Abstract
Background:
One of the key components of multidisciplinary CKD clinics is education; however, kidney disease knowledge among patients followed in these clinics is not routinely measured.
Objective:
The aim of this study was to determine objective and perceived kidney disease knowledge and patient characteristics associated with knowledge among patients followed in a multi-care kidney clinic.
Design:
This is a cross-sectional survey study.
Setting:
This study was conducted in a multi-care kidney clinic in Ontario, Canada.
Patients:
Patients who did not speak English, who were unable to read due to significant vision impairment, or who had a known history of dementia or significant cognitive impairment were excluded.
Measurements:
Perceived kidney disease knowledge was evaluated using a previously validated 9-item survey (PiKS). Each question on the perceived knowledge survey had 4 possible responses, ranging from “I don’t know anything” (1) to “I know a lot” (4). Objective kidney disease knowledge was evaluated using a previously validated survey (KiKS).
Methods:
The association between patient characteristics and perceived and objective kidney disease knowledge was determined using linear regression.
Results:
A total of 125 patients were included, 57% were male, the mean (SD) age and eGFR were 66 (13) years and 16 (5.9) mL/min/1.73 m2, respectively. The median (IQR) objective and perceived knowledge survey scores were 19 out of 27 (16, 21) and 2.9 out of 4 (2.4, 3.2), respectively. Only 25% of patients answered correctly that CKD can be associated with no symptoms, and 64% of patients identified correctly that the kidneys make urine. More than 60% of patients perceived themselves to know nothing or only a little about medications that help or hurt the kidney. Older age was independently associated with lower perceived and objective knowledge, but sex, income, and educational attainment were not.
Limitations:
This is a single-center study. Cognitive impairment was based on the treating team’s informal assessment or prior documentation in the chart; formal cognitive testing was not performed as part of this study.
Conclusions:
Despite resource-intensive care, CKD knowledge of patients followed in a multidisciplinary clinic was found to be modest. Whether enhanced educational strategies can improve knowledge and whether increasing knowledge improves patient outcomes warrants further study.
Keywords: CKD, education, knowledge, survey
Abrégé
Contexte:
L’éducation sur les maladies rénales est une des raisons d’être des cliniques multidisciplinaires d’IRC, mais les connaissances des patients suivis dans ces cliniques ne sont pas mesurées de façon systématique.
Objectif:
Évaluer les connaissances objectives et perçues sur l’insuffisance rénale des patients suivis dans une clinique multidisciplinaire de maladies rénales et déterminer les caractéristiques des patients associées à ces connaissances.
Type d’étude:
Étude transversale menée sous forme de questionnaire.
Cadre:
Une clinique multidisciplinaire de suivi des maladies rénales en Ontario (Canada).
Sujets:
Les patients ne parlant pas anglais, ne pouvant lire en raison d’un important trouble de la vision ou ayant des antécédents de démence ou d’un important déficit cognitif ont été exclus.
Mesures:
Les connaissances perçues quant à l’insuffisance rénale ont été évaluées à l’aide d’un questionnaire préalablement validé composé de neuf questions (PiKS). Chaque question sur la connaissance perçue disposait de quatre choix de réponse allant de « Je n’y connais rien (1) » à « J’en connais beaucoup (4) ». Les connaissances objectives ont été évaluées à l’aide d’un questionnaire préalablement validé (KiKS).
Méthodologie:
L’association entre les caractéristiques du patient et les connaissances objectives et perçues a été établie par régression linéaire.
Résultats:
Au total, 125 patients ont été inclus. L’échantillon était composé à 57 % d’hommes dont l’âge médian (SD) était de 66 (13) ans et dont le DFGe médian (SD) s’établissait à 16 (5,9) mL/min/1,73 m2. Les scores médians (EIQ) obtenus aux tests de connaissances objectives et perçues étaient respectivement de 19 sur 27 (16-21) et de 2,9 sur 4 (2,4-3,2). Seuls 25 % des patients ont répondu correctement que l’IRC peut se manifester en absence de symptômes, et 64 % des patients savaient que les reins produisent l’urine. Plus de 60 % des patients avaient l’impression de ne rien connaître ou d’en savoir très peu sur les médicaments qui aident ou qui nuisent aux reins. De faibles connaissances objectives et perçues ont été indépendamment associées à un âge plus avancé; ce qui n’a pas été le cas pour le sexe, le revenu et le niveau de scolarité.
Limites:
L’étude a été menée dans un seul centre. Le déficit cognitif a été établi sur la base de l’évaluation informelle de l’équipe soignante ou de la documentation antérieure figurant au dossier. Aucun test cognitif formel n’a été effectué dans le cadre de cette étude.
Conclusion:
Malgré les multiples ressources disponibles, les connaissances sur l’IRC des patients suivis dans une clinique multidisciplinaire se sont avérées modestes. Une étude plus approfondie est requise pour déterminer si de meilleures stratégies d’éducation peuvent améliorer les connaissances des patients, et si l’accroissement de ces connaissances est susceptible d’améliorer les issues cliniques chez les patients.
What was known before
Patient education is an important component of multidisciplinary chronic kidney disease (CKD) care. However, patient kidney disease knowledge is not routinely measured.
What this adds
Despite resource intensive care, kidney disease knowledge of patients followed in a multidisciplinary CKD clinic was found to be modest. Strategies to enhance patient kidney disease knowledge and whether improving knowledge leads to better patient outcomes requires further study.
Introduction
In the era of person-centered medicine, it is commonly accepted that informed patients have better health outcomes.1,2 Studies in the CKD population suggest that educational interventions can improve patient outcomes such as reducing hospitalizations, delaying CKD progression, and improving uptake of home dialysis therapies.3-12 However, the delivery of effective education on the various aspects of kidney disease in everyday clinical practice can prove challenging due to multiple barriers.13 Studies have found that knowledge of disease status in patients with CKD is low.14,15 The National Health and Nutrition Examination Survey, administered to a representative sample of the U.S. population, found that only 22% and 45% of respondents with CKD stages 3 and 4, respectively, were actually aware of their kidney disease diagnosis.14 Furthermore, patients followed in a nephrology clinic in the United States were found to have low-to-modest perceived and objective kidney disease knowledge when administered surveys on various aspects of kidney disease.16,17 A Canadian study performed several years ago that asked patients followed in a nephrology clinic to rate their knowledge on various aspects of kidney disease found that approximately one-third of respondents reported no or limited understanding of CKD and no awareness of treatment options.18
Currently in Canada, patients with advanced CKD (estimated glomerular filtration rate [eGFR] < 30 mL/min/1.73 m2) are often followed in multidisciplinary clinics, with education on various aspects of kidney disease being a key component of the care delivered in the clinic. However, kidney disease knowledge of patients followed in multidisciplinary clinics is not routinely evaluated. To inform educational practices, we performed a cross-sectional survey study of patients with advanced CKD followed in an academic multi-care kidney clinic (MCKC). Our primary objective was to determine the objective and perceived kidney disease knowledge using previously validated surveys.16,17 We hypothesized that both objective and perceived kidney disease knowledge levels would be low and that lower income level, lower educational attainment, and lack of renal replacement therapy (RRT) modality education would be associated with lower knowledge levels.
Materials and Methods
Design and Setting
We conducted a cross-sectional survey study that enrolled patients from a MCKC at one academic center (St. Joseph’s Healthcare, Hamilton) in Ontario, Canada. The MCKC provides multidisciplinary care to adult patients (≥18 years of age) with advanced CKD defined by an estimated risk of kidney failure >10% over 2 years, as determined by the Kidney Failure Risk Equation or an eGFR <15 mL/min/1.73 m2.19 A nephrologist, nurse, dietitian, social worker, pharmacist, and diabetes nurse educator provide integrated care to the patients followed in the clinic. The nephrologist, nurse, and pharmacist see patients at each visit; other health care providers see patients on an as-needed basis. Patients are generally seen every 3 to 6 months, but are often seen more frequently when approaching kidney failure or when experiencing a high degree of complications or symptom burden. The focus of the clinic is to manage CKD complications, prevent CKD progression, and prepare patients for RRT.20 Patients receive education on the functions of the kidneys, and how to slow CKD progression. As kidney function declines, patients also receive education about the symptoms of kidney failure and symptom management. Clinic nurses primarily provide the education. Information is delivered in the form of educational booklets and laminated pictures (refer to Online Appendix for further details). Patients complete modality education as an initial step to prepare for RRT. This education is administered as a one-to-one 60- to 90-minute educational session by a specialized nurse with follow-up and refresher sessions as needed. Patients are usually referred for modality education when the requirement for RRT is anticipated in 1 to 2 years. Timing of referral is up to the discretion of the individual treating nephrologist. Patients are seen by the same nephrologist at each clinic visit. There are 11 nephrologists in the clinic, but 3 nephrologists followed 59% of enrolled patients.
Study Population
Patients followed in the MCKC who could read and write in English were eligible. Patients unable to read due to significant vision impairment or with a known history of dementia or significant cognitive impairment, as documented in the chart or reported by their primary nephrologist, were excluded. Patients were recruited from August 25, 2017, to August 28, 2018, and were enrolled following informed consent. Approval to conduct the study was obtained from the local research ethics board. The reporting of this study follows the STROBE guidelines for observational studies.21
CKD Knowledge Surveys and Patient Characteristics
Simultaneous measures of perceived and objective kidney disease knowledge were captured. Patients were asked to complete paper-and-pencil surveys following their routine clinic appointment. Perceived kidney disease knowledge was evaluated using a previously validated 9-item survey (PiKS),17 where patients subjectively rated their knowledge for each item on a scale from 1 (“I don’t know anything”) to 4 (“I know a lot”). Objective kidney disease knowledge was evaluated using a previously validated survey (KiKS).16 This survey normally contains 28 items, but an item that evaluates patients’ knowledge about blood pressure targets was removed, given that blood pressure targets may vary depending on the individual patient’s clinical history.22 The administered objective kidney disease knowledge survey, therefore, contained 27 items. Demographics, comorbidities, and other clinical characteristics were determined by chart review or patient verbal report. Patient eGFR was determined based on the serum creatinine value taken closest to the visit and calculated using the CKD-EPI formula.23
Statistical Analysis
Descriptive statistics were calculated as mean and standard deviation (SD), or median and interquartile range (IQR) for continuous variables, and frequency (%) for categorical variables. Perceived kidney disease knowledge was evaluated by taking the average of a patient’s ratings for each of the items on the 9-item PiKS survey. A patient was considered to have low perceived knowledge for an item if it was rated as 1 (“I don’t know anything”) or 2 (“I know a little amount”). This classification has been used previously.17 Objective kidney disease knowledge was calculated as the number and percentage of correct responses on the 27-item KiKS survey. To examine the association between perceived and objective kidney disease knowledge and patient characteristics, the Kruskal-Wallis test was used for categorical variables and the Spearman rank order correlations were calculated for continuous and ordinal variables. The independent association of age, sex, educational attainment, income, systolic blood pressure, eGFR, and RRT modality education with perceived and objective kidney disease knowledge was examined using multivariable linear regression. All covariates were selected a priori and were retained in the model regardless of statistical significance. Missing values for income (16 patients declined to report income) were imputed using multiple imputation, fully conditional specification method. Logistic regression was performed to examine the association of RRT modality education with a correct response to the question regarding kidney failure treatment options on the KiKS survey and with a response of low perceived knowledge (response of 1 or 2) versus moderate-to-high perceived knowledge (a response of 3 or 4) on the PiKS survey. All statistical analyses were performed using SPSS version 25.
Results
Patient Characteristics
Of the 402 MCKC patients screened for participation in the study, 125 patients met eligibility criteria, provided informed consent, and were included in the final analysis. There was one patient who did not complete the PiKS survey and one patient who did not complete the KiKS survey. The reasons for exclusion are outlined in Figure 1. Patient characteristics are outlined in Table 1. The mean age was 66 years; most patients were male (57%) and most were Caucasian (88%). The most common cause of CKD was diabetes (48%), and the mean eGFR was 16 mL/min/1.73 m2. The median time followed in the clinic was 14 months; 68% of patients had completed modality education. Nearly all patients (98%) were aware of their CKD diagnosis.
Figure 1.
Patient selection.
Note. MCKC = multi-care kidney clinic.
Table 1.
Patient Characteristics.
| Characteristics | No. of patients (%) Total cohort, N = 125 |
|---|---|
| Age, mean (SD) | 66 (13) |
| Men | 71 (57) |
| Educational level | |
| High school or less | 58 (46) |
| Diploma/trade school/some college | 14 (11) |
| Post-graduate degree | 53 (42) |
| Income (Canadian dollars), median (IQR)a | 50 000 (30 000, 80 000) |
| Race | |
| Caucasian | 110 (88) |
| Black | 6 (5) |
| Hispanic | 1 (0.8) |
| Asian | 5 (4) |
| Other | 3 (2) |
| Cause of CKD | |
| Diabetes | 60 (48) |
| Hypertension | 23 (18) |
| Glomerulonephritis | 15 (12) |
| Other | 27 (22) |
| Coronary artery disease | 24 (19) |
| Hypertension | 92 (74) |
| Congestive heart failure | 14 (11) |
| Stroke | 6 (4.8) |
| Peripheral vascular disease | 5 (4.0) |
| Current smoker | 15 (12) |
| Systolic blood pressure, mean (SD) | 134 (19) |
| Diastolic blood pressure, mean (SD) | 71 (12) |
| BMI, mean (SD)b | 31.6 (7.5) |
| eGFR (mL/min/1.73 m2), mean (SD) | 16 (6) |
| Urine albumin-to-creatinine ratio (mg/mmol), median (IQR)b | 89.3 (23.4, 201.7) |
| Angiotensin-converting-enzyme inhibitor or angiotensin receptor blocker use | 77 (62) |
| Serum potassium (mmol/L), mean (SD) | 4.7 (0.6) |
| Serum phosphate (mmol/L), mean (SD) | 1.5 (1.3) |
| Completed modality education | 85 (68) |
| Time followed in the clinic (months), median (IQR) | 14.0 (6.0, 33.5) |
| Time elapsed between modality education and survey completion (months), median (IQR)c | 9.5 (4.0, 23.0) |
| Perceived kidney disease knowledge summary score, median (IQR) | 2.9 (2.4, 3.2) |
| Objective kidney disease knowledge score (% correct), median (IQR) | 70 (59, 78) |
Note. BMI = body mass index; CKD = chronic kidney disease; eGFR = estimated glomerular filtration rate; IQR = interquartile range; SD = standard deviation.
Missing, n = 16.
Missing, n = 1.
Among patients who completed modality education (n = 80), missing values for date of modality education (n = 5).
Objective Kidney Disease Knowledge
The median (IQR) score for objective kidney disease knowledge was 19 (16, 21) out of 27 (70% correct responses). The proportion of patients who responded correctly to each of the 27 questions on the KiKS survey is detailed in Table 2. It was found that 74% of patients correctly identified that ibuprofen should be avoided, 84% of patients correctly identified that dialysis or kidney transplant are the treatments for kidney failure, 74% of patients correctly identified what GFR stands for, 64% of patients correctly identified that the kidneys make urine, and 25% of patients correctly identified that CKD can be associated with no symptoms.
Table 2.
Number (%) of Patients Responding Correctly to Each Question on the Objective Kidney Disease Knowledge (KiKS) Survey.
| Are there certain medications your doctor can prescribe to help keep your kidney(s) as healthy as possible? | 110 (89) |
| Why is too much protein in the urine not good for the kidney? | 24 (19) |
| Select the one medication from the list below that a person with chronic kidney disease should avoid. | 93 (75) |
| If the kidney(s) fail, treatment might include: | 105 (85) |
| What does “GFR” stand for? | 92 (74) |
| Are there stages of chronic kidney disease? | 121 (98) |
| Does chronic kidney disease increase a person’s chances for a heart attack? | 94 (76) |
| Does chronic kidney disease increase a person’s chance for death from any cause? | 100 (81) |
| Does the kidney make urine? | 80 (65) |
| Does the kidney clean the blood? | 110 (89) |
| Does the kidney help keep bones healthy? | 65 (52) |
| Does the kidney help keep a person from losing hair? | 110 (89) |
| Does the kidney help keep blood cell counts normal? | 98 (79) |
| Does the kidney help keep blood pressure normal? | 90 (73) |
| Does the kidney help keep blood sugar normal? | 51 (41) |
| Does the kidney help keep potassium levels in the blood normal? | 111 (90) |
| Does the kidney help keep phosphorus levels in the blood normal? | 106 (85) |
| Please select from the list, all of the symptoms a person might have if they have CKD or kidney failure | |
| Increased fatigue? (yes/no) | 119 (96) |
| Shortness of breath? (yes/no) | 101 (81) |
| Metal taste/bad taste in the mouth? (yes/no) | 79 (64) |
| Unusual itching? (yes/no) | 105 (85) |
| Nausea and/or vomiting? (yes/no) | 94 (76) |
| Hair loss? (yes/no) | 108 (87) |
| Increased trouble sleeping? (yes/no) | 94 (76) |
| Weight loss? (yes/no) | 76 (61) |
| Confusion? (yes/no) | 64 (52) |
| No symptoms at all? (yes/no) | 31 (25) |
Note. GFR = glomerular filtration rate; CKD = chronic kidney disease. In total, 124 patients completed the survey.
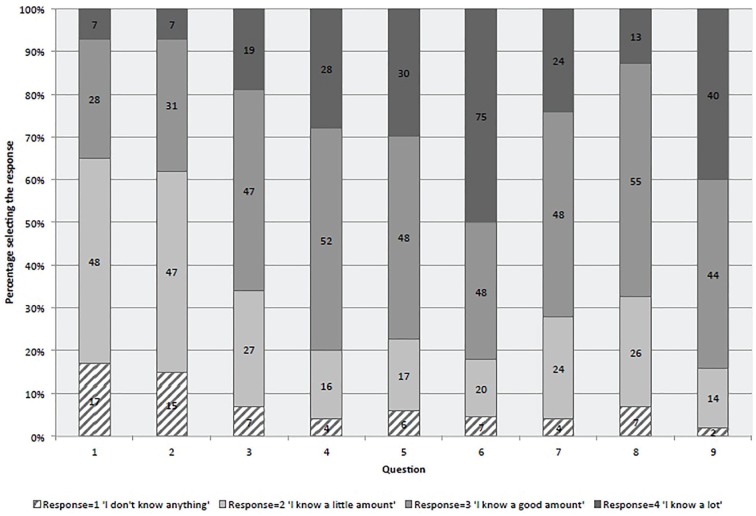
Perceived Kidney Disease Knowledge
The median (IQR) score for perceived kidney disease knowledge was 2.9 out of 4 (2.4, 3.2) (Table 1). Responses to each of the 9 items on the PiKS survey are detailed in Figure 2. The proportion of patients who responded as having low perceived knowledge for each item on the PiKS survey is detailed in Table 3. Most of the patients had low perceived knowledge regarding medications that help or hurt the kidneys (65% and 62%, respectively). Few of the patients (16%) had low perceived knowledge about why they had been sent to see a kidney doctor. Higher perceived kidney disease knowledge was significantly but weakly correlated with higher objective kidney disease knowledge (Spearman correlation = 0.27, P = .002).
Figure 2.
Responses to each item on the Perceived Kidney Disease Knowledge (PiKS) Survey.
Questions: 1. Medications that help the kidney, 2. Medications that hurt the kidney; 3. Foods that should be avoided if a person has low kidney function, 4. Your goal blood pressure, 5. Understanding treatment options if kidney function gets worse, 6. Symptoms of chronic kidney disease, 7. How kidney function is checked by a doctor, 8. Functions of the kidney, 9. Knowledge about why you have been sent to see a kidney doctor.
Table 3.
Perceived Kidney Disease Knowledge (PiKS) Survey Item Responses.
| Question | Low perceived knowledge (%)a |
|---|---|
| 1. Medications that help the kidney | 65 |
| 2. Medications that hurt the kidney | 62 |
| 3. Foods that should be avoided if a person has low kidney function | 35 |
| 4. Your goal blood pressure | 20 |
| 5. Understanding treatment options if kidney function gets worse | 23 |
| 6. Symptoms of chronic kidney disease | 27 |
| 7. How kidney function is checked by a doctor | 28 |
| 8. Functions of the kidney | 32 |
| 9. Knowledge about why you have been sent to see a kidney doctor | 16 |
Note. In total, 124 patients completed the survey.
Low perceived knowledge defined by a response of 1 “I don’t know anything” or 2 “I know a little amount” on the PiKS survey.
Patient Characteristics and Associations With Kidney Disease Knowledge
Patient characteristics and their association with kidney disease knowledge are detailed in Table 4 (objective knowledge linear regression analysis), Table 5 (perceived knowledge linear regression analysis), and Supplementary Table 1 (correlation analysis). Older age was significantly associated with both lower objective and perceived kidney disease knowledge, which persisted after adjustment for other factors (objective knowledge: coefficient = −0.074, P = .004; perceived knowledge: coefficient = −0.015, P = .00). Higher educational attainment was associated with higher objective knowledge in bivariate regression (coefficient = 0.714, P = .05), but this association was no longer statistically significant upon adjustment for other factors (coefficient = 0.611, P = .10). Higher income was weakly but significantly associated with higher objective knowledge (coefficient = 1.285 × 10−5, P = .03), but this association did not persist upon adjustment for other factors (coefficient = 8.103 × 10−6, P = .20). Income and educational attainment were not associated with perceived knowledge. Prior completion of RRT modality education was not associated with objective knowledge (coefficient = 1.016, P = .19) but was associated with higher perceived knowledge, which persisted after adjustment for other factors (coefficient = 0.291, P = .02). Among the individuals who completed modality education, time elapsed between the modality education session and survey completion was not associated with perceived knowledge (coefficient = 0.039, R2 = 0.04, P = .07) or objective knowledge (coefficient = 0.007, R2 = 0.002, P = .72). With respect to knowledge about treatment options for kidney failure, prior completion of RRT modality education was not significantly associated with a correct answer to this question on the KiKS test (odds ratio = 1.18, 95% confidence interval = 0.43-3.22). In contrast, prior completion of RRT modality education was associated with higher perceived knowledge of treatment options should kidney function get worse (odds ratio = 3.28, 95% confidence interval = 1.37-7.83).
Table 4.
Linear Regression Analysis for Associations With Objective Knowledge.
| Variable | Objective knowledge |
||||
|---|---|---|---|---|---|
| Bivariate |
Multivariatea |
||||
| Coefficientb (SE) | R 2 | P-value | Coefficient (SE) | P-value | |
| Age | −0.079 (0.03) | 0.07 | .002 | −0.074 (0.03) | .004 |
| Sex | −0.922 (0.70) | 0.01 | .18 | −0.878 (0.69) | .20 |
| Educational attainment | 0.714 (0.36) | 0.03 | .05 | 0.611 (0.37) | .10 |
| Income | 1.285 × 10−5 (0.00) | 0.04 | .03 | 8.103 × 10−6 (0.00) | .20 |
| Systolic blood pressure | −0.012 (0.02) | 0.003 | .53 | −0.002 (0.02) | .91 |
| eGFR | 0.021 (0.06) | 0.001 | .72 | 0.035 (0.06) | .56 |
| Attended modality education | 0.536 (0.74) | 0.004 | .47 | 1.016 (0.77) | .19 |
| Constant | 20.683 (3.13) | ||||
Note. eGFR = estimated glomerular filtration rate; SE = standard error.
R2 = 0.14.
Unstandardized coefficients (B) are reported.
Table 5.
Linear Regression Analysis for Associations With Perceived Knowledge.
| Variable | Perceived knowledge |
||||
|---|---|---|---|---|---|
| Bivariate |
Multivariatea |
||||
| Coefficient (SE)b | R 2 | P-value | Coefficient (SE) | P-value | |
| Age | −0.015 (0.004) | 0.10 | .00 | −0.015 (0.004) | .00 |
| Sex | −0.024 (0.11) | 0.00 | .82 | −0.091 (0.11) | .39 |
| Educational attainment | 0.005 (0.06) | 0.00 | .93 | 0.040 (0.06) | .49 |
| Income | −9.488 × 10−9 (0.00) | 0.00 | .99 | −2.981 × 10−7 (0.00) | .76 |
| Systolic blood pressure | 0.002 (0.003) | 0.002 | .59 | 0.003 (0.003) | .27 |
| eGFR | −0.008 (0.009) | 0.006 | .37 | 0.001 (0.009) | .92 |
| Attended modality education | 0.305 (0.11) | 0.06 | .007 | 0.291 (0.12) | .02 |
| Constant | 3.144 (0.48) | ||||
Note. eGFR = estimated glomerular filtration rate; SE = standard error.
R2 = 0.17.
Unstandardized coefficients (B) are reported.
Discussion
In this cross-sectional study of 125 patients with advanced CKD followed in a multidisciplinary kidney clinic, we found that objective and perceived kidney disease knowledge were modest. This may be due to ineffective or inadequate education provided in the clinic. However, it should also be noted that patients might have limited knowledge on certain topics due to a lack of direct relevance to their care. Similar characteristics were associated with both types of knowledge. Older age was significantly associated with lower objective and perceived knowledge. Other patient characteristics, such as sex, income, and educational attainment, were not independently associated with knowledge levels. There was a weak correlation between objective and perceived kidney disease knowledge, which is consistent with prior literature and suggests that the two are distinct constructs.17,24 Patients’ interpretation of the perceived knowledge response scale may also in part explain the weak correlation.
Our results for several questions on the PiKS and KiKS tests are similar to the studies that validated these surveys.16,17 The validation studies were carried out in patients with CKD stages 1 to 5 followed in general nephrology clinics in the United States and found a median perceived knowledge score of 2.617 and a mean objective knowledge score of 66%.16 On the PiKS test, more than 60% of patients in our study felt that they had little to no knowledge about medications that help or hurt the kidneys; while on the KiKS test, most patients correctly identified that ibuprofen should be avoided (85%) and that medications can be prescribed to protect the kidneys (89%). These results suggest a discrepancy between patients’ perception of their medication knowledge and their actual knowledge. Currently in our multidisciplinary clinic, a pharmacist performs a medication review with the patient at each visit, and teaching is provided regarding harmful medications and “sick day rules” (i.e., holding medications that could precipitate acute kidney injury during times of illness) at the initial clinic visits. Given that medication management is a critical component of CKD care, it is concerning that most patients perceived themselves to have a lack of knowledge and suggests that better educational strategies and improved provider support are needed to improve patient confidence and self efficacy in this area.2
Also consistent with prior results, most patients in our study felt that they have a good amount or a lot of knowledge about why they had been sent to see a kidney doctor, how kidney function is checked, and what their goal blood pressure should be.17 In contrast to the PiKS validation study, more patients in our study perceived that they had a good amount or a lot of knowledge about foods that should be avoided if a person has low kidney function (65% vs 39%) and the functions of the kidney (68% vs 49%). In relation to dietary knowledge, most patients in our study appropriately identified on the KiKS survey the functions of the kidney that pertain to dietary recommendations (e.g., potassium and phosphate control), but other functions like bone health or the simple, seemingly obvious function of making urine were less commonly correctly identified. These results may reflect what is focused on consistently in terms of education in the clinic. A dietitian is available in every clinic and will meet with patients as needed to provide a detailed dietary review; information pamphlets on sodium, phosphate, and potassium restriction are also provided. With respect to symptoms of kidney failure, overall, patients in our study answered more items on the KiKS survey correctly compared with the prior validation study.16 This may be explained by the fact that our study included patients with more advanced CKD who would be much more likely to have many of the symptoms listed on the survey.
The finding of lower knowledge scores in older patients is consistent with prior studies.16,17 One possible explanation for this association is cognitive impairment. We did not formally screen for cognitive impairment in our study, and this is not routinely performed in the MCKC, but it is well described that cognitive changes occur as a normal part of aging and that many age-associated diseases, such as vascular or Alzheimer’s disease, can further accelerate cognitive decline.25 We hypothesized that higher income and educational attainment would be associated with higher knowledge, and this was found for objective knowledge in bivariate analyses, but the association was no longer significant upon adjustment for other factors. This finding is consistent with the results of the objective knowledge survey (KiKS) validation study.16
One of the primary functions of the multidisciplinary clinic is to prepare patients for RRT, which includes modality education. Prior completion of RRT modality education was not associated with higher objective knowledge, including specific knowledge regarding kidney failure treatment options. Conversely, completion of RRT modality education seemed to increase both overall and kidney failure treatment options–related perceived knowledge. This suggests that the RRT education session may make patients feel that their knowledge has increased when in fact their actual knowledge has not significantly increased. This is not to discount the importance of RRT modality education since studies have shown that targeted RRT education can increase home dialysis uptake,6,11,26 but rather suggests that there is an opportunity to improve upon the education delivered in the clinic.
Using previously validated surveys, we were able to characterize 2 different types of CKD knowledge in patients with advanced CKD followed in a multidisciplinary clinic. Important knowledge gaps and patient characteristics associated with lower knowledge levels were identified, which could inform educational strategies in this patient population, with the ultimate goal of improving patient outcomes. There are, however, a number of limitations to our study. We only included patients from a single center; therefore, our results may not be generalizable to other centers where patient populations and educational strategies may differ. There were 145 patients (36% of screened patients) who declined to participate due to unspecified reasons, which may bias the results. Our cohort was primarily Caucasian and only included English-speaking patients, which also may affect generalizability. Formal cognitive testing was not performed and therefore some individuals with unknown dementia may have been enrolled. Health literacy was not formally assessed; low health literacy could affect the ability of an individual to complete the surveys. However, it should be noted that the KiKS survey was written at a sixth-grade reading level.16
In conclusion, despite resource-intensive care, CKD knowledge of patients followed in a multidisciplinary CKD clinic was found to be modest. Whether enhanced educational strategies, such as the use of more videos, measuring knowledge routinely to identify deficiencies, or formally measuring cognition and health literacy to adjust individual patient education accordingly, can improve knowledge and whether increasing knowledge improves patient outcomes warrants further study.
Supplemental Material
Supplemental material, Education_in_MCKC_1 for Perceived and Objective Kidney Disease Knowledge in Patients With Advanced CKD Followed in a Multidisciplinary CKD Clinic by Amber O. Molnar, Ayub Akbari and K. Scott Brimble in Canadian Journal of Kidney Health and Disease
Supplemental material, Supplementary_Tables for Perceived and Objective Kidney Disease Knowledge in Patients With Advanced CKD Followed in a Multidisciplinary CKD Clinic by Amber O. Molnar, Ayub Akbari and K. Scott Brimble in Canadian Journal of Kidney Health and Disease
Footnotes
Ethics Approval and Consent to Participate: This study received approval from the Hamilton Integrated Research Ethics Board. Project number 3562. Participants provided written informed consent.
Consent for Publication: All authors consent to the publication of this study.
Availability of Data and Materials: Data queries can be emailed to Dr. Amber Molnar at amolnar@stjosham.on.ca.
Author Contributions: AOM, AA, and KSB contributed to the study design and review of the manuscript. AOM drafted the first version of the manuscript; conducted the data analysis; had full access to all data in the study; and takes responsibility for its integrity and the data analysis. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was conducted with the support of Cancer Care Ontario through funding provided by the Government of Ontario.
ORCID iD: Amber O. Molnar  https://orcid.org/0000-0003-4549-0202
https://orcid.org/0000-0003-4549-0202
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Wright-Nunes JA, Luther JM, Ikizler TA, Cavanaugh KL. Patient knowledge of blood pressure target is associated with improved blood pressure control in chronic kidney disease. Patient Educ Couns. 2012;88(2):184-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tuot DS, Plantinga LC. What patients don’t know may hurt them: knowledge and the perception of knowledge among patients with CKD. Kidney Int. 2011;80(12):1256-1257. [DOI] [PubMed] [Google Scholar]
- 3. Devins GM, Mendelssohn DC, Barre PE, Binik YM. Predialysis psychoeducational intervention and coping styles influence time to dialysis in chronic kidney disease. Am J Kidney Dis. 2003;42(4):693-703. [DOI] [PubMed] [Google Scholar]
- 4. Devins GM, Mendelssohn DC, Barre PE, Taub K, Binik YM. Predialysis psychoeducational intervention extends survival in CKD: a 20-year follow-up. Am J Kidney Dis. 2005;46(6):1088-1098. [DOI] [PubMed] [Google Scholar]
- 5. Lacson E, Jr, Wang W, DeVries C, et al. Effects of a nationwide predialysis educational program on modality choice, vascular access, and patient outcomes. Am J Kidney Dis. 2011;58(2):235-242. [DOI] [PubMed] [Google Scholar]
- 6. Mehrotra R, Marsh D, Vonesh E, Peters V, Nissenson A. Patient education and access of ESRD patients to renal replacement therapies beyond in-center hemodialysis. Kidney Int. 2005;68(1):378-390. [DOI] [PubMed] [Google Scholar]
- 7. Fishbane S, Agoritsas S, Bellucci A, et al. Augmented nurse care management in CKD stages 4 to 5: a randomized trial. Am J Kidney Dis. 2017;70(4):498-505. [DOI] [PubMed] [Google Scholar]
- 8. Hsu CK, Lee CC, Chen YT, et al. Multidisciplinary predialysis education reduces incidence of peritonitis and subsequent death in peritoneal dialysis patients: 5-year cohort study. PLoS One. 2018;13(8):e0202781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kurella Tamura M, Li S, Chen SC, et al. Educational programs improve the preparation for dialysis and survival of patients with chronic kidney disease. Kidney Int. 2014;85(3):686-692. [DOI] [PubMed] [Google Scholar]
- 10. Milazi M, Bonner A, Douglas C. Effectiveness of educational or behavioral interventions on adherence to phosphate control in adults receiving hemodialysis: a systematic review. JBI Database System Rev Implement Rep. 2017;15(4):971-1010. [DOI] [PubMed] [Google Scholar]
- 11. Ribitsch W, Haditsch B, Otto R, et al. Effects of a pre-dialysis patient education program on the relative frequencies of dialysis modalities. Perit Dial Int. 2013;33(4):367-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yu YJ, Wu IW, Huang CY, et al. Multidisciplinary predialysis education reduced the inpatient and total medical costs of the first 6 months of dialysis in incident hemodialysis patients. PLoS One. 2014;9(11):e112820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cassidy BP, Getchell LE, Harwood L, Hemmett J, Moist LM. Barriers to education and shared decision making in the chronic kidney disease population: a narrative review. Can J Kidney Health Dis. 2018;5:1-11. doi: 10.1177/2054358118803322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Nickolas TL, Frisch GD, Opotowsky AR, Arons R, Radhakrishnan J. Awareness of kidney disease in the US population: findings from the National Health and Nutrition Examination Survey (NHANES) 1999 to 2000. Am J Kidney Dis. 2004;44(2):185-197. [DOI] [PubMed] [Google Scholar]
- 15. Plantinga LC, Boulware LE, Coresh J, et al. Patient awareness of chronic kidney disease: trends and predictors. Arch Intern Med. 2008;168(20):2268-2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wright JA, Wallston KA, Elasy TA, Ikizler TA, Cavanaugh KL. Development and results of a kidney disease knowledge survey given to patients with CKD. Am J Kidney Dis. 2011;57(3):387-395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wright Nunes JA, Wallston KA, Eden SK, Shintani AK, Ikizler TA, Cavanaugh KL. Associations among perceived and objective disease knowledge and satisfaction with physician communication in patients with chronic kidney disease. Kidney Int. 2011;80(12):1344-1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Finkelstein FO, Story K, Firanek C, et al. Perceived knowledge among patients cared for by nephrologists about chronic kidney disease and end-stage renal disease therapies. Kidney Int. 2008;74(9):1178-1184. [DOI] [PubMed] [Google Scholar]
- 19. Tangri N, Stevens LA, Griffith J, et al. A predictive model for progression of chronic kidney disease to kidney failure. JAMA. 2011;305(15):1553-1559. [DOI] [PubMed] [Google Scholar]
- 20. Multi-Care Kidney Clinic Best Practices. Ontario Renal Network. https://www.ontariorenalnetwork.ca/en/kidney-care-resources/clinical-tools/advanced-kidney-disease/multi-care-kidney-clinic-best-practices. Accessed January 23, 2020.
- 21. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453-1457. [DOI] [PubMed] [Google Scholar]
- 22. Hypertension Canada Guidelines. Prevention and Treatment. https://guidelines.hypertension.ca/prevention-treatment/. Accessed February 10, 2019.
- 23. Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604-612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sepucha KR, Fagerlin A, Couper MP, Levin CA, Singer E, Zikmund-Fisher BJ. How does feeling informed relate to being informed? The DECISIONS survey. Med Decis Making. 2010;30(5 suppl):77s-84s. [DOI] [PubMed] [Google Scholar]
- 25. Murman DL. The impact of age on cognition. Semin Hear. 2015;36(3):111-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Golper T. Patient education: can it maximize the success of therapy. Nephrol Dial Transplant. 2001;16(suppl 7):20-24. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Education_in_MCKC_1 for Perceived and Objective Kidney Disease Knowledge in Patients With Advanced CKD Followed in a Multidisciplinary CKD Clinic by Amber O. Molnar, Ayub Akbari and K. Scott Brimble in Canadian Journal of Kidney Health and Disease
Supplemental material, Supplementary_Tables for Perceived and Objective Kidney Disease Knowledge in Patients With Advanced CKD Followed in a Multidisciplinary CKD Clinic by Amber O. Molnar, Ayub Akbari and K. Scott Brimble in Canadian Journal of Kidney Health and Disease