Abstract
Background and Aims:
Several regional anaesthesia techniques have been described for carcinoma of the breast surgeries in the past but all of them failed to provide adequate surgical anaesthesia and are associated with multiple complications, thus limiting their use. This prospective study was designed to assess the efficacy of erector spinae plane (ESP) block to provide complete surgical anaesthesia without general anaesthesia (GA) and postoperative analgesia in patients undergoing modified radical mastectomy (MRM) surgery.
Methods:
Thirty females of the American Society of Anaesthesiologists physical status I, II or III scheduled for MRM were included in the study to receive unilateral ultrasound-guided ESP block preoperatively (25 ml of 0.5% bupivacaine with dexamethasone 8 mg on the operating side). The primary objective of the study was to evaluate the efficacy of ESP block to provide complete surgical anaesthesia in terms of total number of cases converted to GA.
Results:
Our study shows that ultrasound-guided single-shot ESP block provided complete surgical anaesthesia in all the patients within an average of 31.50 minutes and an average long-lasting postoperative analgesia of 41.73 hours following MRM.
Conclusion:
Our study proves that ESP block is a novel, predictable, secure, and safe option for carcinoma of the breast surgery. Thus, ESP block would surely provide a clinical advantage in these population group.
Key words: Carcinoma of the breast, erector spinae plane block, general anaesthesia, modified radical mastectomy
INTRODUCTION
Owing to the high incidence of breast carcinoma, modified radical mastectomy (MRM) had become one of the most common surgeries. Postmastectomy pain syndrome (PMPS) is a complex disorder associated with MRM which limits the normal functionality and affect the overall quality of life.[1]
Various regional anaesthesia techniques have been described for postoperative pain relief after mastectomy, for example, thoracic epidural anaesthesia,[2] intercostal nerve block, paravertebral block,[3] serratus anterior plane block, and pectoral nerve I and II blocks.[4] All of them offer satisfactory pain relief after mastectomy.
A novel para-spinal regional anaesthesia technique of erector spinae plane block, first described by Mauricio Forero et al., promises to provide effective visceral as well as somatic analgesia after carcinoma of the breast surgeries.[5]
The primary outcome measure of the present prospective study was to evaluate the efficacy of ultrasound-guided ESP block to provide complete surgical anaesthesia without general anaesthesia (GA) in patients undergoing MRM. The efficacy of the technique was assessed in terms of total number of cases converted to GA. The secondary outcome measures were the average duration to perform block procedure, to achieve complete surgical anaesthesia, the average patients' and surgeons' satisfaction score, the average time duration to administer first postoperative analgesia (rescue analgesia), the average total dose requirement of analgesic in the first 48 hours after surgery and the severity of postoperative pain via visual analogue scale (VAS) score.
METHODS
The ethical approval for this study was provided by the Institutional Ethics Committee at Mahatma Gandhi Medical College & Hospital (Jaipur, Rajasthan; reference number MGMCH/IEC/JPR/2018/16). The study was registered prospectively with the Clinical Trials Registry- India (www.ctri.nic.in) with registration no.: CTRI/2018/12/016492, and conducted in accordance with the Declaration of Helsinki.
Thirty female patients of age 25–65 years with American Society of Anaesthesiologists physical status I, II or III scheduled for MRM from December 2018 to May 2019 were included in the study after obtaining informed and written consent. The study was conducted in the oncology operation theatre of a single, tertiary-care medical centre under the supervision of an experienced anaesthesiologist.
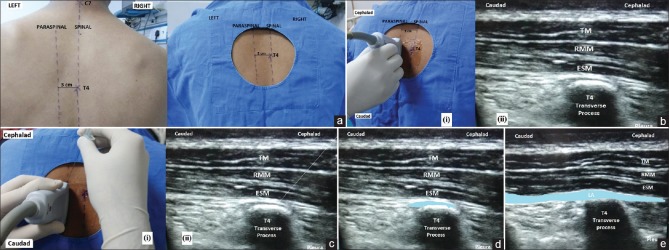
All patients underwent a preoperative assessment on the day and received 40 mg pantoprazole peroral 2 hours before surgery. An 18-gauge intravenous cannula was secured in the nonoperative-side hand or arm along with routine monitoring (electrocardiogram, oxygen saturation and non-invasive blood pressure) in the procedure room. Fentanyl 1 mcg/kg was intravenously administered. With the patient in the sitting position, the spine was palpated from the seventh cervical spinous process (C7) downward to the thoracic fourth spinous process (T4) and the point was marked [Figure 1a]. Thereafter, under all aseptic precautions, a linear array (6–13 MHz) transducer probe of ultrasonography machine (FUJIFILM Sonosite, Inc. Bothell, Washington) was placed 3 cm lateral to the T4 spinous process on the operating side to visualise and identify trapezius, rhomboid major and erector spinae muscle from outward [Figure 1b]. A 21-gauge spinal needle was inserted in the plane cranial to caudal till the tip of the needle reached into the fascial plane between the erector spinae muscle and transverse process [Figure 1c]. The position of the needle tip was confirmed by hydrodissection with 2 ml normal saline [Figure 1d]; thereafter, a total of 25 ml 0.5% bupivacaine with dexamethasone 8 mg was injected with intermittent aspiration. The spread of injectate in both cranial and caudal directions was seen on ultrasound [Figure 1e].
Figure 1.
(a): Landmark for erector spinae plane block. (Original image), C7: Seventh cervical spinous process, T4: Fourth thoracic spinous process, (b): (i) Orientation of ultrasonographic transducer probe for imaging of sonoanatomy of erector spinae plane block. (Original image), (ii) Ultrasonographic anatomy for erector spinae plane block. (Original image), TM: Trapezius muscle, RMM: Rhomboid major muscle, ESM: Erector spinae muscle, (c): (i) Orientation of block needle (in plane cranial to caudal) for erector spinae plane block. (Original image), (ii) Ultrasonographic image showing needle position into the fascial plane between erector spinae muscle and fourth thoracic transverse spinous process. (Original image), TM: Trapezius muscle, RMM: Rhomboid major muscle, ESM: Erector spinae muscle, (d): Ultrasonographic post-hydrodissection image of erector spinae plane block. (Original image), TM: Trapezius muscle, RMM: Rhomboid major muscle, ESM: Erector spinae muscle, and blue coloured area: Deposition site of normal saline for hydrodissection, (e): Ultrasonographic postinjection image of erector spinae plane block. (Original image), TM: Trapezius muscle, RMM: Rhomboid major muscle, ESM: Erector spinae muscle, LA: Local anaesthetic drug, and blue coloured area: spread of local anaesthetic in both cranial and caudal directions
After the completion of block procedure, the patients were made to lie supine with all the monitoring connected and were observed for 40 minutes post-performance of the block in the procedure room for the onset of loss of pin–prick sensation. The levels of the sensory dermatomes T1 to T8 were checked with pin–prick sensation by a blinded investigator every 5 minutes in terms of the total number of dermatomes with less pain or no pain to pin–prick in comparison to the opposite side. While achievement of loss of sensation to pin–prick in T1 to T8 within 40 minutes post block performance was considered as a successful block, the inability to achieve loss of pin–prick sensation in T1 to T8 up to 40 minutes post block performance was considered as a criteria of block failure and those patients were converted to general anaesthesia (GA).
The patients' heart rate, mean blood pressure and SpO2 were monitored every 5 min for 40 minutes after block performance.
After 40 minutes, patients with complete surgical anaesthesia, i.e., loss of pin–prick sensation from T1 to T8 on the operating side were shifted to the operating room. Routine monitoring (electrocardiogram, oxygen saturation and non-invasive blood pressure) was connected. A minute before the first surgical incision, intravenous bolus dose of fentanyl 1 mcg/kg was given and intravenous propofol infusion was started to titrated between 25 mcg/kg/min to 75 mcg/kg/min to maintain moderate sedation[6] (a state where patients were responding to verbal commands, either alone or accompanied by light tactile stimulation) with oxygen supplementation with nasal prongs at the rate of 4 litres per minute. Propofol infusion was continued till the beginning of closure of the skin incision and oxygen supplementation with nasal prongs was discontinued after application of the last suture.
Intraoperative heart rate and mean blood pressure were monitored continuously; >20% increment in heart rate and mean blood pressure demanded an increase in propofol infusion rate in an incremental dose of 10 mcg/kg/min from the baseline. If at any point, the propofol infusion rate exceeded 75 mcg/kg/min, the procedure was considered as block failure and was converted to GA.
An experienced anaesthesiologist vigilantly supervised and observed the patients' level of sedation in terms of response to verbal commands, either alone or accompanied by light tactile stimulation throughout the surgery. Measures to prevent airway compromise were kept ready (such as appropriate sized nasopharyngeal airway and laryngeal mask airway). Any incidence of airway compromise within the allowed limit of sedation (i.e., propofol infusion rate up to 75 mcg/kg/min) was recorded and treated timely with either an appropriate sized nasopharyngeal airway or laryngeal mask airway; depending upon the level of airway compromise.
In cases of block failure, either due to the inability to achieve the loss of pin–prick sensation from T1 to T8 on the operating side within 40 minutes of block performance or intraoperative propofol infusion rate exceeding 75 mcg/kg/min at any time; backup anaesthesia technique in terms of GA would have been used. The general anaesthesia would have been administered as per standard departmental protocol. The following parameters were noted during the study:
-
Efficacy of ESP block to provide complete surgical anaesthesia:
Complete surgical anaesthesia was considered when the following criteria were fulfilled:
- Achievement of loss of sensation to pin–prick in T1 to T8 within 40 minutes post block performance considering the completion of block procedure, i.e., point of visualisation of the spread of local anaesthetic agent ultrasonographically into the fascial plane between erector spinae muscle and transverse process as 'time 0'
- Intraoperative propofol infusion rate equal to or below 75 mcg/kg/min throughout the surgery (1 minute before the first surgical incision to the application of the first suture).
-
Average duration to perform block:
Time taken from point of visualisation and identification of trapezius, rhomboid major and erector spinae muscle at T4 spinous process to the point of visualisation of the spread of local anaesthetic agent ultrasonographically into the fascial plane between erector spinae muscle and transverse process.
-
Average duration to achieve surgical anaesthesia:
Achievement of loss of sensation to pin–prick in T1 to T8 on the operating side post block performance considering the completion of block procedure as 'time 0'.
-
Intraoperative parameters:
Heart rate, mean blood pressure and any complications (hypotension, vascular puncture or local anaesthetic toxicity) were observed.
-
The severity of postoperative pain:
The intensity of postoperative pain was recorded for all the patients using visual analogue scale (VAS) score (0 = no pain and 100 = worst possible pain) both at rest and on the movement of the ipsilateral upper limb at various predetermined time intervals considering the time of last suture application as 'time 0'. (0, 0.5, 1, 1.5, 2, 3, 6, 12, 18, 24, 30, 36, 42, 48h).
-
Average time duration to administer first postoperative analgesia (rescue analgesia):
It was noted, considering the time of last suture application as the reference point (time 0). Rescue analgesia (tramadol 100 mg) was considered in when VAS ≥40.
Average total number of the dose of analgesic (tramadol 100 mg) requirement in the first 48 hours after surgery.
-
Average patient's satisfaction:
Satisfaction related to block performance, postoperative pain relief, postoperative physiotherapy and limb movement were assessed by an 11-point satisfaction score (0 = unsatisfied and 10 = most satisfied).[7]
-
Average Surgeon's satisfaction:
Satisfaction related to intraoperative surgical anaesthesia, haemodynamic stability, and postoperative analgesia was assessed by an 11-point satisfaction score (0 = unsatisfied and 10 = most satisfied).[7]
This study was time-bound and had to be completed within a period of 6 months, between December 2018 and May 2019. Hence, all the patients fulfilling the inclusion criteria and scheduled for MRM from December 2018 to May 2019 were enrolled in our study, which was a total of 30 patients. Thus, a sample size of 30 patients was obtained for this study.
Statistical analysis was performed using SPSS for Windows (Version 16.0, 2007; SPSS Inc, Chicago, IL, USA). All the values are presented as mean ± standard error mean (mean ± SE) or numbers.
RESULTS
A total of 30 patients were included in the study. No patients were excluded in the follow-up period; hence, 30 patients were included in the final analysis as shown in the consort diagram [Figure 2]. The demographic data of all the patients included in the study were comparable [Table 1].
Figure 2.
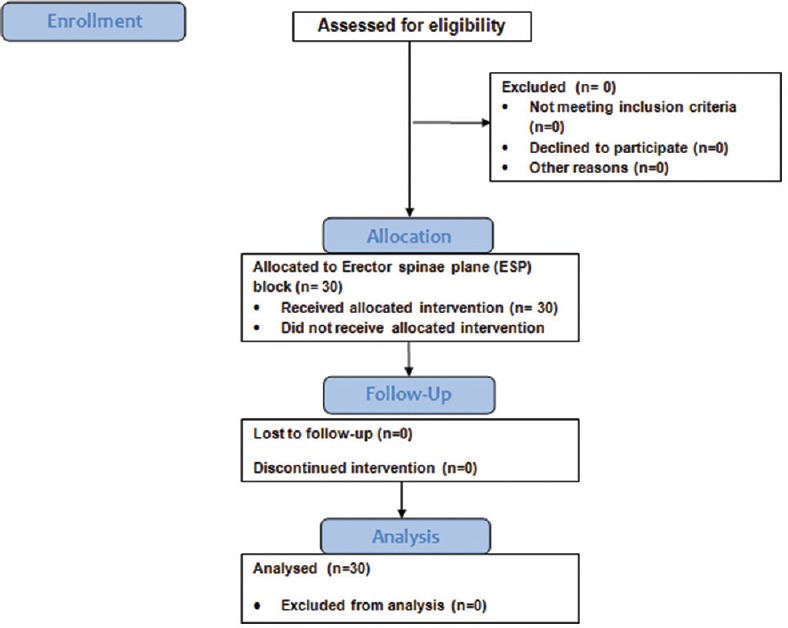
Consort flow diagram. ESP: Erector spinae plane
Table 1.
Demographic and other data
| Demographic data | Mean | SD | Range |
|---|---|---|---|
| Age (Yrs) | 46.67 | 6.81 | 36-60 |
| Height (cm) | 160.43 | 2.48 | 156-164 |
| Weight (kg) | 62.90 | 2.96 | 56-68 |
| Values are mean±SD | |||
There were no significant differences among all the patients in terms of intraoperative heart rate and mean blood pressure. There were no episodes of airway compromise or any other complications (hypotension, vascular puncture or local anaesthetic toxicity) secondary to the performance of the block in any patient.
As per the primary outcome measure, all patients (100%) included in the study achieved complete surgical anaesthesia and, thus, no case was converted to GA.
As per the secondary outcome measures, the average duration to perform block procedure was 8.93 minutes; average duration to achieve complete surgical anaesthesia was 31.50 minutes; average time to administer first postoperative analgesia (rescue analgesia) was 41.73 hours; average total number of dose of analgesic requirement in the first 48 hours was 1; average patient satisfaction score was 8.8 and the average surgeon satisfaction score was 9.4.
All the 30 patients showed significantly low VAS score, both at rest [Table 2a] and movement of the ipsilateral arm [Table 2b] when assessed for severity of postoperative pain at various predetermined time intervals for up to 48 hours.
Table 2.
(a): VAS at rest, (b): VAS at movement of ipsilateral arm
| (a): VAS at rest | ||||
|---|---|---|---|---|
| S. No. | Time Interval* | Mean | Median | SD |
| 1. | 0 h | 0.00 | 0.00 | 0.00 |
| 2. | 0.5 h | 0.00 | 0.00 | 0.00 |
| 3. | 1 h | 0.00 | 0.00 | 0.00 |
| 4. | 1.5 h | 0.00 | 0.00 | 0.00 |
| 5. | 2 h | 0.00 | 0.00 | 0.00 |
| 6. | 3 h | 0.00 | 0.00 | 0.00 |
| 7. | 6 h | 0.00 | 0.00 | 0.00 |
| 8. | 12 h | 0.00 | 0.00 | 0.00 |
| 9. | 18 h | 1.67 | 0.00 | 3.79 |
| 10. | 24 h | 7.67 | 10.00 | 4.30 |
| 11. | 30 h | 7.67 | 10.00 | 4.30 |
| 12. | 36 h | 10.00 | 10.00 | 0.00 |
| 13. | 42 h | 10.00 | 10.00 | 0.00 |
| 14. | 48 h | 10.00 | 10.00 | 0.00 |
| (b): VAS at movement of ipsilateral arm | ||||
| 1. | 0 h | 0.00 | 0.00 | 0.00 |
| 2. | 0.5 h | 0.00 | 0.00 | 0.00 |
| 3. | 1 h | 0.00 | 0.00 | 0.00 |
| 4. | 1.5 h | 0.00 | 0.00 | 0.00 |
| 5. | 2 h | 0.00 | 0.00 | 0.00 |
| 6. | 3 h | 0.00 | 0.00 | 0.00 |
| 7. | 6 h | 1.33 | 0.00 | 3.46 |
| 8. | 12 h | 1.67 | 0.00 | 3.79 |
| 9. | 18 h | 10.00 | 10.00 | 0.00 |
| 10. | 24 h | 10.67 | 10.00 | 2.54 |
| 11. | 30 h | 13.67 | 10.00 | 5.56 |
| 12. | 36 h | 21.00 | 20.00 | 7.12 |
| 13. | 42 h | 27.67 | 20.00 | 9.35 |
| 14. | 48 h | 21.67 | 20.00 | 6.99 |
Values are mean±SD. *Time interval was noted considering the time of last suture application as ‘Time 0’. Visual analogue score (VAS) (0=no pain and 100=worst possible pain)
DISCUSSION
One in every eight women develop carcinoma of the breast during their lifetime as per the carcinoma of female breast statistics.[8] Modified radical mastectomy (MRM), the most common surgical procedure for carcinoma of the breast is associated with severe postoperative pain which results in negative psychological and physiological consequences. Therefore, various regional analgesic techniques have been developed for postoperative pain relief; however, all of them have several limitations; for example, thoracic epidural anaesthesia is technically challenging,[2] thoracic paravertebral block is frequently associated with complications like accidental pneumothorax, vascular puncture[3], risk of sympathetic blockade,[9] pectoral blocks and serratus anterior plane blocks cause intercostobrachial and supraclavicular nerves sparing with disruption of surgical planes.[10]
Mauricio Forero et al. described a comparatively safe and simple technique of ESP block[5,11,12] with an effect profile comparable to that of retrolaminar and paravertebral blocks.[13,14,15]
In this prospective study of 30 patients, preoperative ultrasound-guided ESP block was given to female patients scheduled to undergo MRM surgery with an aim to evaluate the efficacy of ESP block to provide complete surgical anaesthesia with postoperative analgesia. Our study result shows attainment of surgical anaesthesia in 100% cases within an average time duration of 31.50 minutes, with long-lasting postoperative analgesia (average 41.73 hours) and significant patient as well as surgeon satisfaction score without any complications.
Swati Singh et al.,[16] conducted a study on 40 patients undergoing MRM surgery to evaluate the postoperative analgesic efficacy of ESP block for up to 24 hours and observed that only 3 out of 20 patients in the ESP block group required supplemental morphine as compared to the control group in which all patients required supplemental morphine; none of the patients in our study group required rescue analgesia in the first 24 hours. Furthermore, in our study, 25 out of 30 patients required only a single dose of analgesic (tramadol 100 mg) in the next 24 hours.
Gurkan et al.,[17] in their study observed 65% reduction in total morphine consumption at 24 hours with single-shot ultrasound-guided ESP block which was statistically significant, thus concluding that ESP block has an effective postoperative opioid-sparing profile. Nair et al.,[18] in a case series of five patients also reported the same opioid-sparing analgesic profile of ESP block. Similar opioid-sparing profile was validated with our results.
Moreover, these results were comparable with the results of our study as minimal postoperative analgesics in terms of an average single dose of rescue analgesia required over 48 hours.
Most of the studies regarding ESP block described its perioperative analgesic efficacy but Kimachi et al.,[19] reported a case where ESP block provided effective and complete surgical anaesthesia in a patient with high cardiovascular risk. They accomplished complete surgical anaesthesia with ESP block in 20 minutes with patients reporting no pain and showing haemodynamic stability throughout the 2.5-hour surgical procedure for unilateral mastectomy with axillary dissection. This was further validated with our study as the average time required for observation of complete surgical anaesthesia with ESP block in all 30 patients included in our study was 31.50 minutes with same haemodynamic stability throughout the surgery and adequate postoperative analgesia assessed by VAS score for up to 48 hours.
The reason for such extensive anaesthesia and prolonged analgesia can possibly be due to the profound craniocaudal spread of local anaesthetic to the intercostal spaces, epidural and neural foraminal[20] and attainment of a paravertebral coverage of three and four vertebral levels both cranially as well as caudally blocking both the ventral and dorsal branches of the spinal nerves[21,22] along with the communicating branches augmenting the sympathetic chain which contributes to sympathetic block[23] and to extensive somatic and visceral analgesia. In addition, median and lateral pectoral nerves which are thought to be responsible for post-mastectomy pain syndrome are not blocked by ESP block, if performed at a lower thoracic level (T5 or below). But, ESP block performed at T2 or T3 blocks the C5 and C6 nerve roots and thereby blocks the suprascapular nerve, along with the axillary and lateral pectoral nerves.[24] We performed the ESP block at the T4 level using 25 ml of local anaesthetic drug and achieved adequate surgical anaesthesia and it might be possible that our selection of a higher injection point (level above T5, i.e., T4) and injection of high volume of drug might possibly have lead to blockage of lateral pectoral nerve along with the ventral and dorsal branches of the spinal nerves with adjoining communicating branches of the sympathetic chain. However, a contrast study after the injection of a contrasting agent at T4 would be appropriate to further validate these claims.
Besides, there are other advantages of ESP block which make it a rather easy, safe and effective option to any other regional technique of pain relief. First, the ease of block performance due to the ultrasonographic target—the transverse process. Second, safe block performance as the point of injection represented by a musculofascial plane is distant from the adjoining structures, i.e., pleura, neuroaxis and large vascular structures.[23] Thirdly, the extent of erector spinae muscle which stretches through the cervical, thoracic and lumbar areas contributing to the multiple dermatomal anaesthesia of the concerned side even with a single unilateral injection of 20–30 mL in adults.[25]
Thus, ESP block can be an answer to the clinicians seeking simple, safe and effective regional anaesthesia technique[26] for surgical anaesthesia as well as postoperative analgesia in breast surgery.
CONCLUSION
Our study shows that ultrasound-guided single-shot ESP block at the level of the fourth thoracic vertebra is a feasible option for breast surgeries as it provides complete surgical anaesthesia and adequate postoperative analgesia. Thus, ESP block can provide a clinical advantage in these patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Fecho K, Miller N, Merritt S, Klauber-Demore N, Hultman C, Blau WS. Acute and persistent postoperative pain after breast surgery. Pain Med. 2009;10:708–15. doi: 10.1111/j.1526-4637.2009.00611.x. [DOI] [PubMed] [Google Scholar]
- 2.Doss NW, Ipe J, Crimi T, Rajpal S, Cohen S, Fogler RJ, et al. Continous thoracic epidural anaesthesia with 0.2% ropivacaine versus general anaesthesia for perioperative management of modified rad cal mastectomy. Anesth Analg. 2001;92:1552–7. doi: 10.1097/00000539-200106000-00041. [DOI] [PubMed] [Google Scholar]
- 3.Schnabel A, Reichl SU, Kranke P, Pogatzki-Zahn EM, Zahn PK. Efficacy and safety of paravertebral blocks in breast surgery: A meta-analysis of randomized controlled trials. Br J Anaesth. 2010;105:842–52. doi: 10.1093/bja/aeq265. [DOI] [PubMed] [Google Scholar]
- 4.Blanco R. The 'pecs block': A novel technique for providing analgesia after breast surgery. Anesthesia. 2011;66:847–8. doi: 10.1111/j.1365-2044.2011.06838.x. [DOI] [PubMed] [Google Scholar]
- 5.Singh S, Chowdhary NK. Erector spinae plane block an effective block for post-operative analgesia in modified radical mastectomy. Indian J Anaesth. 2018;62:142–50. doi: 10.4103/ija.IJA_726_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miller RD, Eriksson LI, Fleischer LA, Wiener-Kronish JP, Young WL, editors. Miller's Anesthesia. 7th ed. Philadelphia: Churchill Livingstone; 2010. pp. 719–68. [Google Scholar]
- 7.Subramanian B, Shastri N, Aziz L, Gopinath R, Karlekar A, Mehta Y, et al. ASSIST-.Patient satisfaction survey in postoperative pain management from Indian subcontinent. J Anaesthesiol Clin Pharmacol. 2017;33:40–7. doi: 10.4103/joacp.JOACP_245_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DeSantis C, Ma J, Bryan L, Jemal A. Breast cancer statistics, 2013. CA Cancer J Clin. 2014;64:52–62. doi: 10.3322/caac.21203. [DOI] [PubMed] [Google Scholar]
- 9.Garg R, Bhan S, Vig S. Newer regional analgesia interventions (fascial plane blocks) for breast surgeries: Review of literature. Indian J Anaesth. 2018;62:254–62. doi: 10.4103/ija.IJA_46_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Woodworth GE, Ivie RM, Nelson SM, Walker CM, Maniker RB. Perioperative breast analgesia: A qualitative review of anatomy and regional techniques. Reg Anesth Pain Med. 2017;42:609–31. doi: 10.1097/AAP.0000000000000641. [DOI] [PubMed] [Google Scholar]
- 11.Finneran JJ, Gabriel RA, Khatibi B. Erector spinae plane block provide analgesia for breast and axillary surgery: A series of 3 cases. Reg Anaesth Pain Med. 2018;43:101–2. doi: 10.1097/AAP.0000000000000695. [DOI] [PubMed] [Google Scholar]
- 12.Bonivini D, Tagliapietra L, Giacomazzi A, Pizzirani E. Bilateral ultrasound-guided erector spinae plane blocks in breast cancer and reconstruction surgery. J Clin Anaesth. 2018;44:3–4. doi: 10.1016/j.jclinane.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 13.Bonvinci D, Tagliapietra L, Giacomazzi A, Pizzirani E. Bilateral ultrasound-guided erector spinae plane blocks in breast cancer and reconstruction surgery. J Clin Anesth. 2017;44:13–4. doi: 10.1016/j.jclinane.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 14.Murouchi T. Consideration of block nomenclature: Erector spinae plane block or retrolaminar block? Reg Anesth Pain Med. 2017;42:124. doi: 10.1097/AAP.0000000000000525. [DOI] [PubMed] [Google Scholar]
- 15.Ueshima H, Otake H. Similarities between the retrolaminar and erector spinae plane blocks. Reg Anesth Pain Med. 2017;42:1234. doi: 10.1097/AAP.0000000000000526. [DOI] [PubMed] [Google Scholar]
- 16.Singh S, Kumar G, Akhileshwar Ultrasound-guided erector spinae plane block for postoperative analgesia in modified radical mastectomy: A randomized control study. Indian J Anaesth. 2019;63:200–4. doi: 10.4103/ija.IJA_758_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gurkan Y, Aksu C, Kuş A, Yörükoǧlu UH, Kılıç CT. Ultrasound guided erector spinae plane block reduces postoperative opioid consumption following breast surgery: A randomized controlled study. J Clin Anesth. 2018;50:65–8. doi: 10.1016/j.jclinane.2018.06.033. [DOI] [PubMed] [Google Scholar]
- 18.Nair AS, Seelam S, Naik V, Rayani BK. Opioid-free mastectomy in combination with ultrasound - Guided erector spinae block: A series of five cases. Indian J Anaesth. 2018;62:632–4. doi: 10.4103/ija.IJA_314_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kimachi PP, Martins EG, Peng P, Forero M. The erector spinae plane block provides complete surgical anesthesia in breast surgery: A case report. A A Pract. 2018;11:186–8. doi: 10.1213/XAA.0000000000000777. [DOI] [PubMed] [Google Scholar]
- 20.Adhikary SD, Bernard S, Lopez H, Chin KJ. Erector spinae plane block versus retrolaminar block: A Magnetic resonance imaging and anatomical study. Reg Anesth Pain Med. 2018;43:756–62. doi: 10.1097/AAP.0000000000000798. [DOI] [PubMed] [Google Scholar]
- 21.Hannig KE, Jessen C, Soni UK, Borglum J, Bendtsen TF. Erector spinae plane block for elective laparoscopic cholecystectomy in the ambulatory surgical setting. Case Rep Anesthesiol. 2018;2018:5492527. doi: 10.1155/2018/5492527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: A novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41:621–7. doi: 10.1097/AAP.0000000000000451. [DOI] [PubMed] [Google Scholar]
- 23.Chin KJ, Malhas L, Perlas A. The erector spinae plane block provides visceral abdominal analgesia in bariatric surgery: A report of 3 cases. Reg Anesth Pain Med. 2017;42:372–6. doi: 10.1097/AAP.0000000000000581. [DOI] [PubMed] [Google Scholar]
- 24.Forero M, Rajarathinam M, Adhikary SD, Chin KJ. Erector spinae plane block for the management of chronic shoulder pain: A case report. Can J Anaesth. 2018;65:288–93. doi: 10.1007/s12630-017-1010-1. [DOI] [PubMed] [Google Scholar]
- 25.Aksu C, Gurkan Y. Ultrasound-guided bilateral erector spinae block could provide effective postoperative analgesia in laparoscopic cholecystectomy in paediatric patients. Anesth Crit Care Pain Med. 2019;38:87–8. doi: 10.1016/j.accpm.2018.03.008. [DOI] [PubMed] [Google Scholar]
- 26.Garg R. Regional block: Walking away from central to peripheral nerves and planes for local anaesthetic drug deposition. Indian J Anaesth. 2019;63:517–9. doi: 10.4103/ija.IJA_495_19. [DOI] [PMC free article] [PubMed] [Google Scholar]