Abstract
This systematic review and meta-analysis examines the associations of allergic rhinitis with sleep duration and sleep impairment. Observational studies published before August 2019 were obtained through English language literature searches in the PubMed, Embase, and CINAHL databases. Mean differences and odds ratios with 95% confidence intervals were extracted and used for meta-analysis. Heterogeneity was confirmed by the I2-heterogeneity test. Subgroup analysis was conducted to evaluate the influence of study design. The Grading of Recommendations Assessment, Development, and Evaluation approach was used to determine the level of evidence. In total, 2544 records were identified through database searches; 914 duplicate records were excluded, 1452 records were removed after screening of titles and abstracts, 151 records were excluded after full-text screening, and 27 articles were included in the final meta-analyses. A total of 240,706,026 patients (19,444,043 with allergic rhinitis) were considered. No significant difference in sleep duration between the allergic rhinitis and the control groups was found. Patients with allergic rhinitis presented with significantly higher sleep quality scores, sleep disturbances scores, and sleep latency scores; more frequent use of sleep medications; and lower sleep efficiency as measured by the Pittsburgh Sleep Quality Index and polysomnography. Meta-analyses for adjusted odds ratios showed that allergic rhinitis was also associated with higher risks of nocturnal dysfunctions, including insomnia, nocturnal enuresis, restless sleep, sleep-disordered breathing, obstructive sleep apnea, and snoring. Meta-analysis for adjusted odds ratio also showed that allergic rhinitis was associated with daytime dysfunction, including difficulty waking up, daytime sleepiness, morning headache, and the use of sleep medications. The overall quality of evidence ranged from low to very low, indicating that caution is required when interpreting these results. This study demonstrates that there is a significant association of AR with sleep characteristics.
Introduction
Allergic rhinitis (AR) is a common inflammatory disorder generally caused by an immunoglobulin (Ig) E-mediated response to a variety of environmental allergens, including cockroach frass, animal dander, pollens, dust mites, and molds [1]. It is characterized by two or more symptoms of nasal itching, rhinorrhea, nasal congestion, and/or sneezing [2]. AR has been reported to have an adverse impact on sleep, memory ability, quality of life, academic performance, and work productivity [3–7]. In 2010, AR affected 10%–20% of the worldwide population, and that number continues to grow with modern lifestyle and environmental changes [1]. It is estimated that AR results in 3.4 billion dollars of direct medical costs annually [8].
Sleep is crucial for human mood, memory, endocrine and immune system functions, and cognition [9–14]. Poor sleep quality, sleep disorders, and/or inadequate sleep duration are considered to be triggers for the development of hypertension [15], diabetes [16], obesity [17], cardiovascular disease [18], and increased mortality [19]. AR has been shown to be an important factor in altered sleep patterns in previous studies [7].
There is a growing body of population-based research on the association between AR and sleep patterns. AR has been found to be positively associated with sleep- disordered breathing (SDB) [20], obstructive sleep apnea (OSA) [21], shorter sleep duration [22], poor sleep quality [23], sleep bruxism [24], night sweating [25], nocturnal enuresis [26], and daytime dysfunction [27]. However, these results are also controversial, since several studies found a negative or insignificant relationship between AR and the above sleep-related outcomes [7, 28–30]. Currently, there is a lack of systematic reviews to evaluate the association between AR and sleep pattern through meta-analysis.
Thus, the present study aims to assess the association of AR with sleep pattern by conducting a systematic review and meta-analysis of published observational studies.
Materials and methods
This systematic review and meta-analysis was carried out in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [31].
Search strategy
Cross-sectional, case-control, and cohort studies examining associations between AR and sleep published before August 2019 were searched in the following databases: PubMed, Embase, and CINAHL. Combinations of sleep-related search terms (“sleep”, “insomnia”, “somnolence”, or “snoring”) and AR-related search terms (“rhinitis”, “rhino conjunctivitis”, “nasal allergy”, or “hay fever”) were employed when screening titles/abstracts/keywords of articles. The full electronic search strategy can be found in the S1 File. Studies that met the inclusion criteria were retrieved for a full-text review, unless the article was unavailable even after every attempt at retrieval. To reduce potential selection bias, each article was independently evaluated by two of the investigators (J.L. and Y.W.), and the final decision to include/exclude was made jointly with a third investigator (Y.Z.) according to the basic inclusion criteria.
Inclusion criteria
The following inclusion criteria were applied to the literature search process: (1) cross-sectional, case-control, or cohort studies published in refereed English language journals; (2) the study exposure of interest was AR; (3) for studies comparing differences in sleep (sleep quality score, sleep duration, or incidence of adverse sleep events) between AR and a control group, the outcomes were reported as mean + standard deviation (SD), mean + confident interval (CI), mean + standard error (SE), median + interquartile (IQ), median + range, or number of cases with adverse events; (4) for studies evaluating the effect of AR on sleep-related outcomes, estimation of an odds ratio (OR), risk ratio (RR), or hazard ratio (HR) with 95% CI was provided; and (5) study control group was a population without AR.
Data extraction
Data extraction was performed using a standard data extraction form by one investigator (J.L.) and reviewed by another investigator (Y.W.). Disagreements were resolved through negotiations with a third investigator (Y.Z.) until a consensus was reached. The following information was extracted from included studies: title, last name of the first author, country, number and age of subjects, exposure and outcome, measures of exposure and research endpoints, mean + SD/CI/SE, median + IQ/range, number of cases, and HR/OR/RR with 95% CI.
Assessment of study quality
The quality of studies included in this review were assessed by the Newcastle-Ottawa Scale (NOS) [32]. A study was defined as high quality if the total stars were six or greater.
Statistical analysis
We treated HRs as RRs and converted RRs into ORs [33]. Median and CI/SE/IQ/range were converted into mean + SD in accordance with guidelines laid down by Wan et al [34]. For studies providing continuous data for comparative analysis between AR and control groups, pooled mean difference (MD) with 95% CI was used as the effect size. Pooled OR with 95% CI was used to evaluate studies reporting OR/RR/HR with 95% CI. Random effects model was used to incorporate included studies [35]. We also performed a fixed effects model to compare studies [36], and the results of this fixed effects model can be found in S1–S5 Figs. Statistical heterogeneity was assessed by the I2-heterogeneity test [37], with an I2 > 50% indicating high heterogeneity. To evaluate the effects of different study designs on pooled estimates, we performed a subgroup analysis stratified by study design for outcomes with enough included studies. Subgroup analysis stratified by age, patients with OSA, study design, and measurement of outcome was also conducted for sleep duration. For meta-analysis of three or more studies, we omitted one study each time and then calculated the pooled result in order to detect the impact of any one study on the overall results. Since it is suggested that tests for funnel plot asymmetry should be used only when there are at least 10 studies included in the meta-analysis for adequate power, we did not perform the funnel plot or Egger’s test to evaluate publication bias [38]. All statistical analyses were performed through the “meta” package of R software (R Foundation for Statistical Computing, Vienna, Austria).
Assessment of cumulative evidence
A summary of the overall strength of available evidence was performed using the “Grading of Recommendations Assessment, Development and Evaluation” (GRADE) assessment [39]. Evidence summaries and GRADE assessments were discussed and reviewed by all investigators. A Summary of Findings table was produced by GRADEpro software (McMaster University, Hamilton, Canada) [40].
Results and discussion
Literature search and study characteristics
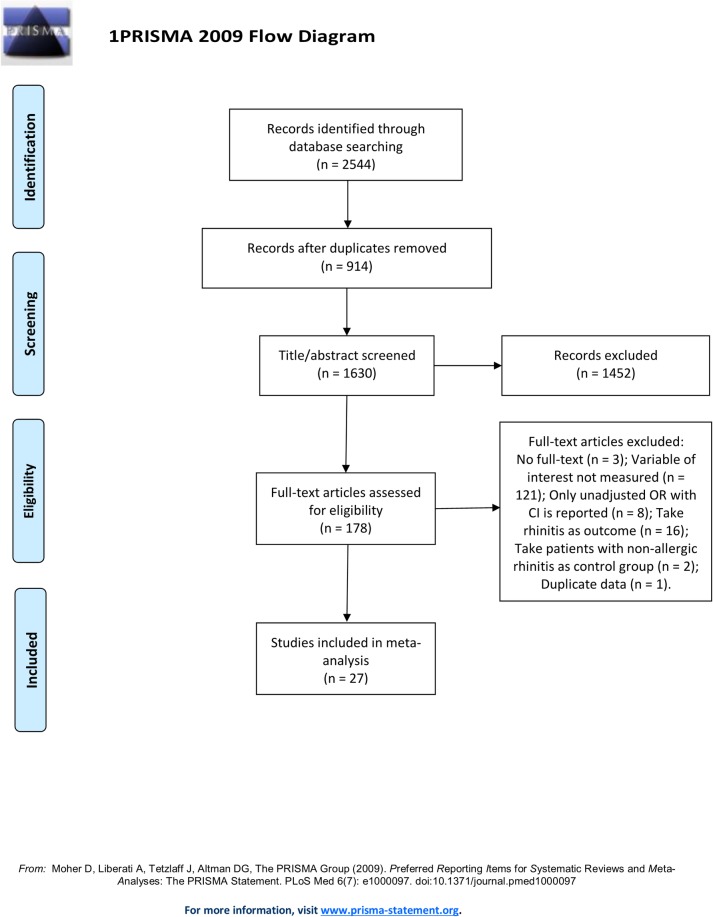
Fig 1 presents the literature search and selection process. 2544 records published before August 2019 were identified. After title, abstract, keyword, and full-text screening, 27 articles were included. The S1 Table lists studies that superficially met the eligibility criteria during full-text screenings; however, failed to meet the criteria on further inspection.
Fig 1. Flow diagram of the literature search and selection processes.
The characteristics of included studies are summarized in Table 1. A total of 240,706,026 patients (19,444,043 AR cases) were included from 13 cross-sectional studies, 10 case-control studies, and 4 cohort studies. Both adult and pediatric patients were included. Medical records, clinical examination findings, skin prick test results, self-reported questionnaires, and face-to-face interviews were reviewed to confirm AR. Sleep–related outcomes were collected and confirmed by medical records, clinical examination findings, self-reported questionnaires, polysomnography (PSG) results, actigraphy results, and face-to-face interviews.
Table 1. Characteristics of included studies.
| Study | Age | Sample size/AR cases | Study type | Measurement-AR | Measurement-sleep outcome | Outcomes |
|---|---|---|---|---|---|---|
| Roxbury et al., 2018 | 45.6 (44.0–47.11) | 5556/1797 | Cross-sectional | Self-reported | Self-reported | Sleep duration, SDB, snoring, OSA, insomnia, restless sleep, use of sleeping pills, daytime dysfunction |
| Loekmanwidjaja et al., 2018 | 4–10 | 167/112 | Case-controlled | Medical records | Self-reported | Sleep duration, daytime sleepiness |
| Lai et al., 2018 | <18 | 655529/327928 | Cohort | Medical records | Medical records | OSA, nocturnal enuresis |
| Filiz et al., 2018 | 8–18 | 287/143 | Cross-sectional | Medical records, clinical examination, and skin prick test | Face-to-face interview | Sleep duration, restless sleep, PSQI outcomes, daytime dysfunction |
| Zhou et al., 2017 | 47±0.2 | 240000000/19100000 | Cross-sectional | Self-reported | Self-reported | Sleep duration |
| Zheng et al., 2017 | 18–70 | 171/65 | Cross-sectional | Medical records, clinical examination, and skin prick test | PSG | Sleep duration, OSA, PSG outcomes |
| Tsai et al., 2017 | 5–18 | 8516/4191 | Case-controlled | Medical records, clinical examination | Medical records | Nocturnal enuresis |
| Nguyen-Hoang et al., 2017 | 9.5±2.1 | 85/52 | Case-controlled | Clinical examination | Medical records | OSA |
| Kim et al., 2017 | 68.3±5.6 | 348/57 | Cross-sectional | Self-reported | PSG | SDB, PSG outcomes, PSQI outcomes |
| Hui et al., 2017 | 49.61±16.27 | 1028/- | Cross-sectional | Medical records | Medical records | OSA |
| Di et al., 2016 | 3–14 | 135/57 | Case-controlled | Medical records, clinical examination, and skin prick test | PSG | PSG outcomes |
| Trikojat et al., 2015 | 18–45 | 83/41 | Case-controlled | Medical records, clinical examination, and skin prick test | Self-reported | Sleep duration, PSQI outcomes, daytime dysfunction |
| Poachanukoon et al., 2015 | 10.6±2.5 | 175/65 | Case-controlled | Medical records, clinical examination, and skin prick test | Self-reported | Sleep duration, difficult waking up, snoring, morning headache, mouth breathing, night sweating, nocturnal enuresis, OSA daytime sleepiness, restless sleep, SDB, sleep bruxism |
| Ng et al., 2014 | 15.3±1.7 | 175/65 | Cohort | Self-reported | Self-reported | Snoring |
| Cai et al., 2013 | - | 1993/123 | Cross-sectional | Medical records | Self-reported | OSA |
| Zhang et al., 2012 | 46.3±5.1 | 2291/211 | Cohort | Self-reported | Self-reported | Restless sleep |
| So et al., 2012 | 9.2 (7.7–10.7) | 6381/2661 | Cross-sectional | Self-reported | Self-reported | Night sweating |
| Park et al., 2012 | 20–68 | 112/37 | Case-controlled | Clinical examination and skin prick test | PSG and self-reported | Sleep duration, AHI, PSG outcomes, ESS |
| Meng et al., 2011 | 18–60 | 128/98 | Case-controlled | Self-reported | PSG | PSG outcomes |
| Li et al., 2010 | 5–14 | 6369/2823 | Cross-sectional | Self-reported | Self-reported | Snoring |
| Rimmer et al., 2009 | >18 | 20/10 | Case-controlled | Self-reported | Actigraphy | Sleep duration |
| Hiraki et al., 2008 | 39.4±9.6 | 852/112 | Cross-sectional | Self-reported | Self-reported | Daytime sleepiness, snoring, ESS |
| Dixon et al., 2006 | ≥15 | 1969/1133 | Cohort | Self-reported | Self-reported | ESS, PSQI outcomes |
| Sogut et al., 2005 | 8.1±1.9 | 992/332 | Case-controlled | Self-reported | Self-reported | Snoring |
| Ng et al., 2005 | 6–12 | 3047/1242 | Cross-sectional | Self-reported | Self-reported | Daytime sleepiness, OSA |
| Chng et al., 2004 | 4–7 | 9362/674 | Cross-sectional | Self-reported | Self-reported | Snoring |
| Anuntaseree et al., 2001 | 7.25±0.58 | 255/14 | Cross-sectional | Self-reported | Self-reported | Snoring |
AR: allergic rhinitis; ESS: Epworth Sleepiness Scale; HS: habitual snoring; NAR: non-allergic rhinitis; OSA: obstructive sleep apnea; PSG: polysomnography; PSQI: Pittsburgh Sleep Quality Index; REM: rapid eye movement; SDB: sleep-disordered breathing.
Comparative analyses of sleep outcomes between AR patients and controls
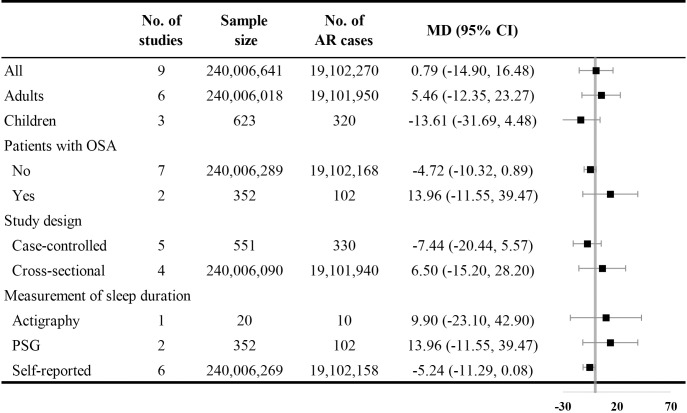
Nine studies reported sleep durations of AR and control groups. Pooled results showed no significant difference in sleep duration between the groups [MD with 95% CI = 0.79 (-14.90, 16.48)] with high heterogeneity (I2 = 93.00%). Subgroup analysis stratified by age, presence of OSA, study design, and measurement of sleep duration were conducted, but no significant differences were observed (Fig 2).
Fig 2. Comparative analysis of sleep duration.
AR: allergic rhinitis; CI: confidence interval; MD: mean difference; OSA: obstructive sleep apnea; PSG: polysomnography.
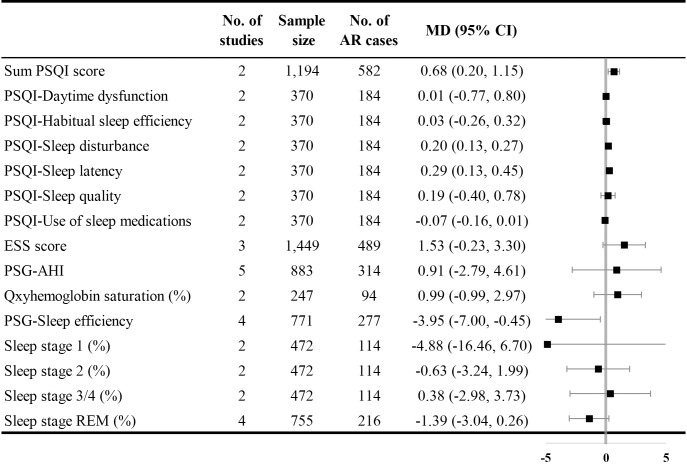
Four studies reported comparisons of Pittsburgh Sleep Quality Index (PSQI) scores in patients with AR. Compared with the control group, the AR group presented with higher sum PSQI scores [MD with 95% CI = 0.68 (0.20, 1.15)], higher sleep disturbances scores [MD with 95% CI = 0.20 (0.13, 0.27)], and higher sleep latency scores (MD with 95% CI = 0.29 (0.13, 0.45)). The I2 was 20.90% for the summed PSQI score and 0.00% for the sleep disturbance and sleep latency scores. Three studies provided comparisons of the Epworth Sleepiness Scale (ESS) in patients with AR. The AR group presented with a higher, though not significant, sum ESS score [MD with 95% CI = 1.53 (-0.23, 3.30)]. Five articles reporting PSG outcomes showed lower scores of sleep efficiency [MD with 95% CI = -3.95 (-7.00, -0.45), I2 = 89.00%] in the AR group (Fig 3).
Fig 3. Comparative analysis of PSQI scale, ESS scale, and PSG outcomes.
AHI: apnea-hypopnea index; ESS: Epworth Sleepiness Scale; PSQI: Pittsburgh Sleep Quality Index; REM: rapid eye movement.
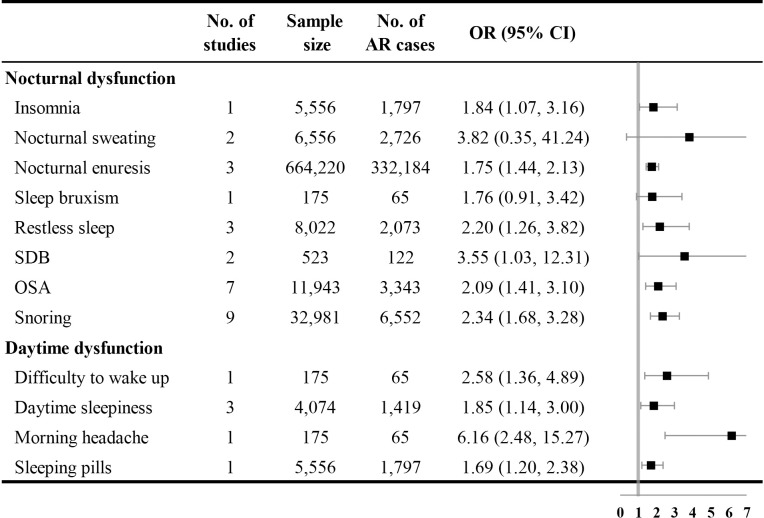
Adjusted associations between AR and sleep outcomes
Fig 4 shows the adjusted relationship between AR and sleep outcomes. Patients with AR were more likely to suffer from nocturnal sleep-related dysfunctions, including insomnia [OR with 95% CI = 1.84 (1.07, 3.16)], nocturnal enuresis [OR with 95% CI = 1.75 (1.44, 2.13), I2 = 28.50%], restless sleep [OR with 95% CI = 2.20 (1.26, 3.82), I2 = 51.20%], SDB [OR with 95% CI = 3.55 (1.03, 12.31), I2 = 85.80%], OSA [OR with 95% CI = 2.09 (1.41, 3.10), I2 = 53.60%], and snoring [OR with 95% CI = 2.34 (1.68, 3.28), I2 = 83.40%]. AR was also associated with a higher risk of daytime sleep-related dysfunctions, including difficulty waking up [OR with 95% CI = 2.58 (1.36, 4.89)], daytime sleepiness [OR with 95% CI = 1.85 (1.14, 3.00), I2 = 53.20%], morning headache [OR with 95% CI = 6.16 (2.48, 15.27)], and the use of sleeping pills [OR with 95% CI = 1.69 (1.20, 2.38)].
Fig 4. Forest plot for adjusted associations between AR and sleep outcomes.
AR: allergic rhinitis; CI: confidence interval; OR: odds ratio; OSA: obstructive sleep apnea; SDB: sleep-disordered breathing.
Evaluation of the effect of study design
We conducted subgroup analysis stratified by study design for sleep duration, apnea-hypopnea index (AHI), sleep efficiency measured by PSG, the percent of sleep stage REM measured by PSG, OSA, and snoring. Significant differences in results from different study designs were observed for AHI, sleep efficiency measured by PSG, and the percent of sleep stage REM measured by PSG, indicating the potential influence of study design on pooled results. Detailed information is shown in the supplemental material (S6–S11 Figs).
Assessment of study quality and sensitivity analysis
Most of the included studies were of high quality according to the NOS criteria. Detailed information is shown in S2–S4 Tables.
By omitting one study each time using a random effects model, sensitivity analysis was conducted for meta-analyses of sleep duration, ESS score, AHI assessed by PSG, sleep efficiency assessed by PSG, the percentage of sleep stage REM assessed by PSG, nocturnal enuresis, restless sleep, OSA, snoring, and daytime sleepiness. Pooled results of sleep duration and AHI assessed by PSG were significantly sensitive to the study of Zheng et al [30], because the direction of the synthesized MD changed after it was omitted. The results of the ESS score, sleep efficiency evaluated by PSG, nocturnal enuresis, restless sleep, and daytime sleepiness also showed instability. Detailed information is presented in S12–S21 Figs.
Assessment of cumulative evidence
The overall quality of evidence using GRADE’s Summary of Findings table was judged to be low or very low. Risk of bias, inconsistencies (methodological, clinical, and statistical), indirectness, and imprecision were found due to lack of adjusting confounding factors, incorporation of different age groups and study designs, self-reported AR, and sleep outcomes. The Summary of Findings table can be found in S5 and S6 Tables.
In the present review, no significant differences in sleep duration between the AR and control groups were observed. AR patients presented with increased sleep quality scores, sleep disturbance scores, and sleep latency scores on the PSQI scale and a decreased sleep efficiency score using PSG. AR was also found to be associated with a higher risk of nocturnal sleep-related dysfunctions, including insomnia, nocturnal enuresis, restless sleep, SDB, OSA, and snoring. Additionally, AR was found to be associated with a higher risk of daytime sleep-related dysfunctions, including difficulty waking up, daytime sleepiness, morning headache, and the use of sleeping pills.
The main underlying mechanisms for the association between AR and altered sleep patterns can be summarized as follows: (1) inflammatory cytokines related to AR produce fatigue directly; (2) AR symptoms and underlying pathophysiologic changes affect sleep indirectly; and (3) the effect of autonomic system dysfunction in patients with AR.
Inflammatory mediators, including histamine, are released in AR and have a direct influence on the central nervous system, contributing to sleep disturbances and daytime sleepiness [41, 42]. Histamine can also affect the regulation of the sleep-wake cycle, which may result in arousal disorder [41, 43]. AR also induces decreased levels of the interleukins (ILs)-1β, IL-4, IL-6 and IL-10, which may increase REM sleep (important in the restorative function of sleep), decrease sleep onset latency, improve circadian rhythm, and regulate slow wave sleep [44]. These changes contribute to why patients with AR often have difficulties with overnight sleep and daytime tiredness.
Symptoms of AR include nasal congestion, rhinorrhea, sneezing, and pruritus. Among these symptoms, nasal obstruction is the most troublesome one for patients [45–47]. Nasal congestion is considered to be a major factor interfering with sleep quality and inducing daytime somnolence. Previous studies suggest that nasal obstruction contributes to higher risks of OSA [48–50] and SDB [51, 52]. The role of nasal congestion as a risk factor for snoring has also been confirmed by a population-based cohort study [53]. A negative effect of nasal congestion was also found on quality of life and daytime productivity [54, 55]. Data on sleep-related end points from clinical trials of nasal decongestants are associated with improved sleep, reduced daytime fatigue, and improved quality of life [56]. Other symptoms including cough and sputum production also contribute to poor sleep quality and sleep disorders [57, 58].
Imbalance of the autonomic system in AR is also thought to be involved to the association between AR and sleep impairment [59]. As one of the most powerful autonomic nerve reflexes, the trigeminocardiac reflex (TCR) is believed to directly influence the development of SDB, OSA, REM sleep apnea, and nasal congestion [60–62]. The nasotrigeminal reflex, a peripheral nervous system equivalent of the TCR, is also thought to have a potential influence on sleep impairment [60]. The extent of autonomic dysfunction in AR and sleep disturbances is still not well-established and needs further investigation.
To the best of our knowledge, this is the first systematic review and meta-analysis evaluating the association between AR and sleep based on observational investigations. A 2018 systematic review focused on the association between AR and OSA and applied a meta-analysis of population-based studies; however, this article concentrated mainly on the prevalence of AR in subjects with or without OSA/SDB [63]. Another related review examined AR and sleep impairment, but focused mainly on the mechanism of their association and the consequences of disordered sleep [64–71].
There are some limitations to the current study. First, most of the included studies are cross-sectional or case-controlled, which do not allow for inferences of causal relationships. Second, some results from this study’s meta-analyses display sensitivity to a single study included in the analysis, potentially due to the limited number of included studies. In terms of the sensitivity analysis of sleep duration and AHI assessed by PSG, the inverse MD is caused by the study of Zheng et al., which was conducted in patients with OSA. We included a limited number of studies focusing on OSA patients and failed to detect a difference between the normal population and patients with OSA. More investigations conducted in patients with OSA are needed. Third, some outcomes of sleep impairment are confirmed by self-reported questionnaires, which are vulnerable to recall bias and potentially affected by social norms. Further longitudinal research with objective measurements are warranted.
Conclusions
There is a significant association of AR with sleep characteristics; however, due to the very low GRADE level of evidence, caution is required when interpreting our results.
Supporting information
CI: confidence interval; MD: mean difference; SD: standard deviation.
(TIF)
CI: confidence interval; MD: mean difference; PSQI: Pittsburgh Sleep Quality Index; SD: standard deviation.
(TIF)
CI: confidence interval; ESS: Epworth Sleepiness Scale; MD: mean difference; SD: standard deviation.
(TIF)
AHI: apnea-hypopnea index; CI: confidence interval; ESS: Epworth Sleepiness Scale; MD: mean difference; PSG: polysomnography; REM: rapid eye movement; SD: standard deviation.
(TIF)
AR: allergic rhinitis; CI: confidence interval; OR: odds ratio; OSA: obstructive sleep apnea; SDB: sleep-disordered breathing.
(TIF)
CI: confidence interval; MD: mean difference; SD: standard deviation.
(TIF)
AHI: apnea-hypopnea index; CI: confidence interval; MD: mean difference; SD: standard deviation.
(TIF)
AHI: apnea-hypopnea index; CI: confidence interval; MD: mean difference; PSG: polysomnography; SD: standard deviation.
(TIF)
CI: confidence interval; MD: mean difference; REM: rapid eye movement; SD: standard deviation.
(TIF)
CI: confidence interval; OR: odds ratio; OSA: obstructive sleep apnea.
(TIF)
CI: confidence interval; OR: odds ratio.
(TIF)
CI: confidence interval; MD: mean difference.
(TIFF)
CI: confidence interval; ESS: Epworth Sleepiness Scale; MD: mean difference.
(TIFF)
AHI: apnea-hypopnea index; CI: confidence interval; MD: mean difference; PSG: polysomnography.
(TIFF)
CI: confidence interval; MD: mean difference; PSG: polysomnography.
(TIFF)
CI: confidence interval; MD: mean difference; PSG: polysomnography; REM: rapid eye movement.
(TIFF)
CI: confidence interval; OR: odds ratio.
(TIFF)
CI: confidence interval; OR: odds ratio.
(TIFF)
CI: confidence interval; OR: odds ratio; OSA: obstructive sleep apnea.
(TIFF)
CI: confidence interval; OR: odds ratio.
(TIFF)
CI: confidence interval; OR: odds ratio.
(TIFF)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
AHI: apnea-hypopnea index; CI: confidence interval; ESS: Epworth Sleepiness Scale; MD: mean difference; REM: rapid eye movement; PSQI: Pittsburgh Sleep Quality Index; PSG: polysomnography.
(DOCX)
CI: confidence interval; MD: mean difference; OR: odds ratio; OSA: obstructive sleep apnea; SD: standard deviation; SDB: sleep-disordered breathing.
(DOCX)
(DOCX)
(TXT)
Acknowledgments
We thank Editage (www.editage.com) for English language editing.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
JM L received award from South Campus of Guang’anmen Hospital, China Academy of Chinese Medical Sciences (http://www.gamhnq.cn/). The grant number is 121102244009641085. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Brożek JL, Bousquet J, Baena-Cagnani CE, Bonini S, Canonica GW, Casale TB, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines: 2010 Revision. J. Allergy Clin. Immunol. 2010;126(3):466–76. 10.1016/j.jaci.2010.06.047 [DOI] [PubMed] [Google Scholar]
- 2.Roberts G, Xatzipsalti M, Borrego LM, Custovic A, Halken S, Hellings PW, et al. Paediatric rhinitis: position paper of the European Academy of Allergy and Clinical Immunology. Allergy. 2013;68(9):1102–16. Epub 2013/08/21. 10.1111/all.12235 . [DOI] [PubMed] [Google Scholar]
- 3.Bousquet PJ, Demoly P, Devillier P, Mesbah K, Bousquet J. Impact of allergic rhinitis symptoms on quality of life in primary care. Int Arch Allergy Immunol. 2013;160(4):393–400. Epub 2012/11/28. 10.1159/000342991 . [DOI] [PubMed] [Google Scholar]
- 4.Trikojat K, Buske-Kirschbaum A, Plessow F, Schmitt J, Fischer R. Memory and multitasking performance during acute allergic inflammation in seasonal allergic rhinitis. Clin Exp Allergy 2017;47(4):479–87. Epub 2017/01/26. 10.1111/cea.12893 . [DOI] [PubMed] [Google Scholar]
- 5.Seok H, Yoon JH, Won JU, Lee W, Lee JH, Jung PK, et al. Concealing Emotions at Work Is Associated with Allergic Rhinitis in Korea. Tohoku J Exp Med. 2016;238(1):25–32. Epub 2015/12/17. 10.1620/tjem.238.25 . [DOI] [PubMed] [Google Scholar]
- 6.Devillier P, Bousquet J, Salvator H, Naline E, Grassin-Delyle S, de Beaumont O. In allergic rhinitis, work, classroom and activity impairments are weakly related to other outcome measures. Clin Exp Allergy. 2016;46(11):1456–64. Epub 2016/10/30. 10.1111/cea.12801 . [DOI] [PubMed] [Google Scholar]
- 7.Roxbury CR, Qiu M, Shargorodsky J, Lin SY. Association between allergic rhinitis and poor sleep parameters in U.S. adults. Int Forum Allergy Rhinol. 2018;8(10):1098–106. 10.1002/alr.22174 [DOI] [PubMed] [Google Scholar]
- 8.Meltzer EO, Bukstein DA. The economic impact of allergic rhinitis and current guidelines for treatment. Ann Allergy Asthma Immunol. 2011;106(2 Suppl):S12–6. Epub 2011/02/10. 10.1016/j.anai.2010.10.014 . [DOI] [PubMed] [Google Scholar]
- 9.Lo JC, Groeger JA, Santhi N, Arbon EL, Lazar AS, Hasan S, et al. Effects of Partial and Acute Total Sleep Deprivation on Performance across Cognitive Domains, Individuals and Circadian Phase. Plos One 2012;7(9):e45987 10.1371/journal.pone.0045987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Walker MP, Stickgold RJN. Sleep-Dependent Learning and Memory Consolidation. Neuron. 2004;44(1):121–33. 10.1016/j.neuron.2004.08.031 [DOI] [PubMed] [Google Scholar]
- 11.Spiegel K, Leproult R, Cauter E, Van %J Lancet. Impact of sleep debt on metabolic and endocrine function. The lancet. 1999;354(9188):1435–9. [DOI] [PubMed] [Google Scholar]
- 12.Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003. Mar 1;26(2):117–26. 10.1093/sleep/26.2.117 [DOI] [PubMed] [Google Scholar]
- 13.Dinges, David F, Douglas, Steven D, Hamarman Steffi, et al. Sleep deprivation and human immune function. Adv Neuroimmunol. 1995;5(2):97–110. 10.1016/0960-5428(95)00002-j [DOI] [PubMed] [Google Scholar]
- 14.Martin BJJEJAPOP. Effect of sleep deprivation on tolerance of prolonged exercise. Eur J Appl Physio Occup Physiol. 1981;47(4):345–54. [DOI] [PubMed] [Google Scholar]
- 15.Wang D, Zhou Y, Guo Y, Zhang R, Li W, He M, et al. The effect of sleep duration and sleep quality on hypertension in middle-aged and older Chinese: the Dongfeng-Tongji Cohort Study. Sleep medicine. 2017;40:78–83. Epub 2017/12/10. 10.1016/j.sleep.2017.09.024 . [DOI] [PubMed] [Google Scholar]
- 16.Cai S, Tan S, Gluckman PD, Godfrey KM, Saw SM, Teoh OH, et al. Sleep Quality and Nocturnal Sleep Duration in Pregnancy and Risk of Gestational Diabetes Mellitus. Sleep. 2017;40(2). Epub 2017/04/02. 10.1093/sleep/zsw058 . [DOI] [PubMed] [Google Scholar]
- 17.Fatima Y, Doi SA, Mamun AA. Sleep quality and obesity in young subjects: a meta-analysis. Obes Rev. 2016;17(11):1154–66. Epub 2016/07/16. 10.1111/obr.12444 . [DOI] [PubMed] [Google Scholar]
- 18.Drager LF, McEvoy RD, Barbe F, Lorenzi-Filho G, Redline S. Sleep Apnea and Cardiovascular Disease: Lessons From Recent Trials and Need for Team Science. Circulation. 2017;136(19):1840–50. Epub 2017/11/08. 10.1161/CIRCULATIONAHA.117.029400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Akerstedt T, Narusyte J, Alexanderson K, Svedberg P. Sleep Duration, Mortality, and Heredity-A Prospective Twin Study. Sleep. 2017;40(10). Epub 2017/10/05. 10.1093/sleep/zsx135 . [DOI] [PubMed] [Google Scholar]
- 20.Tsai JD, Chen HJ, Ku MS, Chen SM, Hsu CC, Tung MC, et al. Association between allergic disease, sleep-disordered breathing, and childhood nocturnal enuresis: a population-based case-control study. Pediatric nephrology (Berlin, Germany). 2017;32(12):2293–301. Epub 2017/07/25. 10.1007/s00467-017-3750-0 . [DOI] [PubMed] [Google Scholar]
- 21.Nguyen-Hoang Y, Nguyen-Thi-Dieu T, Duong-Quy S. Study of the clinical and functional characteristics of asthmatic children with obstructive sleep apnea. J Asthma Allergy. 2017;10:285–92. 10.2147/JAA.S147005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou S, Hur K, Shen J, Wrobel B. Impact of sinonasal disease on depression, sleep duration, and productivity among adults in the United States. Laryngoscope Investig otolaryngology. 2017;2(5):288–94. 10.1002/lio2.87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leger D, Bonnefoy B, Pigearias B, de la Giclais B, Chartier A. Poor sleep is highly associated with house dust mite allergic rhinitis in adults and children. Allergy, Asthma and Clinical Immunology. 2017;13(1). 10.1080/1744666X.2017.1232620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Drumond CL, Souza DS, Serra-Negra JM, Marques LS, Ramos-Jorge ML, Ramos-Jorge J. Respiratory disorders and the prevalence of sleep bruxism among schoolchildren aged 8 to 11 years. Sleep and Breathing. 2017;21(1):203–8. 10.1007/s11325-017-1466-9 [DOI] [PubMed] [Google Scholar]
- 25.Poachanukoon O, Kitcharoensakkul M. Snoring and sleep problems in children with and without allergic rhinitis: A case control study. J Med Assoc Thai. 2015;98:S138–S44. [PubMed] [Google Scholar]
- 26.Lai PH, Yang PS, Lai WY, Lin CL, Hsu CY, Wei CC. Allergic rhinitis and the associated risk of nocturnal enuresis in children: a population-based cohort study. Int Forum Allergy Rhinol. 2018;8(11):1260–6. 10.1002/alr.22219 [DOI] [PubMed] [Google Scholar]
- 27.Ng TP, Tan WC. Prevalence and determinants of excessive daytime sleepiness in an Asian multi-ethnic population. Sleep medicine. 2005;6(6):523–9. 10.1016/j.sleep.2005.01.007 [DOI] [PubMed] [Google Scholar]
- 28.Jernelov S, Lekander M, Almqvist C, Axelsson J, Larsson H. Development of atopic disease and disturbed sleep in childhood and adolescence—a longitudinal population-based study. Clin Exp Allergy. 2013;43(5):552–9. Epub 2013/04/23. 10.1111/cea.12087 . [DOI] [PubMed] [Google Scholar]
- 29.Loekmanwidjaja J, Carneiro ACF, Nishinaka MLT, Munhoes DA, Benezoli G, Wandalsen GF, et al. Sleep disorders in children with moderate to severe persistent allergic rhinitis. Braz J Otorhinolaryngol. 2018;84(2):178–84. 10.1016/j.bjorl.2017.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zheng M, Wang X, Ge S, Gu Y, Ding X, Zhang Y, et al. Allergic and non-allergic rhinitis are common in obstructive sleep apnea but not associated with disease severity. J Clin Sleep Med. 2017;13(8):959–66. 10.5664/jcsm.6694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clinical research ed). 2009;339:b2700 Epub 2009/07/23. 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hartling L, Milne A, Hamm MP, Vandermeer B, Ansari M, Tsertsvadze A, et al. Testing the Newcastle Ottawa Scale showed low reliability between individual reviewers. J Clin Epidemiol. 2013;66(9):982–93. Epub 2013/05/21. 10.1016/j.jclinepi.2013.03.003 . [DOI] [PubMed] [Google Scholar]
- 33.Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. Jama. 1998;280(19):1690–1. Epub 1998/12/01. 10.1001/jama.280.19.1690 . [DOI] [PubMed] [Google Scholar]
- 34.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC medical research methodology. 2014;14:135 Epub 2014/12/20. 10.1186/1471-2288-14-135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update.Contemp Clin Trials. 2007;28(2):105–14. Epub 2006/06/30. 10.1016/j.cct.2006.04.004 . [DOI] [PubMed] [Google Scholar]
- 36.Cheung MW. Fixed- and random-effects meta-analytic structural equation modeling: examples and analyses in R. Behavior research methods. 2014;46(1):29–40. Epub 2013/06/29. 10.3758/s13428-013-0361-y . [DOI] [PubMed] [Google Scholar]
- 37.DerSimonian R, Laird N. Meta-analysis in clinical trials revisited. Contemp Clin Trials. 2015;45(Pt A):139–45. Epub 2015/09/08. 10.1016/j.cct.2015.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Higgins JPT GSe. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 The Cochrane Collaboration, 2011 [updated March 2011]. Available from: www.handbook.cochrane.org.
- 39.Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–6. Epub 2011/01/07. 10.1016/j.jclinepi.2010.07.015 . [DOI] [PubMed] [Google Scholar]
- 40.The Grading of Recommendations Assessment DaEGWG. GRADEpro|GDT. Available from: https://gdt.gradepro.org/app/.
- 41.Naganuma F, Nakamura T, Yoshikawa T, Iida T, Miura Y, Karpati A, et al. Histamine N-methyltransferase regulates aggression and the sleep-wake cycle. Scientific reports. 2017;7(1):15899 Epub 2017/11/23. 10.1038/s41598-017-16019-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shan L, Dauvilliers Y, Siegel JM. Interactions of the histamine and hypocretin systems in CNS disorders. Nat Rev Neurol. 2015;11(7):401–13. Epub 2015/06/24. 10.1038/nrneurol.2015.99 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Williams RH, Chee MJ, Kroeger D, Ferrari LL, Maratos-Flier E, Scammell TE, et al. Optogenetic-mediated release of histamine reveals distal and autoregulatory mechanisms for controlling arousal. The Journal of neuroscience: the official journal of the Society for Neuroscience. 2014;34(17):6023–9. Epub 2014/04/25. 10.1523/jneurosci.4838-13.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zheng M, Wang X, Zhang L. Association between allergic and nonallergic rhinitis and obstructive sleep apnea. Current opinion in allergy and clinical immunology. 2018;18(1):16–25. Epub 2017/11/15. 10.1097/ACI.0000000000000414 . [DOI] [PubMed] [Google Scholar]
- 45.Meltzer EO, Blaiss MS, Derebery MJ, Mahr TA, Gordon BR, Sheth KK, et al. Burden of allergic rhinitis: results from the Pediatric Allergies in America survey. J Allergy Clin Immunol. 2009;124(3 Suppl):S43–70. Epub 2009/07/14. 10.1016/j.jaci.2009.05.013 . [DOI] [PubMed] [Google Scholar]
- 46.Meltzer EO, Nathan R, Derebery J, Stang PE, Campbell UB, Yeh WS, et al. Sleep, quality of life, and productivity impact of nasal symptoms in the United States: findings from the Burden of Rhinitis in America survey. Allergy Asthma Proc. 2009;30(3):244–54. Epub 2009/06/25. 10.2500/aap.2009.30.3230 . [DOI] [PubMed] [Google Scholar]
- 47.Eifan AO, Durham SR. Pathogenesis of rhinitis. Clinical and experimental allergy: Clin Exp Allergy. 2016;46(9):1139–51. Epub 2016/07/20. 10.1111/cea.12780 . [DOI] [PubMed] [Google Scholar]
- 48.Fernandes MBL, Salgueiro A, Bighetti EJB, Trindade-Suedam IK, Trindade IEK. Symptoms of Obstructive Sleep Apnea, Nasal Obstruction, and Enuresis in Children With Nonsyndromic Cleft Lip and Palate: A Prevalence Study. The Cleft palate-craniofacial journal: official publication of the American Cleft Palate-Craniofacial Association. 2019;56(3):307–13. Epub 2018/05/19. 10.1177/1055665618776074 . [DOI] [PubMed] [Google Scholar]
- 49.Craig TJ, Teets S, Lehman EB, Chinchilli VM, Zwillich C. Nasal congestion secondary to allergic rhinitis as a cause of sleep disturbance and daytime fatigue and the response to topical nasal corticosteroids. J Allergy Clin Immunol. 1998;101(5):633–7. Epub 1998/05/26. 10.1016/s0091-6749(98)70171-x . [DOI] [PubMed] [Google Scholar]
- 50.MacLean JE, DeHaan K, Chowdhury T, Nehme J, Bendiak GN, Hoey L, et al. The scope of sleep problems in Canadian children and adolescents with obesity. Sleep medicine. 2018;47:44–50. Epub 2018/06/09. 10.1016/j.sleep.2018.03.006 . [DOI] [PubMed] [Google Scholar]
- 51.Krakow B, Foley-Shea M, Ulibarri VA, McIver ND, Honsinger R. Prevalence of potential nonallergic rhinitis at a community-based sleep medical center. Sleep and breathing 2016;20(3):987–93. Epub 2016/03/20. 10.1007/s11325-016-1322-3 . [DOI] [PubMed] [Google Scholar]
- 52.Izci Balserak B. Sleep disordered breathing in pregnancy. Breathe (Sheffield, England). 2015;11(4):268–77. Epub 2016/04/12. 10.1183/20734735.009215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Young T, Finn L, Palta M. Chronic nasal congestion at night is a risk factor for snoring in a population-based cohort study. Archives of internal medicine. 2001;161(12):1514–9. Epub 2001/06/28. 10.1001/archinte.161.12.1514 . [DOI] [PubMed] [Google Scholar]
- 54.Manzi B, Sykes KJ, Wei JL. Sinonasal Quality of Life in Children After Outfracture of Inferior Turbinates and Submucous Inferior Turbinoplasty for Chronic Nasal Congestion. JAMA otolaryngology—head & neck surgery. 2017;143(5):452–7. Epub 2017/02/06. 10.1001/jamaoto.2016.3889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shedden A. Impact of nasal congestion on quality of life and work productivity in allergic rhinitis: findings from a large online survey. Treat Respir Med. 2005;4(6):439–46. Epub 2005/12/13. 10.2165/00151829-200504060-00007 . [DOI] [PubMed] [Google Scholar]
- 56.Craig TJ, Sherkat A, Safaee S. Congestion and sleep impairment in allergic rhinitis. Curr Allergy Asthma Rep. 2010;10(2):113–21. Epub 2010/04/29. 10.1007/s11882-010-0091-5 . [DOI] [PubMed] [Google Scholar]
- 57.Storms WW. Pharmacologic approaches to daytime and nighttime symptoms of allergic rhinitis. J Allergy Clin Immunol. 2004;114(5 Suppl):S146–53. Epub 2004/11/13. 10.1016/j.jaci.2004.08.045 . [DOI] [PubMed] [Google Scholar]
- 58.Camhi SL, Morgan WJ, Pernisco N, Quan SF. Factors affecting sleep disturbances in children and adolescents. Sleep medicine. 2000;1(2):117–23. Epub 2000/04/18. 10.1016/s1389-9457(99)00005-2 [DOI] [PubMed] [Google Scholar]
- 59.Tobaldini E, Costantino G, Solbiati M, Cogliati C, Kara T, Nobili L, et al. Sleep, sleep deprivation, autonomic nervous system and cardiovascular diseases. Neurosci Biobehav Rev. 2017;74(Pt B):321–9. Epub 2016/07/12. 10.1016/j.neubiorev.2016.07.004 . [DOI] [PubMed] [Google Scholar]
- 60.Bindu B, Singh GP, Chowdhury T, Schaller B. Rhinitis and sleep disorders: The trigeminocardiac reflex link? Med hypotheses. 2017;103:96–9. Epub 2017/06/03. 10.1016/j.mehy.2017.04.019 . [DOI] [PubMed] [Google Scholar]
- 61.Chowdhury T, Bindu B, Singh GP, Schaller B. Sleep Disorders: Is the Trigemino-Cardiac Reflex a Missing Link? Front Neurol. 2017;8:63 Epub 2017/03/16. 10.3389/fneur.2017.00063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Seppanen TM, Alho OP, Seppanen T. Concomitant dynamic changes in autonomic nervous system function and nasal airflow resistance during allergen provocation. Conference proceedings: Annual International Conference of the IEEE Engineering in Medicine and Biology Society IEEE Engineering in Medicine and Biology Society Annual Conference. 2015;2015:3339–42. Epub 2016/01/07. 10.1109/embc.2015.7319107 . [DOI] [PubMed] [Google Scholar]
- 63.Cao Y, Wu S, Zhang L, Yang Y, Cao S, Li Q. Association of allergic rhinitis with obstructive sleep apnea: A meta-analysis. Medicine. 2018;97(51):e13783 Epub 2018/12/24. 10.1097/MD.0000000000013783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lunn M, Craig T. Rhinitis and sleep. Sleep Med Rev. 2011;15(5):293–9. Epub 2011/02/15. 10.1016/j.smrv.2010.12.001 . [DOI] [PubMed] [Google Scholar]
- 65.Calais CJ, Robertson BD, Beakes DE. Association of allergy/immunology and obstructive sleep apnea. Allergy Asthma Proc. 2016;37(6):443–9. Epub 2016/12/10. 10.2500/aap.2016.37.4001 . [DOI] [PubMed] [Google Scholar]
- 66.Chirakalwasan N, Ruxrungtham K. The linkage of allergic rhinitis and obstructive sleep apnea. Asian Pac J Allergy Immunol. 2014;32(4):276–86. Epub 2014/12/30. . [PubMed] [Google Scholar]
- 67.Thompson A, Sardana N, Craig TJ. Sleep impairment and daytime sleepiness in patients with allergic rhinitis: the role of congestion and inflammation. Ann Allergy Asthma Immunol. 2013;111(6):446–51. Epub 2013/11/26. 10.1016/j.anai.2013.05.020 . [DOI] [PubMed] [Google Scholar]
- 68.Kimple AJ, Ishman SL. Allergy and sleep-disordered breathing. Curr Opin Otolaryngol Head Neck Surg. 2013;21(3):277–81. Epub 2013/04/27. 10.1097/MOO.0b013e32835ff132 . [DOI] [PubMed] [Google Scholar]
- 69.Muliol J, Maurer M, Bousquet J. Sleep and allergic rhinitis. J Investig Allergol Clin Immunol. 2008;18(6):415–9. Epub 2009/01/07. . [PubMed] [Google Scholar]
- 70.Santos CB, Pratt EL, Hanks C, McCann J, Craig TJ. Allergic rhinitis and its effect on sleep, fatigue, and daytime somnolence. Ann Allergy Asthma Immunol. 2006;97(5):579–86; quiz 86–9, 671. Epub 2006/12/15. 10.1016/S1081-1206(10)61084-8 . [DOI] [PubMed] [Google Scholar]
- 71.Staevska MT, Mandajieva MA, Dimitrov VD. Rhinitis and sleep apnea. Current allergy and asthma reports. 2004;4(3):193–9. Epub 2004/04/02. 10.1007/s11882-004-0026-0 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
CI: confidence interval; MD: mean difference; SD: standard deviation.
(TIF)
CI: confidence interval; MD: mean difference; PSQI: Pittsburgh Sleep Quality Index; SD: standard deviation.
(TIF)
CI: confidence interval; ESS: Epworth Sleepiness Scale; MD: mean difference; SD: standard deviation.
(TIF)
AHI: apnea-hypopnea index; CI: confidence interval; ESS: Epworth Sleepiness Scale; MD: mean difference; PSG: polysomnography; REM: rapid eye movement; SD: standard deviation.
(TIF)
AR: allergic rhinitis; CI: confidence interval; OR: odds ratio; OSA: obstructive sleep apnea; SDB: sleep-disordered breathing.
(TIF)
CI: confidence interval; MD: mean difference; SD: standard deviation.
(TIF)
AHI: apnea-hypopnea index; CI: confidence interval; MD: mean difference; SD: standard deviation.
(TIF)
AHI: apnea-hypopnea index; CI: confidence interval; MD: mean difference; PSG: polysomnography; SD: standard deviation.
(TIF)
CI: confidence interval; MD: mean difference; REM: rapid eye movement; SD: standard deviation.
(TIF)
CI: confidence interval; OR: odds ratio; OSA: obstructive sleep apnea.
(TIF)
CI: confidence interval; OR: odds ratio.
(TIF)
CI: confidence interval; MD: mean difference.
(TIFF)
CI: confidence interval; ESS: Epworth Sleepiness Scale; MD: mean difference.
(TIFF)
AHI: apnea-hypopnea index; CI: confidence interval; MD: mean difference; PSG: polysomnography.
(TIFF)
CI: confidence interval; MD: mean difference; PSG: polysomnography.
(TIFF)
CI: confidence interval; MD: mean difference; PSG: polysomnography; REM: rapid eye movement.
(TIFF)
CI: confidence interval; OR: odds ratio.
(TIFF)
CI: confidence interval; OR: odds ratio.
(TIFF)
CI: confidence interval; OR: odds ratio; OSA: obstructive sleep apnea.
(TIFF)
CI: confidence interval; OR: odds ratio.
(TIFF)
CI: confidence interval; OR: odds ratio.
(TIFF)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
AHI: apnea-hypopnea index; CI: confidence interval; ESS: Epworth Sleepiness Scale; MD: mean difference; REM: rapid eye movement; PSQI: Pittsburgh Sleep Quality Index; PSG: polysomnography.
(DOCX)
CI: confidence interval; MD: mean difference; OR: odds ratio; OSA: obstructive sleep apnea; SD: standard deviation; SDB: sleep-disordered breathing.
(DOCX)
(DOCX)
(TXT)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.