Abstract
Background:
Death and dying care is an area with less attention in nursing. This even is evidenced as more challenging in some populations such as neonates. Neonatal intensive care unit (NICU) nurses should be aware of the quality of care they provide for dying neonates and their families to find the areas which need attention.
Objective:
The aim of this study was to assess the psychometric features of the Quality of Dying and Death (QODD) questionnaire in NICU nurses in Tehran, the capital city of Iran.
Methods:
This methodological study was conducted in 2017. For this purpose, using census method, 130 NICU nurses working in selected hospitals participated. After the backward–forward translation, based on the method proposed by the International Test Commission, the psychometric properties of the Persian QODD were examined through the assessment of the face, content and construct validity, internal consistency, and stability.
Results:
Final Persian QODD's content and face validity were accepted through a qualitative method. In the confirmatory factor analysis, the original version of QODD was not confirmed. Subsequently, an exploratory factor analysis was carried out in which phrases were included in three dimensions (symptom control, preparation for death of neonate, and professional attention) that explained 75% of the variance. Cronbach's alpha values ranged from 0.82 to 0.88 for these three dimensions. The intraclass correlation coefficient (ICC) was ICC = 0.94 between two tests performed with a 2-week interval on twenty eligible nurses.
Conclusions:
The Persian version of QODD has acceptable psychometric properties in nurses working with the neonatal population and can be used to investigate the NICU nurses' opinion on the QODD provided in NICU patients.
Keywords: Death, intensive care units, neonatal, psychometrics
INTRODUCTION
Nowadays, a large number of neonates with congenital anomalies, prematurity, and other health-threatening conditions survive because of progress in the management of deliveries, initial resuscitation, technologies, and knowledge provided in neonatal intensive care units (NICUs).[1,2] Despite the improvements in life-saving technology and skills of health-care providers, infant's death has the highest percentage of deaths in the pediatric population.[3] The mortality rate of neonates in Iran was estimated 12.5% in 2014 which most of them occurred in the hospitals (93.8%).[4]
When death is inevitable for an infant, a situation free of pain and suffering becomes a goal.[5] Evidences show that neonatal death happens in painful and distressed conditions because of many factors such as lack of protocols for end of life care of infants, lack of knowledge of staff, and or their ignorance.[3] Currently, the concept of good death for hospitalized patients is an issue of increasing interest in the medical literature. The nature of good death for a neonate in NICU would be different from those in other age groups. Therefore, there is little about what it means a good death for a neonate in the NICU.[3,5]
A good death is defined as “being free from avoidable suffering and pain for patients, families and caregivers; and consistent reasonable with cultural, ethical, and clinical standards according with wishes of dying persons and families,” according to the Institute of Medicine.[6] They may take some days to be completed a dying process and ended up to death. For parents of an infant, this process is distressing, as they feel unable to stop their infant's suffering.[7]
Quality of death is a personal evaluation of the experience of the process of dying. The assessment of this concept provides health-care providers more knowledge about specific needs of a population in this regard.[5,7] For qualified and humanistic care and given that provision, peaceful death is a responsibility of health-care team,[6] it is needed to improve the quality of death in all patients in any age group.[3] The assessment of quality of death is influenced by many factors, such as the age group of patients, their sociocultural context, and the nature of the diseases.[8,9] Furthermore, it is needed to consider this fact that in many cases, it is not possible to assess the patient's experience of the dying process after death. Hence, assessments are more focused on perceived attitudes of patient's significant others or caregivers about this process using indirect surveys.[8]
There is limited evidence available on measuring the quality of death in Persian culture and also in NICUs from the point of view of nurses. We selected one of the widely studied tools with the best coverage of psychometric properties, the Quality of Dying and Death Questionnaire (QODD).[10,11,12] The QODD first was developed to assess the quality of dying process from the perspectives family members of died person.[13] Compromising 31 items, the QODD concerns the last days of patient's life and cover six conceptual domains of symptoms, preparation for death, family issues, treatment preference, concerns of patient, and moment of death.[14,15] A modified 14-items form of the QODD was developed to evaluate caregivers' perspectives.[16] Each item is composed of two questions. The first asks the nurse to remember how or whether the patient experienced a symptom such as pain (it is needed to remember one of or the closest patient's death). Then, it is asked to rate how terrible/wonderful the experience was for the patient in an 11-point scale (0–10). Higher total score indicates better quality of death and dying.[17]
In several studies, its good content, construct validity, reliability, and internal consistency were reported.[9,13,14,18,19,20,21] It has been tested in deaths happen in community, hospice, and intensive care units of adults. In addition, the tool has been translated to some other languages for being used in different countries.[8,9,13,21]
The aim of this study was to provide a cross-cultural and age-related adaptation and a psychometric validation of the QODD for the Persian population of nurses in NICUs.
METHODS
The design and participants
This is a methodological study in which the QODD was translated, and its Persian version was validated in NICU nurses in 2017. Using a census method, the enrolled participants were 130 nurses working in NICUs of selected hospitals affiliated to Shahid Beheshti University of Medical Sciences, including Mofid, Maydiyeh, Imam Hossein, Taleghani, and Shohada-e Tajrish. The total number of nurses was 145. The inclusion criteria were being worked in NICU for more than 6 months. Fifteen nurses did not match the criteria.
Translation, cross-cultural, and age-related adaptation
The first researcher obtained permission from the developer through E-mail in March 2017. The translation process was carried out using a method proposed by the International Testing Commission.[22] First, QODD was separately translated into Persian by two experts in English. A panel, including experts in palliative care (n = 2), pediatric palliative care (n = 2), psychologists (n = 2), and neonatal physicians (n = 2) with certified English skill, then evaluated the two preliminary Persian tool, made a consensus, to create a single version. In the next stage, the final translated version was translated back to English by two other separate translators. The produced versions were compared to the original version by the second researcher and the panel of experts. The panelists also had modified items to be suitable for the population of infants in NICUs. The final back-translated version was confirmed by the developer of the questionnaire. The produced Persian QODD then distributed among six eligible nurses to obtain their opinion about the comprehensibility of the items[22,23] [Figure 1].
Figure 1.
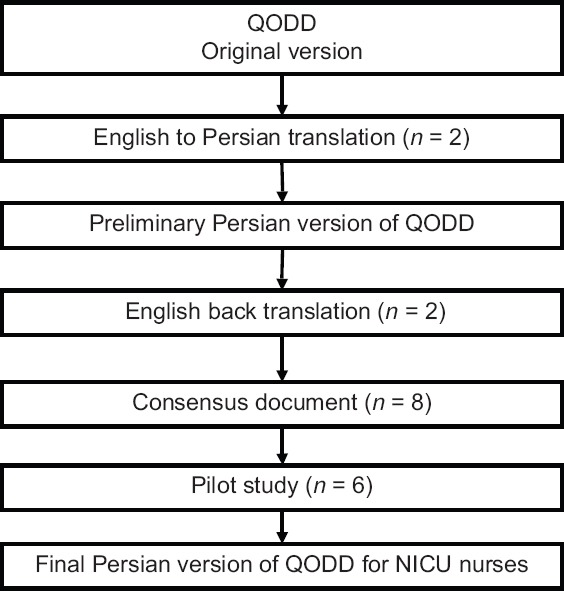
Flowchart of the translation of the Quality of Dying and Death from English to Persian.
Data collection
Two self-administered questionnaire, namely the Persian QODD and the demographic questionnaire were distributed among 130 nurses working in NICUs from June to September of 2017. All the questionnaires were completed by nurses in about 20–30 min, in total.
Data analysis
To ensure the clarity of the items and the assessment of the content validity, the opinions of eight panelists (the same experts mentioned above for the translation phase) were sought.
In order to evaluate the construct validity of the QODD and the fit of the model, confirmatory factor analysis was conducted using LISREL software version 8.5 (Scientific Software International, Chicago, IL, USA).[24] This technique is used to determine the goodness of fit between the obtained data of research and a theoretical model.[25] In this study, goodness-of-fit (GFI), comparative fit index, adjusted GFI, root mean square error of approximation, and normed fit index, as Chi-square GFI indices were used.[26]
Due to the lack of fit with the Iranian NICU nurses, to extract the dimensions, the exploratory factor analysis (EFA) was conducted. The adequacy of sampling was assessed with the Kaiser-Meyer-Olkin (KMO) index and the feasibility of the factor analysis with Bartlett's test.[27] For EFA, two criteria were considered to accept a factor. One, the factors with eigenvalues more than 1.0. Two, the factors with two or more items loading at a significant level (attributing an item to a given factor when the factor loading ≥ 0.45).[26] Furthermore, for the simplification and interpretability of the factor construct, the varimax rotation was used [Table 1].[25]
Table 1.
Fitting indices of Persian Quality of Dying and Death in Iranian neonatal intensive care unit nurses
| GFI indices | The results in the present study | Acceptable amounts |
|---|---|---|
| χ2 (df), P | 7.24 | <3 |
| GFI | 0.64 | >0.9 |
| CFI | 0.86 | >0.9 |
| AGFI | 0.050 | >0.9 |
| RMSEA | 0.22 | <0.08 |
| NFI | 0.84 | >0.9 |
GFI: Goodness-of-fit, CFI: Comparative fit index, AGFI: Adjusted GFI, RMSEA: Root mean square error of approximation, NFI: Normed fit index
Cronbach's alpha was used to assess the internal consistency of the questionnaire.[28] To measure the stability of the tool, twenty nurses were asked to fill out the Persian QODD for the second time after 2 weeks. Using intraclass correlation coefficient (ICC), test-retest reliability was tested.[26] Data were analyzed using Statistical Package for the Social Sciences (SPSS Version 15.0 [SPSS Inc., Chicago, IL, USA]).
Ethical consideration
The University Ethics Committee had approved the study and its process (IR.sbmuritec.rec. 1395.583). All participants were informed about the aims of the study and their role. Written informed consent was obtained from all of them. The anonymous of the given information was assured.
RESULTS
Of 145 nurses working in the NICUs of the selected hospitals, a total of 130 nurses (100% of eligible nurses) completely filled out the questionnaire. All the nurses were females and 99 (76.1%) had bachelor degree in nursing. The mean age of the nurses was 34.2 (standard deviation = 2.3). Details of demographic characteristics are shown in Table 2.
Table 2.
Some demographic characteristics of neonatal intensive care unit nurses (n=130)
| n (%) | |
|---|---|
| Marital state | |
| Married | 49 (37.7) |
| Single | 70 (53.9) |
| Divorced | 11 (8.4) |
| Education | |
| Bachelor degree | 99 (76.1) |
| Master degree | 29 (22.4) |
| PhD (not nursing) | 2 (1.5) |
| Clinical experience (years) | |
| <2 | 18 (13.8) |
| 3-5 | 49 (37.7) |
| 6-10 | 33 (25.4) |
| 10-15 | 30 (23.1) |
| Experience in NICU (years) | |
| <2 | 24 (18.5) |
| 3-5 | 47 (36.2) |
| 6-10 | 32 (24.6) |
| 10-15 | 27 (20.7) |
NICU: Neonatal intensive care unit
In the translation, one of the items (having one or more visits from a religious or spiritual advisor) was removed according to the experts' comments and permission of the developer, as it was not compatible with the settings of this population. Furthermore, all the comments were modified to be compatible with the age of patients who were neonates so that the term neonate was used instead of patient in all items and the term parents was used instead of the family members. Hence, the qualitative content and face validity were confirmed.
To extract the potential factors, an EFA was used. The results of KMO test for sampling adequacy was 0.77; the acceptable amount is when more than 0.7. To determine whether the obtained correlation matrix is significantly different from zero and to justify the factor analysis accordingly, the Bartlett test was used from which 1642.543 was obtained (P < 0.001). Then, after calculating the correlation matrix between variables, factors were extracted. The minimum factor loading of the present study was taken as 0.45. The factor analysis resulted in a three-factor model using the eigenvalue. The three factors had special value above, expressing 75.19% of the variance in total. Table 3 shows the factor loadings of each of the components on the three recognized factors with varimax rotation. Table 4 reports the indices of EFA of Persian QODD. The dimensions were named as “Symptom control,” “Preparation for death of neonate,” and “Professional attention” based on the nature of the items in each subscale. Factor loadings for items 4 and 5 were loaded on factors one and three. This issue was fixed, taking into account the content of each item and thus items were loaded on the first factor three. The factor loads obtained for all the items ranged between 0.52 and 0.88, suggesting the appropriateness of the structure of the Persian QODD.
Table 3.
Factor structure resulted from exploratory factor analysis of Persian Quality of Dying and Death with varimax rotation (n=130), (the items of the back translated to English is shown here)
| Items | Symptom control | Professional attention | Preparation for death of neonate |
|---|---|---|---|
| 1. The neonate’s pain was under control | 0.84 | ||
| 2. The neonate had control on him/her | 0.75 | ||
| 3. The neonate breath comfortably | 0.74 | ||
| 4. The dignity of the neonate was kept | 0.69 | 0.62 | |
| 5. The neonate’s parents spent their time with him/her | 0.60 | 0.56 | |
| 6. The neonate’s siblings spent their time with him/her | 0.52 | ||
| 7. The neonate’s relatives spent their time with him/her | 0.56 | ||
| 8. The neonate was touched or hugged by people who loved him/her | 0.88 | ||
| 9. The predeath religious or spiritual practices were performed for the neonate and his/her family | 0.88 | ||
| 10. The neonate’s parents were there when he/she died | 0.76 | ||
| 11. The quality of neonate’s state was rated at the time of death | 0.84 | ||
| 12. The neonate experienced mechanical ventilation | 0.85 | ||
| 13. The neonate received the right amount of sedation | 0.74 |
Table 4.
Extracted factors, eigenvalues, percentage variances, and cumulative percentage of Persian Quality of Dying and Death
| Factor | Initial eigenvalues | Extraction sums of squared loadings | ||||
|---|---|---|---|---|---|---|
| Total | Percentage variance | Cumulative percentage | Total | Percentage variance | Cumulative percentage | |
| 1 | 7.27 | 55.94 | 55.94 | 3.71 | 28.60 | 28.60 |
| 2 | 1.48 | 11.33 | 67.37 | 3.16 | 24.36 | 52.96 |
| 3 | 1.01 | 7.81 | 75.19 | 2.88 | 22.22 | 75.19 |
Internal consistency and interclass correlations
Cronbach's alpha coefficient of the Persian three-dimensional version of the QODD was measured to calculate the internal consistency which was 0.84. In addition, coefficients of Cronbach's alpha for all three subscales were upper than 0.7. Using the one-way random effect model, the ICC was also calculated. The “Symptom control” and “Preparation for death of neonate” had the highest (0.88) and lowest (0.82) levels of correlation, respectively [Table 5].
Table 5.
Cronbach’s alpha and intraclass correlation coefficient amounts for Quality of Dying and Death-Persian and its subscales
| Domains | Number of items | Cronbach’s alpha | ICC | P |
|---|---|---|---|---|
| Symptom control | 3 | 0.83 | 0.91 | 0.000 |
| Preparation for death of the neonate | 6 | 0.88 | 0.94 | 0.000 |
| Professional attention | 4 | 0.82 | 0.99 | 0.000 |
| Total | 13 | 0.84 | 0.94 | 0.000 |
ICC: Intraclass correlation coefficient
DISCUSSION
This was the first study that shows psychometric properties of a Persian version of the most known tool for assessing the quality of death and dying, QODD. This tool has versions for both family members and caregivers. In this study, the 14-item versions adopted for intensive care unit caregivers, to assess their opinion about the quality of death and dying of their patients, was translated and validated for nurses who work in NICUs.
The Persian version of the QODD used for NICU nurses was translated through a rigorous method and was approved by the questionnaire developers. The questionnaire was acceptable to almost all the participants. The translation led to minimal cultural adaption and only one item was removed in this regard. The German version of the 27-items version of the tool also showed minimal cultural adaptation.[21] Furthermore, the tool showed well content validity in some other cultures.[17,29] In the present study, the only issue in the translation phase was where it became clear that it was difficult to find Persian equivalents that can clearly explain the concepts of understanding pain, being aware of what is going on, and spending time with parents, siblings, relatives, and the like. As a result, after the pretest phase in the translation process, the research team and translators changed the phrases and compiled the final translation. Researchers in another study on the German population also encountered the same problem in translation and cultural adaptation of the Questionnaire in German, who changed the translation in such a way that these concepts would not change.[30]
The results showed that the questionnaire is a reliable and valid tool that can be used in measuring the concept of quality of death and dying of neonates from their nurses' perspective. The results also can be used for cross-cultural comparisons. Similarly, the validity of QODD for family member's version of the tool is well documented.
The results of the coefficients of Cronbach's alpha showed that QODD-Persian has an acceptable internal consistency (α = 0.84) means that the items of the tool have congruence and consistency. Acceptable values range from 0.70 to 0.95.[31] The findings from a study on 252 family members who had lost one recently showed a good internal consistency for the QODD (α = 0.89).[13] Furthermore, the current form of 14-items for ICU nurses' version has showed good internal consistency in the study which in the format of the original version of QODD modified to be suitable for nurses who work in intensive care units (α =0.92).[16] In addition, the validity of the tool in some other cultures is evidenced. The findings of the study on the translation and validation of the QODD based on the results on 226 caregivers showed that it is applied in the German population.[30] Similarly, an α =0.88 in a study on 72 Spanish caregivers of adult cancer patients showed that its Spanish version has internal consistency.[8] Furthermore, in another study using 14-item version of the tool on the Spanish population, Cronbach's alpha >0.7 showed an acceptable validity.[17]
ICC was calculated for stability and test-retest reliability of the tool. Based on the 95% confident interval of the ICC estimate, value <0.5, between 0.5 and 0.75, between 0.75 and 0.9, and more than 0.90 are indicative of poor, moderate, good, and excellent reliability, respectively.[32] According to the results of this study, it can be said that ICC's values for the Persian version of QODD and its dimensions are acceptable. Reliability of the different version of the tool and its equivalent in some other languages are evidenced.[13,14,17,30,33]
The results of the present study indicated acceptable construct validity for 13-items Persian version of QODD modified by Hodde et al. (2004) using EFA and three dimensions were revealed for the questionnaire. The labels for dimensions were attributed according to the names of four dimensions of the version used by Doney et al. (2010) in family members' population of adult patients and the consensus between research team. Items 1–4 in the “Symptom control” dimension relate to pain relief and physical comfort. Items 5–9 in the third dimension named “Preparation of parents for death of neonate” relate to acts that prepare family members for the death of their neonate, and items 10–13 in the second dimension named “Professional attention” relate to the professional attention for a good death of the neonate. Cronbach's alpha coefficients for each of dimensions ranged between 0.82 and 0.88. Two dimensions of “Symptom control” and “Professionals attention” had a lower Cronbach's alpha compared to the “Preparation of parents for death of the neonate.” Considering the lower number of the items in theses subscales and the relationship of Cronbach's alpha coefficient with the number of items, it is expected that if the number of items in the two subscales increase, their alpha will increase. The ICC index for the first and third dimensions had the highest (0.997) and lowest (0.91) values, respectively. According to the values obtained with the required standards, the stability of the Persian version of QODD was desirable.
In general, the psychometric tests of the Persian version of 13-items QODD for caregivers showed satisfactory results. Principle component analysis with varimax rotation supported a three-factor structure for the instrument. The future studies could focus on other psychometric properties of the questionnaire and on different applications of it as it is the most known instrument to evaluate the quality of death and dying, which is a field with increasing interest in Iran.
CONCLUSIONS
In summary, this study showed that the three-factor Persian version of the QODD for nurses was acceptable in terms of psychometric properties. This tool can be used to measure the quality of death and dying for nurses and other professions related to hospitals and health centers. The tool is simple to use and can be completed by individuals in a short time.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The present article was extracted from the thesis written by the first author derived from her M. Sc. thesis in the intensive care unit nursing approved by the Research Vice-chancellor of Shahid Beheshti University of Medical Sciences, Tehran, Iran. The researchers are grateful to the participants recruiting in this study.
REFERENCES
- 1.Sabaghi S, Nourian M, Fallahi M, Nasiri M. Relationships between the duration of mechanical ventilation and its related factors in infants with respiratory distress syndrome in NICU. JHayat. 2016;21:93–102. [Google Scholar]
- 2.Kazemi A, Nikfarid L, Khanali Mojen L, Nasiri M. Obstacles to Parents' Interaction with Neonates in Neonatal Intensive Care Units from Parents' and Nurses' Points of View. Iran J Neonatol. 2019;10:78–85. [Google Scholar]
- 3.Brosig CL, Pierucci RL, Kupst MJ, Leuthner SR. Infant end-of-life care: The parents' perspective. J Perinatol. 2007;27:510–6. doi: 10.1038/sj.jp.7211755. [DOI] [PubMed] [Google Scholar]
- 4.Mojdeh B, Azam M, Asiyeh PY, Nasibeh R, Soheila M, Shirin S. Prevalence and causes of neonatal mortality in hormozgan province, Southern Iran. Int J Pediatrics. 2017;5:6047–8. [Google Scholar]
- 5.Brandon D, Docherty SL, Thorpe J. Infant and child deaths in acute care settings: Implications for palliative care. J Palliat Med. 2007;10:910–8. doi: 10.1089/jpm.2006.0236. [DOI] [PubMed] [Google Scholar]
- 6.Wool C, Kain VJ, Mendes J, Carter BS. Quality predictors of parental satisfaction after birth of infants with life-limiting conditions. Acta Paediatr. 2018;107:276–82. doi: 10.1111/apa.13980. [DOI] [PubMed] [Google Scholar]
- 7.Brooten D, Youngblut JM, Caicedo C, Del Moral T, Cantwell GP, Totapally B, et al. Parents' acute illnesses, hospitalizations, and medication changes during the difficult first year after infant or child NICU/PICU death. Am J Hosp Palliat Care. 2018;35:75–82. doi: 10.1177/1049909116678597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gutiérrez Sánchez D, Cuesta-Vargas AI. Cross-cultural adaptation and psychometric testing of the quality of dying and death questionnaire for the spanish population. Eur J Oncol Nurs. 2018;33:8–13. doi: 10.1016/j.ejon.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 9.Heckel M, Bussmann S, Stiel S, Ostgathe C, Weber M. Validation of the german version of the quality of dying and death questionnaire for health professionals. Am J Hosp Palliat Care. 2016;33:760–9. doi: 10.1177/1049909115606075. [DOI] [PubMed] [Google Scholar]
- 10.Hales S, Zimmermann C, Rodin G. Review: The quality of dying and death: A systematic review of measures. Palliat Med. 2010;24:127–44. doi: 10.1177/0269216309351783. [DOI] [PubMed] [Google Scholar]
- 11.Hales S, Chiu A, Husain A, Braun M, Rydall A, Gagliese L, et al. The quality of dying and death in cancer and its relationship to palliative care and place of death. J Pain Symptom Manage. 2014;48:839–51. doi: 10.1016/j.jpainsymman.2013.12.240. [DOI] [PubMed] [Google Scholar]
- 12.Mah K, Hales S, Weerakkody I, Liu L, Fernandes S, Rydall A, et al. Measuring the quality of dying and death in advanced cancer: Item characteristics and factor structure of the quality of dying and death questionnaire. Palliat Med. 2019;33:369–80. doi: 10.1177/0269216318819607. [DOI] [PubMed] [Google Scholar]
- 13.Curtis JR, Patrick DL, Engelberg RA, Norris K, Asp C, Byock I, et al. Ameasure of the quality of dying and death. Initial validation using after-death interviews with family members. J Pain Symptom Manage. 2002;24:17–31. doi: 10.1016/s0885-3924(02)00419-0. [DOI] [PubMed] [Google Scholar]
- 14.Mularski R, Curtis JR, Osborne M, Engelberg RA, Ganzini L. Agreement among family members in their assessment of the quality of dying and death. J Pain Symptom Manage. 2004;28:306–15. doi: 10.1016/j.jpainsymman.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 15.Mularski RA, Heine CE, Osborne ML, Ganzini L, Curtis JR. Quality of dying in the ICU: Ratings by family members. Chest. 2005;128:280–7. doi: 10.1378/chest.128.1.280. [DOI] [PubMed] [Google Scholar]
- 16.Hodde NM, Engelberg RA, Treece PD, Steinberg KP, Curtis JR. Factors associated with nurse assessment of the quality of dying and death in the intensive care unit. Crit Care Med. 2004;32:1648–53. doi: 10.1097/01.ccm.0000133018.60866.5f. [DOI] [PubMed] [Google Scholar]
- 17.Pérez-Cruz PE, Padilla Pérez O, Bonati P, Thomsen Parisi O, Tupper Satt L, Gonzalez Otaiza M, et al. Validation of the Spanish version of the quality of dying and death questionnaire (QODD-ESP) in a home-based cancer palliative care program and development of the QODD-ESP-12. J Pain Symptom Manage. 2017;53:1042–9e3. doi: 10.1016/j.jpainsymman.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 18.Smith KA, Goy ER, Harvath TA, Ganzini L. Quality of death and dying in patients who request physician-assisted death. J Palliat Med. 2011;14:445–50. doi: 10.1089/jpm.2010.0425. [DOI] [PubMed] [Google Scholar]
- 19.Steinhauser KE, Clipp EC, Tulsky JA. Evolution in measuring the quality of dying. J Palliat Med. 2002;5:407–14. doi: 10.1089/109662102320135298. [DOI] [PubMed] [Google Scholar]
- 20.Levy CR, Ely EW, Payne K, Engelberg RA, Patrick DL, Curtis JR, et al. Quality of dying and death in two medical ICUs: Perceptions of family and clinicians. Chest. 2005;127:1775–83. doi: 10.1378/chest.127.5.1775. [DOI] [PubMed] [Google Scholar]
- 21.Heckel M, Bussmann S, Stiel S, Weber M, Ostgathe C. Validation of the german version of the quality of dying and death questionnaire for informal caregivers (QODD-D-ang) J Pain Symptom Manage. 2015;50:402–13. doi: 10.1016/j.jpainsymman.2015.03.020. [DOI] [PubMed] [Google Scholar]
- 22.Muñiz J, Elosua P, Hambleton RK International Test Commission. International test commission guidelines for test translation and adaptation: Second edition. Psicothema. 2013;25:151–7. doi: 10.7334/psicothema2013.24. [DOI] [PubMed] [Google Scholar]
- 23.Eremenco SL, Cella D, Arnold BJ. A comprehensive method for the translation and cross-cultural validation of health status questionnaires. Eval Health Prof. 2005;28:212–32. doi: 10.1177/0163278705275342. [DOI] [PubMed] [Google Scholar]
- 24.Jöreskog KG, Sörbom D. LISREL 8: User's reference guide. Lincolnwood: Scientific Software International; 1996. [Google Scholar]
- 25.Tinsley HE, Brown SD, editors. Handbook of applied multivariate statistics and mathematical modeling. San Diego: Academic Press; 2000. [Google Scholar]
- 26.Kellar SP, Kelvin EA. Munro's statistical methods for health care research. Philadephia: Wolters Kluwer Health/Lippincott Williams and Wilkins; 2005. [Google Scholar]
- 27.Fabrigar LR, Wegener DT. Exploratory Factor Analysis. Oxford: Oxford University Press; 2011. [Google Scholar]
- 28.Bi J, Kuesten C. Intraclass correlation coefficient (ICC): A framework for monitoring and assessing performance of trained sensory panels and panelists. J Sensory Stud. 2012;27:352–64. [Google Scholar]
- 29.Braun M, Hasson-Ohayon I, Hales S, Zimmermann C, Rydall A, Peretz T, et al. Quality of dying and death with cancer in Israel. Support Care Cancer. 2014;22:1973–80. doi: 10.1007/s00520-014-2163-x. [DOI] [PubMed] [Google Scholar]
- 30.Heckel M, Bussmann S, Stiel S, Weber M, Ostgathe C. Validation of the German version of the quality of dying and death questionnaire for informal caregivers (QODD-D-Ang) J Pain Symptom Manag. 2015;50:402–14. doi: 10.1016/j.jpainsymman.2015.03.020. [DOI] [PubMed] [Google Scholar]
- 31.Cronbach LJ, Shavelson RJ. My current thoughts on coefficient alpha and successor procedures. Edu Psychol Meas. 2004;64:391–418. [Google Scholar]
- 32.Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–63. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mesukko J. Critical Care Nurses' Perceptions of Quality of Dying and Death, Barriers, and Facilitators to Providing Pediatric End-of-Life Care in Thailand. Case Western Reserve University; 2010. [Google Scholar]


