Abstract
The unmet need for highly accurate methods of disease diagnosis poses new challenges for developments in laboratory medicine. Advances in mass spectrometry (MS)-based disease biomarker discoveries are continuously expanding the clinical diagnostic landscape. Although a number of MS-based in vitro diagnostics are already adopted in routine clinical practices, more are expected to undergo transition from bench to bedside in the near future. The ultrahigh sensitivity, specificity, and low turnaround time in molecular detection by MS make this technology highly powerful in disease detection and therapy monitoring. This mini-review highlights how MS has created a new paradigm in clinical diagnosis, which is growing in importance for public health.
Accurate and rapid performance of medical diagnostic tests is greatly desired to foster clinical decision making and improve human healthcare. The continuous development of new analytical methods and techniques over the last five decades has made a dramatic impact on disease detection and therapeutic treatments. While the majority of in vitro diagnostics involves immunoassays to detect the target analyte, some limitations of this method (cross-reactivity, low sensitivity, limited dynamic range, and often expensive and time-consuming processing) make us pay attention to better solutions with alternative approaches, which should be highly sensitive and specific and offer high throughput. Lately, much excitement has met the news that mass spectrometry (MS) can outperform traditional chemical/biochemical measurements in diagnostic molecular pathology with its ultrahigh sensitivity that can go up to the femtomolar range.1 MS technologies are continuously evolving with new ion source design, enhancement of resolution and sensitivity, and miniaturization over more than a hundred years since its first invention by J. J. Thomson. Increased automation and reduced architectural complexity, size, and cost of different types of MS instruments also promise easy housing and operation. Introduction of electrospray ionization (ESI) and matrix-assisted laser desorption/ionization (MALDI) mass spectrometry in the late 1980s had laid the foundation for large protein detection. Coupling liquid chromatography with ESI mass spectrometry (LC-MS) added another dimension to the analysis of the crude biological mixture in less time. Since then, enormous success in accurate measurement and identification of endogenous biomolecules helped in deciphering the biological mechanism of disease progression and pinpointing the potential biomarkers associated with a disease. MS-based discoveries of new diagnostic biomarkers have played increasingly important roles in disease risk assessment, screening, prognosis, therapy selection, and monitoring. The recent development of ambient ionization mass spectrometry has enabled direct analysis of biological samples (blood, urine, tissue, saliva, sweat, skin, and exhaled breath gases) with little or no sample pretreatment, providing the increased utility of the MS through rapid in situ approaches. This also opens opportunities to invoke MS as a point-of-care (POC) device in the clinical setting for rapid detection of biomarkers, while the patient is on the site, enabling early-stage diagnosis and quick medical decision-making. In this context, miniature MS systems are highly desired for their easy implementation in the field (e.g., in ambulances and health camps) and at the bedside, expanding the use of biomarkers for POC diagnostics. Indeed, recent developments of hand-held/palm-portable (weight ∼1.5 kg) and several other types (weight <15 kg) of miniature MS systems equipped with different types of mass analyzers (quadrupole, cylindrical, rectilinear, and toroidal ion traps) drive their potential for clinical integration at the POC.2,3 Though clinical implementations of these miniature MS devices are at the early stage, assessment of their POC performance needs to be evaluated in terms of their reduced cost and size, improved detection limit and ranges, automation, robustness, versatility, and integration with ambient ionization sources.
The nature of ionization also plays a crucial role in discovering disease biomarkers of various sizes and polarities (Figure 1). After the introduction of electron ionization (EI) by Arthur J. Dempster in 1918, several types of other ionization methods have been developed in the last hundred years for mass spectrometric sampling. The classic methods, which have been used for several years, are EI and chemical ionization (CI). However, these techniques are not found to be used much for clinical diagnostics in modern days because of their limitations in analyzing a wide range of polar biomolecules. Most of the mass-spectrometry-based clinical applications nowadays use MALDI, ESI, atmospheric pressure chemical ionization (APCI), and different types of ambient ionization (AI) sources. Figure 1 shows application ranges of different types of ionization techniques in discovering biomarkers of different sizes and polarities. For example, MALDI and ESI provide excellent coverage of a wide range of molecules, especially the large biomolecules (e.g., proteins), whereas APCI and AI generally examine small metabolites and lipids in the biological sample.
Figure 1.
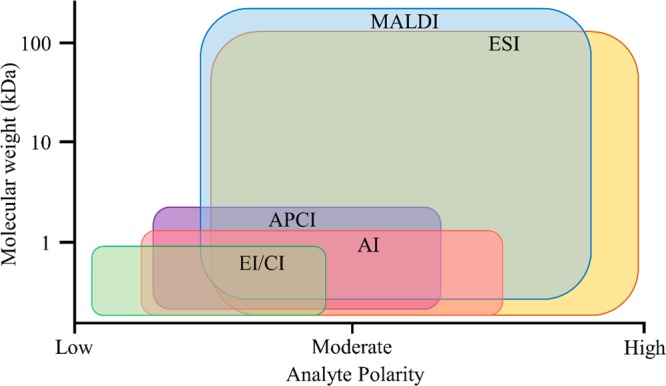
Portrayal ranges of different ionization techniques in the discovery of biomarkers of various molecular weights and polarity.
MALDI- and LC-MS in Clinical Laboratories
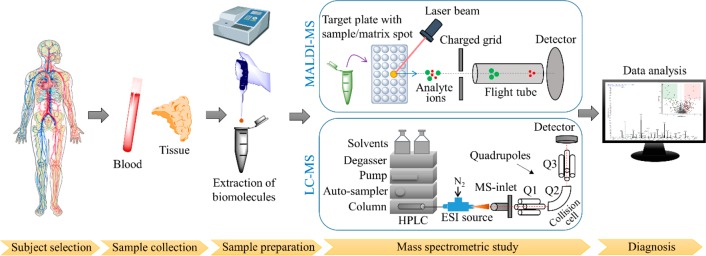
The recent “omics revolution” for biomarker discovery is largely being influenced by the robust performance of soft ionization MS techniques, such as MALDI- and LC-ESI-MS. An enormous amount of work on biological and clinical mass spectrometry, particularly in the last three decades, is unleashing the power of these MS techniques for their ubiquitous role in healthcare. Figure 2 shows the workflow, which is often followed in clinical diagnostics based on MALDI- or LC-MS (often through the ESI interface). Indeed, in the past ten years, the US Food and Drug Administration (FDA) has approved a number of these MS-based in vitro diagnostic methods for the identification of microbes, newborn screening (NBS), quantification of therapeutic drugs in the circulation, and vitamin D assay.
Figure 2.
Schematic overview of the workflow in clinical diagnosis based on mass spectrometry (MALDI-MS or LC-ESI-MS).
The microbial recognition by a benchtop MS (Bruker MALDI Biotyper CA) has revolutionized the way the pathogenic microbes are identified from the culture of human specimens.4 This MS device intercepts characteristic proteome fingerprints of the microorganism colonies and matches them against the reference library spectra to detect it. Thus, the system has gained the ability to identify more than 400 clinically relevant bacteria and yeast species covering nearly 98% of typical bacterial identification tests done conventionally. This has also attained accuracy comparable to that of a nucleic acid sequencing method, but speed, easy operation, robustness, and cost-effectiveness of the MS method can achieve widespread implementation of this technique in microbial testing in the near future.
Likewise, liquid chromatography-tandem mass spectrometry (LC-MS/MS) has emerged as a powerful technique for the simultaneous detection of multiple amino acids, free carnitine, and acylcarnitines from the dried blood spot, providing critical information about inborn errors of metabolism.5 This MS-based method can successfully screen more than 50 different metabolic disorders in one rapid test. This is strikingly different from the conventional enzyme- or immunoassays, which required one test to detect one disorder. Thus, LC-MS/MS has invoked a radical change in newborn screening (NBS), which is routinely being used in many counties. This has significantly contributed to the prevention and medical intervention of many metabolic disorders before they become symptomatic.
Another success of the LC-MS/MS technique in clinical diagnosis is therapeutic drug monitoring, especially the quantification of immunosuppressant drugs in blood, which have a narrow therapeutic index.6 Often this method is applied to estimate the concentration of cyclosporine, tacrolimus, sirolimus, and mycophenolic acid to control their levels in the blood to avoid toxicity and organ rejection during the transplantation. Although immunoassays can be performed here, MS is preferred because of its greater specificity.
Analysis of vitamin D levels in serum by LC-MS/MS is now a gold standard method in clinical laboratories.7 While immunoassays cannot distinguish between 25-hydroxy vitamins D2 and D3, the MS method can separately quantify them with high accuracy. Information on a person’s vitamin D status is important as the deficiency of the same is linked to several skeletal disorders and other diseases. Furthermore, the mass spectrometric study of vitamin D metabolism is tremendously contributing to unraveling the pathophysiology of vitamin D related diseases as well.
The well-documented superiority of the LC-MS/MS technique over traditional immunoassays is often noticed in the literature, which investigates steroids for diagnosing several endocrine disorders.1 Immunoassays often result in the overestimation of those steroids because of cross-reactivity. In contrast, the high specificity of the LC-MS/MS method can successfully analyze steroid hormones with high accuracy. Assessment of thyroid function is crucial in endocrinology. Similarly, the LC-MS/MS technique allows rapid evaluation of thyroid hormones following the isotope dilution method, which can outperform the conventional gold standard equilibrium dialysis method by its speed and sensitivity. These impressive diagnostic capabilities of MS in endocrinology should find potential routine applications in clinics soon. However, many such MS-based endocrinology tests can be found as laboratory-developed tests (LDT) in several companies/institutes in the US.
It is also important to note that the choice of MS instrument varies depending on the clinical application. For example, a triple-quadrupole mass spectrometer coupled to LC is often the choice for quantitative analysis of most of the small molecules for NBS, therapeutic drug monitoring, vitamin D, and steroid assays. A MALDI-TOF (time-of-flight) mass spectrometer is generally used for clinical microbiology as mentioned above.
Although the above selected MS applications in disease diagnosis are followed in several hospitals and clinical settings across the world, there are many more potential MS-based diagnostic tests, which show great promise for the future of laboratory medicine and pathology. The discovery of several diagnostic biomarkers through omics study of blood and tissue samples using MS technology has opened up a new avenue in clinical diagnosis. Several tumor biomarkers, thus, have been identified through intensive research and are awaiting their validation in cohort studies and clinical trials. Evaluation of endogenous metabolic profiles by MS has also demonstrated the usefulness of this technique in disease detection.
In the last two decades, significant trends have been observed in succeeding with artificial intelligence (machine learning) to recognize the complex pattern of omics data recorded by MS for classifying disease and healthy states. In this method, often a training set is first constructed by mining complex MS data (supervised learning) from samples with known pathology (e.g., unhealthy vs healthy) to develop a statistical classifier, which can be further tested with a cross-validation process to access the predictive accuracy within the training set. The performance of the classifier is also judged by applying that to the independent validation set of samples, propelling the discovery of MS diagnostic patterns and therapeutic targets from the omics data. This machine learning approach typically includes (a) dimensionality reduction by decreasing the number of random variables (ion signals), (b) clustering classification to organize ion signals with common characteristics into different groups, (c) density estimation which analyzes ion signals in specific space, and (d) regression analysis to recognize the ion signal patterns for developing the predictive model. More details of the method can be found somewhere else in the literature.8 This pattern recognition approach avoids the tedious job of finding a single or a few biomarkers. Rather, evaluating all MS ion signals (hundreds to thousands) as biomarkers in this process lends much more predicting power of the data, accurately providing the diagnostic information. These types of artificial intelligence-based bioinformatics systems are also found to be vigilant, adaptive, and appropriate to handle the huge dimensionality of omics data, and they also remain open to gain experience through the constant flow of information from the training samples. This MS-based omics pattern diagnosis is also thought to have important implications in detecting diseases at a very early stage when slight but significant molecular dysregulation cascades, and crosstalk specific to a disease is set off.
Ambient Ionization MS: The Future of POC Diagnostics
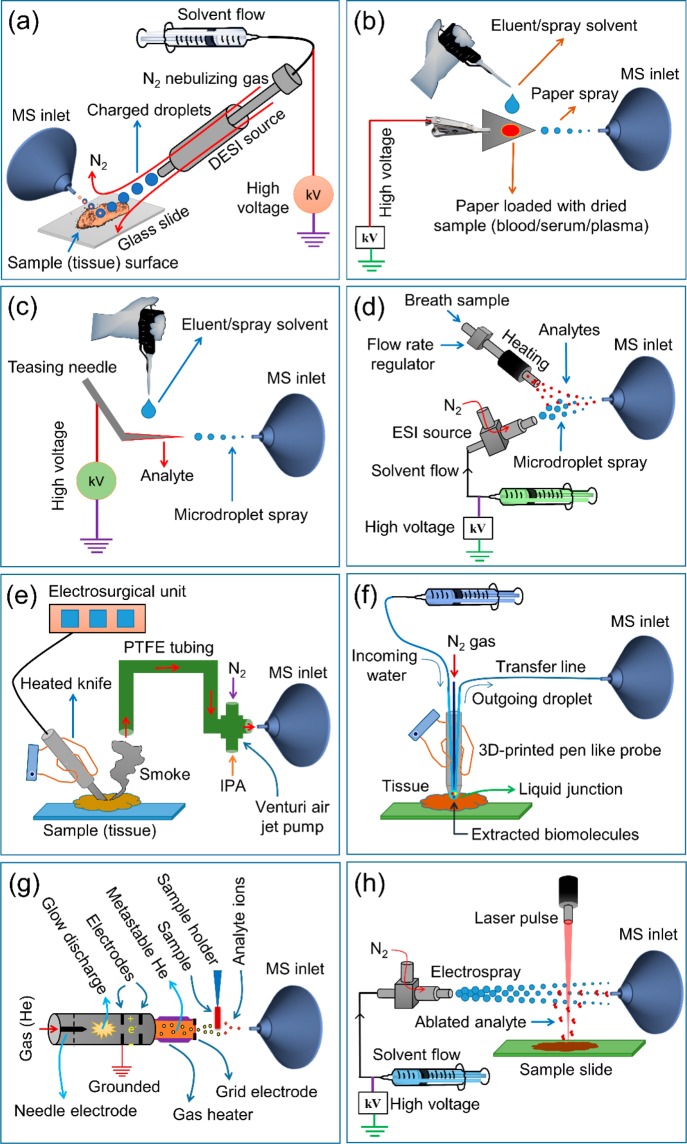
The development of ambient ionization mass spectrometry (AIMS) is another game-changing invention for rapid disease diagnosis with almost no sample pretreatment.9,10 This ionization probe can be directly applied to live organs, skins, tissues, biological fluids, and volatiles open to the air (ambient conditions), aiding instantaneous capture of molecular fingerprints from those samples. Different variants of AIMS have been developed after its first introduction as desorption electrospray ionization mass spectrometry (DESI-MS) in 2004.11Figure 3 represents some of the most promising AIMS, which could ignite a revolution in disease detection. Table 1 summarizes the emerging applications of these AIMS in humans for gaining crucial diagnostic information in a very short time at a much lower cost.
Figure 3.
Schematic diagrams of (a) desorption electrospray ionization mass spectrometry (DESI-MS), (b) paper spray ionization mass spectrometry (PSI-MS), (c) touch spray ionization mass spectrometry (TSI-MS), (d) extractive electrospray ionization mass spectrometry (EESI-MS), (e) rapid evaporative ionization mass spectrometry (REIMS) or iKnife, (f) MassSpec Pen, (g) direct analysis in real-time mass spectrometry (DART-MS), and (h) matrix-assisted laser desorption electrospray ionization mass spectrometry (MALDESI-MS).
Table 1. Use of Some Ambient Ionization Mass Spectrometry Techniques (Figure 3) for the Diagnostic Study in Humans.
| technique | year of inception | type of diagnosis | references |
|---|---|---|---|
| DESI-MS | 2004 | distinguishing cancer and normal specimens, determining cancer aggressiveness and grades, molecular typing of cancer, identifying cancer biomarkers, intraoperative cancer margin assessment, visualizing dermal penetration of sodium channel modulator, acquiring personal information (genders, ethnicities, and ages) from latent fingerprints. | (9, 10, 12, 13, 17, 21) |
| PSI-MS | 2010 | therapeutic drug monitoring and newborn screening from dried blood spot | (10, 14, 15) |
| TSI-MS | 2014 | therapeutic drug monitoring from blood, cancer diagnosis, identification of bacteria from throat swab | (10, 16, 17) |
| EESI-MS | 2006 | skin and breath metabolite detection | (10, 18) |
| REIMS/iKnife | 2009 | intraoperative tissue identification, classification of the tumor and healthy specimens from different organs | (10, 19, 20) |
| MassSpec Pen | 2017 | rapid discrimination of cancer from normal specimens | (3) |
| DART-MS | 2005 | metabolic fingerprinting and quantification | (10, 22) |
| MALDESI-MS | 2006 | mapping the distribution of endogenous and exogenous (drugs) compounds in tissue specimens | (23) |
DESI-MS (Figure 3a) uses a stream of high-speed charged microdroplets to strike the sample (say tissue) surface extracting and transferring molecular species from the sample to the splashed microdroplets, which subsequently undergo evolution to form charged gaseous species to be detected by the MS.11 The DESI experiment can be performed in seconds with minimal or no sample preparation. These characteristics of DESI enable high-throughput analysis of varieties of samples like biopsy specimens, pharmaceutical formulations (tablets, ointments, etc.), and biofluids spotted onto filter paper. DESI-MS can also be operated in two dimensions by scanning the tissue surface in x and y directions, allowing detailed biochemical (lipids, metabolites, etc.) mapping of the tissue.9,12,13 The remarkable success of this label-free molecular imaging technique in rapidly evaluating biopsy specimens promises to employ DESI-MSI as a next-generation histopathology technique (discussed later).
Paper spray ionization mass spectrometry (PSI-MS) is another variant of AIMS (Figure 3b).14 PSI-MS is often used for analyzing a dried sample (e.g., biofluid) spot on a small triangular filter paper, which is clipped to a high-voltage power supply in front of a mass spectrometer. Upon dispensing a spray solvent, analytes are electrosprayed from the sample spot followed by their detection by the mass spectrometer. Thus, human blood, urine, and tissues can be sampled rapidly through this technique under ambient conditions for mass spectrometric analysis (Table 1). These characteristics could make PSI-MS an ideal point of care device for disease detection and clinical diagnosis as the whole workflow, starting from loading the sample to reporting the result, merely takes a few minutes.10 To date, however, the most widespread clinical use of PSI-MS has been for qualitative and quantitative detection of therapeutic drugs in blood, which can be useful in pharmacokinetics and toxicokinetics studies.10,15
Touch spray ionization mass spectrometry (TSI-MS) is a minor modification of PSI-MS, where instead of a paper generally a metallic teasing needle is used for sample loading (Figure 3c).10,16,17 Simple touching of the needle tip with the sample (tissue, blood, throat swab, etc.) causes absorption of analytes in the needle tip, which is then clipped to a high-voltage power source, and the rest of the operation is similar to the PSI source as described above. This convenient and rapid sampling makes TSI-MS remarkably attractive for having low invasiveness and high-throughput performance in blood and tissue analysis (Table 1).
Extractive electrospray ionization mass spectrometry (EESI-MS) works by the fusion of two streams of aerosols, one of which is generated by ESI (Figure 3d).10,18 The sample (urine, serum, exhaled breath, etc.) is nebulized to form aerosol droplets, which are bombarded with the electrospray (ES) droplets, causing coalescence through liquid–liquid extraction. Subsequent droplet evolution by the ES process produces gaseous charged analytes for mass spectrometric detection (Table 1). Rapid in vivo analysis of living objects (e.g., skin) using EESI-MS has been shown to have potential applications in clinical diagnosis and homeland security.10
Rapid evaporative ionization mass spectrometry (REIMS) is another breakthrough in AIMS (Figure 3e).19,20 In REIMS, generally, a heated electrosurgical probe is applied to a tissue to generate a smoke of gaseous ions (generally lipid ions), which are afterward transferred to a mass spectrometer through a flexible tube and Ventury air jet pump. This allows REIMS to provide us in vivo and ex vivo diagnostic information in real time.20 The recent innovation of intelligent knife (iKnife) for cancer surgery is based on REIMS technology. iKnife helps surgeons in determining the cancer resection margin intraoperatively, while the same is applied for cancer ablation simultaneously. The groundbreaking success of iKnife in distinguishing cancer and normal tissues provides a strong platform for its clinical adoption in cancer surgery soon.
The latest invention of a MassSpec pen (Figure 3f) also has huge promise in rapid discrimination of cancer from normal tissues by reading the biochemical signature within ten seconds.3 A MassSpec pen is a hand-held 3D-printed pen consisting of three ports: the incoming port for the delivery of a water droplet, a central port for gas delivery, and the outgoing port for transporting the water droplet containing a biochemical cocktail to the mass spectrometer. Once the pen tip is in contact with the tissue for a few seconds, the water droplet can extract and transfer biomolecules from the tissue to the mass spectrometer. Two important characteristics, e.g., speed and sensitivity, make this pen highly promising to identify the cancer margin rapidly and intraoperatively for complete resection of the tumor.21
DART (direct analysis in real-time) is another versatile ambient ionization technique (Figure 3g), which can ionize species directly desorbed from the sample surface (tablets, biofluids, living organisms, etc.), followed by their mass spectrometric detection. The electrical discharge in the DART ion source delivers excited-state gaseous atoms (e.g., metastable helium), which ionize the surrounding (atmospheric) gases and eventually the analyte species through ion–molecule reaction. As DART can be used in the open environment to analyze samples in their native states (solid, liquid, and gases), this technique promises its widespread implementation for clinical and pharmacological analysis (Table 1) or as a POC device.22
Matrix-assisted laser desorption electrospray ionization (MALDESI) is the hybrid ambient ionization technique combining laser ablation and electrospray post ionization as illustrated in Figure 3h. Upon laser irradiation, the neutral analyte species are desorbed from the sample surface. The plume of these desorbed analytes is allowed to interact with an orthogonal electrospray plume in front of a mass spectrometer. This causes analyte charging by the ESI-like process followed by their mass spectrometric detection. Originally UV laser was used in this ionization, but recently the use of a mid-infrared (IR) laser has been invoked (IR-MALDESI).23 The most common clinical application of MALDESI is the assessment of the distribution of endogenous and exogenous species in the tissue specimens (Table 1). If no matrix is applied for the above ionization, the technique is called electrospray-assisted laser desorption/ionization (ELDI) when UV laser is used or laser ablation electrospray ionization (LAESI) when IR laser is used. Both of these techniques have been used for ex vivo tissue imaging.
Imaging Mass Spectrometry for Disease Diagonsis
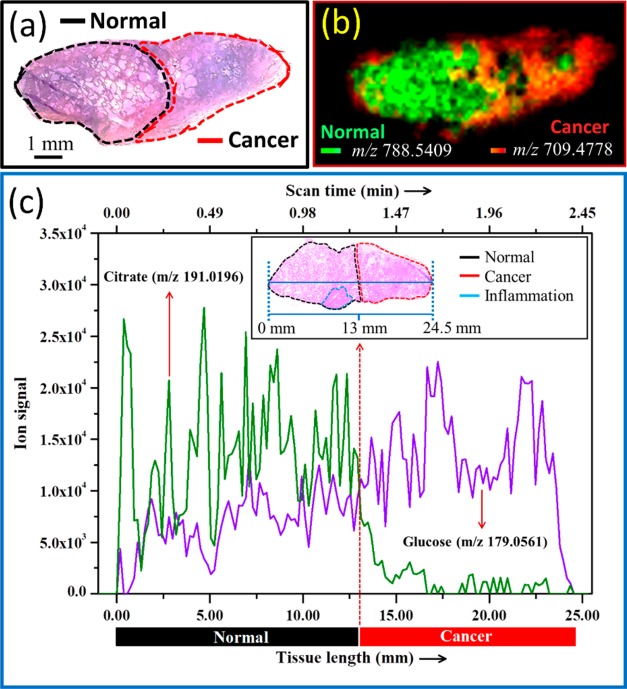
Mass spectrometry imaging (MSI) is a powerful emerging analytical technique that allows simultaneous visualization of the spatial distribution of hundreds of biomolecules (metabolites, lipids, peptides, proteins, etc.) across the tissue specimen without labeling them. DESI and MALDI are the most common ionization techniques used in MSI to desorb analyte species from the tissue surface.9,13,23 Thus, the imaging experiment is performed by scanning the tissue surface in 2D followed by the pixel-to-pixel recording of the mass spectral data, which are plotted finally to construct the ion images. Thus, one MSI scan enables the visualization of hundreds of biomolecules, whatever detected. MSI has great implication in the disease pathology. For example, MSI can be used to pinpoint the biomarker localization in the tissue section for discriminating cancer and normal specimens, evaluating tumor margins from the excision biopsies and diagnosing several other diseases.9,12,13,17,21 While DESI-MSI has the ability to map the distribution of small molecules (metabolites, lipids, etc.), MALDI-MSI can image the distribution of relatively large molecules (peptides, lipids, etc.) and proteins in the tissue. However, DESI has a major advantage over MALDI, particularly because, unlike MALDI, DESI requires minimal sample preparation and does not need a vacuum chamber or an enclosure for ionization. DESI can be operated under ambient conditions (open-air sampling) rapidly to acquire the molecular information in almost real-time. DESI-MSI can be applied to a fresh tissue section or even live organ/skin without any pretreatment. Being less destructive (when the appropriate solvent spray is used), the same section can be evaluated by conventional histopathology (H&E) after its DESI-MSI study. The H&E images can be overlaid with the metabolite/lipid ion map to empower DESI-MSI in understanding the metabolic signature of the healthy and unhealthy tissue. Figure 4 presents an example of diagnosing prostate cancer using DESI-MSI. A typical surgically resected prostate specimen (Figure 4a) was evaluated by a genitourinary pathologist to delineate the areas of cancerous (red outline) and normal (black outline) tissue. DESI-MSI of the adjacent section (Figure 4b) shows the differential distributions of PS(18:0/18:1) (m/z 788.5409) and PA(20:4/17:0) (m/z 709.4778) in cancer and normal cells. While the former (PS) was found to be downregulated, the later (PA) was upregulated in the cancerous area of the tissue.21 Our recent study also revealed that the DESI-MS measurement of glucose and citrate levels can accurately predict the prostate cancer margin rapidly (Figure 4c).24 Further, the application of unsupervised or supervised statistical methods in MSI data pattern recognition can perform well in discriminating the healthy and unhealthy tissues with a very high agreement with the conventional gold standard histopathology (H&E and immune histopathology, etc.).9 Although much of the studies on humans using DESI-MSI focused on cancer,9 the performance of this technique in other diseases (renal, infectious, skin, fertility, transplantation, and metabolic diseases), where tissue analyses are involved, needs to be evaluated in the future. It should be noted that the spatial resolution of DESI-MS images is ∼150–200 μm, which compares well with the thickness of a surgical knife. However, much lower spatial resolution (∼20 μm) can be achieved using MALDI-MSI. Indeed, MALDI-MSI also emerged as a valuable tool with several clinical applications like localizing proteins, mapping the distribution of lipids and neuropeptides at both organ and cellular levels in the context of biomarker discovery, diagnosis, and prognosis of different diseases.23,25 Overall, great sensitivity, chemical specificity, fairly high spatial resolution, and multiplex molecular information make MSI a powerful medical imaging technique, which could serve as a useful adjunct to histology for disease diagnosis.
Figure 4.
(a) H&E of a prostate tissue specimen that contains both normal (black outline) and cancer (red outline) areas. (b) Negative ion mode DESI-MSI of the adjacent section (15 μm thickness) mapping the differential distribution of a phosphatidic acid (m/z 709.4778) and a phosphatidylserine (m/z 788.5409) throughout the tissue (overlaid image in bicolor), distinguishing the areas of cancer and normal. (c) Extracted ion chronograms of glucose and citrate over a line scan of a typical prostate tissue specimen (H&E shown in the inset) that contains both normal (black outline) and cancer (red outline) areas.24
Excitements, Challenges, and Limitations to Overcome
All told, mass spectrometry has opened a new window in the clinical laboratory with its remarkable sensitivity and specificity, which is often not produced by other analytical techniques. Although MS is still underutilized in various clinical settings, it has the potential to extend the current capabilities of disease detection with its high level of accuracy, precision, and reproducibility. Continuous advancements in making MS more robust with various types of automation and robotics also warrant its high-throughput performance with affordable cost-to-benefit balance. From the NBS study, this is now well understood that a single MS test can detect multiple diseases. Therefore, MS can be viewed as a next-generation pathology technique for acquiring multiple pathological information, characteristic of various diseases, in a single test, reducing the financial and technical drain on hospital resources. The development of AIMS has brought a revolution, which is anticipating progression from the time-consuming LC-MS approach to the rapid spatially resolved in situ approach. The use of artificial intelligence in pattern recognition of a huge data set recorded by AIMS lends much more predictive power than that in evaluating the signal of a few diagnostic biomarkers. AIMS has been particularly useful in rapid cancer margin analysis intraoperatively, which is critically needed to augment the success rate of frozen section analysis and to circumvent the need for time in extensive sample processing in conventional histopathology during surgery. The near-future availability of low-cost miniature or hand-held mass spectrometers is likely to play an important role in clinics for the development of POC devices. Taming MS software packages by machine learning algorithms to read the MS data as a “barcode of the disease” should aid the smooth transition of the MS from bench to bedside. Considering all those capabilities, mass spectrometry is appearing as a technique of obvious public health importance, although there could be mixed feelings and anxieties in the clinical diagnostic community as MS could outperform several traditional diagnostic methods. However, cohort studies and clinical trials of many MS-based diagnostic methods should be undertaken on different populations (countries) for their transition from discovery-based approaches to standard clinical practices. Despite the remarkable promise, one of the major limitations of the clinical MS to date is the identification of blood biomarkers for the detection of a disease (say cancer) at a very early stage, when a few maker molecules are released in circulation. So far, most of the MS-based clinical studies have been conducted when the disease is well manifested. This limitation needs to be overcome by appropriate subject selection for the clinical study at the onset of the disease. A biomarker can also present the epiphenomena of a disease, or it could also be found in a similar presentation of a disease. This also needs to be clarified before the clinical practice with the biomarker. Therefore, there are still challenges to overcome in this aspect though we can be optimistic that there should be several MS-based clinical assays approved soon by healthcare regulatory authorities.
Acknowledgments
The author is thankful to the Science and Engineering Research Board, Department of Science and Technology, Government of India, for providing a Ramanujan Fellowship Research Grant (SB/S2/RJN-130/2017) and Early Career Research Award (ECR/2018/001268).
Biography

Shibdas Banerjee completed his M.Sc in chemistry at the Indian Institute of Technology (IIT), Roorkee, India, in 2008 and Ph.D. in chemistry at the Tata Institute of Fundamental Research (TIFR), Mumbai, India, in 2014. He worked as a postdoctoral research associate in the laboratory of Prof. Richard N. Zare, Stanford University, USA, from 2014 to 2017. He is currently an assistant professor in the Department of Chemistry, Indian Institute of Science Education and Research (IISER), Tirupati, India.
The author declares no competing financial interest.
Dedication
Dedicated to Richard N. Zare on the occasion of his 80th birthday.
References
- Yan Z.; Cheng C.; Liu S.. Applications of Mass Spectrometry in Analyses of Steroid Hormones. In LC-MS in Drug Bioanalysis; Xu Q. A., Madden T. L., Eds.; Springer US: Boston, MA, 2012; pp 251–286. [Google Scholar]
- Ferreira C. R.; Yannell K. E.; Jarmusch A. K.; Pirro V.; Ouyang Z.; Cooks R. G. Ambient Ionization Mass Spectrometry for Point-of-Care Diagnostics and Other Clinical Measurements. Clin. Chem. 2016, 62 (1), 99–110. 10.1373/clinchem.2014.237164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J.; Rector J.; Lin J. Q.; Young J. H.; Sans M.; Katta N.; Giese N.; Yu W.; Nagi C.; Suliburk J.; Liu J.; Bensussan A.; DeHoog R. J.; Garza K. Y.; Ludolph B.; Sorace A. G.; Syed A.; Zahedivash A.; Milner T. E.; Eberlin L. S. Nondestructive tissue analysis for ex vivo and in vivo cancer diagnosis using a handheld mass spectrometry system. Sci. Transl. Med. 2017, 9 (406), eaan3968 10.1126/scitranslmed.aan3968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kostrzewa M. Application of the MALDI Biotyper to clinical microbiology: progress and potential. Expert Rev. Proteomics 2018, 15 (3), 193–202. 10.1080/14789450.2018.1438193. [DOI] [PubMed] [Google Scholar]
- Ombrone D.; Giocaliere E.; Forni G.; Malvagia S.; la Marca G. Expanded newborn screening by mass spectrometry: New tests, future perspectives. Mass Spectrom. Rev. 2016, 35 (1), 71–84. 10.1002/mas.21463. [DOI] [PubMed] [Google Scholar]
- Jannetto P. J.Chapter 8 - Therapeutic drug monitoring using mass spectrometry. In Mass Spectrometry for the Clinical Laboratory; Nair H., Clarke W., Eds.; Academic Press: San Diego, 2017; pp 165–179. [Google Scholar]
- Volmer D. A.; Mendes L. R. B. C.; Stokes C. S. Analysis of vitamin D metabolic markers by mass spectrometry: Current techniques, limitations of the “gold standard” method, and anticipated future directions. Mass Spectrom. Rev. 2015, 34 (1), 2–23. 10.1002/mas.21408. [DOI] [PubMed] [Google Scholar]
- Perakakis N.; Yazdani A.; Karniadakis G. E.; Mantzoros C. Omics, big data and machine learning as tools to propel understanding of biological mechanisms and to discover novel diagnostics and therapeutics. Metab., Clin. Exp. 2018, 87, A1–A9. 10.1016/j.metabol.2018.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee S. Ambient ionization mass spectrometry imaging for disease diagnosis: Excitements and challenges. J. Biosci. 2018, 43 (4), 731–738. 10.1007/s12038-018-9785-y. [DOI] [PubMed] [Google Scholar]
- Li L.-H.; Hsieh H.-Y.; Hsu C.-C. Clinical Application of Ambient Ionization Mass Spectrometry. Mass Spectrom. 2017, 6 (2), S0060–S0060. 10.5702/massspectrometry.S0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takáts Z.; Wiseman J. M.; Gologan B.; Cooks R. G. Mass Spectrometry Sampling Under Ambient Conditions with Desorption Electrospray Ionization. Science 2004, 306 (5695), 471–473. 10.1126/science.1104404. [DOI] [PubMed] [Google Scholar]
- Eberlin L. S.; Dill A. L.; Golby A. J.; Ligon K. L.; Wiseman J. M.; Cooks R. G.; Agar N. Y. R. Discrimination of Human Astrocytoma Subtypes by Lipid Analysis Using Desorption Electrospray Ionization Imaging Mass Spectrometry. Angew. Chem., Int. Ed. 2010, 49 (34), 5953–5956. 10.1002/anie.201001452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eberlin L. S.; Ferreira C. R.; Dill A. L.; Ifa D. R.; Cooks R. G. Desorption electrospray ionization mass spectrometry for lipid characterization and biological tissue imaging. Biochim. Biophys. Acta, Mol. Cell Biol. Lipids 2011, 1811 (11), 946–960. 10.1016/j.bbalip.2011.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J.; Wang H.; Manicke N. E.; Lin J.-M.; Cooks R. G.; Ouyang Z. Development, Characterization, and Application of Paper Spray Ionization. Anal. Chem. 2010, 82 (6), 2463–2471. 10.1021/ac902854g. [DOI] [PubMed] [Google Scholar]
- Chiang S.; Zhang W.; Ouyang Z. Paper spray ionization mass spectrometry: recent advances and clinical applications. Expert Rev. Proteomics 2018, 15 (10), 781–789. 10.1080/14789450.2018.1525295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerian K. S.; Jarmusch A. K.; Cooks R. G. Touch spray mass spectrometry for in situ analysis of complex samples. Analyst 2014, 139 (11), 2714–2720. 10.1039/C4AN00548A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ifa D. R.; Eberlin L. S. Ambient Ionization Mass Spectrometry for Cancer Diagnosis and Surgical Margin Evaluation. Clin. Chem. 2016, 62 (1), 111–123. 10.1373/clinchem.2014.237172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu H.; Xu N.; Chen H. Direct analysis of biological samples using extractive electrospray ionization mass spectrometry (EESI-MS). Anal. Bioanal. Chem. 2012, 403 (8), 2145–2153. 10.1007/s00216-012-5874-1. [DOI] [PubMed] [Google Scholar]
- Balog J.; Sasi-Szabó L.; Kinross J.; Lewis M. R.; Muirhead L. J.; Veselkov K.; Mirnezami R.; Dezso B.; Damjanovich L.; Darzi A.; Nicholson J. K.; Takáts Z. Intraoperative Tissue Identification Using Rapid Evaporative Ionization Mass Spectrometry. Sci. Transl. Med. 2013, 5 (194), 194ra93–194ra93. 10.1126/scitranslmed.3005623. [DOI] [PubMed] [Google Scholar]
- Takats Z.; Denes J.; Kinross J. Identifying the margin: a new method to distinguish between cancerous and noncancerous tissue during surgery. Future Oncol. 2012, 8 (2), 113–116. 10.2217/fon.11.151. [DOI] [PubMed] [Google Scholar]
- Banerjee S.; Manna S. K.. Assessment of Metabolic Signature for Cancer Diagnosis Using Desorption Electrospray Ionization Mass Spectrometric Imaging. In Cancer Metabolism: Methods and Protocols; Haznadar M., Ed.; Springer New York: New York, NY, 2019; pp 275–297. [DOI] [PubMed] [Google Scholar]
- Li Y.Application of DART-MS in Clinical and Pharmacological Analysis. In Direct Analysis in Real Time Mass Spectrometry; Dong Y., Ed.; Wiley-VCH Verlag GmbH & Co. KGaA: 2017; pp 223–240. [Google Scholar]
- Barry J. A.; Robichaud G.; Bokhart M. T.; Thompson C.; Sykes C.; Kashuba A. D. M.; Muddiman D. C. Mapping antiretroviral drugs in tissue by IR-MALDESI MSI coupled to the Q Exactive and comparison with LC-MS/MS SRM assay. J. Am. Soc. Mass Spectrom. 2014, 25 (12), 2038–2047. 10.1007/s13361-014-0884-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee S.; Zare R. N.; Tibshirani R. J.; Kunder C. A.; Nolley R.; Fan R.; Brooks J. D.; Sonn G. A. Diagnosis of prostate cancer by desorption electrospray ionization mass spectrometric imaging of small metabolites and lipids. Proc. Natl. Acad. Sci. U. S. A. 2017, 114 (13), 3334–3339. 10.1073/pnas.1700677114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ucal Y.; Durer Z. A.; Atak H.; Kadioglu E.; Sahin B.; Coskun A.; Baykal A. T.; Ozpinar A. Clinical applications of MALDI imaging technologies in cancer and neurodegenerative diseases. Biochim. Biophys. Acta, Proteins Proteomics 2017, 1865 (7), 795–816. 10.1016/j.bbapap.2017.01.005. [DOI] [PubMed] [Google Scholar]