Abstract
This study reports on 632 cycles from 105 women who were using the CREIGHTON MODEL FertilityCare™ System to avoid pregnancy and had either a serious reason to avoid pregnancy or some degree of a lack of confidence. A progesterone level was drawn on the third day after the Peak Day as they were charting, and if the progesterone level was 2.3 ng/mL or greater, then ovulation was determined to have passed. If the level was greater than 3.0 ng/mL, this indicated that an absolute period of infertility had begun. In these cases, no pregnancies were observed. In the 27 cycles in which a specific follow-up relative to pregnancy could not be definitively determined, the progesterone levels in all cases were 2.3 ng/mL or greater with 23 of the 27 cycles being 3.1 ng/mL or greater. It is highly unlikely that any of those became pregnant as well. These cycles were collected over thirteen years (2004–2016). Two case presentations are also a part of this article of two families in which the couples had very serious reasons to avoid pregnancy. In these two couples, each of the women was multi-gravid and had no evidence of subfertility or infertility. They used the family planning progesterone level (the Peak Day +3 progesterone level) for a total of 167 cycles over a number of years successfully without a subsequent pregnancy.
Summary:
This article presents a thirteen-year effort to evaluate the serum progesterone level on the third day after the Peak Day as observed by women charting the CREIGHTON MODEL FertilityCare™ System. It is known that the Peak Day is associated with ovulation, and if the progesterone reaches a certain level, then an absolute period of infertility should follow. In fact, this is what this study reflects.
Keywords: CREIGHTON MODEL FertilityCare™ System, Luteal phase, NaProTechnology, National hormone laboratory, Natural infertility, Natural methods, Peak Day +3, Progesterone
In the study of the natural means to regulate fertility, a great deal of progress has been made in the last fifty years in the practical application of the information provided through a better understanding of the menstrual and fertility cycle. In humans, this has the ability to reveal the stages of naturally occurring fertility and infertility, so that couples can utilize this information to successfully either avoid pregnancy or achieve pregnancy. With regard to avoiding pregnancy, extensive studies have been done of the CREIGHTON MODEL FertilityCare™ System that reveals its practical application and success in the avoidance of pregnancy (Hilgers and Stanford 1998).
There have, however, continued to be certain problems and/or difficulties that arise in the use of natural methods in general, and this has to do specifically with the use of a natural method in complex or difficult circumstances. This would include patients who have a complex set of biomarkers that instill a lack of confidence in the user. While this does not appear to happen very often, it does nonetheless occur, and there are also situations where pregnancy is a major health risk to an individual woman or family, and a high level of certainty in the ability to avoid pregnancy is both morally, ethically, and medically needed and consistent with Catholic teaching (Pope Paul VI 1968).
The purpose of this study is to report on a thirteen-year study of patients who were recommended the use of a serum progesterone level drawn in the early phase of the functioning corpus luteum. This level utilizes the CREIGHTON MODEL FertilityCare™ System and the identification of the third day following the Peak Day. The study commenced in 2004 and concluded in 2016. In addition, this study will present two case summaries of individual patients who have benefited significantly from this approach.
Methods and Materials
The CREIGHTON MODEL FertilityCare™ System uses a standardized observational system for assessing the presence or absence of the cervical mucus discharge, while at the same time, using a universal language for describing these observations, which is objective and taught with the use of a Picture Dictionary (Hilgers et al. 2001), and has been validated over many years of use. In this situation, the woman can identify the flow of cervical mucus from the cervix as she approaches ovulation. This mucus usually begins as a sticky or tacky cloudy-type discharge and becomes clear, stretchy, and/or lubricative. The last day in which the mucus is clear, stretchy, or lubricative is called the Peak Day and has been studied in a variety of different approaches for its correlation to the time of ovulation (Billings et al. 1972; Hilgers, Abraham, and Cavanagh 1978). By the time a woman reaches the third day post-Peak, ovulation should have passed or would be in the process of passing.
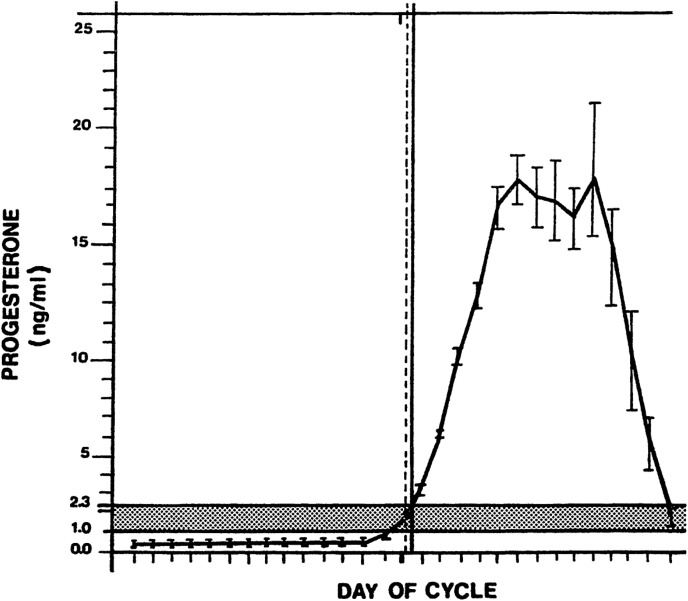
In this study, they were asked to have their blood drawn on Peak Day +3, so that a serum progesterone level could be measured. This measurement was done by chemimmunofluorescence in the National Hormone Laboratory of the Saint Paul VI Institute. Ovulation was presumed to have occurred when the progesterone level goes between 1.0 ng/mL and 2.3 ng/mL. Once it has passed 2.3 ng/mL, then ovulation would have been considered complete, and a time of infertility would have begun (Figure 1).
Figure 1.
This shows the ovulatory time span from 1.0 to 2.3 ng/mL in a group of sixty-five cycles where progesterone levels were measured daily around the time of ovulation. The dotted vertical line is the average observation of the Peak Day and the solid vertical line is the average timing of ovulation in these cycles. Source: Hilgers, Abraham, and Cavanagh (1978).
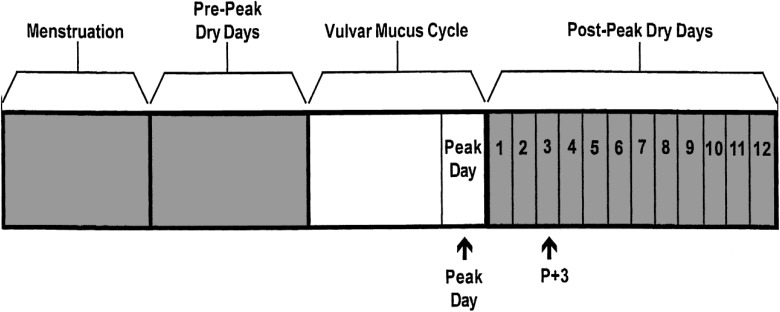
This use of progesterone for the timing of ovulation was first described in 1978 (Hilgers, Abraham, and Cavanagh 1978) and has subsequently been confirmed by the use of serial ultrasound examinations of ovulation (Hilgers 2004; Wetzel and Hoagland 1982). To interpret this, the patient had her blood drawn on Peak Day +3 (Figure 2) and was provided four categories of interpretation. These four categories are:
Figure 2.
This is a schematic sketch of the CREIGHTON MODEL FertilityCare™ System with menstruation, the pre-Peak dry days, the vulvar mucus cycle with the identification of the Peak Day, and the post-Peak dry days with the arrow pointing to Peak Day +3 where the early luteal phase progesterone levels are drawn.
| Progesterone Level | Interpretation of Level |
|---|---|
|
You have either not yet ovulated or you are within twenty-four hours of starting your period. |
|
You are in the midst of ovulating. Repeating another level in forty-eight hours should clarify your situation. You should consider yourself fertile. |
|
You have almost for certain ovulated. To be absolutely sure, a repeat level in twenty-four to forty-eight hours will clarify it. You are most likely not fertile until your next period starts. |
|
You have ovulated, and you are naturally infertile until the start of your next menstrual period. |
Since these progesterone levels are not used for any particular medical purpose except identifying postovulation infertility, a special note is also placed on the report form:
PLEASE NOTE: This test is not for medical, diagnostic or therapeutic purposes. It is for assisting you in identifying your natural state of post-ovulation (post-Peak) infertility and is intended for use in association with the CREIGHTON MODEL FertilityCare™System.
The patients were then informed of the result usually within twenty-four hours, and they can utilize that information to manage their fertility in a way which is completely natural, has no side effects, and should have a very high rate of success.
After thirteen years of collecting this data, it was compiled for this report. In addition, the National Hormone Laboratory, which is located at the Saint Paul VI Institute (PPVI), is a dedicated CLIA-approved reproductive hormone laboratory and has done, over many years, comparative studies with other outside laboratories that have been interested in trying to standardize their own laboratory results to those of the PPVI. In this fashion, we had a number of laboratories that had done correlative studies when the progesterone levels were 3.0 or less. This study also involved a comparison of these results of the National Hormone Laboratory to other laboratories that have submitted specimens to us as a way of validating these results on a more widespread basis in outside laboratories.
Results
There were 105 patients who entered this program between the years 2004 and 2016. They contributed a total of 632 cycles to this assessment. Any patients with known infertility problems were excluded. The number of cycles monitored in this fashion, ranged from 1 to 124 cycles. The age range of the patients ranged from 23 to 45 years.
Of the 105 patients who entered, 83 (79 percent) had follow-up with regard to subsequent pregnancy, while (20.9 percent) were lost to follow-up. The total cycles that were entered was 632 of which 605 (95.7 percent) had follow-up, and only 27 (4.3 percent) were lost to follow-up. During this interval, no pregnancies were observed in either group (see Table 1).
Table 1.
Total Number of Patients and Cycles Entered 2004–2016.
| Total Patients Entered (n) | Patients with Follow-up | Patients Lost to Follow-up | ||
|---|---|---|---|---|
| n | % | n | % | |
| 105 | 83 | 79.0 | 22 | 21.0 |
| Cycles with Follow-up | Cycles Lost to Follow-up | |||
| Total Cycles Entered | n | % | n | % |
| 632 | 605 | 95.7 | 27 | 4.3 |
| Number of Pregnancies Observed | 0 | 0 | ||
When looking further at the loss to follow-up group, most of these were in the early stages of the study between 2004 and 2009, when 63 percent of these cycles and 63.6 percent of these patients were identified. In the last seven years of the study, this decreased to 37 percent of the cycles and 36.4 percent of the patients (see Table 2).
Table 2.
Year Patient Entered and Lost to Follow-up.
| Year Patients Entered and Lost to Follow-up | Patients | Cycles | ||
|---|---|---|---|---|
| n | % | n | % | |
| 2004–2009 | 14 | 63.6 | 17 | 63.0 |
| 2010–2016 | 8 | 37.4 | 10 | 37.0 |
| Total lost to follow-up | 22 | 100.0 | 27 | 100.0 |
Of those total cycles that were lost to follow-up, four had progesterone levels ranging from 2.3 ng/mL to 3.0 ng/mL, while in twenty-three of the twenty-seven cycles, the level was greater than or equal to 3.1 ng/mL (see Table 3). It is highly unlikely that these patients became pregnant, and we have no direct or indirect evidence that any of them did.
Table 3.
Peak Day +3 Progesterone Levels in Patients Lost to Follow-up (n = 27).
| Total Cycles Lost to Follow-up | Progesterone Level | |||
|---|---|---|---|---|
| 2.3–3.0 ng/mL | >3.1 ng/mL | |||
| n | % | n | % | |
| 27 | 4 | 14.8 | 23 | 85.2 |
| Pregnancies observed | 0 | |||
There are situations when the first progesterone level runs low (categories 1 or 2), when it is recommended that a repeat or a “double draw” progesterone is assessed. Of the 632 cycles, 40 of them resulted in “double draw” cycles for an incidence of 6.33 percent. There was an additional group whose Peak Day +3 progesterone levels were between 2.3 ng/mL and 3.0 ng/mL, and they chose not to have a “double draw” but the progesterone levels themselves suggest infertility (n = 29; 4.59 percent) (see Table 4).
Table 4.
Incidence of “Double Draw” Cycles.
| Double Draws in Patients in Study | n | % |
|---|---|---|
| Total number of cycles “Double Draws” | 40 | 6.33 |
| Peak Day +3 progesterone levels 2.3–3.0 ng/mL and no “Double Draws” (patient’s choice) | 29 | 4.59 |
Note: n = 632.
In doing this assessment, we charged the patient $15 for running the progesterone level. That is a significant reduction from laboratories that charge for progesterone levels that would be otherwise on a medical basis (about 25 percent of the normal charge). This does make this approach much more workable and affordable.
A comparison of progesterone levels between the National Hormone Laboratory (PPVI) with outside laboratories is found in Table 5. When the progesterone level at the Institute’s laboratory was between 0.1 ng/mL and 1.0 ng/mL, the average level for the Institute was 0.69 ng/mL, and the comparative level of the outside lab was 1.03 ng/mL with a p < .025. If the level was 1.1 ng/mL to 3.0 ng/mL, the average level for the Institute’s laboratory was 2.25 ng/mL, and for an outside laboratory, it was 2.33 ng/mL. This is not a statistically significant difference, and you will note the 95 percent confidence limits that are also presented in Table 5.
Table 5.
Comparison of Progesterone Levels at National Hormone Laboratory (PPVI) with Outside Laboratories
| Range Testeda | NHL/PPVI | Outside Labb | p Value |
|---|---|---|---|
| 0.1–1.0b (n = 15) | 0.69 | 1.03 | <0.025c |
| 1.1–3.0 (n = 17) | 2.25 [1.98–2.52]d | 2.33 [1.46–3.20]d | NSc |
| 3.1–7.5 (n = 38) | 5.25 | 6.51 | <0.005e |
a From Pope Paul VI Institute (PPVI)/ National Hormone Laboratory (NHL) data. NS: Not statistically significant.
b Comparison levels from multiple different laboratories.
c Paired t-tests.
d95.0 percent confidence limits.
e Wilcoxon Signed-Rank test for difference in medians.
Case Summary No. 1
This patient is a forty-year-old, gravida 8, para 6, who had had one miscarriage and seven Cesarean sections. Her youngest child had a condition called arthrogryposis. They had used natural methods for all of their married life and found that they got pregnant using all of them in one way or another. Pregnancy evaluations were not done to better understand the cause because they weren’t in programs that do these. This child, however, had a severe musculoskeletal disease and in a three-month period of time had forty plaster casts applied. This became very stressful to their marriage, and they entered the CREIGHTON MODEL program, and the family planning progesterone level was recommended to them. Over 124 cycles and almost ten years, she has had the Peak Day +3 progesterone level drawn, and it created a significant certainty in their ability to identify postovulation infertility. Her husband especially liked this approach, and the stress of the marriage was significantly reduced. She has now done this over 124 cycles without a pregnancy.
Case Summary No. 2
This is a forty-five-year-old, gravida 6, para 6, who has a hereditary bone disease called osteogenesis imperfecta. Three of her children also have this condition. She was recommended to have this bone disease treated with pamidronate, and she was warned she could absolutely not get pregnant if she was taking this. She did forty-five cycles with this approach, during which she was pressured by her doctor to take birth control pills or for her husband to have a vasectomy. It should be noted that her husband was not a huge supporter of the use of a natural method, but during this time, their relationship grew stronger by personal testimony and the patient informed us, “I was able to maintain my integrity.” During this period of monitoring, she did not have another pregnancy.
Discussion
This study took a number of years to complete because a relatively small number of CREIGHTON MODEL users actually qualified for the study. There were two indications for its use and these included (1) patients who lacked confidence in the system usually due to continuous mucus discharges and (2) patients who had serious reasons to avoid pregnancy.
There were no pregnancies observed in the eighty-three patients who contributed 605 cycles in which follow-up was present. In the patients who were lost to follow-up (twenty-two patients and a total of 27 cycles), the progesterone level in all cases was 2.3 ng/mL or greater. In fact, in 23 of those 27 cycles the progesterone level was greater than or equal to 3.1 ng/mL and only 4 had a progesterone level between 2.3 ng/mL and 3.0 ng/mL. It is likely that those individuals did not achieve pregnancy since ovulation should have passed by the time the progesterone level reached 2.3 ng/mL or greater. They were each informed of the results of the tests, and a more likely assumption is that they felt like they didn’t need this information any further, and it confirmed their observations. This represented only 4.3 percent of the overall cycles studied. Many of these cycles were collected in the early phase of the study 2004–2009 (63.0 percent) compared to fewer cycles represented in the 2010–2016 group (37.0 percent).
In some cases, the protocol called for them to obtain a second blood draw to measure a second progesterone level. These were referred to as “double draws” and represented only a total of forty cycles in which the overall percentage of the total was 6.33 percent. There were twenty-nine cycles in which the progesterone level was 2.3 ng/mL or greater, and the individual was categorized as “most likely not fertile until the next menstrual period starts,” and by patient’s choice, they elected not to redraw.
Progesterone measurement by immunological assays is most comparable from one laboratory to another at the lowest ranges of progesterone production, in the neighborhood of 4 ng/mL or less. As progesterone increases, there becomes a much wider coefficient of variation between one laboratory and the next. With this understanding, it was noted that when the Institute’s National Hormone Laboratory measured the progesterone level and had it remeasured in an outside laboratory by a similar immunologic technique, the average levels were not statistically significant between the two, and the 95 percent confidence limits were very supportive of virtually no difference between the two. With this in mind, this approach to identifying postovulation infertility, it would seem, could be utilized immediately by laboratories around the country or for that matter around the world.
The marker that was used to identify the postovulation phase of the cycle was a serum progesterone level drawn and targeted during the early luteal phase of the cycle. Ovulation occurs on the Peak Day (on average) with a range of three days before the Peak Day to three days after the Peak Day (Hilgers et al. 1978; Hilgers, 2004). With this in mind, progesterone is being produced and a good marker that ovulation has passed if the progesterone level gets beyond 2.3 ng/mL. In this system, we have accounted for a slight area of “wiggle room” relative to making a 100 percent definitive statement about being postovulatory. So the absolute area of infertility begins with the progesterone levels greater than 3.0 ng/mL. It should be noted that this does not necessarily mean that the patient actually ovulated but rather that if ovulation did occur, it would have occurred by that time. There are some ovulation disorders such as unruptured follicles that form a corpus luteum but are technically anovulatory. There are a number of other ovulation disorders where they may be technically ovulatory, but the ovulation is still disordered. The progesterone marker in these cases remains the same.
The two case summaries that are presented were individuals who had very serious reasons to avoid pregnancy and wanted to continue to use a natural method. They were able to use the method successfully at 100 percent effectiveness rate with the use of the early luteal phase progesterone level giving the CREIGHTON MODEL FertilityCare™ System the capability of being used in the most difficult of circumstances for couples, whereas, up until this time, there would always be some question.
There has come into existence the measurement of a urinary metabolite of progesterone (pregnanediol) by test kit. The upper limits where this becomes measurable are greater than 5 mcg/mL, and this is the equivalent to between 6 and 8 ng/mL of progesterone in the serum. While 92 percent are thought to be sensitive enough to identify this level in the second generation of the “ovulation double-check” protocol, this is not reached until six days after the LH surge (Communication from www.mfbfertility, May 30, 2017). So using a serum marker where the measurement of progesterone can be measured in the ng/mL range and being in the serum it’s a more immediate marker (as opposed to the urine), we would anticipate that this marker would be more sensitive and occur earlier than with the urinary test kit. Granted, it involves a venipuncture to complete this test and some cooperation from the laboratory to reduce the cost (we suggest $15 per test), but it should be more sensitive.
There are some limitations of the study that have been presented here. One is that there were twenty-two patients for a total of twenty-seven cycles in which we had no definitive follow-up relative to pregnancy. At the same time, we had no report from these patients that pregnancy did occur and the progesterone levels were all 2.3 ng/mL or greater, in fact, twenty-three of the twenty-seven cycles were greater than 3.1 ng/mL. So, if the instructions were followed, then it would be a certainty that they would not become pregnant.
Finally, there is always the position put forth that in a natural method, couples have to “abstain,” and as planned parenthood likes so much to promote, couples are not able to do that successfully. But in our experience in working with couples day in and day out who use natural methods, this is not nearly the problem that people have portrayed it to be. Ultimately, it is a question of whether or not the couple wants to get pregnant or does not want to get pregnant, and under those conditions, they “select” the best time to have intercourse in the cycle. If they have a very serious medical reason, then the utilization of the family planning progesterone level (Peak Day +3) can be utilized with great success as the case summaries support. In both of those cases, the women reported that their husbands liked this approach because of its certainty.
It is an honor for me to present this work in the year 2018 which is the Fiftieth Anniversary of Humanae Vitae. So many people over so many years have suggested that it is not possible to develop natural methods in this fashion and Pope Paul VI came under extraordinary criticism for Humanae Vitae. However, as we study more and more, we begin to realize the wisdom of this decision and the far-reaching positive nature of treating fertility as a gift as opposed to a disease.
Biographical Note
Thomas W. Hilgers, MD, Dip ABOG, SRS, SPS, is a board-certified ob-gyn in obstetrics and gynecology and in gynecologic laser surgery and specializes in reproductive medicine. He is a clinical professor in the Department of Obstetrics and Gynecology at Creighton University School of Medicine, Omaha, Nebraska, and director of the Saint Paul VI Institute for the Study of Human Reproduction. He is also the director of a fellowship program in Medical & Surgical NaProTECHNOLOGY.
Footnotes
Author’s Note: This article was submitted in response to a request for papers in celebration of the Fiftieth Anniversary of Humanae Vitae.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Billings E. L., Billings J. J., Brown J. B., Burger H. G. 1972. “Symptoms and Hormonal Changes Accompanying Ovulation.” Lancet 1 no. 7745: 282. [DOI] [PubMed] [Google Scholar]
- Hilgers T. W. 2004. Correlation of Peak Day to Observation of Follicular Rupture by Serial Ultrasound: Results from 432 Cycles. Omaha, NE: Pope Paul VI Research. [Google Scholar]
- Hilgers T. W., Abraham G. E., Cavanagh D. 1978. “Natural Family Planning-I. The Peak Symptom and Estimated Time of Ovulation.” Obstetrics and Gynecology 52 no. 5: 575–58. [PubMed] [Google Scholar]
- Hilgers T. W., Prebil A. M., Daly K. D., Hilgers S. K. 2001. The Picture Dictionary of the CREIGHTON MODEL FertilityCare™ System. Omaha, NE: Pope Paul VI Institute Press. [Google Scholar]
- Hilgers T. W., Stanford J. B. 1998. “Creighton Model NaProEducation Technology for Avoiding Pregnancy: Use-effectiveness.” The Journal of Reproductive Medicine 43 no. 6: 495–502. [PubMed] [Google Scholar]
- Paul VI Pope. 1968. Encyclical “Humanae Vitae,” July 25 Libraria Editrice Vaticana. [Google Scholar]
- Wetzel L. C. G., Hoagland H. J. 1982. “Relation between Ultrasonographic Evidence of Ovulation and Hormonal Parameters: Luteinizing Hormone Surge and Initial Progesterone Rise.” Fertility and Sterility 37 no. 3: 336–41. [DOI] [PubMed] [Google Scholar]