Abstract
Background:
There is a lack of large-scale data that examine complications in plastic surgery. A description of baseline rates and patient outcomes allows better understanding of ways to improve patient care and cost-savings for health systems. Herein, we determine the most frequent complications in plastic surgery, identify procedures with high complication rates, and examine predictive risk factors.
Methods:
A retrospective analysis of the 2012 to 2016 American College of Surgeons National Surgical Quality Improvement Program plastic surgery data set was conducted. Complication rates were calculated for the entire cohort and each procedure therein. Microsurgical procedures were analyzed as a subgroup, where multivariate logistic regression models determined the risk factors for surgical site infection (SSI) and related reoperation.
Results:
We identified 108 303 patients undergoing a plastic surgery procedure of which 6 264 (5.78%) experienced ≥1 complication. The outcome with the highest incidence was related reoperation (3.31%), followed by SSI (3.11%). Microsurgical cases comprised 6 148 (5.68%) of all cases, and 1211 (19.33%) experienced ≥1 complication. Similar to the entire cohort, the related reoperation (12.83%) and SSI (5.66%) were common complications. Increased operative time was a common independent risk factor predictive of a related reoperation or development of an SSI (P < 001). Of all microsurgeries, 23.3% had an operative time larger than 10 hours which lead to faster increase in reoperation likelihood.
Conclusions:
The complication rate in plastic surgery remains relatively low but is significantly increased for microsurgery. Increased operative time is a common risk factor. Two-team approaches and staged operations could be explored, as a large portion of microsurgeries are vulnerable to increased complications.
Keywords: plastic, surgery, microsurgery, surgical site infection, postoperative complications, outcomes, ACS NSQIP
Abstract
Historique :
Les données à grande échelle sur les complications de la chirurgie plastique font défaut. Une description des taux de référence et des résultats cliniques des patients permettrait de mieux déterminer comment améliorer les soins aux patients et réaliser des économies dans les systèmes de santé. Dans le présent article, les chercheurs recensent les complications les plus fréquentes en chirurgie plastique, dégagent les interventions aux taux de complication élevés et examinent les facteurs de risque prédictifs.
Méthodologie :
Les chercheurs ont réalisé une analyse rétrospective des données de chirurgie plastique tirées du programme national d’amélioration de la qualité chirurgicale de l’American College of Surgeons entre 2012 et 2016. Ils ont calculé les taux de complications de toute la cohorte et de chaque intervention recensée. Ils ont analysé les interventions microchirurgicales en sous-groupe, où ils ont utilisé des modèles de régression logistique multivariée pour déterminer les facteurs de risque d’infection des plaies opératoires (IPO) et de réopérations s’y rapportant.
Résultats :
Les chercheurs ont dénombré 108 303 patients qui avaient subi une intervention en chirurgie plastique, dont 6 264 (5,78 %) avaient souffert d’au moins une complication. Les réopérations (3,31 %), suivies des IPO (3,11 %) étaient les résultats à la plus forte incidence. Les cas de microchirurgie représentaient 6 148 (5,68 %) de toutes les occurrences, et 1211 (19,33 %) ont souffert d’au moins une complication. Tout comme dans l’ensemble de la cohorte, les réopérations (12,83 %) et les IPO (5,66 %) étaient des complications courantes. La plus longue durée de l’opération était un facteur de risque indépendant fréquent, prédicteur d’une réopération ou d’une IPO (p<0,001). Ainsi, 23,3 % des microchirurgies duraient plus de dix heures, ce qui s’associait à une plus forte augmentation du risque de réopération.
Conclusions :
Le taux de complications demeure relativement faible en chirurgie plastique, mais est significativement plus élevé en microchirurgie. La longue durée des opérations représente un facteur de risque courant. On pourrait explorer les approches à deux équipes et les opérations échelonnées, car une forte proportion des microchirurgies sont vulnérables à un accroissement des complications.
Background
With the growing interest in patient safety and system sustainability, increased public scrutiny has been placed on providing high-value care. Although surgical care has significantly improved over the past 10 years, postoperative complications remain a significant source of morbidity, mortality and cost to health systems.1-3
To our knowledge, there has been no study that has characterized postoperative outcomes in plastic surgery on a population-based scale. Because plastic surgeons treat a breadth of conditions, establishing baseline complication rates would provide surgeons the ability to compare surgical procedures that exist for the management of the same condition. In addition, baseline rates are necessary to compare outcomes between different health conditions and various specialties.
One database that provides a robust cohort of patients for high-powered retrospective studies is the American College of Surgeons National Surgical Quality Improvement Program (NSQIP). The NSQIP is multi-institutional, validated, and collects over 250 demographic variables and 30-day postoperative outcomes. Previous NSQIP studies in plastic surgery use data derived from a single procedure with a narrow focus.
The primary objective of this study is to use the NSQIP database to determine the most common 30-day postoperative outcomes and to identify procedures with high complication rates. The secondary objective of this study is to characterize the volume and complications associated with these “high-risk” procedures and to investigate their predictive clinical risk factors, respectively. A better understanding of these cases may help plastic surgeons to improve the delivery of surgical care by identifying patients at higher risk of postoperative complications and developing risk reduction strategies.
Methods
Data Sets
A retrospective analysis of the 2012 to 2016 NSQIP data sets was conducted. The methods of NSQIP including data collection, sampling, and validation have been described previously.4,5 The full list of variables can be found on the NSQIP website (http://site.acsnsqip.org/). The participant use files were compiled and queried for plastic surgery cases as defined by the principal operative procedure. Approval from our local institutional review board was obtained for this study (H17-00420).
We excluded patients with Current Procedural Terminology (CPT) codes less than 10 cases (specifically, 15842, 42894, 20955, 20962, 26551, 26553) within the database. To reduce noise in the estimation, patients with at least 1 of the following conditions were also excluded: ELECTSURG = Unknown, DYSPNEA = At rest, FNSTATUS2 = Unknown, FNSTATUS2 = Total dependent, and FLAP = Trunk, as they contained less than 15 observations.
Only variables that were collected for all 5 years were included in the analysis. To improve the power of the study, composite variables were created by grouping clinical risk factors together. For example, a cardiac history was defined as having a history of congestive heart failure. A pulmonary history was defined as having a history of dyspnea, ventilator dependence, or chronic obstructive pulmonary disease. A renal history was defined as having a history of acute renal failure or current use of dialysis. A liver history was defined as having history of ascites. Body mass index (BMI; kg/m2) was calculated and stratified into definitions based on the World Health Organization definition of obesity.
Post-Operative 30-Day Outcomes
The incidence of each post-operative 30-day outcome was calculated and categorized as a complication or a system performance measure (SPM). The complications included acute renal failure, cardiac arrest requiring cardiopulmonary resuscitation (CPR), death, deep vein thrombosis (DVT) requiring therapy, failure to wean, myocardial infarction, pneumonia, pulmonary embolism, renal insufficiency, sepsis, septic shock, stroke/cerebrovascular accident (CVA), surgical site infection (SSI), transfusion, urinary tract infection, and wound dehiscence. The SPMs included still in hospital after 30 days, related reoperation, and unplanned and related readmission.
Subgroup Analysis
A trend analysis was used to determine the procedures associated with a higher occurrence of complications. Based on the 2010 CPT codes, all procedures with n > 100 were ranked and ordered based on the cumulative incidence of all postoperative complications and SPMs.
Given the complexity associated with microsurgery, free flap surgeries requiring microvascular anastomosis were analyzed as a subgroup. Two independent reviewers identified the following 11 CPT codes as microsurgery procedures: breast reconstruction free flap (19 364), free muscle or myocutaneous flap with microvascular anastomosis (15 756), free skin flap with microvascular anastomosis (15 757), free fascial flap with microvascular anastomosis (15 758), breast reconstruction with transverse rectus abdominis myocutaneous flap (19 368), free muscle flap by micro-technique (15 842), bone graft from fibula with microvascular anastomosis (20 955), bone graft with microanastamosis, other than fibular, iliac crest or metatarsal (20 962), transfer, toe-to-hand with microanastamosis (26 551), transfer, toe-to-hand with microanastamosis, other than great toe, single (26 553), and reconstruction of pharyngeal wall closure with flap or flap with microvascular anastomosis (42 894).
Statistical Analysis
We used descriptive statistics for patient demographics and clinical characteristics. For the microsurgical subgroup, we identified independent predictors of the most frequent complication events and quality measure using separate multivariate logistic regression to study the impact of certain variables on binary outcome such as SSI and related reoperation while keeping other variables constant. We reported the significant predictive risk factors (P < .05) with odds ratios (ORs).
We compared different models of operative time (ie, quadratic and piecewise linear) to test its impact on the likelihood of SSI and related reoperation. For each model, we estimated the coefficients with 95% confidence intervals. The goodness of fitness was measured by the area under receiver–operating characteristic curves (AUC-ROC). To find the appropriate piecewise linear model, we conducted 5-fold cross-validation tests. All analyses were conducted in R software, version 3.4.3.
Results
Population Characteristics
Over the 5-year study period, NSQIP captured a total of 108 303 plastic surgery cases. Table 1 summarizes the demographic, clinical characteristics, and descriptive statistics of the population-based cohort. Breast procedures comprised the majority of cases, specifically reduction mammoplasty (17%), breast reconstruction (15%), mastopexy (11%), and breast free flaps (4.5%). Other frequent procedures included infraumbilical panniculectomies (9%) and muscle myocutaneous/fasciocutaneous truncal flaps (2%).
Table 1.
Population Characteristics and Microsurgical Population Characteristics.
| Clinical Variable | All Patients, N = 108 303, Count (Proportion)/Mean (±Standard Deviation) | Microsurgery Subgroup, n = 6148, Count (Proportion)/Mean (±Standard Deviation) |
|---|---|---|
| Sex | ||
| Female | 90 499 (84%) | 5330 (90%) |
| Male | 17 804 (16%) | 618 (10%) |
| Outpatient | ||
| Yes | 77 728 (72%) | 202 (3.3%) |
| Age | 49 (±7) | 51 (±6) |
| BMI | ||
| Underweight (<18.5) | 1803 | 54 |
| Normal (18.5-24.9) | 33 641 | 1426 |
| Overweight (25.0-29.9) | 34 348 | 2222 |
| Obese class I (30.0-34.9) | 21 190 | 1549 |
| Obese class II (35.0-39.9) | 9573 | 619 |
| Obese class III (>40) | 6138 | 248 |
| Missing | 1610 | 30 |
| Diabetes | ||
| Insulin | 3025 (2.8%) | 112 (1.8%) |
| Non-insulin | 5243 (4.8%) | 298 (4.8%) |
| No diabetes | 100 035 (92.4%) | 5738 (93.3%) |
| Smoking | 14 100 (13%) | 633 (10%) |
| Pulmonary history | 3609 (3.3%) | 144 (2.3%) |
| Liver history | 35 (0.033%) | 0 (0%) |
| Cardiac history | 270 (0.25%) | 5 (0.081%) |
| Renal history | 503 (0.46%) | 5 (0.081%) |
| Hypertension | 27 155 (25%) | 1549 (25%) |
| Wound infection | 6478 (6.0%) | 317 (5.2%) |
| Steroid use | 2345 (2.2%) | 113 (1.8%) |
| Weight loss | 361 (0.33%) | 45 (0.73%) |
| Bleeding disorder | 1585 (1.5%) | 55 (0.89%) |
| Transfusion | 258 (0.24%) | 9 (0.15%) |
| Other procedure | 38 570 (36%) | 1682 (27%) |
| Concurrent procedure | 16 075 (15%) | 2634 (43%) |
| Wound class | ||
| I | 94 855 (87.6%) | 5563 (90.5%) |
| II | 6100 (5.6%) | 361 (5.9%) |
| III | 4078 (3.8%) | 128 (2.1%) |
| IV | 3270 (3.0%) | 96 (1.6%) |
| ASA class | ||
| I | 18 859 (17.4%) | 308 (5.01%) |
| II | 61 120 (56.4%) | 3299 (53.7%) |
| III | 25 888 (23.9%) | 2483 (40.4%) |
| IV | 15 454 (1.3%) | 53 (0.9%) |
| V | 13 (0.012%) | 0 (0%) |
| None assigned | 869 (8.024%) | 5 (0.081%) |
| Operative time, hours | 2.553 (±2.210) | 8.025 (±2.954) |
Abbreviation: BMI, body mass index.
The study cohort consisted of mostly women (84%) and outpatients (72%). The mean age was 49 ± 7 years, and the mean BMI was 28.5 ± 5.9 kg/m2. The overall prevalence of comorbidities was low with the exception of medically treated hypertension (25%). The majority of patients were categorized as ASA class II (56%) and wound class I (88%). The mean operative time was 2.553 ± 2.210 hours.
Thirty-Day Postoperative Outcomes Profile
Of all the plastic surgery cases, 6264 (5.78%) had the occurrence of ≥1 complication. The complications with the highest incidences were SSI (3.11%) and transfusion (1.87%). The SPM with the highest incidences were related reoperation (3.31%) and unplanned related readmission (2.62%). The incidences of the post-operative 30-day outcomes are listed in Table 2 and stratified by procedure in Table 3.
Table 2.
Incidences of 30-Day Postoperative Outcomes for All Plastic Surgery Procedures and Microsurgical Procedures.
| Outcome | All Plastic Surgery Procedures, N = 108 303 | Microsurgical Procedures, n = 6148 | ||
|---|---|---|---|---|
| Number of Cases (n) | Proportion of Cases (%) | Number of Cases (n) | Proportion of Cases (%) | |
| Complication | ||||
| Any | 10 983 | 10.14 | 1211 | 19.96 |
| Surgical site infection | 3366 | 3.11 | 717 | 5.66 |
| Transfusion | 2020 | 1.87 | 348 | 11.66 |
| Wound dehiscence | 915 | 0.84 | 113 | 1.84 |
| Sepsis | 596 | 0.55 | 66 | 1.07 |
| Urinary tract infection | 449 | 0.41 | 47 | 0.76 |
| Pneumonia | 267 | 0.25 | 54 | 0.88 |
| DVT requiring therapy | 242 | 0.22 | 55 | 0.89 |
| Death | 189 | 0.17 | 7 | 0.11 |
| Fail to wean | 188 | 0.17 | 38 | 0.62 |
| Pulmonary embolism | 171 | 0.16 | 25 | 0.41 |
| Unplanned intubation | 158 | 0.15 | 27 | 0.44 |
| Septic shock | 135 | 0.12 | 9 | 0.15 |
| Acute renal failure | 64 | 0.06 | 5 | 0.08 |
| Cardiac arrest requiring CPR | 51 | 0.05 | 7 | 0.11 |
| Myocardial infarction | 59 | 0.05 | 7 | 0.11 |
| Renal insufficiency | 52 | 0.05 | 4 | 0.07 |
| Stroke/CVA | 41 | 0.04 | 4 | 0.07 |
| System performance measure | ||||
| Unplanned, related reoperation | 3589 | 3.31 | 789 | 12.83 |
| Unplanned, related readmission | 2835 | 2.62 | 329 | 5.25 |
| Still in hospital | 329 | 0.3 | 18 | 0.29 |
Table 3.
Incidences of 30-Day Postoperative Outcomes Stratified by the Most Common Procedures.a
| N | Death | Cardiac Arrest Requiring CPR | DVT Requiring Therapy | Fail to Wean | Myocardial Infection | Pneumonia | Pulmonary Embolism | Renal Insufficiency | Septic Shock | Stroke/CVA | Surgical Site Infection | Wound Dehiscence | Unplanned Intubation | Urinary Tract Infection | Related Readmission | Related Reoperation | Still in Hospital | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reduction mammaplasty | 18 417 | 0.01 | 0.00 | 0.26 | 0.01 | 0.01 | 0.05 | 0.09 | 0.01 | 0.01 | 0.02 | 3.12 | 0.68 | 0.01 | 0.14 | 1.31 | 1.83 | 0.02 |
| BRST RCNSTJ IMMT/DLYD W/TISS EXPANDER SBSQ XPNSJ | 10 067 | 0.01 | 0.00 | 0.61 | 0.00 | 0.00 | 0.02 | 0.13 | 0.01 | 0.01 | 0.01 | 3.40 | 0.75 | 0.00 | 0.26 | 4.14 | 5.51 | 0.02 |
| Revision reconstructed breast | 6500 | 0.02 | 0.00 | 0.29 | 0.02 | 0.01 | 0.06 | 0.00 | 0.00 | 0.00 | 0.02 | 1.18 | 0.37 | 0.05 | 0.23 | 1.66 | 1.72 | 0.00 |
| Excision SKIN ABD infraumbilical panniculectomy | 6461 | 0.05 | 0.05 | 2.65 | 0.12 | 0.01 | 0.19 | 0.42 | 0.05 | 0.15 | 0.03 | 4.89 | 1.18 | 0.12 | 0.65 | 4.23 | 2.86 | 0.11 |
| IMMT INSJ BRST PROSTH FLWG MASTOPEXY MAST/RCNSTJ | 5313 | 0.00 | 0.00 | 0.30 | 0.04 | 0.01 | 0.08 | 0.08 | 0.00 | 0.02 | 0.00 | 2.13 | 0.70 | 0.02 | 0.24 | 2.90 | 3.76 | 0.00 |
| Breast reconstruction free flap | 4898 | 0.06 | 0.06 | 11.31 | 0.10 | 0.02 | 0.59 | 0.39 | 0.02 | 0.06 | 0.04 | 4.74 | 1.80 | 0.24 | 0.78 | 5.23 | 12.21 | 0.02 |
| DLYD INSJ BRST PROSTH FLWG MASTOPEXY MAST/RCNSTJ | 4718 | 0.06 | 0.02 | 0.08 | 0.00 | 0.01 | 0.00 | 0.06 | 0.00 | 0.00 | 0.00 | 1.40 | 0.38 | 0.00 | 0.19 | 1.95 | 1.93 | 0.04 |
| Mammaplasty augmentation W/prosthetic implant | 4665 | 0.00 | 0.00 | 0.04 | 0.00 | 0.00 | 0.00 | 0.06 | 0.00 | 0.00 | 0.00 | 0.47 | 0.11 | 0.00 | 0.17 | 0.84 | 1.41 | 0.02 |
| Mastopexy | 2345 | 0.04 | 0.04 | 0.21 | 0.00 | 0.00 | 0.00 | 0.13 | 0.00 | 0.04 | 0.00 | 1.11 | 0.51 | 0.04 | 0.21 | 1.32 | 1.36 | 0.13 |
| Breast reconstruction other technique | 2110 | 0.09 | 0.00 | 0.95 | 0.00 | 0.01 | 0.05 | 0.19 | 0.00 | 0.00 | 0.00 | 1.80 | 0.95 | 0.00 | 0.24 | 2.13 | 2.84 | 0.00 |
| Musc myocutaneous/fasciocutaneous flap trunk | 2094 | 0.81 | 0.29 | 10.79 | 1.19 | 0.04 | 1.67 | 0.57 | 0.33 | 1.15 | 0.19 | 8.60 | 3.49 | 1.48 | 2.29 | 6.92 | 6.40 | 2.15 |
| Periprosthetic capsulectomy breast | 2,075 | 0.10 | 0.00 | 0.24 | 0.00 | 0.00 | 0.10 | 0.00 | 0.00 | 0.00 | 0.00 | 1.93 | 0.43 | 0.00 | 0.24 | 1.78 | 2.27 | 0.00 |
| BRST RCNSTJ W/LATSMS D/SI FLAP WO PRSTHC IMPL | 2023 | 0.10 | 0.00 | 1.88 | 0.00 | 0.01 | 0.10 | 0.20 | 0.00 | 0.10 | 0.10 | 4.35 | 1.53 | 0.00 | 0.35 | 4.25 | 5.09 | 0.00 |
| Nipple/areola reconstruction | 1715 | 0.00 | 0.00 | 0.06 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.70 | 0.35 | 0.00 | 0.17 | 0.76 | 0.87 | 0.00 |
| Open periprosthetic capsulotomy breast | 1166 | 0.09 | 0.00 | 0.09 | 0.00 | 0.00 | 0.09 | 0.09 | 0.00 | 0.00 | 0.00 | 1.89 | 0.26 | 0.00 | 0.34 | 2.23 | 1.63 | 0.09 |
a Only procedures with >1000 occurrences are listed.
Related Reoperation Qualitative Analysis
The most common reason for reoperation included hemorrhage, hematoma, or seroma complicating a procedure (n = 802), postoperative infection (n = 192), disruption of wound (n = 175), infection and inflammatory process related to internal prosthetic, implant, or graft (n = 130), and mechanical complication of prosthetic, implant, or graft (n = 127).
High-Risk Procedures
The incidence of ≥1 complication was calculated for all 1040 unique procedures, and the 10 procedures with the highest incidences were included in a trend analysis. The average incidence of ≥1 complication was highest for free flap surgeries requiring microvascular anastomosis (24.9%), followed by debridement procedures (22.7%) and other flap surgeries (21.7%). This procedure was repeated for the SPMs. Eight of the procedures with the highest incidence of ≥1 complication also have the poorest SPMs.
Microsurgery Subgroup
Population characteristics
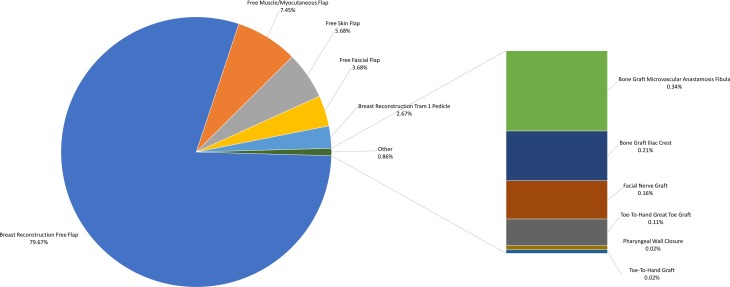
Since microsurgery procedures had the highest incidence of complications, we sought to study these procedures further. Microsurgeries made up 6148 (5.68%) of all plastic surgery cases, where the majority were breast reconstruction free flaps (80%), followed by free muscle/myocutaneous flaps (7.5%), and free skin flaps (5.7%). The proportion of each procedure is represented in Figure 1.
Figure 1.
Proportion of procedures in the microsurgery subgroup.
The microsurgical demographics and clinical characteristics are presented in Table 1. In contrast to the larger cohort of plastic surgery patients, the microsurgery subgroup had a greater proportion of inpatients (96%) undergoing a higher rate of concurrent procedures (43%). Similar to the larger cohort, the majority of patients were categorized as ASA class II (54%), but a larger proportion were categorized as ASA class III (40%). The mean operative time was 2.7 times longer at 8.025 ± 2.954 hours.
Thirty-day post-operative outcomes profile
As a subgroup, microsurgeries accounted for 19.33% of any plastic surgery complication in the NSQIP database. Within the subgroup, 1211 (19.96%) cases reported ≥1 complication. The top complications included transfusion (11.66%) and SSI (5.66%). The SPM with the highest incidences were related reoperation (12.83%) and unplanned related readmission (5.35%). The incidences of all outcomes are listed in Table 2.
Related reoperation qualitative analysis
The most common reasons for reoperation in the microsurgery group included hemorrhage or hematoma or seroma complicating a procedure (n = 159), other complications of internal prosthetic device (n = 60), mechanical complication of prosthetic device, implant, or graft (n = 46), disruption of wound (n = 44), postoperative infection (n = 31), and arterial or venous embolism and thrombosis (n = 24).
Multivariate logistic regression
We included 6020 microsurgery cases for the multivariate logistic regression. Generally, the top complication and SPM (SSI and related reoperation) were predicted by different independent risk factors (Table 4). The significant patient risk factors for SSIs included a history of diabetes requiring insulin (OR: 2.1107, P < .05), diabetes not requiring insulin (OR: 1.4878, P < .01), smoking (OR: 2.0551, P < .001), and steroid use (OR: 3.3275, P < .001). The operative risk factors included head and neck surgeries (OR: 1.9387, P < .05), wound class II to IV (OR: 1.7182, P < .05; OR: 2.2854, P < .01; OR: 2.0888, P < .05). Patients undergoing multiple procedures (OR: 0.9011, P < .01) were predictive for less SSIs. Patients in higher ASA classes were also predictive for less SSIs; however, this trend was not significant.
Table 4.
Microsurgery Subgroup Multivariate Regression Analysis.
| Complication | Variable | Odds Ratio | P Value |
|---|---|---|---|
| Surgical site infection | Outpatient status | 0.3790 | .0474a |
| Diabetes: requiring insulin | 2.1107 | .0139a | |
| Diabetes: not requiring insulin | 1.4878 | .0776b | |
| Smoking | 2.0241 | .0000064c | |
| Steroid use | 3.3275 | .0000112c | |
| Number of other procedures | 0.9011 | .00364b | |
| Wound class: 2 | 1.7183 | .0277a | |
| Wound class: 3 | 2.2854 | .00901b | |
| Wound class: 4 | 2.0888 | .0490a | |
| Flap: Head and Neck | 1.9387 | .0175a | |
| Related reoperation | Outpatient status | 0.3023 | .00294b |
| Hypertension | 1.2254 | .0352a | |
| Functional status: independent | 0.5971 | .0371a | |
| Number of concurrent procedures | 1.0547 | .0327a | |
| Operative time | 1.0910 | 3.44e10−10c |
a P < .05.
b P < .01.
c P < .001.
The only modifiable patient factor predicting related reoperations was hypertension requiring medication (OR: 1.2254, P < .05). Outpatient surgeries and patients who were functionally independent were at lower risk for a related reoperation (OR: 0.3023, P < .01 and OR: 0.5971, P < .05, respectively).
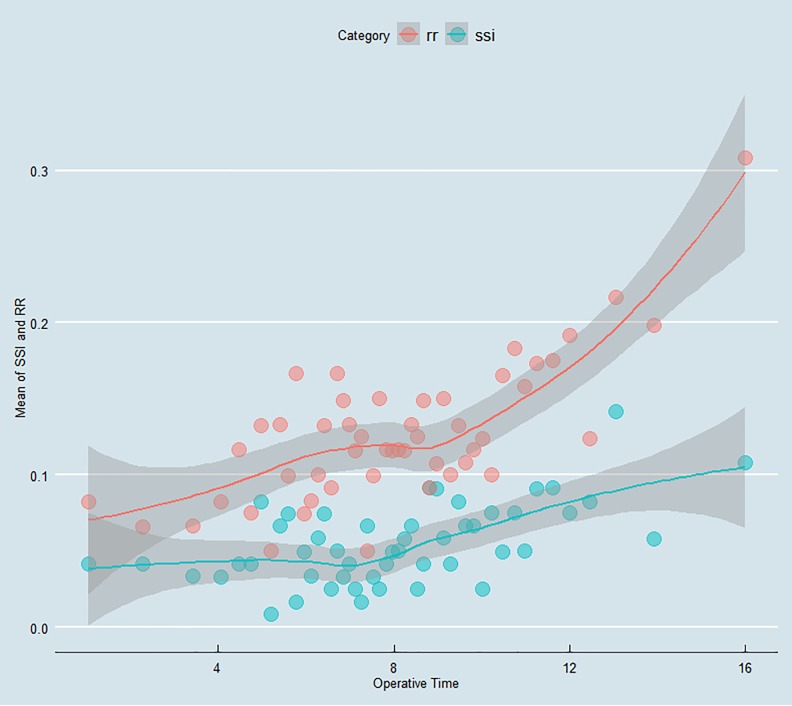
Operative time analysis
Increased operative time was a common independent predictor for both outcomes. For every additional hour of operative time, the odds of developing an SSI or reoperation increased (OR: 1.0827, P < .001; OR: 1.0910, P < .001). This is illustrated by the marginal analysis showing that procedures <6 hours had less complications than procedures ≥8 hours (P < .05; Table 5).
Table 5.
Microsurgery Surgical Site Infection and Related Reoperation Rates Stratified by Operative Time.
| Complication | Operative Time, hours | Number of Cases, n | Proportion of Cases, % | Occurrence Rate, % | P Value |
|---|---|---|---|---|---|
| Surgical site infection | <6 | 1433 | 23.80 | 4.33 | |
| 6-8 | 1677 | 27.85 | 4.11 | .796 | |
| 8-10 | 1521 | 25.26 | 5.98 | .049a | |
| >10 | 1389 | 23.07 | 7.99 | 2e10−10b | |
| Related reoperation | <6 | 1433 | 23.80 | 9.56 | |
| 6-8 | 1677 | 27.85 | 11.63 | .083 | |
| 8-10 | 1521 | 25.26 | 12.23 | .029a | |
| >10 | 1389 | 23.07 | 17.64 | 1e10−10b |
a P < .05.
b P < .001.
A scatterplot of operative time versus SSI and related reoperation (Figure 2) validated that the likelihood of SSI and related reoperation increase with longer operative times. Moreover, the fitted curves of scatterplot suggested that operative time may have a non-linear impact on the likelihood of SSI and related reoperation. For SSIs, the mean AUC-ROC values suggest that linear model is slightly better (0.6814 > 0.6813) but is not statistically significant (P = .816). For related reoperations, the mean AUC-ROC suggest that the piecewise linear model significantly outperformed the linear model than that of the linear model (0.5993 > 0.5988, P = .027). Taken together, these results imply that for microsurgeries, the likelihood of a related reoperation increases with operative time and that the likelihood increases 3-fold once the operative time has exceeded 10 hours.
Figure 2.
Scatter plot of operative time versus surgical site infection (SSI) and related reoperation (RR).
It should be noted that the number of microsurgeries that had an operative time ≥10 hours was 23.3% (1434), and of these procedures, 51.7% (742) had at least one concurrent procedure. For microsurgeries that had an operative time of ≤10 hours, 45.2% (1892) had at least 1 concurrent procedure.
Discussion
Herein, we provide the largest examination of plastic surgery postoperative complications to date using a validated, multicenter surgical outcomes database. Overall, complication rates after plastic surgery remain low (5.78%).
Microsurgery Complication Rates
Microsurgery has become a pillar of plastic surgery, allowing surgeons to perform single-stage reconstructions of complex defects. However, microsurgery is still associated with a high rate of postoperative complications (19.33% in our study), including flap failure, thrombosis, wound dehiscence, and SSI.6-9
From a health systems perspective, microsurgical complications are a significant driver of cost by prolonging hospital stays and the need for additional interventions.10 Depending on the type of intervention needed, costs increase from US$20 00011 to US$50 000.10,12 In our study, there was a higher rate of reoperation and readmission in the microsurgery subgroup. Although we cannot differentiate which were due to flap failures, other NSQIP studies have found flap failure rates of 5% to 10%.13 The high rates of microsurgical complications indicate that there is a significant strain on health system resources, and the need to perform microsurgeries should continually be justified.
Risk Factors for Poor Outcomes in Microsurgery
Studies have found that overall microsurgeries are cost-effective14,15 and improve patient satisfaction and quality-of-life outcomes.16 Compared to previous NSQIP studies,8,17-22 our study found similar risk factors for surgeries that developed complications. By providing the largest and most generalizable analysis to date, we hope to support plastic surgeons apply the current evidence to their preoperative risk assessments.
Surgical Site Infections
Surgical site infections cause significant patient morbidity and mortality and cost between US$1 billion to US$10 billion annually.23 Our large, heterogenous cohort found that the modifiable risk factors of smoking, diabetes, and preoperative steroid use are predictive of SSIs—all well characterized by previous studies.24-27 The characteristics that put patients at higher risk included head and neck surgeries and higher wound classes, likely due to the clean contaminated nature of the surgical site.17,19
Interestingly, our study found that lower ASA classes are associated with more SSIs, conflicting with the majority of previously published studies.6,17,20,28 A likely explanation for this finding is because our regression controlled for operative time, lower ASA classes with operative times equal to higher ASA classes represent a subset of cases with “prolonged” operative times. These cases may have experienced unforeseen events leading to the prolonged operative times, which we and others have shown to independently increase the risk of SSIs.17,29-31
Related Reoperation
Previous studies have established that unplanned reoperations are a useful measure of quality32-35 and that outcomes can be optimized by identifying patients at higher risk.
There has only been 1 NSQIP study that identified risk factors for unplanned reoperation of microsurgical procedures as an ASA class ≥3 and operative time ≥10 hours.35 Similarly, our study found that longer operative times is a risk factor. However, we found that hypertension was the only modifiable risk factor.36 The differences in our findings is likely related to the differences in our analyses: Kwok et al included only the variables significant on univariate analysis in the multivariate regression model, while we included all preoperative and intra-operative variables.
The Effect of Operative Time on Microsurgical Outcomes
It has been widely reported in the existing literature that operative duration is an independent risk factor for a variety of complications,37 including free flap failure,13,38 infection,37 reoperation,37 and readmission.21,22 Studies suggest that complications occur more frequently when operative times have exceeded a certain threshold.39 For plastic surgery, this recommendation is 6 hours.40,41
To validate this, our analysis evaluated a best-fit model for SSIs and reoperations. Although we could not make a strong conclusion for SSIs, the likelihood of related reoperations increases 3-fold for operations >10 hours. This has important implications as a substantial proportion of microsurgery procedures (with no concurrent procedures) have an operative time >10 hours (11.3%). Our study urges surgeons to recognize that risk increases significantly after this threshold.
Consideration can be given to 2-team approaches and staged operations, as a large portion of microsurgeries are vulnerable to poor outcomes. There have been several small patient series, which have shown that there is no increase in complication rates for combined procedures.42-47 Whether or not this strategy is feasible and if it will improve patient outcomes still needs to be explored.
Limitations
Limitations to this study include those inherent to the NSQIP database. The NSQIP does not capture important procedures (ie, traumas and burns) and perioperative outcomes specific to plastic surgery.48 For example, these include prophylactic antibiotic use, free flap failure, and functional, long-term, and quality-of-life outcomes. In addition, NSQIP data are derived from a sample of voluntary institutions that pay an annual fee to participate. This cohort may be biased toward institutions that are more quality conscious and able to invest in quality improvement initiatives.
Conclusion
The overall complication rate in plastic surgery remains relatively low. However, in microsurgery, there are higher rates of SSIs and reoperations. The one independent predictive risk factor that spans both outcomes is increased operative time. This study better informs plastic surgeons of the risk factors for the most frequent complications and provides evidence-based data for better informed consent. No surgery is without risk; the authors encourage both surgeons and patients to decide what their tolerance for risk is. The authors recommend a continued judicious patient selection and continued research in order to provide quality and high-value care.
Footnotes
Level of Evidence: Level 4, Prognostic
Authors’ Note: Presented at 72nd Annual Meeting of the Canadian Society of Plastic Surgeons; June 19, 2018; Jasper, Canada.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr Marija Bucevska is a full-time employee of the University of British Columbia and receives salary for her position as a Clinical Research Coordinator.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Melissa Wan received a summer studentship grant from the BC Children’s Hospital Research Institute. Dr Yichuan Ding and Mr Yiwen Jin received funding support from by National Sciences and Engineering Research Council of Canada (NSERC) PGPIN 436156-13 13R81646, and 2019-05539.
References
- 1. Khan NA, Quan H, Bugar JM, Lemaire JB, Brant R, Ghali WA. Association of postoperative complications with hospital costs and length of stay in a tertiary care center. J Gen Intern Med. 2006;21(2):177–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fuller RL, McCullough EC, Bao MZ, Averill RF. Estimating the costs of potentially preventable hospital acquired complications. Health Care Financ Rev. 2009;30(4):17–32. [PMC free article] [PubMed] [Google Scholar]
- 3. Healy MA, Mullard AJ, Campbell DA, Jr, Dimick JB. Hospital and payer costs associated with surgical complications. JAMA Surg. 2016;151(9):823–830. [DOI] [PubMed] [Google Scholar]
- 4. ACS National Surgical Quality Improvement Program. About ACS NSQIP. https://www.facs.org/quality-programs/acs-nsqip/about. Accessed May 20, 2017.
- 5. ACS National Surgical Quality Improvement Program. ACS NSQIP Participant Use Data File. https://www.facs.org/quality-programs/acs-nsqip/participant-use. Accessed May 20, 2017.
- 6. Chung CU, Wink JD, Nelson JA, Fischer JP, Serletti JM, Kanchwala SK. Surgical site infections after free flap breast reconstruction: an analysis of 2,899 patients from the ACS-NSQIP datasets. J Reconstr Microsurg. 2015;31(6):434–441. [DOI] [PubMed] [Google Scholar]
- 7. Las DE, de Jong T, Zuidam JM, Verweij NM, Hovius SE, Mureau MA. Identification of independent risk factors for flap failure: a retrospective analysis of 1530 free flaps for breast, head and neck and extremity reconstruction. J Plast Reconstr Aesthet Surg. 2016;69(7):894–906. [DOI] [PubMed] [Google Scholar]
- 8. Lo SL, Yen YH, Lee PJ, Liu CC, Pu CM. Factors influencing postoperative complications in reconstructive microsurgery for head and neck cancer. J Oral Maxillofac Surg. 2017;75(4):867–873. [DOI] [PubMed] [Google Scholar]
- 9. Bekara F, Herlin C, Somda S, de Runz A, Grolleau JL, Chaput B. Free versus perforator-pedicled propeller flaps in lower extremity reconstruction: what is the safest coverage? A meta-analysis: Meta-analysis of free vs. propeller flaps in lower extremity reconstruction. Microsurgery. 2018;38(1):109–119. [DOI] [PubMed] [Google Scholar]
- 10. Heinz TR, Cowper PA, Levin LS. Microsurgery costs and outcome. Plast Reconstr Surg. 1999;104(1):89–96. [PubMed] [Google Scholar]
- 11. Jones NF, Jarrahy R, Song JI, Kaufman MR, Markowitz B. Postoperative medical complications not microsurgical complications-negatively influence the morbidity mortality and true costs after microsurgical reconstruction for head and neck cancer. Plast Reconstr Surg. 2007;119(7):2053–2060. [DOI] [PubMed] [Google Scholar]
- 12. Setälä L, Koskenvuori H, Gudaviciene D, Berg L, Mustonen P. Cost analysis of 109 microsurgical reconstructions and flap monitoring with microdialysis. J Reconstr Microsurg. 2009;25(9):521–526. [DOI] [PubMed] [Google Scholar]
- 13. Kwok AC, Agarwal JP. An analysis of free flap failure using the ACS NSQIP database. Does flap site and flap type matter? Microsurgery. 2017;37(6):531–538. [DOI] [PubMed] [Google Scholar]
- 14. Grover R, Padula WV, Van Vliet M, Ridgway EB. Comparing five alternative methods of breast reconstruction surgery: a cost-effectiveness analysis. Plast Reconstr Surg. 2013;132(5):709e–723e. [DOI] [PubMed] [Google Scholar]
- 15. Gao LL, Basta M, Kanchwala SK, Serletti JM, Low DW, Wu LC. Cost-effectiveness of microsurgical reconstruction for head and neck defects after oncologic resection: cost-effectiveness of microsurgical reconstruction. Head Neck. 2017;39(3):541–547. [DOI] [PubMed] [Google Scholar]
- 16. Hsing CY, Wong YK, Wang CP, et al. Comparison between free flap and pectoralis major pedicled flap for reconstruction in oral cavity cancer patients—a quality of life analysis. Oral Oncol. 2011;47(6):522–527. [DOI] [PubMed] [Google Scholar]
- 17. Karakida K, Aoki T, Ota Y, et al. Analysis of risk factors for surgical-site infections in 276 oral cancer surgeries with microvascular free-flap reconstructions at a single university hospital. J Infect Chemother. 2010;16(5):334–339. [DOI] [PubMed] [Google Scholar]
- 18. Kim B, Ver Halen J, Grant DW, Kim JY. Anesthesia duration as an independent risk factor for postoperative complications in free flap surgery: a review of 1,305 surgical cases. J Reconstr Microsurg. 2014;30(4):217–226. Epub 2013. [DOI] [PubMed] [Google Scholar]
- 19. Kamizono K, Sakuraba M, Nagamatsu S, Miyamot S, Hayash R. Statistical analysis of surgical site infection after head and neck reconstructive surgery. Ann Surg Oncol. 2014;21(5):1700–1705. [DOI] [PubMed] [Google Scholar]
- 20. Miller TJ, Jeong HS, Davis K, et al. Evaluation of the American society of anesthesiologists physical status classification system in risk assessment for plastic and reconstructive Surgery patients. Aesthet Surg J. 2014;34(3):448–456. [DOI] [PubMed] [Google Scholar]
- 21. Kim BD, Ver Halen JP, Lim S, Kim JY. Predictors of 61 unplanned readmission cases in microvascular free tissue transfer patients: multi-institutional analysis of 774 patients: unplanned readmission in free flap. Microsurgery. 2015;35(1):13–20. [DOI] [PubMed] [Google Scholar]
- 22. Garg RK, Wieland AM, Hartig GK, Poore SO. Risk factors for unplanned readmission following head and neck microvascular reconstruction: results from the National Surgical Quality Improvement Program, 2011-2014. Microsurgery. 2017;37(6):502–508. [DOI] [PubMed] [Google Scholar]
- 23. Anderson DJ, Kay KS. Staphylococcal surgical site infections. Infect Dis Clin North Am. 2009;23(1):53–72. [DOI] [PubMed] [Google Scholar]
- 24. Goltsman D, Munabi NCO, Ascherman JA. The association between smoking and plastic surgery outcomes in 40,465 patients: an analysis of the American College of Surgeons National Surgical Quality Improvement Program Data Sets. Plast Reconstr Surg. 2017;139(2):503–511. [DOI] [PubMed] [Google Scholar]
- 25. Toyoda Y, Fu RH, Li L, Otterburn DM, Rohde CH. Smoking as an independent risk factor for postoperative complications in plastic surgical procedures: a propensity score–matched analysis of 36454 patients from the NSQIP database from 2005 to 2014. Plast Reconstr Surg. 2018;141(1):226–236. [DOI] [PubMed] [Google Scholar]
- 26. Ismael H, Horst M, Farooq M, Jordon J, Patton JH, Rubinfeld IS. Adverse effects of preoperative steroid use on surgical outcomes. Am J Surg. 2011;201(3):305–308. [DOI] [PubMed] [Google Scholar]
- 27. Greenhalgh DG. Wound healing and diabetes mellitus. Clin Plast Surg. 2003;30(1):37–45. [DOI] [PubMed] [Google Scholar]
- 28. Jubbal KT, Chang D, Izaddoost SA, Pederson W, Zavlin D, Echo A. Resident involvement in microsurgery: an American College of Surgeons National Surgical Quality Improvement Program Analysis. J Surg Educ. 2017;74(6):1124–1132. [DOI] [PubMed] [Google Scholar]
- 29. Fischer JP, Nelson JA, Au A, Tuggle CT, III, Serletti JM, Wu LC. Complications and morbidity following breast reconstruction—a review of 16,063 cases from the 2005–2010 NSQIP datasets. J Plast Surg Hand Surg. 2014;48(2):104–114. [DOI] [PubMed] [Google Scholar]
- 30. Cheng H, Chen BP, Soleas IM, Ferko NC, Cameron CG, Hinoul P. Prolonged operative duration increases risk of surgical site infections: a systematic review. Surg Infect. 2017;18(6):722–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kimata Y, Matsumoto H, Sugiyama N, Onoda S, Sakuraba M. Lessons learned from unfavorable microsurgical head and neck reconstruction. Clin Plast Surg. 2016;43(4):729–737. [DOI] [PubMed] [Google Scholar]
- 32. Kroon HM, Breslau PJ, Lardenoye JW. Can the incidence of unplanned reoperations be used as an indicator of quality of care in surgery? Am J Med Qual. 2007;22(3):198–202. [DOI] [PubMed] [Google Scholar]
- 33. Birkmeyer JD, Hamby LS, Birkmeyer CM, Decker MV, Karon NM, Dow RW. Is unplanned return to the operating room a useful quality indicator in general surgery? Arch Surg. 2001;136(4):405–411. [DOI] [PubMed] [Google Scholar]
- 34. Morris AM, Baldwin LM, Matthews B, et al. Reoperation as a Quality Indicator in Colorectal Surgery: a population-based analysis. Ann Surg. 2007;245(1):73–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kwok AC, Agarwal JP. Unplanned reoperations after microvascular free tissue transfer: an analysis of 2,244 patients using the American College of Surgeons National Surgical Quality Improvement Program Database: reoperations after microvascular tissue transfer. Microsurgery. 2017;37(3):184–189. [DOI] [PubMed] [Google Scholar]
- 36. Fawcett A, Shembekar M, Church JS, Vashisht R, Springall RG, Nott DM. Smoking, hypertension, and colonic anastomotic healing; a combined clinical and histopathological study. Gut. 1996;38(5):714–718.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rambachan M, Mioton LM, Saha S, FineJohn N, Kim JYS. The impact of surgical duration on plastic surgery outcomes. Eur J Plast Surg. 2013;36(11):707–714. [Google Scholar]
- 38. Offodile AC, Aherrera A, Wenger J, Rajab TK, Guo L. Impact of increasing operative time on the incidence of early failure and complications following free tissue transfer? A risk factor analysis of 2,008 patients from the ACS-NSQIP database: Operative time and early flap failure. Microsurgery. 2017;37(1):12–20. [DOI] [PubMed] [Google Scholar]
- 39. Daley BJ, Cecil W, Clarke PC, Cofer JB, Guillamondegui OD. How slow is too slow? correlation of operative time to complications: an analysis from the Tennessee Surgical Quality Collaborative. J Am Coll Surg. 2015;220(4):550–558. [DOI] [PubMed] [Google Scholar]
- 40. Fogarty BJ, Khan K, Ashall G, Leonard AG. Complications of long operations: a prospective study of morbidity associated with prolonged operative time (>6 h). Br J Plast Surg. 1999;52(1):33–36. [DOI] [PubMed] [Google Scholar]
- 41. Haeck PC, Swanson JA, Iverson RE. Evidence-based patient safety advisory: patient selection and procedures in ambulatory surgery. Plast Reconstr Surg. 2009;124(suppl 4):6S–27S. [DOI] [PubMed] [Google Scholar]
- 42. Weiler J, Taggart P, Khoobehi K. A case for the safety and efficacy of lipoabdominoplasty: a single surgeon retrospective review of 173 consecutive cases. Aesthet Surg J. 2010;30(5):702–713. [DOI] [PubMed] [Google Scholar]
- 43. Stevens WG, Cohen R, Vath SD, Stoker DA, Hirsch EM. Does lipoplasty really add morbidity to abdominoplasty? Revisiting the controversy with a series of 406 cases. Aesthet Surg J. 2005;25(4):353–358. [DOI] [PubMed] [Google Scholar]
- 44. Swanson E. Prospective clinical study of 551 cases of liposuction and abdominoplasty performed individually and in combination. Plast Reconstr Surg Glob Open. 2013;1(5):e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Swansonands E. Prospective comparative clinical evaluation of 784 consecutive cases of breast augmentation and vertical mammaplasty performed individually and in combination. Plast Reconstr Surg. 2013;132(1):30e–45e. [DOI] [PubMed] [Google Scholar]
- 46. Stevens WG, Repta R, Pacella SJ, et al. Safe and consistent outcomes of successfully combining breast Surgery and abdominoplasty: an update. Aesthet Surg J. 2009;29(2):129–134. [DOI] [PubMed] [Google Scholar]
- 47. Heller JB, Teng E, Knoll B. I, Persing J. Outcome analysis of combined lipoabdominoplasty versus conventional abdominoplasty. Plast Reconstr Surg. 2008;121(5):1821–1829. [DOI] [PubMed] [Google Scholar]
- 48. Zhu VZ, Tuggle CT, Au AF. Promise and limitations of big data research in plastic surgery. Ann Plast Surg. 2016;76(4):453–458. [DOI] [PubMed] [Google Scholar]