Abstract
Purpose
To objectively evaluate the effect different management strategies have on the following post-surgical outcomes.
Methods
The PubMed, Embase and Cochrane Library databases were reviewed for articles published between January 1st, 2000 to September 18, 2019 that reported on studies comparing techniques for handling the capsule during hip arthroscopy. After applying the inclusion and exclusion criteria, our final analysis included 10 studies. In total, these articles included 1556 hips. The following capsular management strategies were implemented: complete repair (n = 444; 28.53%), partial repair (n = 32; 2.06%), plication (n = 223; 14.33%) and release/no-repair (n = 857; 55.08%). A meta-analysis was performed on outcomes presented in three or more studies using sufficient pooled statistical analysis data.
Results
Our meta-analysis demonstrated an improvement in the HOS-SS with capsular repair without being statistically significant (95%CI [-6.71, 8.21], p = 0.06). However, a significant improvement in the mHHS was detected with capsular repair (95%CI [-1.37, 9.39], p = 0.03). Of the Four studies evaluating HOS-ADL, two reported improved outcomes with capsular repair (p < 0.05 for both) while the other two reported no significant difference. While mixed results were demonstrated for reoperation rates, no difference was found across capsular management strategies regarding radiological outcomes, NAHS (all p-values >0.05) pain (p > 0.05), flexion (p > 0.05), and patient satisfaction (p > 0.05).
Conclusion
Capsular repair has the potential to improve patient reported outcomes after hip arthroscopy. While there was no consensus in literature, studies consistently reported similar or superior outcomes in the capsular repair cohorts compared to capsular release. Further randomized controlled studies need to be conducted for better evaluation of outcomes.
Keywords: Hip arthroscopy, Capsule, Repair, Plication, Patient reported outcomes (PROs), Capsular management
1. Introduction
Non-arthritic hip pathologies, such as femoroacetabular impingement (FAI) and labral tears, are frequently managed through hip arthroscopy. Partly due to the development of less invasive surgical techniques, procedural volume for hip arthroscopies has surged over the past decade.1,2 However, while these hip procedures have generally yielded high rates of success,3 there has recently been an increased incidence of reported iatrogenic instability events reported in the literature. Specifically, these include rapidly progressive osteoarthritis, as well as joint subluxation or dislocation, following hip arthroscopy.4, 5, 6, 7, 8 Thus, in order to maintain positive outcomes, there has been a growing interest in ways to prevent these complications following hip arthroscopy. Capsular management strategies have been extensively explored in this domain9, 10, 11, 12, 13, 14.
The hip capsule is comprised of the iliofemoral, ischiofemoral, and pubofemoral ligaments which form a capsuloligamentous envelope that encloses the hip joint.10,14,15 Frequently, the capsule is incised in order to obtain atraumatic entry into the joint and to allow for adequate maneuverability of surgical instruments.16, 17, 18 Due to the technically demanding nature of capsular repair,19 the capsule is traditionally left open, or released.20 However, given that the capsule has been shown to contribute significantly to joint stability,11,13,21 it has been suggested that capsular closure may restore native biomechanical properties following arthroscopic procedures.21,22 Options for closure include complete repair, partial repair, and plication, the tightening of the hip capsule that results from thermal capsular shrinkage. Despite the possible benefits that result from closure, there is lack of consensus among surgeons regarding which strategy should be implemented.
As hip arthroscopy procedures continue to rise, identifying factors that can maintain positive outcomes has become essential. Much interest has focused on management of the hip capsule intra-operatively. However, there is a paucity of information regarding which management strategy yields superior outcomes while also reducing complication risk. Therefore, the purpose of this systematic review was to objectively evaluate the effect different management strategies have on post-surgical outcomes.
2. Methods
2.1. Search strategy
The PubMed, Embase and Cochrane Library electronic databases were comprehensively reviewed for all articles published between January 1st, 2000 to September 18, 2019 that reported on studies comparing techniques for handling the capsule during hip arthroscopy procedures. The following keywords were used in our search along with the AND and OR Boolean operators: “hip”; “arthroscopy”; “outcomes”; “capsulotomy”; “repair”.
2.2. Eligibility criteria
We utilized the following as inclusion criteria: 1) English, full-text articles must be available and 2) articles comparing the outcomes of capsulotomy (capsular release) without further intervention versus partial repair, 3) complete repair, 4) plication, or 5) comparing different repair techniques. Exclusion criteria were: 1) duplicates between the databases, 2) cadaveric studies, 3) single or double case reports, 4) systematic reviews, 5) studies utilizing non-arthroscopic capsular interventions and 6) studies that do not provide measurable functional or radiographic outcomes. A meta-analysis was conducted if a single outcome was; 1) described using sufficient pooled analysis data (mean, standard deviation and sample size), and 2) reported in three or more of the included studies. Of the multiple outcomes reported, a meta-analysis was conducted on a total of two outcomes deemed to have satisfied the aforementioned pre-requisites; the modified Harris Hip Score (mHHS) and the Sports-Specific sub-domain of the Hip Outcome Score (HOS-SS). The remaining outcomes which did not satisfy the criteria for meta-analysis, were discussed without being statistically analyzed.
2.3. Data extraction
Two independent investigators conducted the literature search utilizing the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guidelines. The senior author, a board certified orthopaedic surgeon, arbitrated on disagreements. Outcomes of interest were isolated in a tabulated spreadsheet prior to their incorporation into the current review.
2.4. Quality assessment
All included studies were stratified according to the level of evidence. Furthermore, the Methodological Index for Non-Randomized Studies (MINORS) scale was utilized to assess the implemented methodology within the included studies. The MINORS criteria for comparative studies comprise twelve elements, each conferring a score between zero and two with a maximum total of 24 points.
2.5. Statistical analysis
Two independent reviewers carried out the data extraction process from the included articles. The extracted data was then analyzed using Review Manager 5.3 (Cochrane Collaboration, Oxford, UK). Continuous outcomes were assessed using weighted mean differences (WMD), while dichotomous outcomes were evaluated by calculating the odds ratio (OR). A confidence interval of 95% (95%CI) was used for both types of outcomes. Heterogeneity of the analyzed data was evaluated using the I2 and chi-squared tests. High data heterogeneity was defined as I2>50% and warranted the implementation of a random effects model for analysis. On the other hand, in case of low data heterogeneity (I2<50%), a fixed effects model was used for the analysis.23
3. Results
3.1. Study selection
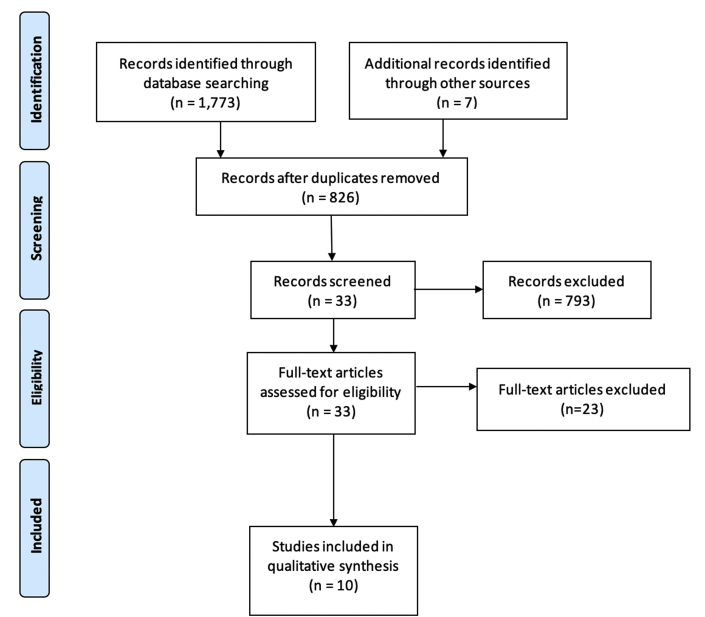
Our initial query resulted in a total of 1773 articles. Following the removal of 947 articles, 826 unique studies were identified. Inclusion and exclusion criteria were then applied. This resulted in a total of 33 being considered further. After each manuscript was thoroughly evaluated, 10 articles remained for consideration. Given that stepwise review of each article's references did not yield any additional related studies, our final analysis consisted of 10 studies17,19,20,24, 25, 26, 27, 28, 29, 30 (Table 1). In total, these articles reported on 1556 hips. The following capsular management strategies were implemented: complete repair (n = 444; 28.53%), partial repair (n = 32; 2.06%), plication (n = 223; 14.33%) and release/no-repair (n = 857; 55.08%). The selection process for included studies is available in (Fig. 1).
Table 1.
Studies included in our analysis.
| Study | Level of Evidence | Capsular Treatment | Sample Size (Hips) | Follow-Up | Outcomes Assessed |
|---|---|---|---|---|---|
| Amar et al. (2015)2 | III | Repair vs. Non-Repair | 100 (Repair: n = 50; Non-Repair: n = 50) | 2-weeks | Occurrence of heterotrophic ossification (HO) |
| 6-weeks | |||||
| 6-months | |||||
| 1-year | |||||
| Atzmon et al. (2019)4 | II | Repair vs. Non-Repair | 64 (Repair: 35; Non-repair: 29) | Mean: Repair: 40.4 months; Non-Repair: 60.7 months | mHHS |
| HOS | |||||
| Patient satisfaction | |||||
| Bolia et al. (2019)7 | III | Repair vs. Non-Repair | 126 (Repair: n = 42; Non-Repair: 84) | Mean: Repair: 6.4 ± 2.3 years Non-repair: 7.3 ± 2.7 years |
mHHS |
| HOS-ADL | |||||
| HOS-SS | |||||
| Patient satisfaction | |||||
| Rates of conversion to THA | |||||
| Domb et al. (2015)12 | IV | Repair vs. Release | 403 (Repaired: n = 168; Unrepaired: n = 235) | Mean: Repaired: 2.09 ± 0.26 years Unrepaired: 2.23 ± 0.36 years |
mHHS |
| HOS-ADL | |||||
| HOS-SS | |||||
| NAHS | |||||
| VAS | |||||
| Patient satisfaction | |||||
| Domb et al. (2018)10 | III | Repair vs. Release | 130 (Repair: n = 65; Release: n = 65) | Mean: Repair: 64.8 ± 4.2 months Release: 75.7 ± 8.6 |
mHHS |
| HOS-SS | |||||
| VAS | |||||
| Patient satisfaction | |||||
| Need for revision/THA | |||||
| Frank et al. (2014)18 | III | Partial vs. Complete | 64 (Partial: n = 32; Complete: n = 32) | Mean: 29.9 months (Range: 24.7–35.4 months) | mHHS |
| HOS-ADL | |||||
| HOS-SS | |||||
| Patient satisfaction | |||||
| Strickland et al. (2018)45 | I | Repair vs. Release | 30 (Repair: n = 15, Release: n = 15) | 6-weeks 24-weeks |
Size of capsular defect Capsular thickness Continuity of capsule |
| Larson et al. (2014)25 | III | Plication - Revision vs. Release - Primary | 305 (Plication -Revision: n = 85; Release – Primary: n = 220) | 2-weeks | mHHS |
| 6-weeks | VAS | ||||
| 3-months | ROM | ||||
| 6-months | AA | ||||
| 1-year | CEA | ||||
| Larson et al. (2016)27 | III | Repair vs. Plication vs. Release | 88 (Repair: n = 37; Plication: n = 32; Release: n = 19) | Mean: 22.7 months | mHHS VAS |
| Newman et al.35 | II | Plication vs. Release | 246 (Plication: n = 106; No Plication n = 140) | 2-years | mHHS |
| HOS-ADL | |||||
| HOS-SS | |||||
| Patient satisfaction |
mHHS: modified Harris Hip Score; HOS: Hip Outcome Score; ADL: Activities of Daily Living; SS: Sports Score; VAS: Visual Analog Scale; NAHS: Non-Arthritic Hip Score; AA: Alpha Angle; CEA: Center Edge Angle; ROM: Range of Motion; THA: Total Hip Arthroplasty.
Fig. 1.
PRISMA diagram for study selection demonstrating the number of studies identified, screened, assessed for eligibility and the final number of included studies (n = 10).
3.2. Quality assessment
The level of evidence of the included studies is as follows: One level I,19 two level II,17,31 six level III24,28, 29, 30,32,33 and one level IV20 (Table 1). MINORS scale ranged between 16 and 21 with an average of 17.8 indicating an overall acceptable quality of evidence34
3.3. Outcome analysis
3.3.1. Hip Outcome Scores
A majority of the included studies (n = 6) reported on the Hip Outcome Score (HOS),17,20,26, 27, 28, 29 with four studies reporting on the activities of daily living sub-scale (HOS-ADL),20,26, 27, 28 and four studies reporting on the sports sub-scale (HOS-SS).20,27, 28, 29 One study did not stratify by subscale and reported on the total HOS score instead.17 Together, there was a lack of homogeneity regarding which capsular management strategy yielded the highest HOS values.
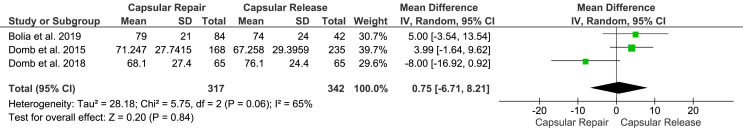
Among the reported HOS subsets, HOS-SS alone satisfied the criteria for meta-analysis. Specifically, three of the four studies comparing post-operative HOS-SS between capsular repair and capsular release cohorts were analyzed.20,28,29 A random effects model was utilized for the analysis due to the high heterogeneity exhibited within the reported data (I2 = 65%). Despite having a better overall trend, capsular repair did not demonstrate a significantly higher HOS-SS compared to capsular release (95%CI [-6.71, 8.21], p = 0.06) (Fig. 2).
Fig. 2.
Forest plot to assess the hip outcomes score sports-specific subscale (HOS-SS) demonstrating better trends in favor of capsular repair without reaching statistical significance.
Within the studies analyzing HOS-SS, Domb et al. reported a trend favoring capsular repair, with no significant difference being found between repair and release cohorts (p > 0.05).20 This was further shown by the authors in their later study, with no differences between the two cohorts at minimum 5-years post-op (repair: 76.1 ± 24.4 vs. non-repair: 68.1 ± 27.4; p = 0.32).29 Furthermore, Bolia et al. reported no difference between repair (mean: 79 ± 21) and non-repair (74 ± 24) cohorts (p = 0.363).28 However, the authors did report a higher percentage of patients in the repair group that reached MCID (77% vs. 55%; p = 0.036).28
Interestingly, complete repair appeared to yield improved outcomes for HOS-SS compared to partial repair in the analysis by Frank et al.27 Specifically, the complete repair cohort yielded higher HOS-SS values than patients with partially repaired capsule at 6-months (72.2 ± 16.1 vs. 63.8 ± 31.1, respectively; p = 0.039), 1-year (82.5 ± 10.7 vs. 72.7 ± 14.7, respectively; p = 0.006), and 2.5 years (87.3 ± 8.3 vs. 83.6 ± 9.6, respectively; p = 0.001).27 Furthermore, there were significant increases for the complete repair cohort between 6-months and 1-year (p < 0.0001) and between 1-year and 2.5 years (p = 0.017).27 For the partial repair cohort, while there was a significant improvement between the earlier time frame (p < 0.0001) there was no difference found between 1-year to 2.5 years follow-up intervals (p = 0.059).27
Evaluating HOS-ADL, Bolia et al. found significantly higher scores for the repair cohort compared to patients who did not have their capsule repaired (91 ± 11 vs. 84 ± 14; p = 0.010).28 The authors additionally reported that there was a higher percentage of patients in the repair cohort that reached minimal clinical important difference (MCID) (71% vs. 52%; p = 0.002).28 Similarly, Domb et al. found that patients with capsular repair yielded higher mean (±SD) post-operative scores compared to the release cohort (86.1085 ± 17.2680 vs 82.2186 ± 18.5467; p = 0.0336). Additionally, the probability of reporting good or excellent outcomes, was significantly higher for the capsular repair cohort (75% vs. 66%; OR: 1.586, 95% CI: 1.018–2.472; p = 0.0417). However, when adjusting for variables such as sex, age, and acetabular labrum articular classification, there were no differences found between the two management strategies (p > 0.05).
Newman et al. was the only study that evaluated the effects of plication on HOS-ADL scores.26 In their cohort of revision patients, patients with capsular plication were more likely to report HOS-ADL scores ≥10 compared to patients without plication (75% vs. 31%; p = 0.001).26
When comparing partial to complete closure, Frank et al. found no differences in HOS-ADL scores.27 Specifically, there was no difference between the partial closure cohort and the complete closure cohort at 6-months, 1-year, and 2.5 years following the arthroscopy procedure (all p-values >0.05).27
When evaluating the total HOS, Atzmon et al. found no difference between closure and non-closure cohorts post-operatively (87.2 vs. 85.4; p = 0.718).17 Both cohorts experienced significant improvements following the hip arthroscopy procedure (p > 0.001).17
3.3.2. Modified Harris Hip Score
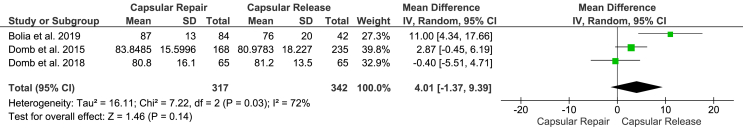
Differences in the modified Harris Hip Scores (mHHS) between capsular management strategies were evaluated in five of the included studies.17,20,24,25,28,29 Variable results were demonstrated in the four Studies comparing the postoperative mHHS obtained after capsular repair versus release.17,20,28,29 However, by incorporating data from three studies found to be eligible for meta-analysis,20,28,29 a significantly higher mHHS was demonstrated in favor of capsular repair (95%CI [-1.37, 9.39], p = 0.03). These results were obtained through applying a random effects model of analysis due to the high heterogeneity of the presented data (I2 = 72%) (Fig. 3). Although not sufficient for meta-analysis, data from the two studies comparing capsular plication to capsular release similarly demonstrated superior outcomes in the capsular plication cohorts.24,25
Fig. 3.
Forest Plot to Assess the Modified Harris Hip Score (mHHS) Demonstrating Significantly Improved mHHS with Capsular Repair Compared to Capsular Release.
Comparing capsular closure to non-closure, Atzmon et al. reported no significant differences in both pre-operative (58.4 vs. 63.2, respectively; p = 0.223) and post-operative (88.7 vs. 85.7, respectively; p = 0.510) mHHS values.17 Similarly, at a minimum 2-year follow-up, Domb et al. reported no differences between repair and non-repair cohorts for mHHS (p > 0.05).20 Additionally, patients with capsular repair did not have significantly greater odds of developing good or excellent outcomes (71% vs. 62%; OR: 1.507, 95% CI: 0.986–2.304, p = 0.0579).20 This was defined as mHHS scores ≥71. Domb et al. then extended these findings to patients with a minimum 5-year follow-up, with no differences in mHHS reported between repair (81.2 ± 13.5) and non-repair cohorts (80.8 ± 16.1; p = 0.72).29 Additionally, when examining MCID, no difference was found between cohorts for the following time intervals: pre-op to minimum 5-years (repair: 67% vs. non-repair: 71%; p = 0.657), pre-op to 2-year follow-up (74% vs. 82%; p = 0.232), and 2-year follow-up to 5-year follow-up (22% vs. 13%; p = 0.136).29
These findings contradict the findings of Bolia et al. which indicate that mean mHHS was significantly higher for the repair cohort compared to those with capsular release (87 ± 13 vs. 76 ± 20; p = 0.007).28 However, the authors found no differences between the percentage of patients that reached minimally important change (MIC) between the cohorts (repair: 71%, non-repair: 52%; p = 0.60).28
Relating to the effects of plication on mHHS values, Larson et al. analyzed a cohort of patients undergoing revision hip arthroscopy and found that with plication patients had significantly greater mHHS values compared to those that did not undergo plication (26.4 vs. 14.8; p = 0.032).24 Additionally, capsular repair/plication was identified as a predictive variable for greater mHHS outcomes (p = 0.032).24 In a later study, the authors similarly demonstrated that there was a higher percentage of patients in the plication cohort that experienced good or excellent results (73% vs. 53%; p = 0.06).25 However, it is noteworthy that numerous confounding variables, such as the additional factor of labral repair, may have influenced these findings.25
3.3.3. Non-arthritic hip score
Only two included studies evaluated the differences between capsular repair and capsular release on non-arthritic hip scores (NAHS).20,29 Both studies showed no significant differences in the NAHS obtained by either capsular management strategies.
Domb et al. reported greater improvement in NAHS for patients with capsular repair at a minimum 2-year follow-up (repair: 82.8395 ± 17.1327 vs. non-repair:79.0024 ± 17.8038; p = 0.03).20 Additionally, the authors found that the repair cohort had a significantly higher probability of achieving good or excellent outcomes compared to non-repaired patients (79% vs. 60%; OR: 1.547, 95% CI: 1.1014–2.359; p = 0.0428).20 However, following adjustment for age, sex, and other pre-operative metrics, no significant differences were found between the two cohorts. When evaluating patients at a longer follow-up period, Domb et al. reported no significant differences between repair and release cohorts (84.9 ± 16.7 vs. 82.8 ± 15.1; p = 0.99).29
3.3.4. Patient satisfaction
A total of five studies examined the differences in patient satisfaction between different capsular management strategies.17,20,27, 28, 29 However, only two studies20,29 compared capsular release versus capsular repair and provided sufficient data on the pooled statistical analysis. Nevertheless, across the five studies, there were no significant differences between the results obtained with complete repair, partial repair, or capsular release.
At a minimum 2-year follow-up, Atzmon et al. reported no differences in mean satisfaction between patients with capsule closure (88.6%) compared to the non-closure cohort (86.3%; p = 0.672).17 In a similar follow-up period, Domb et al. found no difference between release (mean ± SD: 7.9485 ± 2.2335) and repair 7.9818 ± 2.2264) cohorts (p = 0.8834).20 When looking at longer follow-up periods, similar findings were observed. Specifically, at a minimum follow-up of 5 years, Domb et al. demonstrated that satisfaction was not significantly different between repair (7.6 ± 2.3) and release (8.1 ± 2.1) groups (p = 0.83).29 This was further shown by Bolia et al. with mean follow-up periods of 6.4 ± 2.3 years and 7.3 ± 2.7 years for the repair and non-repair cohorts, respectively. The authors reported that, compared to patients with capsular repair, patients without repair had the same mean satisfaction on a scale from 1 to 10 (9 vs. 9; p = 0.85).28
Frank et al. was the only study to explore the differences between patients with partial closure repair and those with complete repair of the capsule.27 Although their analysis yielded higher satisfaction scores for the complete closure cohort (8.63 ± 1.07 vs. 8.35 ± 1.02), no statistical analysis was performed to identify the significance of this difference.27 However, both patient cohorts had significant improvements in satisfaction between pre-operative and post-operative scores (p < 0.0001).27
3.3.5. Necessity for additional procedures
Four studies reported on the need for subsequent procedures between capsular management strategies.25,27, 28, 29 Specifically, these procedures included conversion to total hip arthroplasty (THA) and the need for revision hip arthroscopy. Out of the four studies, only two provided sufficient data from their pooled statistical analysis of capsular repair versus release.28,29 By reviewing the reported outcomes in each study, it is clear that no consensus was reached regarding the superior approach in mitigating the need for future reoperation.
Regarding conversion to THA, Bolia et al. reported that patients with capsular repair had significantly lower rates of conversion compared to the non-repair cohort (4% vs. 14%; p = 0.01).28 Similarly, Domb et al. found a greater number of conversions in the cohort without repair of the capsule compared to those with capsular plication.29 However, these findings were not statistically significant (p > 0.05).29 Notably, it appeared that those with capsular plication (mean: 38.5 months, range: 3.4–62 months) converted to THA earlier than the release cohort (mean: 57.8 months, range: 24.3–83.4 months).29 Additionally, Larson et al. found lower failure rates in patients with capsular plication and labrum compared to other patients in the dysplastic hip cohort (18% vs. 40%; p = 0.03).25 Failure was defined as either conversion to THA, the need for subsequent osteotomy, or a mHHS ≤ 70.25
When examining rates of revision hip arthroscopy, Bolia et al. found no significant difference between the number of patients in the non-repair (n = 4; 10%) and repair (n = 9; 11%) cohorts that required the procedure (p = 0.8). Conversely, Frank et al. reported a revision rate of 13% in the partial repair cohort compared to 0% among complete repair patients.27 However, no statistics were reported.
3.3.6. Radiographic outcomes
Radiographic analysis was utilized by three studies to evaluate the differences between capsular management approaches.19,27,30 Of the three included studies, two compared radiographic outcomes between capsular repair and capsular release19,30 while the third compared the radiographic outcomes between complete and partial capsular repair.27 A thorough review of the reported outcomes in all three studies demonstrated no differences among the utilized treatment strategies for any of the radiographic outcome measures.19,27,30
Amar et al. examined the rates of heterotrophic ossification between patients that underwent capsular repair and those without repair of the capsule.30 Their analysis of radiographs yielded no significant difference between the two cohorts (28% vs. 44%, respectively; p = 0.144).30 Additionally, capsular management was not found to significantly impact the incidence of heterotrophic ossification following multivariate logistic analysis (p > 0.05).30
Similarly, Strickland et al. used MRI to evaluate 30 hips that underwent interportal capsulotomies that was either repaired (n = 15) or unrepaired (n = 15).19 The authors found that capsular thickness was not significantly different between the two cohorts at 6-weeks and 24-weeks (p > 0.05).19 Additionally, there were no significant differences between the two groups regarding capsular defect size (p > 0.05) or the continuity of the hip capsule (p > 0.05) at both follow-up intervals.19 Furthermore, the soft tissue appearance, including the presence of periarticular muscle and subchondral edema, was not significantly different between the management strategies (p > 0.05).19
Frank et al. was the only study to evaluate alpha angle (AA) and center edge angle (CEA) between capsular repair approaches.27 Patients in the partial closure and complete closure cohorts experience improvements in both measurements following arthroscopy.27 However, there was no significant difference between the two cohorts for both AA (p = 0.0667) and CEA (p = 0.1461).27
3.3.7. Pain
Two studies evaluated pain between management strategies through the use of visual analog scales (VAS).20,29 Both studies reported no significant difference between repair and release cohorts. Specifically, Domb et al. reported no differences for both adjusted and unadjusted VAS values between cohorts (p > 0.05).20 Similarly, no difference was found between strategies at longer follow-up (repair: 2.5 ± 2.4 vs. non-repair: 1.9 ± 2.0; p = 0.42).29
3.3.8. Range of motion
Larson et al. was the only study to evaluate range of motion (ROM).27 The authors found that there were no differences between the partial repair and closure repair cohorts.27 Specifically, there were no differences found for forward flexion (PR: 120.5 ± 14.7° vs. CR: 126.1 ± 15.2°; p = 0.1422), external rotation (PR: 45.2 ± 13° vs CR: 46 ± 11.5°; p = 0.7936), and internal rotation (PR: 22.7 ± 6.8° vs CR: 23.7 ± 6.2°; p = 0.5522).27
4. Discussion
Although hip arthroscopy is a generally safe and successful procedure, as procedural volume rises there is a growing emphasis on methods of maintaining positive outcomes while managing higher case load. This has been highlighted by the recent focus on capsular management strategy and its impact on outcomes. Our systematic review represents the most comprehensive analysis of studies comparing outcomes across management strategies. We found mixed evidence across the literature, with no clear indication regarding which approach yields superior outcomes. Therefore, we are unable to conclude that one strategy is superior to the other.
There are numerous studies in the current literature that indicate the need for capsular repair in order to adequately maintain joint stability. For example, Myers et al. demonstrated that hip joint mechanics were not fully restored following labral repair unless the capsule was concomitantly repaired.35 This was similarly supported by numerous cadaveric studies that indicate capsular release does not restore hip kinematics to the same level as capsular closure.36, 37, 38, 39, 40, 41 Given that laxity of the hip joint has been indicated as one of the leading causes for primary failure following hip arthroscopy,42, 43, 44 capsular repair may be indicated in order to help prevent various complications such as dislocation.45
There is some evidence in the current literature of a trend favoring capsular repair.46 This was made evident by Gupta et al. in their evaluation of capsular management practices among 27 high-volume surgeons.47 Their analysis found that only 11% of providers indicated never closing the capsule, with a majority (78%) considering instability in their capsular repair decision.47 This may suggest that surgeons are more cognizant of the potential complications that arise from capsular release. Furthermore, there have been various novel approaches proposed in the literature regarding easier and more effective strategies for closing the capsule.48, 49, 50, 51 Given the previously demanding nature of intraoperative capsular closure, these innovative techniques may further encourage providers to perform capsular repair.
The present review demonstrated a significant heterogeneity in the reported data. Heterogeneity within the incorporated literature could be attributed in part to the variation in the reparative capsular interventions; capsular plication,24,31,33 complete repair17,20,29,30,52 and partial repair.32 In addition, slight variation in technique among operating surgeons might influence the yielded outcomes.53,54 Similarly, the variation in the extent of capsular release for intra-articular arthroscopic access might be another contributor to data heterogeneity.41 Future large-scale prospective cohort studies can mitigate the effect of the aforementioned confounders while providing sufficient power for subgroup analyses.
The current study exhibits some limitations inherent to the currently available literature. While there is limited information in general, many of the studies consisted of Level III or Level IV evidence. Therefore, more randomized control trials (RCTs) are needed in order to provider stronger comparisons.55 Additionally, there were oftentimes various confounding variables that likely influenced results. For example, the study by Larson et al. compared dysplastic hips to those with FAI when reporting on how plication impacts outcomes.25 Similarly, Atzmon et al. reported on significantly different follow-up periods between repair and non-repair cohorts (Repair: 40.4 months; Non-Repair: 60.7 months; p < 0.001).17 It was unclear whether the patient datasets of the earlier study by Domb et al.20 was incorporated into their later study29 looking into the same outcomes with a longer follow-up interval. Furthermore, despite unifying the capsular management strategies and the measured outcomes for studies incorporated into the meta-analysis, significant heterogeneity was present among the analyzed data. One plausible explanation could be that most decisions regarding how to manage the capsule were done based on surgeon discretion, therefore, it is difficult to truly determine whether outcomes were based solely on capsule integrity or whether more severe pathology discovered intraoperatively could have impacted results. Furthermore, variations in surgical technique (extent of capsulotomy, type of repair and number of sutures used in repair), even within the same capsular repair or release cohorts could present another confounding factor. Domb et al. acknowledged these limitations and stated that their statistically significant findings likely were not clinically significant.20 Despite these limitations, the current study comprehensively presents on the current literature that evaluates outcomes based on how the capsule is managed following hip arthroscopy procedures.
There has been recent debate among providers regarding how to handle the hip capsule following arthroscopy procedures. Review of the current literature demonstrated significantly higher mHHS with capsular repair compared to capsular release. However, while a trend of better outcomes with capsular repair could be observed in HOS-SS, HOS-ADL, overall HOS and NAHS, no consensus on a significant advantage could be established. Furthermore, despite the mixed results regarding the eventual need for reoperation between the two interventions, the time intervals between the index arthroscopy and the second surgery were longer in patients who underwent capsular repair. Finally, both interventions demonstrated similar results in terms of patient satisfaction, pain, range of motion and radiographic outcomes. Given the relatively poor quality of available research, further studies should be conducted that prospectively evaluate outcomes while controlling for additional patient- and surgeon-related factors. However, it is notable that none of the studies included in this review demonstrated superior results with capsular release in any of the reported outcomes.
Funding
This review did not require the approval of the Cleveland Clinic Foundation Institutional Review Board.
No funding or financial support was received for this review.
Declaration of competing interest
A.F.K. reports the following disclosures: research support (Zimmer Biomet, DePuy Synthes), paid presenter or speaker (Corin, DePuy Synthes, Heraeus Medical, and Zimmer Biomet), paid consultant (Pacira Pharmaceuticals, Heraeus Medical, DePuy Synthes, and Zimmer Biomet), stock or stock options (Zimmer Biomet, Johnson & Johnson, and Procter & Gamble), IP royalties (Innomed), board or committee member (AAOS and AAHKS), and editorial or governing board (BMC Musculoskeletal Disorders). A.J.A., L.T.S., A.K.E., and A.R. have nothing to disclose.
References
- 1.Flores S.E., Borak K.R., Zhang A.L. Hip arthroscopic surgery for femoroacetabular impingement: a prospective analysis of the relationship between surgeon experience and patient outcomes. Orthop J Sport Med. 2018;6 doi: 10.1177/2325967118755048. 2325967118755048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yu E., Cil A., Harmsen W.S., Schleck C., Sperling J.W., Cofield R.H. Arthroscopy and the dramatic increase in frequency of anterior acromioplasty from 1980 to 2005: an epidemiologic study. Arthroscopy. 2010;26:S142–S147. doi: 10.1016/j.arthro.2010.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Youm T., Wolfson T., Ryan M.K. Outcome trends after hip arthroscopy for femoroacetabular impingement: when do patients improve? J Hip Preserv Surg. 2016;3 doi: 10.1016/j.arthro.2019.06.020. [DOI] [PubMed] [Google Scholar]
- 4.Matsuda D.K. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthrosc J Arthrosc Relat Surg. 2009;25:400–404. doi: 10.1016/j.arthro.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 5.Benali Y., Katthagen B.D. Hip subluxation as a complication of arthroscopic debridement. Arthrosc J Arthrosc Relat Surg. 2009;25:405–407. doi: 10.1016/j.arthro.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 6.Parvizi J., Bican O., Bender B. Arthroscopy for labral tears in patients with developmental dysplasia of the hip: a cautionary note. J Arthroplasty. 2009;24:110–113. doi: 10.1016/j.arth.2009.05.021. [DOI] [PubMed] [Google Scholar]
- 7.Ranawat A.S., McClincy M., Sekiya J.K. Anterior dislocation of the hip after arthroscopy in a patient with capsular laxity of the hip. J Bone Jt Surg Am. 2009;91:192–197. doi: 10.2106/JBJS.G.01367. [DOI] [PubMed] [Google Scholar]
- 8.Matsuda D.K., Khatod M. Rapidly progressive osteoarthritis after arthroscopic labral repair in patients with hip dysplasia. Arthrosc J Arthrosc Relat Surg. 2012;28:1738–1743. doi: 10.1016/j.arthro.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 9.Philippon M.J. Hip instability. J Am Acad Orthop Surg. 2011;19:340–349. doi: 10.5435/00124635-201106000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Shu B., Safran M.R. Hip instability: anatomic and clinical considerations of traumatic and atraumatic instability. Clin Sports Med. 2011;30:349–367. doi: 10.1016/j.csm.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 11.Martin H.D., Savage A., Braly B.A., Palmer I.J., Beall D.P., Kelly B. The function of the hip capsular ligaments: a quantitative report. Arthrosc J Arthrosc Relat Surg. 2008;24:188–195. doi: 10.1016/j.arthro.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 12.Ito H., Song Y., Lindsey D.P., Safran M.R., Giori N.J. The proximal hip joint capsule and the zona orbicularis contribute to hip joint stability in distraction. J Orthop Res. 2009;27:989–995. doi: 10.1002/jor.20852. [DOI] [PubMed] [Google Scholar]
- 13.Domb B.G., Philippon M.J., Giordano B.D. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: relation to atraumatic instability. Arthrosc J Arthrosc Relat Surg. 2013;29:162–173. doi: 10.1016/j.arthro.2012.04.057. [DOI] [PubMed] [Google Scholar]
- 14.Shindle M.K., Ranawat A.S., Kelly B.T. Diagnosis and management of traumatic and atraumatic hip instability in the athletic patient. Clin Sports Med. 2006;25:309–326. doi: 10.1016/j.csm.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 15.Telleria J.J.M., Lindsey D.P., Giori N.J., Safran M.R. An anatomic arthroscopic description of the hip capsular ligaments for the hip arthroscopist. Arthrosc J Arthrosc Relat Surg. 2011;27:628–636. doi: 10.1016/j.arthro.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 16.Philippon M.J., Stubbs A.J., Schenker M.L., Maxwell R.B., Ganz R., Leunig M. Arthroscopic management of femoroacetabular impingement. Am J Sports Med. 2007;35:1571–1580. doi: 10.1177/0363546507300258. [DOI] [PubMed] [Google Scholar]
- 17.Atzmon R., Sharfman Z.T., Haviv B. Does capsular closure influence patient-reported outcomes in hip arthroscopy for femoroacetabular impingement and labral tear? J Hip Preserv Surg. 2019:1–8. doi: 10.1093/jhps/hnz025. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ekhtiari S., de Sa D., Haldane C.E. Hip arthroscopic capsulotomy techniques and capsular management strategies: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25:9–23. doi: 10.1007/s00167-016-4411-8. [DOI] [PubMed] [Google Scholar]
- 19.Strickland C.D., Kraeutler M.J., Brick M.J. MRI evaluation of repaired versus unrepaired interportal capsulotomy in simultaneous bilateral hip arthroscopy: a double-blind, randomized controlled trial. J Bone Jt Surg Am. 2018;100:91–98. doi: 10.2106/JBJS.17.00365. [DOI] [PubMed] [Google Scholar]
- 20.Domb B.G., Stake C.E., Finley Z.J., Chen T., Giordano B.D. Influence of capsular repair versus unrepaired capsulotomy on 2-year clinical outcomes after arthroscopic hip preservation surgery. Arthrosc J Arthrosc Relat Surg. 2015;31:643–650. doi: 10.1016/j.arthro.2014.10.014. [DOI] [PubMed] [Google Scholar]
- 21.Kuhns B.D., Weber A.E., Levy D.M. Capsular management in hip arthroscopy: an anatomic, biomechanical, and technical review. Front Surg. 2016;3:13. doi: 10.3389/fsurg.2016.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nepple J.J., Smith M.V. Biomechanics of the hip capsule and capsule management strategies in hip arthroscopy. Sports Med Arthrosc. 2015;23:164–168. doi: 10.1097/JSA.0000000000000089. [DOI] [PubMed] [Google Scholar]
- 23.Green edited by JPTH and S. Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons; Chichester, West Sussex ; Hoboken NJ: 2008. ©2008; n.d. [Google Scholar]
- 24.Larson C.M., Giveans M.R., Samuelson K.M., Stone R.M., Bedi A. Arthroscopic hip revision surgery for residual femoroacetabular impingement (FAI) Am J Sports Med. 2014;42:1785–1790. doi: 10.1177/0363546514534181. [DOI] [PubMed] [Google Scholar]
- 25.Larson C.M., Ross J.R., Stone R.M. Arthroscopic management of dysplastic hip deformities. Am J Sports Med. 2016;44:447–453. doi: 10.1177/0363546515613068. [DOI] [PubMed] [Google Scholar]
- 26.Newman J.T., Briggs K.K., McNamara S.C., Philippon M.J. Revision hip arthroscopy. Am J Sports Med. 2016;44:2499–2504. doi: 10.1177/0363546516650888. [DOI] [PubMed] [Google Scholar]
- 27.Frank R.M., Lee S., Bush-Joseph C.A., Kelly B.T., Salata M.J., Nho S.J. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement. Am J Sports Med. 2014;42:2634–2642. doi: 10.1177/0363546514548017. [DOI] [PubMed] [Google Scholar]
- 28.Bolia I.K., Fagotti L., Briggs K.K., Philippon M.J. Midterm outcomes following repair of capsulotomy versus nonrepair in patients undergoing hip arthroscopy for femoroacetabular impingement with labral repair. Arthrosc J Arthrosc Relat Surg. 2019;35:1828–1834. doi: 10.1016/j.arthro.2019.01.033. [DOI] [PubMed] [Google Scholar]
- 29.Domb B.G., Chaharbakhshi E.O., Perets I., Walsh J.P., Yuen L.C., Ashberg L.J. Patient-reported outcomes of capsular repair versus capsulotomy in patients undergoing hip arthroscopy: minimum 5-year follow-up—a matched comparison study. Arthrosc J Arthrosc Relat Surg. 2018;34:853–863. doi: 10.1016/j.arthro.2017.10.019. e1. [DOI] [PubMed] [Google Scholar]
- 30.Amar E., Warschawski Y., Sampson T.G., Atoun E., Steinberg E.L., Rath E. Capsular closure does not affect development of heterotopic ossification after hip arthroscopy. Arthrosc J Arthrosc Relat Surg. 2015;31:225–230. doi: 10.1016/j.arthro.2014.08.026. [DOI] [PubMed] [Google Scholar]
- 31.Newman J.T., Briggs K.K., McNamara S.C., Philippon M.J. Revision hip arthroscopy: a matched-cohort study comparing revision to primary arthroscopy patients. Am J Sports Med. 2016;44:2499–2504. doi: 10.1177/0363546516650888. [DOI] [PubMed] [Google Scholar]
- 32.Frank R.M., Lee S., Bush-Joseph C.A., Kelly B.T., Salata M.J., Nho S.J. Improved outcomes after hip arthroscopic surgery in patients undergoing t-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: a comparative matched-pair analysis. Am J Sports Med. 2014;42:2634–2642. doi: 10.1177/0363546514548017. [DOI] [PubMed] [Google Scholar]
- 33.Larson C.M., Ross J.R., Stone R.M. Arthroscopic management of dysplastic hip deformities: predictors of success and failures with comparison to an arthroscopic FAI cohort. Am J Sports Med. 2016;44:447–453. doi: 10.1177/0363546515613068. [DOI] [PubMed] [Google Scholar]
- 34.Slim K., Nini E., Forestier D., Kwiatkowski F., Panis Y., Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 35.Myers C.A., Register B.C., Lertwanich P. Role of the acetabular labrum and the iliofemoral ligament in hip stability. Am J Sports Med. 2011;39:85–91. doi: 10.1177/0363546511412161. [DOI] [PubMed] [Google Scholar]
- 36.Abrams G.D., Hart M.A., Takami K. Biomechanical evaluation of capsulotomy, capsulectomy, and capsular repair on hip rotation. Arthrosc J Arthrosc Relat Surg. 2015;31:1511–1517. doi: 10.1016/j.arthro.2015.02.031. [DOI] [PubMed] [Google Scholar]
- 37.van Arkel R.J., Amis A.A., Cobb J.P., Jeffers J.R.T. The capsular ligaments provide more hip rotational restraint than the acetabular labrum and the ligamentum teres. Bone Joint Lett J. 2015;97-B doi: 10.1302/0301-620X.97B4.34638. 484–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Philippon M.J., Michalski M.P., Campbell K.J. A quantitative analysis of hip capsular thickness. Knee Surg Sports Traumatol Arthrosc. 2015;23:2548–2553. doi: 10.1007/s00167-014-3030-5. [DOI] [PubMed] [Google Scholar]
- 39.Hewitt J., Guilak F., Glisson R., Parker Vail T. Regional material properties of the human hip joint capsule ligaments. J Orthop Res. 2001;19:359–364. doi: 10.1016/S0736-0266(00)00035-8. [DOI] [PubMed] [Google Scholar]
- 40.Hewitt J.D., Glisson R.R., Guilak F., Vail T.P. The mechanical properties of the human hip capsule ligaments. J Arthroplasty. 2002;17:82–89. doi: 10.1054/arth.2002.27674. [DOI] [PubMed] [Google Scholar]
- 41.Wuerz T.H., Song S.H., Grzybowski J.S. Capsulotomy size affects hip joint kinematic stability. Arthrosc J Arthrosc Relat Surg. 2016;32:1571–1580. doi: 10.1016/j.arthro.2016.01.049. [DOI] [PubMed] [Google Scholar]
- 42.Bogunovic L., Gottlieb M., Pashos G., Baca G., Clohisy J.C. Why do hip arthroscopy procedures fail? Clin Orthop Relat Res. 2013;471:2523–2529. doi: 10.1007/s11999-013-3015-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Clohisy J.C., Nepple J.J., Larson C.M., Zaltz I., Millis M., Members the AN of CHOR (ANCHOR) Persistent structural disease is the most common cause of repeat hip preservation surgery. Clin Orthop Relat Res. 2013;471:3788–3794. doi: 10.1007/s11999-013-3218-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Philippon M.J., Schenker M.L., Briggs K.K., Kuppersmith D.A., Maxwell R.B., Stubbs A.J. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918–1921. doi: 10.1177/0363546507305097. [DOI] [PubMed] [Google Scholar]
- 45.Duplantier N.L., McCulloch P.C., Nho S.J., Mather R.C., Lewis B.D., Harris J.D. Hip dislocation or subluxation after hip arthroscopy: a systematic review. Arthrosc J Arthrosc Relat Surg. 2016;32:1428–1434. doi: 10.1016/j.arthro.2016.01.056. [DOI] [PubMed] [Google Scholar]
- 46.Ortiz-Declet V., Mu B., Chen A.W. Should the capsule Be repaired or plicated after hip arthroscopy for labral tears associated with femoroacetabular impingement or instability? A systematic review. Arthrosc J Arthrosc Relat Surg. 2018;34:303–318. doi: 10.1016/j.arthro.2017.06.030. [DOI] [PubMed] [Google Scholar]
- 47.Gupta A., Suarez-Ahedo C., Redmond J.M. Best practices during hip arthroscopy: aggregate recommendations of high-volume surgeons. Arthrosc J Arthrosc Relat Surg. 2015;31:1722–1727. doi: 10.1016/j.arthro.2015.03.023. [DOI] [PubMed] [Google Scholar]
- 48.Trindade C.A.C., Sawyer G.A., Fukui K., Briggs K.K., Philippon M.J. Arthroscopic capsule reconstruction in the hip using iliotibial band Allograft. Arthrosc Tech. 2015;4:e71–e74. doi: 10.1016/j.eats.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mei-Dan O., Young D.A. A novel technique for capsular repair and labrum refixation in hip arthroscopy using the SpeedStitch. Arthrosc Tech. 2012;1:e107–e112. doi: 10.1016/j.eats.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Harris J.D., Slikker W., Gupta A.K., McCormick F.M., Nho S.J., Nho S.J. Routine complete capsular closure during hip arthroscopy. Arthrosc Tech. 2013;2:e89–94. doi: 10.1016/j.eats.2012.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fagotti L., Soares E., Bolia I.K., Briggs K.K., Philippon M.J. Early outcomes after arthroscopic hip capsular reconstruction using iliotibial band Allograft versus dermal allograft. Arthrosc J Arthrosc Relat Surg. 2019;35:778–786. doi: 10.1016/j.arthro.2018.10.110. [DOI] [PubMed] [Google Scholar]
- 52.Bolia I.K., Fagotti L., Briggs K.K., Philippon M.J. Midterm outcomes following repair of capsulotomy versus nonrepair in patients undergoing hip arthroscopy for femoroacetabular impingement with labral repair. Arthrosc J Arthrosc Relat Surg. 2019;35:1828–1834. doi: 10.1016/j.arthro.2019.01.033. [DOI] [PubMed] [Google Scholar]
- 53.Buyukdogan K., Utsunomiya H., Bolia I. Right versus left hip arthroscopy for surgeons on the learning curve. Arthrosc Tech. 2017;6:e1837–e1844. doi: 10.1016/j.eats.2017.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.de Sa D., Lian J., Sheean A.J. A systematic summary of systematic reviews on the topic of hip arthroscopic surgery. Orthop J Sport Med. 2018;6 doi: 10.1177/2325967118796222. 2325967118796222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dippmann C., Kraemer O., Lund B. Multicentre study on capsular closure versus non-capsular closure during hip arthroscopy in Danish patients with femoroacetabular impingement (FAI): protocol for a randomised controlled trial. BMJ Open. 2018;8 doi: 10.1136/bmjopen-2017-019176. [DOI] [PMC free article] [PubMed] [Google Scholar]