Abstract
Excessive anterior pelvic tilt is suspected of causing femoroacetabular impingement, low back pain, and sacroiliac joint pain. Non-surgical treatment may decrease symptoms and is seen as an alternative to invasive and complicated surgery. However, the effect of non-surgical modalities in adults is unclear. The aim of this review was to investigate patient- and observer-reported outcomes of non-surgical intervention in reducing clinical symptoms and/or potential anterior pelvic tilt in symptomatic and non-symptomatic adults with excessive anterior pelvic tilt, and to evaluate the certainty of evidence.
MEDLINE, EMBASE, Web of Science and Cochrane (CENTRAL) databases were searched up to March 2019 for eligible studies. Two reviewers assessed risk of bias independently, using the Cochrane Risk of Bias tool for randomized trials and the ROBINS-I tool for non-randomized studies. Data were synthesized qualitatively. The GRADE approach was used to assess the overall certainty of evidence.
Of 2013 citations, two randomized controlled trials (RCTs) (n = 72) and two non-RCTs (n = 23) were included. One RCT reported a small reduction (< 2°) in anterior pelvic tilt in non-symptomatic men. The two non-RCTs reported a statistically significant reduction in anterior pelvic tilt, pain, and disability in symptomatic populations. The present review was based on heterogeneous study populations, interventions, and very low quality of evidence.
No overall evidence for the effect of non-surgical treatment in reducing excessive anterior pelvic tilt and potentially related symptoms was found. High-quality studies targeting non-surgical treatment as an evidence-based alternative to surgical interventions for conditions related to excessive anterior pelvic tilt are warranted.
Cite this article: EFORT Open Rev 2020;5:37-45. DOI: 10.1302/2058-5241.5.190017
Keywords: femoroacetabular impingement, non-surgical interventions, pelvic tilt
Introduction
Excessive anterior pelvic tilt is a position of the pelvis in a standing posture where the tilt is larger than what is considered normal. Pelvic tilt measurements obtained from radiographic imaging are used in surgical planning and research assessments. In the clinic, pelvic tilt is measured using inclinometry as the angle between a line connecting the anterior and posterior superior iliac spine (ASIS and PSIS) and in the normal healthy population, the reference value of anterior pelvic tilt is about 8 degrees.1–3 However, as excessive anterior pelvic tilt is not defined by a fixed cutoff point in the literature, the present study uses a definition of an anterior angle greater than 8 degrees.
Excessive anterior pelvic tilt is not an isolated clinical disorder or pathology. Nonetheless it is commonly suspected of causing unspecific low back pain (LBP) and pelvic girdle pain.4–8 The pelvis is closely related to the hip joint as it rotates/tilts anteriorly and posteriorly, around a bicoxofemoral axis, in the sagittal plane.9 Anterior pelvic tilt decreases normal acetabular anteversion (opening towards anterior),10,11 which potentially may affect patients with acetabular retroversion. Acetabular retroversion is a type of developmental hip dysplasia causing an excessive anterior coverage of the femoral head and therefore potentially causing primary femoroacetabular impingement (FAI).12 Primary FAI, which occurs as a result of morphological abnormalities (e.g. acetabular retroversion), should be distinguished from secondary FAI (e.g. excessive pelvic tilt).13 Acetabular retroversion is associated with pain, functional limitations and early development of osteoarthritis of the hip.14 Present curative treatment of acetabular retroversion is anterior osteoplasty or re-orientation of the acetabulum by a periacetabular osteotomy (PAO).15,16 In the normal pelvis, without anatomical signs of acetabular retroversion, excessive anterior tilt may cause a functional positive sign of acetabular retroversion resulting in secondary FAI earlier in the arc of motion.12,17 Thus, a reduction of anterior pelvic tilt may lead to reduced symptoms of primary and/or secondary FAI, which may have implications regarding non-surgical treatment in patients with acetabular retroversion.17 Treatment methods focusing on reducing excessive anterior pelvic tilt are therefore of importance, and textbooks in the field of physical therapy, training, and rehabilitation18–23 suggest various procedures in the therapeutic treatment of symptoms associated with excessive anterior pelvic tilt. Most commonly, physical training focusing on musculoskeletal correction of the postural alignment through increased muscle strength, flexibility, and functional coordinative training is suggested.18–23 However, there seems to be a lack of evidence for the different non-surgical treatment modalities used to correct excessive anterior pelvic tilt and their potential effect on symptoms and level of pelvic tilt.
Therefore, the objective of this systematic review was to investigate the effect of non-surgical treatments in improving patient- and observer-reported outcomes related to symptoms, function and pelvic tilt in symptomatic and non-symptomatic adults, and to assess the overall certainty of evidence.
Methods
Protocol and registration
The systematic review protocol was developed in accordance with the PRSMA-P statement24 and registered online at PROSPERO id: CRD42017056927. Literature search criteria and methods were established and agreed on by all authors.
Eligibility criteria
Studies were eligible if they were non-surgical interventions aiming at reducing symptoms and/or anterior pelvic tilt in symptomatic or healthy participants over 18 years old with excessive anterior pelvic tilt.
Studies were excluded in cases with populations restricted to specific diseases or severe conditions such as neurological diseases (e.g. cerebral palsy, stroke), diseases affecting the posture (e.g. Duchenne muscular dystrophy, spondylolisthesis), degenerative conditions (e.g. spondylosis, hip osteoarthritis), intervertebral discus herniation and osteosynthesis of the lumbopelvic region. Finally, studies on pregnancy were excluded because of the naturally changed spinopelvic posture.
No language restrictions were imposed. In cases of articles reported in other languages than English or Nordic languages, Google translate would have been used.
Information sources
The electronic databases MEDLINE, EMBASE, Web of Science and Cochrane Central Register for Controlled Trials (CENTRAL) were searched for relevant studies up to February 2017. The electronic search was complemented by reference tracking of the included studies. An additional search for relevant new studies added to the databases was carried out in March 2019, and yielded no further studies to be included.
Search
The specific search strategy was created with input from the project team together with a Health Sciences Librarian Tove Faber Frandsen (Appendix 1).
Study selection
The first reviewer (AFB) screened titles and abstracts for potentially eligible studies. Two independent review authors (AFB and AH-L) screened the full text articles for final inclusion. Disagreement was resolved through discussion. Reasons for excluding trials were recorded.
Data collection process
Data item extraction was carried out by one reviewer (AFB), using a standard extraction form developed for this review. Study (author, year of publication, study design), participants (eligible criteria, sample size, age, type of impairment and symptoms), intervention type, outcomes (patient reported and/or observer reported), results and adverse effects.
Assessment of patient-reported outcomes extracted from the included studies was primary for the present study. These outcomes were: pain (e.g. visual analogue scale (VAS), numeric ranking scale (NRS) and questionnaire subscales), health-related quality of life (questionnaire subscale) and level of function (questionnaire subscale). Assessment of observer-reported outcomes was secondary. These outcomes were: radiographs in standing, inclinometry in standing and potentially other validated measures of pelvic tilt in standing. In case of incomplete outcome reporting, the study authors would be contacted for additional information.
Risk of bias in individual studies
The risk of bias for each study was assessed independently and then discussed by two authors (AFB and AH-L) using Cochrane Collaboration’s tool for assessing risk of bias in randomized controlled trials25 and the ROBINS-I tool (Risk Of Bias In Non-randomized Studies – of Interventions).26 In case of disagreement, a third author (AH) was consulted. The overall risk of bias across the studies for both the randomized controlled trials (RCTs) and intervention studies without control was assessed finally.
Synthesis of results
Due to expected and encountered variation of study designs and heterogeneity in results, data were synthesized qualitatively. Assessment of the overall certainty of the evidence was inspired by The Grades of Research, Assessment, Development and Evaluation (GRADE) approach.27
Results
Study selection
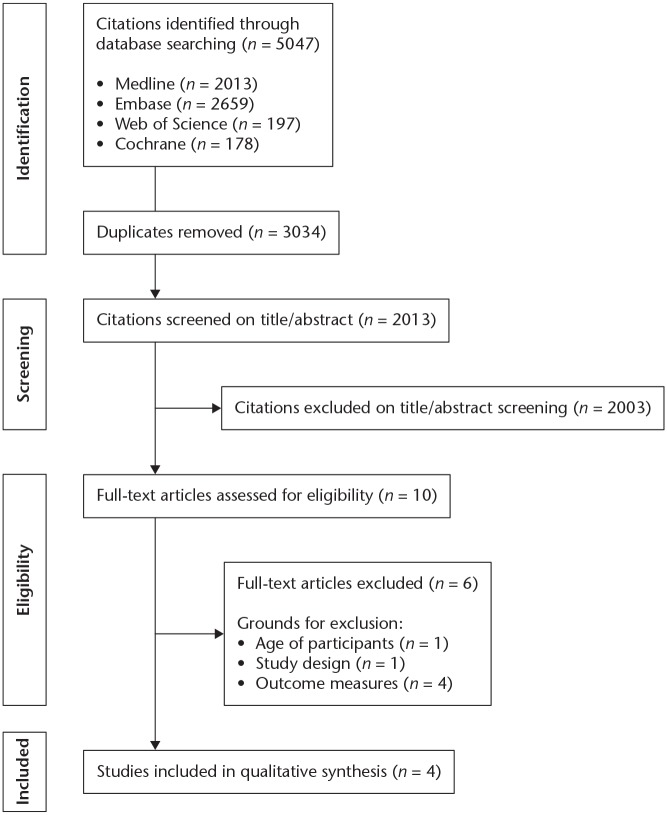
Of 2013 citations, 10 full-text articles were assessed for eligibility; of those 10, four were included in the final qualitative synthesis (Fig. 1).
Fig. 1.
Summary of search strategy results.
Study characteristics
The four studies included in the final qualitative synthesis (two RCTs and two intervention studies without control) contained in total 95 patients with sample sizes ranging from 728 to 40 patients29 (Table 1). Study population and type of intervention differed between all studies.
Table 1.
Characteristics of the included studies
| Authors, year | Design | Sample* | Impairment (symptoms) | Intervention (Experiment/Control) |
Outcomes (Patient/Observer) |
Results | Adverse effects |
|---|---|---|---|---|---|---|---|
| Cottingham et al, 198830 | RCT |
n = 32 males Mean age = 27 years Allocation 1:1 |
Pelvic anteversion > 9o. Healthy non-symptomatic. | The immediate and 24-hour follow-up effect. E: Rolfing soft tissue manipulation of the pelvic region (3 x 15 minutes). The three primary myofascial regions manipulated were the iliopsoas, deep hip rotator, and hamstring muscles. C: Lying in the same positions as those receiving treatment (3 x 15 minutes), without soft tissue manipulation. |
O: Inclinometry of pelvis tilt in standing defined as the angle between an ASIS/PSIS line and the horizontal plane. Parasympathetic activity assessed with a Vagal Tone Monitor |
The experimental group demonstrated immediate and 24-hour decreases of 1.7 o (12.3 o vs. 10.6 o) and 1.4 o (12.3o vs. 10.9 o) (p < 0.01), respectively, in standing anterior pelvic tilt angle, and a significant increase in vagal tone. The control group did not show significant pretest-posttest differences. |
No |
| Levine et al, 199729 | RCT | n = 40; F/M: 32/8 Mean age = 24.5 years Exp/control group F/M distribution: NA Allocation 1:1 |
Healthy subjects with no LBP. Abdominal muscle weakness (Kendall double leg lowering test) | E: Eight-week (5 of 7 days) individual prescribed programme of primarily abdominal strengthening and supplementary hip/lumbar spine stretching exercises. Supervised once a week for programme adjustments. C: Instructed not to change their activity level during the eight weeks. |
O: Inclinometry of pelvis tilt in standing defined as the angle between an ASIS/PSIS line and the horizontal plane. Theta, an index of lumbar lordosis calculated from the length and depth of the lordosis, measured using a flexible ruler in standing position. Abdominal muscle strength (Kendall double leg lowering test). |
Analysis of covariance in the experimental group vs. controls showed an increased abdominal muscle strength (p = 0.001), but no relationship to a mean reduction of 0.5o
(pre 8.7 o vs. post 8.2o) anterior pelvic tilt was found (p = 0.17). |
12 subjects were replaced during the intervention period |
| Barbosa et al, 201328 | Intervention study without control |
n = 7; F/M: NA Age: 18–35 years |
Anterior pelvic tilt and LBP without radiculopathy | Eight weeks (3 sessions per week). HVLA thrust applied to the SIJ. At MVC 12%, isotonic eccentric contractions for knee flexion and concentric contractions of knee flexion were applied. The number of repetitions and series varied in each session. | P: VAS O: Digital photogrammetry in standing of pelvis tilt defined as the angle between an ASIS/PSIS line and the horizontal plane. |
P: Baseline 5.83 ± 1.59 cm and final assessments 1.29 ± 0.58 cm (p = 0.009). O: Baseline 20.38 ± 5.70 degrees and final assessment 14.63 ± 2.17 degrees. Change of 5.8 degrees (p = 0.009). |
No |
| Lee et al, 201431 | Intervention study without control | n = 16 females Mean age ± SD = 23.63 ± 3.18 years |
Habitually wearing high-heeled shoes and having pain in both SIJs during ASLR | The immediate and 24-hour follow-up effect of an application of posterior pelvic tilt taping (PPTT) using kinesiology tape aiming at decreasing anterior pelvic tilt | P: A six-point scale for disability on the ASLR test ranging from 0 (not difficult at all) to 5 (unable to perform). O: Inclinometry of pelvis tilt in standing defined as the angle between an ASIS/PSIS line and the horizontal plane. |
After one day of PPTT all results (p < 0.001) P: ASLR scores (mean ± SD)** Dominant side 3.00 ± 1.10 to 1.38 ± 1.08 Non-dominant side 2.75 ± 1.18 to 1.25 ± 1.13. O: Pelvic tilt (meano ± SD)** Dominant side 11.97 ± 2.81 to 7.16 ± 2.87. Change of 4.8 degrees. Non-dominant side 12.68 ± 2.76 to 7.25 ± 2.45. Change of 5.4 degrees. |
No |
Note. Studies are presented methodologically with RCTs before non-RCTs and publication year.
LBP, low back pain; NA, not applicable; HVLA, high velocity, low amplitude; SIJ, sacroiliac joint; MVC, maximum isometric voluntary contractions; ASIS, anterior superior iliac spine; PSIS, posterior superior iliac spine; VAS, visual analogue scale; RCT, randomized controlled trial; ASLR, active straight leg raise test; SIJ, sacroiliac joint.
*n (number of participants), F/M (female/male).
**Criteria for dominant/non-dominant side are not defined. All patients are described as right-side dominant.
Regarding the RCT studies: Cottingham et al30 included healthy non-symptomatic patients (32 males, mean age 27 years) having an anterior pelvic tilt exceeding nine degrees. The treatment consisted of soft tissue myofascial manipulation of the pelvic region. The immediate and 24-hour effect was assessed as the level of pelvic tilt measured using inclinometry.
Levine et al29 included healthy non-symptomatic patients (32 females/8 males, mean age 24.5 years) having a mean anterior pelvic tilt of 8–10 degrees and abdominal muscle weakness to the extent of not being able to maintain posterior pelvic tilt during a double leg lowering test in supine position. The eight-week intervention consisted primarily of abdominal strengthening exercises supplemented with stretching exercises. Pelvic tilt was measured using inclinometry.
Regarding the intervention studies without control: Barbosa et al28 included patients with non-pre-specified degree of anterior pelvic tilt (mean 20.4 degrees) in combination with low back pain without radiculopathy (n = 7, gender ratio not reported, age range 18–35 years). The eight-week intervention consisted of high-velocity low-amplitude (HVLA) manipulative thrust applied to the sacroiliac joint, followed by quadriceps eccentric and hamstring concentric contractions. The effect was assessed using ‘VAS-pain intensity’ and digital photogrammetry analysis where the pelvic tilt angle was found between two digitally drawn lines.
Lee et al31 included patients having an anterior pelvic tilt at baseline between 11 and 13 degrees, habitually wearing high-heeled shoes in combination with bilateral sacroiliac joint pain (16 females, mean age 23.6 years). Posterior pelvic tilt taping was applied and the effect on symptoms and pelvic tilt was assessed immediately and after one day using a ‘6-point scale for disability’ and inclinometry measuring pelvic tilt.
Risk of bias within studies
Risk of bias within the two RCTs was rated as High (Table 2). Regarding both RCTs, no description of randomization or allocation concealment methods were presented, no reporting of a priori protocols and no blinding of participants or therapists. In the study from Cottingham et al,30 the assessor was not blinded whereas Levine et al29 used two assessors independent from the authors. However, assessor blinding procedure was not described. Furthermore, in the study by Levine et al29 12 out of 20 subjects were replaced during the eight-week intervention due to lack of adherence to the training protocol. No baseline characteristics or analysis of the excluded subjects was provided.
Table 2.
Cochrane Collaboration tool to assess risk of bias for randomized controlled trials
| Authors, year | Risk of bias within each domain | Overall risk of bias across studies | ||||||
|---|---|---|---|---|---|---|---|---|
| Selection bias Random sequence generation |
Selection bias Allocation concealment |
Reporting bias Selective reporting |
Other bias Other sources of bias |
Performance bias Blinding (participants and personnel) |
Detection bias Blinding (outcome assessment) |
Attrition bias Incomplete outcome data |
||
| Cottingham et al, 198830 | Unclear | Unclear | Unclear | High | High | High | Low | High |
| Levine et al, 199729 | Unclear | Unclear | Unclear | High | High | Unclear | High | |
Judgement: Bias is assessed as a judgment (high, low, or unclear) for individual elements from five domains (selection, performance, attrition, reporting, and other).
Assessment of risk of bias (version 5.1.0):
(Within a study) Low risk of bias: Low risk of bias for all key domains
Unclear risk of bias: Unclear risk of bias for one or more key domains
High risk of bias: High risk of bias for one or more key domains
(Across studies) Low risk of bias: Most information is from studies at low risk of bias
Unclear risk of bias: Most information is from studies at low or unclear risk of bias
High risk of bias: The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results
Risk of bias within the two intervention studies without control28,31 was rated as High (Table 3). Without a control group, the studies are at high risk of bias regardless of other weaknesses or strengths.26
Table 3.
The risk of bias in non-randomized studies of interventions (ROBINS-I) assessment tool
| Authors, year | Risk of bias within each domain | Overall risk of bias across domains | Overall risk of bias across studies | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Confounding | Participant selection |
Intervention classification |
Departure from intended interventions | Missing data | Measurement of outcomes | Selection of reported results | |||
| Barbosa et al, 201328 | Critical | Critical | Serious | Moderate | Moderate | Critical | Moderate | Critical | High |
| Lee et al, 201431 | Critical | Serious | Serious | Moderate | Moderate | Serious | Moderate | Critical | |
Judgement (within a study): Low risk of bias (comparable to a well performed randomized controlled trial: RCT), Moderate risk of bias (sound, but not comparable to a well performed RCT), Serious risk of bias (important problems), Critical risk of bias (too problematic to provide useful evidence), No information.
(Across studies) Low risk of bias: Most information is from studies at low risk of bias
Unclear risk of bias: Most information is from studies at low or unclear risk of bias
High risk of bias: The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results
Results of individual studies
Regarding the two RCTs: Cottingham et al30 demonstrated, on 16 healthy non-symptomatic males with pelvic anterior pelvic tilt exceeding nine degrees, that 45 minutes of Rolfing soft tissue manipulation/pelvic mobilization resulted in significant between-group effects. The test group had an immediate and 24-hour mean decrease of anterior pelvic tilt of 1.7 o and 1.4 o (p < 0.01), respectively. The control group did not show significant differences of pelvic tilt.
Levine et al29 demonstrated that an eight-week abdominal strengthening dominated programme on 20 healthy non-symptomatic subjects significantly (p = 0.001) increased the abdominal muscle strength compared to the control group, but no relationship to anterior pelvic tilt was found.
Regarding the two intervention studies without control, Barbosa et al28 showed, over an eight-week intervention via HVLA thrusts applied to the sacroiliac joints in combination with muscle activation for improving pelvic stabilization on seven LBP patients, a significant 4.5 cm (p = 0.009) reduction of low back pain on a 10 cm VAS and 5.8 degrees (p = 0.009) of anterior pelvic tilt. Lee et al31 demonstrated that a one-day application of posterior pelvic tilt taping (PPTT) on 16 women, habitually wearing high-heeled shoes and having pain in both sacroiliac joints during active straight leg raise (ASLR) test, significantly decreased perceived disability in the ASLR test and averagely reduced anterior pelvic tilt with 5.1 degrees (p < 0.001), during and one day after PPTT application.
Synthesis of results
Pelvic tilt was, in all four included studies, measured as the angle between the ASIS/PSIS line and the horizontal plane. In one study digital photogrammetry was used,28 and for the rest, hand-held inclinometry.29–31
The two studies intervening on symptomatic patients demonstrated a significant reduction in LBP28 and sacroiliac joint pain during the ASLR test31 in combination with a significant reduction in anterior pelvic tilt. The type and length of treatment were not comparable as one of the studies28 used HVLA thrusts applied to the sacroiliac joint in combination with muscle activation for eight weeks, and the other study used a one-day application of posterior pelvic kinesiology taping.31 Neither of the two studies used a control group.
Three of the four included studies demonstrated a significant reduction in anterior pelvic tilt.28,30,31 Common to the three studies with a positive outcome on pelvic tilt, was that subjects presented a more pronounced excessive anterior pelvic tilt at baseline (12.0–20.4o), leaving more room for improvement, than the study not observing reduced pelvic tilt (8.7o) following the intervention.29 The significant reductions in anterior pelvic tilt were 1.7o,30 5.1 o,31 and 5.8o.28
Risk of bias across studies
The overall risk of bias across the two randomized controlled trials29,30 is assessed as High (Table 2), due to missing description of randomization, allocation concealment and blinding of participants, therapists, and assessors. Therefore, the information from the studies is at high risk of affecting the interpretation of the results.
The overall risk of bias across domains for the two non-randomized studies is presented in Table 3. Barbosa et al28 was assessed as having Critical risk of bias, indicating that the study is methodologically problematic and cannot provide useful evidence. Lee et al31 was assessed as having Serious risk of bias, indicating important methodological problems resulting in a limited level of evidence.
Inspired by the GRADE approach,27 the overall quality of evidence was due to differences in populations and types of interventions downgraded due to Very serious ′Risk of bias′ with Very serious ′Inconsistency′ in the reported results. Furthermore, as no evidence for which type of intervention is effective for a specific group of patients was presented, Very serious ′Indirectness′ was observed. Finally, the category ′Impression′ was determined as Very serious as no outcomes were reported with confidence intervals, change standard deviations, and small sample sizes were used. Thus, the overall certainty of evidence on the effect of non-surgical treatment in reducing excessive anterior pelvic tilt in adults was graded as Very low.
Discussion
The present systematic review investigated the effect of non-surgical treatment in reducing anterior pelvic tilt and potential related clinical symptoms in adults, and evaluated the risk of bias and the certainty of evidence. Of 5047 citations, four studies were included: two RCTs (n = 72) and two trials without a control group (n = 23). All four types of intervention were different. Three studies demonstrated a statistically significant reduction in anterior pelvic tilt. The two studies without a control group intervening on symptomatic subjects reported a statistically significant reduction in pain and disability. The overall certainty of evidence was assessed as very low.
Strengths and limitations
The strengths of this systematic review include a PROSPERO study protocol that was made publicly available a priori ensuring methodological transparency, a systematic search to maximize identification of all relevant published studies and usage of recognized quality assessment tools.25–27 This systematic review is the first to investigate the effect of non-surgical treatment in reducing anterior pelvic tilt and potential related clinical symptoms in adults, therefore making it difficult to compare the results. A previous narrative review by Hrysomallis and Goodman referred to mechanistic objective outcomes only (e.g. muscle strength and length) and was not restricted to the pelvic area only.32 The authors found it questionable whether resistance training would produce an adaptive shortening of a muscle and elicit postural changes, even if potential tight agonist muscles were lengthened by stretching. However, the narrative review was limited by its lack of systematic literature search and neither of the two RCTs included in the present systematic review were included in the review from Hrysomallis and Goodman. Furthermore, this systematic review included patient-reported outcomes too, as they are important in understanding the relevance and full potential clinical benefits from the patient’s point of view. We did not investigate other postural relationships that potentially can affect pelvic tilt including spinal alignment and deformity, leg alignment and deformity, and leg length differences. This review focused on the isolated effect of non-surgical treatment in reducing anterior pelvic tilt. This review is limited by the paucity of studies in this research area and thus a lack of a meta-analysis, and the heterogeneity in study methods, populations and types of intervention.
Clinical relevance
Spinopelvic sagittal balance is described as an interrelation of muscle function,22,33 and spinal and pelvic morphology9,34 and variations in sagittal posture are tolerated to some extent.9,35 Despite a suggested interrelationship in the literature, there is no causal evidence that excessive anterior pelvic tilt leads to pain, loss of function or reduced quality of life. The relationship between mechanical factors and incidence of LBP was assessed in 600 individuals and no association between anterior pelvic tilt and LBP was found.36 This systematic review found a very limited number (n = 4) of eligible intervention studies. A reason could be that excessive anterior pelvic tilt is not well defined and/or directly causing symptoms.
Levine et al29 found no relationship between anterior pelvic tilt in standing and an increase in abdominal muscle strength, which is consistent with previous studies on asymptomatic subjects37–39 as well as patients with chronic low back pain.40 The cutoff level defining excessive anterior pelvic tilt was set at eight degrees in the present review. It is therefore questionable whether the baseline value of 8.7 degrees of anterior pelvic tilt, in the study by Levine et al, is clinically relevant to attempt reducing by strengthening the abdominal muscles. It is suggested that attention should be given to the complex sensorimotor control system integrating muscle coordination, rather than muscle strength alone, in avoiding excessive anterior pelvic tilt.41 That theory was successfully investigated in a study42 on 54 male adolescents (aged 13–17 years, and consequently excluded from the present systematic study due to the low age) with excessive pelvic tilt (> 14°) randomized into three groups (strength training, strength training and sensorimotor training, and non-exercising control). A significant larger degree of reduction in anterior pelvic tilt in the strength training and sensorimotor training group (3.3°+ 2.2°) compared to the strength training only group (1.6°+ 1.8°) was observed. Thus, it cannot be excluded that patients suffering from clinical symptoms related to excessive anterior pelvic tilt may benefit from sensorimotor training.
Barbosa et al28 found a significant reduction in symptoms (LBP) and the largest numeric reduction in anterior pelvic tilt (5.8°, p = 0.009) of the four included studies. However, due to serious risk of bias, the positive results of HVLA thrusts applied to the sacroiliac joints in combination with muscle activation of the thigh could be due to coincidence, be biased or a placebo effect, and should be interpreted with caution. The long-term effect of the two other studies, Cottingham et al30 and Lee et al,31 presenting a positive treatment effect, is inconclusive due to a follow-up time of only one day.
Clinical perspective and future research
No evidence supports excessive anterior pelvic tilt as an isolated clinical disorder or pathology, and a valid cutoff point defining excessive anterior pelvic tilt is problematic as the spinopelvic sagittal balance can be individually regulated to maintain a proper posture.43,44 Consequently, excessive anterior pelvic tilt must be addressed within a specific condition and possibly also on an individual level. Thus, methodologically high-quality interventions targeting specific types of impairments, biomechanically related to, and in combination with, excessive anterior pelvic tilt are warranted. An area for future research could therefore be to investigate the effect of a non-surgical treatment aiming to reduce excessive anterior pelvic tilt and symptoms in patients with FAI caused by acetabular retroversion, as a potential alternative to surgery. The use of patient-reported outcome measures in combination with objective measures of pelvic tilt is important to differentiate whether the effect of interventions is related to a reduction of pelvic tilt (change of posture) per se, or to mechanical/mechanistic alterations.
Conclusions
Due to limited literature and in general low-quality designs no overall evidence for the effect of non-surgical treatment in reducing excessive anterior pelvic tilt and potentially related symptoms was found. The absence of evidence suggests that high-quality interventions targeting non-surgical treatment as an alternative to invasive surgery in reducing anterior pelvic tilt and/or related symptoms are warranted.
Acknowledgments
The authors wish to thank Health Sciences Librarian Tove Faber Frandsen for helping with the search strategies.
Appendix 1.
Search strategy for MEDLINE
Search strings
(spinopelvic OR spino-pelvic OR pelvic OR pelvis [MeSH]) AND (tilt OR tilts OR anteversion OR anteflexion)
(Posture [MeSH] OR postures OR postural) AND (alignment OR realigning OR realignment OR realignments OR malalignment OR malalignments OR mal-alignment OR mal-alignments)
Footnotes
ICMJE Conflict of interest statement: SO reports grants from Zimmer Biomet outside the submitted work.
AH-L reports consultancy to the EUREKA expert panel reviewing scientific applications for EUREKA outside the submitted work.
The other authors declare no conflict of interest relevant to this work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Herrington L. Assessment of the degree of pelvic tilt within a normal asymptomatic population. Man Ther 2011;16:646–648. [DOI] [PubMed] [Google Scholar]
- 2. Gajdosik R, Simpson R, Smith R, DonTigny RL. Pelvic tilt: intratester reliability of measuring the standing position and range of motion. Phys Ther 1985;65:169–174. [DOI] [PubMed] [Google Scholar]
- 3. Nguyen AD, Shultz SJ. Sex differences in clinical measures of lower extremity alignment. J Orthop Sports Phys Ther 2007;37:389–398. [DOI] [PubMed] [Google Scholar]
- 4. Cailliet R. Low back pain syndrome. Fifth ed. Philadelphia, PA: F. A. Davis Company, 1995. [Google Scholar]
- 5. Jull G, Janda V. Muscles and motor control in low back pain: assessment and management. In: Twomey L, ed. Physical therapy of the low back. First ed. New York: Churchill Livingstone, 1987. [Google Scholar]
- 6. Key J, Clift A, Condie F, Harley C. A model of movement dysfunction provides a classification system guiding diagnosis and therapeutic care in spinal pain and related musculoskeletal syndromes: a paradigm shift-Part 2. J Bodyw Mov Ther 2008;12:105–120. [DOI] [PubMed] [Google Scholar]
- 7. Sahrmann S. Posture and muscle imbalance: faulty lumbar-pelvic alignment and associated musculoskeletal pain syndromes. Orthop Div Rev 1992:13–20. [Google Scholar]
- 8. Kendall FP, McCreary EK, Provance PG, Rodgers MM, Romani WA. Muscles testing and function with posture and pain. Fifth ed. Baltimore, MD: Lippincott Williams & Wilkins, 2005. [Google Scholar]
- 9. Lazennec JY, Brusson A, Rousseau MA. Lumbar-pelvic-femoral balance on sitting and standing lateral radiographs. Orthop Traumatol Surg Res 2013;99:S87–S103. [DOI] [PubMed] [Google Scholar]
- 10. Zahn RK, Grotjohann S, Pumberger M, Ramm H, Zachow S, Putzier M, et al. Influence of pelvic tilt on functional acetabular orientation. Technol Health Care 2017;25:557–565. [DOI] [PubMed] [Google Scholar]
- 11. Fukushima K, Miyagi M, Inoue G, et al. Relationship between spinal sagittal alignment and acetabular coverage: a patient-matched control study. Arch Orthop Trauma Surg 2018;138:1495–1499. [DOI] [PubMed] [Google Scholar]
- 12. Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum: a cause of hip pain. J Bone Joint Surg Br 1999;81:281–288. [DOI] [PubMed] [Google Scholar]
- 13. Langlais F, Lambotte JC, Lannou R, Gedouin JE, Belot N, Thomazeau H, et al. Hip pain from impingement and dysplasia in patients aged 20–50 years. Workup and role for reconstruction. Joint Bone Spine 2006;73:614–62l [DOI] [PubMed] [Google Scholar]
- 14. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003;417:112–120. [DOI] [PubMed] [Google Scholar]
- 15. Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion: treatment with periacetabular osteotomy. J Bone Joint Surg Am 2003;85:278–286. [DOI] [PubMed] [Google Scholar]
- 16. Zurmühle CA, Anwander H, Albers CE, et al. Periacetabular osteotomy provides higher survivorship than rim trimming for acetabular retroversion. Clin Orthop Relat Res 2017;475:1138–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ross JR, Nepple JJ, Philippon MJ, Kelly BT, Larson CM, Bedi A. Effect of changes in pelvic tilt on range of motion to impingement and radiographic parameters of acetabular morphologic characteristics. Am J Sports Med 2014;42:2402–2409. [DOI] [PubMed] [Google Scholar]
- 18. Page P, Frank C, Lardner R. Assessment and treatment of muscle imbalance: the Janda approach. Champaign, IL: Human Kinetics, 2010. [Google Scholar]
- 19. Kisner C, Colby LA. Therapeutic exercise: foundations and techniques. Fifth ed. Philadelphia, PA: FA Davis, 2007. [Google Scholar]
- 20. Liebenson C. Functional training handbook. Philadelphia, PA: Lippincott Williams & Wilkins, 2014. [Google Scholar]
- 21. Sahrmann S. Diagnosis and treatment of movement impairment syndromes. London: Elsevier Health Sciences, 2002. [Google Scholar]
- 22. Lee DG. The pelvic girdle: an integration of clinical expertise and research. Fourth edition. London: Churchill Livingstone, Elsevier, 2011. [Google Scholar]
- 23. Yılmaz Yelvar GD, Baltacı G, Bayrakcı Tunay V, Atay AO. The effect of postural stabilization exercises on pain and function in females with patellofemoral pain syndrome. Acta Orthop Traumatol Turc 2015;49:166–174. [DOI] [PubMed] [Google Scholar]
- 24. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006–1012. [DOI] [PubMed] [Google Scholar]
- 25. Higgins J, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration; Wiley Online Library; 2011. [Google Scholar]
- 26. Sterne JACHM, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Atkins D, Best D, Briss PA, et al. ; GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004;328:1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Barbosa AC, Martins FL, Barbosa MC, Dos Santos RT. Manipulation and selective exercises decrease pelvic anteversion and low-back pain: a pilot study. J Back Musculoskelet Rehabil 2013;26:33–36. [DOI] [PubMed] [Google Scholar]
- 29. Levine D, Walker JR, Tillman LJ. The effect of abdominal muscle strengthening on pelvic tilt and lumbar lordosis. Physiother Theory Pract 1997;13:217–226. [Google Scholar]
- 30. Cottingham JT, Porges SW, Richmond K. Shifts in pelvic inclination angle and parasympathetic tone produced by Rolfing soft tissue manipulation. Phys Ther 1988;68:1364–1370. [DOI] [PubMed] [Google Scholar]
- 31. Lee JH, Yoo WG, Kim MH, Oh JS, Lee KS, Han JT. Effect of posterior pelvic tilt taping in women with sacroiliac joint pain during active straight leg raising who habitually wore high-heeled shoes: a preliminary study. J Manipulative Physiol Ther 2014;37:260–268. [DOI] [PubMed] [Google Scholar]
- 32. Hrysomallis C, Goodman C. A review of resistance exercise and posture realignment. J Strength Cond Res 2001;15:385–390. [PubMed] [Google Scholar]
- 33. Neumann DA. Kinesiology of the hip: a focus on muscular actions. J Orthop Sports Phys Ther 2010;40:82–94. [DOI] [PubMed] [Google Scholar]
- 34. Vaz G, Roussouly P, Berthonnaud E, Dimnet J. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J 2002;11:80–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. During J, Goudfrooij H, Keessen W, Beeker TW, Crowe A. Toward standards for posture: postural characteristics of the lower back system in normal and pathologic conditions. Spine (Phila Pa 1976) 1985;10:83–87. [PubMed] [Google Scholar]
- 36. Nourbakhsh MR, Arab AM. Relationship between mechanical factors and incidence of low back pain. J Orthop Sports Phys Ther 2002;32:447–460. [DOI] [PubMed] [Google Scholar]
- 37. Walker ML, Rothstein JM, Finucane SD, Lamb RL. Relationships between lumbar lordosis, pelvic tilt, and abdominal muscle performance. Phys Ther 1987;67:512–516. [DOI] [PubMed] [Google Scholar]
- 38. Youdas JW, Garrett TR, Harmsen S, Suman VJ, Carey JR. Lumbar lordosis and pelvic inclination of asymptomatic adults. Phys Ther 1996;76:1066–1081. [DOI] [PubMed] [Google Scholar]
- 39. Heino JG, Godges JJ, Carter CL. Relationship between hip extension range of motion and postural alignment. J Orthop Sports Phys Ther 1990;12:243–247. [DOI] [PubMed] [Google Scholar]
- 40. Youdas JW, Garrett TR, Egan KS, Therneau TM. Lumbar lordosis and pelvic inclination in adults with chronic low back pain. Phys Ther 2000;80:261–275. [PubMed] [Google Scholar]
- 41. Borghuis J, Hof AL, Lemmink KA. The importance of sensory-motor control in providing core stability: implications for measurement and training. Sports Med 2008;38:893–916. [DOI] [PubMed] [Google Scholar]
- 42. Ludwig O, Frohlich M, Schmitt E. Therapy of poor posture in adolescents: sensorimotor training increases the effectiveness of strength training to reduce increased anterior pelvic tilt. Cogent Med 2016;3:1262094. [Google Scholar]
- 43. Legaye J, Duval-Beaupere G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 1998;7:99–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 2005;30:346–353. [DOI] [PubMed] [Google Scholar]