Abstract
Background:
Bone marrow edema lesions around the knee are a common magnetic resonance image finding. They constitute a central component of a wide variety of inflammatory and noninflammatory conditions affecting the knee joint. Those lesions are not only a significant source of pain, but are also connected to many musculoskeletal pathologies.
Case Report:
We describe 2 cases of bone marrow edema of the knee joint treated with the aid of Classical Homeopathy. In both of the cases, Arnica montana was the chosen homeopathic remedy.
Conclusions:
The results of the treatment are promising, encouraging for more research on this area.
Keywords: Arnica, bone marrow, homeopathy, knee, edema
Introduction
Wilson et al1 introduced the term “bone marrow edema” (BME) to describe ill-defined bone marrow hyperintensities on T2 (transverse relaxation time)-weighted magnetic resonance images from patients suffering from knee and hip pain. The specific term was used because of “a lack of a better term and to emphasize the generic character of the condition.”
The cause of primary bone edema is still not certain. Possibly, a local ischemic episode, of varied etiology, initiates a chain of events resulting in this specific bone pathology.2
A hypothetical etiologic pathway of the condition may involve (1) bone injury (vascular, traumatic, inflammation, metabolic), (2) bone compromise (increased turnover, elevated intraosseous pressure, stress microfracture), (3) BME (increased intraosseous pressure—compartment syndrome), and (4) reparative mechanisms (sufficient: slow resolution—insufficient: bone necrosis).3,4
Pain is the predominant symptom of this pathology. Pain is caused by increased intraosseous pressure (normal pressure is 20-30 mm Hg), because of the abnormal high fluid content in the marrow spaces.5 Pain during mechanical loading is characteristic, combined with more or less severe complaints during night. Also typical is pain in the affected area when it is tapped.
Magnetic resonance imaging (MRI) is the gold-standard for the diagnosis of BME. The characteristic finding is the altered bone marrow signal, with high signal on T2 and STIR (short-T1 inversion recovery) sequences, with or without low T1 (longitudinal relaxation time) signal. Those magnetic resonance findings might indicate histologically true edema, but can correspond, as well, to trabecular bone necrosis, cyst formation, fibrosis, and cartilage fragmentation.6
The differential diagnosis involves several pathologies: traumatic contusions, fractures, bone cysts, infiltrated marrow, developmental chondral lesions, subchondral insufficiency fractures, and of course, true osteonecrosis.6
Treatment of BME will be determined according to the cause and the size of the bone necrosis area. Osteonecrotic areas exceeding 40% to 50% of the condyle (femoral or tibial) or lesion greater than 5 cm2 usually lead to collapse, requiring knee arthroplasty.7 On the other hand, medium-sized lesions (3.5-5 cm2) may or may not regress, whereas smaller lesions (<3.5 cm2) will most probably regress with conservative treatment.8
Conservative treatment involves analgesic medications, nonsteroidal anti-inflammatory drugs (NSAIDs), protected weight-bearing for a period of 3 to 8 months along with physiotherapy, according to the patients’ symptoms and radiological findings. Pulsed electromagnetic fields therapy seems to have promising results in the reduction of pain and the necrotic area after 6 months.9 Prostacyclin and bisphosphonates are 2 medications which have been used in the treatment of BME. They have different pathway actions and therefore may offer parallel beneficial effects.9
Surgical treatment, reserved for the late stages, involves simple drilling, stabilization of the fragment, curettage combined with drilling, and finally osteochondral or chondrocyte transplantation.5
Homeopathy, the “energy medicine,” is a branch of medical science based on the principle that a disease can be cured by strengthening the body’s defense mechanism with substances selected for their energy-giving properties. Founded in the 19th century by Dr Samuel Hahnemann, Homeopathy is derived from the Greek words “homeo” and “pathos,” meaning “similar suffering.”10 From our knowledge, this is the first published case-report series describing treatment of BME of the knee with the aid of classical homeopathy.
Case No. 1
The patient was a 55-year-old male who presented to the clinic complaining for 3 months of pain and swelling of his right knee. He was very active, working as a teacher of traditional Greek dances and he could recall a tortional injury of his right knee some time ago. The knee joint was swollen, painful in full flexion and especially when tapping the medial femoral condyle. He was walking with a small limp and was hardly able to run or dance.
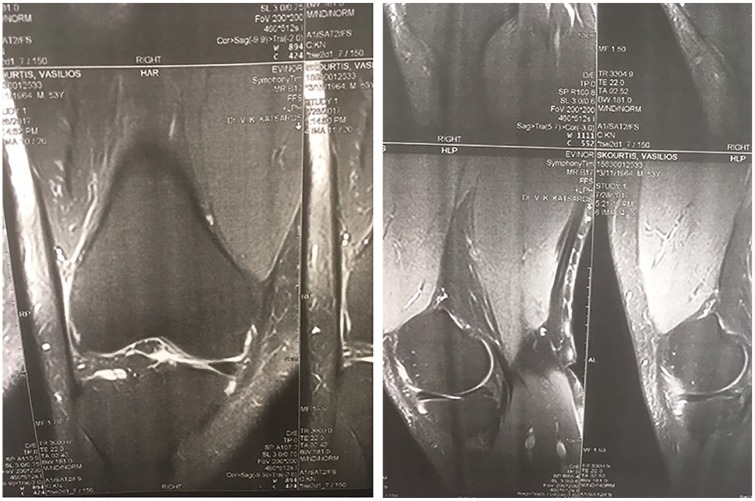
The MRI scan showed a grade 2 to 3 rupture of the posterior horn of the medial meniscus, along with extensive BME of the anterior aspect of the medial femoral condyle, occupying 40% of the femoral condyle (Figure 1). The patient was proposed to undergo an arthroscopy, primarily to deal with the meniscal injury but he was reluctant to proceed. Conservative treatment proposed to the patient included protected-partial weight-bearing for at least 8 weeks, along with physiotherapy and NSAIDs. The patient was suffering from chronic hypertension so anti-inflammatory drugs were excluded and was not keen on giving up his dance teaching, even for a few weeks.
Figure 1.
MRI scan of the first patient on first consultation.
The treatment regimen which we agreed to follow was physiotherapy and classical homeopathy. The patient had 2 sessions of physiotherapy per week, aiming to preserve range of motion of the knee joint, along with the integrity of the quadriceps muscle. Repertorisation of the case was done using the Vithoulkas Compass 2.3 Software. Arnica Montana was the chosen remedy. The patient was relatively healthy, belonging, according to Vithoulkas, to group B, regarding his Level of Health,11 so the 200CH potency was prescribed, 1 capsule given initially, and the next doses according to the follow-up symptoms (he needed another 4 doses of the remedy).
Over the next 2 months, there was a slow but steady improvement of the patient’s symptomatology, although he barely rested his knee. In 3 months’ time, he was pain-free and was back to his previous activities without any limitations. Five months after the first MRI scan, the patient underwent a second scan. The new scan showed that the BME of the medial femoral condyle had completely reduced, whereas the meniscal injury was still present and unchanged (Figure 2). We were very happy with the outcome of the case, so we discharged the patient from our care.
Figure 2.
Five months after treatment.
Case No. 2
The second patient was a female 56-year-old supermarket owner, who was suffering from severe pain of her left knee for at least 3 months. There was no history of trauma and the symptoms worsened progressively. On presenting to the clinic the patient was walking with a severe limp. There was obvious swelling of the left knee joint and flexion of the joint was limited to 60°. There was severe pain on tapping the lateral femoral condyle along with severe night pain.
The MRI scan of the knee showed extensive BME of the lateral femoral condyle, occupying almost all the condyle, with an area of osteonecrosis on its lateral aspect. On the lateral tibial condyle, the MRI scan also showed the initial signs of BME (Figure 3).
Figure 3.
MRI scan of the second patient on first consultation.
Based on the above clinical and radiological findings, surgical treatment was the appropriate one5,7 and was proposed to the patient. The patient declined to proceed, so we had to offer her conservative treatment, consisting of non-weight-bearing, and physiotherapy. Due to her history of peptic ulcer with hemorrhage, she was not a candidate for treatment with NSAIDs or bisphosphonates. Having in mind the successful treatment of the first patient, we proposed classical homeopathy for she was keen to take. Arnica montana was the remedy chosen after the repertorisation of the case. The initial potency selected was 200CH, followed by daily doses of 30CH.
The patient did not follow the non-weight-bearing that was proposed to her—stating that she could not abstain from her work in the supermarket but used a light knee brace instead, full weight-bearing. For the next 3 months she followed physiotherapy treatment along with the homeopathy treatment while occasionally using simple analgesics (paracetamol). Her clinical condition was slowly improving.
Three months after the initial MRI scan, we proceeded to a follow-up scan (Figure 4). The BME of the femoral condyle deteriorated, involving the whole lateral femoral condyle and the lateral part of the medial femoral condyle as well, whereas the osteonecrosis area of the lateral femoral condyle increased in size. On the other hand, the BME of the lateral tibial condyle completely disappeared. The overall clinical picture of the patient, in terms of pain and mobility, was better. Based on those findings, we strongly advised for an operative treatment.
Figure 4.
Three months after treatment.
The patient underwent arthroscopy with drilling of both the femoral and the tibial condyles. Intraoperatively, in contrast to the very soft feeling of the femoral condyle, the tibial condyle had a definitely hard feeling during the drilling procedure. The postoperative treatment involved non-weight-bearing for 1 month, followed by partial weight-bearing for another month. A new MRI scan is being scheduled 6 months after the procedure.
Discussion
After the introduction of MRI in clinical practice, bone marrow lesions have emerged as a central component of many different inflammatory and noninflammatory diseases affecting the musculoskeletal system. Eriksen12 proposed a comprehensive system for the cause of those lesions: (1) trauma: fracture, local transient osteoporosis, osteochondral injuries; (2) degenerative lesions: osteoarthritis; (3) inflammatory lesions: inflammatory arthropathies and enthesitis; (4) ischemic lesions: avascular necrosis, chronic regional pain syndrome, sickle cell anemia; (5) infectious lesions: osteomyelitis; (6) metabolic/endocrine lesions: hydroxyapatite deposition disease, gout; (7) iatrogenic lesions: surgery, radiotherapy, immunosuppressants (glucocorticoids, cyclosporine), cytostatics. Although our first patient seems to belong to the trauma category, we could not find a definite cause for the second more serious of our cases.
Non-weight-bearing or partial weight-bearing seems to be the gold standard treatment for this condition.5 Physiotherapy along with extracorporal shock wave therapy has been reported to provide significant pain relief and functional improvement. Pharmaceutical options include the use of bisphosphonates, prostaglandin derivatives, and tumor necrosis factor (TNF) inhibitors.12
Both our patients did not comply with the recommended protected weight-bearing for at least 8 weeks, stating that they were obliged to continue their daily-working activities. Bearing in mind favorable reported outcomes of treatment of various musculoskeletal pathologies with the aid of classical homeopathy, we offered them this treatment option.
Brinkhaus et al13 reported that A montana, in patients receiving knee surgery showed a trend toward less postoperative edema compared with patients receiving placebo. Tveiten and Bruset14 reported that A montana in the D30 potency had a positive effect on muscle soreness—but not on cell damage measured by enzymes. Even more recently, Sarkar et al15 reported that Homeopathic remedy Guaiacum officinale possesses antirheumatic and antioxidant activity in experimental animal model and these activities may be more significant in higher potencies. On the other hand, Koley et al,16 in a double-blinded randomized placebo-controlled study, evaluating individualized Homeopathy in managing pain in knee osteoarthritis (using various Homeopathic remedies—Bryonia alba, Rhus toxicodendron, Calcarea carbonica, A montana, and Natrum muriaticum), did not find statistically significant differences to justify the superiority of Homeopathic treatment in comparison with placebo.
Arnica montana is a widely used therapeutic plant used traditionally to treat various pathologic conditions. It possesses significant anti-inflammatory, anti-osteoarthritic, anti-osteoporotic, and anti-hemorrhagic activity, shows significant antioxidant and protective effect, improves circulation, and also has analgesic properties.17 The homeopathic remedy A montana, according to Vithoulkas, is indicated when
a part of the body is bruised, with a sore feeling . . . This can be produced by an injury, but from other causes, such as the overexertion of an organ, or a strain, or an acute disease as well.18
The first case had an excellent outcome, both clinical and radiological. Having received in fact only the homeopathic treatment, with almost no weight-bearing protection, the patient was pain-free in 4 months’ time, whereas the MRI scan 5 months after the first one showed that the BME of the femoral condyle had almost disappeared (Figure 2).
The second case was, of course, a different one. Surgical treatment was proposed to the patient from the first examination at the clinic, since the BME of the femoral condyle was extensive and already osteonecrosis of the condyle was present. Nevertheless, the patient decided to choose the homeopathic treatment with only minimal weight-bearing protection. The second MRI scan, 3 months after the initial one showed that the femoral condyle lesions were deteriorating, but, interestingly, the tibial condyle lesions, obvious on the first scan, had almost disappeared (Figure 4). The osteonecrosis of the femoral condyle, being permanent organ damage, represents a very difficult physical obstacle, almost impossible to be treated by classical homeopathy.10 So, as a matter of fact, we do not regard the case as a Homeopathic failure, since the tibial condyle was saved, and, in fact the actual joint was saved as well, since the involvement of necrosis of the lateral tibial condyle as well would mean that the patient would most probably need a total knee arthroplasty.
Conclusions
Our experience from the above 2 cases shows that individualized treatment with the aid of classical homeopathy definitely has a place in the treatment of the common, but difficult to treat condition of BME of the knee. Research with more cases is needed to prove the effectiveness of this therapeutic method.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Authors’ Note: The work was conducted at International Center of Classical Homeopathy, Alonissos, Greece.
Author Contributions: Dr Dionysis Tsintzas is the main physician who contributed the case information. Dr Seema Mahesh edited the article. The article took form under George Vithoulkas’ guidance.
Patient Consent: The patients have consented to their case details and scans being used for publication.
ORCID iDs: Dionysis Tsintzas  https://orcid.org/0000-0002-0715-4438
https://orcid.org/0000-0002-0715-4438
Seema Mahesh  https://orcid.org/0000-0002-4765-5595
https://orcid.org/0000-0002-4765-5595
References
- 1. Wilson AJ, Murphy DA, Hardy DC, Totty WG. Transient osteoporosis: transient bone marrow oedema? Radiology. 1989;171:135-140. [DOI] [PubMed] [Google Scholar]
- 2. Patel S. Primary bone marrow oedema syndromes. Rheumatology (Oxford). 2014;53:785-792. [DOI] [PubMed] [Google Scholar]
- 3. Trevisan C, Orolani S, Monteleone M, Marinoni EC. Regional migratory osteoporosis: a pathogenic hypothesis based on three cases and a review of the literature. Clin Rheumatol. 2002;21:418-425. [DOI] [PubMed] [Google Scholar]
- 4. Elder GJ. From marrow oedema to osteonecrosis: common paths in the development of post-transplant bone pain. Nephrology (Carlton). 2006;11:560-567. [DOI] [PubMed] [Google Scholar]
- 5. Hofmann S, Kramer J, Vakil-Adli A, Aigner N, Breitenseher M. Painful bone marrow edema of the knee: differential diagnosis and therapeutic concepts. Orthop Clin North Am. 2004;35:321-333, ix. [DOI] [PubMed] [Google Scholar]
- 6. Kon E, Ronga M, Filardo G, et al. Bone marrow lesions and subchondral bone pathology of the knee. Knee Surg Sports Traumatol Arthrosc. 2016;24:1797-1814. [DOI] [PubMed] [Google Scholar]
- 7. Mont MA, Marker DR, Zywiel MG, Carrino JA. Osteonecrosis of the knee and related conditions. J Am Acad Orthop Surg. 2011;19:482-494. [DOI] [PubMed] [Google Scholar]
- 8. Karim AR, Cherian JJ, Jauregui JJ, Pierce T, Mont MA. Osteonecrosis of the knee: review. Ann Transl Med. 2015;3:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Marchegianni Muccioli GM, Grassi A, Setti S, et al. Conservative treatment of spontaneous osteonecrosis of the knee in the early stages: pulsed electromagnetic fields therapy. Eur J Radiol. 2013;82:530-537. [DOI] [PubMed] [Google Scholar]
- 10. Vithoulkas G. The Science of Homeopathy. 6th ed Alonnisos, Greece: International Academy of Classical Homeopathy; 2012. [Google Scholar]
- 11. Vithoulkas G. Levels of Health. The Second Volume of the Science of Homeopathy. Alonissos, Greece: International Academy of Classical Homeopathy; 2017. [Google Scholar]
- 12. Eriksen EF. Treatment of bone marrow lesions (bone marrow edema). Bonekey Rep. 2015;4:755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brinkhaus B, Wilkens JM, Ludtke R, et al. Homeopathic arnica therapy in patients receiving knee surgery: results of three randomized double-blind trials. Complement Ther Med. 2006;14:237-246. [DOI] [PubMed] [Google Scholar]
- 14. Tveiten D, Bruset S. Effect of Arnica D30 in marathon runners. Pooled results from two double-blind placebo-controlled studies. Homeopathy. 2003;92:187-189. [DOI] [PubMed] [Google Scholar]
- 15. Sarkar A, Datta P, Das AK, Gomes A. Anti-rheumatoid and anti-oxidant activity of homeopathic Guaiacum officinale in an animal model. Homeopathy. 2014;103:133-138. [DOI] [PubMed] [Google Scholar]
- 16. Koley M, Saha S, Ghosh S. A double-blind randomized placebo-controlled feasibility study evaluating individualized homeopathy in managing pain of knee osteoarthritis. J Evid Based Complementry Altern Med. 2015;20:186-191. [DOI] [PubMed] [Google Scholar]
- 17. Kriplani P, Guarve K, Baghael U. Arnica Montana L.—a plant of healing: review. J Pharm Pharmacol. 2017;69:925-945. [DOI] [PubMed] [Google Scholar]
- 18. Vithoulkas G. Materia Medica Viva, vol. 3 Alonissos, Greece: International Academy of Classical Homeopathy; 2006. [Google Scholar]