Abstract
Hip joint subluxation and dislocations are very common in cerebral palsy (CP) patients and are directly related to a patient's degree of spasticity. Hip dislocation and subluxation leads to hip pain and difficulty in hygiene maintenance by a caregiver. Most cases require surgical intervention to improve the quality of life in these patients. For many years pelvic and proximal femoral osteotomies with soft tissue releases were the mainstay of treatment for affected hips in CP patients. Recently, hip arthroplasty has been proposed as a very successful operation which provides a pain free and mobile joint in CP patients. The purpose of this review is to evaluate the current evidence for effectiveness of total hip arthroplasty in CP patients.
Keywords: Cerebral palsy, Functional outcomes, Total hip arthroplasty, Pain
1. Introduction
Cerebral Palsy (CP) is a neuromuscular disease caused by perinatal asphyxia, resulting in permanent damage to portions of the brain controlling movement, balance, and resting muscle tone.1,2 CP has many subtypes, depending upon the degree of anoxic insult and resulting symptomology. Spastic CP presents with muscle stiffness and hypertonicity, whereas athetoid and ataxic CP involves writhing movements and poor coordination respectively.1 CP is a non-progressive disorder without any cure. The reported incidence of CP is between 2.7 and 3.2 per 1000 live births.3,4 The first documented description of CP appears in the work of Hippocrates in the 5th century BCE.5 In the 19th century, the spastic diplegia characteristic of CP was named “Little disease” after William John Little, and ultimately “cerebral palsy” by William Osler from the German descriptive, Zerebrale Kinderlahmung (cerebral child-paralysis).6
Musculoskeletal disorders involving the hip are common in children with CP.7 Hip joint subluxation and dislocation are related to the degree of spasticity within periarticular musculature, and range widely from 1% with spastic hemiplegia to 75% with spastic quadriplegia.8 In most patients, spasticity increases gradually, leading first to subluxation followed by dislocation.9 This gives rise to secondary osteoarthritis of the acetabulum and degeneration of the femoral head. Many children with CP develop severe pain and have reduced quality of life and impaired function, including aberrant posturing, sitting, standing, walking, and sleeping.10,11 For the caregiver, this functional impairment at the hip often results in difficulty with perineal hygiene and increased burden of care.11
Orthopaedic surgeons serve a significant role in alleviating hip pain and increasing function in patients with CP, through both surgical and non-surgical modalities. These include, for example, neuromuscular blocking agents, proximal femoral head resection, valgus femoral osteotomy, hip arthrodesis, and total hip arthroplasty (THA), the subject of this analysis. The success of each modality is variable; for instance, the injection of botulinum toxin into the adductor muscles typically provides only temporary relief of pain and spasm around the hip.12 Distal resection arthroplasty has historically yielded the greatest pain relief,13 but increases overall morbidity and renders patients non-weight bearing on the operative limb. Valgus osteotomy of the femur14 can similarly be used to correct hip subluxation and dislocation, and carries the benefit of avoiding long-term immobilization and cast application or skeletal traction. Hip arthrodesis can further serve a palliative role in addressing hip pain and chronic subluxation or dislocation.
Total hip arthroplasty (THA) is likewise an important surgical treatment of CP-related hip disorders, and is the focus of this study. THA can both serve as a palliative procedure in patients with CP, and improve overall function as well. Particularly in spastic CP without weakness and in spastic hemiplegic CP, THA has been shown to often significantly improve patients’ quality of life and decrease associated morbidity. Similarly, several studies have demonstrated positive results with hip reconstructive surgery for CP associated hip instability.15, 16, 17
Total hip arthroplasty is a well-established procedure which preserves patient mobility, unlike resection arthroplasty or arthrodesis, and can prove particularly beneficial in patients with CP who can ambulate preoperatively. The risks of THA have previously been thought to be similar to those in traditional patients, including intra- or post-operative fractures and prosthesis dislocation or loosening, especially in spastic and mentally impaired young patients.18, 19, 20 However, the outcomes of THA have not been widely reported in CP patients, despite THA becoming a more acceptable form of treatment for patients 50 years or younger.21, 22, 23, 24, 25 Buly et al.22 reported a survivorship among CP patients of 95% at 10 years for loosening and 86% with removal for any reason. This is comparable to THA survivorship in the general population (82%–99% at 10 years follow-up).26, 27, 28 To our knowledge, no systematic review to date has looked at the outcomes of THA in CP patients.
We performed a systematic review to determine the functional outcomes, complications and prosthesis survival in CP patients following total hip arthroplasty.
2. Materials and methods
2.1. Literature search
In order to determine overall outcomes of THA in patients with CP, an extensive literature search was completed by two independent researchers (C.A. and A.L) to query what are the functional outcomes, complications, and implant survival of THA in CP patients. Only English literature publications were included in this review. The keywords used for this literature search were as follows:
-
1.
“Cerebral palsy” (MeSH and text word)
-
2.
“Cerebral palsy” AND “hip arthritis”
-
3.
“Cerebral palsy” AND “osteoarthritis hip”
-
4.
“Cerebral palsy” AND “total hip arthroplasty”
-
5.
“Cerebral palsy” AND “total hip replacement”
-
6.
“Cerebral palsy” AND “hip”
-
7.
“Cerebral palsy” AND “hip subluxation”
-
8.
“Cerebral palsy” AND “hip dislocation”
-
9.
“Cerebral palsy” AND “total hip arthroplasty” AND “implant survival”
-
10.
“Cerebral palsy” AND “total hip arthroplasty” AND “functional outcomes”
-
11.
“Cerebral palsy” AND “functional outcomes”
-
12.
“Cerebral palsy” AND “patient reported outcomes”
-
13.
“Cerebral palsy” AND “complications” AND “total hip arthroplasty”
-
14.
“Cerebral palsy” AND “complications” AND “total hip replacement”
-
15.
“Total hip arthroplasty” AND “patient reported outcomes” AND “total hip arthroplasty”
2.2. Eligibility criteria
Articles were chosen for inclusion by both independent researchers on the basis of information provided in the title and abstract. When there was question over eligibility, the entire article was read prior to a decision made regarding inclusion. To resolve any disagreement over eligibility, a third reviewer (A.D.) was consulted in order to reach a majority consensus. Published studies regarding THA for children with CP and hip arthritis, subluxation, dislocation, and dysplasia were included based upon the following criteria:
-
1.
Study must address THA intervention in CP patients
-
2.
Study must include data on 10 or more patients
-
3.
Study must identify the surgical procedure utilized and report functional outcomes or patient reported outcomes, complications, quality of life, and implant survival
-
4.
Study must involve patients with a primary diagnosis of CP and a secondary diagnosis of hip pathology as an indication for surgery
-
5.
Study must detail all approaches and instrumentation used in THA, and enumerate on any simultaneous surgical procedures performed
-
6.
Study must be published originally in the English language
In order to provide background, studies were also included that addressed risk factors associated with poor outcomes following THA in CP patients. Once the inclusion criteria were met, the full text of each study was read, and all relevant data retrieved and analyzed.
3. Results
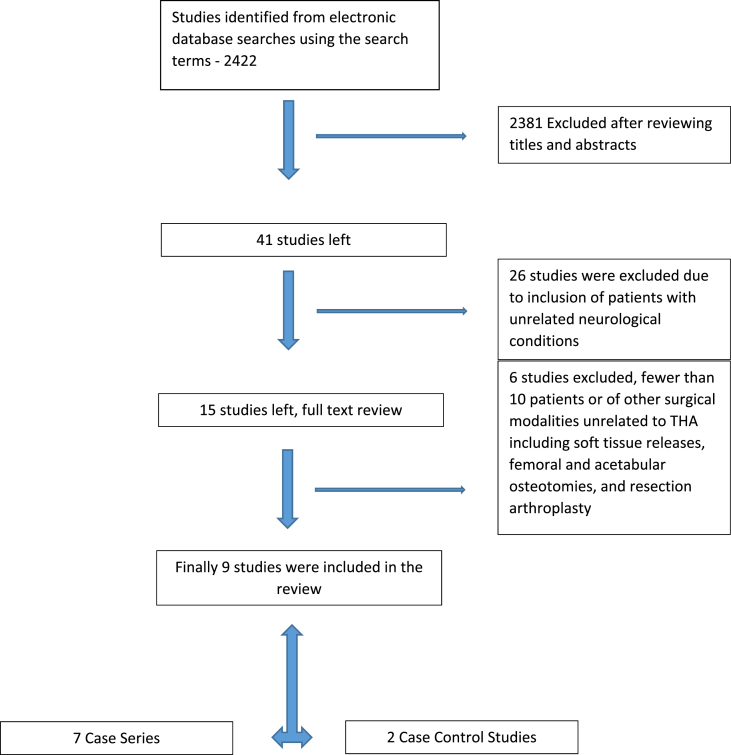
An initial PubMed literature search identified a total of 2422 articles using the above search terms and combinations. After reviewing titles and abstracts, 2381 articles were excluded. Another 26 studies were excluded due to inclusion of patients with unrelated neurological conditions, leaving 15 relevant studies. After a full text review of each article, 6 of these were excluded given their evaluation of fewer than 10 patients or of other surgical modalities unrelated to THA including soft tissue releases, femoral and acetabular osteotomies, and resection arthroplasty, Fig. 1.
Fig. 1.
Flow diagram showing systematic searching process.
A total of 9 articles were ultimately included in this review, per Table 1. Of these, 7 studies represented case series and 2 were retrospective case control studies. All studies included involved 10 or more patients with CP who underwent THA. These studies were published between the years 1986 and 2017. 5 studies were published between 2010 and 2017 and are the most recent studies. Minimum average follow-up was 3.3 years and maximum average follow-up was 10 years. Average age of the youngest cohort was 19.2 (13.5–31.6) years and average age of the oldest cohort was 54 (range, 43 to 61) years in one of the studies. The smallest included study reported data on 10 patients and the largest study reported data on 389 patients. Two retrospective case control studies had totals of 389 and 39 THA procedures, respectively.
Table 1.
Studies included in the review.
| Study | Year | No. of Hips | CP class | Mean age (years) | Avg Follow-up (years) | Indication for surgery | Surgical Approach | Soft tissue release | Complications | Revision | Implant survival |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Root et al. | 1986 | 15 | 6 Spastic paraplegia, 6 triplegia, 1 spastic athetoid, 1 hemiplegia | 31 (16–52) | 6.75 (2.5–1.2) | Painful, degenerated, unstable hip | 2 Posterolateral approach, 13 lateral approach with trochantric osteotomy | 11 adductor and hip-flexor | 1 case breakage of trochanteric wires, 1 dislocation (12 days after surgery), 1 dislocation (4 months) | 1 all component revision and 1 femoral component revision | |
| Buly et al. | 1993 | 19 | 6 Spastic quadriplegia, 5 Diplegia, 3 triplegia, 2 hemiplegia, 1 athetoid quadriplegia, 1 mixed quadriplegia | 30 (16–52) | 10 (3–17) | End-stage hip degeneration, pain, subluxation, dislocation, and limited functional activity | 14 transtrochanteric approach, 5 posterolateral approach | 12 flexor or adductor tendon releases | 2 recurrent dislocations, 3 trochantric bursitis | One stem and one acetabular component | 95% at 10 years for loosening and 86% with removal for any reason |
| Weber et al. | 1999 | 16 | 7 hemiplegia, 4 diplegia, 2 quadriplegia, 2 athetoid quadriplegia, 1 athetoid diplegia | 48.5 (22–79) | 9.7 (2.5–21) | 3 primary OA, 8 secondary OS because of hip dysplasia, 5 failed treatment fracture neck of femur | 8 anterolateral, 7 transtrochanteric, 1 posterolateral | None | one trochanteric and one acetabular fracture intraoperatively, One trochanteric avulsion post-operatively | One aseptic loosening at 13 years | |
| Schroeder et al. | 2010 | 18 | 8 spastic quadriplegia, 3 hemiplegia, 4 diplegic, 1 unclassified | 42.0 (32–58) | 10.0 (2–18) | Painful OA with severely limited functional ability | Transgluteal lateral bauer approach | 5 tenotomy of adductor tendons, 1 lengthening of adductor tendon, 4 psoas-and rectus tendon release, 1 transposition of outer rotators | One hip revision for infection at 12 years, one hip dislocated at 3 months after surgery | 3 cups were revised for aseptic loosening | |
| Raphael et al. | 2009 | 59.0 | 11 athetoid, 21 spastic diplegic, 6 spastic hemiplegic, 18 spastic quadriplegic, 3 triplegic. | 30.7 (14–61) | 9.7 (2–28) | painful, subluxated, or dislocated hip | 14 transtrochanteric approach, 45 posterolateral approach | 28 adductor tendon releases | one trochanteric nonunion, 5 trochanteric bursitis, one pulmonary embolism, 2 infection, and one periprosthetic fracture | 7 acetabular component revisions, and 2 femoral stem component revision | 2-year survival was 95%, and 10-year survivorship was 85%. |
| Sanders et al. | 2013 | 10 | 2 quadriplegic, 2 hemiplegic, 4 diplegic on the lower limbs (two bilateral cases) | 54 (43–61) | 3.3 (1.8–4.7) | 7 painful OA, 1 fracture | Posterolateral approach | One adductor tenotomy | One periprosthetic fracture in hospital after fall a few days after initial surgery | ||
| King et al. | 2015 | 389 | 53 (40–64) | 7 Periprosthetic fractures leading to revision, 6 aseptic loosening, Pain in 5, and 4 dislocations | 22 revisions (10 within one year) | 93.6% 5-year survival | |||||
| Morin et al. | 2016 | 40 | No ambulatory patients | 19.2 (13.5–31.6) | 5.3 (.75–12.25) | Pain confirmed by family or care staff | Lateral with trochanteric osteotomy | 2 septic complications (one treated with lavage and antibiotics and one with revision THA) | 6 revisions | ||
| Houdek et al. | 2017 | 39 | GMFCS type I = 3, type II = 18, type III = 12, type IV = 6 | 49 (21–74) | 7 (2–20) | Hip OA, and failure of non-operative measures to alleviate hip pain | Anterolateral in 19 and Posterior in 20 | Adductor tendon release in 7, and psoas release in 2 | 2 acetabular aseptic loosening, 2 recurrent instability, one deep infection, 3 dislocations, 1 wound dehiscence, one DVT | 5 revisions | 92% at 2 years, 88% at 5 years, 81% at 10 years, and 81% at 15 years |
3.1. Methodological quality
All studies underwent a methodological quality assessment. None of the studies represented high quality review or randomized case control studies. 7 studies were retrospective cohort studies and 2 were retrospective case control studies. One study did not report the classification of CP used, 7 studies used the descriptive classification based upon the spasticity and extremity involvement, and one study used the gross motor functional classification system (GMFCS). Various hip systems were used for performing THA in these studies. The results of these studies are described below under their respective subheadings.
3.2. Indications for surgery
Reported common indications for surgery were a painful hip with degenerative joint disease, an unstable hip joint on exam, evidence of subluxation, dislocation, or hip dysplasia leading to secondary osteoarthritis, failed treatment for neck of femur fracture, limited functional ability, and failure of non-operative measures to alleviate hip pain. One included study did not report the indications for surgery.29 The most common indication was painful degenerative joint disease followed by hip subluxation or dislocation.
3.3. Pain
All of the patients included in this review reported moderate to severe pain; however, the duration of pain varied between studies. In all included studies, pain levels were reported by patients, family members or care givers. When patients were non-ambulatory, pain was reported by caregivers during performance of hygiene or patient positioning. There was no consistent method used to quantify reported pain as a result of hip pathology, in part due to the inability of many patients with CP to convey the level of pain experienced. Only one study by Schroeder et al.30 used the narrative analogue pain scale (NAS) to quantify pain. All 9 studies reported a significant improvement in pain in nearly all patients who underwent THA, with the least successful rate reported by Weber et al.25 at 87% pain relief. This last study involved a cohort of 16 patients, with 3 patients reporting mild to moderate pain at their most recent recorded postoperative visit. The pooled findings of these 9 studies strongly suggest that pain relief can be achieved after total hip arthroplasty in CP patients. This is consistent with the conclusions of the three most persuasive studies, those by Houdek et al.,31 Schroeder et al.,30 and Weber et al.,25 each of which reported significant improvement in pain experienced by CP patients after THA.
3.4. Surgical approach
The most commonly utilized surgical approach was the lateral approach with trochanteric osteotomy followed by posterolateral and anterolateral approaches. There was no consistency and consensus regarding the appropriate approach to the hip joint in CP patients. King et al.29 did not comment upon the approach used in their cohort. Overall, the 9 studies suggested that the surgical approach is directed both by severity of CP and preoperative deformity at the hip joint. Of note, the lateral approach combined with trochanteric osteotomy consistently resulted in complications with the osteotomy site.24,25,32
3.5. Concomitant soft tissue procedures
6 of the 9 included studies discussed concomitant soft tissue release and bony procedures at the time of THA. 2 additional studies did not report on adjunct soft tissue procedures, and the final study by Weber et al.25 specified that no soft tissue or bony procedure was done in conjunction with each THA analyzed. In those patients who underwent concomitant procedure, the most commonly performed were a tenotomy of the adductors and hip flexors, including iliopsoas release. The decision to do an additional soft tissue procedure depended in each case upon the extent of contractions around the hip joint.
3.6. Functional outcomes
All of the included studies discussed functional outcomes as one of their primary endpoints, but used different measures to assess functional improvement. In 5 of the included studies, the functional status was reported along a continuum including function restoration to pre-pain level, improved but not fully restored function, no change in function, and only improvement in hygienic care.22,24,25,30,32 Schroeder et al.5 reported that out of 18 patients, 6 patients reported improved function, 4 reported no problem with pre- or postoperative function, 1 reported no change in function, and 7 had improved hygienic care. Similarly, King et al.29 used patient reported outcomes (PROCs) data to report improvement in functional status. This study was a retrospective joint registry-based case control study. King noted that the PROCs were improved in the CP cases compared to the controls, although the improvement was not significant. Morine et al.34 assessed functional status by measuring improvement in flexion at the hip joint, finding a significant improvement in hip flexion after THA when compared to pre-operative flexion. Houdek et al.31 used the Harris hip score as a measure of functional outcomes, and found a significant improvement in functional Harris hip score in CP patients after THA. Weber et al.25 in their case series reported functional improvement in 79% of CP patients following THA. The only study to report poor functional outcomes was that conducted by Sanders et al.,33 which used the SF-36 questionnaire to broadly study physical health and functioning compared to a standard SF-36. They noted patients with CP to have consistently lower SF-36 scores overall.
3.7. Revision
Studies varied in terms of the number of THA cases which required revision. Revision rates of greater than 15% were reported by Schroeder et al.,30 Raphael et al.,32 and Morin et al.34 3 studies noted lower revision rates of between 10% and 15%.22,24,31 Weber et al.,25 and King et al.29 reported a revision rate of 6.3% and 5.7%, respectively. Sanders et al.33 reported a zero percent revision rate in their series of 10 cases, noting that they used dual mobility acetabular cups in all their hip arthroplasties, and that their longest follow-up was 4.7 years.
3.8. Prosthetic hip survival
Implant survival was reported by 4 of the 9 studies in our review. King et al.29 reported a 93.6% 5 year implant survival in their retrospective case control study in the CP patient population, a number comparable to that seen in THA for osteoarthritis in their control cohort. Raphael et al.32 reported a 2 year and 10 year survival of 95% and 85%, respectively, among 59 CP patients after THA. Similarly, Houdek et al.31 in their case series of 39 hips reported a survivorship of 92% at 2 years, 88% at 5 years, 81% at 10-years, and 81% at 15 years. Buly et al.22 reported a survivorship of 95% at 10 years for loosening and 86% for removal for any reason.
3.9. Complications
The most common reported complication among all studies included in this review was recurrent prosthetic hip dislocation. Periprosthetic hip fracture was the second most common reported complication. The latter primarily occurred intraoperatively or within 6 months of the index THA. Other complications reported were aseptic loosening, periprosthetic joint infections (PJI), complications related to the trochanteric osteotomy (hardware failure, nonunion, trochanteric bursitis, and malunion), heterotopic ossification, wound dehiscence, and deep vein thrombosis (DVT). Most of the complications listed required return to the operating room for management.
The highest complication rate was observed by Buly et al.22 in their 19 hip case series. They noted 5 complications (26% of their patient cohort), including 2 patients with recurrent dislocations, and 3 patients with trochanteric bursitis. Houdek et al.31 demonstrated similar findings in 39 hips, describing 10 complications over an average follow-up period of 7 years. These included 2 instances of acetabular cup aseptic loosening, 2 cases of recurrent instability, and 3 dislocations, in addition to wound dehiscence, DVT and periprosthetic infection. Conversely, Morin et al.34 reported only 2 complications, both septic joints, in a 40 hip case series, similar findings to King et al.29 in their series of 389 hips.
4. Discussion
Painful hip pathology is a major concern in patients suffering from cerebral palsy. Many children with cerebral palsy have normal hip joints at birth, but develop pathology and resulting pain at an early age. Their symptoms may arise directly from dysplasia, subluxation, dislocation, or from resulting secondary osteoarthritis. Primary osteoarthritis is also a major concern in this patient population. Patients with CP typically undergo many soft tissue and bony procedures for hip pain. Many procedures, such as tendon releases for spasticity, or proximal femoral osteotomy for subluxation, are palliative procedures associated with significant morbidity. These procedures often alleviate a degree of pain, but rarely increase function, as the above literature has shown. Of note, all of the patients included in this review had undergone a soft tissue or bony procedure during the course of their treatment prior to THA.
Our systematic review was performed to describe the outcomes and complications of total hip arthroplasty in adolescent to adult CP patients with moderate to severe hip pain. All the studies included in our review suggest that total hip arthroplasty is a successful procedure to alleviate debilitating hip pain and to increase hip function or ease of caregiving in patients with CP. Based on current literature, THA is a largely successful procedure in this patient population, and can be safely considered as a primary management strategy alongside possible adjunctive soft tissue or bony procedures.
The majority of our 9 studies involved retrospective cohorts, with two retrospective case control studies. Our literature search found no relevant controlled trials. All studies and their data were assessed for methodological quality and statistical significance.35,36
The most common surgical approaches utilized in our included studies were the lateral trans-trochanteric, posterolateral, and anterolateral approaches. As noted above, complications included periprosthetic fracture or infection, hardware failure, trochanteric bursitis, or non- or malunion at the trochanteric osteotomy site.25,29,32,33
Our most significant finding was the consistent majority improvement of functional outcomes regardless of the measurement tool utilized. Despite the lack of consensus in current literature regarding how to report functional outcomes in patients with CP, our findings showed clear overall functional improvement in every cohort examined. In both of the retrospective studies included, postoperative function was assessed and compared to preoperative scores and functional improvement in control cohorts, and in both cases, demonstrated similar significant improvement.29,31
Implant survivorship, previously a concern in patients with CP, was very favorable across our included studies. In the two cohorts that examined long-term survivorship at 10 years or more, both groups of implants showed greater than 80%, comparable to that seen in a standard patient population. As Sanders et al. noted in one of the smaller studies, implant design, such as dual mobility acetabular cups, may decrease the rate of component failure or dislocation.33
We acknowledge some limitations to this review. First, the patient population with CP demonstrates significant variability of symptomatology and anatomical pathology; hence, results from a small cohort may not be generalizable to all patients with CP. Similarly, the included studies were not differentiated by patient age, implant design, surgical approach, or functional outcome assessment utilized, all of which may have bearing on the ultimate success of the procedure. Specifically, the majority of included studies did not quantify pain levels by objective, patient-reported data. In addition, our literature search was restricted to those studies indexed on PubMed and published in the English language. Finally, perioperative care for the patient with CP, including adjunctive surgical and nonsurgical treatment modalities, can prove critical to the success of performing a THA for pain relief or functional improvement. Because of interpatient variation, perioperative care is challenging to objectively assess.
5. Conclusion
Our review supports the conclusion that undergoing total hip arthroplasty has an overall positive result profile in patients with cerebral palsy. THA, performed as an index procedure or in conjunction with adjunctive soft tissue and bony procedures, can significantly alleviate pain with sitting and shifting, and may ease the caregiver's burden of hygiene care. More prospective studies are needed in this area to further examine the patient profiles best suited to THA, and to identify positive or negative prognostic factors relating to postoperative complications.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
None.
Contributor Information
Curtis T. Adams, Email: docadamsortho@gmail.com.
Akshay Lakra, Email: lakraakshay@gmail.com, akshayf@amc.edu.
References
- 1.Palsy Cerebral. National institute of neurological disorder and stroke; July 2013. Hope through Research. [Google Scholar]
- 2.Oskoui M, Coutinho F, Dykeman J, Jette N, Pringsheim T. An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol. 55(6): 509-519. Doi: 10.1111/dmcn.12080. [DOI] [PubMed]
- 3.Park M.S., Kim S.J., Chung C.Y., Kwon D.G., Choi I.H., Lee K.M. Prevalence and lifetime healthcare cost of cerebral palsy in South Korea. Health Pol. 2011 May;100(2-3):234–238. doi: 10.1016/j.healthpol.2010.09.010. Epub 2010 Oct 16. [DOI] [PubMed] [Google Scholar]
- 4.Rosen M.G., Dickinson J.C. The incidence of cerebral palsy. Am J Obstet Gynecol. 1992 Aug;167(2):417–423. doi: 10.1016/s0002-9378(11)91422-7. [DOI] [PubMed] [Google Scholar]
- 5.Panteliadis C., Panteliadis P., Vassilyadi F. Hallmarks in the history of cerebral palsy: from antiquity to mid-20th century. Brain Dev. Apr 2013;35(4):285–292. doi: 10.1016/j.braindev.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 6.What Is Cerebral Palsy? the Cerebral Palsied Association of the Philippines Inc.
- 7.Poutney T., Green E.M. Hip dislocation in cerebral palsy. BMJ. 2006;332:772–775. doi: 10.1136/bmj.332.7544.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scrutton D., Baird G., Smeeton N. Hip dysplasia in bilateral cerebral palsy: incidence and natural history in children aged 18 months to 5 years. Dev Med Child Neurol. 2001 Sep;43(9):586–600. doi: 10.1017/s0012162201001086. [DOI] [PubMed] [Google Scholar]
- 9.Reimers J. The stability of the hip in children. A radio-logical study of the results of muscle surgery in cerebral palsy. Acta Orthop Scand Suppl. 1980;184:1–100. doi: 10.3109/ort.1980.51.suppl-184.01. [DOI] [PubMed] [Google Scholar]
- 10.Knapp D.R., Cortes H. Untreated hip dislocation in cerebral palsy. J Pediatr Orthop. 2002;22:668–671. [PubMed] [Google Scholar]
- 11.Krebs A., Srobl W.M., Grill F. Neurogenic hip dislocation in cerebral palsy: quality of life and results after hip reconstruction. J Child Orthop. 2008;2:125–131. doi: 10.1007/s11832-008-0080-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lundy CT, Doherty GM, Fairhurst CB. Botulinum toxin type A injection can be an effective treatment for pain in children with hip spasms and cerebral palsy. Dev Med Child Neurol; 51:705-710. [DOI] [PubMed]
- 13.Boldingh E.J., Jacobs-van der Bruggen M.A., Bos C.F., Lankhorst G.J., Bouter L.M. Determinants of hip pain in adult patients with severe cerebral palsy. J Pediatr Orthop B. 2005;14:120–125. doi: 10.1097/01202412-200503000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Schanz A. The treatment of outdated congenital hip dislocation. Z Orthop. 1921;42:442–444. [Google Scholar]
- 15.Barakat M.J., While T., Pyman J., Gargan M., Monsell F. Bilateral hip reconstruction in severe whole-body cerebral palsy: ten-year follow-up results. J Bone Jt Surg Br. 2007 Oct;89(10):1363–1368. doi: 10.1302/0301-620X.89B10.18446. [DOI] [PubMed] [Google Scholar]
- 16.Howard C.B., Mckibbin B., Williams L.A., Mackie I. Factors affecting the incidence of hip dislocation in cerebral palsy. J Bone Jt Surg Br. 1985 Aug;67(4):530–532. doi: 10.1302/0301-620X.67B4.4030844. [DOI] [PubMed] [Google Scholar]
- 17.Huh K., Rethlefsen S.A., Wren T.A., Kay R.M. Surgical management of hip subluxation and dislocation in children with cerebral palsy: isolated VDRO or combined surgery? J Pediatr Orthop. 2011 Dec;31(8):858–863. doi: 10.1097/BPO.0b013e31822e0261. [DOI] [PubMed] [Google Scholar]
- 18.Chandler H.P., Reineck F.T., Wixson R.L., McCarthy J.C. Total hip replacement in patients younger than thirty years old: a five-year follow-up study. J Bone Jt Surg Am. 1981;63:1426–1434. [PubMed] [Google Scholar]
- 19.Dorr L.D., Kane T.J., 3rd, Conaty J.P. Long-term results of cemented total hip arthroplasty in patients 45 years old or younger: a 16-year follow-up study. J Arthroplasty. 1994;9:453–456. doi: 10.1016/0883-5403(94)90090-6. [DOI] [PubMed] [Google Scholar]
- 20.Ranawat C.S., Atkinson R.E., Salvati E.A., Wilson P.D., Jr. Conventional total hip arthroplasty for degenerative joint disease in patients between the ages of forty and sixty years. J Bone Jt Surg Am. 1984;66:745–752. [PubMed] [Google Scholar]
- 21.Blake S.M., Kitson J., Howell J.R., Gie G.A., Cox P.J. Constrained total hip arthroplasty in a pediatric patient with cerebral palsy and painful dislocation of the hip: a case report. J Bone Jt Surg Br. 2006;88:655–657. doi: 10.1302/0301-620X.88B5.17206. [DOI] [PubMed] [Google Scholar]
- 22.Buly R.L., Huo M., Root L., Binzer T., Wilson P.D., Jr. Total hip arthroplasty in cerebral palsy: long-term follow-up results. Clin Orthop Relat Res. 1993;296:148–153. [PubMed] [Google Scholar]
- 23.Ries M.D., Wolff D., Shaul J.A. Hip arthroplasty in mentally impaired patients. Clin Orthop Relat Res. 1994;308:146–154. [PubMed] [Google Scholar]
- 24.Root L., Goss J.R., Mendes J. The treatment of the painful hip in cerebral palsy by total hip replacement or hip arthrodesis. J Bone Jt Surg Am. 1995;77:703–712. [PubMed] [Google Scholar]
- 25.Weber M., Cabanela M.E. Total hip arthroplasty in patients with cerebral palsy. Orthopedics. 1999;22:425–427. doi: 10.3928/0147-7447-19990401-12. [DOI] [PubMed] [Google Scholar]
- 26.Callaghan J.J., Forest E.E., Sporer S.M., Goetz D.D., Johnston R.C. Total hip arthroplasty in the young adult. Clin Orthop Relat Res. 1997;344:257–262. [PubMed] [Google Scholar]
- 27.de Jong P.T., de Man F.H., Haverkamp D., Marti R.K. The long-term outcome of the cemented weber acetabular component in total hip replacement using a second-generation cementing technique. J Bone Jt Surg Br. 2009;91:31–36. doi: 10.1302/0301-620X.91B1.19748. [DOI] [PubMed] [Google Scholar]
- 28.Makela K., Eskelinen A., Pulkkinen P., Paavolainen P., Remes V. Cemented total hip replacement for primary osteoarthritis in patients aged 55 years or older: results of the 12 most common cemented implants followed for 25 years in the Finnish Arthroplasty Register. J Bone Jt Surg Br. 2008;90:1562–1569. doi: 10.1302/0301-620X.90B12.21151. [DOI] [PubMed] [Google Scholar]
- 29.King G., Hunt L.P., Wilkinson J.M., Blom A.W. Good outcome of total hip replacement in patients with cerebral palsy: a comparison of 389 patients and 425,813 controls from the national joint registry for England and wales. Acta Orthop. 2016;87(2):93–99. doi: 10.3109/17453674.2015.1137439. Epub 2016 Feb 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schroeder K., Hauck C., Wiedenhofer B., Braatz F., Aldinger P.R. Long-term results of hip arthroplasty in ambulatory patients with cerebral palsy. Int Orthop. 2010;34:335–339. doi: 10.1007/s00264-009-0771-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Houdek M.T., Watts C.D., Wyles C.C., Trousdale R.T., Milbrandt T.A., Taunton M.J. Total hip arthroplasty in patients with cerebral palsy. A cohort study matched to patients with osteoarthritis. J Bone Jt Surg Am. 2017;99:488–493. doi: 10.2106/JBJS.16.00528. [DOI] [PubMed] [Google Scholar]
- 32.Raphael B.S., Dines J.S., Akerman M., Root L. Long-term followup of total hip arthroplasty in patients with cerebral palsy. Clin Orthop Relat Res. 2010;468:1845–1854. doi: 10.1007/s11999-009-1167-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sanders R.J.M., Swierstra B.A., Goosen J.H.M. The use of dual-mobility concept in total hip arthroplasty patients with spastic disorders. No dislocations in a series of ten cases at midterm follow-up. Arch Orthop Trauma Surg. 2013;133:1011–1016. doi: 10.1007/s00402-013-1759-9. [DOI] [PubMed] [Google Scholar]
- 34.Morin C., Ursu C., Delecourt C. Total hip replacement in young non-ambulatory cerebral palsy patients. J Orthop Traumatol: Surg Res. 2016;102 doi: 10.1016/j.otsr.2016.07.010. 854-849. [DOI] [PubMed] [Google Scholar]
- 35.Steultjens E.M.J., Dekker J., Bouter L.M., van de Nes J.C.M., Lambregts B.L.M., van den Ende C.H.M. Occupational therapy for children with cerebral palsy: a systematic review. Clin Rehabil. 2004;18:1–14. doi: 10.1191/0269215504cr697oa. [DOI] [PubMed] [Google Scholar]
- 36.Van Tulder M.W., Assendelft W.J.J., Koes B.W., Bouter L. Method guidelines for systematic reviews in the Cochrane Collaboration back review group for spinal disorders. Spine. 1997;22:2323–2330. doi: 10.1097/00007632-199710150-00001. [DOI] [PubMed] [Google Scholar]