Abstract
Socioeconomic factors correlate with mental health and affect individual life chances. However, the influence of specific and cumulative social disadvantages on children's mental health problems has received little attention. Previous studies have primarily used global measures of mental health problems or aggregated indicators of socioeconomic status. We contribute to this research by including multiple indicators of parental social disadvantage to study independent and accumulative effects. The study focuses on the Attention Deficit/Hyperactivity Disorder (ADHD), which is known to affect children's educational and socioeconomic trajectories. ADHD is one of the most common child mental health problems and although heredity has been estimated to 76 percent, research suggests that a large social component remains in the prevalence. We exploit comprehensive high-quality registry data for the entire population of children born 1990–1999 in Denmark (N = 632,725). The ADHD prevalence is 3.68 percent. Estimates from linear probability models show that parental unemployment, relative income poverty, and low educational attainment increase children's risk of ADHD with 2.1 (95% CI 1.8–2.3), 2.3 (95% CI 2.1–2.5), and 3.5 percentage points (95% CI 3.3–3.7), respectively. Children who live with all three disadvantages face an increased risk of 4.9 percentage points.
Keywords: Cumulative social disadvantage, Mental health, ADHD, Social gradient in diagnosis
Highlights
-
•
Socioeconomic disadvantage correlates with the risk of ADHD.
-
•
Yet, the specific and cumulative influence of social disadvantages has received little attention.
-
•
Parental unemployment, relative income poverty and low educational attainment increases children's risk of ADHD.
-
•
Accumulated social disadvantages add substantially to the risk of ADHD.
Introduction
The increased prevalence of children's mental health problems is a major societal concern and the disparities associated with mental health constitute an important aspect of social inequality. In line with cumulative disadvantage theory (DiPrete & Eirich, 2006; Goldman, 2001; Thoits, 2010), both social science research and health research have shown that the effects of separate social disadvantages such as poverty or unemployment can accumulate and thereby cause more severe individual detriment and in turn increase social inequality (e.g., Bauman, 2006; Kallio; Kauppinen, & Erola, 2016).
Several mental disorders are associated with adult socioeconomic status (SES)—one such example is Attention Deficit/Hyperactivity Disorder (ADHD). The ADHD disorder, which is one of the most common chronic mental health problems among school-aged children, is characterized by problems with inattention, hyperactivity, and impulsivity, and the estimated worldwide prevalence is 3–5 percent (Polanczyk, Salum, Sugaya, Caye, & Rohde, 2015; Sayal, Prasad, Daley, Ford, & Coghill, 2018). Western societies have seen a marked increase in the diagnosis and treatment rates of ADHD in recent decades (Atladottir et al., 2014; Danish Health and Medicines Authority, 2014; Kessler et al., 2005; Polanczyk, Lima, Horta, Biederman, & Rohde, 2007; Sayal et al., 2018). Although studies show a strong genetic link in the susceptibility to ADHD and an estimated heredity factor of 76 percent, both genetic and non-genetic factors may contribute to the development of ADHD (Faraone, Perlis, Doyle, & Smoller, 2005). Several questions concerning the role of socioeconomic factors remain to be addressed. This study investigates the association between individual and accumulative social disadvantages and the risk of ADHD.
Prior research shows that children diagnosed with ADHD face risks of poorer performance in school, lower educational attainment, weaker labor market attachment, and criminal behavior (Currie & Stabile, 2004; Dalsgaard, Nielsen, & Simonsen, 2014; Ding, Lehrer, Rosenquist, & Audrian, 2008; Fletcher, 2014; McLeod & Kaiser, 2004; McLeod, Uemura, & Rohrman, 2012). In other words, ADHD may reduce children's life chances significantly and result in negative social consequences for the individual's life course. However, the negative social trajectories associated with ADHD might not be accounted for entirely by the challenges inherent in the disorder; social disadvantage associated with the risk of ADHD and with socioeconomic outcomes could be a significant explanatory factor. If family resources (material or immaterial) constitute protective factors, the risk of ADHD will be greater in families characterized by (more) social disadvantage.
Though previous research links risk of ADHD to key socioeconomic factors (e.g. Bøe, Hysing, Skogen, & Breivik, 2016; Froehlich et al., 2007; Miech, Caspi, Moffitt, Wright, & Silva, 1999), the mechanisms through which the accumulation of such factors affect the risk of ADHD in children are not fully understood, and research that explores this association within a sociological framework is scarce. We contribute to this field of research by investigating the association between distinct individual-level measures of parental social disadvantage (including education, income, and unemployment) and children's risk of receiving an ADHD diagnosis before age 18. We further expand the research by investigating cumulative effects from the combination of these social disadvantages.
Previous research
Several studies reveal a significant association between parental SES and children's mental health (Comeau & Boyle, 2018; McLaughlin et al., 2011; McLeod & Shanahan, 1993). In a systematic review summarizing 52 studies, Reiss identifies a consistent inverse relationship between socioeconomic disadvantage and various mental health problems; overall, children with a disadvantaged background are 2–3 times more likely to develop mental health problems (Reiss, 2013). The association is found to be stronger for externalizing disorders (e.g. disorders such as ADHD that involve behaviors directed at or easily noticeable by other people) than for internalizing disorders (e.g. depression, anxiety, or other emotional disorders where symptoms are typically directed inwards). The magnitude of the correlation between SES and mental health varies with different socioeconomic indicators; household income and parental education are among the strongest predictors of children's overall mental health (Reiss, 2013). The following section reviews the literature on associations between specific SES factors and ADHD.
Family income poverty and relative income are the most commonly used socioeconomic measures in studies on ADHD occurrence. Transitions into poverty or persistent poverty in childhood predicts higher levels of child hyperactivity/inattention symptom scores and higher risk of parent-reported ADHD (Bøe, Øverland, Lundervold, & Hysing, 2012; Davis, Sawyer, Lo, Priest, & Wake, 2010; Fitzsimons, Goodman, Kelly, & Smith, 2017; Hegelund; Flensborg-Madsen, Vassard; Niclasen, & Mortensen, 2019; Miller et al., 2018; Russell, Ford, & Russell, 2018; Russell, Ford, Rosenberg, & Kelly, 2014). These findings concur with recent Danish research which shows that children in families with financial instability have higher levels of especially externalizing behaviors such as ADHD (Pryor, StrandbergNyboHulvejMelchior, Hulvej, & Pryor, 2018). Pryor and colleagues find that especially poverty around the time of birth is associated with worse symptoms of hyperactivity/inattention. Several studies suggest that a dose-dependent association between income and risk of ADHD exist, i.e. that levels of poverty matter (Larsson, Sariaslan, Långström, D’Onofrio, & Lichtenstein, 2014; Miech et al., 1999) such that children who live in families in the lowest income quintile are more likely than the wealthiest (fifth quintile) to fulfill ADHD diagnostic criteria (Froehlich et al., 2007).
Parent educational attainment is also associated with the risk of ADHD. Hjern, Weitoft, and Lindblad (2010) use Swedish medical registry data and find a significant social gradient for the receipt of ADHD medication with levels of maternal education. Other studies identify a similar inverse relationship between parental educational attainment and symptom scores of hyperactivity/inattention (Bøe et al., 2012; Davis et al., 2010) or risk of ADHD diagnosis in children (Miech et al., 1999; Rowland et al., 2018; Russell et al., 2014).
A few studies identify significant associations between childhood ADHD and other SES factors such as parent unemployment (Davis et al., 2010), occupational status (Miech et al., 1999), or receipt of social assistance (Anderson, 2018; Hjern et al., 2010).
Although previous research identify significant negative associations between measures of SES and childhood ADHD, several questions and issues remain to be addressed. First, the question of whether cumulative effects from combinations of specific social disadvantages exist has not been fully answered. Second, previous findings often rely on general categorizations of SES rather than precise indicators (and levels) of actual social disadvantage or adversity. Third, studies on this topic often use broad measures of mental health or domains that encompass several diagnoses and thus do not capture specific pathways. Fourth, studies are often small, and research that includes full population information from both diagnosis and medical treatment to define cases of ADHD is needed. This study proposes to address these limitations by investigating the association between specific individual-level measures of parental social disadvantage and children's risk of ADHD and by exploring the cumulative effects from combinations of these disadvantages. To ensure data quality and limit bias from self-report diagnoses, we follow full nationwide cohorts and use comprehensive Danish registry data on both diagnosis and medical treatment to identify ADHD. We pose the following two research questions:
-
1.
How is the risk of ADHD related to parental social disadvantages in terms of low educational attainment, relative income poverty, and unemployment?
-
2.
Does the accumulation of such social disadvantages increase the risk of child ADHD?
Compared to the common practice in studies concerned with the first research question, we use more distinct and comprehensive measures of social disadvantages and include levels of disadvantage. According to previous studies, parents' income and educational attainment especially affect children's risk of ADHD and similar diagnoses. To measure parental social disadvantages in detail, we consider levels of relative income poverty and levels of educational attainment. We also include levels of unemployment in the analysis because this measure is underexplored in existing research.
With the second research question, we wish to add to prior research by exploring the potential cumulative effects of social disadvantage for the risk of ADHD. The literature in this area is very scarce. Bøe et al. (2012) compare the influence of education and family economy on different domains of mental health, one of which is hyperactivity/inattention, yet do not investigate the cumulative influence of several indicators within single domains. Other studies similarly investigate the importance of different SES indicators for the onset of a wide range of overall categories of mental diagnoses, for example, behavioral disorders (McLaughlin et al., 2011), or across broad domains of mental health problems (Comeau & Boyle, 2018; Davis et al., 2010). Yet these studies compare such associations across disorders rather than within single disorders and do not investigate cumulative effects from combinations of social disadvantages.
Various possible reasons for a general social gradient in mental health have been proposed, some of which may be relevant specifically for the unequal socioeconomic distribution of ADHD. We address two such questions in a supplementary analysis; namely, whether parents' mental health problems mediate social disadvantage effects on children's risk of ADHD, and whether social disadvantage effects on this risk vary by parents' history of ADHD. Studies have suggested that prenatal maternal stress affects children’ mental health (Daskalakis, Bagot, Parker, Vinkers, & Kloet, 2013) and in particular increases the risk of children's externalizing disorders such as ADHD (MacKinnon, Kingsbury, Mahedy, Evans, & Colman, 2018). The association of poverty with childhood mental health problems may even be mediated by parents' psychological distress (Wickham, Whitehead, Taylor-Robinson, & Barr, 2017).
Given the heritability of ADHD and the known negative impact of the disorder on social, academic, and career outcomes, it is plausible that ADHD clusters in families with lower SES and create circles of disadvantage across generations (Reiss, 2013, p. 24). We account for part of such heritability effects by including parental ADHD in all analyses. We also investigate if the association of ADHD with social disadvantage varies across parents’ history of ADHD (Rowland et al., 2018).
Data and methods
Study setting and sample
For the analysis of this study, we consider the full population cohorts of children born in Denmark in the years 1990–1999. We exploit comprehensive high-quality data with the unique potential to combine and link individual and parent level medical and socioeconomic information provided by Statistics Denmark. Our follow-up time for the onset of ADHD (defined as getting a diagnosis and/or entering medical treatment for ADHD) is 18 years for all children included in the study. 18 years is currently the maximum possible data window available in the registers with respect to tracing diagnosis and treatment of ADHD and ensuring the availability of relevant socioeconomic data to measure parent social disadvantage. The study population consists of 632,725 individuals (Table 1).
Table 1.
Study population as well as number and percentage of children with ADHD across birth cohorts.
| Birth cohort | N | ADHD | % ADHD |
|---|---|---|---|
| 1990 | 59,173 | 808 | 1.37 |
| 1991 | 59,928 | 1,159 | 1.93 |
| 1992 | 63,314 | 1,632 | 2.58 |
| 1993 | 63,235 | 2,050 | 3.24 |
| 1994 | 65,852 | 2,475 | 3.76 |
| 1995 | 66,170 | 2,754 | 4.16 |
| 1996 | 64,023 | 2,885 | 4.51 |
| 1997 | 64,015 | 3,002 | 4.69 |
| 1998 | 63,278 | 3,067 | 4.85 |
| 1999 | 63,621 | 3,455 | 5.43 |
| All | 632,609 | 23,287 | 3.68 |
Notes: The ADHD sample includes all children born in the years 1990–1999 who receive an ADHD diagnosis or enter medical ADHD treatment before age 18.
In Denmark, healthcare is universal and free. Both the diagnostic and medical prescription practices for ADHD are regulated with national clinical guidelines that require evaluation by specialist doctors or psychiatrists rather than general practitioners (Danish Health and Medicines Authority, 2014, 2018). Due to the high data quality and the national clinical guidelines for diagnostic practice in Denmark, we expect fewer mild cases of ADHD and fewer false positive cases. However, similar to international time trends in the prevalence of ADHD, Denmark has seen a marked increase in both the diagnosis and treatment rates (Table 1) (Atladottir et al., 2014; Pottegård et al., 2012; The Danish State Serum Institute (SSI), 2012, pp. 1–6; Wallach-Kildemoes, Skovgaard, Thielen, Pottegård, & Mortensen, 2015). The national guidelines for diagnosing ADHD were introduced in 2008 and the awareness of the diagnosis has increased among professionals as well as in public debates. In addition, new and enhanced medical products for the treatment of ADHD have entered the market, which may have affected both the propensity to treat and diagnose ADHD. Moreover, the propensity to diagnose and treat ADHD varies across regions and psychiatric wards (Dalsgaard et al., 2014; Madsen, Ersbøll, Olsen, Parner, & Obel, 2015). To capture the effect that such trends may have on our results, we control for birth cohort and residential region in all analyses.
Medical expenses for ADHD treatment are heavily and universally subsidized in Denmark and most children with ADHD are eligible for a subsidy from the state that covers full costs of their prescription medicine. This system possibly reduces any direct influence of family financial resources on entering and maintaining medical treatment for the disorder; such financial barriers have been identified in countries with less welfare distribution (Currie & Stabile, 2004; Froehlich et al., 2007; Galera et al., 2014). Nevertheless, socio-cultural norms or lack of immaterial resources associated with lower SES may cause parents to refrain from seeking a diagnosis or from entering medical treatment. We find evidence in data to suggest that among children with registered ADHD diagnoses, very low income and long-term unemployment is associated with a lower probability of entering treatment. The reverse argument has been proposed as well; i.e. that families with more (material or immaterial) resources refrain from entering medical treatment and maybe compensate for the child's difficulties in other ways or seek alternative treatment. We find no evidence of such trends. Still, we cannot test the argument for children, whose diagnosis is not registered.
Due to the circumstances accounted for in this section, we expect any social gradient identified in the analyses to be medium or lower bound estimates compared to countries with less social redistribution than the Danish welfare system and therefore consider Denmark an interesting case for this type of analysis.
Data and measures
We combine comprehensive medical and sociodemographic data from national registers provided by Statistics Denmark to investigate the individual risk of ADHD across indicators of family social disadvantage for an entire population cohort. From the Danish National Patient Registry and Prescription Registry, we obtain information on ADHD diagnosis and medical treatment, respectively. We then merge these data through unique personal identification numbers with registers that contain rich socioeconomic and demographic data from parents.
Dependent variable – ADHD diagnosis. ADHD diagnosis is the dependent variable in all analyses and defined as receiving an ADHD diagnosis and/or entering medical ADHD treatment before age 18. This age restriction provides equal follow-up time for the entire sample. From the Danish National Patient Registry (Lynge, Sandegaard, & Rebolj, 2011; Mors, Perto, & Mortensen, 2011), we retrieve data on the psychiatric history and diagnoses of all sampled children and their parents. Data include all diagnoses of Hyperkinetic Disorder as defined in the WHO International Classification of Diagnosis (ICD versions 8–10). Hyperkinetic disorder is the ICD equivalent to the ADHD diagnosis described in the American Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). Children who meet full criteria for Hyperkinetic disorder also meet full DSM-IV criteria for ADHD though not all children who meet the DSM-IV criteria for ADHD meet the criteria for Hyperkinetic disorder (Lahey et al., 2006).
Danish clinical guidelines require that trained psychiatric or specialist doctors diagnose ADHD (Danish Health and Medicines Authority, 2014; Ministry of Health, 2012) and the general validity of psychiatric diagnoses in this registry is considered good (Mors et al., 2011). A study by Linnet et al. (2009) investigated the validity specifically of the ADHD diagnoses assigned by Danish health services using medical records of children registered with ADHD (Hyperkinetic Disorder) in the Danish Psychiatric Registry and found 83 percent agreement for the full diagnosis of ADHD. The agreement percentage was 100 percent for Subthreshold ADHD or Possible ADHD (defined as children who lacked one or more symptoms, respectively, in meeting the criteria for one of the three subtypes).
In most cases, diagnoses are established within general hospitals—either at psychiatric wards or in general hospitals by neurologists or pediatricians. In these instances, data are near complete. However, parents may seek a diagnosis from a private practicing child psychiatrist, in which case diagnostic registration is not mandatory and data hence incomplete. Therefore, to ensure the most inclusive identification of ADHD, we supplement the diagnostic data with information on purchases of ADHD medication from the Danish National Prescription Registry (Kildemoes, Sørensen, & Hallas, 2011). Due to public reimbursement of medical expenses, the prescription registry has very high completeness and validity and holds comprehensive information on all prescriptions for drugs filled by Danish residents at outpatient pharmacies since 1995. Using historic case records to reassess for DSM-IV ADHD criteria, Dalsgaard et al. found that 65 percent of those treated for ADHD according to the medical registers met full criteria for an ADHD diagnosis, while 81 percent met criteria for subthreshold ADHD (Dalsgaard, Hansen, Mortensen, Damm, & Thomsen, 2001).
We use the categorization of drugs according to the Anatomic Therapeutic Chemical (ATC) index (World Health Organization (WHO), 2016) to include in our definition all prescriptions for the drugs approved specifically for ADHD in Denmark (Danish Health and Medicines Authority, 2014; Pottegård; Bjerregaard; Kortegaard, & Zoëga, 2015).
3.68 percent (23,287) children in our sample either have a registered ADHD diagnosis in the Danish National Patient Registry or have been in medical ADHD treatment before age 18, according to the Danish National Prescription Registry. Of this group, 12,610 children have a registered ADHD diagnosis and have entered medical treatment, 4,049 children have a registered diagnosis with no medical treatment, and 6,628 children entered medical treatment with no registered diagnosis. The majority of children in this group are likely diagnosed by private practicing psychiatrists.
Independent variables – Social disadvantage. We include the following three specific indicators to measure parental social disadvantages. Relative income poverty is measured using gross parental income adjusted for family status being single-parenthood or nuclear family (income divided by the number of parents in the family). We then present income quintiles and set the highest (fifth) quintile as the reference category. We measure unemployment as months of unemployment adjusted for family status (total number of months divided by the number of parents in the family) and split into three categories: <1 month (reference), 1–5 months and 6–12 months in a year. We obtain educational attainment information from ISCED-codes (UNESCO Institute of Statistics, 2012) and use the highest level of completed education for parents: Compulsory school or less (equal to lower secondary education), upper secondary education, and tertiary education (reference category), respectively. To measure the accumulative effects of the social disadvantages, we investigate all possible logical combinations of the three social disadvantage indicators described. To reduce complexity, we include one variable for each social disadvantage indicator: Compulsory school or less, 6–12 months of unemployment, and first (lowest) income quintile. ‘No disadvantage’ is set as the reference and indicate children who live in families with a high income-level, high educational attainment and without unemployment.
Having a child with ADHD may affect a family's socioeconomic situation. Effects on the probability of divorce and labor supply of parents have been identified (Kvist, Nielsen, & Simonsen, 2011), yet Russell and colleagues find no significant effect of child ADHD on parent income reduction (2014). To account for any potential issues of reverse causality, we measure all socioeconomic characteristics except educational attainment in the calendar year two years before childbirth. We also test if our estimates of educational attainment, income and unemployment are robust to definitions with different timings (one to five years before childbirth).
Control variables. We include information on the parental history of ADHD in all models to account for the known heredity of ADHD (Faraone et al., 2005). However, due to data limitations in terms of the available timespan in registers, these data are less complete for parent generations than for the child cohorts included in this study.
We also include several variables known to correlate with socioeconomic characteristics. Elevated risks of prenatal, perinatal or childhood (physical) exposures that cause birth complications or premature birth may increase the risk of ADHD (Ask et al., 2018; Franz et al., 2018; Froehlich et al., 2007; Heinonen et al., 2010; Lindblad, RingbäckWeitoft, & Hjern, 2010; K M; Linnet et al., 2006; MacKinnon et al., 2018; Russell et al., 2014). Examples of such exposures are smoking, alcohol use, toxins, maternal stress or other parental health behaviors. We address this possible influence by adjusting for the following birth characteristics: birth weight, duration of the pregnancy (gestational age), an interaction between birth weight and duration of the pregnancy, and the 5-min. APGAR score. The APGAR score (0–10 points) summarizes the health of newborn children (the higher score, the better) and is found to be associated with the risk of ADHD (Apgar, 1953; Li, Olsen, Vestergaard, & Obel, 2011).
Control variables also include gender, immigrant status (descendant of an immigrant or non-immigrant Dane; the latter is the reference), an indicator for living in single-parent-families and a categorized variable for the number of children in the family (one, two or minimum three children; two children is the reference). Finally, fixed effect dummies for birth year and for earliest residential region are included to account for the increase in the ADHD prevalence across birth cohorts (Atladottir et al., 2014; Kessler et al., 2005; Polanczyk et al., 2007) and for any variation in prevalence across regions in Denmark (Madsen et al., 2015; Pottegård et al., 2012).
In a supplementary analysis, we include two variables to indicate if one or both parents have received a psychiatric diagnosis (not including ADHD) and if one or both parents have ever had psychoactive substance use (alcohol or drugs). 4.2% of children in the sample have a parent with registered substance abuse problems, and 16.8% of children have a parent with a psychiatric diagnosis.
Statistical methods
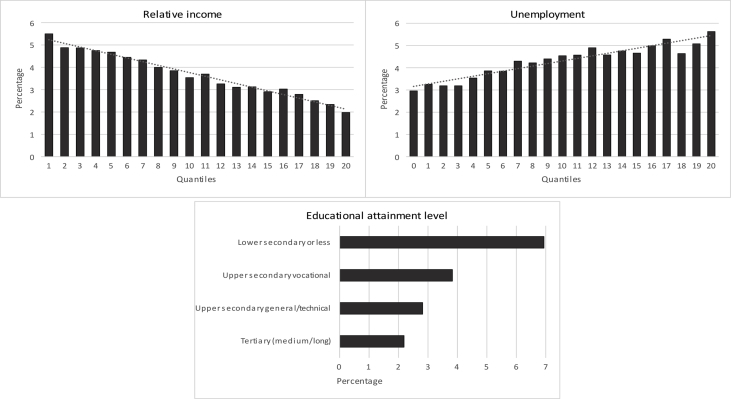
We want to estimate the difference in the risk of ADHD that is associated with select indicators of social disadvantage and their combinations. Because the outcome of the analysis is binary, linear probability models (LPM) and average marginal effects (AME) from logistic regression models are both relevant estimation strategies, yet each method possesses advantages and drawbacks. The risk of mis-specifying the functional form of the relationship is the most critical concern with LPM compared to logistic regression methods, i.e. to assume a linear relationship when the true functional form is non-linear, in which case logistic regression in principle is superior. From non-parametric distributions (Fig. 1), we argue that it is reasonable to assume that the independent variables mainly vary over a range where the curve is roughly linear, which warrants the use of LPM. From a simulation study, Mood shows that the coefficients of LPM and AME are almost equal and that the advantage of logistic regression is not fully exploited when estimating average effects such as AME (2010). Mood argues that “As long as the misspecification of functional form does not alter (more than marginally) the substantive conclusions that are relevant to the questions asked, it is reasonable to choose LPM over logistic regression” (Mood, 2010, p. 78).
Fig. 1.
Percentage of children with ADHD across parents' level of income, unemployment, and educational attainment.
Notes: Employment is illustrated as ‘0’ on the x-axis and levels of unemployment are shown in 20-quantiles. For relative income, the graph presents 20-quantiles across the entire distribution.
ADHD is by definition an uncommon event in the population (3.68 percent in our data), wherefore LPM may predict negative probabilities. This is a drawback for LPM compared to AME, especially when predicting very infrequent (or frequent) events. Negative probabilities are predicted for nine percent in our data. However, predicting unrealistic values is even a common issue for linear regression with continuous variables (Long, 1997), and is not a major concern in LPM unless it concerns a large fraction of the sample (Mood, 2010).
An important advantage of LPM over logistic regressions is a more straightforward interpretation of model estimates as risk differences (percentage points) and a simpler interpretation when comparing models with different independent variables (Mood, 2010). Moreover, LPM possesses clear advantages in terms of the interpretation of interactions, for which logistic models are problematic (Tutz, 2018). We therefore present results from LPM to investigate the risk differences in terms of receiving an ADHD diagnosis given the following social disadvantage indicators: relative income, educational attainment, and unemployment. All models are adjusted for the control variables described in the Data and measures section, including regional and cohort fixed effects. We estimate robust standard errors to correct for heteroscedastic and non-normal residuals that may lead to inefficiency and invalid standard errors. To acknowledge the potential pitfalls of the LPM, especially the risk of mis-specifying the functional form, we test the robustness of all main results by re-estimating AME from logistic regression. These estimates (available upon request) are almost identical to the results presented in the following. We also re-estimated our results using Cox regression models to account for the fact that the occurrence of ADHD is a function of time. These results are also comparable to those presented in the following.
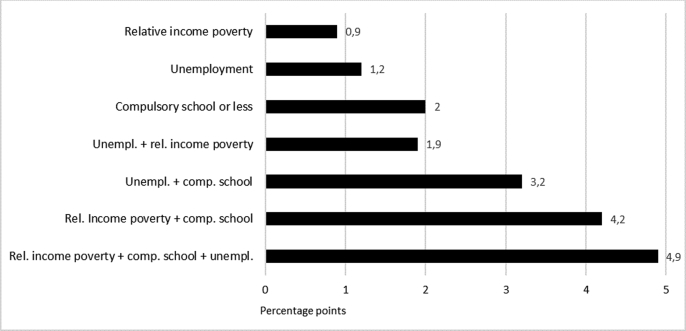
We first estimate each association between the social disadvantage indicators and the risk of ADHD in separate models (Models 1–3). These estimates represent unconditional effects because they do not take other socioeconomic factors that correlate with the included indicator into account. Next, we include all three social disadvantage indicators simultaneously to investigate possible independent effects of each (Model 4). Last, we include interaction terms for all possible combinations of the three social disadvantage indicators to assess independent as well as cumulative effects (Fig. 2).
Fig. 2.
Increase in the risk of ADHD for combinations of social disadvantage measures. Percentage points from a linear probability model.
Notes: Model estimates are presented in Table A1 in the supplementary material. Estimates are adjusted for gender, immigrant status, birth characteristics (weight, gestational age, and 5-min. APGAR score), single-parenthood, parent ADHD diagnosis, and the number of children in the household. All models include fixed effect dummies for birth year and residential region.
In a supplementary analysis, we investigate if parents' mental health in terms of substance abuse or psychiatric diagnosis (apart from ADHD) mediates social disadvantage effects. We further test whether our main results vary across family history of ADHD to see if parental ADHD modifies the influence of social disadvantage on children's risk of ADHD.
A key challenge for studies on ADHD is that although the severity of the disorder follows a continuum, the diagnosis is a binary category determined by a combination of clinical observations, history, and reports of the child's daily life behavior by parents and teachers. Potentially overly inclusive diagnosis among certain subpopulations is a non-negligible challenge and has been subject to an ongoing debate. Therefore, we test if the effect of parent social disadvantage on the risk of ADHD differs across regions and birth cohorts, respectively. We perform several sensitivity tests as well to try the specification of our outcome variable and to test the specification and timing of all social disadvantage indicators.
Results
Table 2 presents the descriptive statistics and the unadjusted percentage of children with ADHD for each group. The prevalence of ADHD in data is 3.68 percent, yet this distribution varies greatly with social disadvantage characteristics (Table 2).
Table 2.
Descriptive statistics by family characteristics.
| N | % | % with ADHD | |
|---|---|---|---|
| Level of education | |||
| Compulsory school or less (lower secondary) | 48,656 | 7.69 | 6.91 |
| Upper secondary | 285,795 | 45.18 | 4.11 |
| Tertiary or more (ref.) | 298,158 | 47.13 | 2.75 |
| Unemployment | |||
| 6–12 months | 25,115 | 3.97 | 5.57 |
| 1–5 months | 182,774 | 28.89 | 4.69 |
| <1 months (ref.) | 424,720 | 67.14 | 3.14 |
| Relative income | |||
| 1. Quintile (lowest) | 126,522 | 20.00 | 5.00 |
| 2. Quintile | 126,522 | 20.00 | 4.36 |
| 3. Quintile | 126,522 | 20.00 | 3.59 |
| 4. Quintile | 126,522 | 20.00 | 3.05 |
| 5. Quintile (highest) (ref.) | 126,521 | 20.00 | 2.41 |
| Social disadvantages | |||
| None (ref.) | 343,473 | 54.29 | 2.84 |
| Unemployment | 207,889 | 32.86 | 4.79 |
| Relative income poverty | 126,522 | 20.00 | 5.00 |
| Compulsory school or less | 48,656 | 7.69 | 6.91 |
| Unemployment + rel. income poverty | 58,699 | 9.28 | 5.90 |
| Unemployment + comp. school | 27,120 | 4.29 | 7.47 |
| Rel. income poverty + comp. school | 20,521 | 3.24 | 8.54 |
| Rel. income poverty + comp. school + Unemployment | 12,409 | 1.96 | 8.90 |
| All | 632,609 | 100.00 | 3.68 |
For each characteristic, we see that the more disadvantaged, the higher the raw proportion of children with an ADHD diagnosis (Table 2). These patterns are also visible in Fig. 1, which shows the distribution of ADHD across relative levels of parents' income and unemployment (in quantiles), and across parents’ educational attainment level (corresponding to ISCED-codes (UNESCO Institute of Statistics, 2012)).
All three social disadvantage measures are inversely associated with the risk of ADHD (Fig. 1). For relative income and unemployment, the graphs suggest linear associations.
We now turn to the main results. Table 3 presents adjusted estimates from the linear probability models. The results represent risk differences compared to the general 3.68 percent prevalence of ADHD.
Table 3.
Effects of parental social disadvantages on child risk of ADHD. Estimates from linear probability models.
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| Level of education (ref. ≥ tertiary) | ||||
| Compulsory school or less | 0.035*** (0.001) [0.033; 0.037] | 0.030*** (0.001) [0.012; 0.014] | ||
| Upper secondary | 0.013*** (0.000) [0.012; 0.014] | 0.012*** (0.000) [0.012; 0.014] | ||
| Unemployment (ref. < 1 month) | ||||
| 6–12 months | 0.021*** (0.001) [0.018; 0.023] | 0.011*** (0.001) [0.012; 0.014] | ||
| 1–5 months | 0.013*** (0.001) [0.012; 0.014] | 0.008*** (0.001) [0.012; 0.014] | ||
| Relative income (ref. 5. Quintile) | ||||
| 1. Quintile | 0.023*** (0.001) [0.021; 0.025] | 0.017*** (0.001) [0.015; 0.018] | ||
| 2. Quintile | 0.019*** (0.001) [0.017; 0.020] | 0.012*** (0.001) [0.010; 0.013] | ||
| 3. Quintile | 0.013*** (0.001) [0.012; 0.014] | 0.008*** (0.001) [0.006; 0.009] | ||
| 4. Quintile | 0.008*** (0.001) [0.006; 0.009] | 0.005*** (0.001) [0.004; 0.006] | ||
| R-squared | 4.7 | 4.6 | 4.7 | 4.9 |
| N | 632,609 | 632,609 | 632,609 | 632,609 |
*p < 0.05, **p < 0.01, ***p < 0.001.
Notes: Robust standard errors in parentheses and 95% confidence intervals in brackets. All estimates are adjusted for gender, immigrant status, birth characteristics (weight, gestational age, and 5-min. APGAR score), single-parenthood, parent ADHD diagnosis, and the number of children in the household. Models include fixed effect dummies for birth year and residential region.
All measures of social disadvantage significantly and independently affect the risk of ADHD when adjusted for the observable covariates (Models 1–3, Table 3). The largest unconditional estimate is measured for educational attainment; having parents who complete no more than compulsory school is associated with a 3.5 percentage point higher risk of getting an ADHD diagnosis, and upper secondary education is associated with an increased risk of 1.3 percentage points. Upper secondary education includes vocational and academic (college preparatory) tracks. Splitting results in these tracks, we find that the 1.3 estimate is driven primarily by parents who complete vocational tracks. These children face 1.73 percentage points increase in risk (p < 0.001), whereas children whose parents complete college preparatory tracks face merely 0.17 percentage points increase (p < 0.05).
Children whose parents experience unemployment face an increased risk of 2.1 percentage points for 6–12 months' unemployment in a year and 1.3 percentage points for 1–5 months. Longer periods of unemployment seem to increase the risk of children's ADHD. Relative income poverty is significantly associated with the risk of ADHD in a similar manner. Compared to being in the fifth and highest income quintile (the reference), the first and lowest quintile is associated with an increased risk of 2.3 percentage points, the second with 1.9 percentage points, the third with 1.3 percentage points, and the fourth with 0.8 percentage points.
All social disadvantage estimates indicate dose-response type relationships, i.e. that greater levels of disadvantage are associated with a greater risk of ADHD. We now turn to see if a similar pattern exists in terms of collective social disadvantages. When measured simultaneously (Model 4), the independent effects of each social disadvantage are slightly reduced. This is expected due to the known correlation between social disadvantage measures. Nevertheless, all estimates remain large and equally significant, which suggests that cumulative effects exist.
Next, we estimate interaction effects of all three social disadvantage measures to assess whether any combinations add to (or subtract from) the risk of ADHD over and above cumulative effects. Fig. 2 illustrates the percentage point increase for each logical combination of the social disadvantages for the risk of ADHD. All estimates reflected in Fig. 2 are presented in Table A1 in the supplementary material.
Compared to Model 4 in Table 3, the estimates for each social disadvantage indicator (Fig. 2) remain significant and unaltered; children who live in relative income poverty face a 0.9 percentage points increase in the risk of ADHD, the risk increase is 1.2 percentage points for unemployment and 2.0 percentage points for compulsory school. The combination of unemployment and income poverty is associated with a 1.9 percentage point increase. For children whose parents complete no more than compulsory school and who are either unemployed or live in relative income poverty, the risk of ADHD increases with 3.2 and 4.2 percentage points, respectively. Last, children who live with all three disadvantages face an increased risk of ADHD equal to 4.9 percentage points. Two percent of children in the sample live under these conditions of cumulative social disadvantage.
Last, we investigate whether parents’ mental health in terms of substance abuse or psychiatric diagnosis mediates the association of ADHD with social disadvantages. Both indicators are significantly associated with an increased risk of ADHD equal to 1.5 percentage points (95% CI, 1.12–1.19, p < 0.001) for substance abuse and 1.8 percentage points (95% CI, 1.6–1.19, p < 0.001) for psychiatric diagnosis. However, when we re-estimate Model 4 of Table 3 with these variables included (results not shown) they reduce neither effects nor significance of the social disadvantages. We further test whether the social disadvantage effects differ across parental history of ADHD by estimating interaction terms between each social disadvantage measure and parental history of ADHD (results not shown). These estimates are significant and show that social gradient patterns in the risk of ADHD are more pronounced in families with no prior history of ADHD compared to families with parent ADHD.
Sensitivity analyses
To test the main results in terms of model misspecification, we re-estimate them as AME from logistic regression. These results (not shown) are almost identical to the presented estimates and therefore do not alter any conclusions.
Next, to test the sensitivity of the definition of our outcome variable we use data on either diagnosis or medical treatment to define ADHD. The estimated associations are smaller when definitions of ADHD rely solely on diagnosis or medical treatment rather than the combination, yet conclusions remain unaltered. The relationship between social disadvantage and ADHD is also robust to the timing and specification of the social disadvantage measures from one to five years before the birth of the respondent. We find no discernible time trend in the social disadvantage effects estimated, i.e. the development across time in terms of an increased prevalence of ADHD does not reflect changes in the relative risk of ADHD given the levels of social disadvantage. Some variation across regions exist, yet these regional differences do not appear systematic and are not all significant.
Discussion and conclusions
This study shows that specific and well-measured parental social disadvantages in terms of unemployment, relative income poverty, and low educational attainment independently affect the risk of ADHD. The significant independent effects of the social disadvantage measures on the risk of ADHD suggest that they are not interchangeable factors in terms of measuring social disadvantage effects on child mental health and that they should not be treated as such. The magnitude of the coefficients is substantial relative to the 3.68 percent prevalence of ADHD in the population, and our sensitivity tests show that the social disadvantage effect is stable across included cohorts and regions. Moreover, if socio-cultural norms or the lack of material or immaterial resources in any way constitutes barriers for receiving an ADHD diagnosis or entering treatment, the results presented here are lower bound.
Several studies argue that psychological stressors due to conditions in families with fewer socioeconomic resources affect children's general mental health and socioemotional development (Korenman, Miller, & Sjaastad, 1995; McLeod & Shanahan, 1996; Thoits, 2010). In line with these results, we find that worse socioeconomic conditions in childhood increase the risk of ADHD. This finding, in turn, suggests that cumulative social disadvantages heighten the externalizing behaviors that are characteristic of ADHD and result in an increased risk of diagnosis.
Parents' educational attainment remains the strongest influential factor for the risk of ADHD across all model specifications. Indeed, the individual effect of low educational attainment seems to be the main contributor to the effect of all three disadvantages. Children whose parents complete no more than compulsory school face 3.5 percentage points higher risk of receiving an ADHD diagnosis. Several studies have established significant associations between children's symptoms of ADHD and educational achievement (Currie & Stabile, 2004; Ding et al., 2008; McLeod et al., 2012; McLeod & Kaiser, 2004). Adding the results from the present study to this research lead us to propose that future studies explore the intergenerational associations between parents' and children's educational attainment in the context of ADHD to determine the potential impact on intergenerational social mobility.
The estimated effects of social disadvantage on child ADHD remain large and significant even when adjusted for parental ADHD and a range of individual and family-level characteristics. Due to the heritability factor of ADHD, children whose parents are themselves diagnosed with ADHD face 21 percentage points higher risk of developing the disorder compared to children with no family history of ADHD according to our analyses. This risk is stable across all models. Bearing in mind that the data on parental ADHD are incomplete, the estimate is likely lower bound.
Rowland and colleagues find that parents' history of ADHD interacts with family income to affect children's risk of ADHD (2018); the social gradient in children's ADHD is stronger in families with no prior history of ADHD compared to families with parental ADHD. Our results concur with this finding, and we find similar patterns for education and unemployment. We interpret this as evidence that parental ADHD moderates the influence of social disadvantage on children's risk of ADHD. In other words, parental ADHD partially explains both parents' social disadvantage and children's risk of ADHD.
In line with previous studies (Fitzsimons et al., 2017; Joelsson et al., 2017), we find that parents’ psychopathology (apart from ADHD) and substance abuse affect the risk of ADHD in children, though we do not find that these factors mediate the effects of socioeconomic disadvantage.
Strengths and limitations
High-quality detailed data from Danish registers enable us to follow an entire unselected nationwide cohort of children and to analyze and systematically map the individual risk of ADHD for more than 632,000 children with full population coverage. We consider this a major strength of the study. Moreover, data allow for an equal follow-up time of 18 years for all included cohorts.
We use both medical and diagnostic registry data for our outcome variable and thereby rely on registrations from health services that follow national diagnostic regulations concerning ADHD. Findings that rely exclusively on caregiver reports of diagnosis may reflect differential access to health care or diagnostic bias rather than an actual difference in the prevalence of diagnoses reported by the health services. We adjust results for several important confounders known to predict ADHD symptoms and correlate with SES, including birth characteristics and parent psychopathology available from the registers. Furthermore, we account for part of the heritability factor by including information on parent ADHD diagnosis. However, due to the available timespan in the Danish national registers, the diagnostic and medical data for parents is less complete. This is a limitation of the study.
Danish national guidelines require that specialists initiate pharmacological treatment for ADHD and the quality of both medical and diagnostic data in the Danish health registers have been assessed in terms of the diagnosis (Dalsgaard et al., 2001; Linnet et al., 2009); we rely on these circumstances to warrant the diagnostic validity of the included cases. However, children who receive an ADHD diagnosis from private practicing psychiatrists and who do not enter medical ADHD treatment are unobserved in this study. These excluded children likely have milder symptoms, though there could be other reasons than severity for refraining from medical treatment. Data do not allow us to account for such cases nor observe the reasons for their exclusion, which is an important limitation of this study.
Implications
The main contribution of this study is the use of specific and comprehensive indicators for social disadvantage to investigate the previously unexplored influence of cumulative social disadvantage for the risk of ADHD. Studies that rely on a single socioeconomic indicator (e.g. income) likely underestimate the role of social disadvantage for the risk of ADHD and, at the same time, they risk overestimating the influence of any single indicators used. The results of this study show that accumulated social disadvantages have extensive consequences for children's mental health and add substantially to the risk of ADHD. Future studies on social inequality in terms of ADHD or other mental health measures should explore these patterns further.
Early onset disorders with profound direct effects on children's cognitive development such as ADHD may cause negative effects from interactions between socioeconomic disadvantage and diagnostic symptoms of the disorder to aggregate from childhood and affect later life chances. Consequently, the findings of this study motivate future research to investigate if children with ADHD who live in socially disadvantaged families are increasingly underprivileged in terms of their educational trajectories or later socioeconomic outcomes. Welfare policies should explore early identification and interventions for children with low SES and known parental history of ADHD and support initiatives to reduce any negative impacts of ADHD on intra-generational mobility.
Ethics approval/Statement EA not required
The study uses anonymized register data provided by Statistics Denmark and its use was approved by the Danish Data Protection Agency. All use is subject to national rules for the collection and storage of such data.
CRediT authorship contribution statement
Maria Keilow: Conceptualization, Methodology, Formal analysis, Data curation, Investigation, Writing - original draft, Writing - review & editing, Project administration, Funding acquisition. Chunsen Wu: Methodology, Validation, Formal analysis, Writing - review & editing, Supervision. Carsten Obel: Methodology, Validation, Formal analysis, Data curation, Writing - review & editing, Supervision, Project administration, Funding acquisition.
Acknowledgements
The authors would like to thank chief research analyst Christoffer Scavenious and senior researcher Jens-Peter Thomsen for their valuable feedback and helpful comments during earlier phases of the study. Data manager Katrine Svendsen provided invaluable assistance in procuring and preparing the raw datasets used for the analyses. We are also thankful for the input from members of the ‘Quant Club’ network at the Department of Sociology, University of Copenhagen and the participants at the GRASPH summer school held by the Danish National Network for Research Training on Public Health. The authors have no conflicts of interests to report. The authors have no financial disclosures to report.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2020.100548.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Anderson L.R. Adolescent mental health and behavioural problems, and intergenerational social mobility: A decomposition of health selection effects. Social Science & Medicine. 2018;197:153–160. doi: 10.1016/j.socscimed.2017.11.026. October 2017. [DOI] [PubMed] [Google Scholar]
- Apgar V. A proposal for a new method of evaluation of the newborn infant. Anesthesia & Analgesia. 1953;120(5):1056–1059. doi: 10.1213/ANE.0b013e31829bdc5c. [DOI] [PubMed] [Google Scholar]
- Ask H., Gustavson K., Ystrom E., Havdahl K.A., Tesli M., Askeland R.B. Association of gestational age at birth with symptoms of attention-deficit/hyperactivity disorder in children. JAMA Pediatrics. 2018;172(8):749–756. doi: 10.1001/jamapediatrics.2018.1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atladottir H.O., Gyllenberg D., Langridge A., Sandin S., Hansen S.N., Leonard H. The increasing prevalence of reported diagnoses of childhood psychiatric disorders: A descriptive multinational comparison. European Child & Adolescent Psychiatry. 2014;24(2):173–183. doi: 10.1007/s00787-014-0553-8. [DOI] [PubMed] [Google Scholar]
- Bauman L.J. Cumulative social disadvantage and child health. Pediatrics. 2006;117(4):1321–1328. doi: 10.1542/peds.2005-1647. [DOI] [PubMed] [Google Scholar]
- Bøe T., Hysing M., Skogen J.C., Breivik K. The Strengths and Difficulties Questionnaire (SDQ): Factor structure and gender equivalence in Norwegian adolescents. PloS One. 2016;11(5):1–15. doi: 10.1371/journal.pone.0152202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bøe T., Øverland S., Lundervold A.J., Hysing M. Socioeconomic status and children's mental health: Results: From the bergen child study. Social Psychiatry and Psychiatric Epidemiology. 2012;47(10):1557–1566. doi: 10.1007/s00127-011-0462-9. [DOI] [PubMed] [Google Scholar]
- Comeau J., Boyle M.H. Patterns of poverty exposure and children's trajectories of externalizing and internalizing behaviors. SSM - Population Health. 2018;4:86–94. doi: 10.1016/j.ssmph.2017.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie J., Stabile M.B. Child mental health and human capital accumulation: The case of ADHD. NBER Working Paper Series. 2004;10435:1–42. doi: 10.1016/j.jhealeco.2006.03.001. [DOI] [PubMed] [Google Scholar]
- Dalsgaard S., Hansen N., Mortensen P.B., Damm D., Thomsen P.H. Reassessment of ADHD in a historical cohort of children treated with stimulants in the period 1969-1989. European Child & Adolescent Psychiatry. 2001;10(4):230–239. doi: 10.1007/s007870170012. [DOI] [PubMed] [Google Scholar]
- Dalsgaard S., Nielsen H.S., Simonsen M. Consequences of ADHD medication use for children's outcomes. Journal of Health Economics. 2014;37:137–151. doi: 10.1016/j.jhealeco.2014.05.005. [DOI] [PubMed] [Google Scholar]
- Danish Health and Medicines Authority . Sundhedsstyrelsen; 2014. National klinisk retningslinje for udredning og behandling af ADHD hos børn og unge - med fokus på diagnoserne ”Forstyrrelse af aktivitet og opmærksomhed” og ”Opmærksomhedsforstyrrelse uden hyperaktivitet” i henhold til ICD-10. [Google Scholar]
- Danish Health and Medicines Authority . 2018. National klinisk retningslinje for udredning og behandling af ADHD hos børn og unge. [Google Scholar]
- Daskalakis N.P., Bagot R.C., Parker K.J., Vinkers C.H., de Kloet E.R. The three-hit concept of vulnerability and resilience: Towards understanding adaptation to early-life adversity outcome. Psychoneuroendocrinology. 2013;38(9):1858–1873. doi: 10.1016/j.psyneuen.2013.06.008. (The) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis E., Sawyer M.G., Lo S.K., Priest N., Wake M. Socioeconomic risk factors for mental health problems in 4-5-year-old children: Australian population study. Academic Pediatrics. 2010;10(1):41–47. doi: 10.1016/j.acap.2009.08.007. [DOI] [PubMed] [Google Scholar]
- Ding W., Lehrer S.F., Rosenquist J.N., Audrian-McGovern J. The impact of poor health on academic performance: New evidence using genetic markers. Journal of Health Economics. 2008;28:579–597. doi: 10.1016/j.jhealeco.2008.11.006. [DOI] [PubMed] [Google Scholar]
- DiPrete T.A., Eirich G.M. Cumulative advantage as a mechanism for inequality: A review of theoretical and empirical developments. Annual Review of Sociology. 2006;32(1):271–297. [Google Scholar]
- Faraone S.V., Perlis R.H., Doyle A.E., Smoller J.W. Molecular genetics of attention-deficit/hyperactivity disorder. Biological Psychiatry. 2005;57:1313–1323. doi: 10.1016/j.biopsych.2004.11.024. [DOI] [PubMed] [Google Scholar]
- Fitzsimons E., Goodman A., Kelly E., Smith J.P. Poverty dynamics and parental mental health: Determinants of childhood mental health in the UK. Social Science & Medicine. 2017;175(December):43–51. doi: 10.1016/j.socscimed.2016.12.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher J. The effects of childhood ADHD on adult labor market outcomes. Health Economics. 2014;23(2) doi: 10.1002/hec.2907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franz A.P., Bolat G.U., Bolat H., Matijasevich A., Santos I.S., Silveira R.C. Attention-Deficit/hyperactivity disorder and very preterm/very low birth weight: A meta-analysis. Pediatrics. 2018;141(1) doi: 10.1542/peds.2017-1645. [DOI] [PubMed] [Google Scholar]
- Froehlich T.E., Lanphear B.P., Epstein J.N., Barbaresi W.J., Katusic S.K., Kahn R.S. Prevalence, recognition, and treatment of attention-deficit/hyperactivity disorder in a national sample of US children. Archives of Pediatrics and Adolescent Medicine. 2007;161(9):857–864. doi: 10.1001/archpedi.161.9.857. [DOI] [PubMed] [Google Scholar]
- Galera C., Pingault J.-B., Michel G., Bouvard M.-P., Melchior M., Falissard B. Clinical and social factors associated with attention-deficit hyperactivity disorder medication use: Population-based longitudinal study. The British Journal of Psychiatry. 2014;205(4):291–297. doi: 10.1192/bjp.bp.113.141952. [DOI] [PubMed] [Google Scholar]
- Goldman N. Social inequalities in health. Annals of the New York Academy of Sciences. 2001;954(1):118–139. [PubMed] [Google Scholar]
- Hegelund E.R., Flensborg-Madsen T., Vassard D., Niclasen J., Mortensen E.L. Parental socioeconomic position and risk of ADHD in offspring: A cohort study of 9648 individuals in Denmark 1976–2013. European Child & Adolescent Psychiatry. 2019;28(5):685–693. doi: 10.1007/s00787-018-1235-8. [DOI] [PubMed] [Google Scholar]
- Heinonen K., Raikkonen K., Pesonen A.K., Andersson S., Kajantie E., Eriksson J.G. Behavioural symptoms of attention deficit/hyperactivity disorder in preterm and term children born small and appropriate for gestational age: A longitudinal study. BMC Pediatrics. 2010;10 doi: 10.1186/1471-2431-10-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjern A., Weitoft G.R., Lindblad F. Social adversity predicts ADHD-medication in school children - a national cohort study. Acta Pædiatrica. 2010;99(6):920–924. doi: 10.1111/j.1651-2227.2009.01638.x. [DOI] [PubMed] [Google Scholar]
- Joelsson P., Chudal R., Uotila J., Suominen A., Sucksdorff D., Gyllenberg D. Parental psychopathology and offspring attention-deficit/hyperactivity disorder in a nationwide sample. Journal of Psychiatric Research. 2017;94:124–130. doi: 10.1016/j.jpsychires.2017.07.004. [DOI] [PubMed] [Google Scholar]
- Kallio J.M., Kauppinen T.M., Erola J. Cumulative socio-economic disadvantage and secondary education in Finland. European Sociological Review. 2016;32(5):649–661. [Google Scholar]
- Kessler R.C., Demler O., Frank R.G., Olfson M., Pincus H.A., Walters E.E. Prevalence and treatment of mental disorders, 1990 to 2003. New England Journal of Medicine. 2005;352(24):2515–2523. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kildemoes H.W., Sørensen H.T., Hallas J. The Danish national prescription registry. Scandinavian Journal of Public Health. 2011;39(7 suppl):38–41. doi: 10.1177/1403494810394717. [DOI] [PubMed] [Google Scholar]
- Korenman S., Miller J.E., Sjaastad J.E. Long-term poverty and child development in the United States: Results from the NLSY. Children and Youth Services Review. 1995;17(1–2):127–155. [Google Scholar]
- Kvist A.P., Nielsen H.S., Simonsen M. IZA Discussion Paper; 2011. The effects of children's ADHD on parents' relationship dissolution and labor supply; p. 6092. [Google Scholar]
- Lahey, Pelham, Chronis, Massetti, Ehrhardt, Lee Predictive validity of ICD-10 hyperkinetic disorder relative to DSM-IV attention-deficit/hyperactivity disorder among younger children. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2006;47(5):472–479. doi: 10.1111/j.1469-7610.2005.01590.x. [DOI] [PubMed] [Google Scholar]
- Larsson H., Sariaslan A., Långström N., D'Onofrio B., Lichtenstein P. Family income in early childhood and subsequent attention deficit/hyperactivity disorder: A quasi-experimental study. Journal of Child Psychology and Psychiatry. 2014;55(5):428–435. doi: 10.1111/jcpp.12140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindblad F., Ringbäck Weitoft G., Hjern A. ADHD in international adoptees: A national cohort study. European Child & Adolescent Psychiatry. 2010;19(1):37–44. doi: 10.1007/s00787-009-0038-3. [DOI] [PubMed] [Google Scholar]
- Linnet K.M., Wisborg K., Agerbo E., Secher N.J., Thomsen P.H., Henriksen T.B. Gestational age, birth weight, and the risk of hyperkinetic disorder. Archives of Disease in Childhood. 2006;91(8):655–660. doi: 10.1136/adc.2005.088872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linnet K.M., Wisborg K., Secher N.J., Hove Thomsen P., Obel C., Dalsgaard S. Coffee consumption during pregnancy and the risk of hyperkinetic disorder and ADHD: A prospective cohort study. Acta Paediatrica, International Journal of Paediatrics. 2009;98(1):173–179. doi: 10.1111/j.1651-2227.2008.00980.x. [DOI] [PubMed] [Google Scholar]
- Li J., Olsen J., Vestergaard M., Obel C. Low Apgar scores and risk of childhood attention deficit hyperactivity disorder. The Journal of Pediatrics. 2011;158(5):775–779. doi: 10.1016/j.jpeds.2010.10.041. [DOI] [PubMed] [Google Scholar]
- Long J.S. SAGE; Thousand Oaks: 1997. Regression models for categorical and limited dependent variables. [Google Scholar]
- Lynge E., Sandegaard J.L., Rebolj M. The Danish national patient register. Scandinavian Journal of Public Health. 2011;39(7 suppl):30–33. doi: 10.1177/1403494811401482. [DOI] [PubMed] [Google Scholar]
- MacKinnon N., Kingsbury M., Mahedy L., Evans J., Colman I. The association between prenatal stress and externalizing symptoms in childhood: Evidence from the avon longitudinal study of parents and children. Biological Psychiatry. 2018;83(2):100–108. doi: 10.1016/j.biopsych.2017.07.010. [DOI] [PubMed] [Google Scholar]
- Madsen K.B., Ersbøll A.K., Olsen J., Parner E., Obel C. Geographic analysis of the variation in the incidence of ADHD in a country with free access to healthcare: A Danish cohort study. International Journal of Health Geographics. 2015;14(1):24. doi: 10.1186/s12942-015-0018-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin K.A., Breslau J., Green J.G., Lakoma M.D., Sampson N.A., Zaslavsky A.M. Childhood socio-economic status and the onset, persistence, and severity of DSM-IV mental disorders in a US national sample. Social Science & Medicine. 2011;73(7):1088–1096. doi: 10.1016/j.socscimed.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod J.D., Kaiser K. Childhood emotional and behavioral problems and educational attainment. American Sociological Review. 2004;69(5):636–658. [Google Scholar]
- McLeod J.D., Shanahan M.J. Poverty, parenting, and children's mental health. American Sociological Review. 1993;58(3):351–366. [Google Scholar]
- McLeod J.D., Shanahan M.J. Trajectories of poverty and children's mental health. Journal of Health and Social Behavior. 1996;37(3):207–220. [PubMed] [Google Scholar]
- McLeod J.D., Uemura R., Rohrman S. Adolescent mental health, behavior problems, and academic achievement. Journal of Health and Social Behavior. 2012;53(4):482–497. doi: 10.1177/0022146512462888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech R.A., Caspi A., Moffitt T.E., Wright B.R.E., Silva P.A. Low socioeconomic status and mental disorders: A longitudinal study of selection and causation during young adulthood. American Journal of Sociology. 1999;104(4):1096–1131. [Google Scholar]
- Miller L.L., Gustafsson H.C., Tipsord J., Song M., Nousen E., Dieckmann N. Is the association of ADHD with socio-economic disadvantage explained by child comorbid externalizing problems or parent ADHD? Journal of Abnormal Child Psychology. 2018;46(5):951–963. doi: 10.1007/s10802-017-0356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health . 2012. VEJ nr 9415 af 01/06/2012 - Gældende (Vejledning om medikamentel behandling af børn og unge med psykiske lidelser) [Google Scholar]
- Mood C. Logistic regression: Why we cannot do what we think we can do, and what we can do about it. European Sociological Review. 2010;26(1):67–82. [Google Scholar]
- Mors O., Perto G.P., Mortensen P.B. The Danish psychiatric central research register. Scandinavian Journal of Public Health. 2011;39(7 suppl):54–57. doi: 10.1177/1403494810395825. [DOI] [PubMed] [Google Scholar]
- Polanczyk G.V., de Lima M.S., Horta B.L., Biederman J., Rohde L.A. The worldwide prevalence of ADHD: A systematic review and metaregression analysis. American Journal of Psychiatry. 2007;164(6):942–948. doi: 10.1176/ajp.2007.164.6.942. [DOI] [PubMed] [Google Scholar]
- Polanczyk G.V., Salum G.A., Sugaya L.S., Caye A., Rohde L.A. Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. The Journal of Child Psychology and Psychiatry and Allied Disciplines. 2015;56(3):345–365. doi: 10.1111/jcpp.12381. [DOI] [PubMed] [Google Scholar]
- Pottegård A., Bjerregaard B., Glintborg D., Hallas J., Moreno S., Glintborg K. The use of medication against attention deficit hyperactivity disorder in Denmark: A drug use study from a national perspective. European Journal of Clinical Pharmacology. 2012;68(10):1443–1450. doi: 10.1007/s00228-012-1265-y. [DOI] [PubMed] [Google Scholar]
- Pottegård A., Bjerregaard B.K., Kortegaard L.S., Zoëga H. Early discontinuation of attention-deficit/hyperactivity disorder drug treatment: A Danish nationwide drug utilization study. Basic and Clinical Pharmacology and Toxicology. 2015;116:349–353. doi: 10.1111/bcpt.12325. [DOI] [PubMed] [Google Scholar]
- Pryor L., Strandberg-Larsen K., Nybo-Anderson A.-M., Hulvej-Rod N., Melchior M., Hulvej N. Trajectories of family poverty and children's mental health: Results from the Danish National Birth Cohort. Social Science & Medicine. 2018;220:371–378. doi: 10.1016/j.socscimed.2018.10.023. August 2018. [DOI] [PubMed] [Google Scholar]
- Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: A systematic review. Social Science & Medicine. 2013;90:24–31. doi: 10.1016/j.socscimed.2013.04.026. [DOI] [PubMed] [Google Scholar]
- Rowland A.S., Skipper B.J., Rabiner D.L., Qeadan F., Campbell R.A., Naftel A.J. Attention-Deficit/Hyperactivity Disorder (ADHD): Interaction between socioeconomic status and parental history of ADHD determines prevalence. The Journal of Child Psychology and Psychiatry and Allied Disciplines. 2018;59(3):213–222. doi: 10.1111/jcpp.12775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell G., Ford T., Rosenberg R., Kelly S. The association of attention deficit hyperactivity disorder with socioeconomic disadvantage: Alternative explanations and evidence. The Journal of Child Psychology and Psychiatry and Allied Disciplines. 2014;55(5):436–445. doi: 10.1111/jcpp.12170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell A.E., Ford T., Russell G. The relationship between financial difficulty and childhood symptoms of attention deficit/hyperactivity disorder: A UK longitudinal cohort study. Social Psychiatry and Psychiatric Epidemiology. 2018;53(1):33–44. doi: 10.1007/s00127-017-1453-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayal K., Prasad V., Daley D., Ford T., Coghill D. ADHD in children and young people: Prevalence, care pathways, and service provision. The Lancet Psychiatry. 2018;5(2):175–186. doi: 10.1016/S2215-0366(17)30167-0. [DOI] [PubMed] [Google Scholar]
- The Danish State Serum Institute (SSI) The Danish State Serum Institute (SSI); Lægemiddelstatistik: 2012. Salget af ADHD medicin fra 2002 - 2011. 1–6. [Google Scholar]
- Thoits P.A. Stress and health. Major findings and policy implications. Journal of Health and Social Behavior. 2010;51(1 suppl):S41–S53. doi: 10.1177/0022146510383499. [DOI] [PubMed] [Google Scholar]
- Tutz G. Binary response models with underlying heterogeneity: Identification and interpretation of effects. European Sociological Review. 2018;34(2):211–221. [Google Scholar]
- UNESCO Institute of Statistics . UNESCO Institute for Statistics; Montreal, Canada: 2012. International standard classification of education. ISCED 2011. [Google Scholar]
- Wallach-Kildemoes H., Skovgaard A.M., Thielen K., Pottegård A., Mortensen L.H. Social adversity and regional differences in prescribing of ADHD medication for school-age children. Journal of Developmental and Behavioral Pediatrics. 2015;36(5):330–341. doi: 10.1097/DBP.0000000000000170. [DOI] [PubMed] [Google Scholar]
- Wickham S., Whitehead M., Taylor-Robinson D., Barr B. The effect of a transition into poverty on child and maternal mental health: A longitudinal analysis of the UK millennium cohort study. The Lancet Public Health. 2017;2(3):e141–e148. doi: 10.1016/S2468-2667(17)30011-7. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) Vol 1. 2016. World health organization. Guidelines for ATC classification and DDD assignment 2016. (WHO collaborating centre for drug statistics methodology). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.