Short abstract
Mindfulness-based art therapy (MBAT) combines mindfulness practices with art therapy to promote health, wellness, and adaptive responses to stress. Mindfulness-based stress reduction programs have been demonstrated to reduce anxiety symptoms in people with generalized anxiety disorder and serious medical conditions such as cancer. However, the benefits of MBAT specifically—not just in clinical anxiety disorders, but also for routine day-to-day anxiousness—have received little attention until recently. In this mini-review, we summarize how several established mindfulness-based interventions affect mental health with a specific focus on MBAT. We also describe and evaluate data indicating involvement of specific neural circuits and neuroendocrine markers of stress and/or anxiety. Lastly, we suggest areas of focus for future rigorous research on MBAT interventions and propose multiple biobehavioral and physiological mechanisms through which therapeutic benefits may be achieved.
Impact statement
Recent studies demonstrate the therapeutic potential of intensive MBAT and other mindfulness-based interventions for severe health conditions including cancer, heart disease, and anxiety, with effectiveness that rivals and sometimes even exceeds cognitive behavior therapy. MBAT-based approaches appear to be poised to mature into large-scale, cost-effective therapies for mental health disorders and symptoms comorbid with other serious health issues. However, the field currently suffers from inconsistent deployment protocols and needs additional validation data—at the behavioral, neuroendocrine, and neural levels—in order to establish best practices.
Keywords: Biomarkers, brain, mindfulness, neuroendocrinology, neuroscience, stress
Anxiety and stress
Anxiety disorders constitute the largest group of mental disorders in most parts of the world and are a leading cause of disability. In the United States, anxiety disorders and mood disorders are the most common mental health disorders with 12-month prevalence rates of approximately 18.1% and 9.5%, respectively.1 Of note, although anxiety disorders and major depression are often comorbid with one another and can present with common symptoms, these disorders are distinct clinically and involve dysfunctions in distinct brain circuits and molecules. Nevertheless, both anxiety disorders and mood disorders are related to poor physical health outcomes,2–4 in addition to diminished quality of life, impairments in daily functioning, and lost occupational/academic productivity.5–7 Specifically, both anxiety disorders and mood disorders are associated with cardiovascular disease, metabolic disorders, cancer, sleep disorders, and decreased longevity. Links between poor physical health and anxiety or mood disorders are distinct, reciprocal, and complicated, but it is also appreciated that there are shared neural and endocrine mechanisms. Interestingly, research suggests that the etiological pathways are similar between poor physical health outcomes and chronic daily stress, a common risk factor in the onset of both anxiety disorders and mood disorders.8,9
Beyond clinically diagnosed anxiety disorders, approximately 7 out of 10 adults in the United States report moderately impairing levels of stress or anxiety on a daily basis.10 Poorly managed anxiety and/or stress can contribute to economic and global burdens, including student loan debt,11 work productivity loss,12 and healthcare costs.13 In terms of years lived in less than ideal health, anxiety disorders are the sixth leading cause of disability throughout the world14 and account for 390 disability-adjusted life years per 100,000 individuals. Chronic daily stress and anxiety increase the risk of physical pathology like sleep quality, weight gain, decreased cognitive functioning, cardiovascular disease, autoimmune diseases, and gastrointestinal problems.9,15,16 Similar to anxiety and mood disorders, the association between chronic daily stress and anxiety and poor physical health are due to the effects that chronic daily stress and anxiety have on biological systems essential for optimal health. Stress induces neuro-immune and neuro-endocrine responses, and individual differences in these effects contribute to vulnerability and resilience.17 At a mechanistic level, stress can even transform signals in the brain that are typically related to reward into punishment signals and thus bias individuals towards negative expectations, anxiety symptoms, and depression-related behaviors.18
Chronic stress and anxiety disorders have both been previously associated with dysregulation of stress hormones, neuro-inflammatory markers, and neural circuit activation.15,19–25 These maladaptations are in turn correlated with negative health consequences including metabolic syndrome,26,27 cardiovascular disease risk,9,16,28 and chronic pain.29–32 Circulating cytokines, including tumor necrosis factor alpha (TNF-α) and interleukin-6 (IL-6), help inter-connect signals between the central nervous system and peripheral immune system.33 Moreover, they can amplify the production of other secreted molecules and intensify immune responses. Cytokines play a variety of roles within the nervous system, including the initiation of immune processes, the promotion of repair after cell injury, and regulation of endocrine signals and feedback.17,34 Several studies support altered cytokines and other inflammatory markers in anxiety disorders.19–22
Approaches to mindfulness and established effects of mindfulness interventions on mental health and neural systems
Mindfulness refers to the psychological process of attending to experiences happening in the present moment; it is originally derived from ancient Eastern roots, especially Buddhist traditions and yogic practices. It focuses on progressively orienting a person to an awareness of connections and interaction between body and mind. Recently, such practices have been adopted and adapted by Western cultures for wellness management and clinical interventions. Research demonstrates a strong relationship between mindfulness practices and quality mental health. The most common method of mindfulness-based intervention for reducing stress is mindfulness-based stress reduction (MBSR).35,36 A standard MBSR curriculum is eight weeks long and structured in a group therapy format, with each session typically lasting between 1 and 2 h in length. Mindfulness-based interventions exert positive impacts on an individual’s mental health in addition to physical health.37–44 Effectiveness has been established not only for clinically diagnosed anxiety disorders but also for subclinical levels of anxiety and stress. Two meta-analyses have established that mindfulness-based interventions are at least as efficacious as cognitive behavioral therapy (CBT).38,45 Possible biological mediators of positive effects include improved sleep quality,23,46 brain structure changes,47 and enhanced cortisol regulation.23,48 A mindfulness intervention also reduced stress and improved mental well-being in caregivers for family members with dementia,49 suggesting that a wide array of stress-related burdens might be responsive to these therapies. However, studies in this area are not always well controlled, and randomized control trials of behavioral therapies are more difficult to design and interpret than are pharmaceutical interventions.50 For example, effectiveness in a behavioral intervention is dependent on not only characteristics of the intervention provider but also factors relating to the recipient and how they engage with the intervention. A therapist providing a behavioral intervention is equipped with a unique combination of training and clinical experience, meaning subtle variations may exist between therapists and how they adhere to and facilitate a behavioral intervention protocol. Consequently, this will have an impact on how a recipient responds to the intervention. Moreover, regardless of the background, skill, and decisions of the provider, a recipient independently decides their level of engagement with the intervention, while their cultural background and personal experience can impact how they interpret and respond to it. This differs greatly from a medication trial where dosage and provision of services can be strictly controlled.
Hoge et al.51 recently defined changes in blood levels of cortisol, ACTH, IL-6, and TNF-α following mindfulness meditation in adults with generalized anxiety disorder (GAD). The most sensitive indicators appeared to be ACTH and IL-6, after use of the Trier Social Stress Test to induce an acute stress response. This study provided direct evidence that biological substrates of stress responses may be altered in response to a mindfulness-based therapy intervention. MBSR attenuated stress hormone and inflammatory marker responses to stress in patients with GAD. An additional study from the same group suggested that mindfulness-induced improvements in anxiety may be mediated primarily through a practice called decentering.52 Decentering is an ability to recognize that thoughts, feelings, and urges are transient internal events and not inherent, permanent aspects of the self or accurate depictions of reality. Investigation of underlying neural mechanisms of an MBSR-intervention in patients with GAD using functional magnetic resonance imaging (fMRI)53 revealed that at baseline, GAD patients exhibited enhanced amygdala activation than did controls in response to neutral faces; thus, ambiguous stimuli produced stronger reactions in patients with the anxiety disorder. In GAD patients, amygdala activation to neutral faces decreased following MBSR and activation in the prefrontal cortex increased. Changes in amygdala-to-prefrontal functional connectivity were correlated with changes in self-reported anxiety, and interestingly, amygdala-to-prefrontal connectivity changed from negative coupling (typically seen as part of emotional down-regulation), to positive coupling. These data suggest a potential neuronal mechanism by which mindfulness can regulate brain circuit activation and processing.
A more specific approach is termed mindfulness-based cognitive therapy (MBCT).54,55 MBCT follows the same eight-week group therapy structure as MBSR and is made up of similar content. It employs the tenets of mindfulness and CBT to address specific symptoms and patterns of negative thinking associated with major depressive disorder (MDD).56 In systematic reviews of MBCT for MDD and associated depressive outcomes,57 and MBSR compared to MBCT,58 there is strong evidence that ameliorations in emotional reactivity and cognitive augmentation contribute to the underlying mechanisms of these mindfulness-based interventions. There are also indications that they may have predicting or mediating roles in things like rumination, worry, mindfulness, compassion, and meta-awareness. However, as with most research of psychological interventions, there are some inconsistencies in the theoretical frameworks between researchers, and strong conclusions regarding the mechanisms at play are still elusive.
Yet another variant of a mindfulness intervention is termed integrative body-mind training (IBMT), and this approach focuses on integrative central and autonomic nervous system training through body relaxation, mental imagery, mindfulness training, and music. Studies suggest that IBMT can improve emotion regulation,59,60 improve cognitive control,59,60 reduce salivary cortisol,61 and alter brain structure and function.59,62–64 In one particularly interesting study, investigators found improved emotion regulation, self-control, and stress reduction after IBMT training; these improvements correlated with augmented activity in the prefrontal and anterior cingulate cortices following training.59 People who smoke exhibited diminished prefrontal cortical activity in the network ahead of training (as compared to nonsmoking participants), and training ameliorated these deficits, demonstrating that this approach may be useful in the treatment and prevention of drug addiction.
MBAT
Art therapy is a mental health service that integrates creative processes with traditional talk therapy.65 It has been used in a variety of settings, with individual, family, and group therapies, to address multiple mental health challenges.66,67 One of the advantages of art therapy is that it provides a mode of communication that can be less intimidating than traditional verbal communication. Additionally, the creative process and art materials may contain intrinsic therapeutic properties that may be a valuable asset to mental health services. As with the mindfulness interventions described above, with brain imaging technologies and unobtrusive tests of biological markers, there are emerging data that support art playing an active and effective role in stress management and addressing symptoms of anxiety.
For example, Kaimal et al.68 gave 39 healthy individuals the choice of collage materials, modeling clay, and/or markers for a brief art-making session. Most participants had a small but significant decrease in salivary cortisol levels after art making. Although the extent of the changes were widely varied between individuals—the source of this likely complex heterogeneity in responses was unclear, despite the authors fairly detailed analysis of prior experience with art, art materials used, gender, ethnicity, and age. In a more recent study, the same research group69 looked at blood flow in the medial prefrontal cortex. Participants were asked to complete three visual self-expression tasks including coloring a pre-drawn mandala, personalized doodling, and free drawing on a blank sheet of paper. Data on cerebral blood flow in the brain were collected for each task, in addition to resting periods in between. All of the tasks produced activation of prefrontal cortical regions, with no statistically significant difference among tasks. They also included a self-report measure regarding self-perception of creativity, which increased for all participants at the end of the session. Building healthy habits typically requires practice and positive reinforcement. The activation of this pathway during art making suggests that practicing art making can have lasting benefits in healthy habit building that combats stress.
Another intriguing study compared clay work to drawing.70 Electroencephalograms were used to monitor brain activity patterns in healthy female participants engaged in the two different art tasks; the study found that both drawing and clay sculpting increased gamma power, which is associated with information-rich task processing, but only clay sculpting resulted in increased theta power. Theta waves are associated with deep meditative states, imagination, and internal focus.71 These findings suggest that clay carries intrinsic therapeutic properties that may complement mindfulness, as the act of clay sculpting alone appears to be able to induce relaxation and even a meditative state. We note, however, that the study of Kaimal did not observe any effects of art media choice on cortisol levels.68
Art therapy and mindfulness practices have complementary effects on neurological and biological processes as well as mental health. MBSR protocols are integrated with art therapy prompts and art making in order to perform MBAT; in other words, MBAT typically combines the MBSR protocol with complementary art therapy directives.72 MBAT has been examined using randomized controlled trials, typically for severe illness management like cancer73–78 and coronary artery disease.79 Monti et al.73 used fMRI and successfully correlated brain activation responses to stress and anxiety measures with engagement in their MBAT regimen. MBAT-receiving participants showed increases in blood flow in several limbic brain regions, including the insular cortex, amygdala, hippocampus, and the striatum. These changes occurred both at rest and during meditation. Moreover, reactions to a stressor involved decreased activation of the cingulate cortex in MBAT-receiving participants, demonstrating regulation of a specific neural circuit—one that is already known to be involved in stress responses and anxiety regulation25,80—by MBAT.
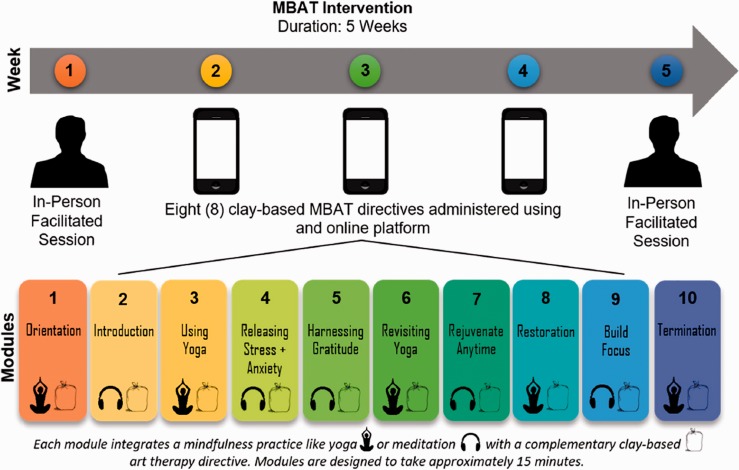
Our group recently demonstrated significant decreases in anxiety symptoms and salivary cortisol in anxious but healthy college students receiving MBAT.81 The most typical MBAT protocol consists of 2-h sessions weekly for eight weeks72—this is more time- and cost-intensive than even CBT. Validation of more abbreviated and efficient MBAT approaches is crucial in determining whether this therapeutic approach can be effective in large-scale deployments. Thus, rather than following the standardized eight-week protocol, ours utilizes one initial in-person facilitated session, eight 15-min easily reproducible, clay-based MBAT directives, administered through an online platform, and then one final in person session (Figure 1). Although our initial proof-of-concept study was small, a follow-up study of 77 participants demonstrated positive effects on both anxiety and perceived stress (Beerse, Van Lith and Stanwood, unpublished data). Therefore, it appears that MBAT has the capacity to improve mind and body outcomes by concurrently activating and reorganizing behavioral, neurobiological, and neuroendocrine processes while supporting the healthy development of social and emotional processes. The fundamental science underlying MBAT—and a mechanistic understanding of its endocrine and neural mechanisms—will potentially lead to a novel biobehavioral approach to help reduce the burden of anxiety symptoms, anxiety disorders, and protect against chronic daily stress. Our utilization of a web-based application offers a feasible strategy for increasing access to mental health services while circumnavigating the issue of stigma that still surrounds mental health. This may be especially true for those who are wary of traditional services and for those who feel their symptoms are distressing but not yet dysfunctional. Mental health apps are increasing in popularity, but few have been rigorously studied,82–84 and most rely on self-report measures,85 failing to investigate the biobehavioral implications. Ours appears to represent the first project adapting a systemized MBAT intervention to an electronic delivery system that can be up-scaled quickly and efficiently.
Figure 1.
Structure of MBAT intervention designed to maximize user accessibility and implemented by our group. (A color version of this figure is available in the online journal.)
MBAT: mindfulness-based art therapy.
Future directions
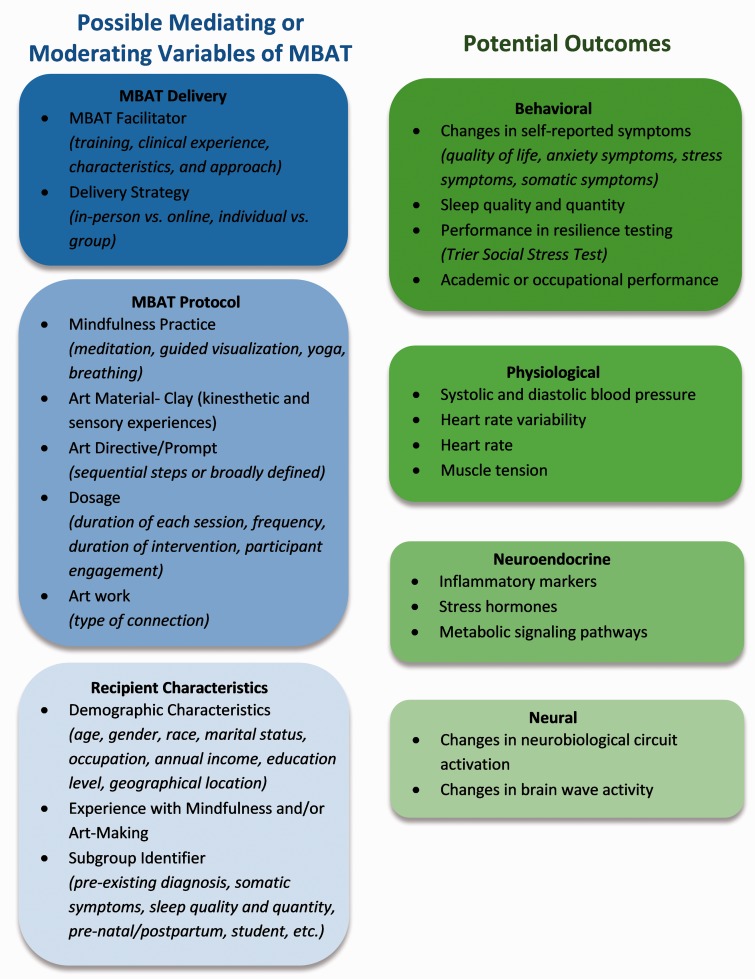
The neural basis of the nature and benefits of mindfulness, and especially MBAT specifically, is still in its early days. Nonetheless, a good deal of data have been already generated, and published work in this area is growing very rapidly. It is important to assess what has been learned to date and to further improve experimental designs and approaches. There is a need for more rigorous and transparent studies, delineation of subpopulations of individuals showing differing responsiveness to the interventions, and a more complete understanding of the host of neuroendocrine, behavioral, and neural changes that mediate therapeutic success. These behavioral approaches have great promise in the treatment of complex mental health conditions, but additional science is needed to discern how to best deploy them. As described in a recent meta-analysis,44 there is a lack of consistency across studies in type of mindfulness intervention and control conditions used in studies. Furthermore, few studies include subgroup analyses and the field needs to do better. With regard to MBAT specifically, to our knowledge, only one study has examined changes in neural activation patterns,73 and that was in only 18 patients with brain cancer (of course, many others—some cited above in this article—have used functional neuroimaging to better understand meditation and mindfulness themselves). Comprehensive identification of the neuroprotective circuits recruited by MBAT interventions and resultant modifications of stress hormone and metabolic signaling pathways are sorely needed. In Figure 2, we present a potential conceptual framework that may be of utility in this effort.
Figure 2.
Proposed methodologies, experimental design considerations, and analyses to improve our understanding of the therapeutic benefits of MBAT and biobehavioral mechanisms through which these benefits are achieved. (A color version of this figure is available in the online journal.)
MBAT: mindfulness-based art therapy.
Cognitive and emotion regulation mechanisms in the brain are often discussed as being based in “top-down” or “bottom-up” in nature. Quite simply, top down processing refers to processing based on what is already in the mind or highest levels of the brain. In contrast, bottom up processing refers to processing based on what is in the stimulus array reaching sensory organs. Some authors have suggested that mindfulness is a top-down strategy to regulate emotion, while other groups propose that mindfulness is, instead, bottom-up.86–89 Discrepancies are produced in part from the distinct definitions, descriptions, and uses of mindfulness. One suggestion is that mindfulness training produces top-down emotional regulation in the beginning, but with practice and time, recruits bottom-up neural mechanisms in longer-term, expert practitioners/users.86 However, this has yet to be fully tested or established. The particularly effectiveness of MBAT might also be based on a more unified joint processing from both directions, given the direct engagement of art materials and art-making with one’s sensory organs. Directed study of these possibilities is warranted.
The reciprocal relationship between anxiety, stress, and sleep disruption should be addressed in future treatment research designs of MBAT. It is commonly known that anxiety and stress, characterized by cognitive difficulty and emotional reactivity, are also associated with sleep disruption and the development of insomnia.90–97 Several etiological models have highlighted shared mechanisms between anxiety, stress, and sleep disruption that may explain the reciprocal risk and high comorbidity.91,98–100 Specifically, cognitive and emotional arousal, sleep-stress reactivity, and emotion regulation mechanisms, including mindfulness, may all play an important role.101–106 Mindfulness-based treatments, as discussed previously, are effective for the reduction of stress and anxiety symptoms and, interestingly, are effective for improvements in sleep disruption and insomnia.107–109 However, improvements in sleep disruption as a result of MBAT have not been examined. Therefore, the assessment of sleep characteristics in MBAT treatment research designs for anxiety and stress would add to the growing evidence concluding that mindfulness-based treatments are effective for promoting healthy sleep, and potentially confirm that targeting shared mechanisms in treatment can improve anxiety, stress, and sleep difficulties simultaneously (Figure 2).
Even though the American Psychiatric Association reorganized the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM) away from a multi-axial system, there has since been an appeal for a symptom-based approach to mental health research rather than based on diagnosis.110 A symptom-based approach acknowledges that most mental disorder diagnoses are not rooted in neurobiological evidence, but rather supported by neurobiological research ex post facto. In this approach, research cohorts are organized by their predominant symptoms and complaints. With MBAT research still in its infancy, there is an opportunity to collect data in a symptom-based approach that withstands the evolution of diagnostic criteria relating to anxiety disorders as well as mood disorders. Instead, researchers can determine how MBAT interventions interact with a variety of somatic symptoms that are often associated with anxiety and stress, such as migraines, gastrointestinal problems, muscle pain or spasms, fatigue, and sleep disruptions. Additionally, research cohorts could be organized by group characteristics. For instance, a recent review has summarized emerging literature suggesting that mindfulness-based programs can decrease psychological stress during pregnancy and improve maternal mental health.111 Similarly, cohorts could be organized by other characteristics like unique cultural groups or individuals within a set geographical location which could all provide insight into the more nuanced variables that interact with mental health research.
While variables on the receiving end can be strategically organized, so, too, can the intervention strategy be manipulated to better understand the mechanisms at play. The MBAT protocol and delivery strategy could be altered to determine whether a face-to-face intervention would elicit stronger positive outcomes than an electronically delivered intervention. Recipients of MBAT could also be divided into individual or group therapy structures, since MBSR emphasizes the importance of using a group therapy format. Lastly, MBAT is fundamentally unique in the realm of mental health approaches due to the valuable role art materials and the creative process hold. Even subtle manipulations in art-making instruction and material can further breakdown the mechanisms underlying this intervention.
ACKNOWLEDGMENTS
We thank Florida State University for funding our time to write this manuscript.
Authors’ contributions
All authors participated in the writing and review of the article.
DECLARATION OF CONFLICTING INTERESTS
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
FUNDING
This project received financial support from the Florida State University Council on Research and Creativity.
References
- 1.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry 2005; 62:617–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ressler KJ, Mayberg HS. Targeting abnormal neural circuits in mood and anxiety disorders: from the laboratory to the clinic. Nat Neurosci 2007; 10:1116–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mendlowicz MV, Stein MB. Quality of life in individuals with anxiety disorders. Am J Psychiatry 2000; 157:669–82 [DOI] [PubMed] [Google Scholar]
- 4.Bokma WA, Batelaan NM, van Balkom AJ, Penninx BW. Impact of anxiety and/or depressive disorders and chronic somatic diseases on disability and work impairment. J Psychosom Res 2017; 94:10–6 [DOI] [PubMed] [Google Scholar]
- 5.DuPont RL, Rice DP, Miller LS, Shiraki SS, Rowland CR, Harwood HJ. Economic costs of anxiety disorders. Anxiety 1996; 2:167–72 [DOI] [PubMed] [Google Scholar]
- 6.Olatunji BO, Cisler JM, Tolin DF. Quality of life in the anxiety disorders: a meta-analytic review. Clin Psychol Rev 2007; 27:572–81 [DOI] [PubMed] [Google Scholar]
- 7.Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen HU. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res 2012; 21:169–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sareen J, Cox BJ, Afifi TO, de Graaf R, Asmundson GJ, ten Have M, Stein MB. Anxiety disorders and risk for suicidal ideation and suicide attempts: a population-based longitudinal study of adults. Arch Gen Psychiatry 2005; 62:1249–57 [DOI] [PubMed] [Google Scholar]
- 9.Schneiderman N, Ironson G, Siegel SD. Stress and health: psychological, behavioral, and biological determinants. Annu Rev Clin Psychol 2005; 1:607–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.America AaDAo. Highlights: workplace stress & anxiety disorders survey, https://adaa.org/workplace-stress-anxiety-disorders-survey (2006, accessed 11 October 2019)
- 11.Goldy-Brown S. Student loan debt statistics, https://www.studentdebtrelief.us/student-loans/studentdebt-statistics/ (2019, accessed 11 October 2019)
- 12.World Health Organization. Mental health in the workplace World Health Organization, www.who.int/mental_health/in_the_workplace/en/ (2017, accessed 6 October 2017)
- 13.Marciniak MD, Lage MJ, Dunayevich E, Russell JM, Bowman L, Landbloom RP, Levine LR. The cost of treating anxiety: the medical and demographic correlates that impact total medical costs. Depress Anxiety 2005; 21:178–84 [DOI] [PubMed] [Google Scholar]
- 14.Baxter A, Vos T, Scott K, Ferrari A, Whiteford H. The global burden of anxiety disorders in 2010. Psychol Med 2014; 44:2363–74 [DOI] [PubMed] [Google Scholar]
- 15.McEwen BS. Neurobiological and systemic effects of chronic stress. Chronic Stress 2017; 1:2470547017692328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sterling P, & Eyer J. Allostasis: A new paradigm to explain arousal pathology. In S. Fisher & J. Reason (Eds.), Handbook of life stress, cognition and health (pp. 629–649). Oxford, England: John Wiley & Sons, 2019
- 17.Menard C, Pfau ML, Hodes GE, Russo SJ. Immune and neuroendocrine mechanisms of stress vulnerability and resilience. Neuropsychopharmacology 2017; 42:62–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shabel SJ, Wang C, Monk B, Aronson S, Malinow R. Stress transforms lateral habenula reward responses into punishment signals. Proc Natl Acad Sci USA 2019;116(25):12488–12493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Copeland WE, Shanahan L, Worthman C, Angold A, Costello EJ. Generalized anxiety and C-reactive protein levels: a prospective, longitudinal analysis. Psychol Med 2012; 42:2641–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liukkonen T, Räsänen P, Jokelainen J, Leinonen M, Järvelin M-R, Meyer-Rochow V, Timonen M. The association between anxiety and C-reactive protein (CRP) levels: results from the Northern Finland 1966 birth cohort study. European Psychiatry 2011; 26:363–9 [DOI] [PubMed] [Google Scholar]
- 21.Lengacher CA, Kip KE, Barta M, Post-White J, Jacobsen PB, Groer M, Lehman B, Moscoso MS, Kadel R, Le N. A pilot study evaluating the effect of mindfulness-based stress reduction on psychological status, physical status, salivary cortisol, and interleukin-6 among advanced-stage cancer patients and their caregivers. J Holist Nurs 2012; 30:170–85 [DOI] [PubMed] [Google Scholar]
- 22.O’Donovan A, Hughes BM, Slavich GM, Lynch L, Cronin M-T, O’Farrelly C, Malone KM. Clinical anxiety, cortisol and interleukin-6: evidence for specificity in emotion–biology relationships. Brain, Behav Immun 2010; 24:1074–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brand S, Holsboer-Trachsler E, Naranjo JR, Schmidt S. Influence of mindfulness practice on cortisol and sleep in long-term and short-term meditators. Neuropsychobiology 2012; 65:109–18 [DOI] [PubMed] [Google Scholar]
- 24.Sandi C, Haller J. Stress and the social brain: behavioural effects and neurobiological mechanisms. Nat Rev Neurosci 2015; 16:290. [DOI] [PubMed] [Google Scholar]
- 25.Stanwood GD. Dopamine and stress In: Fink G. (ed.) Stress: physiology, biochemistry and pathology. London: Academic Press, 2019, pp.105–13 [Google Scholar]
- 26.Rebolledo-Solleiro D, Roldán-Roldán G, Díaz D, Velasco M, Larqué C, Rico-Rosillo G, Vega-Robledo GB, Zambrano E, Hiriart M, de la Mora MP. Increased anxiety-like behavior is associated with the metabolic syndrome in non-stressed rats. PloS One 2017; 12:e0176554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Révész D, Verhoeven JE, Milaneschi Y, Penninx BW. Depressive and anxiety disorders and short leukocyte telomere length: mediating effects of metabolic stress and lifestyle factors. Psychol Med 2016; 46:2337–49 [DOI] [PubMed] [Google Scholar]
- 28.McEwen BS. Protective and damaging effects of stress mediators: central role of the brain. Dialog Clin Neurosci 2006; 8:367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Blackburn‐Munro G, Blackburn‐Munro RE. Chronic pain, chronic stress and depression: coincidence or consequence? J Neuroendocrinol 2001; 13:1009–23 [DOI] [PubMed] [Google Scholar]
- 30.Asmundson GJ, Katz J. Understanding the co‐occurrence of anxiety disorders and chronic pain: state‐of‐the‐art. Depress Anxiety 2009; 26:888–901 [DOI] [PubMed] [Google Scholar]
- 31.Ullrich PM, Turner JA, Ciol M, Berger R. Stress is associated with subsequent pain and disability among men with nonbacterial prostatitis/pelvic pain. Ann Behav Med 2005; 30:112–8 [DOI] [PubMed] [Google Scholar]
- 32.Culpepper L. Generalized anxiety disorder and medical illness. J Clin Psychiatry 2009; 70:20–4 [DOI] [PubMed] [Google Scholar]
- 33.Vezzani A, Viviani B. Neuromodulatory properties of inflammatory cytokines and their impact on neuronal excitability. Neuropharmacology 2015; 96:70–82 [DOI] [PubMed] [Google Scholar]
- 34.Gadek-Michalska A, Tadeusz J, Rachwalska P, Bugajski J. Cytokines, prostaglandins and nitric oxide in the regulation of stress-response systems. Pharmacol Rep: PR 2013; 65:1655–62 [DOI] [PubMed] [Google Scholar]
- 35.Kabat‐Zinn J. Mindfulness‐based interventions in context: past, present, and future. Clin Psychol: Sci Pract 2003; 10:144–56 [Google Scholar]
- 36.Kabat-Zinn J, Massion AO, Kristeller J, Peterson LG, Fletcher KE, Pbert L, Lenderking WR, Santorelli SF. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry 1992; 149:936–43 [DOI] [PubMed] [Google Scholar]
- 37.Henderson VP, Massion AO, Clemow L, Hurley TG, Druker S, Hébert JR. A randomized controlled trial of mindfulness-based stress reduction for women with early-stage breast cancer receiving radiotherapy. Integr Cancer Ther 2013; 12:404–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J Consult Clin Psychol 2010; 78:169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Prazak M, Critelli J, Martin L, Miranda V, Purdum M, Powers C. Mindfulness and its role in physical and psychological health. Appl Psychol: Health Well‐Being 2012; 4:91–105 [DOI] [PubMed] [Google Scholar]
- 40.Ratanasiripong P, Park JF, Ratanasiripong N, Kathalae D. Stress and anxiety management in nursing students: biofeedback and mindfulness meditation. J Nurs Educ 2015; 54:520–4 [DOI] [PubMed] [Google Scholar]
- 41.Schure MB, Christopher J, Christopher S. Mind–body medicine and the art of self‐care: teaching mindfulness to counseling students through yoga, meditation, and qigong. J Counsel Dev 2008; 86:47–56 [Google Scholar]
- 42.Sundquist J, Lilja Å, Palmér K, Memon AA, Wang X, Johansson LM, Sundquist K. Mindfulness group therapy in primary care patients with depression, anxiety and stress and adjustment disorders: randomised controlled trial. Br J Psychiatry 2015; 206:128–35 [DOI] [PubMed] [Google Scholar]
- 43.Chiesa A, Serretti A. A systematic review of neurobiological and clinical features of mindfulness meditations. Psychol Med 2010; 40:1239–52 [DOI] [PubMed] [Google Scholar]
- 44.Zhang MF, Wen YS, Liu WY, Peng LF, Wu XD, Liu QW. Effectiveness of mindfulness-based therapy for reducing anxiety and depression in patients with cancer: a meta-analysis. Medicine 2015; 94:e0897–0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Huang J, Nigatu YT, Smail-Crevier R, Zhang X, Wang J. Interventions for common mental health problems among university and college students: a systematic review and meta-analysis of randomized controlled trials. J Psychiatr Res 2018; 107:1–10 [DOI] [PubMed] [Google Scholar]
- 46.Black DS, O'Reilly GA, Olmstead R, Breen EC, Irwin MR. Mindfulness meditation and improvement in sleep quality and daytime impairment among older adults with sleep disturbances: a randomized clinical trial. JAMA Intern Med 2015; 175:494–501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kurth F, Luders E, Wu B, Black DS. Brain gray matter changes associated with mindfulness meditation in older adults: an exploratory pilot study using voxel-based morphometry. Neuro Open J 2014; 1:23–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pawlow LA, Jones GE. The impact of abbreviated progressive muscle relaxation on salivary cortisol and salivary immunoglobulin A (sIgA). Appl Psychophysiol Biofeedback 2005; 30:375–87 [DOI] [PubMed] [Google Scholar]
- 49.Whitebird RR, Kreitzer M, Crain AL, Lewis BA, Hanson LR, Enstad CJ. Mindfulness-based stress reduction for family caregivers: a randomized controlled trial. Gerontologist 2013; 53:676–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rosenkranz MA, Dunne JD, Davidson RJ. The next generation of mindfulness-based intervention research: what have we learned and where are we headed? Curr Opin Psychol 2019; 28:179–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hoge EA, Bui E, Palitz SA, Schwarz NR, Owens ME, Johnston JM, Pollack MH, Simon NM. The effect of mindfulness meditation training on biological acute stress responses in generalized anxiety disorder. Psychiatry Res 2018; 262:328–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hoge EA, Bui E, Goetter E, Robinaugh DJ, Ojserkis RA, Fresco DM, Simon NM. Change in decentering mediates improvement in anxiety in mindfulness-Based stress reduction for generalized anxiety disorder. Cogn Ther Res 2015; 39:228–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Holzel BK, Hoge EA, Greve DN, Gard T, Creswell JD, Brown KW, Barrett LF, Schwartz C, Vaitl D, Lazar SW. Neural mechanisms of symptom improvements in generalized anxiety disorder following mindfulness training. NeuroImage Clin 2013; 2:448–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Coelho HF, Canter PH, Ernst E. Mindfulness-based cognitive therapy: evaluating current evidence and informing future research. J Consult Clin Psychol 2007; 75:1000–5 [DOI] [PubMed] [Google Scholar]
- 55.Teasdale JD, Segal Z, Williams JM. How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness) training help? Behav Res Ther 1995; 33:25–39 [DOI] [PubMed] [Google Scholar]
- 56.School UoMMMBCT & MBSR: The differences. The Center for Mindfulness, www.umassmed.edu/cfm/mindfulness-based-programs/mbct-courses/about-mbct/mbct-mbsr-differences/ (2017, accessed 11 October 2019)
- 57.van der Velden AM, Kuyken W, Wattar U, Crane C, Pallesen KJ, Dahlgaard J, Fjorback LO, Piet J. A systematic review of mechanisms of change in mindfulness-based cognitive therapy in the treatment of recurrent major depressive disorder. Clin Psychol Rev 2015; 37:26–39 [DOI] [PubMed] [Google Scholar]
- 58.Gu J, Strauss C, Bond R, Cavanagh K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin Psychol Rev 2015; 37:1–12 [DOI] [PubMed] [Google Scholar]
- 59.Tang YY, Tang R, Posner MI. Mindfulness meditation improves emotion regulation and reduces drug abuse. Drug and alcohol dependence. Suppl 2016; 163:1:S13–8 [DOI] [PubMed] [Google Scholar]
- 60.Tang YY, Yang L, Leve LD, Harold GT. Improving executive function and its neurobiological mechanisms through a mindfulness-based intervention: advances within the field of developmental neuroscience. Child Dev Perspect 2012; 6:361–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fan Y, Tang YY, Posner MI. Cortisol level modulated by integrative meditation in a dose-dependent fashion. Stress Health 2014; 30:65–70 [DOI] [PubMed] [Google Scholar]
- 62.Tang YY, Lu Q, Fan M, Yang Y, Posner MI. Mechanisms of white matter changes induced by meditation. Proc Natl Acad Sci USA 2012; 109:10570–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tang YY, Tang Y, Tang R, Lewis-Peacock JA. Brief mental training reorganizes large-scale brain networks. Front Syst Neurosci 2017; 11:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Xue SW, Tang YY, Tang R, Posner MI. Short-term meditation induces changes in brain resting EEG theta networks. Brain Cogn 2014; 87:1–6 [DOI] [PubMed] [Google Scholar]
- 65.Association AAT. About art therapy. Alexandria, VA: American Art Therapy Association, https://arttherapy.org/about-art-therapy/ (2017, accessed 11 October 2019) [Google Scholar]
- 66.Slayton SC, D'Archer J, Kaplan F. Outcome studies on the efficacy of art therapy: a review of findings. Art Therapy 2010; 27:108–18 [Google Scholar]
- 67.Reynolds MW, Nabors L, Quinlan A. The effectiveness of art therapy: does it work? Art Therapy 2000; 17:207–13 [Google Scholar]
- 68.Kaimal G, Ray K, Muniz J. Reduction of cortisol levels and participants' responses following art making. Art Therapy 2016; 33:74–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kaimal G, Ayaz H, Herres J, Dieterich-Hartwell R, Makwana B, Kaiser DH, Nasser JA. Functional near-infrared spectroscopy assessment of reward perception based on visual self-expression: coloring, doodling, and free drawing. Arts Psychother 2017; 55:85–92 [Google Scholar]
- 70.Kruk KA, Aravich PF, Deaver SP, deBeus R. Comparison of brain activity during drawing and clay sculpting: a preliminary qEEG study. Art Therapy 2014; 31:52–60 [Google Scholar]
- 71.Tang YY, Tang R, Rothbart MK, Posner MI. Frontal theta activity and white matter plasticity following mindfulness meditation. Curr Opin Psychol 2019;28:294–297 [DOI] [PMC free article] [PubMed]
- 72.Stull OA. Mindfulness based art therapy. Eight session manual 2016, https://newbooksinpolitics.com/get/ebook.php?id=dD79MAAACAAJ (accessed 11 October 2019)
- 73.Monti DA, Kash KM, Kunkel EJ, Brainard G, Wintering N, Moss AS, Rao H, Zhu S, Newberg AB. Changes in cerebral blood flow and anxiety associated with an 8‐week mindfulness programme in women with breast cancer. Stress Health 2012; 28:397–407 [DOI] [PubMed] [Google Scholar]
- 74.Monti DA, Kash KM, Kunkel EJ, Moss A, Mathews M, Brainard G, Anne R, Leiby BE, Pequinot E, Newberg AB. Psychosocial benefits of a novel mindfulness intervention versus standard support in distressed women with breast cancer. Psycho-Oncology 2013; 22:2565–75 [DOI] [PubMed] [Google Scholar]
- 75.Monti DA, Peterson C, Kunkel EJS, Hauck WW, Pequignot E, Rhodes L, Brainard GC. A randomized, controlled trial of mindfulness‐based art therapy (MBAT) for women with cancer. Psycho‐Oncology 2006; 15:363–73 [DOI] [PubMed] [Google Scholar]
- 76.Meghani SH, Peterson C, Kaiser DH, Rhodes J, Rao H, Chittams J, Chatterjee A. A pilot study of a mindfulness-based art therapy intervention in outpatients with cancer. Am J Hosp Palliat Care 2018; 35:1195–200 [DOI] [PubMed] [Google Scholar]
- 77.Peterson C. Walkabout: Looking In, Looking Out: A Mindfulness-Based Art Therapy Program, Art Therapy 32;2:78–82
- 78.Jang S-H, Kang S-Y, Lee H-J, Lee S-Y. Beneficial effect of mindfulness-based art therapy in patients with breast cancer – a randomized controlled trial. Explore 2016; 12:333–40 [DOI] [PubMed] [Google Scholar]
- 79.Jang SH, Lee JH, Lee HJ, Lee SY. Effects of mindfulness-based art therapy on psychological symptoms in patients with coronary artery disease. J Korean Med Sci 2018; 33:e88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hiser J, Koenigs M. The multifaceted role of the ventromedial prefrontal cortex in emotion, decision making, social cognition, and psychopathology. Biol Psychiatry 2018; 83:638–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Beerse ME, Van Lith T, Stanwood GD. Is there a biofeedback response to art therapy? A technology-assisted approach for reducing anxiety and stress in college students. SAGE Open 2019; 9:2158244019854646 [Google Scholar]
- 82.Conley CS, Durlak JA, Shapiro JB, Kirsch AC, Zahniser E. A meta-analysis of the impact of universal and indicated preventive technology-delivered interventions for higher education students. Prev Sci 2016; 17:659–78 [DOI] [PubMed] [Google Scholar]
- 83.Donker T, Petrie K, Proudfoot J, Clarke J, Birch M-R, Christensen H. Smartphones for smarter delivery of mental health programs: a systematic review. J Med Internet Res 2013; 15:e247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bakker D, Kazantzis N, Rickwood D, Rickard N. Mental health smartphone apps: review and evidence-based recommendations for future developments. JMIR Mental Health 2016; 3:e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Conley CS, Shapiro JB, Kirsch AC, Durlak JA. A meta-analysis of indicated mental health prevention programs for at-risk higher education students. J Counsel Psychol 2017; 64:121. [DOI] [PubMed] [Google Scholar]
- 86.Chiesa A, Serretti A, Jakobsen JC. Mindfulness: top-down or bottom-up emotion regulation strategy? Clin Psychol Rev 2013; 33:82–96 [DOI] [PubMed] [Google Scholar]
- 87.Reive C. The biological measurements of mindfulness-based stress reduction: a systematic review. Explore (New York, NY) 2019; 15:295–307 [DOI] [PubMed] [Google Scholar]
- 88.Garland EL. Restructuring reward processing with mindfulness-oriented recovery enhancement: novel therapeutic mechanisms to remediate hedonic dysregulation in addiction, stress, and pain. Ann NY Acad Sci 2016; 1373:25–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Guendelman S, Medeiros S, Rampes H. Mindfulness and emotion regulation: insights from neurobiological, psychological, and clinical studies. Front Psychol 2017; 8:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Baglioni C, Spiegelhalder K, Lombardo C, Riemann D. Sleep and emotions: a focus on insomnia. Sleep Med Rev 2010; 14:227–38 [DOI] [PubMed] [Google Scholar]
- 91.Harvey AG. A cognitive model of insomnia. Behav Res Ther 2002; 40:869–93 [DOI] [PubMed] [Google Scholar]
- 92.Jansson-Frojmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res 2008; 64:443–9 [DOI] [PubMed] [Google Scholar]
- 93.Morphy H, Dunn KM, Lewis M, Boardman HF, Croft PR. Epidemiology of insomnia: a longitudinal study in a UK population. Sleep 2007; 30:274–80 [PubMed] [Google Scholar]
- 94.Kaneita Y, Yokoyama E, Harano S, Tamaki T, Suzuki H, Munezawa T, Nakajima H, Asai T, Ohida T. Associations between sleep disturbance and mental health status: a longitudinal study of Japanese junior high school students. Sleep Med 2009; 10:780–6 [DOI] [PubMed] [Google Scholar]
- 95.Taylor DJ, Bramoweth AD, Grieser EA, Tatum JI, Roane BM. Epidemiology of insomnia in college students: relationship with mental health, quality of life, and substance use difficulties. Behav Ther 2013; 44:339–48 [DOI] [PubMed] [Google Scholar]
- 96.Trockel M, Manber R, Chang V, Thurston A, Taylor CB. An e-mail delivered CBT for sleep-health program for college students: effects on sleep quality and depression symptoms. J Clin Sleep Med 2011; 7:276–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gress-Smith JL, Roubinov DS, Andreotti C, Compas BE, Luecken LJ. Prevalence, severity and risk factors for depressive symptoms and insomnia in college undergraduates. Stress Health 2015; 31:63–70 [DOI] [PubMed] [Google Scholar]
- 98.Espie CA. Insomnia: conceptual issues in the development, persistence, and treatment of sleep disorder in adults. Annu Rev Psychol 2002; 53:215–43 [DOI] [PubMed] [Google Scholar]
- 99.Kales A, Caldwell AB, Preston TA, Healey S, Kales JD. Personality patterns in insomnia. Arch Gen Psychiatry 1976; 33:1128–4 [DOI] [PubMed] [Google Scholar]
- 100.Ong JC, Ulmer CS, Manber R. Improving sleep with mindfulness and acceptance: a metacognitive model of insomnia. Behav Res Ther 2012; 50:651–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Drake CL, Pillai V, Roth T. Stress and sleep reactivity: a prospective investigation of the stress-diathesis model of insomnia. Sleep 2014; 37:1295–304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Howell AJ, Digdon NL, Buro K. Mindfulness predicts sleep-related self-regulation and well-being. Person Individual Diff 2010; 48:419–24 [Google Scholar]
- 103.Fairholme CP, Nosen EL, Nillni YI, Schumacher JA, Tull MT, Coffey SF. Sleep disturbance and emotion dysregulation as transdiagnostic processes in a comorbid sample. Behav Res Ther 2013; 51:540–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Fernandez-Mendoza J, Vela-Bueno A, Vgontzas AN, Ramos-Platon MJ, Olavarrieta-Bernardino S, Bixler EO, De la Cruz-Troca JJ. Cognitive-emotional hyperarousal as a premorbid characteristic of individuals vulnerable to insomnia. Psychosom Med 2010; 72:397–403 [DOI] [PubMed] [Google Scholar]
- 105.Kirwan M, Pickett SM, Jarrett NL. Emotion regulation as a moderator between anxiety symptoms and insomnia symptom severity. Psychiatry Res 2017; 254:40–7 [DOI] [PubMed] [Google Scholar]
- 106.Cincotta AL, Gehrman P, Gooneratne NS, Baime MJ. The effects of a mindfulness‐based stress reduction programme on pre‐sleep cognitive arousal and insomnia symptoms: a pilot study. Stress Health 2011; 27:e299–e305 [Google Scholar]
- 107.Hood HK, Rogojanski J, Moss TG. Cognitive-behavioral therapy for chronic insomnia. Curr Treat Options Neurol 2014; 16:321. [DOI] [PubMed] [Google Scholar]
- 108.Ong J, Sholtes D. A mindfulness-based approach to the treatment of insomnia. J Clin Psychol 2010; 66:1175–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ong JC, Manber R, Segal Z, Xia Y, Shapiro S, Wyatt JK. A randomized controlled trial of mindfulness meditation for chronic insomnia. Sleep 2014; 37:1553–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Schmidt U. A plea for symptom-based research in psychiatry. Eur J Psychotraumatol 2015; 6:27660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Isgut M, Smith AK, Reimann ES, Kucuk O, Ryan J. The impact of psychological distress during pregnancy on the developing fetus: biological mechanisms and the potential benefits of mindfulness interventions. J Perinatal Med 2017; 45:999–1011 [DOI] [PubMed] [Google Scholar]