with silver nitrate cautery, Merocel®, petroleum gauze packing, nasal clip and observation being the most common treatment modalities. This study found that the success rate of treatment was highest among patients who received silver nitrate cautery; however the authors raised epistaxis severity to be a possible confounding factor.10 Recently, Farneti et al11 completed a retrospective cohort study and found a new treatment using submucosal infiltrations of lauromacrogol to provide an improved success rate as well as a reduction of bleeding recurrence, morbidity and costs compared to nasal packing.
Epistaxis accounts for 450,000 emergency department (ED) visits each year in the United States, representing 0.46% of all ED visits,3 and presentation to the ED has been associated with patients' socioeconomic status.12 Given this reported complaint frequency and the high incidence in the general population, it is critical to understand the economic burdens of managing epistaxis. Such information is critical as it can be used to inform effective epistaxis care, and it may aid clinicians and health policy-makers to identify epistaxis management practices that are both effective and economical. Few studies have reported the costs of providing treatment for patients who present to hospital due to epistaxis. Goddard and Reiter13 found that the costs of inpatient management of epistaxis ranged from $6282 to $7616 (USD) in 2000, depending on the type of treatment. More recently, Goljo et al14 conducted a retrospective cross-sectional study of 16,828 in patients with an admitting diagnosis of epistaxis and reported an average hospital cost of $6925 (USD). Hospital costs reported in these US studies may not be generalizable to other countries with different health care systems; especially those with a publicly funded health care system. Moreover, they represent the costs of care for inpatient or hospitalized patients with epistaxis. As anterior epistaxis management occurs primarily in the ED, the costs of outpatient management are expected to differ greatly from inpatient hospital care. Therefore, the purpose of this study was to estimate the total hospital costs of the commonly utilized management strategies for anterior epistaxis at a tertiary care hospital emergency department in Canada.
Materials and methods
We conducted a cost analysis based on a retrospective cohort study of all patient visits to the emergency department at The Ottawa Hospital (TOH), a Canadian tertiary care center, with a primary diagnosis of anterior epistaxis during the period of January 2012 to May 2014. Participant selection criteria and results of treatment outcomes have been reported elsewhere.10 Anterior epistaxis was identified using the ICD-10-CA (International Statistical Classification of Diseases and Related Health Problems, 10th revision, Canada): R04.0.15
Patient demographics, comorbidities, the applied treatment modality, course in the emergency department, admission, concurrent medical disorders, medications and finally recurrence and/or ED follow-up information were recorded for each patient included in the study. Treatment modalities utilised at the academic center that were identified for data abstraction included nasal clip, Merocel® packing, conservative (no treatment), “other”, silver nitrate cautery, and petroleum gauze packing (Vaseline). The “other” group included patients treated with Surgicel®/Surgifoam®, cotton pledgets with decongestant, topical lidocaine/epinephrine, topical tranexamic acid, or a similar intervention, and did not require any additional treatment. These treatments were classified as “other” as individually there were few of these individual treatments.
Only primary single modality treated anterior epistaxis cases were included. Follow-up was defined as patients who were administered a specific treatment and who were subsequently booked and received follow-up care in the ED for either packing removal, to check the site of epistaxis, or for any other reason. Recurrence was defined as return of the participant to the ED within 14 days of their original epistaxis presentation, with the epistaxis occurring on the same side of the nose as the initial presentation. Fourteen days has been recently used in an epistaxis trial as the timeframe for epistaxis recurrence following treatment.16
The outcome of interest was total hospital costs which was the sum of all costs that borne to the hospital, including treatment cost as well as direct and indirect hospital costs, over the 30-day period after the diagnosis of anterior epistaxis. We measured the propensity and frequency of health care utilization that occurred in the hospital including emergency department visits from the Ottawa Hospital Data Warehouse for each patient during the study period. We estimated overall costing from direct and indirect hospital cost for each inpatient encounter within the case-costing system of the Ottawa Hospital Data Warehouse. The case-costing system links financial, clinical and patient activity information stored within information systems of the Data Warehouse to define intermediate products, such as nursing time, medications, and laboratory tests. The total hospital costs were equal to the sum of the direct and indirect costs for each intermediate product used during an encounter for each patient. The system is based on a standardized case-costing methodology developed by the Ontario Case Costing Initiative and the Canadian Institute for Health Information Management Information Systems guidelines.17,18 For patients who had multiple hospital encounters for recurrence(s) within the follow-up period, their total costs were equal to the sum of hospital costs incurred during each encounter. Key unit costs are shown in Table 1. All costs are expressed in 2017 Canadian Dollars.
Table 1.
Key input parameters used for a cost analysis.
| Variables | Unit Cost (C$) | Source |
|---|---|---|
| Nasal clip | 0.58 | TOH Finance Department |
| Silver Nitrate | 11.82 | TOH Finance Department |
| Merocel® | 25.35 | TOH Finance Department |
| Vaseline packing | 17.38 | TOH Finance Department |
| Hospitalization cost per visit (inclusive of direct and indirect hospital costs), mean (SD) | 259.79 (115.11) | TOH Data Warehouse |
Univariate and bivariate analyses were performed. As cost data are highly skewed, median values and interquartile ranges were reported. Hospital costs were also categorized as initial costs incurred during the index visit (inclusive of treatment and hospital costs) and subsequent costs that included removing and follow-up visit costs. We used multiple regression analysis to compare the difference in hospital costs across the treatment modalities while controlling for potential confounding factors. The selection of controlled variables was guided by previous cost studies and subject to its availability in our dataset. To identify the regression model that best fits the cost data, we followed the steps suggested by Manning and Mullahy.18 We first ran ordinary least squares (OLS) of the logarithmic transformation of cost data on treatment modalities and other confounding factors; however, the OLS regression was deemed inappropriate because the residuals were not normally distributed. Therefore, the generalised linear model (GLM) with a log-link function and identity distribution was chosen.
A P-value less than 0.05 was considered statistically significant. All statistical analyses were performed using SAS software, Version 9.4 (SAS Institute Inc. Cary, NC, USA).
Results
A total of 353 patients were included in this study. The mean age of all patients in this study was 69.9 (SD = 18.5) years. A summary of patient characteristics is presented in Table 2.
Table 2.
Characteristics of study cohort.
| Item | Nasal clip | Merocel® | No treatment | Other Treatment | Silver Nitrate | Vaseline | Total |
|---|---|---|---|---|---|---|---|
| N | 17 | 81 | 52 | 21 | 152 | 30 | 353 |
| Mean age (SD), years | 72.3 (16.5) | 71.4 (14.8) | 69.2 (17.2) | 69.3 (17.2) | 70.3 (19.4) | 63.9 (21.4) | 69.9 (18.5) |
| Sex, % | |||||||
| Male | 58.8 | 51.9 | 42.3 | 57.7 | 51.3 | 63.3 | 51.0 |
| Female | 41.2 | 48.1 | 57.7 | 42.3 | 48.7 | 36.7 | 49.0 |
| Type of visit, % | |||||||
| Initial | 94.1 | 90.1 | 100.0 | 90.5 | 88.2 | 80.0 | 90.1 |
| Recurrent | 5.9 | 9.9 | 0.0 | 9.6 | 11.8 | 20.0 | 9.9 |
| Side | |||||||
| Right | 29.4 | 37.0 | 21.2 | 47.6 | 48.0 | 43.3 | 40.3 |
| Left | 35.3 | 44.4 | 34.6 | 28.6 | 41.5 | 40.0 | 39.9 |
| Bilateral | 23.5 | 17.2 | 11.5 | 19.1 | 9.2 | 16.7 | 13.3 |
| Unknown | NA | NA | 32.7 | NA | NA | NA | 6.5 |
| Presence of medical illness, % | |||||||
| Have at least 1 condition | 82.3 | 83.9 | 63.5 | 66.7 | 64.5 | 73.3 | 70.5 |
| No medical illness | 17.7 | 16.1 | 36.5 | 33.3 | 35.5 | 26.7 | 29.5 |
| Concurrent anticoagulant/antiplatelet medications, % | |||||||
| Have at least 1 concomitant medication | 82.4 | 71.6 | 51.9 | 47.6 | 58.3 | 64.5 | 61.5 |
| No medication | 17.6 | 28.4 | 48.1 | 52.4 | 41.7 | 35.5 | 38.5 |
Note: NA, not available: statistics with cell sizes < 5 were not reported.
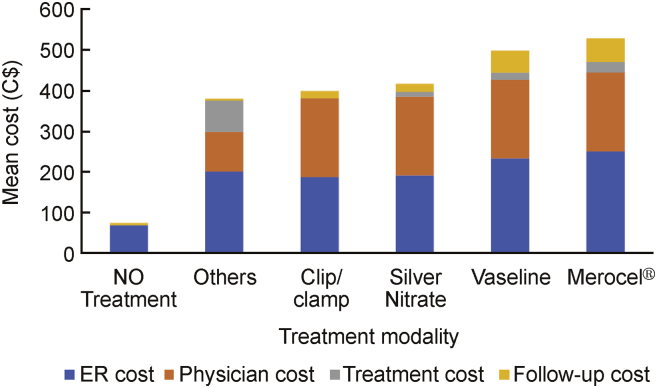
The major comorbidities noted in this analysis included hypertension (56.1%), atrial fibrillation (26.6%), no medical comorbidities (29.5%) and diabetes (19.0%), respectively. The total hospital cost incurred by our cohort was C$155,871.65. Fig. 1 shows the total mean hospital costs by the type of costs for each treatment modality. Initial hospital costs accounted for the largest component of costs for “No treatment” and “Other” treatment modalities. On the contrary, the subsequent costs were the largest component for nasal clip/clamp, Silver Nitrate cautery, Vaseline gauze packing, and Merocel®. The overall median and mean total hospital costs incurred across all modalities for the management of anterior epistaxis were C$566.24 (C$459.61, C$753.46) and C$599.51 (C$459.61, 753.46), respectively. Merocel® packing treatment incurred the highest hospital cost (median = C$763.98, (C$632.25, C$830.230)), followed by Vaseline gauze packing (median = C$723.12 (C$658.94, C$810.54)) and Silver Nitrate cautery (median = C$521.96 (C$458.52, C$656.94)) treatment, respectively. The median hospital costs of nasal clips, “other”, and “No Treatment,” are outlined in Table 3.
Fig. 1.
Distribution of unadjusted mean ER hospital costs by treatment modalities and type of costs.
Table 3.
Median costs and interquartile ranges (Q1,Q3) by patient characteristics and treatment modality.
| Item | Nasal clip | Merocel® | No treatment | Others | Silver Nitrate | Vaseline | Total | P-value |
|---|---|---|---|---|---|---|---|---|
| N | 17 | 85 | 52 | 21 | 152 | 30 | 353 | |
| All sample | 510.66 (477.44, 688.51) | 763.98 (632.25, 830.23) | 227.83 (167.96, 328.69) | 303.23 (257.41, 357.80) | 521.96 (458.52, 656.94) | 723.12 (658.94, 810.54) | 566.24 (459.61, 753.46) | <0.0001 |
| Sex | 0.2026 | |||||||
| Male | 512.99 (477.44, 760.97) | 785.82 (688.49, 852.90) | 227.83 (200.14, 259.90) | 337.71 (265.71, 492.79) | 526.35 (457.67, 690.13) | 723.12 (670.72, 912.04) | 614.13 (483.99, 788.66) | |
| Female | 494.05 (469.03, 531.62) | 743.07 (579.56, 796.50) | 240.31 (158.70, 376.13) | 267.53 (257.41, 330.57) | 490.66 (459.37, 654.78) | 723.12 (653.25, 772.18) | 531.62 (457.67, 723.12) | |
| Side | 0.9017 | |||||||
| Right | 688.51 (512.99, 707.92) | 751.09 (664.34, 854.92) | 175.00 (175.00, 294.22) | 303.23 (257.41, 357.80) | 508.56 (457.67, 654.78) | 702.55 (670.72, 733.81) | 582.82 (457.67, 726.26) | |
| Left | 477.44 (469.03, 510.66) | 764.93 (579.75, 804.69) | 256.94 (156.47, 292.86) | 336.00 (250.36, 441.22) | 524.20 (473.46, 722.68) | 723.12 (658.94, 787.46) | 566.26 (474.44, 760.97) | |
| Bilateral | 521.14 (482.07, 680.22) | 813.88 (544.89, 846.07) | 275.46 (174.34, 475.39) | 301.71 (261.56, 337.71) | 480.99 (451.07, 557.74) | 912.04 (647.55, 951.05) | 528.97 (450.28, 828.82) | |
| Presence of medical illness, % | 0.0001 | |||||||
| Have at least 1 condition | 510.66 (477.44, 707.92) | 761.83 (583.02, 818.64) | 288.87 (175.00, 389.09) | 337.70 (257.41, 407.99) | 559.76 (486.34, 705.31) | 726.90 (692.11, 826.56) | 601.65 (488.68, 776.95) | |
| No medical illness | 492.55 (453.47, 531.62) | 797.52 (731.82, 835.10) | 181.38 (160.92, 225.28) | 264.86 (257.41, 271.05) | 483.07 (435.64, 545.25) | 664.83 (595.58, 674.90) | 490.66 (415.78, 670.72) | |
| Concurrent anticoagulant/antiplatelet medications | 0.0043 | |||||||
| Have at least 1 concomitant medication | 510.66 (477.44, 688.51) | 762.78 (586.28, 830.23) | 256.94 (167.96, 328.69) | 337.70 (271.05, 407.99) | 528.86 (483.99, 642.41) | 725.01 (683.51, 869.30) | 586.95 (483.07, 760.33) | |
| No medication | NA | 763.98 (731.82, 846.07) | 181.38 (165.74, 288.43) | 260.71 (247.05, 264.86) | 472.85 (420.56, 568.51) | 658.94 (595.58, 670.72) | 480.49 (410.57, 718.27) | |
Note: NA, not available: statistics with cell sizes < 5 were not reported.
Table 3 shows the variation in unadjusted total hospital costs across treatment modalities and patient characteristics. Total hospital costs of epistaxis were statistically higher in patients who had at least one comorbidity (P < 0.001) or those received at least one concurrent anticoagulation/antiplatelet medication (P < 0.01).
Table 4 outlines the results of the generalized linear model, which suggested that compared to Merocel® packing, receiving silver nitrate (coefficient = −0.2391, P < 0.0001), nasal clip/clamp (coefficient = −0.2748, P < 0.0001), no treatment (coefficient = −0.9752, P < 0.0001), and “other” packing (coefficient = −0.7523, P < 0.0001) were significantly associated with lower total hospital costs even after controlling for potential confounders.
Table 4.
Results of the generalized linear model with log-link and identity distribution.
| Item | Parameter | Co-efficient | Standard error | 95% Confidence interval (CI) | Z-value | Pr>|Z| | |
|---|---|---|---|---|---|---|---|
| Intercept | 6.4430 | 0.0640 | 6.3176 | 6.5683 | 100.74 | <0.0001 | |
| Treatment modality | Nasal clip | −0.2748 | 0.0650 | −0.4023 | −0.1474 | −4.23 | <0.0001 |
| No treatment | −0.9752 | 0.1351 | −1.2401 | −0.7104 | −7.22 | <0.0001 | |
| Other treatment | −0.7523 | 0.0907 | −0.9301 | −0.5745 | −8.29 | <0.0001 | |
| Silver nitrate | −0.2391 | 0.0373 | −0.3123 | −0.1659 | −6.40 | <0.0001 | |
| Vaseline | 0.0062 | 0.0505 | −0.0929 | 0.1053 | 0.12 | 0.9024 | |
| Merocel® | Reference | ||||||
| Gender | Male | 0.0564 | 0.0309 | −0.0041 | 0.1169 | 1.83 | 0.0675 |
| Female | Reference | ||||||
| Co-morbid condition | At least 1 condition | 0.0527 | 0.0410 | −0.0276 | 0.1331 | 1.29 | 0.1981 |
| No condition | Reference | ||||||
| Age | 0.0010 | 0.0010 | −0.0009 | 0.0029 | 1.06 | 0.2907 | |
| Concomitant medication | At least 1 medication | 0.0272 | 0.0444 | −0.0599 | 0.1143 | 0.61 | 0.5405 |
| No medication | Reference | ||||||
| Type of epistaxis | Recurrent | −0.0694 | 0.0486 | −0.1647 | 0.0259 | −1.43 | 0.1533 |
| Initial | Reference | ||||||
| Quasi-Akaike information criterion | 268.61 | ||||||
Discussion
The purpose of this study was to delineate the total hospital costs of managing anterior epistaxis at a Canadian emergency department, and to determine whether differences in treatment costs to the healthcare system vary based on the choice of treatment modality. Our analysis found that the median total cost of managing anterior epistaxis in our sample of 353 patients was C$566.24 (C$459.61, C$753.46) but ranged from C$227.83 (C$167.96, C$328.69) for patients not receiving a specific treatment to C$763.98 (C$632.25, C$830.23) for patients treated with Merocel® packing. The reported cost of anterior epistaxis management in our study is substantially lower than the reported costs from Goljo et al,14 who reported an average cost of $6925 USD per patient in their retrospective cross-sectional study of inpatients admitted for epistaxis management. The higher costs in their study were associated with patients receiving surgical interventions, a greater number of procedures, and possibly with the use of private insurance in some patients.
In the present study, many factors influenced the total cost of care for anterior epistaxis including the selected treatment modality, the duration of a patient's stay in the ED and the need for a follow-up assessment, or repeated treatment. For instance, no active treatment still requires a stay in the ED and incurs a cost to the hospital. No treatment may have been considered by the treating emergency physician due to the limited or low severity of epistaxis or because of the spontaneous resolution of bleeding prior to ED assessment. Yet these patients are often observed for potential recurrence and the need for intervention. It is possible that this group may also represent patients who do not need assessment at a hospital but are unaware of basic measures for epistaxis treatment.
The use of Merocel® and Vaseline packing incurred substantial hospital costs, with their higher failure rates, 26% and 59% respectively, impacting the need for additional clinical treatment.10 Furthermore, follow-up in the ED contributes greatly to the overall cost of a treatment modality. For instance, the hospital cost associated with a Merocel® is higher than any other treatment modality because it has high material costs and the pack must be removed necessitating follow-up and potentially, further treatment. Despite the slightly higher recurrence rate that occurred in the cohort with silver nitrate treatment, the cost of this treatment approach is significantly lower than treatment with a Merocel® pack. The success rates of each treatment modality in this population has been reported elsewhere.10 However, it is unclear from this data if patients who receive a nasal pack differ in the severity of epistaxis from patients receiving other treatment modalities, as this could not be assessed with the current study design. Further, it remains to be determined if the severity of anterior epistaxis impacts both treatment modality selection and success.10 Given the greater frequency of patients treated with silver nitrate in this study, it is possible that physicians at this center are already considering cost when treating these patients, or potentially, this represents an unrealized clinician treatment bias.
Goljo et al14 outlined various factors associated with higher costs of epistaxis management which included comorbid alcohol abuse, sinonasal disease, patients with private insurance and patient treatment at large hospitals. Similar to their study, our study did also find that hospital cost for anterior epistaxis treatment was higher for all treatment modalities when the patient had one or more comorbid illnesses although the association was statistically insignificant after controlling confounders. Importantly, the variability of anterior epistaxis management between hospitals in Canada has not been investigated to date making it difficult to comment on hospital size and cost for anterior epistaxis management.
Our group recently reported the outcomes of anterior epistaxis management in the emergency department.10 The treatment modality with the greatest success rate was silver nitrate cautery at 80%. Treatment groups with the highest rates of epistaxis recurrence were nasal clip, Merocel®, and petroleum gauze packing. Notably, as mentioned, the added benefit of silver nitrate cautery is that there is no need for follow-up to remove any material from the nose.10 In conjunction with the results of the present study, it appears that the use of silver nitrate cautery should be encouraged as a first treatment modality for anterior epistaxis given its lower cost and its superior success rate. The use of this treatment modality is highly successful when the source of bleeding is identifiable.7,19 However, it is as of yet unknown whether bleeding severity has any influence on treatment modality selection and success.
There are limitations to this study including the limited sample size for some treatment groups as well as the possibility of bleeding severity being a confounding factor in the analysis of the treatment modality success for anterior epistaxis treatment. Small sample size also limited the number of independent variables in our multivariate analysis. Further, it is difficult to ascertain using the retrospective methodology the clinical reasoning utilised for the selection of a treatment modality for each patient as they may have been administered based upon physician preference or experience, bleeding severity, bleeding site visualization, or other case or physician specific factors. Each of these factors may confound the association between treatment modality and total hospital costs.
Conclusion
In conclusion, we report on total hospital costs for treating anterior epistaxis at a single Canadian center. The results support the use of silver nitrate cautery when dealing with a visible bleeding site given its success rate reported in a previous study and lower associated hospital costs compared to the other treatment modalities.10 Future studies should evaluate the influence of bleeding severity on choice of treatment modality and success of the modality, and the cost-effectiveness of silver nitrate cautery against other treatment modalities. We believe that treating physicians may be better able to choose appropriate treatment modalities for the management of anterior epistaxis based on treatment success and cost.
Ethical approval
Ethics approval for this study was obtained from the Ottawa Health Sciences Network Research Ethics Board.
Consent for publication
Not applicable.
Funding
No funding.
Authors' contributions
SK: Study design, data interpretation, manuscript preparation.
KM: Data interpretation, manuscript preparation.
AL: Data collection, data analysis.
KT: Design the cost analysis study, data analysis, interpretation of study results and manuscript preparation.
FB: Manuscript preparation.
HN: Data interpretation and manuscript preparation.
All authors read and approved the final manuscript.
Declaration of Competing Interest
The authors declare that they have no competing interests.
Edited by Yi Fang
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Mangussi-Gomes J., Enout M.J., Castro T.C., de Andrade J.S., Penido N.O., Kosugi E.M. Is the occurrence of spontaneous epistaxis related to climatic variables? A retrospective clinical, epidemiological and meteorological study. Acta Otolaryngol. 2016;136:1184–1189. doi: 10.1080/00016489.2016.1191673. [DOI] [PubMed] [Google Scholar]
- 2.Petruson B., Rudin R. The frequency of epistaxis in a male population sample. Rhinology. 1975;13:129–133. [PubMed] [Google Scholar]
- 3.Pallin D.J., Chng Y.M., McKay M.P., Emond J.A., Pelletier A.J., Camargo C.A. Epidemiology of epistaxis in US emergency departments, 1992 to 2001. Ann Emerg Med. 2005;46:77–81. doi: 10.1016/j.annemergmed.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 4.Padgham N. Epistaxis: anatomical and clinical correlates. J Laryngol Otol. 1990;104:308–311. doi: 10.1017/s0022215100112563. [DOI] [PubMed] [Google Scholar]
- 5.Shukla P.A., Chan N., Duffis E.J., Eloy J.A., Prestigiacomo C.J., Gandhi C.D. Current treatment strategies for epistaxis: a multidisciplinary approach. J Neurointerventional Surg. 2013;5:151–156. doi: 10.1136/neurintsurg-2011-010223. [DOI] [PubMed] [Google Scholar]
- 6.Kucik C.J., Clenney T. Management of epistaxis. Am Fam Physician. 2005;71:305–311. [PubMed] [Google Scholar]
- 7.Toner J.G., Walby A.P. Comparison of electro and chemical cautery in the treatment of anterior epistaxis. J Laryngol Otol. 1990;104:617–618. doi: 10.1017/s0022215100113398. [DOI] [PubMed] [Google Scholar]
- 8.Badran K., Malik T.H., Belloso A., Timms M.S. Randomized controlled trial comparing Merocel and RapidRhino packing in the management of anterior epistaxis. Clin Otolaryngol. 2005;30:333–337. doi: 10.1111/j.1365-2273.2005.01019.x. [DOI] [PubMed] [Google Scholar]
- 9.Bachelet J.T., Bourlet J., Gleizal A. [Hemostatic absorbable gel matrix for severe post-traumatic epistaxis] Rev Stomatol Chir Maxillofac Chir Orale. 2013;114:310–314. doi: 10.1016/j.revsto.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 10.Newton E., Lasso A., Petrcich W., Kilty S.J. An outcomes analysis of anterior epistaxis management in the emergency department. J Otolaryngol Head Neck Surg. 2016;45:24. doi: 10.1186/s40463-016-0138-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Farneti P., Pasquini E., Sciarretta V., Macrì G., Gramellini G., Pirodda A. Comparison of local sclerotherapy with lauromacrogol versus nasal packing in the treatment of anterior epistaxis. Clin Exp Otorhinolaryngol. 2016;9:131–135. doi: 10.21053/ceo.2015.00416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Masoudian P., McDonald J.T., Lasso A., Kilty S.J. Socioeconomic status and anterior epistaxis in adult population. World J Otorhinolaryngol Head Neck Surg. 2018;4:263–267. doi: 10.1016/j.wjorl.2017.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goddard J.C., Reiter E.R. Inpatient management of epistaxis: outcomes and cost. Otolaryngol Head Neck Surg. 2005;132:707–712. doi: 10.1016/j.otohns.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 14.Goljo E., Dang R., Iloreta A.M., Govindaraj S. Cost of management in epistaxis admission: impact of patient and hospital characteristics. Laryngoscope. 2015;125:2642–2647. doi: 10.1002/lary.25374. [DOI] [PubMed] [Google Scholar]
- 15.Kilty S.J., Al-Hajry M., Al-Mutairi D. Prospective clinical trial of gelatin-thrombin matrix as first line treatment of posterior epistaxis. Laryngoscope. 2014;124:38–42. doi: 10.1002/lary.24240. [DOI] [PubMed] [Google Scholar]
- 16.Data Standards Unit, Health Data Branch . Ministry of Health and Long Term Care; 2013. Ontario Case Costing Guide: Version 9.0. [Google Scholar]
- 17.Canadian Institute for Health Information . 2011. Canadian Patient Cost Database Technical Document: MIS Patient Costing Methodology. [Google Scholar]
- 18.Manning W.G., Mullahy J. Estimating log models: to transform or not to transform. J Health Econ. 2001;20:461–494. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- 19.Viehweg T.L., Roberson J.B., Hudson J.W. Epistaxis: diagnosis and treatment. J Oral Maxillofac Surg. 2006;64:511–518. doi: 10.1016/j.joms.2005.11.031. [DOI] [PubMed] [Google Scholar]