Abstract
The eosinophil granule proteins, major basic protein (MBP) and eosinophil cationic protein (ECP), activate mast cells during inflammation; however the mechanism responsible for this activity is poorly understood. We found that some theoretical tryptase-digested fragments of MBP and ECP induced degranulation of human cord blood-derived mast cells (HCMCs). The spectrum of activities of these peptides in HCMCs coincided with intracellular Ca2+ mobilization activities in Mas-related G-protein coupled receptor family member X2 (MRGPRX2)-expressing HEK293 cells. Two peptides corresponding to MBP residues 99–110 (MBP (99–110)) and ECP residues 29–45 (ECP (29–45)), respectively, induced degranulation of HCMCs and intracellular Ca2+ mobilization in MRGPRX2-expressing HEK293 cells in a concentration-dependent manner. Stimulation with MBP (99–110) or ECP (29–45) induced the production of prostaglandin D2 by HCMCs. The activities of MBP (99–110) and ECP (29–45) in both HCMCs and MRGPRX2-expressing HEK293 cells were inhibited by MRGPRX2-specific antagonists. In conclusion, these results indicated that MBP and ECP fragments activate HCMCs, and it may occur via MRGPRX2. Our findings suggest that tryptase-digested fragments of eosinophil cationic proteins acting via the MRGPRX2 pathway may further our understanding of mast cell/eosinophil communication.
Keywords: Cationic peptide, ECP, MBP, Mast cell/eosinophil communication, MRGPRX2, Tryptase
Abbreviations: ECP, eosinophil cationic protein; GPCR, G protein-coupled receptor; HCMC, human cord blood-derived mast cell; MBP, major basic protein; MC, mast cell; MRGPRX2, Mas-related G protein-coupled receptor X2; PGD2, prostaglandin D2
Highlights
-
•
Mast cell activators were found in tryptase-fragments from MBP and ECP.
-
•
These fragments activated MRGPRX2-expressing cells.
-
•
MRGPRX2 antagonists inhibited mast cell activation caused by active fragments.
-
•
Active fragments may work as mediators in mast cell/eosinophil communication.
1. Introduction
Systemic or localized tissue eosinophilia is a frequent occurrence in atopic diseases, parasitic infections, and other chronic inflammatory states [1]. The main constituents of eosinophil-derived granules are major basic protein (MBP), eosinophil cationic protein (ECP), eosinophil-derived neurotoxin, and eosinophil peroxidase. Elevated concentrations of MBP and ECP have been observed in serum from patients with eosinophilia [2], sputum from asthmatic patients [3], and at sites of eosinophil-rich inflammation [4]. These proteins are able to exert a variety of biological actions and can indirectly affect microvascular permeability by stimulating perivascular mast cells (MCs) [5]. It has been suggested that cross-talk occurs between MCs and eosinophils that infiltrate the tissue in increased numbers during the late-phase reaction [6]. Eosinophil granule proteins act on MCs, and MC degranulation induces the onset of hyper-reactivity at sites of chronic inflammation [7]. In addition, an association between activated eosinophils and MCs has been demonstrated in the pathology of allergic diseases [8].
Initial studies of the histamine-releasing ability of eosinophil granule proteins investigated the ability of MBP to induce histamine release from human basophils and rat peritoneal MCs [9]. ECP, but not eosinophil-derived neurotoxin, is known to stimulate histamine release from rat peritoneal MCs via a process requiring both Ca2+ and metabolic energy [10]. Furthermore, antigen-challenged rat peritoneal MCs release histamine following incubation with MBP or ECP, suggesting that MCs in vivo can be reactivated during a late-phase reaction to release histamine via a non-IgE mechanism [7]. Okayama et al. suggested that MBP affects the same binding site on skin MCs as that of substance P [11]. Furthermore, rat peritoneal and human skin MCs release histamine when incubated with MBP or ECP in a pertussis toxin-sensitive Gi protein-dependent mechanism, similar to the mechanisms of cationic compounds such as compound 48/80 and substance P [7,12]. Fujisawa et al. reported that histamine release by MBP was reduced in skin-derived cultured MCs transduced with short hairpin RNA targeting Mas-related G protein-coupled receptor family member X2 (MRGPRX2) [13].
MRGPRX2 has been identified as a human G protein-coupled receptor (GPCR) for basic secretagogues, including cortistatin, somatostatin, substance P [14], and pro-adrenomedullin peptide, as well as for antimicrobial peptides human-beta defensins and LL-37, and several drugs, including morphine and icatibant [15,16]. MRGPRX2 ligands are less than 4000 Da in size and include cationic regions or hydrophobic amino acids, but have no common sequence [14,16]. MBP residues 89–117 can mimic the abilities of MBP to stimulate histamine release and leukotriene C4 production by basophils [17]. However, despite substantial evidence supporting the participation of MCs in inflammation induced by MBP and ECP, the physiological mechanisms responsible for the degranulation of MCs by these proteins remain unresolved.
MCs and eosinophils occur in close proximity in several disorders, forming an allergic effector unit (AEU) [18]. Several tryptases from MCs are detected in the local area of asthma and other allergic disorders [19]. Considering that MC tryptases can stimulate eosinophil activation and degranulation by cleavage of protease-activated receptor 1 and 2 [20,21], it is conceivable that MC tryptase can also digest MBP and ECP released from eosinophils at inflammatory sites. We hypothesized that fragments from MBP and ECP could subsequently stimulate MRGPRX2 resulting in the activation of MCs, and that this degradation pathway might provide a novel communication system between MCs and eosinophils. The present study aimed to test this hypothesis by investigating the effects of fragments of MBP and ECP based on the theoretical fragmentation of these proteins at tryptase-digestion sites, and to determine whether these MBP and ECP fragments could induce MC degranulation via MRGPRX2 by this mechanism.
2. Methods
2.1. Materials
Sequential peptides of MBP and ECP were designed as presented in Table 1 and were synthesized automatically by solid-phase methods, as described previously [16]. The theoretical tryptic-cleavage fragments of MBP and ECP used in the present study are summarized in Table 1. MRGPRX2 antagonists were obtained from a screening of house chemical library [22]. Briefly, our in-house chemical library consists of approximately 12,000 commercially available compounds. A screening campaign led us to identify two different heterocyclic compounds, compound 1 (MW. 223.26) and compound 2 (MW. 268.31), which inhibit MRGPRX2-mediated intracellular Ca2+ mobilization induced by basic secretagogues, including substance P, by use of a stable-expression system in HEK293 cells. These compounds inhibit MRGPRX2-mediated intracellular Ca2+ mobilization by a concentration mechanism with IC50 values in the lower single-digit micromolar range. To verify the specificities of the compounds for MRGPRX2, we tested the inhibitory activities of these compounds in two representative G protein-coupled receptors distinct from MRGPRX2: (1) classical substance P receptor, NK-1R; and (2) M2R, a Gi protein-coupled receptor. These compounds did not block NK-1R or M2R-mediated intracellular Ca2+ mobilization. Furthermore, we confirmed that these compounds blocked GTP-γS-binding activities in MRGPRX2-expressing membranes stimulated with substance P.
Table 1.
Synthetic peptide sequences of MBP and ECP and their pI valuesa.
| MBP peptide | |||
|---|---|---|---|
| No. | Position | Sequence | pI |
| 1 | 1–8 | TCRYLLVR | 9.50 |
| 2 | 9–21 | SLQTFSQAWFTCR | 7.96 |
| 3 | 9–22 | SLQTFSQAWFTCRR | 10.35 |
| 4 | 22–39 | RCYRGNLVSIHNFNINYR | 10.05 |
| 5 | 23–39 | CYRGNLVSIHNFNINYR | 9.31 |
| 6 | 26–39 | GNLVSIHNFNINYR | 8.75 |
| 7 | 40–57 | IQCSVSALNQGQVWIGGR | 8.25 |
| 8 | 58–65 | ITGSGRCR | 10.35 |
| 9 | 58–66 | ITGSGRCRR | 11.70 |
| 10 | 58–74 | ITGSGRCRR FQWVDGSR | 11.52 |
| 11 | 64–74 | CRRFQWVDGSR | 10.26 |
| 12 | 66–74 | RFQWVDGSR | 9.60 |
| 13 | 67–74 | FQWVDGSR | 5.84 |
| 14 | 75–88 | WNFAYWAAHQPWSR | 8.75 |
| 15 | 89–98 | GGHCVALCTR | 8.08 |
| 16 | 89–103 | GGHCVALCTRGGYWR | 8.96 |
| 17 | 99–109 | GGYWRRAHCLR | 10.76 |
| 18 | 99–110 | GGYWRRAHCLRR | 11.54 |
| 19 | 99–117 | GGYWRRAHCLRRLPFICSY | 10.09 |
| 20 | 104–117 | RAHCLRRLPFICSY | 9.69 |
| 21 | 105–117 | AHCLRRLPFICSY | 8.96 |
| 22 |
110–117 |
RLPFICSY |
8.22 |
| ECP peptide | |||
| No. |
Position |
Sequence |
pI |
| 1 | 8–24 | AQWFAIQHISLNPCT | 9.80 |
| 2 | 23–34 | CTIAMRAINNYR | 9.50 |
| 3 | 23–36 | CTIAMRAINNYRWR | 10.76 |
| 4 | 24–38 | TIAMRAINNYRWRCK | 10.92 |
| 5 | 29–36 | AINNYRWR | 10.84 |
| 6 | 29–38 | AINNYRWRCK | 10.05 |
| 7 | 29–45 | AINNYRWRCKNQNTFLR | 10.92 |
| 8 | 35–45 | WRCKNQNTFLR | 10.86 |
| 9 | 37–45 | CKNQNTFLR | 9.51 |
| 10 | 46–61 | TTFANVVNVCGNQSIR | 7.91 |
| 11 | 62–73 | CPHNRTLNNCHR | 9.02 |
| 12 | 62–75 | CPHNRTLNNCHRSR | 10.41 |
| 13 | 62–77 | CPHNRTLNNCHRSRFR | 11.53 |
| 14 | 67–75 | TLNNCHRSR | 10.35 |
| 15 | 67–77 | TLNNCHRSRFR | 11.70 |
| 16 | 78–97 | VPLLHCDLINPGAQNISNCR | 6.70 |
| 17 | 98–105 | YADRPGRR | 10.74 |
| 18 | 98–114 | YADRPGRRFYVVACDNR | 9.31 |
| 19 | 98–117 | YADRPGRRFYVVACDNRDPR | 9.31 |
| 20 | 105–114 | RFYVVACDNR | 8.22 |
| 21 | 105–117 | RFYVVACDNRDPR | 8.22 |
| 22 | 105–121 | RFYVVACDNRDPRDSPR | 8.22 |
| 23 | 106–114 | FYVVACDNR | 5.83 |
| 24 | 106–117 | FYVVACDNRDPR | 5.95 |
| 25 | 106–117 | FYVVACDNRDPRDSPR | 6.03 |
| 26 | 115–133 | DPRDSPRYPVVPVHLDTTI | 5.30 |
| 27 | 118–133 | DSPRYPVVPVHLDTTI | 5.21 |
| 28 | 122–133 | YPVVPVHLDTTI | 5.08 |
Theoretical isoelectric points (pI) were calculated using the algorithm in the ExPASy Compute pI/Mw program [31].
2.2. Preparation of HCMCs
Human cord blood CD34 + cells were separated from human cord blood mononuclear cells (Stemcyte, Covina, CA) by a CD34 + progenitor cell isolation kit (Miltenyi Biotec, North Rhine-Westphalia, Germany). Human cord blood-derived MCs were induced from cord blood CD34 + cells as described previously [16].
2.3. DNA construction and MRGPRX2-Expressing cells
MRGPRX2-stably expressing HEK293 cells were established and grown in Dulbecco's Modified Eagle Medium containing 200 μg/ml hygromycin B supplemented with 10% fetal bovine serum, 100 U/ml penicillin, and 100 μg/ml streptomycin, as described [16].
2.4. Activation of HCMCs and PGD2 EIA assays
Human CMCs cultured for over 8 weeks as described above were washed twice with Iscove's modified Dulbecco's medium supplemented with 0.1% bovine serum albumin, 1% insulin-transferrin-selenium, and 2-mercaptoethanol, and resuspended in the same medium at a density of 1 × 105 cells/ml. Cells (1.5 × 104) were aliquoted in 96-well culture plates, and then challenged with the peptides in triplicate for 30 min with or without MRGPRX2 antagonists. The supernatant was incubated for 2 h with an assay mixture containing 1 mM p-nitrophenyl-N-acetyl-b-d-glucosamine in 0.1 M citrate buffer (pH 4.0), and the reaction was then stopped by adding 0.1 M carbonate buffer (pH 10). Total cellular content of β-hexosaminidase was established by adding distilled water to achieve complete cell lysis. Colorimetric absorbance was measured at 405 nm. The percentage degranulation was calculated as ((x − b)/(t − b)) × 100, where x is the amount of β-hexosaminidase released from the stimulated cells, b is a blank, and t is total cellular content. The generation of PGD2 in the supernatants was measured with an EIA for PGD2 (Cayman Chemical, Ann Arbor, MI).
2.5. Intracellular calcium measurement
Cells were loaded with 2 μM Fura-2 AM (Dojindo laboratories, Kumamoto, Japan) for 30 min at room temperature. The intracellular calcium concentration was measured in response to activation by stimuli using a Functional Drug Screening System (FDSS, Hamamatsu Photonics, Hamamatsu, Japan) as described previously [16].
2.6. Statistical analysis
The results are shown as the means ± SD. Parametric analysis (ANOVA, followed by Tukey-Kramer post-hoc test) was used to compare the effects between groups. The level of statistical significance used was P < 0.01.
3. Results
3.1. MBP and ECP peptides increased degranulation of human cord blood-derived mast cells (HCMCs) and stimulated MRGPRX2 activities
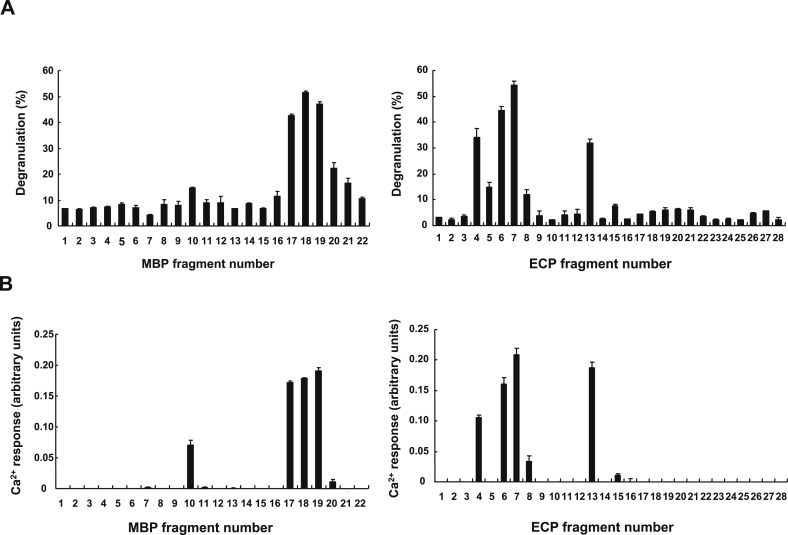
We investigated the abilities of several synthesized peptides covering the full sequences of MBP and ECP, respectively (Table 1), to induce the degranulation of HCMCs. Some synthetic fragments of both proteins showed potent induction of HCMC degranulation (Figs. 1A and B). The degranulation-inducing activities were located in the C-terminal region of MBP and in the N-terminal region of ECP. Among these functional fragments, MBP residues 99–110 (MBP (99–110)) and ECP residues 29–45 (ECP (29–45)) were the most active. The spectrum of activities of the MBP and ECP peptide fragments for intracellular Ca2+ mobilization in MRGPRX2-expressing HEK293 cells was closely consistent with their activities in HCMCs (Figs. 1A and B). The two peptides corresponding to MBP (99–110) and ECP (29–45) showed greater activities in relation to HCMC degranulation and intracellular Ca2+ mobilization in MRGPRX2-expressing HEK293 cells compared with the other tested peptides. The activities of MBP (99–110) and ECP (29–45) in HCMCs were therefore characterized further.
Fig. 1.
Effects of synthetic peptides of MBP and ECP on HCMC degranulation (A) and intracellular Ca2+mobilization in MRGPRX2-expressing HEK293 cells (B). HCMCs (1 × 104) were incubated with 10 μM synthetic peptides for 30 min and degranulation was assessed by the release of β-hexosaminidase activity into the supernatant (no peptide control value; 2.0 ± 0.2). MRGPRX2-expressing HEK293 cells (1 × 104) loaded with Fura-2-AM were stimulated with 30 μM peptides (no peptide control value; 0.001 ± 0.001). The activity values of 10 μM Substance P, which activates both mast cells and MRGPRX2 we previously reported [16,22], were 64.4 ± 0.5 for A and 0.239 ± 0.022 for B. Data represent mean ± standard deviation of triplicate determinations.
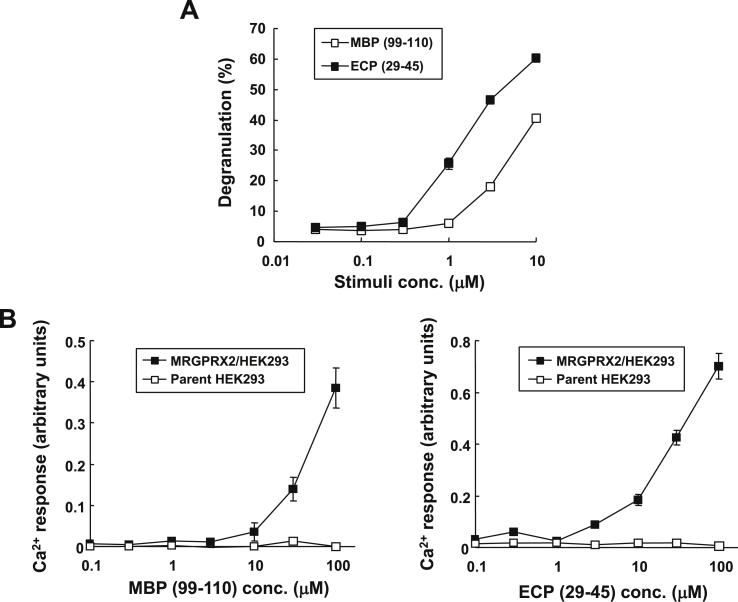
3.2. MBP and ECP peptides induced HCMC degranulation
We characterized the HCMC-degranulation activities of MBP (99–110) and ECP (29–45) and showed that both peptides induced the degranulation of HCMCs in concentration-dependent manners, with maximal effects at 10 μM (40% ± 3% and 60% ± 2%, respectively; Fig. 2A). To demonstrate the activation of MRGPRX2 by MBP (99–110) and ECP (29–45), we used the intracellular Ca2+ mobilization assay in MRGPRX2-expressing HEK293 cells, comparing parent HEK293 cells. Fig. 2B showed that MBP (99–110) and ECP (29–45) induced the mobilization of intracellular Ca2+ in MRGPRX2-expressing HEK293 cells in a concentration-dependent manner, but not in parent HEK293 cells.
Fig. 2.
Degranulation of HCMCs (A) and intracellular Ca2+mobilization in MRGPRX2-expressing cells (B) by MBP (99–110) and ECP (29–45). HCMCs were incubated with the indicated concentrations of MBP (99–110, fragment No. 18 in Fig. 1) and ECP (29–45, fragment No. 7 in Fig. 1) for 30 min and degranulation was assessed by the release of β-hexosaminidase activity into the supernatants. MRGPRX2-expressing HEK293 cells or parental HEK293 cells (1 × 104 cells) loaded with Fura-2-AM were stimulated with the indicated concentrations of MBP (99–110) and ECP (29–45). Data represent mean ± standard deviation of triplicate determinations.
3.3. MRGPRX2 was responsible for the activation of HCMCs by MBP and ECP peptides
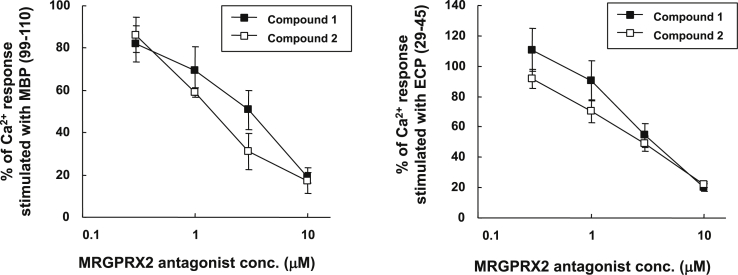
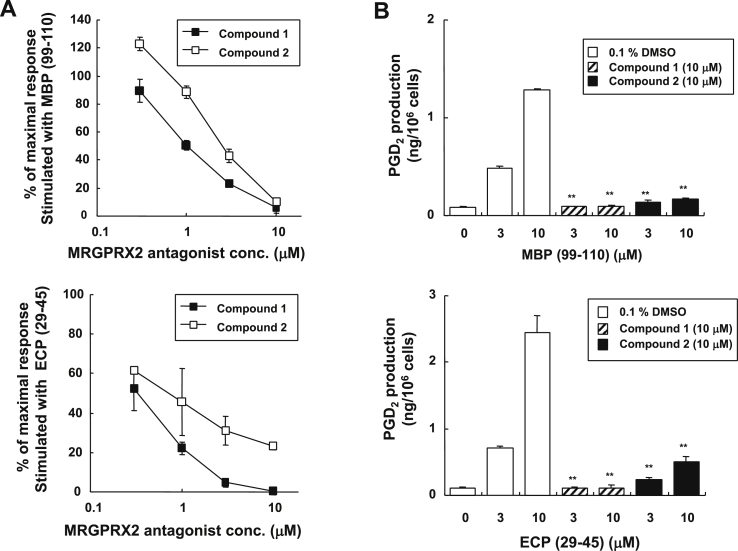
Through chemical library screening, we previously identified novel antagonists against MRGPRX2 for blocking the MRGPRX2-mediated Ca2+ mobilization using MRGPRX2-expressing HEK293 cells [22]. Two chemically distinct types of antagonists were identified, referred to as compound 1 and 2. We assessed the inhibitory effects of these two MRGPRX2 antagonists on intracellular Ca2+ mobilization by MBP (99–110) and ECP (29–45). Compound 1 and 2 inhibited the intracellular Ca2+ mobilization induced by 30 μM MBP (99–110) and 30 μM ECP (29–45) in dose-dependent manners, with half maximal inhibitory concentration (IC50) values of 3.1 μM and 1.4 μM (MBP), and 3.5 μM and 2.9 μM (ECP), respectively (Fig. 3). Moreover, we examined the effects of these MRGPRX2 antagonists on the degranulation of HCMCs stimulated by MBP (99–110) and ECP (29–45). The inhibitory evaluation of compound 1 and 2 on HCMC degranulation was based on the intracellular Ca2+ mobilization in MRGPRX2-expressing HEK293 cells. Compounds 1 and 2 both inhibited HCMC degranulation induced by MBP (99–110) (IC50 values of 1.0 and 2.5 μM, respectively; Fig. 4A) and by ECP (29–45) (IC50 values of 0.3 and 0.7 μM, respectively; Fig. 4A) in concentration-dependent manners. Several studies have demonstrated that eicosanoids are released from MCs in response to MBP and ECP [7,12,23]. We therefore evaluated the production of the mediator PGD2 in response to increasing concentrations of MBP (99–110) and ECP (29–45). No additional increase of PGD2 was detected in parallel samples in a 0.5% Nonidet P-40-treated HCMC lysate, suggesting that PGD2 released in the supernatants was synthesized by HCMCs de novo. The MBP and ECP peptides both caused the de novo synthesis of PGD2 by HCMCs (Fig. 4B). Consistent with the degranulation data (Fig. 4A), we observed a strong suppression of PGD2 production by MRGPRX2 antagonists (Fig. 4B). These results demonstrate that MBP (99–110) and ECP (29–45) could activate HCMCs via MRGPRX2.
Fig. 3.
Inhibitory effects of MRGPRX2 antagonists on intracellular Ca2+mobilization in MRGPRX2-expressing HEK293 cells stimulated by MBP (99–110) or ECP (29–45). MRGPRX2-expressing HEK293 cells were stimulated with 30 μM MBP (99–110) and ECP (29–45) in the presence of the indicated concentrations of compound 1 or compound 2. Data represent mean ± standard deviation of triplicate determinations. All experiments using antagonists were performed in the presence of 0.1% DMSO. We confirmed that the solvents did not affect on HEK293 cell activation.
Fig. 4.
Effects of MRGPRX2 antagonists on HCMC activation stimulated by MBP (99–110) and ECP (29–45). Cells were stimulated with 10 μM MBP (99–110) and ECP (29–45) in the presence of the indicated concentrations of compound 1 or 2, and HCMC degranulation was assessed by the release of β-hexosaminidase activity into the supernatants after 30 min (A). PGD2 production was assessed after 30 min of incubation with MBP (99–110) or ECP (29–45) at the concentrations indicated (B). A value of 100% was given to cells without antagonists. Data represent mean ± standard deviation of triplicate determinations. **, P < 0.01 compared with cells without MRGPRX2 antagonists. All experiments using antagonists were performed in the presence of 0.1% DMSO. We confirmed that the solvents did not affect on mast cell activation.
4. Discussion
The current results showed that the peptides that are mapped near the C-terminal of MBP and the N-terminal of ECP with high calculated pI values, but not other peptides with high pI values, elicited MC degranulation (Table 1, Fig. 1). The biological actions of MBP and ECP are usually associated with their high arginine content and strong net positive charge [24]. Full-length MBP and ECP are highly cationic and can activate MC, but EDN/EPX, which lacks MC activation, is less cationic [13]. These findings indicate that several cationic molecules derived from eosinophil will work as mediators in mast cell-eosinophil communication. However, the positive charge cannot solely explain the effect of cationic eosinophil granule proteins on MCs, because if MC activation was solely due to the cationic charge, all cationic peptides with a high pI value would elicit mediator release from MCs (Table 1, Fig. 1). The ability to release mediators from MCs was therefore not correlated with the pI value. In support of this conclusion, Furuta et al. suggested that poly-l-arginine is not an ideal alternative to authentic native MBP in terms of MBP/MC interactions [25]. Our findings therefore implied that MBP and ECP fragments activated MCs via a mechanism mediated specifically through MRGPRX2, but that this mechanism was not simply a positive-charge-dependent mechanism. Moreover, we clarified that both active fragments, MBP (99–110) and ECP (29–45), activated HCMCs through the GPCR MRGPRX2, using MRGPRX2 antagonists (Fig. 4). These MRGPRX2 antagonists inhibited both HCMC degranulation and the de novo synthesis of PGD2 by HCMCs induced by MBP (99–110) and ECP (29–45) (Fig. 4). Both antagonists seemed to inhibit the response to MBP (99–110) and ECP (29–45) almost equally in MRGPRX2-expressing cells. But, compound 1 inhibited the HCMC responses more potently than compound 2 (Fig. 3, Fig. 4). We previously reported that HCMCs were more sensitive to basic secretagogues such as substance P, known as MRGPRX2 ligands, than MRGPRX2-expressing HEK293 cells [16,22]. Similarly, HCMCs were more sensitive to MBP (99–110) and ECP (29–45) than MRGPRX2-expressing HEK293 cells (Fig. 2). Thus, the more sensitive assay with HCMCs may be able to detect the difference in the inhibitory activity between two antagonists. Based on these findings, we concluded that the active peptides of MBP and ECP elicited inflammatory mediators from HCMCs through MRGPRX2. We propose that the MBP (99–110) and ECP (29–45) fragments may share the MC-activation activities of MBP and ECP, respectively. Several studies of the crystal structures of MBP and ECP indicated that the sites corresponding to their respective potentially active fragments are not exposed effectively [[26], [27]], such that the MBP (99–110) region sits in a shallow groove, while the ECP (29–45) region is buried in a groove at the interface by two internal loops (Supplementary Fig. S1). Strong conformational changes may therefore be required to allow these regions of MBP and ECP to act as ligand-binding sites for MRGPRX2 in the respective full-length proteins. Serine protease tryptase is the most abundant mediator stored in MC granules, and several studies reported elevated levels of this enzyme, as well as MBP and ECP, in relation to inflammatory actions [28]. Tryptase localized in MC granules constitutes up to 25% of the total MC protein content [29]. Unlike most trypsin-like serine proteases, tryptases are activated intracellularly and exocytosed from secretory granules as a consequence of inflammatory activation of MCs, together with histamine and other preformed mediators [30]. After release, tryptases are resistant to circulating inhibitors of other trypsin-like proteases and may remain active for longer after release than other proteases [30]. Although the presence of biologically active peptides of MBP and ECP at inflammatory sites remains unclear, it is possible that tryptase-digested fragments of MBP and ECP may exist in patients with chronic inflammatory conditions. MRGPRX2 on MCs exhibits promiscuous ligand recognition, and it is therefore plausible if several fragments of MBP and ECP could activate MCs via MRGPRX2 like the single intact molecules. Late/chronic allergy is known to involve both MCs and eosinophils, though the manner in which these two cell types co-function to perpetuate the response is less well known. We propose that tryptase-digested fragments of MBP and ECP may serve as novel amplification factors to augment short- and long-term activation of MCs via MRGPRX2 in the allergic effector unit.
In summary, the data presented here indicate that the theoretical tryptase-digested peptide fragments from MBP and ECP could activate human MCs via an MRGPRX2 pathway. The active fragments may mediate MC/eosinophil communication in inflammation.
Authorship contributions
H.O. directed and performed experiments for all biological assays. M.F. and K.E. carried out chemical library screening for MRGPRX2 antagonists. M.N. directed all experiments and led the project as a representative. All authors contributed to the manuscript writing. H.O. wrote the manuscript with input from all coauthors.
CRediT authorship contribution statement
Hiroyuki Ogasawara: Conceptualization, Writing - review & editing. Masahiro Furuno: Validation. Koji Edamura: Validation. Masato Noguchi: Writing - review & editing.
Declaration of competing interest
The authors declare that they have no conflict of interest.
Acknowledgments
We thank Dr. Tatemoto for providing peptide synthesis, and Yuko Nozaki and Keiko Tomura for supporting the construction of the plasmids.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bbrep.2019.100719.
Contributor Information
Hiroyuki Ogasawara, Email: hiroyuki.ogasawara@jt.com.
Masahiro Furuno, Email: masahiro.furuno@jt.com.
Koji Edamura, Email: koji.edamura@jt.com.
Masato Noguchi, Email: martn@t00.itscom.net.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Klion A.D. Eosinophilia: a pragmatic approach to diagnosis and treatment. Hematol. Am. Soc. Hematol. Educ. Program. 2015:92–97. doi: 10.1182/asheducation-2015.1.92. [DOI] [PubMed] [Google Scholar]
- 2.Wassom D.L., Loegering D.A., Solley G.O., Moore S.B., Schooley R.T., Fauci A.S., Gleic G.J. Elevated serum levels of the eosinophil granule major basic protein in patients with eosinophilia. J. Clin. Investig. 1981;67:651–661. doi: 10.1172/JCI110080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frigas E., Loegering D.A., Solley G.O., Farrow G.M., Gleich G.J. Elevated levels of the eosinophil granule major basic protein in the sputum of patients with bronchial asthma. Mayo Clin. Proc. 1981;56:345–353. [PubMed] [Google Scholar]
- 4.Filley W.V., Holley K.E., Kephart G.M., Gleich G.J. Identification by immunofluorescence of eosinophil granule major basic protein in lung tissues of patients with bronchial asthma. Lancet. 1982;2:11–16. doi: 10.1016/s0140-6736(82)91152-7. [DOI] [PubMed] [Google Scholar]
- 5.Foreman J.C., Lichtenstein L.M. Induction of histamine secretion by polycations. Biochim. Biophys. Acta. 1980;629:587–603. doi: 10.1016/0304-4165(80)90164-6. [DOI] [PubMed] [Google Scholar]
- 6.Levi-Schaffer F., Temkin V., Malamud V., Feld S., Zilberman Y. Mast cells enhance eosinophil survival in vitro, role of TNF-alpha and granulocyte-macrophage colony-stimulating factor. J. Immunol. 1998;160:5554–5562. http://www.jimmunol.org/content/160/11/5554 [PubMed] [Google Scholar]
- 7.Piliponsky A.M., Pickholtz D., Gleich G.J., Levi-Schaffer F. Human eosinophils induce histamine release from antigen-activated rat peritoneal mast cells: a possible role for mast cells in late-phase allergic reactions. J. Allergy Clin. Immunol. 2001;107:993–1000. doi: 10.1067/mai.2001.114656. [DOI] [PubMed] [Google Scholar]
- 8.Beasley R., Roche W.R., Roberts J.A., Holgate S.T. Cellular events in the bronchi in mild asthma and after bronchial provocation. Am. Rev. Respir. Dis. 1989;139:806–817. doi: 10.1164/ajrccm/139.3.806. [DOI] [PubMed] [Google Scholar]
- 9.O'Donnell M.C., Ackerman S.J., Gleich G.J., Thomas L.L. Activation of basophil and mast cell histamine release by eosinophil granule major basic protein. J. Exp. Med. 1993;157:1981–1991. doi: 10.1084/jem.157.6.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zheutlin L.M., Ackerman S.J., Gleich G.J., Thomas L.L. Stimulation of basophil and rat mast cell histamine release by eosinophil granule-derived cationic proteins. J. Immunol. 1984;133:2180–2185. http://www.jimmunol.org/content/133/4/2180 [PubMed] [Google Scholar]
- 11.Okayama Y., el-Lati S.G., Leiferman K.M., Church M.K. Eosinophil granule proteins inhibit substance P-induced histamine release from human skin mast cells. J. Allergy Clin. Immunol. 1994;93:900–909. doi: 10.1016/0091-6749(94)90384-0. [DOI] [PubMed] [Google Scholar]
- 12.Piliponsky A.M., Gleich G.J., Nagler A., Bar I., Levi-Schaffer F. Non-IgE-dependent activation of human lung- and cord blood-derived mast cells is induced by eosinophil major basic protein and modulated by the membrane form of stem cell factor. Blood. 2003;101:1898–1904. doi: 10.1182/blood-2002-05-1488. [DOI] [PubMed] [Google Scholar]
- 13.Fujisawa D., Kashiwakura J., Kita H., Kikukawa Y., Fujitani Y., Sasaki-Sakamoto T., Kuroda K., Nunomura S., Hayama K., Terui T., Ra C., Okayama Y. Expression of Mas-related gene X2 on mast cells is upregulated in the skin of patients with severe chronic urticaria. J. Allergy Clin. Immunol. 2014;134:622–633. doi: 10.1016/j.jaci.2014.05.004. e9. [DOI] [PubMed] [Google Scholar]
- 14.Robas N., Mead E., Fidock M. MRGPRX2 is a high potency cortistatin receptor expressed in dorsal root ganglion. J. Biol. Chem. 2003;278:44400–44404. doi: 10.1074/jbc.M302456200. [DOI] [PubMed] [Google Scholar]
- 15.Kamohara M., Matsuo A., Takasaki J., Kohda M., Matsumoto M., Matsumoto S., Soga T., Hiyama H., Kobori M., Katou M. Identification of MRGPRX2 as a human G-protein-coupled receptor for proadrenomedullin N-terminal peptides. Biochem. Biophys. Res. Commun. 2005;330:1146–1152. doi: 10.1016/j.bbrc.2005.03.088. [DOI] [PubMed] [Google Scholar]
- 16.Tatemoto K., Nozaki Y., Tsuda R., Konno S., Tomura K., Furuno M., Ogasawara H., Edamura K., Takagi H., Iwamura H., Noguchi M., Naito T. Immunoglobulin E-independent activation of mast cell is mediated by Mrg receptors. Biochem. Biophys. Res. Commun. 2006;349:1322–1328. doi: 10.1016/j.bbrc.2006.08.177. [DOI] [PubMed] [Google Scholar]
- 17.Thomas L.L., Kubo H., Loegering D.J., Spillard K., Weaver A.J., McCormick D.J., Weiler C., Gleich G.J. Peptide-based analysis of amino acid sequences important to the biological activity of eosinophil granule major basic protein. Immunol. Lett. 2001;78:175–181. doi: 10.1016/s0165-2478(01)00249-8. [DOI] [PubMed] [Google Scholar]
- 18.Minai-Fleminger Y., Elishmereni M., Vita F., Soranzo M.R., Mankuta D., Zabucchi G., Levi-Schaffer F. Ultrastructural evidence for human mast cell-eosinophil interactions in vitro. Cell Tissue Res. 2010;341:405–415. doi: 10.1007/s00441-010-1010-8. [DOI] [PubMed] [Google Scholar]
- 19.Schwartz L.B., Yunginger J.W., Miller J., Bokhari R., Dull D. Time course of appearance and disappearance of human mast cell tryptase in the circulation after anaphylaxis. J. Clin. Investig. 1989;83:1551–1555. doi: 10.1172/JCI114051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Temkin V., Kantor B., Weg V., Hartman M.L., Levi-Schaffer F. Tryptase activates the mitogen-activated protein kinase/activator protein-1 pathway in human peripheral blood eosinophils, causing cytokine production and release. J. Immunol. 2002;169:2662–2669. doi: 10.4049/jimmunol.169.5.2662. [DOI] [PubMed] [Google Scholar]
- 21.Elishmereni M., Bachelet I., Nissim Ben-Efraim A.H., Mankuta D., Levi-Schaffer F. Interacting mast cells and eosinophils acquire an enhanced activation state in vitro. Allergy. 2013;68:171–179. doi: 10.1111/all.12059. [DOI] [PubMed] [Google Scholar]
- 22.Ogasawara H., Furuno M., Edamura K., Noguchi M. Novel MRGPRX2 antagonists inhibit IgE-independent activation of human umbilical cord blood-derived mast cells. J. Leukoc. Biol. 2019;106:1069–1077. doi: 10.1002/JLB.2AB1018-405R. [DOI] [PubMed] [Google Scholar]
- 23.Patella V., de Crescenzo G., Marinò I., Genovese A., Adt M., Gleich G.J., Marone G. Eosinophil granule proteins activate human heart mast cells. J. Immunol. 1996;157:1219–1225. http://www.jimmunol.org/content/157/3/1219 [PubMed] [Google Scholar]
- 24.Plager D.A., Loegering D.A., Weiler D.A., Checkel J.L., Wagner J.M., Clarke N.J., Naylor S., Page S.M., Thomas L.L., Akerblom I., Cocks B., Stuart S., Gleich G.J. A novel and highly divergent homolog of human eosinophil granule major basic protein. J. Biol. Chem. 1999;274:14464–14473. doi: 10.1074/jbc.274.20.14464. [DOI] [PubMed] [Google Scholar]
- 25.Furuta G.T., Ackerman S.J., Lu L., Williams R.E., Wershil B.K. Stem cell factor influences mast cell mediator release in response to eosinophil-derived granule major basic protein. Blood. 1998;92:1055–1061. http://www.bloodjournal.org/content/92/3/1055 [PubMed] [Google Scholar]
- 26.Boix E., Leonidas D.D., Nikolovski Z., Nogués M.V., Cuchillo C.M., Acharya K.R. Crystal structure of eosinophil cationic protein at 2.4 A resolution. Biochemistry. 1999;38:16794–16801. doi: 10.1021/bi9919145. [DOI] [PubMed] [Google Scholar]
- 27.Swaminathan G.J., Weaver A.J., Loegering D.A., Checkel J.L., Leonidas D.D., Gleich G.J., Acharya K.R. Crystal structure of the eosinophil major basic protein at 1.8 A. An atypical lectin with a paradigm shift in specificity. J. Biol. Chem. 2001;276:26197–26203. doi: 10.1074/jbc.M100848200. [DOI] [PubMed] [Google Scholar]
- 28.Walls A.F. Neutral proteases in asthma and rhinitis. In: Busse W.W., Holgate S.T., editors. Asthma and Rhinitis. 2nd EdnBoston; Blackwell: 2000. pp. 968–998. [Google Scholar]
- 29.Schwartz L.B., Irani A.M., Roller K., Castells M.C., Schechter N.M. Quantitation of histamine, tryptase, and chymase in dispersed human T and TC mast cells. J. Immunol. 1987;138:2611–2615. http://www.jimmunol.org/content/138/8/2611 [PubMed] [Google Scholar]
- 30.Caughey G.H. Of mites and men: trypsin-like proteases in the lungs. Am. J. Respir. Cell Mol. Biol. 1997;16:621–628. doi: 10.1165/ajrcmb.16.6.9191463. [DOI] [PubMed] [Google Scholar]
- 31.Bjellqvist B.1, Hughes G.J., Pasquali C., Paquet N., Ravier F., Sanchez J.C., Frutiger S., Hochstrasser D. The focusing positions of polypeptides in immobilized pH gradients can be predicted from their amino acid sequences. Electrophoresis. 1993;10:1023–1031. doi: 10.1002/elps.11501401163. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.