Highlights
-
•
There was high prediabetes incidence among participants of medical examinations.
-
•
Lower relative handgrip strength (HS) predicted higher prediabetes incidence risk.
-
•
Results significant in individuals < 40 and ≥ 40 years old.
-
•
HS predicted lower prediabetes incidence risk among normal weight individuals.
Abbreviations: aHR, adjusted hazard ratios; BMI, body mass index; CI, confidence interval; COI, center of innovation; FPG, fasting plasma glucose; HbA1c, hemoglobin A1c; HDL, high density lipoprotein; IQR, interquartile range; JA Ibaraki, agricultural cooperative of Ibaraki; LDL, low density lipoprotein; OGTT, oral glucose tolerance test; SD, standard deviation
Keywords: Prediabetes, Incident, Muscle strength, Handgrip strength, Normal weight, Physical activity
Abstract
Conventional risk factors for prediabetes and type 2 diabetes such as obesity do not completely explain the higher prevalence of prediabetes; therefore, research to investigate the role of other independent risk factors is required. A few cross-sectional studies have reported an association between muscle strength and prediabetes among normal-weight adults, but the longitudinal relationship of muscle strength with incident prediabetes among adults has not been reported. This prospective cohort study was conducted to investigate whether relative handgrip strength in adults predicted prediabetes incidence after 2 years of follow-up. The study was conducted in Ibaraki prefecture, Japan and recruited individuals without prediabetes and diabetes attending lifestyle related medical examinations between April 2016 and March 2017 (n = 2054). Individuals who came for the follow-up medical examinations between April 2018 and March 2019 were included in the analysis (n = 1075). One hundred sixty-nine individuals (15.7%) developed prediabetes after a mean follow-up of 24.2 months (SD = 1.9 months). Multivariable adjusted hazard ratios (aHR) of new prediabetes cases were calculated using Cox regression. Higher baseline relative handgrip strength predicted a lower risk (aHR [95% CI] = 0.38 [0.21–0.71] of prediabetes incidence among adults. Importantly, relative handgrip strength predicted new prediabetes cases among normal weight individuals (aHR [95% CI] = 0.39 [0.16–0.96]). The findings suggest that handgrip strength measurement is useful to identify individuals at high risk of newly diagnosed prediabetes, importantly, among normal weight individuals. The identified individuals may benefit from early intervention to reduce the risk of prediabetes.
1. Introduction
There were 451 million people with diabetes and 5 million deaths due to diabetes in 2017 with this prevalence expected to rise to 693 million by 2045 (Cho et al., 2018). Before developing type 2 diabetes, individuals undergo an intermediate state termed prediabetes, which is characterized by blood glucose concentrations that are higher than normal but not high enough for diagnosis (Heianza et al., 2011, Tabák et al., 2012). Japan is among the countries with a high prevalence (15%–35%) of prediabetes (Uehara et al., 2014, Mukai et al., 2014). Individuals with prediabetes defined as impaired glucose tolerance, impaired fasting glucose, or raised haemoglobin A1c (HbA1c) have a high risk of composite cardiovascular events, coronary heart disease, stroke, and all-cause mortality (Huang et al., 2016). Early intervention in prediabetic individuals significantly reduces the risk of progression to type 2 diabetes (Ligthart et al., 2016), but identifying individuals at higher risk of prediabetes would provide the best opportunity for implementation of preventive strategies.
Whilst conventional factors such as obesity are well studied, they do not completely explain the higher prediabetes prevalence observed in Japan, which has a lower rate of obesity than those of western populations (Finucane et al., 2011). Therefore, other independent risk factors may explain the high prevalence. For instance, it is postulated that Japanese, as well as other Asians, have a limited innate ability of insulin secretion, making them more susceptible to insulin resistance with small changes in body composition (Uemura et al., 2017). Studies are required to clarify the pathogenesis of prediabetes and type 2 diabetes among such populations to help in formulating preventive programs that incorporate new messages on the identified independent risk.
Handgrip strength, a simple measure of muscle strength that is well correlated with other strength measures such as quadriceps strength (Newman et al., 2006), was reported to be associated with metabolic syndrome (Kawamoto et al., 2016, Ishii et al., 2014, Atlantis et al., 2009), type 2 diabetes mellitus (Li et al., 2016, Wander et al., 2011, Van der Kooi et al., 2015, Momma et al., 2019), and overall mortality (Lopez-Jaramillo et al., 2014, Leong et al., 2015, Celis-Morales et al., 2018). Whilst the underlying mechanism has not been well explained, studies exploring the role of muscle resistance exercises in glucose metabolism have reported that such muscle strengthening activities improve muscle function and glucose deposition (Richter and Hargreaves, 2013, Castorena et al., 2015). Furthermore, such studies have shown that the impact of exercise training favors insulin-mediated glucose uptake in skeletal muscle rather than in adipose tissue (Reichkendler et al., 2013). The results of these studies suggest that muscle strength (a proxy measure of muscle quality) may be an important factor in the development of prediabetes and type 2 diabetes.
However, the longitudinal relationship of handgrip strength with newly diagnosed prediabetes has not been reported. Therefore, whether handgrip strength can be used to identify individuals at high risk of prediabetes who would benefit from early interventions is unknown. Additionally, the association between handgrip strength and type 2 diabetes has not been consistently reported (Marques-Vidal et al., 2017, Larsen et al., 2016), with some studies reporting no association and others suggesting that the observed association is a result of reverse causation. The confounding effect of body size has been cited as one of the reasons for the conflicting findings; hence, relative handgrip strength has been recommended as a better indicator for considering both the effect of body mass and muscular strength (Lawman et al., 2016). This study was therefore conducted to investigate whether relative handgrip strength predicted prediabetes incidence among adults participating in annual medical examinations in Japan after 2 years of follow-up.
2. Methods
2.1. Study area and population
The present study was instituted under the Center of Innovation (COI) program of Japan, which aims to improve the health status of the population. The study was conducted in Ibaraki prefecture, whose capital city, Mito, is situated about 125 km north-east of Tokyo. Most of the study participants belonged to the Japan Agriculture Cooperative of Ibaraki (JA Ibaraki). Participants were invited to attend annual medical examinations organized in partnership with JA at the regional hospital (Mito-Kyodo Hospital) and at outreach services in the area or to attend medical examinations organized by employers, with an annual attendance of about 5000 individuals. Annual medical examinations are conducted along with the Japanese Industry Safety and Health Act (Ministry of Justice, Japan, 2009) and are performed to facilitate lifestyle change and early disease diagnosis, which in turn would lower health expenditure and improve quality of life.
This prospective study recruited individuals without prediabetes and diabetes who performed handgrip strength measurement during lifestyle related medical examinations at a regional hospital and outreach sites between April 2016 and March 2017 (n = 2054). We excluded individuals who were aged younger than 20 (n = 10) or older than 75 years (n = 37); or had handgrip strength measured in one hand or while seated (n = 6); or had a history of stroke (n = 18), heart disease (n = 31), chronic renal failure (n = 6) at baseline. Some individuals met more than one of the exclusion criteria. Persons were followed up between April 2018 and March 2019 with 1075 (54.7%) individuals attending the 2-years follow-up medical examinations (men: 55.2%; age, mean [SD]: 42.2 [12.7] years). Participants who attended follow-up medical examination within one year after baseline examinations were not included in this analysis. Supplementary Figure A shows the flowchart of the participants.
This study was reviewed and approved by the ethics review committee of the University of Tsukuba. It was conducted according to the principles of the Declaration of Helsinki. Written informed consent was obtained from each participant.
2.2. Measures and definitions
Anthropometric measurements such as body weight (kg) and height (cm) using a Tanita DC250 (TANITA Co, Japan), waist circumference (cm), and blood pressure (mmHg) were performed at the regional hospital or at the outreach medical examination by trained personnel. Fasting blood samples were collected, and biochemical tests including hemoglobin A1c (HbA1c), fasting plasma glucose (FPG), high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, and triglycerides were conducted at the regional hospital laboratory.
Body mass index (BMI; calculated as weight/height2) was categorized as underweight (<18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), or obese (≥30 kg/m2). Hypertension was defined as any of the following: systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, or use of antihypertensive medication, whilst dyslipidemia was defined as triglycerides ≥ 150 mg/dL, LDL-cholesterol ≥ 140 mg/dL, HDL-cholesterol < 40 mg/dL, or self-reported use of anticholesteremic agents (Kinoshita et al., 2018).
2.3. Handgrip strength
We assessed handgrip strength using a Smedley digital handgrip test machine (Takei Corporation, Japan) following standard operating procedures (NHNES, 2016). The participants were instructed to stand upright and to look straight ahead. The dynamometer handle was adjusted to ensure a comfortable fit. The participants were then told to hold the handle in the hand to be tested, with arms straight down by the sides of the body but not touching it or any other object. The participants were instructed to squeeze the dynamometer with a maximum isometric effort for about 5 s, and no other body movements were allowed. Handgrip strength was measured twice in each hand, and the average of the maximum handgrip strength values (kg) from each hand was displayed in the machine and used for our analysis.
2.4. Relative handgrip strength
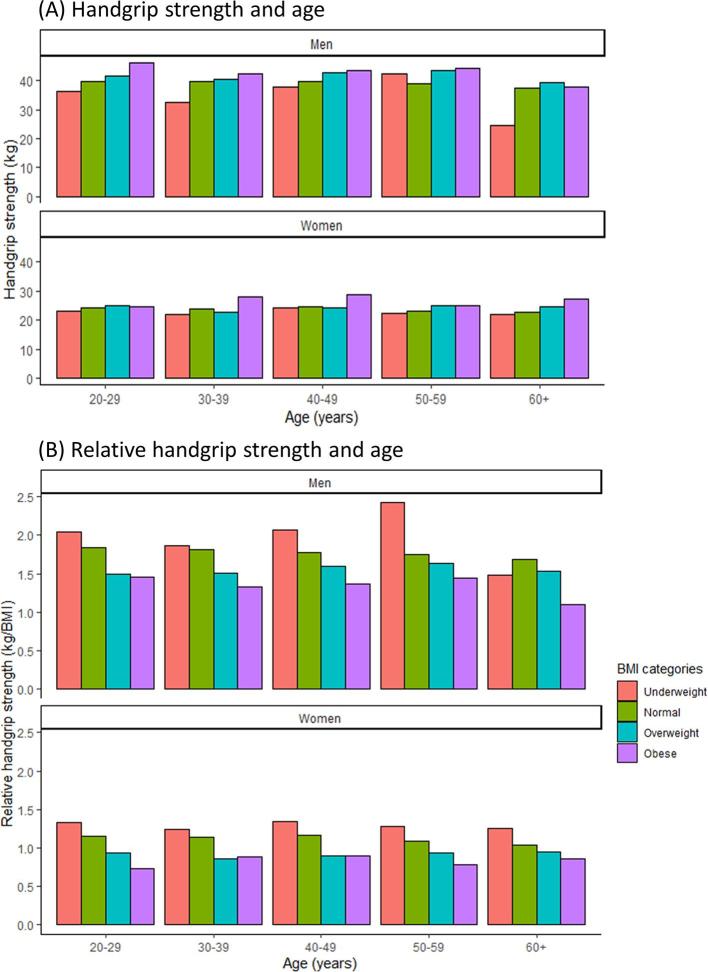
Relative handgrip strength was calculated as absolute handgrip strength (kg) divided by BMI (reported as kg/BMI). The use of relative handgrip strength over absolute handgrip strength has been proposed to adjust for the direct relationship between mass and force (Lawman et al., 2016). Absolute handgrip strength is indicative not only of muscle quality but also of the combined effect of fat mass and muscle mass. This was also observed in our data showing that whilst overweight and obese individuals may have a higher absolute handgrip strength, their relative handgrip strength is lower than that of normal weight individuals. This is shown in Supplementary Figure B.
2.5. Prediabetes and type 2 diabetes mellitus
Prediabetes was defined as one or a combination of the following blood glucose results: HbA1c of 5.7% to 6.4% or FPG of 110 to 125 mg/dL (Heianza et al., 2011). Type 2 diabetes mellitus was defined as any of the following: physician’s diagnosis, use of antidiabetic medication, FPG ≥ 126 mg/dL, or HbA1c ≥ 6.5%.
2.6. Lifestyle and medical history
A standardized self-administered questionnaire of 22 items recommended by the Japan Ministry of Health, Labor and Welfare was used to collect lifestyle-related information and medical history (MHLW, 2017). It included questions on current smoking (smoking in the past month) and weight change in the past year (±3 kg), regular physical activity (exercising ≥ 30 min per session, ≥ 2 times per week for ≥ 1 year, or daily walking or physical activity equal to walking ≥ 1 h per day), and alcohol consumption frequency (rarely, sometimes, or every day). The questionnaire included the medical history of type 2 diabetes mellitus, hypertension, heart disease, stroke, renal failure, cancer, and anemia. It also asked about the use of antihypertensive, antidiabetic, and anticholesteremic agents.
2.7. Statistical analyses
Participants’ baseline demographics, anthropometrics, and lifestyle characteristics were reported as mean values with standard deviations (SD) or median values with interquartile ranges for continuous variables and percentages for categorical variables. Continuous and categorical variables were analyzed using the t test and chi-square test, respectively. Mean biomarker values were presented by sex to show the cardiovascular risk differences between men and women among our study participants. We thereafter used the ANOVA test to analyze the mean biomarkers values within age and sex adjusted tertiles of relative handgrip strength. Skewed variables such as triglycerides, γ-glutamyl transferase, and alanine transaminase were log-transformed, and their geometric means and standard deviations were presented.
We calculated the follow-up period in months from the date of the baseline medical examination to the date of diagnosis of prediabetes at the follow-up medical examination or the date of the last medical examination. Cox proportional hazards regression analysis was conducted to assess whether baseline relative handgrip strength predicted prediabetes incidence. The analysis was firstly performed among all participants. Thereafter, stratified analyses were performed with age (<40 or ≥ 40 years), and BMI (18.5–24.9 or ≥ 25.0 kg/m2). The stratified analyses with BMI were conducted to assess whether relative handgrip strength predicted the risk of newly diagnosed cases among normal weight individuals who made up most of our study participants. We conducted further multivariable adjusted Cox regression analysis for the risk of new prediabetes cases within tertiles of age and sex adjusted relative handgrip strength. Hazard ratios were reported with 95% confidence intervals at a 0.05 significance level. Variance inflation factors (VIFs) were used to assess multicollinearity, and the VIF values of the fitted models were below 3. The models were adjusted for body composition, lifestyle characteristics, and other metabolic disease factors. Model 1 was adjusted for age and sex only. Model 2 was adjusted for age, sex, current smoking, dyslipidemia, alcohol consumption frequency, and hypertension. Model 3 was adjusted for the same variables as those in model 2 but included further adjustment for regular physical activity. We also tested if there was any interaction between relative handgrip strength and regular physical activity.
We conducted sensitivity analysis using a multiple imputed dataset since 4.4% missing data were observed on some covariates (smoking status, alcohol consumption and regular physical activity). We conducted multiple imputation with chained equations (White et al., 2011). In addition, the models were further adjusted for baseline fasting plasma glucose.
All statistical analyses were conducted with SPSS version 24 (IBM, USA) and R statistics version 3.5.2.
3. Results
During a mean follow-up period of 24.2 months (SD = 1.9 months), 169 (15.7%) of the 1075 normoglycemic individuals at baseline developed prediabetes. The baseline demographics and anthropometric and lifestyle characteristics are shown in Table 1. The mean (SD) age and BMI of the participants at baseline were 42.2 (12.7) years and 22.8 (3.5) kg/m2, respectively. The women were relatively older than the men at baseline (43.7 ± 13.0 vs 41.0 ± 12.3 years, P = .001). Higher proportions of the participants were within the age groups of 20 to 39 (44.9%) and 40 to 59 years (44.8%), whilst only a few (10.3%) individuals were aged older than 60 years. The proportion of underweight women was higher than that of men (14.7% vs 3.2%, P < .001), and the proportion of overweight or obese men was higher than that of women (30.0% vs 15.8%, P < .001). The mean (SD) absolute handgrip strength and relative handgrip strength were 32.8 (9.8) kg and 1.5 (0.4) kg/BMI, respectively, and the relative handgrip strength peaked among individuals aged between 30 and 40 years.
Table 1.
Demographics, anthropometrics and lifestyle characteristics at baseline.
| Characteristic | All n = 1075 |
Men n = 593 (55.2%) |
Women n = 482 (44.8%) |
|---|---|---|---|
| Age (years), mean ± SD | 42.2 ± 12.7 | 41.0 ± 12.3 | 43.7 ± 13.0 |
| 20–39 | 483 (44.9) | 294 (49.6) | 189 (39.2) |
| 40–59 | 482 (44.8) | 248 (41.8) | 238 (48.5) |
| 60–75 | 110 (10.3) | 51 (8.6) | 59 (12.3) |
| BMI (kg/m2), mean ± SD | 22.8 ± 3.5 | 23.7 ± 3.3 | 21.8 ± 3.6 |
| Underweight | 90 (8.4) | 19 (3.2) | 71 (14.7) |
| Normal | 731 (68.0) | 396 (66.8) | 335 (69.5) |
| Overweight | 208 (19.3) | 150 (25.3) | 58 (12.1) |
| Obese | 46 (4.3) | 28 (4.7) | 18 (3.7) |
| Alcohol consumption frequencya | |||
| Rarely | 472 (45.9) | 205 (36.0) | 267 (58.2) |
| Sometimes | 332 (32.3) | 200 (35.1) | 132 (28.8) |
| Every day | 225 (21.8) | 165 (28.9) | 60 (13.0) |
| Regular physical activitya | |||
| Yes | 340 (33.0) | 211 (37.0) | 129 (28.1) |
| No | 689 (67.0) | 359 (63.0) | 330 (68.5) |
| Current smokinga | |||
| Yes | 248 (24.1) | 192 (33.7) | 56 (12.2) |
| No | 781 (75.9) | 378 (66.3) | 403 (87.8) |
| Hypertension | |||
| Yes | 287 (26.7) | 191 (32.2) | 96 (19.9) |
| No | 788 (73.3) | 402 (67.8) | 386 (80.1) |
| Dyslipidemia | |||
| Yes | 379 (35.3) | 246 (41.5) | 133 (27.6) |
| No | 696 (64.7) | 347 (58.5) | 349 (72.4) |
Abbreviations: BMI, body mass index. Means and standard deviations (SD) are shown for continuous variables, and the number of participants and percentages, for categorical variables. aNumber of participants = 1029.
Men and women differed significantly in terms of mean values of waist circumference (83.6 ± 8.9 vs 77.4 ± 10.1 cm, P < .001), systolic blood pressure (129.3 ± 16.3 vs 121.7 ± 18.1 mmHg, P < .001), diastolic blood pressure (79.5 ± 12.1 vs 73.1 ± 12.0 mmHg, P < .001), HDL cholesterol (55.7 ± 13.6 vs 67.3 ± 15.1 mg/dL, P < .001), LDL cholesterol (119.5 ± 30.9 vs 114.3 ± 30.0 mg/dL, P < .001), triglycerides (median [IQR]: 93.0 [65.0–138.0] vs 67.0 [50.0–92.0] mg/dL, P < .001), and creatinine (0.9 ± 0.1 vs 0.6 ± 0.1 mg/dL, P < .001), with women tending to have healthier cardiovascular biomarker values (Table 2).
Table 2.
Biomarker values by sex at baseline.
| Characteristic | Men n = 593 |
Women n = 482 |
P-valueb |
|---|---|---|---|
| Waist circumference (cm) | 83.6 ± 8.9 | 77.4 ± 10.1 | <0.001 |
| Systolic blood pressure (mmHg) | 129.3 ± 16.3 | 121.7 ± 18.1 | <0.001 |
| Diastolic blood pressure (mmHg) | 79.5 ± 12.1 | 73.1 ± 12.0 | <0.001 |
| Total cholesterol (mg/dL) | 195.4 ± 32.8 | 199.2 ± 35.4 | 0.069 |
| HDL cholesterol (mg/dL) | 55.7 ± 13.6 | 67.3 ± 15.1 | <0.001 |
| LDL cholesterol (mg/dL) | 119.5 ± 30.9 | 114.3 ± 30.0 | 0.006 |
| Triglycerides (mg/dL)a | 93.0 (65.0–138.0) | 67.0 (50.0–92.0) | <0.001 |
| Creatinine (mg/dL) | 0.9 ± 0.1 | 0.6 ± 0.1 | <0.001 |
| Relative handgrip strength (kg/BMI) | 1.7 ± 0.3 | 1.1 ± 0.2 | <0.001 |
Abbreviations: HDL, high-density lipoprotein; LDL, low-density lipoprotein.
Means and standard deviations are shown for continuous variables, and number of participants and percentages, for categorical variables.
Data for triglycerides were skewed and therefore are presented as median (interquartile range) values and P-values obtained with the Kruskal-Wallis test.
P-values obtained with the t test.
Compared with the lower tertile of age and sex-adjusted relative handgrip strength, the middle and higher tertiles were significantly associated with more favorable waist circumference (P < .001), systolic blood pressure (P = .012), diastolic blood pressure (P = .016), total cholesterol (P = .004), HDL-cholesterol (P < .001), LDL cholesterol (P < .001), non-HDL cholesterol (P < .001), and triglycerides (P < .001). The results of the mean biomarker values of age and sex-specific tertiles of relative handgrip strength are shown in Supplementary Table A.
The results from analysis of baseline relative handgrip strength for prediabetes incidence after 2 years of follow-up is shown in Table 3. A unit increase in relative handgrip strength predicted a lower and significant risk of prediabetes incidence among all the participants (adjusted hazard ratio, aHR [95% CI] = 0.40 [0.21–0.71]) after adjusting for age (continuous), sex, current smoking, dyslipidemia, alcohol consumption frequency, and hypertension in model 2. Moreover, the results remained significant even after further adjustment for regular physical activity in model 3 (aHR [95% CI] = 0.38 [0.21–0.71]), whilst no significant interaction was found between relative handgrip strength and regular physical activity.
Table 3.
Adjusted hazard ratios for the risk of new prediabetes cases with increasing relative handgrip strength.
| Model 1a |
Model 2b |
Model 3c |
|||
|---|---|---|---|---|---|
| Cases (%), n | aHR (95% CI) | Cases (%), nd | aHR (95% CI) | aHR (95% CI) | |
| All participants | 169 (15.8), 1073 | 0.33 (0.18–0.60) | 165 (16.1), 1027 | 0.40 (0.21–0.71) | 0.38 (0.21–0.71) |
| Age (years) | |||||
| <40 | 43 (8.9), 483 | 0.27 (0.10–0.73) | 43 (9.5), 455 | 0.25 (0.09–0.74) | 0.25 (0.08–0.72) |
| ≥40 | 126 (21.3), 590 | 0.37 (0.21–0.95) | 122 (21.3), 572 | 0.47 (0.22–0.98) | 0.45 (0.21–0.95) |
| BMI (kg/m2) | |||||
| 18.5–25.0 | 100 (13.7), 729 | 0.37 (0.15–0.90) | 98 (14.0), 698 | 0.39 (0.16–0.95) | 0.39 (0.16–0.96) |
| ≥25.0 | 61 (24.0), 254 | 0.66 (0.24–1.84) | 59 (24.4), 242 | 0.78 (0.26–2.33) | 0.75 (0.25–2.26) |
Abbreviations: aHR, Adjusted hazard ratio; CI, confidence interval.
Boldface indicates statistical significance (P < .05).
Model 1: adjusted for age and sex.
Model 2: adjusted for age, sex, dyslipidemia, hypertension, smoking status, and alcohol consumption frequency.
Model 3: model 2+regular physical activity.
n, only participants with complete information on covariates included in models 2 and 3.
In stratified analyses, similar and significant results were observed among individuals younger than 40 years (aHR [95% CI] = 0.25 [0.08–0.72]) and those 40 years or older (aHR [95% CI] = 0.45 [0.21–0.95]) after adjusting for age (continuous), sex, current smoking, dyslipidemia, alcohol consumption frequency, hypertension and regular physical activity. Importantly, a unit increase in relative handgrip strength predicted a lower and significant risk (aHR [95% CI] = 0.39 [0.16–0.96]) of prediabetes incidence among individuals with normal BMI (18.5–24.9 kg/m2). And a lower but not significant risk (aHR [95% CI] = 0.75 [0.25–2.26]) was also observed among those with BMI ≥ 25.0 kg/m2 after adjusting for age (continuous), sex, current smoking, dyslipidemia, alcohol consumption frequency, hypertension and regular physical activity.
Additional analysis using sex and age adjusted tertiles of relative handgrip strength produced similar results. Compared with those in the lower tertile of relative handgrip strength, lower risk of prediabetes incidence was observed among those in the middle (aHR [95% CI] = 0.61 [0.42–0.87]) and upper tertiles (aHR [95% CI] = 0.59 [0.40–0.86]) [Supplementary Table B]. Sensitivity analysis using multiple imputed dataset showed comparable results with analyses using complete-case analysis even when baseline fasting plasma glucose was considered [Supplementary Table C].
4. Discussion
This study examined whether relative handgrip strength predicts incident prediabetes among a sample of Japanese adults attending annual medical examinations. Fifteen percent of individuals had incident prediabetes within 2 years of follow-up, suggesting a high risk of prediabetes among the participants. This study found that lower baseline relative handgrip strength predicted a higher risk of prediabetes incidence among the participants. An important finding of this study was that relative handgrip strength predicted a lower and significant risk of prediabetes incidence among individuals with normal weight (BMI 18.5–24.9 kg/m2). The use of handgrip strength, a simple measure of muscle strength, may have utility in the identification of individuals at high risk of prediabetes who can then be targeted for intervention. Participants of annual medical examinations could be motivated to improve muscle strength after understanding the risk that lower relative handgrip strength may indicate for future prediabetes incidence and risk of type 2 diabetes.
This is the first study to report the impact of handgrip strength on prediabetes incidence after 2-years of follow-up. It extends the findings on the cross-sectional association of relative handgrip strength with fasting blood glucose (Lawman et al., 2016), prediabetes (Hu et al., 2019, Mainous et al., 2016), and incident type 2 diabetes (Momma et al., 2019). Relative handgrip strength was also associated with a number of cardiovascular biomarkers in our study, similar to findings from an earlier study (Lawman et al., 2016). Prediabetes is associated with higher cardiovascular risk (Huang et al., 2016); therefore, the use of simple indicators combining various risk states such as relative handgrip strength may have utility in screening and intervention programs for both conditions in the community.
The findings suggest that reduction in muscle strength may precede the development of prediabetes, thereby providing a favorable window where meaningful intervention programs can be implemented. In addition, interventions targeted to high-risk individuals may result in more individuals taking part in community self-exercise campaigns, which we believe would benefit this community. Some simple exercises such as elastic resistance training that can be performed at home are already known to improve muscle strength and functional performance (De Oliveira et al., 2016).
The current study shows that relative handgrip strength may be used to stratify prediabetes risk among populations with lower rates of obesity such as Japan, where a higher risk of prediabetes and type 2 diabetes is observed even in individuals with normal body mass index (Kim et al., 2015, Uehara et al., 2014, Price et al., 2018). Indeed, baseline relative handgrip strength predicted newly diagnosed prediabetes cases among individuals with normal weight (BMI 18.5–24.9 kg/m2). This is to our knowledge the first study to report such findings. The association was however not significant among overweight and obese individuals in our study. Whilst the result may be due to the smaller number of individuals with BMI ≥ 25.0 kg/m2 in our study, a few studies investigating the association of muscle mass and metabolic syndrome reported significant results only in non-obese individuals in Asia. Several explanations have been suggested including that muscle mass may have a lesser impact because of pre-existing imbalances in obese participants (Kim et al., 2015). The greater fat content in skeletal muscle disrupts glucose metabolism since it is associated with reduced insulin sensitivity. Additionally, BMI does not distinguish between fat mass and fat-free mass which may contribute to the failure to detect significant association in the overweight/obese stratum since fat mass contributes minimal to muscular strength as compared to fat-free mass (FFM). Studies are required to further investigate the association of relative handgrip strength with incident prediabetes among overweight and obese individuals. These studies may explore the use of fat-free mass in the denominator of the strength metric (kg/kgFFM).
These findings also suggest that muscle strength may play a role in the development of prediabetes. Whilst the underlying mechanism has not been well explained, physiological research suggests potential causal pathways and benefits of muscle strength. For example, muscle strength affects the abundance of GLUT-4 receptors involved in insulin-mediated glucose uptake in muscles (Reichkendler et al., 2013), and several studies investigating the effects of muscle training exercise have reported significant increases in skeletal muscle GLUT-4 expression and glucose uptake (Richter and Hargreaves, 2013, Sénéchal et al., 2015). Our study, however, did find that the association between relative handgrip strength and incident prediabetes was still significant even after adjusting for regular physical activity. A finding suggesting that this association may be independent of regular physical activity or that resistance exercises are not well highlighted in the standard regular physical activity questionnaire implemented in the annual medical examinations, thereby necessitating the inclusion of handgrip strength in these examinations to fully ascertain the muscle function capacity of participants.
The strength of this study was the wide age range of the individuals attending the annual medical examinations, which enables its generalizability with age. This advantage is lost when dealing with similar examinations conducted among company working individuals in which the age range is narrow. In addition, the use of both hemoglobin A1c and fasting plasma glucose may have increased our ability to detect individuals with prediabetes (Heianza et al., 2011, Heianza et al., 2012). Finally, these annual medical examinations are open not only to farmers but also to their dependents and to nonfarming community members, making the data representative of the community.
5. Limitations
The present study has some limitations. Firstly, an oral glucose tolerance test (OGTT), which is used to identify individuals with impaired glucose tolerance, was not performed, which may have resulted in misclassification of some individuals. Selection bias is also possible since we used data from individuals taking annual medical examinations who may be more health conscious than the general population. Furthermore, most individuals join medical examinations at an average of 1.5 years therefore some participant did not come for medical examinations during the 2018 fiscal year. However, the age and sex distributions of those who did not participate at the 2-year follow-up were comparable to those who came for the follow-up examinations. We also followed up the participants for 2 years only, which may not be enough time to rule out reverse causation; however, our study results still have utility in identification of individuals at high risk of prediabetes in medical examinations who may benefit from early interventions. We also had no information on family history of type 2 diabetes and, therefore, did not adjust for genetic influence.
Further studies are required to examine the association of muscle strength with incident prediabetes, especially among overweight and obese individuals. Furthermore, studies to identify age-specific cutoff values of relative handgrip strength to identify the target population with a high risk of developing prediabetes are required to facilitate easy interpretation and feedback to participants.
6. Conclusions
This study found that baseline relative handgrip strength predicts incident prediabetes among adults in Japan. The findings suggest that relative handgrip strength may be used to identify individuals at high risk of prediabetes especially among normal weight individuals who may benefit from early intervention to reduce the risk of type 2 diabetes and cardiovascular disease.
Acknowledgments
Acknowledgments
The authors are grateful to the participants who took part in this cohort study; the Japan Agricultural Cooperative Ibaraki Kouseiren for their cooperation throughout the period of the study; the doctors, nurses, and staff of Mito-Kyodo Hospital who administered the medical examinations; and Dr. Mizuho Fukushige who helped with reviewing the manuscript. Finally, the authors would like to greatly appreciate Ms Flaminia Miyamasu, associate professor of English for Medical Purposes, Medical English Communications Center, University of Tsukuba, for her native English editorial assistance.
Author contributions
Yukiko Wagatsuma was responsible for designing and initiation of the cohort study, securing funding, overseeing data preparation, analysis, interpretation and revising the manuscript. Chrispin Mahala Manda was responsible for preparing data, analyzing, interpreting and, preparing the initial draft of the manuscript. Takahiro Hokimoto was involved in initial data preparation, formulation of data analysis plan and revising the manuscript. Tomohiro Okura and Hiroko Isoda provided guidance on data interpretation and helped to revise the manuscript, Hitoshi Shimano was involved in the designing and implementation of the COI project, and revising the manuscript.
Funding
This work was supported by JST COI grant number JPMJCE1301. The funding body was not involved in the study design, data collection, analysis, interpretation of results, or decision to submit the manuscript for publication.
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2020.101056.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Supplementary figure 1.
Supplementary figure 2.
References
- Cho N.H., Shaw J.E., Karuranga S., Huang Y., da Rocha Fernandes J.D., Ohlrogge A.W. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 2018;138:271–281. doi: 10.1016/j.diabres.2018.02.023. [DOI] [PubMed] [Google Scholar]
- Heianza Y.R., Saito K., Fujiwara K., Kodama S., Shimano H., Yamada N. HbA 1c 5.7-6.4% and impaired fasting plasma glucose for diagnosis of prediabetes and risk of progression to diabetes in Japan (topics 3): a longitudinal cohort study. Lancet. 2011;378:147–155. doi: 10.1016/S0140-6736(11)60472-8. [DOI] [PubMed] [Google Scholar]
- Tabák A.G., Herder C., Rathmann W., Brunner E.J., Kivimäki M. Prediabetes: a high-risk state for diabetes development. Lancet. 2012;379:2279–2290. doi: 10.1016/S0140-6736(12)60283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uehara A., Kurotani K., Kochi T., Kuwahara K., Eguchi M., Imai T. Prevalence of diabetes and pre-diabetes among workers: Japan Epidemiology Collaboration on Occupational Health Study. Diabetes Res. Clin. Pract. 2014;106:118–127. doi: 10.1016/j.diabres.2014.07.013. [DOI] [PubMed] [Google Scholar]
- Mukai, N., Doi, Y., Ninomiya, T., Hirakawa, Y., Nagata, M., Yoshida, D., et al., 2014. Trends in the prevalence of type 2 diabetes and prediabetes in community-dwelling Japanese subjects: the Hisayama Study. J. Diabetes Investig. 5, 162–169. Doi:10.1111/jdi.12136. [DOI] [PMC free article] [PubMed]
- Huang Y., Cai X., Mai W., Li M., Hu Y. Association between prediabetes and risk of cardiovascular disease and all cause mortality: systematic review and meta-analysis. BMJ. 2016;355 doi: 10.1136/bmj.i5953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ligthart S., van Herpt T.T.W., Leening M.J.G., Kavousi M., Hofman A., Stricker B.H.C. Lifetime risk of developing impaired glucose metabolism and eventual progression from prediabetes to type 2 diabetes: a prospective cohort study. Lancet Diabetes Endocrinol. 2016;4:44–51. doi: 10.1016/S2213-8587(15)00362-9. [DOI] [PubMed] [Google Scholar]
- Finucane M.M., Stevens G.A., Cowan M.J., Danaei G., Lin J.K., Paciorek C.J. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet. 2011;377:557–567. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uemura H., Katsuura-Kamano S., Yamaguchi M., Bahari T., Ishizu M., Fujioka M. Relationships of serum high-sensitivity C-reactive protein and body size with insulin resistance in a Japanese cohort. PLoS One. 2017;12:1–11. doi: 10.1371/journal.pone.0178672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman A.B., Kupelian V., Visser M., Simonsick E.M., Goodpaster B.H., Kritchevsky S.B. Strength, but not muscle mass, is associated with mortality in the Health, Aging and Body Composition Study Cohort. J. Gerontol. A Biol. Sci. Med. Sci. 2006;61:72–77. doi: 10.1093/gerona/61.1.72. [DOI] [PubMed] [Google Scholar]
- Kawamoto R., Ninomiya D., Kasai Y., Kusunoki T., Ohtsuka N., Kumagi T. Handgrip strength is associated with metabolic syndrome among middle-aged and elderly community-dwelling persons. Clin. Exp. Hypertens. 2016;38:245–251. doi: 10.3109/10641963.2015.1081232. [DOI] [PubMed] [Google Scholar]
- Ishii S., Tanaka T., Akishita M., Ouchi Y., Tuji T., Iijima K. Metabolic syndrome, sarcopenia and role of sex and age: cross-sectional analysis of Kashiwa cohort study. PLoS One. 2014;9 doi: 10.1371/journal.pone.0112718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atlantis E., Martin S.A., Haren M.T., Taylor A.W., Wittert G.A. Inverse associations between muscle mass, strength, and the metabolic syndrome. Metabolism. 2009;58:1013–1022. doi: 10.1016/j.metabol.2009.02.027. [DOI] [PubMed] [Google Scholar]
- Li J.J., Wittert G.A., Vincent A., Atlantis E., Shi Z., Appleton S.L. Muscle grip strength predicts incident type 2 diabetes: population-based cohort study. Metabolism. 2016;65:883–892. doi: 10.1016/j.metabol.2016.03.011. [DOI] [PubMed] [Google Scholar]
- Wander P.L., Boyko E.J., Leonetti D.L., McNeely M.J., Kahn S.E., Fujimoto W.Y. Greater hand-grip strength predicts a lower risk of developing type 2 diabetes over 10 years in leaner Japanese Americans. Diabetes Res. Clin. Practice. 2011;92:261–264. doi: 10.1016/j.diabres.2011.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Kooi, A.-L.L.L.F.F., Snijder, M.B., Peters, R.J.G.G., van Valkengoed, I.G.M.M., 2015. The association of handgrip strength and type 2 diabetes mellitus in six ethnic groups: an analysis of the HELIUS Study. PLoS One, 10, e0137739. Doi:10.1371/journal.pone.0137739. [DOI] [PMC free article] [PubMed]
- Momma H., Sawada S.S., Kato K., Gando Y., Kawakami R., Miyachi M. Physical fitness tests and type 2 diabetes among Japanese: a longitudinal study from the Niigata Wellness Study. J. Epidemiol. 2019;29:8–13. doi: 10.2188/jea.JE20170280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Jaramillo P., Cohen D.D., Gómez-Arbeláez D., Bosch J., Dyal L., Yusuf S. Association of handgrip strength to cardiovascular mortality in pre-diabetic and diabetic patients: a subanalysis of the ORIGIN trial. Int. J. Cardiol. 2014;174:458–461. doi: 10.1016/j.ijcard.2014.04.013. [DOI] [PubMed] [Google Scholar]
- Leong D.P., Teo K.K., Rangarajan S., Lopez-Jaramillo P., Avezum A., Orlandini A. Prognostic value of grip strength: findings from the Prospective Urban Rural Epidemiology (PURE) Study. Lancet. 2015;386:266–273. doi: 10.1016/S0140-6736(14)62000-6. [DOI] [PubMed] [Google Scholar]
- Celis-Morales C.A., Welsh P., Lyall D.M., Steell L., Petermann F., Anderson J. Associations of grip strength with cardiovascular, respiratory, and cancer outcomes and all cause mortality: prospective cohort study of half a million UK Biobank participants. BMJ. 2018;361 doi: 10.1136/bmj.k1651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter E.A., Hargreaves M. Exercise, GLUT4, and skeletal muscle glucose uptake. Physiol Rev. 2013;93:993–1017. doi: 10.1152/physrev.00038.2012. [DOI] [PubMed] [Google Scholar]
- Castorena C.M., Arias E.B., Sharma N., Bogan J.S., Cartee G.D. Fiber type effects on contraction-stimulated glucose uptake and GLUT4 abundance in single fibers from rat skeletal muscle. Am. J. Physiol. Endocrinol. Metab. 2015;308:223–230. doi: 10.1152/ajpendo.00466.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichkendler M.H., Auerbach P., Rosenkilde M., Christensen A.N., Holm S., Petersen M.B. Exercise training favors increased insulin-stimulated glucose uptake in skeletal muscle in contrast to adipose tissue: a randomized study using FDG PET imaging. Am. J. Physiol. Metab. 2013;305:E496–E506. doi: 10.1152/ajpendo.00128.2013. [DOI] [PubMed] [Google Scholar]
- Marques-Vidal P., Vollenweider P., Waeber G., Jornayvaz F.R. Grip strength is not associated with incident type 2 diabetes mellitus in healthy adults: the CoLaus Study. Diabetes Res. Clin. Pract. 2017;132:144–148. doi: 10.1016/j.diabres.2017.08.004. [DOI] [PubMed] [Google Scholar]
- Larsen B.A., Wassel C.L., Kritchevsky S.B., Strotmeyer E.S., Criqui M.H., Kanaya A.M. Association of muscle mass, area, and strength with incident diabetes in older adults: the Health ABC Study. J. Clin. Endocrinol. Metab. 2016;101:1847. doi: 10.1210/jc.2015-3643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawman H.G., Troiano R.P., Perna F.M., Wang C.Y., Fryar C.D., Ogden C.L. Associations of Relative Handgrip Strength and Cardiovascular Disease Biomarkers in U.S. Adults, 2011–2012. Am. J. Prev. Med. 2016;50:677–683. doi: 10.1016/j.amepre.2015.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Justice, Japan, 2009. Industrial safety and health act, article 66 (medical examination). http://www.japaneselawtranslation.go.jp/law/detail/?id=3257&vm=04&re=01 (accessed June 26, 2019).
- Kinoshita, M., Yokote, K., Arai, H., Iida, M., Ishigaki, Y., Umemoto, S., et al., 2018. Committee for Epidemiology and Clinical Management of Atherosclerosis. Japan Atherosclerosis Society (JAS) guidelines for prevention of atherosclerotic cardiovascular diseases 2017. J. Atheroscler. Thromb. 25, 846–984. doi:10.5551/jat.GL2017. [DOI] [PMC free article] [PubMed]
- NHNES, 2016. Muscle strength procedure Manual. https://wwwn.cdc.gov/nchs/data/.../2011.../manuals/muscle_strength_proc_manual.pdf (accessed June 25, 2016).
- MHLW, 2017. Japanese ministry of health, labour and welfare standard health examination questionnaire. http://www.mhlw.go.jp/seisakunitsuite/bunya/kenkou_iryou/kenkou/seikatsu/dl/hoken-program2_02.pdf. (accessed December 25, 2017).
- White I.R., Royston P., Wood A.M. Multiple imputation using chained equations: issues and guidance for practice. Stat. Med. 2011;30:377–399. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- Hu S., Gu Y., Lu Z., Zhang Q., Liu L., Meng G. Relationship between grip strength and prediabetes in a large-scale adult population. Am. J. Prev. Med. 2019;56:844–851. doi: 10.1016/j.amepre.2019.01.013. [DOI] [PubMed] [Google Scholar]
- Mainous A.G., Tanner R.J., Anton S.D., Jo A. Low grip strength and prediabetes in normal-weight adults. J. Am. Board. Fam. Med. 2016;29:280–282. doi: 10.3122/jabfm.2016.02.150262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Oliveira P.A., Blasczyk J.C., Junior G.S., Lagoa K.F., Soares M., de Oliveira R.J. Effects of elastic resistance exercise on muscle strength and functional performance in healthy adults: a systematic review and meta-analysis. J. Phys. Act Heal. 2016;14:317–327. doi: 10.1123/jpah.2016-0415. [DOI] [PubMed] [Google Scholar]
- Price, A.J., Crampin, A.C., Branson, K., Glynn, J.R., Nyirenda, M., Smeeth FMedSCi, L., et al., 2018. Prevalence of obesity, hypertension, and diabetes, and cascade of care in sub-Saharan Africa: a cross-sectional, population-based study in rural and urban Malawi. Lancet Diabetes Endocrinol. 6, 208–230. doi:10.1016/S2213-8587(17)30432-1. [DOI] [PMC free article] [PubMed]
- Kim B.C., Kim M.K., Han K., Lee S.-Y., Lee S.-H., Ko S.-H. Low muscle mass is associated with metabolic syndrome only in nonobese young adults: the Korea National Health and Nutrition Examination Survey 2008–2010. Nutr. Res. 2015;35:1070–1078. doi: 10.1016/j.nutres.2015.09.020. [DOI] [PubMed] [Google Scholar]
- Sénéchal M., Johannsen N.M., Swift D.L., Earnest C.P., Lavie C.J., Blair S.N. Association between changes in muscle quality with exercise training and changes in cardiorespiratory fitness measures in individuals with type 2 diabetes mellitus: results from the HART-D Study. PLoS One. 2015;10 doi: 10.1371/journal.pone.0135057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heianza Y., Arase Y., Fujihara K., Tsuji H., Saito K., Hsieh S.D. Screening for pre-diabetes to predict future diabetes using various cut-off points for HbA1c and impaired fasting glucose: the Toranomon Hospital Health Management Center Study 4 (TOPICS 4) Diabet Med. 2012;29:e279–e285. doi: 10.1111/j.1464-5491.2012.03686.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.