Abstract
Background
Prompted voiding is a behavioural therapy used mainly in North American nursing homes. It aims to improve bladder control for people with or without dementia using verbal prompts and positive reinforcement.
Objectives
To assess the effects of prompted voiding for the management of urinary incontinence in adults.
Search methods
We searched the Cochrane Incontinence Group Specialised Trials Register (searched 31 January 2006) and reference lists of relevant articles. We contacted investigators in the field to locate extra studies.
Selection criteria
All randomised or quasi‐randomised trials which addressed prompted voiding for the management of urinary incontinence. The trials included adult men and women, with or without cognitive impairment, diagnosed as having urinary incontinence as identified by the trialists, either by symptom classification or by urodynamic investigation.
Data collection and analysis
The identified reports were assessed for eligibility. Two reviewers independently reviewed the selected studies for methodological quality. Data describing six pre‐specified outcomes were extracted independently by each reviewer and consensus reached when there was disagreement. Trial investigators were consulted when clarification or further detail was required. A third reviewer was recruited to proof read the review at different stages.
Main results
Nine trials were included in the review. These involved 674 elderly people, the majority of whom were women. Prompted voiding was compared with no prompted voiding in nine trials. The limited evidence suggested that prompted voiding increased self‐initiated voiding and decreased incontinent episodes in the short‐term. There was no evidence about whether these effects are sustained over a long period of prompted voiding, or persist after stopping prompted voiding.
Authors' conclusions
There was insufficient evidence to reach firm conclusions for practice. There was suggestive evidence of short‐term benefit from prompted voiding, but longer‐term effects are not known, and prompted voiding has significant resource implications.
Plain language summary
Regular reminding to prompt going to the toilet for the management of urinary incontinence in adults
Urinary incontinence is very common amongst elderly long‐term residents of nursing homes or hospitals. Prompted voiding is a behavioural therapy used mainly in North American nursing homes. It aims to improve bladder control for people with or without dementia using verbal prompts and positive reinforcement. The review found that although there is suggestive evidence of short‐term benefit from prompted voiding, it is not known if these persist. Prompted voiding is also resource‐intensive for nursing staff. Prompted voiding can take up a lot of carers time and this hinders its wider use. There was no evidence about long‐term effects.
Background
Urinary incontinence is common amongst elderly long term residents of nursing homes or hospitals. Estimates of prevalence range between 31% to over 70% (Borrie 1992; Fonda 1990; Ouslander 1993; Ouslander 1995b; Schnelle 1995; Williams 1995). Reflecting this, urinary incontinence is costly to those providing care, estimated at approximately $3 million in North American institutions (Hu 1990) and up to £1.4 billion overall in the United Kingdom (Hu 2004; Roy 1997) and up to $19.5 billion overall in the United States (in year 2000). Behavioural interventions are often the first choice of treatment (Beckman 1995) especially in institutional care (Colling 1996). These include bladder re‐education programmes, such as prompted voiding, habit training, timed voiding and bladder training. The differences between these can be easily misunderstood.
Prompted voiding is used to teach people with or without cognitive impairment to initiate their own toileting through requests for help and positive reinforcement from carers when they do this (Button 1998; Kennedy 1992; Norton 1996; Palmer 2005). This is distinctive from some other therapies because of the participation of the individual in the process. In contrast, habit training (Colling 1992) attempts to determine the micturition pattern for an individual, which can then be used to achieve continence, but does not necessarily rely on the individual to participate. Timed toileting (Hadley 1986) is fixed by time or event, which is carer led and not individualised. Bladder training actively includes the individual in attempting to increase the interval between the desire to void and the actual void (Wallace 2004), and hence would not be suitable for those who are cognitively impaired.
Prompted voiding requires assisting a resident to walk, or be taken, to the toilet and is more labour intensive than practices that aim to suit available resources, such as changing protective pads after two or three incontinent episodes at the convenience of carers. It involves the education of both the person with incontinence and the staff, using a programme of scheduled voids that requires prompting from the caregiver (Pinkowski 1996). Implementing and maintaining prompted voiding therefore has resource implications (Pinkowski 1996). Commitment and motivation need to be coupled with increased staff time to enable implementation.
Prompted voiding is used in particular in North America, mainly in long term facilities for people with cognitive impairment or dementia. Most research on prompted voiding has been done by gerontologists in the USA, Schnelle in particular (Burgio 1994;Creason 1989; Hu 1989; Hu 1990; Ouslander 1995c; Schnelle 1989; Schnelle 1983; Surdy 1992). Some investigators have described the effects of introducing prompted voiding, others have compared prompted voiding with other therapies such as exercise (Schnelle 1995) and bladder relaxant drugs (Ouslander 1995a), and others have compared prompted voiding plus an exercise programme against no intervention. Although much of this work suggests that prompted voiding is useful, methodological weaknesses are common. They include the lack of appropriate control groups, the use of research staff to implement the intervention, and the short term perspective taken.
Objectives
To determine the effects of prompted voiding for the management of urinary incontinence.
The following hypotheses were addressed:
1. Prompted voiding is better than no prompted voiding for the management of urinary incontinence. 2. Prompted voiding is better than other treatments for the management of urinary incontinence.
3. Prompted voiding in combination with another therapy is better than that therapy alone.
Methods
Criteria for considering studies for this review
Types of studies
Randomised or quasi randomised trials of prompted voiding for the management of urinary incontinence.
Types of participants
Adult men and women with or without cognitive impairment diagnosed as having urinary incontinence, as defined by the trialists, either by symptom classification or by urodynamic study.
Types of interventions
(a) Prompted voiding compared with no prompted voiding (b) Prompted voiding compared with other treatments (c) Prompted voiding combined with another treatment compared with that other treatment
Types of outcome measures
A. Patient symptoms
1. No improvement of wet episodes 2. Self initiated episodes of toileting in 24 hours (as indicated from completed bladder charts) 3. Pad changes in 24 hours (as indicated from completed bladder charts, total number and mean) 4. Number of incontinent episodes in 24 hours (as indicated from completed bladder charts, total number and mean)
B. Health Status Measures
For example Activities of Daily Living (eg Katz ADL (Burgio 1994))
C. Health Economic Measures
D. Other outcomes
Non pre‐specified outcomes judged important when performing the review
Search methods for identification of studies
This review has drawn on the search strategy developed for the Incontinence Group as a whole. Relevant trials have been primarily identified from the Cochrane Incontinence Group Specialised Trials Register. The methods used to derive this, including the search strategy, are described under the Group's details in The Cochrane Library (For more details please see the ‘Specialized Register’ section of the Group’s module in The Cochrane Library). The register contains trials identified from MEDLINE, CINAHL and the Cochrane Central Register of Controlled Trials (CENTRAL) and hand searching of journals and conference proceedings.
The Incontinence Group Trials Register was searched using the Group's own keyword system. The search terms used were:
{design.rct* or design.cct*} AND {TOPIC.URINE.INCON*} AND {INTVENT.PSYCH.promptedVoid*} (All searches were of the keyword field of Reference Manager 9.5 N, ISI ResearchSoft). Date of the most recent search of the register for this review: 31 January 2006. The trials in the Incontinence Group Specialised Register are also contained in CENTRAL.
The following additional searches were conducted for this review:
We checked all reference lists of identified trials and other relevant articles. We contacted authors and trialists in the field to identify any additional or unpublished studies or data.
We did not impose any language or other limits on the searches.
Data collection and analysis
The methodological quality of the included studies was assessed using the Cochrane Incontinence Group's criteria, which are described in the Cochrane Library. These are based on the assumption that the avoidance of bias is best achieved by secure concealment of random allocation prior to formal entry; few and identifiable withdrawals and dropouts; and analysis on an intention to treat basis. Of the trials included, none fulfilled all the criteria for good methodological quality. Quality assessment was performed by all three reviewers (SE, BR, JP) with a consensus reached through discussion. Two reviewers independently performed data extraction. Any discrepancies were discussed until agreement was reached. Authors of trial reports were consulted where clarification was necessary. Trial data were analysed using the Cochrane software, Review Manager, and processed as described in the Cochrane Collaboration Handbook (Deeks 2005). Studies were excluded from the review if they were not randomised or quasi‐randomised trials, or if they made comparisons other than those pre‐specified. Excluded studies are listed with reasons for their exclusion.
Results
Description of studies
Nine trials involving 674 participants (Engberg 2002; Hu 1989; Linn 1995; Ouslander 2005; Schnelle 1983; Schnelle 1989; Schnelle 2003; Surdy 1992; Smith 1992) compared prompted voiding against no prompted voiding and were included in the review. In one of these (Ouslander 2005) prompted voiding was a part of a wider intervention that included exercise tanning. There was one cross over trial (Ouslander 1995a) which compared prompted voiding combined with another therapy (Oxybutinin) versus prompted voiding alone, which was excluded because both groups received prompted voiding. Three of the included trials (Hu 1989; Schnelle 1989; Ouslander 2005) have also been reported in supplementary papers. These additional papers were treated in the same way as the original papers in order to extract more complete data. See Table of Included Studies.
Women predominated in most trials. However there were more men in Ouslander 2005 (97 out of 107) and two trials (Schnelle 2003; Smith 1992) do not report gender (n=46). The average age was 84 years. One trial (Linn 1995) did not report age. All but three trials (Ouslander 2005; Schnelle 1983; Schnelle 2003) performed urological assessment on the participants at baseline. A baseline period was included in all the trials, ranging from two days to six months, although Linn (Linn 1995) does not report the duration of baseline. The duration of the interventions ranged from 20 days to 32 weeks. Linn and Hu et al (Hu 1989; Linn 1995) reported a follow‐up period of 12 and 22 weeks respectively, whereas the other studies did not address longer term effects. The investigators in the majority of each trials applied analysis of variance (ANOVA) to the data, with the addition of t tests in Ouslander (Ouslander 2005), Hu et al (Hu 1989) and Engberg (Engberg 2002). Research assistants were utilised to perform the intervention within four of the trials (Hu 1989; Ouslander 2005; Schnelle 1989; Schnelle 2003). The investigators of the other trials (Engberg 2002; Linn 1995; Surdy 1992; Schnelle 1983; Smith 1992) used the regular nursing assistant staff or informal caregivers to implement the intervention. The studies were conducted in the main during daytime hours, from 7am to 7 or 9pm, except for Surdy (Surdy 1992) who used a 24 hour schedule, but participants were not disturbed unless they were awake.
All but two trials (Linn 1995; Schnelle 1983) reported the average scores for the Mini‐Mental State Examination (MMSE range 0 to 30, the lower the score, the greater the cognitive impairment). Linn (Linn 1995) used the Dementia Rating Scale (DRS) but did not include any data on this. Schnelle (Schnelle 1983) noted that 95% of the sample had senile dementia or organic brain syndrome. In the Surdy trial (Surdy 1992) the intervention group had an average score of 14, whereas the control group scored an average of 11. Schnelle et al (Schnelle 1989) reported an average score of eight, with 25% having no score at all. Thirty percent of participants were ambulant.
In respect of functional ability, six trials reported details. Surdy (Surdy 1992) did not include any profile, whereas Hu et al (Hu 1989) used the Katz Activities of Daily Living tool. He reported a high dependency for both treatment and control groups (average score for treatment was 5.1 and for control was 5.5; range 0 to 6 with the higher score being the most dependent). In Schnelle's (Schnelle 1983) trial he reports that none of the sample were independent in toileting or ambulation. Only two participants assist with transferring from a commode to the chair and vice versa. In the later trial, Schnelle (Schnelle 1989) reported that 11% of his sample could independently ambulate (14 subjects out of a sample of 126).
Risk of bias in included studies
1. Potential for selection bias at trial entry
All nine studies stated that the order of treatment had been randomly allocated. However, the method of random allocation was not described for six trials (Hu 1989; Linn 1995; Schnelle 1983; Schnelle 1989; Smith 1992; Surdy 1992). It was not initially possible to assess whether randomisation was concealed before allocation to groups as the details provided were insufficient. However, following consultation with the main investigators from five of the studies (Hu 1989; Linn 1995; Schnelle 1983; Schnelle 1989; Smith 1992), more detail on the randomisation process was obtained. Random number tables were used in three trials (Hu 1989; Linn 1995;Schnelle 1989) and three used computerised programs (Engberg 2002; Ouslander 2005; Schnelle 2003) for sequence generation, but it is not clear whether the allocation was concealed up to the time of formal entry.
2. Potential for bias at time of treatment or outcome assessment
Blinding of the research staff who completed standardised assessments was included within two studies (Schnelle 2003; Ouslander 2005), but there was no reporting of this for the other studies. 'Blinding' of the intervention is not possible for a behavioural therapy such as prompted voiding.
3. Potential for bias in trial analysis
Seven studies mentioned the numbers and reasons for withdrawals or dropouts (Engberg 2002; Hu 1989; Ouslander 2005; Schnelle 1983; Schnelle 1989; Schnelle 2003; Surdy 1992). One study had an attrition of three participants, but did not include any detail (Linn 1995) and Smith's study (Smith 1992) did not have any withdrawals or dropouts.
Effects of interventions
1. Prompted voiding versus no prompted voiding
All nine trials compared prompted voiding with no prompted voiding (Engberg 2002; Hu 1989; Linn 1995; Ouslander 2005; Schnelle 1983; Schnelle 1989; Schnelle 2003; Smith 1992; Surdy 1992)
Numbers with no improvement of wet episodes: Data were available for one trial (Hu 1989) involving a total of 65 participants in the treatment group and 68 in the control group. This favoured prompted voiding although the difference was not statistically significant.
Proportion of hourly checks that were wet: Six trials (Engberg 2002; Ouslander 2005; Schnelle 1983; Schnelle 2003; Smith 1992; Surdy 1992) reported data describing the proportion of hourly checks that were wet. Only two of these provided summary data as means and standard deviations (Engberg 2002; Schnelle 2003). Schnelle (Schnelle 2003) showed a significantly lower proportion in the prompted voiding group (mean difference 12.00%; 95% CI ‐18.79% to ‐5.21%). Engberg (Engberg 2002) compared groups in terms of the change from baseline to follow‐up in the mean proportion of hourly checks that were wet. The change was higher in the prompted voiding group, but this difference was not statistically significant (17.60; 95% CI ‐14.58 to 49.78). In the other four trials, the data were reported as means without standard deviation (Smith 1992; Schnelle 2003; Surdy 1992) or as medians (Ouslander 1995a). (Other data table 01.03). All four showed lower proportions in the prompted voiding group. Ouslander (Ouslander 2005), for example reported data before the groups crossed over, which found that wet checks reduced from a median of 54% to 25% in the immediate intervention group. The control group increased wet episodes from 41% to 50%.
Incontinent episodes in 24 hours: Hu (Hu 1989) and Schnelle (Schnelle 1989) both found a decrease in the number of incontinent episodes per day in the prompted voiding group and the pooled result was statistically significant (WMD ‐0.92; CI 95% ‐1.32 to ‐0.53). However this is largely due to a relatively large estimated effect in the Schnelle trial (Schnelle 1989), and this is reflected in the significant chi square test of heterogeneity (Chi‐square 18.07; df=1; p<0.01), I2 = 94.5%.
Other trials reported this outcome measure, in a way that could not be included in the meta‐analysis. Engberg (Engberg 2002) reported that the treatment group reduced incontinent episodes by 60% compared with 37% in the control group. Smith (Smith 1992) found that the treatment group reduced incontinence from 80% to 20%, whereas the control group almost remained the same. Similarly, Linn (Linn 1995) found treatment group improvement during the intervention in that the incontinence reduced from 42% at baseline to 17% following treatment. Pad changes in 24 hours: No trial reported details of pad changes in 24 hours.
Self‐initiated toileting: Only one trial reported data suitable for analysis in Review Manager for this outcome. Schnelle (Schnelle 1989) found a statistically significant increase in independent requests for the toilet as a result of the intervention (comparison 01.07: Mean difference per day ‐1.9; 95% CI ‐1.51 to ‐2.29). The baseline frequency of requesting the toilet was 4.5 times per 12 hours on a one hour prompted voiding schedule and 2.8 times per 12 hours on a two hour prompted voiding schedule (time cost = 17 minutes per subject). Hu et al (Hu 1989) also addressed this outcome measure, but the data could not be included in the meta‐analysis as no standard deviations were available. However, the treatment group reported a mean of 2.65 per day versus 1.12 requests per day in the controls for the last four weeks of the treatment period. Schnelle (Schnelle 1983) reported that the number of requests for toileting increased from 0.31 per day in the treatment group to an average of twice per day as opposed to the control group which decreased to 0.23 per day. Engberg (Engberg 2002) reported that the number of self‐initiated toilets increased from a baseline of 2.0 to 3.3 after treatment. Likewise, Linn (Linn 1995) found that requests for toileting assistance increased in the treatment group from an average of 0.38 per day to 2.3. The control group did not show such changes.
Health status measures: No analysis could be applied to the types of data presented by the investigators related to health status.
Health economic measures:
Cost data were reported for two trials, Surdy (Surdy 1992) and Hu et al (Hu 1989). Hu et al (Hu 1989) reported the cost of implementing a prompted voiding schedule as being equal to one hour of time per patient per day. Surdy (Surdy 1992) estimated the cost of implementation to be US $8.51 for a patient receiving prompted voiding but this was associated with a reduction in other costs of US $23.57.
2. Prompted voiding versus other treatments
No trials addressed this comparison.
3. Prompted voiding combined with another treatment versus that treatment alone
No trials addressed this comparison.
Discussion
This review has examined the evidence for the effectiveness of prompted voiding in the management of urinary incontinence in adults. The few data that are available suggest that prompted voiding appears promising for the management of urinary incontinence in the elderly.
Because the Cochrane search strategy is tried and tested, there is some confidence that all the relevant trials have been identified. Published data have been relied upon and the problems associated with depending on aggregate data for analysis have probably weakened the results. For instance, it has not been possible to calculate and analyse the times to specific events reliably. Also checking and correcting data is limited, essentially there is an element of trust needed when extracting the data. We struggled for example to interpret data within Schnelle's trial (Schnelle 1989), as assumptions had to be made that there must have been a typological error, so that sense could be made of the data.
Although literature searching has been extensive, only fourteen trials were identified that met the inclusion criteria. These trials involved physically and cognitively impaired adults aged over sixty five years, mostly female, who had urinary incontinence.
The nine trials that were included in the review, were of modest methodological quality, with minimal confirmation of allocation concealment and lack of blinding. Wet checks were used as an outcome measure for most of the trials, for which the method was not clearly described. However, checking varied between hourly or two‐hourly. It has been suggested that the greater the number of wet checks performed, the greater would be the reliability for the actual number of wet episodes (Fonda 1998). Important limitations of the included trials involves the overall small sample size (n=674 completed the trials). In most studies, withdrawal due to dropout or death was not clearly identified or if these events were trial‐related. Prompted voiding has been argued as particularly suitable for a US nursing home population (Ouslander 1995a; Schnelle 1989), so caution may need to be applied to generalising the results outside the settings of the trials. Other limitations were the questions addressed by eligible trials and the limited reporting. The trials that examined prompted voiding alone were of varying treatment duration and intensity (Engberg 2002; Hu 1989; Linn 1995; Schnelle 1989; Schnelle 1983; Smith 1992; Surdy 1992). These issues affect the interpretation, but are not directly relevant to the internal validity.
In respect of short‐term effectiveness there is an apparently consistent effect across two trials (Hu 1989; Schnelle 1983) suggesting improvement of incontinence as a result of prompted voiding.
External validity has been weakened due to the use of research staff to implement the intervention in four of the trials (Hu 1989; Ouslander 2005; Schnelle 1989; Schnelle 2003). The other trials have demonstrated that it is possible to use direct caregivers during the trial period (Engberg 2002; Linn 1995; Smith 1992; Surdy 1992; Schnelle 1983). Reliability checks were performed for the wet checks in seven trials, which may be partly responsible for the compliance of staff with the programme. Two trials did not report reliability checks (Linn 1995; Smith 1992). Without robust trials that address these issues, our understanding of the factors that influence the successful management of urinary incontinence will remain unclear. Nevertheless, these trials are important for exposing the multidimensional aspects of managing incontinence in a frail, elderly population. Therefore, this work adds to the literature on behavioural treatment of urinary incontinence, but the body of knowledge remains incomplete, especially within the nursing home environment.
A specific consequence to be expected from prompted voiding therapy is an increase in self‐initiated toileting: as a result of operant conditioning (Grosicki 1968). The five trials that report this outcome all show increased rates in the prompted voiding group. However, only one of these (Schnelle 1989) provides a measure of dispersion (S.D.), and in this trial the difference is highly statistically significant. However, a concern with this therapy is the possibility that patients become dependent on the caregiver is a concern with this therapy, especially as success can be related to the frequency of prompts, be it hourly, two or three hourly. The intensity of the intervention has varied among the trials and therefore it is difficult to make predictions about which frequency is most effective.
Longer‐term outcomes have not been measured. This raises questions about the feasibility of maintaining the therapy. Indeed, the compliance of both patient and caregiver may be undermined over time, as the client group studied are not likely to improve cognitively or physically. It also leaves unaddressed the question of whether any effects would persist after prompted voiding is withdrawn.
Two trial reports indicate that there is increased time and cost associated with implementing prompted voiding (Surdy 1992; Hu 1989) but this may be more than offset by subsequent savings. Ouslander (Ouslander 2005) reports that improving continence care as a result of their intervention is four times more costly than regular care. Implementation may be an issue of reallocation of resources, however, such that staff who currently use pads to 'take care of the problem' become motivated and committed to prompted voiding. Nevertheless, the balance between costs and benefits cannot be defined on the basis of the data currently available.
The nursing home environment and the attitudes of staff are likely to impact on the patients' ability to maintain continence on admission and these are issues that deserve investigation. Jirovec and Wells (Jirovec 1990) advocate attention to mobility, as reduced mobility has a profound effect on the ability to remain continent, especially in a nursing home, where reliance on staff to keep the patient dry is necessary. Perhaps this partially explains why prompted voiding might be effective, because of the key elements of prompting memory and prompting the patient to walk (Schnelle 1983). Therefore, it could be argued that although predicting the onset of urinary incontinence is not difficult, finding the resources to enable an individualised approach is more problematical.
The review did provide some evidence that those with a higher cognitive ability (Hu 1989; Surdy 1992), higher dependency (Hu 1989) and normal cystometry are more likely to benefit. Selecting appropriate patients will require caregivers to be aware of the factors influencing urinary incontinence. Furthermore, there are educational and training needs of caregivers if patients are to have a chance to reduce the degree of urinary incontinence. The applicability of the prompted voiding has, so far, not been tested outside US settings. Decisions about the transferability of findings need to consider the characteristics of the client group and the circumstances in which they are being nursed.
Every effort has been made to make this review trustworthy. It is possible that more data might have become available if there had been more active dialogue with the trialists. This might have influenced the interpretation of the results. Collecting individual patient data would have been useful and therefore more reliable, but due to the resource intensity and time anticipated for this, it was not pursued.
Authors' conclusions
Implications for practice.
While a prompted voiding therapy appears promising as a form of care for the management of urinary incontinence as opposed to no prompted voiding, there is insufficient evidence to reach firm conclusions for practice. There is suggestive short‐term benefits from prompted voiding. But there are significant resource implications of prompted voiding, although the size of these is not clear from the trials studied within this review.
Implications for research.
Perhaps the main value of the review is as a guide to future priorities for research. Larger well conducted trials are needed, with a longer term follow up if prompted voiding is to have a secure place within care settings as an effective adjunct to continence care for a frail, elderly population. Outcome measures need further definition and validated tools will increase the robustness of future studies. Evaluation in wider settings outside the USA would enhance generalisability.
Tackling the factors that influence urinary incontinence before it happens is also a major area for further research. Prevention and early identification are likely to be key to reducing the impact of incontinence.
What's new
| Date | Event | Description |
|---|---|---|
| 9 October 2008 | Amended | Converted to new review format. |
History
Protocol first published: Issue 2, 1999 Review first published: Issue 2, 2000
| Date | Event | Description |
|---|---|---|
| 26 January 2006 | New search has been performed | five studies were added: Engberg 2002; Linn 95; Ouslander 2005; Schnelle 2003; Smith 92 |
| 26 February 2002 | New search has been performed | minor update |
| 23 February 2000 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
We thank the members of the Editorial team in Aberdeen, who have been inspirational, and particular thanks goes to Adrian Grant, Cathryn Glazener and June Cody for their time, patience and generous hospitality. Gratitude is extended to Dr Ouslander, Dr Schnelle, Dr Engberg, Dr Hu, Dr Linn, Dr Smith and Dr Jirovec for their time and attention to requests for information.
Data and analyses
Comparison 1. PROMPTED VOIDING vs NO PROMPTED VOIDING.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of people with no improvement in wet episodes | 1 | 133 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.60 [0.29, 1.26] |
| 2 Mean proportion of hourly checks that are wet | 1 | 147 | Mean Difference (IV, Fixed, 95% CI) | ‐12.0 [‐18.79, ‐5.21] |
| 3 Mean or median of proportion of hourly checks that are wet | Other data | No numeric data | ||
| 4 Change in mean proportion of hourly checks that are wet | 1 | 19 | Mean Difference (IV, Fixed, 95% CI) | 17.6 [‐14.58, 49.78] |
| 5 Incontinent episodes in 24 hours | 2 | 257 | Mean Difference (IV, Fixed, 95% CI) | ‐0.92 [‐1.32, ‐0.53] |
| 6 Pad changes in 24 hours | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Self‐initiated toileting | 1 | 126 | Mean Difference (IV, Fixed, 95% CI) | ‐1.90 [‐2.29, ‐1.51] |
| 8 Health Status Measures | 0 | 0 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Health Economic Measures | 0 | 0 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
1.1. Analysis.
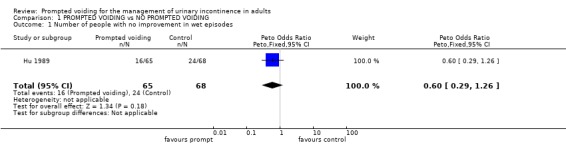
Comparison 1 PROMPTED VOIDING vs NO PROMPTED VOIDING, Outcome 1 Number of people with no improvement in wet episodes.
1.2. Analysis.
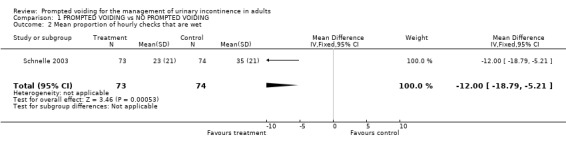
Comparison 1 PROMPTED VOIDING vs NO PROMPTED VOIDING, Outcome 2 Mean proportion of hourly checks that are wet.
1.3. Analysis.
Comparison 1 PROMPTED VOIDING vs NO PROMPTED VOIDING, Outcome 3 Mean or median of proportion of hourly checks that are wet.
| Mean or median of proportion of hourly checks that are wet | ||
|---|---|---|
| Study | Treatment | Control |
| Ouslander 2005 | treatment n = 35 median no. of wet checks 25% | control = 43 median no. of wet checks 50% |
| Schnelle 1983 | treatment n = 5 mean wet checks 15% | control n = 4 mean wet checks 25.5% |
| Smith 1992 | treatment n = 10 mean wet checks 21% | control n = 10 mean wet checks 85% |
| Surdy 1992 | treatment n = 6 mean wet checks 13.25% | control n = 6 mean wet checks 45.95% |
1.4. Analysis.
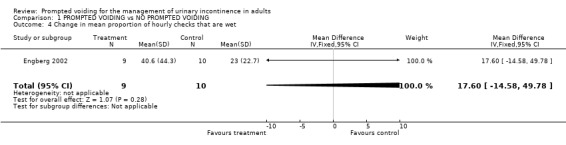
Comparison 1 PROMPTED VOIDING vs NO PROMPTED VOIDING, Outcome 4 Change in mean proportion of hourly checks that are wet.
1.5. Analysis.
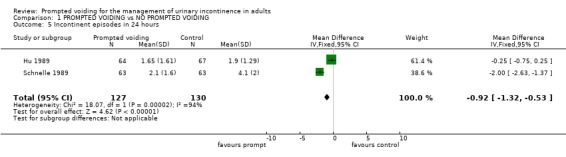
Comparison 1 PROMPTED VOIDING vs NO PROMPTED VOIDING, Outcome 5 Incontinent episodes in 24 hours.
1.7. Analysis.
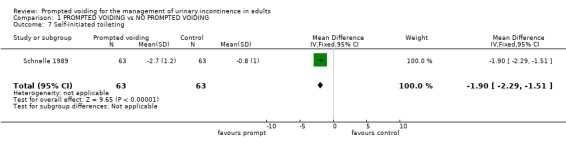
Comparison 1 PROMPTED VOIDING vs NO PROMPTED VOIDING, Outcome 7 Self‐initiated toileting.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Engberg 2002.
| Methods | Prospective, controlled with cross‐over design. Randomised using computerised minimisation algorthim. | |
| Participants | 19 cognitively impaired participants were eligible. 14 participants completed the treatment phase, mean age 83 years, SD 5.4, range 69.3‐91.5 years, 10 female, 4 male. Inclusion criteria: homebound with full‐time caregiver; age >=60 years; minimum urinary incontinence on average twice weekly and for a minimum of 3 months. Setting: participant's home | |
| Interventions | Treatment group = 8 week treatment phase Control group = followed for 8 weeks, reassessed, then crossed over to treatment protocol. All participants reassessed at end of treatment protocol | |
| Outcomes | Reduction of day and night time incontinent episodes. | |
| Notes | Treatment implemented by full‐time caregiver. Wet checks every 2 hours ‐ waking hours only. During treatment weekly intervention visits by study nurse. Follow‐up of all participants for 1 year following treament completion with reasssessment visit every 3 months. Cognitively intact participants were entered into a separate crossover trial of pelvic floor muscle training with biofeedback | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Hu 1989.
| Methods | RCT Randomisation ‐ open or closed random number tables (via author communication) No blinding | |
| Participants | Inclusion Criteria: female; >65 years; incontinence during daytime; ability to recognise own name 143 females met selection criteria (72 to treatment and 71 to control) Average age = 85 years Withdrawal due to hospitalisation, death, transfer or catherisation = 8 from treatment group by the last four weeks and 4 from control group by the last four weeks Setting: seven nursing homes in Pennsylvania | |
| Interventions | Treatment group = prompted voiding for 13 weeks; with hourly checks 7am ‐ 9pm every day Control group = usual incontinence related care | |
| Outcomes | Changes in incontinence status measured by frequency of incontinence per day before, during and after the programme | |
| Notes | Treatment implemented by project trained nursing research assistants Follow up at 22 weeks with three data collection periods Reliability check on wet episodes by research staff for first three weeks then randomly Subjects had urologic evaluation prior to entering trial for bladder diagnosis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Linn 1995.
| Methods | Randomised clinical trial | |
| Participants | 78 participants recruited; attrition of 3. All male veterans ‐ allocated to treatment or control group. Setting: intermidiate care ward | |
| Interventions | Baseline data collection; a PV intervention; post‐intervention assessment and 3 month follow up | |
| Outcomes | Wet checks reduced from 42% at baseline to 17% during treatment; number of requests to toilet increased from av. of 0.38 per day to 2.3. Control group did not show significant changes. | |
| Notes | No detail on how many patients in each group. No data on health status outcomes. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Ouslander 2005.
| Methods | Randomised, controlled cross‐over trial in four phases: screening and enrollment, baseline assessments and computer‐gernerated randomisation | |
| Participants | 178 subjects over 60 yrs eligible; 107 randomised to immediate intervention group 1 n = 52 and delayed intervention group 2 n = 55. 64 completed the intervention phase of trial. Setting: nursing homes | |
| Interventions | Functional incidental training, including PV, 4 times daily, 5 days per week for 8 weeks. Group 1 received intervention while group 2 was control, then crossed over so group 2 received intervention and group 1 had no intervention. | |
| Outcomes | Measures of mobility, edurance, strength and continence during each study phase. Wet checks reduced from 54% to 25% in Group 1 and increased in the control group from 41% to 50% | |
| Notes | Trained research staff provided the FIT intervention. Subjects did not sustain improvement when crossed over into the non‐intervention group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Schnelle 1983.
| Methods | Pretest‐posttest control group design Randomisation ‐ not described No blinding | |
| Participants | 26 subjects identified from two nursing homes in Tennessee n=14 in nursing home A; average age = 83 years; withdrawal = 1 died; 3 incontinence; 1 medical permission not granted (n=5 treatment and n=4 control) n=12 in nursing home B; average age = 81 years; no withdrawals (n=6 treatment and n=6 control) Total: n=11 entered treatment and n=10 remained control | |
| Interventions | Treatment group = received prompted voiding schedule; nursing aides checked subjects hourly between 7am ‐ 7pm for 21 days | |
| Outcomes | Increase of appropriate toileting behaviour | |
| Notes | Reliability checks: a nursing aide and trainer independently, but concurrently checked the subject (17% of contacts, baseline and 10% during treatment); aides correctly implemented the procedure for 97.2% of the contacts Standard deviations not reported Average time spent with the subject was 2.5 minutes (6 patients = 20 minutes per hour; this includes time moving between patients) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Schnelle 1989.
| Methods | Multiple baseline design Randomisation ‐ random number tables (via author communication) No blinding | |
| Participants | Inclusion Criteria: age > 65 years; incontinent for minimum of two times in a five day period; correctly identifying an object out of two on three separate occasions 319 subjects identified as incontinent; withdrawals = 57 by behavioural screen, 36 refused by physicians, 70 not consented 156 entered baseline; 30 dropouts = continent, transferred, hospitalisation, died, or withdrew consent 126 subjects (25% male and 75% female) completed trial Average age = 82 years Setting: six nursing homes in Tennessee | |
| Interventions | Three phases ‐ phase 1 = baseline; phase 2 = subjects randomly assigned to two groups; phase 3 = control group entered treatment Phase 2 = Group 1 (n=63) received prompted voiding for 10 days every hour between 7am ‐ 7pm Phase 2 = Group 2 (n=63) remained in baseline assessment for 5 days ‐ no prompted voiding Subjects who responded to hourly PV, moved to 2 hourly PV (phase 3) | |
| Outcomes | % of time subject wet during treatment freqency of incontinence from baseline to treatment | |
| Notes | Comparison between the two groups within phase 2 weakened due to different duration of treatment and control Validity checks ‐ research staff marked bedding with chalk to identify non‐research staff intervention Reliability checks ‐ 10% of checks by two independent assessors and 5% of checks randomly assessed Research staff implemented all treatment Subjects had urologic evaluation to identify the bladder diagnosis before entering trial | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Schnelle 2003.
| Methods | RCT ‐ randomisation by computerised programs | |
| Participants | 148 residents across 4 nursing home completed the study. 74 in each of the intervention and control groups. | |
| Interventions | Research staff implemented PV for 5 days a week, every 2 hours between 8am and 4pm. Assessments on physical activity, incontinence and functional status were conducted pre‐intervention and at 8 and 32 weeks (including the control group) by research staff other than those who performed the intervention. They were blinded to group assignment. | |
| Outcomes | Impact of FIT (Functional Incidental Training) on upper body strength, urinary and faecal incontinence, physical activity and mobility endurance. | |
| Notes | Trained research staff performed the intervention over the 8 months. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Smith 1992.
| Methods | Treatment group method ‐ no detail on randomisation | |
| Participants | 10 in treatment group (av. age 92.4) and 10 in control group (av. age 90.3); Setting: nursing section of a life‐care community | |
| Interventions | Phase 1: baseline recording for both groups; Phase 2: pad and pant system; Phase 3: PV for treatment group; Phase 4: addition of anticholinergic meds for treatement group ‐ all phases over 3.5 months | |
| Outcomes | Percent of wet checks calculated daily. Treatment group improved incontinence from 80% to 20% | |
| Notes | No details about gender | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Surdy 1992.
| Methods | RCT no blinding random assignment ‐ no description | |
| Participants | Exclusion critieria: obstructive incontinence;urinary tract infection; catheter insitu; neurological or untreatable cause for incontinence n=12; treatment=6, average age=82 and control=6, average age=78 no withdrawals 9 weeks duration (7 weeks of treatment) | |
| Interventions | treatment = checking and changing every 2 hours, social praise and a prompting protocol control = received checking and changing every 2 hours only | |
| Outcomes | % decrease in percent wet % increase in percent dry % increase in correct discrimination of continence status % increase in independent requests for toileting | |
| Notes | two protocols used, one for treatment group and one for control group regular staff implemented treatment urodynamic assessment at baseline random reliability checks performed ‐ 21 inter‐observer agreements for each group weekly staff meetings ‐ staff carried pocket‐sized protocols, colour‐coded to match data sheets | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Jirovec 2001 | Intervention is timed voiding with an element of habit training for some patients |
| Lewis 1990 | Prompted voiding plus uristop one arm of trial, prompted voiding other arm |
| Ouslander 1995a | Prompted voiding on both arms of the trial |
| Schnelle 1995 | This randomised trial reports the effects on mobility endurance and physical activity of an exercise intervention combined with prompted voiding compared with prompted voiding alone. Excluded as no outcomes reported that relate to urinary incontinence. The authors will be contacted for more information |
| Yu 1990 | Baseline data of a possible RCT |
Contributions of authors
One reviewer (S. Eustice) wrote the initial protocol. Two reviewers (S. Eustice, B. Roe) independently assessed the relevance and quality of the studies and selected which to include in the review. The same two reviewers independently extracted the data from trial reports of identified studies. One reviewer (S. Eustice) wrote the review and both co‐reviewers commented on the review.
Declarations of interest
None known.
Edited (no change to conclusions)
References
References to studies included in this review
Engberg 2002 {published data only}
- Engberg S, Sereika SM, McDowell BJ, Weber E, Brodak I. Effectiveness of prompted voiding in treating urinary incontinence in cognitively impaired homebound older adults. Journal of Wound, Ostomy, & Continence Nursing 2002;29(5):252‐65. [DOI] [PubMed] [Google Scholar]
Hu 1989 {published data only}
- Hu T, Igou J, Kaltreider L, Yu L, Rohner T, Dennis P, Craighead E. A clinical trial of a behavioural therapy to reduce urinary incontinence in nursing homes. Neurourology and Urodynamics. 7 1988; Vol. 7, issue 3:279‐80.
- Hu TW, Igou JF, Kaltreider DL, Yu LC, Rohner TJ, Dennis PJ, et al. A clinical trial of a behavioral therapy to reduce urinary incontinence in nursing homes. Outcome and implications. JAMA 1989;261(18):2656‐62. [MEDLINE: ] [PubMed] [Google Scholar]
- Hu TW, Kaltreider DL, Igou JF, Yu LC, Rohner TJ. Cost effectiveness of training incontinent elderly in nursing homes: a randomized clinical trial. Health Services Research 1990;25(3):455‐77. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Linn 1995 {published data only}
- Linn JG. Prompted voiding in the treatment of urinary incontinence. Rehabilitation: R & D Progress Reports. Vol. 32, Washington (DC): Department of Veterans Affairs, VA Rehabilitation Research and Development Service, 1995:323. [Google Scholar]
- Linn JG, Best HL, Holzapfel KM. Geriatrics. Behavioral treatment of urinary incontinence. Rehabilitation: R&D Progress Reports 1994;30‐31:106‐7. [Google Scholar]
- Linn JG, Best HL, Holzapfel KM. Geriatrics: behavioral treatment of urinary incontinence. Rehabilitation: R & D Progress Reports 1996;33:100‐1. [Google Scholar]
Ouslander 2005 {published data only}
- Ouslander JG, Griffiths P, McConnell E, Riolo L, Schnelle J. Functional Incidental Training: applicability and feasibility in the Veterans Affairs nursing home patient population. Journal of the American Medical Directors Association 2005;6(2):121‐7. [DOI] [PubMed] [Google Scholar]
- Ouslander JG, Griffiths PC, McConnell E, Riolo L, Kutner M, Schnelle J. Functional incidental training: a randomized, controlled, crossover trial in Veterans Affairs nursing homes. Journal of the American Geriatrics Society 2005;53(7):1091‐100. [DOI] [PubMed] [Google Scholar]
Schnelle 1983 {published data only}
- Schnelle JF, Traughber B, Morgan DB, Embry JE, Binion AF, Coleman A. Management of geriatric incontinence in nursing homes. Journal of Applied Behavior Analysis 1983;16(2):235‐41. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schnelle 1989 {published data only}
- Schnelle JF. Treatment of urinary incontinence in nursing home patients by prompted voiding. Journal of the American Geriatrics Society 1990;38(3):356‐60. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Schnelle JF, Traughber B, Sowell VA, Newman DR, Petrilli CO, Ory M. Prompted voiding treatment of urinary incontinence in nursing home patients. A behavior management approach for nursing home staff. Journal of the American Geriatrics Society 1989;37(11):1051‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Schnelle 2003 {published data only}
- Bates‐Jensen BM, Alessi CA, Al Samarrai NR, Schnelle JF. The effects of an exercise and incontinence intervention on skin health outcomes in nursing home residents. Journal of the American Geriatrics Society 2003;51(3):348‐55. [DOI] [PubMed] [Google Scholar]
- Schnelle JF, Alessi CA, Simmons SF, Al Samarrai NR, Beck JC, Ouslander JG. Translating clinical research into practice: a randomized controlled trial of exercise and incontinence care with nursing home residents. Journal of the American Geriatrics Society 2002;50(9):1476‐83. [DOI] [PubMed] [Google Scholar]
- Schnelle JF, Kapur K, Alessi C, Osterweil D, Beck JG, Al Samarrai NR, et al. Does an exercise and incontinence intervention save healthcare costs in a nursing home population?. Journal of the American Geriatrics Society 2003;51(2):161‐8. [DOI] [PubMed] [Google Scholar]
- Simmons SF, Ouslander JG. Resident and family satisfaction with incontinence and mobility care: sensitivity to intervention effects?. Gerontologist 2005;45(3):318‐26. [DOI] [PubMed] [Google Scholar]
- Simmons SF, Schnelle JF. Effects of an exercise and scheduled‐toileting intervention on appetite and constipation in nursing home residents. Journal of Nutrition, Health & Aging 2004;8(2):116‐21. [PubMed] [Google Scholar]
Smith 1992 {published data only}
- Smith DA, Newman DK, McDowell BJ, Burgio LD. Reduction of incontinence among elderly in a nursing home setting. In: Funk SG, Tornquist EM, Champagne MT, Wiese RA editor(s). Key aspects of elder care: managing falls, incontinence, and cognitive impairment. New York: Springer Publishing Co, 1992. [19779] [Google Scholar]
Surdy 1992 {published data only}
- Surdy TM. Rehabilitation of urinary incontinent nursing home patients [doctoral thesis]. Milwaukee (WI): University of Wisconsin‐Milwaukee, 1992. [Accession No 1995007623. UMI Order No. PUZ9307340] [Google Scholar]
References to studies excluded from this review
Jirovec 2001 {published data only}
- Jirovec MM, Templin T. Predicting success using individualized scheduled toileting for memory‐impaired elders at home. Research in Nursing & Health 2001;24(1):1‐8. [DOI] [PubMed] [Google Scholar]
Lewis 1990 {published data only}
- Lewis AM, Travis ML, Gordon AL, Wenver HB, Reding MJ. Sensory‐motor biofeedback for treatment of urinary urge‐incontinence following stroke. Clinical Research 1990;38(1):10A. [Google Scholar]
Ouslander 1995a {published data only}
- Ouslander JG, Schnelle JF, Uman G, Fingold S, Nigam JG, Tuico E, et al. Does oxybutinin add to the effectiveness of prompted voiding for urinary incontinence among nursing home residents? A placebo‐controlled trial. Journal of the American Geriatrics Society 1995;43(6):610‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Schnelle 1995 {published data only}
- Schnelle JF, MacRae PG, Ouslander JG, Simmons SF, Nitta M. Functional Incidental Training, mobility performance, and incontinence care with nursing home residents. Journal of the American Geriatrics Society 1995;43(12):1356‐62. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Yu 1990 {published data only}
- Yu LC, Rohner TJ, Kaltreider DL, Hu TW, Igou JF, Dennis PJ. Profile of urinary incontinent elderly in long‐term care institutions [see comments]. Journal of the American Geriatrics Society 1990;38(4):433‐9. [DOI] [PubMed] [Google Scholar]
Additional references
Beckman 1995
- Beckman NJ. An overview of urinary incontinence in adults: assessments and behavioral interventions. Clinical Nurse Specialist 1995;9(5):241‐7, 274. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Borrie 1992
- Borrie MJ, Davidson HA. Incontinence in institutions: costs and contributing factors. Canadian Medical Association Journal 1992;147(3):322‐8. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
Burgio 1994
- Burgio LD, McCormick KA, Scheve AS, Engel BT, Hawkins A, Leahy E. The effects of changing prompted voiding schedules in the treatment of incontinence in nursing home residents. Journal of American Geriatric Society 1994;42(3):315‐20. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Button 1998
- Button D, Roe B, Webb C, Frith T, Colin Thome D, Gardner L. Continence: Promotion and Management by Primary Health Care Teams: Consensus Guidelines. London: Whurr Publishers, 1998. [DOI] [PubMed] [Google Scholar]
Colling 1992
- Colling J, Ouslander J, Hadley BJ, Eisch J, Campbell E. The effects of patterned urge‐response toileting (PURT) on urinary incontinence among nursing home residents. Journal of American Geriatric Society 1992;40(2):135‐41. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Colling 1996
- Colling J. Noninvasive techniques to manage urinary incontinence among care‐dependent persons. Journal of Wound Ostomy, & Continence Nursing 1996;23(6):302‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Creason 1989
- Creason NS, Grybowski JA, Burgener S, Whippo C, Yeo S, Richardson B. Prompted voiding therapy for urinary incontinence in aged female nursing home residents. Journal of Advanced Nursing 1989;14(2):120‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Deeks 2005
- Deeks JJ, Higgins JPT. Analysing and Presenting Results. Cochrane Handbook for Systematic Reviews of Interventions 4.2.5 [updated May 2005]; Section 8. www.cochrane.org/resources/handbook/hbook.htm (accessed 31 January 2006).
Fonda 1990
- Fonda D. Improving management of urinary incontinence in geriatric centres and nursing homes. Victorian Geriatricians Peer Review Group. Australian Clinical Review 1990;10(2):66‐71. [MEDLINE: ] [PubMed] [Google Scholar]
Fonda 1998
- Fonda D, Resnick NM, Colling J, Burgio K, Ouslander JG, Norton C, et al. Outcome measures for research of lower urinary tract dysfunction in frail older people. Neurology and Urodynamics 1998;17(3):273‐81. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Grosicki 1968
- Grosicki JP. Effect of operant conditioning on modification of incontinence in neuropsychiatric geriatric patients. Nursing Research 1968;17(4):304‐11. [MEDLINE: ] [PubMed] [Google Scholar]
Hadley 1986
- Hadley EC. Bladder training and related therapies for urinary incontinence in older people. JAMA 1986;256(3):372‐9. [MEDLINE: ] [PubMed] [Google Scholar]
Hu 1990
- Hu TW. Impact of urinary incontinence on health‐care costs. Journal of American Geriatric Society 1990;38(3):292‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hu 2004
- Hu TW, Wagner TH, Bentover JD, Leblanc K, Zhou SZ, Hunt T. Costs of urinary incontinence and overactive bladder in the United States: a comparative study. Urology 2004;63:461‐5. [DOI] [PubMed] [Google Scholar]
Jirovec 1990
- Jirovec MM, Wells TJ. Urinary incontinence in nursing home residents with dementia: the mobility‐cognition paradigm. Applied Nursing Research 1990;3(3):112‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kennedy 1992
- Kennedy AP. Bladder re‐education for the promotion of continence. In: Roe B editor(s). Clinical Nursing Practice: The Promotion and Management of Continence. London: Prentice Hall, 1992. [Google Scholar]
Norton 1996
- Norton C (Ed). Treating and managing urinary incontinence. Nursing for continence. 2nd Edition. Beaconsfield Publishers Ltd, 1996. [Google Scholar]
Ouslander 1993
- Ouslander JG, Palmer MH, Rovner BW, German PS. Urinary incontinence in nursing homes: incidence, remission and associated factors. Journal of the American Geriatric Society 1993;41(10):1083‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ouslander 1995b
- Ouslander JG, Schnelle JF. Incontinence in the nursing home. Annals of Internal Medicine 1995;122(6):438‐449. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ouslander 1995c
- Ouslander JG, Schnelle JF, Uman G, Fingold S, Nigam JG, Tuico E, et al. Predictors of successful prompted voiding among incontinent nursing home residents. JAMA 1995;273(17):1366‐70. [MEDLINE: ] [PubMed] [Google Scholar]
Palmer 2005
- Palmer M H. Effectiveness of prompted voiding for incontinent nursing home residents. In: Melnyk B, Fineout‐Overholt E editor(s). Evidence‐based practice in nursing and healthcare: a guide to best practice. Baltimore: Lippincott Williams and Wilkins, 2005. [Google Scholar]
Pinkowski 1996
- Pinkowski PS. Prompted voiding in the long‐term care facility. Journal of Wound, Ostomy and Continence Nursing 1996;23(2):110‐4. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Roy 1997
- Roy S. The cost of continence. Elder Care 1997;9(Suppl 6):3‐4. [MEDLINE: ] [PubMed] [Google Scholar]
Wallace 2004
- Wallace S, Roe B, Williams K, Palmer M. Bladder training for urinary incontinence in adults. Cochrane Database of Systematic Reviews 2004, Issue 1. [Art. No.: CD001308. DOI: 10.1002/14651858.CD001308.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 1995
- Williams K, Roe B, Sindhu F. Evaluation of Nursing Developments for Continence Care. Report No 10. Oxford: National Institute for Nursing, 1995. [Google Scholar]


