Abstract
This study explores differences in the use of CycleProGo™ (CPG), a fertility-tracking app developed by Couple to Couple League (CCL), between those exposed to it as a part of natural family planning (NFP) instruction versus those who find it on their own. An anonymous data set of 17,543 CPG accounts opened between April 2013 and June 2016 was used for analysis. Nonmember users opened the most accounts (58 percent, n = 10,134), CCL members represented 38 percent (n = 6,758) of new accounts, and 207 CCL teachers (4 percent) were using CPG for personal charting. Significantly more nonmember accounts had zero days of use after the initial opening compared to CCL member accounts (61 percent vs. 23 percent, respectively, χ2 = 2,405.9, p < .001). Conversely, significantly more CCL member accounts were used for ninety days or longer than nonmember accounts (47 percent vs. 13 percent, respectively, χ2 = 2,404.2, p < .001). CCL students—those who began using the app as part of a formal NFP teaching curriculum—were more likely to use the app for > six cycles compared to nonmembers. In accounts with at least one complete cycle, CCL students were the most diligent at daily recording (95 percent of cycle days with observation recorded) followed by CCL members (88 percent) and nonmembers (76 percent). CCL teachers had the lowest frequency of cycle days with a recorded observation (73 percent). Within each cohort, accounts with > six recorded cycles had a lower proportion of cycle days with an observation recorded, likely reflecting increasing knowledge of their personal fertility patterns. Long-term users who had no known formal training in NFP still had the lowest proportion cycle days with a fertility observation. We conclude formal NFP instruction increases the probability of long-term app use, and regardless of training, long-term users will likely record observations on about 70 percent of cycle days.
Summary:
“CycleProGo™ users with NFP training were more persistent and diligent about daily data input than those without training.”
Keywords: Fertility awareness, Fertility awareness information technology, Natural fertility care, NFP, Persistence with app use, Women’s reproductive health
Fertility-tracking apps are extremely popular; they are the fourth most common health app among adults and second most popular among adolescent females (Moglia et al. 2016). With the widespread availability of fertility-tracking apps and the increasing emphasis on lifestyles that avoid synthetic chemicals to live more naturally, it is likely fertility-tracking apps are exposing more women to consider using a fertility awareness–based method of family planning as an alternative to hormonal or barrier-based contraceptives.
Many apps claim to be useful for avoiding pregnancy and automatically identify the fertile window, but a systematic review (Duane et al. 2016) demonstrated a large proportion are not based on evidenced-based methods of fertility awareness. More recently, Freis et al. (2018) evaluated twelve apps claiming to assist with identifying the optimal days in the cycle to conceive and found that most were poor predictors of the most fertile days unless they measured some aspect of estrogenic activity to indicate the days most proximate to ovulation.
Natural Cycles is the first fertility-tracking app approved by the Food and Drug Administration (FDA), demonstrating effectiveness in preventing pregnancy when combined with barrier use during the app-identified fertile window. The clinical trial used to support FDA approval enrolled over 25,000 users, but only 30 percent completed a full year of app use suggesting persistence with a fertility app may be a barrier to long-term use (Berglund Scherwitzl et al. 2017). Conversely, researchers found recruitment for a clinical trial of the DOT app among eligible DOT users difficult until enrollment procedures were fully automated, underscoring the importance of ease of use and autonomy for app users (Shattuck, Haile, and Simmons 2018). Thus, more data are needed to understand the appropriate balance of autonomy or independence with ongoing support from experts who will optimize fertility-tracking app adoption and use.
CycleProGo™ (CPG) is a fertility-tracking app developed by Couple to Couple League (CCL) available in both Apple and Android formats. It is available to the public and provided to everyone who takes a CCL natural family planning (NFP) class. In addition, all CCL teachers have an account to be able to review and comment on charts shared with them by CPG users. Examination of CPG accounts provides an opportunity to compare the charting behaviors of different cohorts of app users; experienced NFP users (CCL Teachers), those who learned NFP in a formal curriculum (CCL members); and the public who may or may not have any knowledge of NFP beyond the app itself.
This study explores differences in the use of a fertility-tracking app between those exposed to it as a part of NFP instruction versus those who find it on their own and to compare the charting behaviors of these different cohorts. Specifically, we sought to determine whether those who have no known training in NFP persist in their use of CPG at rates comparable to those who began using the app during formal instruction. Further, we wanted to know whether differing levels of knowledge of NFP (NFP teachers, CCL students, non-CCL users) influence daily use patterns of CPG.
Method
To conduct this study, an anonymous data set of all CPG accounts opened between April 2013 and June 30, 2016, was obtained from the CPG administrator. Users of CPG consent to allow their data to be used in summary reports when they open an account, and individual identities are not revealed. User data are stored in a secure, cloud-based structured query language database that was queried by the CPG administrator to obtain the data set used for this investigation. The data set consisted of account-level information including date of account opening, source of the account (CCL member, public, or teacher account), counts of daily activity, demographics, and other background information (optionally entered by the user). In addition, a separate anonymous cycle data set contained all cycle and fertility observations uploaded by the users. Because the data provided did not allow the author to connect any information to any individual using CPG and there was no funding source requiring review, Institutional Review Board review was not undertaken. The study was conducted following the principles of the Declaration of Helsinki.
To create the needed cohorts for comparison, the account-level and cycle-specific data sets were merged using Access (Microsoft Corp. Redmond, Washington, 2007), so all information recorded was linked via a unique account identifier. After removing all data related to administrative accounts, the accounts were then segregated into three cohorts: nonmember users—those who opened an account from an app store and have no known membership connection to CCL, CCL members—those who opened an account via a mechanism promoted only to CCL members (this group includes new CCL students enrolled in a class who are provided a link to the app on registration for class), and CCL teacher accounts. Comparisons between groups were conducted using either χ2 or Fisher’s exact test for categorical data or t-test for continuous data with (two tailed) significance set at p < .05. No adjustments were made for multiple comparisons. Analysis of variance with Tukey’s ‘honestly’ significant difference (HSD) posttest was used to compare average daily uploads/cycle between groups.
CycleProGo™
The CPG app uses the symptothermal method taught by CCL to interpret the data entered by the user. Users have flexibility to select which rules define the fertile window in each cycle and can also manually override the calculated fertile window if they wish. It is programmed to be somewhat conservative if left in its default mode.
To calculate a cycle’s fertile window automatically, CPG requires user to enter both daily basal body temperatures and cervical mucus observations along with the start of the cycle and menstrual-bleeding patterns. A cycle is considered complete when the user designates a specific day as the start of a new cycle. Additional fertility observations can be entered (e.g., cervix observations, luteinizing hormone measurements, and extensive personal notes), but these are not used in the calculation of the fertile window. The algorithm to determine the fertile window in default mode employs the rules clinically tested by Frank-Herrmann et al. (2007) in the first year of that trail.
For the first cycle, all days are considered fertile until the end of the fertile window is calculated (consistent with how CCL teaches new members). From cycle #2 onward, the default beginning of the fertile window is defined as the earliest of the first day of observed cervical mucus or cycle day 6 (i.e., days 1–5 of the cycle are considered infertile unless mucus is observed). Once twelve complete cycle lengths are entered (via historical and/or prospectively captured data), this “Day 5” rule will automatically switch to the “Day 6” (fertile window begins day 7) if all cycles in the previous twelve are twenty-six days or longer. If a cycle of < twenty-six days is recorded, the rule reverts to “Day 5” until the next twelve cycles are again twenty-six days or longer.
To calculate the end of the fertile window, CPG uses the symptothermal rule as the default. This rule requires both three days of cervical mucus dry up past the peak day and three postpeak day temperatures all higher than the low temperature level (LTL)—defined as the highest temperature of the six days immediately prior to the temperature rise—with the third day at least 0.4 F above the LTL. If these conditions are not met, the fertile window ends after four days of mucus dry up plus four elevated postpeak temperatures (above the LTL).
Results
During the period examined, 17,543 accounts were opened and included over 55,000 cycles. Most of the accounts opened were by nonmember users (58 percent, n = 10,134), while CCL members represented 38 percent (n = 6,758) of new accounts. All CCL teachers have a CPG account to be able to provide counseling to app users who share their charts with them. In this data set, 207 of the 639 teachers were also using CPG to track their own cycles, reflecting that paper charts are commonly used, and some CCL teaching couples are no longer charting due to menopause.
To understand how long the accounts are used once opened, the number of days between the account opening date and the last data upload date was calculated and used as a rough measure of length of use. Although more numerous, significantly more nonmember accounts have zero days of use after the initial opening compared to CCL member accounts (61 percent [n = 6,214] vs. 23 percent [n = 1,549], respectively, χ2 = 2,405.9, p < .001). In addition, significantly more CCL member accounts are used for ninety days or longer than nonmember accounts (47 percent [n = 3,147] vs. 13 percent [n = 1,285], respectively, χ2 = 2,404.2, p < .001). This higher proportion of CCL members using the app longer could reflect selection bias since CCL members are more likely self-selected to be NFP users, whereas the nonmember accounts may reflect a more generalized population.
To explore this further, we compared the proportion of accounts with six or more complete cycles in nonmember and CCL new student accounts. Table 1 illustrates that CCL students are more likely to use the app for six cycles or more compared to nonmembers. This difference is observed whether examining all accounts with at least one complete cycle (26 percent vs. 20 percent, respectively) or if the analysis is limited to only those accounts opened in 2014 or 2015, allowing at least six months charting time for all enrollees (38 percent vs. 23 percent, respectively).
Table 1.
Frequency of Six or More Complete Cycles in Accounts Opened by CCL Students in Comparison to Nonmembers.
| No. of Complete Cycles | All Accounts | Accounts Opened in 2014–2015 Only | ||
|---|---|---|---|---|
| Nonmember (Percent) | CCL Student (Percent) | Nonmember (Percent) | CCL Student (Percent) | |
| 1–5 cycles | 1,069 | 622 | 736 | 330 |
| >Six cycles | 254 (20 percent) | 218 (26 percent)a | 220 (23 percent) | 201 (38 percent)b |
Note: The number of accounts with at least one complete cycle for nonmembers and CCL students is shown. Accounts opened only in 2014–2015 allow comparison of new CycleProGo™ users (nonmembers or students) who have > six months since opening the account. CCL = Couple to Couple League.
a Significantly different than nonmember accounts (p < .0003, Fisher’s exact test [two-tailed]).
b Significantly different than nonmember accounts (p < .0001, Fisher’s exact test [two-tailed]).
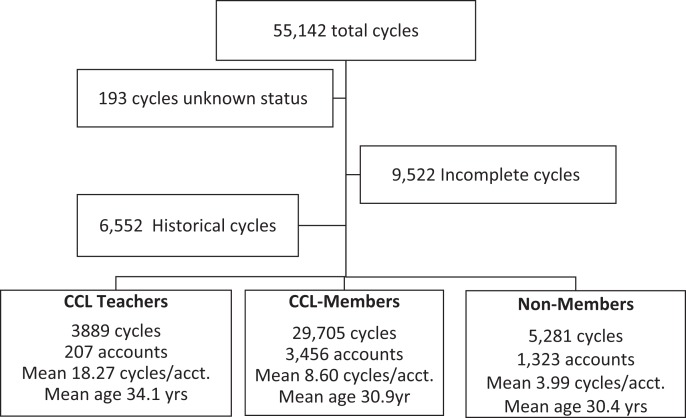
An examination of the cycle-specific information provides further perspective on the charting behaviors of these cohorts (Figure 1). Of the 55,142 total cycles captured, 6,552 were entered as historical cycles, and 193 cycles could not be assigned to specific type of user so were excluded from analysis. Of the cycles captured prospectively, 9,522 were defined as incomplete—either because a new cycle start date was not designated or they were longer than 100 days. The average length of the 38,875 complete cycles was 29.9 days; 88 percent of all cycles were between 21 and 35 days long, just over 10 percent were > thirty-five days long and <2 percent were shorter than 21 days.
Figure 1.
Distribution of cycles by type and cohort. Historical cycles are those entered by the user on account opening. Incomplete cycles are missing the start date for the following cycle or are one hundred days or longer. The remaining cycles, distributed between the three types of users, are complete. Mean ages shown include accounts where an age was provided by the user at account opening (nonmembers: n = 403; CCL members: n = 1,852; CCL teachers: n = 68); teachers are significantly older than either CCL members (p < .001, t-test) or nonmembers (p = .0002, t-test). CCL = Couple to Couple League.
Interestingly, 81 percent of accounts containing incomplete cycles indicated they were trying to conceive, whereas just 7 percent of accounts with complete cycles indicated they were trying to conceive. Caution is called for in drawing too much from the disparity between complete and incomplete cycles because this question is not required to be answered and is set to “trying to avoid” by default, but the differences suggest potentially different charting behaviors depending on a couple’s pregnancy intentions.
CCL members are the largest cohort both in accounts with a complete cycle and in total cycles. Around 51 percent (3,456 of 6,758) of all CCL member accounts have at least one complete cycle; 61 percent (804 of 1,304) of the known student accounts within this cohort have at least one complete cycle. In comparison, just 13 percent (1,323 of 10,124) of nonmember accounts have at least one complete cycle.
The CCL teacher cohort has the fewest accounts of the three yet has the largest average number of cycles per account (eighteen cycles/account). This is not surprising as one would expect CCL teachers to be regularly charting since they are, on average, significantly older than either the nonmember or CCL member cohorts (p < .0001) so have had more time to accumulate charts.
Regardless of cohort, most cycles employed the default rules in CPG to determine the fertile window. Among those with six or more complete cycles, the beginning of the fertile window was identified by the default “day5/6” rule in 94 percent of nonmember and CCL member cycles (CCL students used default rule in 96 percent of cycles), while CCL teachers employed it in 85 percent of cycles. Similarly, the end of the fertile widow was most commonly defined by the symptothermal rule, 88 percent of nonmember and CCL member cycles (CCL students in 89 percent of cycles) and 85 percent of CCL teacher cycles.
To explore potential differences in daily use of the app between groups, we compared the number of days with a fertility observation recorded to the total number of days of the cycle within each cohort. As shown in Table 2, when looking at all accounts with at least one complete cycle, CCL students are the most diligent at daily recording (95 percent of cycle days have an observation recorded) followed by CCL members (88 percent) and nonmembers (76 percent). CCL teachers have the lowest frequency of cycle days with a recorded observation (73 percent).
Table 2.
Comparison of Average Daily Uploads by Different User Groups.
| Nonmember | CCL Member (n = 3,334) | CCL TCs | ||
|---|---|---|---|---|
| Nonstudent Member | CCL Student | |||
| All complete cycles | ||||
| No. of accounts | 1,150 | 2,532 | 803 | 210 |
| Average upload/cycle (SD) | 23.73 (18.59) | 27.38 (18.87) | 29.48 (18.91) | 22.85 (21.29) |
| Percent cycle days with upload | 76.5 percenta | 87.8 percent | 95 percentb | 72.7 percent |
| Six or more complete cycles | ||||
| No. of accounts | 226 | 1,451 | 236 | 146 |
| Average, upload/cycle (SD) | 18.81 (12.20) | 23 (12.05) | 23.67 (11.14) | 21.43 (17.13) |
| Percent cycle days with upload | 62.8 percentc | 76 percent | 78 percent (ns) | 70.7 percent |
Note: The proportion of cycle days with a fertility observation was used to compare the daily usage patterns between nonmembers, CCL members, and CCL TCs. Nonstudent members were further segregated from students to evaluate the potential time effects of natural family planning instruction on CycleProGo™ use behaviors. Analysis of variance with Tukey’s HSD posttest was used to compare between group differences. ns = students not significantly different than members or TCs (p > .40). CCL = Couple to Couple League; CCL TCs = CCL Teachers.
a Significantly different than members and students (p < .0001), ns versus TCs (p = .91).
b Significantly different than all other groups (p < .001).
c Significantly different than members and students (p < .001), ns versus TCs (p = .27).
Within each cohort, those accounts with six or more recorded cycles have a consistently lower proportion of cycle days with an observation recorded compared to the entire cohort. The mean number of cycles days with a fertility observation uploaded was not significantly different when comparing experienced CCL members (members, students, and teachers not significantly different). Interestingly, however, even among those who have adopted app-based charting, those who had no known formal training in NFP still have the fewest cycle days with a fertility observation.
Discussion
This may be the first study to explore the daily charting behaviors of app users and provides an initial look at the differences in use between those who are exposed to the app as part of a formal NFP training program and those who simply begin to use the app on their own.
Although more accounts are opened by those not known to be connected to formal NFP training, those exposed to the app as part of NFP instruction are significantly more likely to adopt long-term use. Compared to CCL members, nonmembers using the app have significantly fewer complete cycles and record fertility observations significantly less often.
CCL teachers using the app to track their own cycles have significantly more complete cycles than either members or nonmembers reflecting both their commitment to using NFP and their longer time of use. Interestingly, this cohort had the fewest proportion of cycles days with a fertility observation entered. This may reflect their experience and knowledge of their personal fertility patterns, allowing better “targeting” of days where recording observations is crucial.
CCL members and especially CCL students—those who opened a CPG account because of registering for a CCL class—average significantly more daily updates than either nonmembers or teachers indicating better adherence to the daily behavior of the method. By six months, however, CCL members and CCL students daily update averages are no different than CCL teachers, which suggests growing confidence in use of the method reduces the need for strict daily compliance.
Importantly, prior to training, CCL students are not necessarily more inclined to chart regularly than the general population; CCL has reported over 80 percent of all CCL class attendees are engaged and 70–90 percent of student couples indicate they are attending NFP classes as requirement for marriage (data not shown). A previous two-year study in a single diocese that required NFP as part of marriage prep found 54 percent and 23 percent of class attendees were current or former contraceptive users, respectively (Manhart 2012).
From this, we conclude formal NFP instruction increases the probability of long-term app use. New app users without NFP training are more likely to stop using the app altogether, are more likely to skip recording fertility observations, and make fewer daily recordings with continued use. Taken together, this may make use of NFP more confusing and/or be perceived as less effective to the user who does not have the benefit of some training while learning.
Whether or not training can be in person or online and what elements are critical to effective training that promotes good long-term charting behaviors remain to be explored. It is likely many of the CCL student accounts in this study belong to students who made use of CCL’s online training course launched in 2015, but the anonymous nature of the data sets used precludes isolation of these accounts. The randomized trial of the Marquette method, where all new users learned and were provided ongoing support online, suggests that online learning can be effective (Fehring et al. 2013). A retrospective study of billingsMentor (Smith and Smith 2014), a web-based portal that both trains and interprets fertility observations using the Billings method, indicated it was comparable to personal training, but prospective adoption and use has yet to be reported. It would be of interest to compare the adoption and use of NFP between those who learn online and those who learn in person in future research.
This study is strengthened by the fact the data collection is passive and reflects real-world users unimpacted by potential influences on subjects who are part of a formal clinical study. It also benefits from relatively large cohorts particularly the nonmember and CCL member groups, limiting selection bias that smaller cohorts might introduce. This approach does have inherent weaknesses, however. For example, the intermittent user who stops using the app for a time and then begins using it regularly again will look like a continuous user and the inability to pinpoint the type and timing of formal NFP instruction among CCL members. While these reduce specificity of the conclusions we can draw, they do not materially impact the general themes identified. Finally, it is notable that regardless of the level of NFP training users have, most complete cycles had the fertile window defined by the default rules set in CPG.
Acknowledgment
Brian Frackleton is to be thanked for pulling the data from the CycleProGo™ servers and organizing it into a workable file for use in this investigation.
Biographical Note
Michael D. Manhart, PhD, is currently serves as a senior scientific consultant for CCL and is a member of the FACTS Advisory Council. After receiving his doctorate in microbiology from the University of Cincinnati College of Medicine, he embarked on a career in research and development (R&D) with Procter& Gamble. While there, he held numerous management roles of increasing responsibility in various global healthcare and pharmaceutical organizations; he retired in 2008 as a director of R&D. He also served on the CCL Board of Directors from 2007 to 2009. In July 2009, he was appointed as executive director and led the organization until 2016. He and his wife have served as volunteer CCL teachers for over thirty years. He resides in Cincinnati, Ohio, and is the proud father of four and grandfather of five.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Michael D. Manhart, PhD  https://orcid.org/0000-0003-1727-1846
https://orcid.org/0000-0003-1727-1846
References
- Berglund Scherwitzl E., Lundberg O., Kopp Kallner H., Gemzell Danielsson K., Trussle J., Scherwitzl R. 2017. “Perfect-Use and Typical-Use Pearl Index of a Contraceptive Mobile App.” Contraception 96:420–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duane M., Contreras A., Jensen E. T., White A. 2016. “The Performance of Fertility Awareness-Based Method Apps Marketed to Avoid Pregnancy.” Journal of the American Board of Family Medicine 29:508–11. [DOI] [PubMed] [Google Scholar]
- Fehring R. J., Schneider M., Raviele K., Rodriguez D., Pruszynski J. 2013. “Randomized Comparison of Two Internet-Supported Fertility-awareness-Based Methods of Family Planning.” Contraception 88:24–30. [DOI] [PubMed] [Google Scholar]
- Frank-Herrmann P., Heil J., Gnoth C., Toledo E., Baur S., Pyper C., Jenetzky E., Strowitzki T., Freundl G. 2007. “The Effectiveness of a Fertility Awareness Based Method to Avoid Pregnancy in Relation to a Couple’s Sexual Behavior during the Fertile Time: A Prospective Longitudinal Study.” Human Reproduction 22:1310–19. doi:10.1093/humrep/dem003 [DOI] [PubMed] [Google Scholar]
- Freis A., Freundl-Schuett T., Wallwiener L., Bauer S., Strowitzki T., Freundl G., Frank-Herrmann P. 2018. “Plausibility of Menstrual Cycle Apps Declaring Support to Conceive.” Frontiers in Public Health 6:98. doi: 10.3389/fpubh.2018.00098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manhart M. D. 2012. “Natural Family Planning Instruction as a Marriage Requirement: A Retrospective Analysis of the First Two Years’ Experience in the Diocese of Covington.” The Linacre Quarterly 79:487–98. doi: 10.1179/002436312804827136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moglia M. L., Nguyen H. V., Chyjek K., Chen K. T., Castano P. M. 2016. “Evaluation of Smartphone Menstrual Cycle Tracking Applications Using an Adapted Application Scoring System.” Obstetrics & Gynecology 127:1153–60. [DOI] [PubMed] [Google Scholar]
- Shattuck D., Haile L. T., Simmons R. G. 2018. “Lessons from the Dot Contraceptive Efficacy Study: Analysis of the Use of Agile Development to Improve Recruitment and Enrollment for mHealth Research.” JMIR mHealth uHealth 6:e99 http://mhealth.jmir.org/2018/4/e99/. doi:10.2196/mhealth.9661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A. D., Smith J. L. 2014. “billingsMentor: Adapting Natural Family Planning to Information Technology and Relieving the User of Unnecessary Tasks.” The Linacre Quarterly 81:219–38. doi: 10.1179/2050854914Y.0000000024. [DOI] [PMC free article] [PubMed] [Google Scholar]