Supplemental Digital Content is available in the text.
Objectives:
To distinguish characteristics of Medicare beneficiaries who will have an acute inpatient admission for sepsis from those who have an inpatient admission without sepsis, and to describe their further trajectories during and subsequent to those inpatient admissions.
Design:
Analysis of paid Medicare claims via the Centers for Medicare and Medicaid Services DataLink Project.
Setting:
All U.S. acute care hospitals, excepting federal hospitals (Veterans Administration and Defense Health Agency).
Patients:
Medicare beneficiaries, 2012–2018, with an inpatient hospital admission including one or more explicit sepsis codes.
Interventions:
None.
Measurements and Main Results:
Prevalent diagnoses in the year prior to the inpatient admission; healthcare contacts in the week prior to the inpatient admission; discharges, transfers, readmissions, and deaths (trajectories) for 6 months following discharge from the inpatient admission. Beneficiaries with no sepsis inpatient hospital admission for a year prior to an index hospital admission for sepsis were nearly indistinguishable by accumulated diagnostic codes from beneficiaries who had an index hospital admission without sepsis. Although the timing of healthcare services in the week prior to inpatient hospital admission was similar among beneficiaries who would be admitted for sepsis versus those whose inpatient admission did not include a sepsis code, the setting differed: beneficiaries destined for a sepsis admission were more likely to have received skilled nursing or unskilled nursing (e.g., nursing aide for activities of daily living) care. In contrast, comparing beneficiaries who had been free of any inpatient admission for an entire year and then required an inpatient admission, acute inpatient stays that included a sepsis code led to more than three times as many deaths within 1 week of discharge, with more admissions to skilled nursing facilities and fewer discharges to home. Comparing all beneficiaries who were admitted to a skilled nursing facility after an inpatient hospital admission, those who had sepsis coded during the index admission were more likely to die in the skilled nursing facility; more likely to be readmitted to an acute inpatient hospital and subsequently die in that setting; or if they survive to discharge from the skilled nursing facility, they are more likely to go next to a custodial nursing home.
Conclusions:
Although Medicare beneficiaries destined for an inpatient hospital admission with a sepsis code are nearly indistinguishable by other diagnostic codes from those whose admissions will not have a sepsis code, their healthcare trajectories following the admission are worse. This suggests that an inpatient stay that included a sepsis code not only identifies beneficiaries who were less resilient to infection but also signals increased risk for worsening health, for mortality, and for increased use of advanced healthcare services during and postdischarge along with an increased likelihood of an inpatient hospital readmission.
There are three periods during which the burdens of sepsis potentially can be mitigated: prior to an acute inpatient hospital admission; during the index sepsis admission; and (among survivors) following discharge from the acute care hospital. Although prevention of infection prevents descent into sepsis associated with that infection (this is the rationale for vaccination and other public health preparedness measures aimed at preventing exposure to pathogens), infection is so common that additional countermeasures— such as sensors of presymptomatic infection and predictors of decompensation subsequent to infection to guide more timely and targeted therapies—are required.
Early treatment of infection, including antibiotic therapy and fluid administration, aims to reduce the number of patients who might sustain subsequent organ dysfunction. More advanced treatments such as organ system supports (such as mechanical ventilation and renal dialysis) aim to mitigate those dysfunctions by reducing their severity, shortening their duration, and enabling healing. Despite seemingly successful treatments of infection and organ dysfunction, sepsis survivors frequently fail to fully recover their health and their prior quality of life. The first article of this set showed that an inpatient hospital admission with the mildest severity of sepsis was associated with 3-year mortality above 50%; for inpatient stays coded as septic shock, the 3-year mortality exceeds 75% (1). Many beneficiaries die of (or at least with) persistent and recurrent infections.
Prevention and early intervention are understood to be pivotal to relieving the burdens of sepsis. We, therefore, sought to describe the clinical experience of Medicare Fee-For Service (FFS) beneficiaries who were free from a sepsis-related inpatient hospital admission for at least 1 year and who then required inpatient hospital admission for sepsis, comparing and contrasting their trajectories with a reference beneficiary cohort similarly free from any sepsis inpatient hospital admission for 1 year and further requiring that the index acute inpatient admission did not result in sepsis coding. Our purpose was to determine whether there were clues among administrative codes—diagnostic codes, procedure codes, and encounter codes—that might flag those who eventually would acquire sepsis versus those who would be hospitalized for some other reason. We then expanded the study population by relaxing the “prior-year-admission-free” restriction: we studied healthcare utilization in the week prior to inpatient hospital admission for all beneficiaries 2012–2017, dividing the cohort into those who would be assigned a sepsis diagnostic code and those who would not. More simply, we intended to: 1) identify any common conditions that might identify a beneficiary at higher risk of a sepsis-linked inpatient hospital admission and 2) identify the characteristics of interactions with the healthcare professionals during the week prior to their sepsis admission to identify an at-risk profile.
We then sought to describe the compounded impact of a sepsis diagnosis on the subsequent health trajectory of affected beneficiaries, again comparing and contrasting with a reference cohort of “not septic but hospitalized” beneficiaries with respect to survival and subsequent intensity of care. For this study, we wanted beneficiaries to have comparable health status prior to the index inpatient admission. We, therefore, required that they be free of any inpatient admission for the year prior to the index admission. Thus, we intended to: 1) compare and contrast the initial outcome and disposition of inpatient admission for sepsis with the sepsis population and 2) describe the sequential venues of care of sepsis survivors for 6 months following initial discharge from the inpatient hospital.
METHODS
We used explicit International Classification of Diseases, 9th Edition (ICD-9) and International Classification of Diseases, 10th Edition (ICD-10) code sets for sepsis, where the crosswalk from ICD-9 to ICD-10 was made according to a common industry standard of a generalized equivalence mapping. We also stratified sepsis patients according to whether sepsis was present on admission (POA), and according to a hierarchy of severity, as described in greater detail in the first article of this set (1).
To evaluate whether there were differences in the chronic health status of patients destined to become septic, and to avoid any confounding that could conceivably be associated with the change in coding basis from ICD-9 to ICD-10, we restricted our initial analysis to beneficiaries who had an inpatient hospital admission in January, 2017, a discharge prior to August 2017, and no inpatient sepsis admissions in the prior year. Inpatient admissions for other reasons were allowed (such admissions reflect chronic health status) provided there was no sepsis code assigned during any of those admissions. We used the sepsis CMS quality metric (SEP-1) (a superset of the ICD-10 crosswalk) codes to identify sepsis in order to maximize capture of sepsis admissions and thereby minimize misclassification as nonsepsis admissions. There were 69,401 beneficiaries with a sepsis inpatient admission and 613,895 beneficiaries with a nonsepsis inpatient admission beginning sometime in the month of January 2017.
To evaluate whether there were differences in contact with the healthcare system between patients who would have an index hospitalization for sepsis versus those who would not, we analyzed the week prior to all Medicare FFS acute inpatient admissions over the interval January 2012–December 2017. For this part of the study, we removed the “one year clean period” restriction: as a practical matter, we wished to determine whether the immediate lead-up to any sepsis-coded stay could be distinguished from the immediate lead-up to a sepsis-free stay regardless of the beneficiaries’ chronic health status. Considering the week prior to index hospital admission either for sepsis or nonsepsis patients, any observation or emergency department services delivered at the admitting hospital from the 3 days prior to the formal inpatient admission are supposed to be bundled into the inpatient claim itself and were not billed separately as professional and/or outpatient claims. (That does not exclude care delivered at sequential acute care hospitals for the same illness during that period, such as might occur with interhospital transfer. However, we additionally excluded any professional or outpatient claims with dates of service on the same day as the start of the inpatient claim [which matches the start of the observation or emergency department services wherever applicable].) Therefore, all claims for services recorded and reported for the week prior to the inpatient admission are taken to have occurred in a venue different from the emergency department, observation unit, or site of the index inpatient admission.
We restricted analysis to beneficiaries continuously enrolled through the 1-year look-back and 1-year look-forward period in Medicare Part A and Part B (traditional Medicare Fee-For-Service) beneficiaries, thus excluding beneficiaries who were either not continuously enrolled in Part A/B or else enrolled in Part C (Medicare Advantage [MA]) for any part of the look-back, inpatient admission, or look-forward period. We restricted attention to FFS patients because the encounter data of MA patients are only available for inpatient hospital services, and the study required other claim types (such as outpatient visits in the week prior to hospitalization) in the analysis.
Some index hospitalizations end in the death of the beneficiary. Other beneficiaries are well enough to return to their personal homes, at least initially. Some others require long-term custodial care, as in a bed licensed to a nursing home (NH). Still others require prolonged continuous higher level care, either in skilled nursing facilities (SNFs) or ongoing inpatient care (such as in a long-term care hospital [LTCH]).
For a comparison of trajectories following an index admission, we restricted focus to acute inpatient admissions with start dates in or after 2012, end dates prior to 2018, and those for which the beneficiary had no inpatient admissions of any kind in the prior year. All subsequent inpatient acute, SNF, and hospice admissions were tracked over the 6-month period after the end of the initial acute inpatient stay. Deaths and any discharge to family home or to a NH for custodial care also were tracked. We report the initial discharge location for each hospitalized beneficiary, and then describe their subsequent 6-month trajectories without reference to dwell time in any location. For example, initial discharge to a SNF followed by return to an inpatient bed within the next 24 hours until the beneficiary died is counted as initial discharge to a SNF provided a claim for the SNF admission was submitted. The trajectories of each patient in both the sepsis and nonsepsis cohorts are described for 6 months following discharge from the index inpatient admission. Absent a charge on the last day of the admission in an inpatient hospital or a SNF, without a report of the beneficiary death and without evidence of admission to a NH, the beneficiary was considered to have returned to their family (personal) home. Therefore, the 6-month trajectory reports represent the most optimistic assessment of posthospitalization trajectory.
The analyses for this report were generated using SAS software, Version 9.4 of the SAS System for Windows (SAS Institute, Cary, NC). Herein, we report only descriptive (counts, rates, and costs) statistics.
This analysis and publication is exempt from institutional review board oversight. It was performed as a healthcare quality improvement analysis. Center for Medicare and Medicaid Services (CMS) is a covered entity. Deidentification methods were implemented in accordance with CMS policy, Privacy Act of 1974 (5 U.S.C. § 552a) and HIPAA (45 Code of Federal Regulations Part 160 and Subparts A and E of Part 164) requirements.
The data used to generate the figures are reported in Supplement 1 (Supplemental Digital Content 1, http://links.lww.com/CCM/F246), Supplement 2 (Supplemental Digital Content 2, http://links.lww.com/CCM/F247), and Supplement 3 (Supplemental Digital Content 3, http://links.lww.com/CCM/F248).
RESULTS
Trajectories Prior to the Index inpatient Admission
We began with a study of all patients who had an inpatient admission in January 2017 and who had no sepsis inpatient admission during the prior 12 months. We focused first on the 10 most prevalent diagnostic codes among patients destined for an index admission with a sepsis code. We observed that the diagnoses are typical of the age group: individually and collectively, these “top ten” are common among beneficiaries offer no particular predictive insight when compared with the 10 most prevalent diagnostic codes among patients who would be hospitalized for nonsepsis conditions and who would not become septic during the stay (Fig. 1, A and B). We then searched for the top prevalent diagnoses among patients who would have a sepsis-coded admission relative to those who would have an inpatient admission free of sepsis. We refer to these as potentially discriminant diagnostic codes. The top discriminant diagnosis is “other sepsis,” indicating that sepsis had occurred previously in about 10% of the patients, a rate 3.5 times higher than the patients who would not have a sepsis diagnosis during the index admission. Among the other less discriminant diagnoses are several that are suggestive of infection such as fever, but they are seen in 20% or fewer of the patients who had a sepsis diagnosis during their inpatient admission (Fig. 1C).
Figure 1.
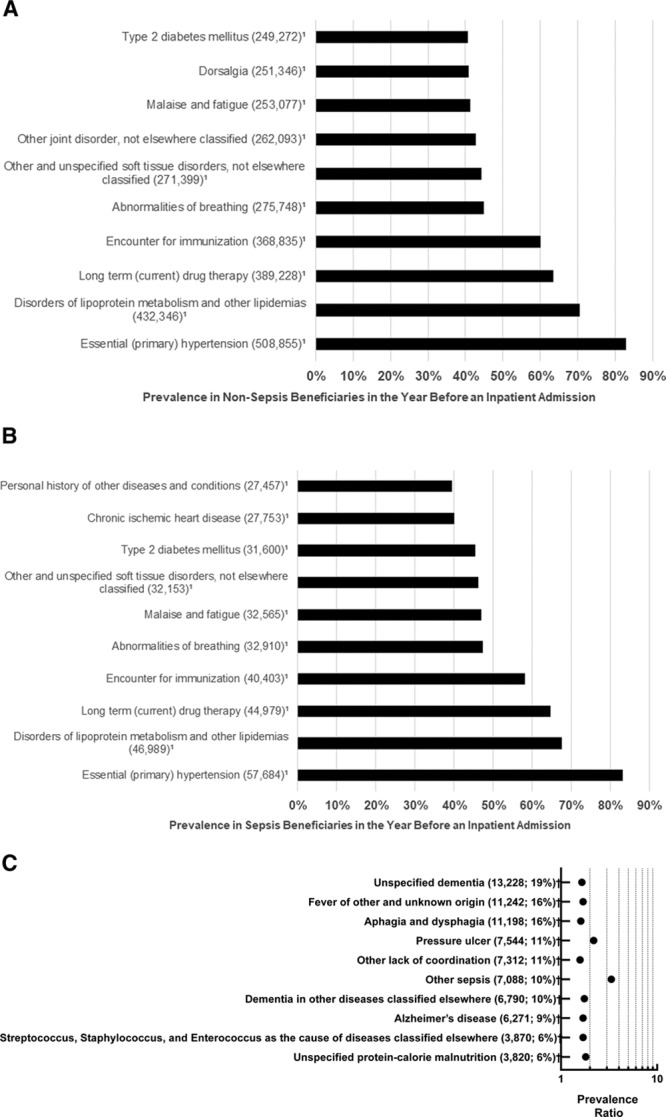
Prevalent and disproportionate diagnoses. A, Most prevalent diagnoses before a sepsis admission. Most prevalent International Classification of Diseases, 10th Edition (ICD-10) codes reported for the CY2016 prior to an acute inpatient admission in January 2017 that includes a sepsis code in January 2017. B, Most prevalent diagnoses before a nonsepsis admission. Most prevalent ICD-10 codes reported for the CY2016 prior to an acute inpatient admission in January 2017 that does not include a sepsis code in January 2017. C, Top prevalent diagnoses before a sepsis admission relative to a nonsepsis admission. The top disproportionally prevalent ICD-10 codes relative to an acute inpatient admission in January 2017 that did not include a sepsis code. Neither the sepsis nor the nonsepsis patients had any inpatient admission during the prior year. Note that the top disproportionally prevalent diagnoses (other sepsis and pressure ulcer) affected only 10–11% of the patients whose inpatient admission would have a sepsis code. The remaining disproportionally prevalent diagnoses had prevalence ratios less than 2.
Next, we determined the healthcare contacts during the week prior to admission for beneficiaries whose inpatient admissions would—and would not—have a sepsis code. We did not require any clean period. During the week prior to a sepsis inpatient admission, more than 60% had a professional claim, more than 20% had an outpatient claim, and many had home health, SNF, and unskilled nursing assessment claims (Fig. 2). Thus although the specific diagnoses were relatively uninformative, the type and location of care rendered in the week prior to the inpatient admission did suggest that patients sick enough to require skilled and/or unskilled nursing services were at greater risk of experiencing an inpatient admission with a sepsis diagnosis.
Figure 2.
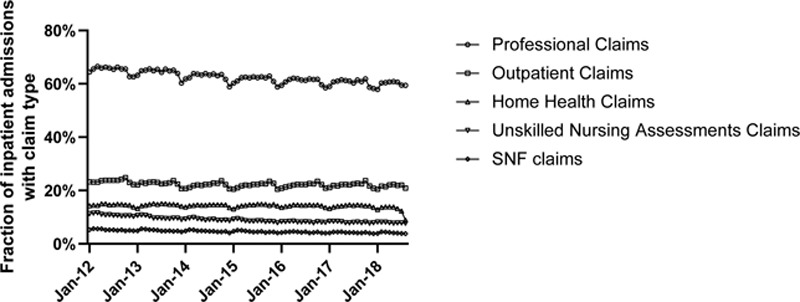
Percentage of inpatient sepsis admissions who had a claim in the week prior to admission, by claim type. The seasonal dips in the outpatient professional evaluation and management codes appear to slightly precede the seasonal rise in admissions, mortality, and costs. SNF = skilled nursing facility.
Given the fraction of sepsis patients who had evaluation and management claims in the week prior to inpatient admission, we wished to determine when those claims occurred during that week prior to inpatient admission, and whether there was any difference in the patterns of claims for sepsis POA, not POA, and for patients who required admission for a nonsepsis diagnosis. The timing of the most recent claim for preadmission evaluation and management (E/M) professional services referenced to the day of admission were indistinguishable (Fig. 3).
Figure 3.
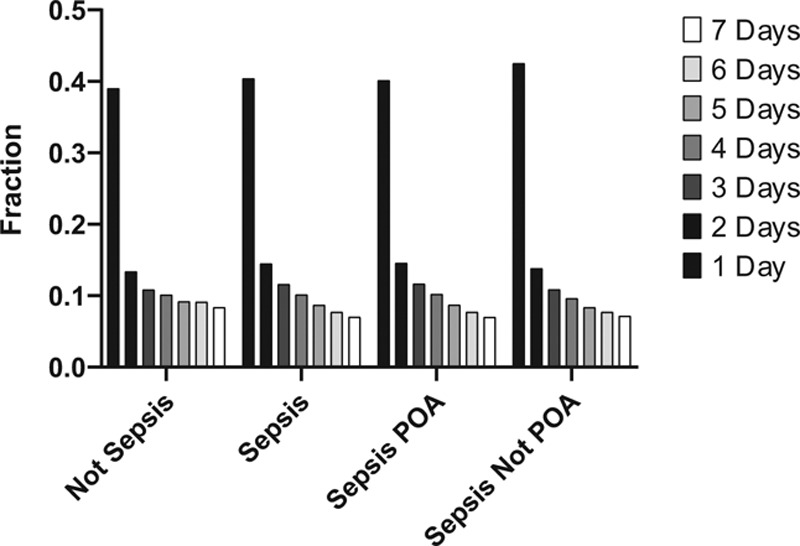
Distribution of acute inpatient stays by the number of days between the most recent evaluation and management and the acute inpatient admission date. Data are summarized at the admission level (not the beneficiary level). The majority of the claims occur on the day prior to admission, suggesting that beneficiaries present themselves for care and are admitted to hospital soon thereafter. The pattern of claims is indistinguishable among patients with sepsis or not and irrespective of whether the sepsis was present on admission (POA) or not.
Next, we determined whether inpatient sepsis admissions had inpatient claims in the week prior to that admission. More than 15% of patients with septic shock had an inpatient claim in the week prior to the sepsis inpatient admission. More than 10% of patients with other severities of sepsis had an inpatient claim in the week prior. In comparison, only 8% of patients who had acute inpatient hospital admission had an inpatient claim in the week prior (Fig. 4).
Figure 4.
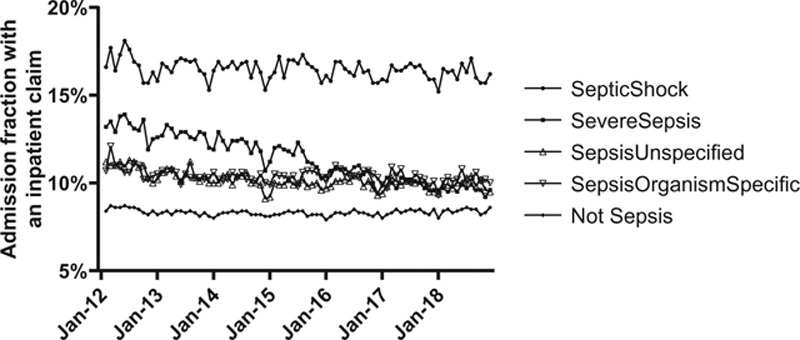
Percentage of inpatient sepsis admissions who had an inpatient claim in the week prior to admission, by sepsis severity. An inpatient claim may be made by an acute care hospital, a long-term acute care hospital, a rehabilitation hospital, or a psychiatric hospital.
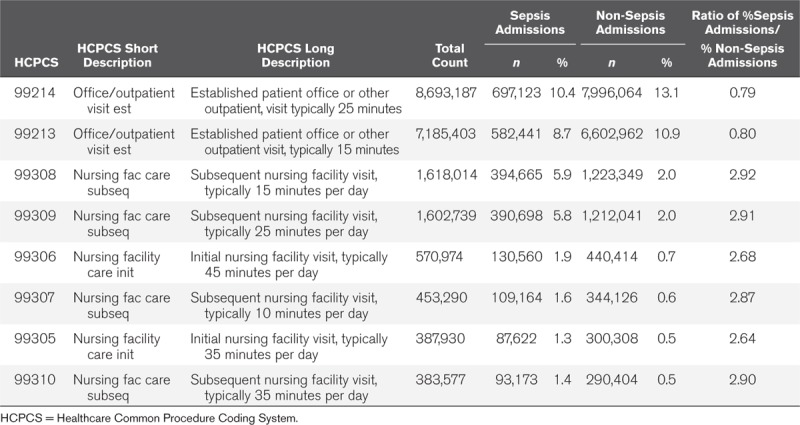
Those findings raised a question of the types and settings of E/M services used by patients destined for a sepsis admission versus an admission that would never include a sepsis code. The most frequent visit codes in both groups were established patient office (or other outpatient) visits of intermediate complexity; 19% of sepsis claims and 15% of nonsepsis claims fell into one of these two categories (Table 1). In contrast, the claims for services in nursing facilities were 2.8 times more likely to have been made in a patient who would experience a sepsis admission versus those who would experience a nonsepsis admission. The use of skilled or unskilled nursing care in the week prior to inpatient admission appeared to be a stronger indicator (vs the accumulation of a specific diagnostic code) that a beneficiary would have a sepsis code applied during that admission.
TABLE 1.
Evaluation and Management Services in Preceding Professional and Outpatient Claims, by Inpatient Admission Type
Trajectories During the Index Admissions: Lengths of Stay
Sepsis accounts for an increasing fraction of all inpatient hospital admissions. This fraction is increasing regardless of the duration of inpatient hospitalization required (length of stay). The rise is due to sepsis POA. In contrast, nonsepsis hospital inpatients account for a decreasing fraction of all inpatient hospital admissions, with the decrease fastest among those who require five or more inpatient days. More generally, sepsis inpatient admissions not only account for a rising fraction of inpatient admissions but also account for an even greater fraction of the long inpatient stay patients (Fig. 5).
Figure 5.
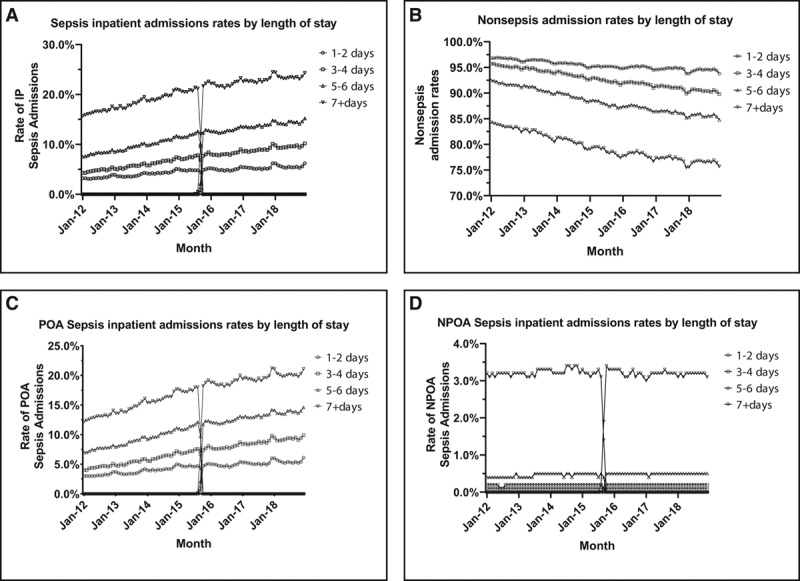
Sepsis and nonsepsis inpatient (IP) admissions by length of stay. A, Sepsis admission rates out of all IP admissions. B, Present on admission (POA) sepsis admission rates out of all IP admissions. C, Not POA (NPOA) sepsis admission rates out of all IP admissions. D, Nonsepsis admission rates out of all IP admissions. For each length of stay band, total sepsis admission rates (A) and nonsepsis admission rates (D) total 100%; similarly POA and NPOA sum to the total admission rate.
Trajectories Subsequent to the Index Admission
The trajectories of beneficiaries subsequent to a sepsis inpatient admission contrasts sharply with those admissions that do not include sepsis (Fig. 6).
Figure 6.
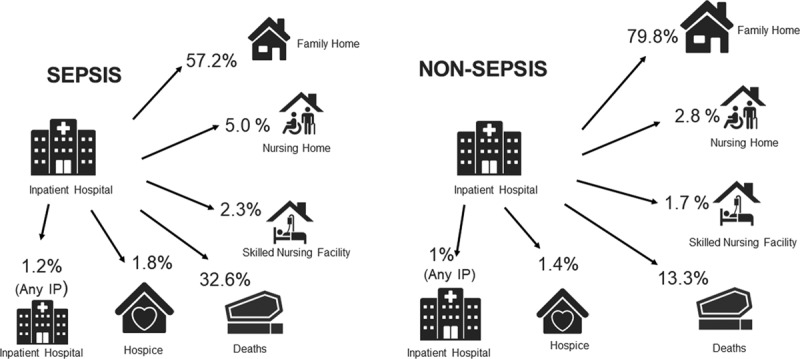
Six-month trajectories of patients whose inpatient (IP) admission included a sepsis code or not. From the acute IP hospital, at 6 mo, patients could be back in an IP hospital (acute, rehabilitation, or psychiatric), at their family (personal) home, in custodial care, in a nursing home, in a skilled nursing facility, in hospice, or deceased. Percentages sum to 100%.
For example, at 6 months following discharge from the inpatient hospital, 32.6% of beneficiaries with a sepsis code are deceased, compared with 13.3% of those whose admission did not include a sepsis code. A larger fraction of sepsis beneficiaries are transferred to SNFs compared with their nonsepsis counterparts. Furthermore, among beneficiaries who are transferred to SNFs, the beneficiaries whose index admission included sepsis are more likely to return to the inpatient setting or die within the ensuing 6 months (Fig. 7).
Figure 7.
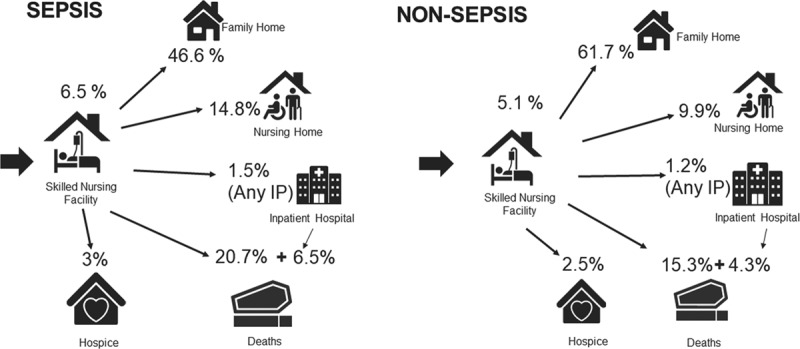
Six-month trajectories of patients whose inpatient (IP) admission included a sepsis code, or not, and who were initially sent to a skilled nursing facility (SNF). From the acute IP hospital and admission to a SNF, at 6 mo, patients could still be in a SNF, an IP hospital (acute, rehabilitation, or psychiatric), at their family (personal) home, in custodial care, in a nursing home, in hospice, or deceased. Percentages sum to 100%.
All sepsis admissions are not the same. Breaking the trajectories down by severity, we observed that those with septic shock are more likely to die in the hospital and less likely to reach a SNF (Table 2). From a patient/family perspective, the chance of reaching the family (patient) home 6 months after any inpatient sepsis admission is only 57% compared with 80% for the patients whose inpatient admission did not carry any sepsis code. For the beneficiary who experienced septic shock during the inpatient stay, the odds of making it home after 6 months are much worse, only 36%.
TABLE 2.
Summary Statistics Comparing Post-Inpatient Sepsis and Post-Inpatient Non-Sepsis Trajectories
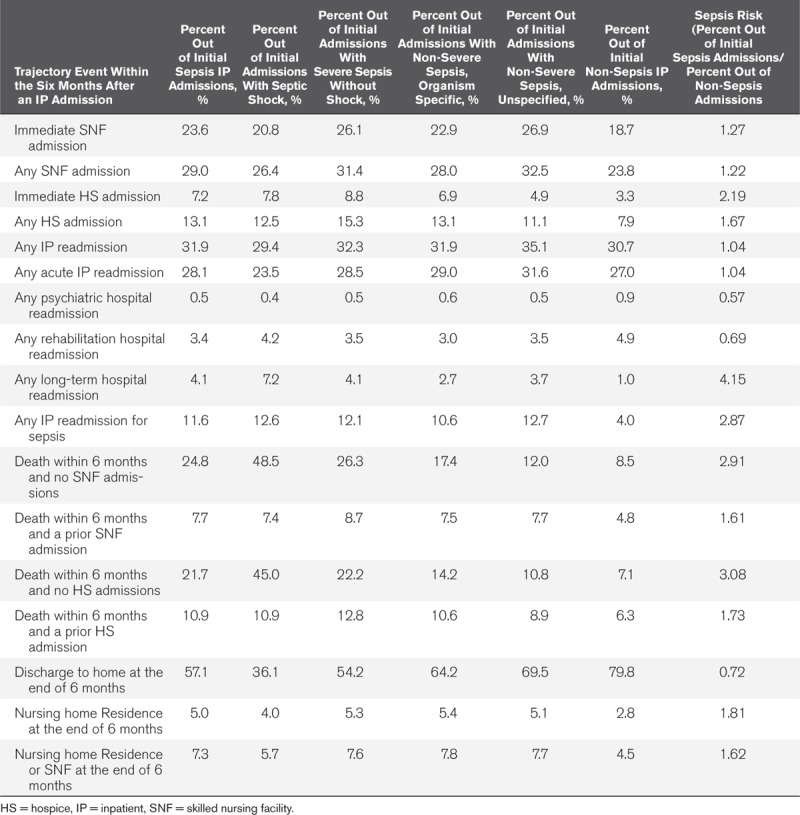
We compared the discharge to home and SNF admission rates across the sepsis severity tiers and observed that the seemingly lower rate of SNF admissions among the sickest patients (septic shock) was likely due to “crowding out” of that destination owing to death within a week of the index inpatient admission, meaning that patients who otherwise would have required skilled nursing care following the acute inpatient stay died before that disposition could have occurred (Table 2). Detailed information about these trajectories is given in Supplement 3 (Supplemental Digital Content 3, http://links.lww.com/CCM/F248).
There are differences in trajectory depending on whether the patient presented to hospital with sepsis versus whether the sepsis was diagnosed after admission (Table 3). Sepsis acquired during hospitalization (i.e., not POA) carries a substantially greater probability of death within 6 months of discharge. Furthermore, 54% of inpatient admissions of beneficiaries whose sepsis was diagnosed at admission ended in return to their patient/family homes within 6 months, compared with only 32% of those whose sepsis was diagnosed during the inpatient hospital admission.
TABLE 3.
Post Inpatient Admission Summary Statistics by Status on Inpatient Admission (Present or Not Present)
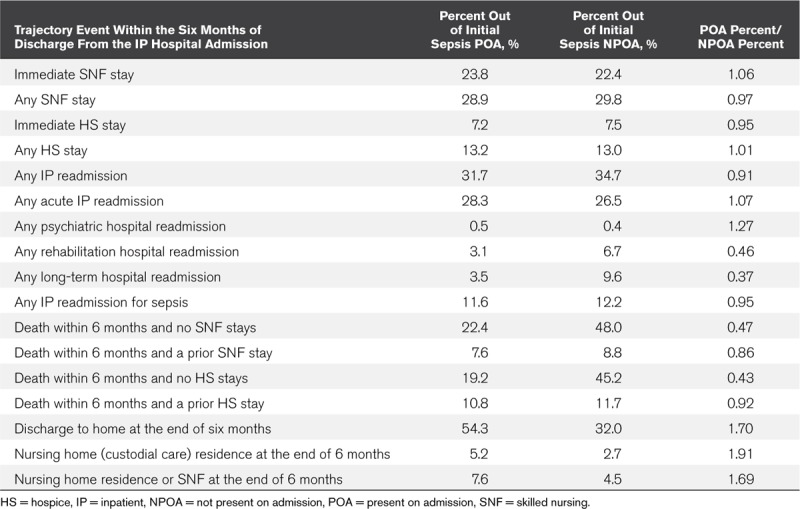
However, if the beneficiary who becomes septic while hospitalized survives to SNF transfer, then the subsequent trajectories are only slightly worse when compared with those whose sepsis was POA. Regardless, the odds of discharge to the family (patient) home directly from the SNF are quite dismal for both groups, 29%–30%. The remaining approximately 70% will either die in the SNF or be transferred among various facilities. Those transfers in and out of inpatient, long-term acute care, SNF, NH and hospice, allows only an additional 15% of the original SNF cohort to reach the family (patient) home by the end of 6 months. Rather, there is a greater chance that the transferred beneficiary will end up residing in a NH receiving custodial care (Table 4).
TABLE 4.
Trajectories and Status at Six Months Following Discharge From an Inpatient Admission Directly to a Skilled Nursing Facility Analyzed by Sepsis Status at Time of Inpatient Admission
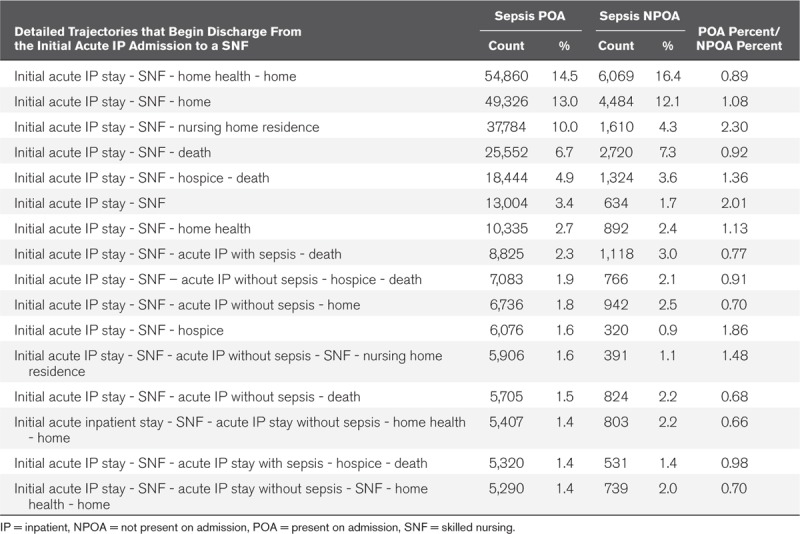
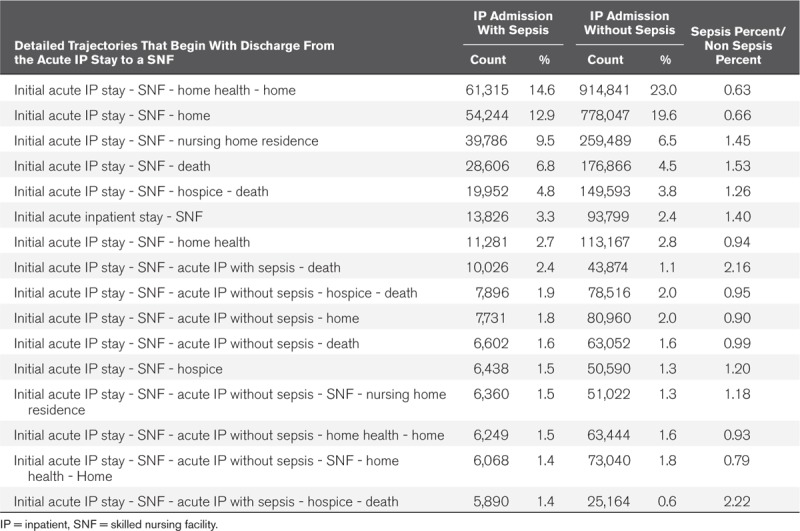
The sepsis diagnosis nevertheless carries risk into the SNF admission. Those whose index admission includes a sepsis diagnosis have worse trajectories through SNF compared with those whose index admission did not include a sepsis diagnosis: only 29% of sepsis patients who survive their hospitalization and are discharged to a SNF make it home from that stay, compared with 44% of those who require a SNF following a nonsepsis admission. The sepsis patients who survive their SNF stay are 1.43 times more likely to be transferred to a NH (Table 5).
TABLE 5.
Detailed Trajectories That Begin With Discharge From the Acute Inpatient Stay to a Skilled Nursing Facility
The data on early trajectories are helpful yet insufficient to allow for longer-term prediction of the outcome of any particular beneficiary. The longer-term outcomes stratified by severity and presented as monthly cohorts clarify that fewer than half of the deaths will occur 6 months following inpatient admission across all severities (Fig. 8). Deaths following a sepsis inpatient admission continue to accumulate at least to 3 years. The trajectories following an inpatient severe sepsis admission appear to be improving faster than those for septic shock, or for milder forms of sepsis. These rapid improvements appear to be associated with inpatient treatment, as the longer-term mortality declines in parallel fashion.
Figure 8.
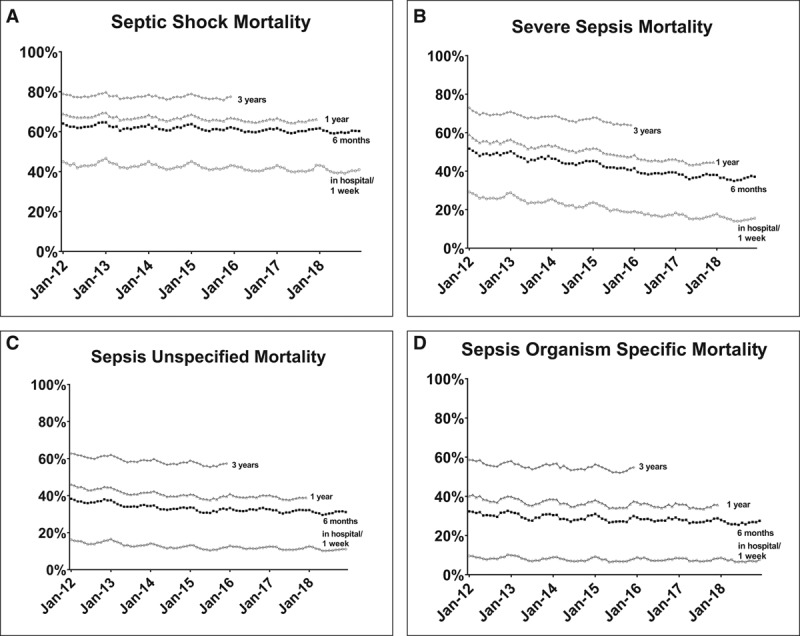
Mortality of sepsis stratified by severity and presented as monthly cohorts. Filled circles, 1-wk mortality; filled squares, 6-mo mortality; filled triangles (pointing up), 1-yr mortality; filled triangles (pointing down), 3-yr mortality. Each month represents a cohort of ≈70,000–100,000 Medicare Fee-For Service sepsis patients, of which approximately one-quarter of the total are septic shock admissions, one-fifth of the total are severe sepsis admissions, and the balance are less severe sepsis admissions. Among the four stratifications, no monthly cohort (i.e., no column representing 1 mo in any of the four graphs) contains fewer than 11,000 admissions. The mortality decline is greatest among those with severe sepsis, and the lives appear to be being saved during the hospitalization (the longer-term mortalities decline in parallel). One hypothesis is that early and aggressive case finding and treatment are preventing progression (i.e., to more severe organ dysfunction and shock).
DISCUSSION
Prevention, detection, and mitigation are cornerstones of management of every serious illness. We evaluated 1) whether administrative healthcare data could distinguish patients who would experience initial hospitalization for sepsis from those who would be hospitalized for other reasons and 2) the consequences of experiencing sepsis on early outcomes of that hospitalization. We observed that beneficiaries who would be hospitalized for sepsis were practically indistinguishable by diagnostic codes from those who would be hospitalized for some other reason (2). Once a sepsis diagnosis was made, the trajectories of the two cohorts diverged: sepsis beneficiaries experienced disproportionate early and late mortality, often punctuated by admission to nursing facilities and by subsequent hospital readmissions.
Close examination of the data that discriminate those who will have a sepsis admission from the reference groups suggest that there is an excess of claims that include diagnosed fever, conditions that predispose to infection (e.g., pressure sores) or infection during the prior year. This excess suggests (but does not prove) that for some beneficiaries, sepsis may be a manifestation of a more chronic state of infection, debilitation, and/or immunodeficiency. Indeed, new incident diagnoses following a sepsis hospitalization similarly hint at an excess of infectious processes. Collectively, these findings suggest that for at least some patients, sepsis of any severity might be a manifestation of chronic conditions more than bad luck following an otherwise ordinary incident infection. We observe that sepsis that is not POA but is rather acquired during hospitalization carries even greater risk of immediate mortality (3, 4). Together, these data support an emerging perspective that an acute inpatient admission for sepsis exposes underlying immunoinflammatory derangements that adversely affect the chronic health status of survivors. What cannot be determined from the data is whether the immunoinflammatory response was normal prior to the sepsis acute inpatient admission (and deranged consequent to the sepsis event) or whether the immunoinflammatory response was compromised prior to the sepsis event. Unraveling those relationships is important to prognosis, diagnosis, and long-term management of at-risk populations.
Sepsis diagnoses in Medicare beneficiaries thus may be a marker of deeper physiologic fragility as much as it is an acute diagnosis (5–7). The notion of underlying conditions that predispose to sepsis begs the questions of 1) what are the chronic states that renders beneficiaries susceptible to the acute exacerbation labeled sepsis and 2) are there strategies that might enable more timely recognition of the transition from predisposition to acute illness (4)? A detailed reporting of healthcare conditions that predispose to sepsis and adverse outcomes is included in the third article in this set (8). Regardless, there is a pressing need for a strategy that does not require identification of a specific causative organism and yet can facilitate early notification to act, control, and treat the infections that culminate in sepsis. There is an equally pressing need for a strategy that does not require identification of the specific pathogen to sense and identify the transition from local infection to systemic inflammation and/or decompensation that defines the staged progression of sepsis (9).
Once sepsis is diagnosed, contemporary management is only partially successful (10–13). Although many beneficiaries survive the initial hospitalization, the first article in this series reported that the 3-year mortality following a sepsis diagnosis ranged from 50% to 75% depending on the severity inferred from the specific diagnostic code (1, 14). The postdischarge trajectories reported herein suggest that only a minority of Medicare beneficiaries with an initial sepsis admission are promptly discharged to their personal home—fewer than 1/3. Those whose chronic illnesses require prolonged continuous care in LTCH and SNF are at disproportionate risk for cycling back into the inpatient hospital and for death. Even those who do make it to their personal/family home are at increased risk for all-cause mortality for at least the next 3 years. These data pertain to the contemporary Medicare beneficiary population and should not be extrapolated to other populations; studies should be conducted in those populations to identify similarities and differences in trajectories in and out of an inpatient sepsis admission.
Several questions arise. Does current inpatient care optimally prepare Medicare beneficiaries with sepsis for transfer or discharge? For which beneficiaries does transfer to prolonged continuous care (SNF or LTCH) enable recovery sufficient to eventually return home (15)? What, if any, home health monitoring modalities, can reduce readmissions or otherwise improve outcomes? How should beneficiaries and their families be informed of their trajectories in order to make the healthcare decisions that are right for them? These questions cannot be answered with the existing data.
In the first article of this set, we discussed potential explanations for the rise in inpatient admissions assigned a sepsis code (1). In this report, we observe that stays with different severity tiers have differently improving survival over the study interval. Separating the study population into monthly cohorts (each monthly cohort contains 70,000 to >100,000 sepsis inpatient admissions) and further stratifying by severity, we observed that the survival data of the septic shock cohorts and of the nonsevere sepsis (either organism specified or organism unspecified) cohorts show modest improvements over the interval, a finding consistent with reports by others (1, 14). In contrast, the data show a marked improvement in survival of the severe sepsis patients. Although this may be due to changes in coding practices, it may also be due to more timely recognition and/or timeliness of effective countermeasures. We reported in the first article of this set that the proportion of severe sepsis patients remained nearly stable over the study interval (Fig. 2C of the first article) suggesting that excess identification of cases as severe sepsis was not the cause of the more rapid (compared with septic shock and to milder forms of sepsis) improvement in outcomes. We do not think that the relative improvement in survival of severe sepsis versus septic shock is attributable to the reported tendency of hospitals to code for sepsis in the sickest of patients because we would have expected even better improvements in the nonsevere cohorts (16). These observed improvements in survival of severe sepsis also are not likely related to reclassifications related the issuance of the Sepsis-3 definitions, which occurred in 2016 (in the middle of the study period); there is no visible discontinuity in the survival data at that point (17).
There are limitations to the current study. First, although we required a clean periods before entering beneficiaries into the risk and trajectory study cohorts, there is no a priori reason to assume that 1 year free of an inpatient hospitalization is either necessary or sufficient to create comparable cohorts; rather freedom from an inpatient admission is a practical and convenient marker for relative health. Second, although we evaluated the hospitalized cohorts for 6 months, there is no a priori reason to assume that their final trajectories are well established by that point; indeed, we demonstrated in the prior report that mortality effects persisted for at least 3 years following a sepsis admission. Our purpose was better understanding of the short-term trajectories, particularly of those sepsis survivors who continue to require continuous care, and better understanding of their near-term risk for cycling back into the inpatient hospital. Third, there is an inevitable interaction—and conflation—of the sequelae of sepsis with the sequelae of other serious conditions. For example, a beneficiary with advanced heart failure who experiences pneumonia and organ dysfunction will be labeled properly as septic—whether it is the heart failure or the sepsis that accounts for the need for skilled nursing. Similarly, whether it is deterioration of the cardiac condition or reappearance of sepsis that triggers readmission to an acute care hospital cannot be readily determined. Causality is not claimed and cannot be inferred for any particular patient. We assert only that acquisition of a sepsis diagnosis code during the inpatient admission is sufficient to predict a markedly different trajectory for that admission and following discharge. Teasing apart the influencers of sepsis trajectory and destination is addressed in the third report of this set (8).
CONCLUSIONS
The count of inpatient Medicare hospitalizations that include sepsis codes is rising annually. Examining diagnostic codes accumulated during the prior year and healthcare service utilization during the prior week, cohorts of beneficiaries who have a sepsis-coded inpatient admissions appear largely indistinguishable from reference cohorts of beneficiaries who require hospitalization and have sepsis neither POA nor acquired during hospitalization. If distinguishing characteristics exist, they are more likely to be found in the beneficiaries’ use of skilled or unskilled nursing services or in specific clinical data. Both cohorts have substantial contact with professional health caregivers in the week prior to hospitalization, suggesting an opportunity for earlier assessment and recognition of evolving sepsis. However, this will require both an index of suspicion and novel diagnostic strategies.
Once sepsis is recognized during an acute inpatient admission, previously compensated (to the extent they were not hospitalized for a prior year) Medicare beneficiaries have excess adverse outcomes compared with those hospitalized with nonsepsis diagnoses. Beneficiaries who acquire sepsis during the hospitalization are especially likely to die within a week of discharge. The severity of the sepsis event appears to influence the early trajectory, and sepsis patients are not only more likely to die but also are less likely to return to their family (personal) home and more likely to require advanced care compared with the reference group that did not experience sepsis. Although the current analysis illuminates the proportion on each trajectory, it does not explain why a particular beneficiary follows a particular trajectory, nor does it consider the social determinants of that trajectory.
The importance of sepsis prevention and of early detection are apparent. Those strategies, which likely will require innovation in public health as well as improving individual immunoinflammatory health, are among the most promising strategies toward protecting populations and saving lives. Once sepsis is established, improving the immediate postsepsis trajectory—either by actions during the inpatient hospitalization or by actions during and after transfer to a facility offering prolonged care—appears to be an essential step toward value-based transformation of sepsis care.
Supplementary Material
Footnotes
*See also p. 422.
The views expressed are solely those of the authors and do not necessarily represent those of the U.S. Department of Health and Human Services.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
Dr. Buchman’s institution received funding from the United States government as a Senior Advisor under an intergovernmental personnel agreement with Emory University, and his institution received funding from the Society of Critical Care Medicine (Editor-in-Chief of Critical Care Medicine). He received funding from Philips Corporation (lecture on the future of ICU telehealth at a conference sponsored by Philips Corporation, which paid for his travel and lodging expense; the honorarium was donated to Emory University). Drs. Buchman, Sciarretta, Sowers, Collier, Chavan, Oke, Pennini, Sathosh, Wax, Woodbury, Chu, Merkeley, Disbrow, Bright, MaCurdy, and Kelman disclosed government work. Dr. Simpson received support for article research from Biomedical Advanced Research and Development Authority (BARDA). Dr. Sciarretta received funding from at The Bioprocessing Summit (sponsored by Cambridge HealthTech Institute) and GTCbio meeting (waived conference fees). Dr. Finne received funding from the U.S. Department of Health and Human Services (HHS), BARDA. Drs. Sowers, Collier, Chavan, Oke, and Santhosh’s disclosed that this work was performed by Acumen, LLC, under contract with the Centers for Medicare & Medicaid Services, HHS (Contract No. HHSM-500-2014-00027I; Task Order No. HHSM-500-T0004), with funding from HHS, Office of the Assistant Secretary for Preparedness and Response. Drs. Pennini, Wax, and Woodbury disclosed that they are a government support contractor employed by Aveshka Inc., which receives funds from the U.S. government under contract to provide technical and programmatic support for HHS-BARDA. Dr. MaCurdy’s institution received funding and research support from Centers for Medicare & Medicaid Services.
REFERENCES
- 1.Buchman TG, Simpson SQ, Sciarretta KL, et al. Sepsis Among Medicare Beneficiaries: 1. The Burdens of Sepsis, 2012–2018. Crit Care Med 2020; 48:276–288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu VX, Escobar GJ, Chaudhary R, et al. Healthcare utilization and infection in the week prior to sepsis hospitalization. Crit Care Med 2018; 46:513–516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rothman M, Levy M, Dellinger RP, et al. Sepsis as 2 problems: Identifying sepsis at admission and predicting onset in the hospital using an electronic medical record-based acuity score. J Crit Care 2017; 38:237–244 [DOI] [PubMed] [Google Scholar]
- 4.Leisman DE, Angel C, Schneider SM, et al. Sepsis presenting in hospitals versus emergency departments: Demographic, resuscitation, and outcome patterns in a multicenter retrospective cohort. J Hosp Med 2019; 14:340–348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maley JH, Mikkelsen ME. Short-term gains with long-term consequences: The evolving story of sepsis survivorship. Clin Chest Med 2016; 37:367–380 [DOI] [PubMed] [Google Scholar]
- 6.McPeake J, Mikkelsen ME. The evolution of post intensive care syndrome. Crit Care Med 2018; 46:1551–1552 [DOI] [PubMed] [Google Scholar]
- 7.Meyer N, Harhay MO, Small DS, et al. Temporal trends in incidence, sepsis-related mortality, and hospital-based acute care after sepsis. Crit Care Med 2018; 46:354–360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buchman TG, Simpson SQ, Sciarretta KL, et al. Sepsis Among Medicare Beneficiaries: 3. The Methods, Models, and Forecasts of Sepsis, 2012–2018. Crit Care Med 2020; 48:302–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.United States Department of Health and Human Services. Division of Research, Innovation, and Ventures. 2019. Available at: https://drive.hhs.gov. Accessed December 1, 2019
- 10.Prescott HC, Angus DC. Postsepsis morbidity. JAMA 2018; 319:91. [DOI] [PubMed] [Google Scholar]
- 11.Prescott HC, Angus DC. Enhancing recovery from sepsis: A review. JAMA 2018; 319:62–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prescott HC, Costa DK. Improving long-term outcomes after sepsis. Crit Care Clin 2018; 34:175–188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prescott HC, Iwashyna TJ, Blackwood B, et al. Understanding and enhancing sepsis survivorship. Priorities for research and practice. Am J Respir Crit Care Med 2019; 200:972–981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iwashyna TJ, Cooke CR, Wunsch H, et al. Population burden of long-term survivorship after severe sepsis in older Americans. J Am Geriatr Soc 2012; 60:1070–1077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Flint LA, David DJ, Smith AK. Rehabbed to death. N Engl J Med 2019; 380:408–409 [DOI] [PubMed] [Google Scholar]
- 16.Whittaker SA, Mikkelsen ME, Gaieski DF, et al. Severe sepsis cohorts derived from claims-based strategies appear to be biased toward a more severely ill patient population. Crit Care Med 2013; 41:945–953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016; 315:801–810 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


