Key Points
Question
Is 2 hours per week of protected nonclinical time associated with decreased burnout and increased well-being in otolaryngology residents?
Findings
In this prospective, nonrandomized crossover study, 2 hours per week of protected nonclinical time was associated with decreased burnout and increased well-being in otolaryngology residents.
Meaning
The preliminary results of this intervention in a small sample size are encouraging and warrant further investigation in larger cohorts of residents in randomized clinical trials to confirm the effectiveness of the protected time intervention to decrease burnout and increase well-being.
Abstract
Importance
Burnout among physicians is high, with resulting concern about quality of care. With burnout beginning early in physician training, much-needed data are lacking on interventions to decrease burnout and improve well-being among resident physicians.
Objectives
To design a departmental-level burnout intervention, evaluate its association with otolaryngology residents’ burnout and well-being, and describe how residents used and perceived the study intervention.
Design, Setting, and Participants
A prospective, nonrandomized crossover study was conducted from September 25, 2017, to June 24, 2018, among all 19 current residents in the Department of Otolaryngology at the University of Minnesota. Statistical analysis was performed from June 28 to August 7, 2018.
Interventions
All participants were assigned 2 hours per week of protected nonclinical time alternating with a control period of no intervention at 6-week intervals.
Main Outcomes and Measures
Burnout was measured by the Maslach Burnout Inventory and Mini-Z Survey. Well-being was measured by the Resident and Fellow Well-Being Index and a quality-of-life single-item self-assessment. In addition to a baseline demographic survey, participants completed the aforementioned surveys at approximately 6-week intervals during the study period.
Results
Among the 19 residents in the study (10 men [53%]), the overall protected time intervention (week 0 to week 32) was associated with a mean decrease of 0.63 points (95% CI, −1.03 to −0.22 points) in the Maslach Burnout Inventory emotional exhaustion score, indicating a clinically meaningful decrease in burnout, and a mean decrease of 1.26 points (95% CI, −2.18 to −0.34 points) in the Resident and Fellow Well-Being Index score, indicating a clinically meaningful improvement in well-being. The baseline to week 32 mean changes in the Maslach Burnout Inventory depersonalization score, Maslach Burnout Inventory personal accomplishment score, and quality-of-life single-item self-assessment were not clinically meaningful. There were clinically meaningful improvements in 4 of 6 tested Mini-Z Questionnaire items from baseline to week 32: job stress (weighted κ statistic, 0.21; 95% CI, −0.11 to 0.53), burnout (weighted κ statistic, 0.25; 95% CI, −0.02 to 0.53), control over workload (weighted κ statistic, 0.26; 95% CI, −0.01 to 0.53), and sufficient time for documentation (weighted κ statistic, 0.31; 95% CI, 0.08 to 0.54).
Conclusions and Relevance
This study found that 2 hours per week of protected nonclinical time was associated with decreased burnout and increased well-being in a small sample of otolaryngology residents. Future randomized clinical studies in larger cohorts are warranted to infer causality of decreased burnout and increased well-being as a result of protected nonclinical time.
This nonrandomized crossover study describes the design of a departmental-level burnout intervention, evaluates the intervention’s association with otolaryngology residents’ burnout and well-being, and describes how residents used and perceived the intervention.
Introduction
Burnout, as defined by Maslach et al,1 is a work-related syndrome of emotional exhaustion (EE), depersonalization (DP), and decreased personal accomplishment (PA). Prevalence rates of burnout among resident physicians range from 27% to 89%, depending on specialty, and a recent multisite review identified 44.8% of postgraduate year 2 (PGY2) otolaryngology residents as burned out.2,3,4,5,6 Rosen et al5 found that 4.3% of interns were burned out at the beginning of the year vs 55.3% at the end of the year.
On an individual level, burnout is associated with an increased risk of motor vehicle accidents, medical illnesses, depression, cardiovascular disease, substance abuse, and suicide.4,7,8,9,10,11,12 On a systems level, burnout is associated with decreased productivity, job satisfaction, ability to establish rapport with patients, and ability to work through complex medical decision-making.10 Studies show that burnout is directly associated with increased risk of medical errors, negative effects on patient safety, lower patient satisfaction, and longer postdischarge recovery time.13
Resident burnout is a multifactorial problem. Key factors that have been identified include long work hours; problems with work-life balance; time spent documenting; lack of autonomy, flexibility, and control; excessive workload; inefficient work environment; inadequate support; loss of meaning in work; fatigue; and poor self-care.2,4,9,10 In background pilot data that we collected prior to this study, tertiary care residents (n = 11) in the otolaryngology department at the University of Minnesota spent a mean of 5.5 hours per week on work-related activity outside of the hospital. This time was independent of time spent studying. These data are consistent with findings by Arndt et al,14 who examined the large amount of clerical work performed by physicians during personal time. They found that the average physician spends 28 hours on clinical documentation during nights and weekends each month.
Although a sizeable body of research quantifying the high rate of resident burnout exists, there is a paucity of data on interventions to decrease burnout. The most commonly studied interventions focus on the individual, specifically mindfulness, meditation, stress management, communication, and small group discussions. Results have been inconsistent, with some studies reporting a positive association and other studies reporting no association.15,16,17,18,19,20,21 The only intervention that has been shown to consistently lower overall burnout rates is limiting resident work hours.20 Studies on organizational-level interventions are less common, and it is for this reason that we designed an intervention focused at the departmental level.16 The primary aim of this study was to design a departmental-level burnout intervention for residents in the form of 2 hours per week of protected nonclinical time and to evaluate the association of this intervention with burnout and well-being in otolaryngology residents at a tertiary care residency program. The secondary aim of this study was to describe how individual residents used and perceived the 2 hours per week of protected nonclinical time.
Methods
Participants
All current residents in the Department of Otolaryngology at the University of Minnesota were solicited for participation via email. Inclusion criteria included all resident physicians (PGY1-PGY5) in the department of otolaryngology who were willing to complete the study protocol. Exclusion criteria included the principal investigator. All 19 of the eligible residents verbally consented to participate. This study was approved as exempt from review under federal guidelines 45 CFR Part 46.101(b) category 2 (Surveys/Interviews; Standardized Educational Tests; Observation of Public Behavior) by the University of Minnesota Institutional Review Board.
Study Design
This crossover study lasted 40 weeks and took place from September 25, 2017, to June 24, 2018. During this study period, participants completed 3 different 13-week rotations at 1 of the following hospitals: the University of Minnesota Medical Center, Hennepin County Medical Center, Regions Hospital, Masonic Children’s Hospital, Minneapolis Children’s Hospital, and the Minneapolis Veterans Administration Health Care System. At the beginning of the study, demographic data (sex, relationship status, and program year) and baseline measurements of burnout and well-being were collected. Burnout was measured primarily by the Maslach Burnout Index (MBI) and secondarily by the Mini-Z Survey (Mini-Z). Well-being was measured primarily by the Resident and Fellow Well-Being Index (WBI) and secondarily by a quality-of-life (QOL) single-item self-assessment (SA). Participants completed these 4 questionnaires at approximately 6-week intervals throughout the study. The outcomes of interest for this study are changes from baseline to week 32 (end of intervention).
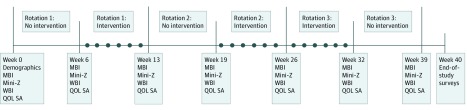
Based on the background pilot data, we designed an intervention for burnout and well-being for residents in our program. When residents were in the intervention phases of the study, they were assigned 2 hours of protected, nonclinical time by the chief resident of the service. Chief residents were instructed to assign this time when clinical learning opportunities were lowest. Each participant acted as his or her own control and was in the intervention phase of the study for the first or last 6 weeks of a quarterly rotation. Residents were concurrently assigned to the same phase of the study (intervention vs control). Participants were not specifically limited in what they could do during their nonclinical time, but they were encouraged to use this time in a way they felt would decrease their own personal burnout and increase their well-being, whether performing work-related administrative duties previously performed on personal time or fulfilling obligations that are integral to personal health and well-being that can only be completed during normal business hours. At the end of their 2 hours of nonclinical time, participants completed a weekly survey detailing how they used the 2 hours that week. At the end of the study, residents and attending physicians completed a survey assessing their overall perceptions and experiences with the study (Figure 1).
Figure 1. Study Design.
The x-axis represents time measured in weeks, from 0 to 40. Starting at week 0, the Maslach Burnout Inventory (MBI), Mini-Z survey (Mini-Z), Resident and Fellow Well-Being Index (WBI), and a quality-of-life single-item self-assessment (QOL SA) were administered to study participants at approximately 6-week intervals. In addition, a demographic survey was conducted at baseline. The circles on the x-axis represent the weeks during the intervention phase of the study in which participants filled out a weekly survey describing how they used their 2 hours of protected, nonclinical time that week. End-of-study surveys were completed by resident participants and attending physicians at week 40.
Outcome Measures
The MBI is a 22-item questionnaire considered to be the reference standard for the assessment of burnout. Three subscales are calculated for EE, DP, and PA. There is no single score that defines burnout; instead, a lower score for EE, a lower score for DP, and a higher score for PA are associated with decreased burnout. As directed by the MBI scoring manual, the MBI subscale scores were calculated as the mean of the component MBI items (9 items for the MBI EE subscale, 5 items for the MBI DP subscale, and 8 items for the MBI PA subscale), with each scale resulting in MBI scale scores that ranged from 0 to 6. The interpretations of MBI scale scores are therefore consistent with the item coding of 0 = never, 1 = a few times a year or less, 2 = once a month or less, 3 = a few times a month, 4 = once a week, 5 = a few times a week, and 6 = every day.1 In this study, a 0.5-point or greater change in MBI scale scores was considered to be a clinically meaningful change because it represents a change from midpoint between 2 response options to the next higher or lower response option.
The Mini-Z is derived from the “Z” Clinician Questionnaire and has been validated with 10 standalone questions.22 Not all questions were relevant to this study, so we chose to analyze the 6 questions that were most related to the topics of resident physician burnout: satisfaction with job (question 1), stress because of job (question 2), burnout (question 3), control over workload (question 4), sufficiency of time for documentation (question 5), and time spent on the electronic medical record at home (question 9). The topics excluded from analysis were the atmosphere in the primary work area (question 6), the alignment of professional values with department leader values (question 7), the efficiency of the care team working together (question 8), and proficiency with the electronic medical record (question 10). Mini-Z items have 5 response options that vary across the items. The single-item burnout measure (question 3) has been validated externally against the MBI with very good correlations with the MBI EE subscale. Respondents who answer the single-item burnout measure (question 3) with a 3 (“burning out”), 4 (“burnout symptoms won’t go away”), or 5 (“completely burned out”) are considered to be burned out.23 In this study, a difference in change proportions (described in the Statistical Analysis subsection) of 30% or more was considered a clinically meaningful change in Mini-Z items.
The WBI is a 7-item validated screening tool designed specifically for resident physicians to evaluate fatigue, depression, burnout, anxiety and stress, and mental and physical QOL.24 The WBI scale score is the total number of negative conditions that were experienced in the past month, resulting in a scale score ranging from 0 to 7 (with lower scores indicating a higher level of well-being). In this study, a 1-point change or greater in the WBI scale score, representing 1 additional or 1 fewer negative condition experienced in the past month, was considered to be clinically meaningful. The QOL SA had 5 response options to the question “Which of the following best describes your overall quality of life?” (0 = as bad as it can be, 1 = somewhat bad, 2 = neutral, 3 = somewhat good, and 4 = as good as it can be), with higher QOL scores indicating higher QOL. In this study, a mean change of 0.50 points or more was considered to be clinically meaningful because it represented a change from the midpoint between 2 response levels to the next response level.
Statistical Analysis
Statistical analysis was performed from June 28 to August 7, 2018. Descriptive statistics included the mean (SD) value for continuous (MBI scales and WBI) and ordinal (QOL SA) variables and the number and percentage for categorical variables (program year, sex, relationship, and Mini-Z items). Mean changes with 95% CIs from baseline to week 32 in MBI, WBI, and QOL SA scale scores were calculated as measures of effect size and precision in scale outcomes. For all scale scores, the mean change was calculated as week 32 score minus baseline score so that a positive mean change indicated an increase from baseline and a negative mean change represented a decrease from baseline. The proportions with positive, negative, and no mean change from baseline to week 32 in Mini-Z items were calculated using all 5 response options. The difference in change proportions (proportion with a positive response minus proportion with a negative response) was calculated as a measure of effect size. The weighted κ statistic25 with 95% CI was calculated to provide a measure of disagreement (ie, change) from baseline to week 32, along with a measure of the precision of the change. The weighted κ statistic contributes more weight to larger magnitudes of change (eg, change to a response option more than 1 level higher or lower). κ Statistics greater than 0 indicate more agreement than would be expected by chance, and κ statistics less than 0 indicate less agreement than would be expected by chance. Mean MBI, WBI, and QOL SA scale scores at interim time points and 7 weeks beyond the last intervention period are represented graphically. However, effect sizes for interim time periods were not reported owing to lack of sensitivity for short-duration changes for some outcome measures. Statistical analysis was performed using SAS, version 9.4 (SAS Institute Inc).
Results
No participants were lost to follow-up. There were no missing data for any demographic or survey items at any time point. Participating residents were evenly distributed across the 5 program years with 4 in each of PGY1, 2, 4, and 5 and 3 residents in PGY3. Residents were also evenly distributed across sex, with 9 women (47%) and 10 men (53%). All but 1 participant was married (n = 9) or not married but in a steady relationship (n = 9).
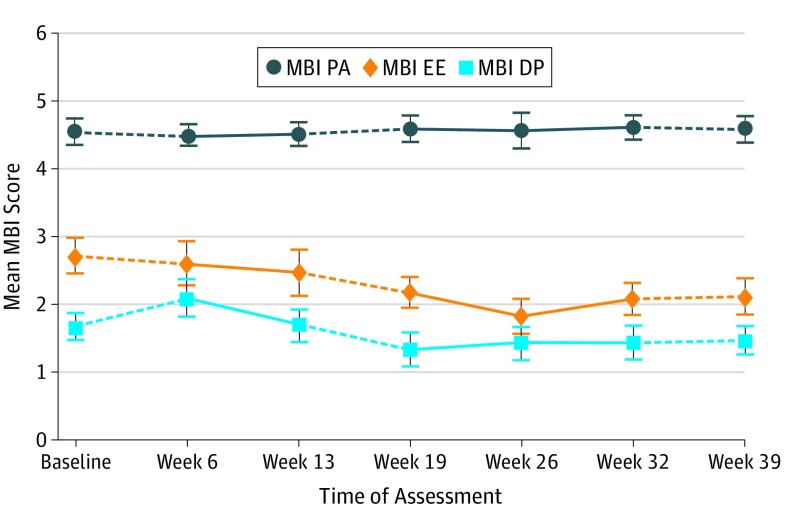
Burnout
Our primary measure of burnout was the MBI. From baseline to week 32, there was a mean decrease of 0.63 points (95% CI, −1.03 to −0.22 points) in the MBI EE score (Figure 2 and Table 1). This level of decrease represents a clinically meaningful decrease in the MBI EE score from a mean (SD) score of 2.70 (1.17) at baseline (where a score of 3 represents “a few times a week” for MBI EE items) to a mean (SD) score of 2.08 (1.04) at week 32 (where a score of 2 represents “once a month or less” for MBI EE items). Baseline to week 32 mean changes in MBI DP and MBI PA scores were not clinically meaningful.
Figure 2. Mean (SE) Maslach Burnout Inventory (MBI) Scores at Each Assessment for 19 Residents.
Solid lines indicate intervention phases, and dashed lines indicate no-intervention phases. DP indicates depersonalization; EE, emotional exhaustion; and PA, personal accomplishment.
Table 1. Mean Change From Baseline to Week 32 in MBI, WBI, and QOL SA Scores.
| Scale | Scale Score Range | Mean (SD) | Baseline to Week 32 Change, Mean (95% CI)a | |
|---|---|---|---|---|
| Baseline (Week 0) Score | Week 32 Score | |||
| No. | 19 | 19 | 19 | |
| MBI EE | 0-6 | 2.70 (1.17) | 2.08 (1.04) | −0.63 (−1.03 to –0.22) |
| MBI DP | 0-6 | 1.67 (0.85) | 1.43 (1.12) | −0.24 (−0.69 to 0.21) |
| MBI PA | 0-6 | 4.55 (0.88) | 4.60 (0.80) | 0.05 (−0.17 to 0.26) |
| WBI | 0-7 | 3.11 (2.56) | 1.84 (2.01) | −1.26 (−2.18 to –0.34) |
| QOL SA | 0-4 | 2.53 (0.96) | 2.89 (0.57) | 0.37 (−0.03 to 0.77) |
Abbreviations: DP, depersonalization; EE, emotional exhaustion; MBI, Maslach Burnout Inventory; PA, personal accomplishment; QOL SA, quality-of-life single-item self-assessment; WBI, Resident and Fellow Well-Being Index.
Mean change may not exactly equal the difference in means at each time point owing to rounding.
Our secondary measure of burnout was the Mini-Z. Based on the single-item burnout measure (question 3), 7 participants (37%) were burned out at the beginning of this study, and 4 participants (21%) were burned out at week 32 (eTable in the Supplement). The results of calculated proportions with positive, negative, and no change from baseline to week 32, along with the difference in change proportions and weighted κ statistics for agreement for the 6 Mini-Z items, are reported in Table 2. The difference in change proportions indicated that there were clinically meaningful improvements for 4 of the 6 Mini-Z items: job stress (weighted κ statistic, 0.21; 95% CI, −0.11 to 0.53), burnout (weighted κ statistic, 0.25; 95% CI, −0.02 to 0.53), control over workload (weighted κ statistic, 0.26; 95% CI, −0.01 to 0.53), and sufficient time for documentation (weighted κ statistic, 0.31; 95% CI, 0.08 to 0.54).
Table 2. Mean Difference in Change Proportions From Baseline to Week 32 in Mini-Z Survey Items.
| Mini-Z Survey Item | Baseline to Week 32 Changes (N = 19) | Weighted κ Statistic (95% CI)a | ||||||
|---|---|---|---|---|---|---|---|---|
| Change, No. (%) | Difference in Change Proportions (Positive − Negative) | |||||||
| None | Positive | Negative | ||||||
| Question 1: job satisfactionb | 13 (68) | 4 (21) | 2 (11) | 11 | 0.36 (0.08 to 0.64) | |||
| Question 2: job stressc | 6 (32) | 10 (53) | 3 (16) | 37 | 0.21 (−0.11 to 0.53) | |||
| Question 3: burnoutd | 10 (53) | 8 (42) | 1 (5) | 37 | 0.25 (−0.02 to 0.53) | |||
| Question 4: control over workloade | 10 (53) | 8 (42) | 1 (5) | 37 | 0.26 (−0.01 to 0.53) | |||
| Question 5: sufficient time for documentationf | 9 (47) | 9 (47) | 1 (5) | 42 | 0.31 (0.08 to 0.54) | |||
| Question 9: time spent at home on EMRg | 8 (42) | 5 (26) | 6 (32) | −5 | 0.32 (−0.004 to 0.65) | |||
Abbreviation: EMR, electronic medical record.
Weighted κ statistic is a measure of disagreement or change with higher change contributing more weight.
“Overall I am satisfied with my current job.”
“I feel a great deal of stress because of my job.”
“Using your own definition of burnout choose one of the answers.”
“My control over my workload is.”
“Sufficiency of time for documentation is.”
“The amount of time I spend on electronic medical record at home is.”
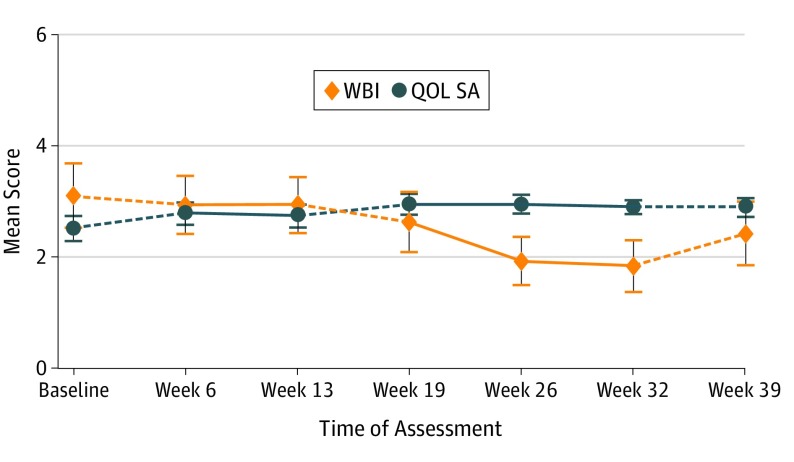
Well-being
Our primary measure of well-being was the WBI. From baseline to week 32, there was a mean decrease of 1.26 points (95% CI, −2.18 to −0.34 points) in the WBI scale score, representing a clinically meaningful decrease of slightly more than 1 fewer negative conditions experienced in the past month on average (Table 1 and Figure 3). Our secondary measure of well-being, the QOL SA, did not have a clinically meaningful change from baseline to week 32 (Table 1 and Figure 3).
Figure 3. Mean (SE) Resident and Fellow Well-Being Index (WBI) and Quality-of-Life Single-Item Self-Assessment (QOL SA) Scores at Each Assessment for 19 Residents.
For the WBI, lower scores indicate better well-being, and for the QOL SA, higher scores indicate better well-being. Solid lines indicate intervention phases, and dashed lines indicate no-intervention phases.
Weekly Protected Nonclinical Time
All residents filled out the weekly survey once per intervention week, for a total of 342 weekly surveys. For weeks in which residents were able to complete the intervention (230 of 342 [67%]), they were asked to describe how they spent their 2 hours of protected time. Participants were not limited to 1 selection and could select as many different activities that were completed during the 2 hours. Responses included research (65 of 424 [15%]), personal or other (55 of 424 [13%]), reviewing upcoming cases (57 of 424 [13%]), logging cases (47 of 424 [11%]), preparing a residency-required presentation (47 of 424 [11%]), dictating or reviewing dictations (43 of 424 [10%]), logging work hours (39 of 424 [9%]), responding to work-related emails (32 of 424 [8%]), onboarding or regulatory tasks (19 of 424 [5%]), and creating a work schedule (20 of 424 [5%]). Free-form responses to “personal or other” were grouped into personal health and wellness (21 of 424 [5%]), studying (12 of 424 [3%]), running errands (6 of 424 [1%]), postresidency job search (5 of 424 [1%]), department-related administrative activities (4 of 424 [1%]), and no response (7 of 424 [2%]) (eFigure 1 in the Supplement).
For weeks in which residents were unable to complete the intervention (112 of 342 [33%]), they were asked to describe why. Participants were limited to 1 selection. Responses included patient care and clinical duties (36 of 342 [11%]), resident off-service (36 of 342 [11%]), vacation (17 of 342 [5%]), service too busy (12 of 342 [4%]), co-resident on vacation (7 of 342 [2%]), scheduled on day off (2 of 342 [1%]), and scheduled while on call (2 of 342 [1%]) (eFigure 2 in the Supplement). All but 4 residents reported 1 or more weeks that they were unable to complete the intervention owing to patient care or clinical duties. Uncompleted intervention weeks were fairly evenly distributed across the 3 intervention periods: 17 in period 1, 21 in period 2, and 20 in period 3.
End-of-Study Surveys
All 19 study participants completed the resident end-of-study survey: 14 residents (74%) felt that 2 hours of weekly nonclinical time was an appropriate amount of time, 17 residents (90%) felt that this study intervention did not affect their clinical learning, and 12 residents (63%) felt that the residency program cares about their QOL and well-being as a resident. However, 17 residents (90%) said they are not more likely to approach the program director or a faculty member with a personal concern as a direct result of this study.
A total of 21 attending physicians completed the attending end-of-study survey; 17 attending physicians (81%) were aware of residents’ involvement in this study. When asked if any surgical cases or clinic went uncovered directly because of this project, 10 (48%) responded “no,” 7 (33%) responded “unsure,” and 4 (19%) responded “yes.” No respondents reported an increased workload because of this study. A total of 15 of 20 respondents (75%) felt that the intervention did not detract from resident education, and 17 of 18 (94%) felt that the intervention did not affect patient care.
Discussion
Physician burnout is markedly affecting the viability of our current health care system by decreasing the quality of patient care delivery. For this reason, efforts targeting burnout have become an active area of research; new requirements have been established by the Accreditation Council for Graduate Medical Education (ACGME). Effective July 1, 2017, the ACGME expanded Section VI of the Common Program Requirements to include greater attention to patient safety and resident well-being.26 Physician impairment and maintenance of personal well-being are now key professionalism targets within the ACGME milestones.26 According to the ACGME’s website, one of the key components of Section VI includes “establishing policies and programs supporting optimal resident and faculty member well-being, including the opportunity to attend appointments for personal care, even during working hours.”27 The intervention tested in this study serves as an easily implementable policy that directly satisfies the new ACMGE Common Program Section VI requirements.
Although our study intervention was not associated with clinically meaningful changes in the MBI DP or PA scores, 2 hours of nonclinical time were associated with a clinically meaningful decrease in MBI EE scores from baseline to the end of the intervention. The mean decrease of 0.63 points in the MBI EE score from baseline to the end of the intervention is greater than we initially hypothesized based on a prior study by Golub et al,28 which found that the MBI EE score increased by 0.19 for every additional hour worked per week among otolaryngology residents. The study intervention was also associated with a clinically meaningful improvement in our primary measure of well-being, the WBI, and difference in change proportions indicated that there were clinically meaningful improvements for 4 of the 6 Mini-Z items (job stress, burnout, control over workload, and sufficient time for documentation).
Based on the Mini-Z single-item burnout measure (question 3), 37% of participants reported burnout at the beginning of this study, while only 21% reported burnout at week 32 (eTable in the Supplement). This rate is lower than the 44.8% rate of burnout in PGY2 otolaryngology residents recently reported by Dyrbye et al.6 However, Dyrbye et al6 used 2 single-item questions adapted from the MBI as an abbreviated, surrogate measure of burnout.29,30 Given that the full 22-item MBI was administered to participants in our study, we chose to score the MBI per the MBI scoring manual; for this reason, burnout prevalence based on the MBI is not reported.22
As previously discussed, resident burnout is a multifactorial problem. The intervention tested in this study was intentionally designed in an attempt to address many of the factors associated with burnout. In analyzing how residents spent their 2 hours of nonclinical time, 69% of the time residents performed tasks required by their job as an ACGME-accredited otolaryngology resident (department-related administrative activities, onboarding and regulatory tasks, creating a work schedule, responding to work-related emails, logging hours, dictating and reviewing dictations, research [required by program], logging cases, and preparing a residency-required presentation). Had they not had this time during their normal workday, they would have performed this required work either at the end of the workday, increasing already long work hours, or at home on their own time, further exacerbating the problems of excessive workload, decreased work-life balance, inefficient work environment, and fatigue. The other 31% of the time, residents performed tasks either unrelated to or not directly required by their job as an otolaryngology resident. Outside of studying and elective research, the ability to complete many of these tasks is limited by the mismatch between normal business hours and a resident’s schedule. Traditionally, residents have been unable to complete such activities, which leads to poor self-care, decreased work-life balance, and inadequate support.
Although most attending physicians were supportive of this project, a few had concerns about the potential negative effect on resident education. We agree that any burnout intervention must be carefully designed to maximally address the different factors associated with burnout and simultaneously diminish the potential for missed educational opportunities. It is for this reason that we instructed the chief residents to assign the nonclinical time when educational opportunities were lowest. Although this was dependent on individual chief residents, most attending physicians felt that this intervention did not detract from resident education.
Similarly, most attending physicians reported that this intervention did not affect patient care. This fact is further seen when analyzing why residents were unable to complete the intervention. Excluding residents on vacation or off-service, the main reason participants were unable to complete the intervention was owing to patient care. This intervention did not, and will not, change the fact that if there is a patient in need, the commitment is always to the patient. The nonclinical protected time can simply be rescheduled.
Limitations
Our study has limitations. This study was conducted solely among otolaryngology residents in 1 department, which limits the generalizability of the results. There was also a large number of surveys, which could reasonably lead to survey fatigue over time. The effect size estimates are less precise than in a study with a larger sample. The nonrandomized assignment of intervention periods is also a limitation in that it prevents estimation of order and carryover effects and does not allow for inference of causality. The crossover design also limits inferences of causality, and the lack of a concurrent control group limits the ability to separate outcomes of the intervention from trends owing to other confounding factors during the study period. Other sources of potential bias include the lack of blinding, observer bias, cause-effect bias, secondary gain bias, the Hawthorne effect, and the Dunning-Kruger effect.
Conclusions
Two hours of protected, nonclinical time were associated with clinically meaningful decreased burnout and increased well-being in a small sample of otolaryngology resident physicians. The preliminary results of this intervention are encouraging and warrant further investigation in larger resident cohorts with randomized clinical trials to confirm effectiveness of the protected time intervention to decrease burnout and increase well-being.
eTable. Baseline and Week 32 Mini-Z Responses
eFigure 1. Use of Weekly Nonclinical Time by Residents
eFigure 2. Flowchart of Resident Participation in Weekly Intervention While on Intervention Phase
References
- 1.Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. 4th ed Menlo Park, CA: Mind Garden; 2016. [Google Scholar]
- 2.Martini S, Arfken CL, Churchill A, Balon R. Burnout comparison among residents in different medical specialties. Acad Psychiatry. 2004;28(3):240-242. doi: 10.1176/appi.ap.28.3.240 [DOI] [PubMed] [Google Scholar]
- 3.West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306(9):952-960. doi: 10.1001/jama.2011.1247 [DOI] [PubMed] [Google Scholar]
- 4.Holmes EG, Connolly A, Putnam KT, et al. Taking care of our own: a multispecialty study of resident and program director perspectives on contributors to burnout and potential interventions. Acad Psychiatry. 2017;41(2):159-166. doi: 10.1007/s40596-016-0590-3 [DOI] [PubMed] [Google Scholar]
- 5.Rosen IM, Gimotty PA, Shea JA, Bellini LM. Evolution of sleep quantity, sleep deprivation, mood disturbances, empathy, and burnout among interns. Acad Med. 2006;81(1):82-85. doi: 10.1097/00001888-200601000-00020 [DOI] [PubMed] [Google Scholar]
- 6.Dyrbye LN, Burke SE, Hardeman RR, et al. Association of clinical specialty with symptoms of burnout and career choice regret among US resident physicians [retracted in: JAMA. 2019;321(12):1220-1221]. JAMA. 2018;320(11):1114-1130. doi: 10.1001/jama.2018.12615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fahrenkopf AM, Sectish TC, Barger LK, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336(7642):488-491. doi: 10.1136/bmj.39469.763218.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.West CP, Tan AD, Habermann TM, Sloan JA, Shanafelt TD. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302(12):1294-1300. doi: 10.1001/jama.2009.1389 [DOI] [PubMed] [Google Scholar]
- 9.Balch CM, Freischlag JA, Shanafelt TD. Stress and burnout among surgeons: understanding and managing the syndrome and avoiding the adverse consequences. Arch Surg. 2009;144(4):371-376. doi: 10.1001/archsurg.2008.575 [DOI] [PubMed] [Google Scholar]
- 10.Ishak WW, Lederer S, Mandili C, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;1(2):236-242. doi: 10.4300/JGME-D-09-00054.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Melamed S, Shirom A, Toker S, Berliner S, Shapira I. Burnout and risk of cardiovascular disease: evidence, possible causal paths, and promising research directions. Psychol Bull. 2006;132(3):327-353. doi: 10.1037/0033-2909.132.3.327 [DOI] [PubMed] [Google Scholar]
- 12.West CP, Tan AD, Shanafelt TD. Association of resident fatigue and distress with occupational blood and body fluid exposures and motor vehicle incidents. Mayo Clin Proc. 2012;87(12):1138-1144. doi: 10.1016/j.mayocp.2012.07.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Halbesleben JR, Rathert C. Linking physician burnout and patient outcomes: exploring the dyadic relationship between physicians and patients. Health Care Manage Rev. 2008;33(1):29-39. doi: 10.1097/01.HMR.0000304493.87898.72 [DOI] [PubMed] [Google Scholar]
- 14.Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med. 2017;15(5):419-426. doi: 10.1370/afm.2121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272-2281. doi: 10.1016/S0140-6736(16)31279-X [DOI] [PubMed] [Google Scholar]
- 16.Goldhagen BE, Kingsolver K, Stinnett SS, Rosdahl JA. Stress and burnout in residents: impact of mindfulness-based resilience training. Adv Med Educ Pract. 2015;6:525-532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kashani K, Carrera P, De Moraes AG, Sood A, Onigkeit JA, Ramar K. Stress and burnout among critical care fellows: preliminary evaluation of an educational intervention. Med Educ Online. 2015;20:27840. doi: 10.3402/meo.v20.27840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gunasingam N, Burns K, Edwards J, Dinh M, Walton M. Reducing stress and burnout in junior doctors: the impact of debriefing sessions. Postgrad Med J. 2015;91(1074):182-187. doi: 10.1136/postgradmedj-2014-132847 [DOI] [PubMed] [Google Scholar]
- 19.Martins AE, Davenport MC, Del Valle MP, et al. Impact of a brief intervention on the burnout levels of pediatric residents. J Pediatr (Rio J). 2011;87(6):493-498. doi: 10.2223/JPED.2127 [DOI] [PubMed] [Google Scholar]
- 20.Busireddy KR, Miller JA, Ellison K, Ren V, Qayyum R, Panda M. Efficacy of interventions to reduce resident physician burnout: a systematic review. J Grad Med Educ. 2017;9(3):294-301. doi: 10.4300/JGME-D-16-00372.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Romani M, Ashkar K. Burnout among physicians. Libyan J Med. 2014;9:23556. doi: 10.3402/ljm.v9.23556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Linzer M, Poplau S, Babbott S, et al. Worklife and wellness in academic general internal medicine: results from a national survey. J Gen Intern Med. 2016;31(9):1004-1010. doi: 10.1007/s11606-016-3720-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rohland BM, Kruse GR, Rohrer JE. Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress Health. 2004;20(2):75-79. doi: 10.1002/smi.1002 [DOI] [Google Scholar]
- 24.Dyrbye LN, Satele D, Sloan J, Shanafelt TD. Ability of the Physician Well-Being Index to identify residents in distress. J Grad Med Educ. 2014;6(1):78-84. doi: 10.4300/JGME-D-13-00117.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-174. doi: 10.2307/2529310 [DOI] [PubMed] [Google Scholar]
- 26.Accreditation Council for Graduate Medical Education. Milestones. http://www.acgme.org/acgmeweb/tabid/430/ProgramandInstitutionalAccreditation/NextAccreditationSystem/Milestones.aspx. Accessed October 17, 2017.
- 27.Accreditation Council for Graduate Medical Education. Summary of changes to ACGME Common Program Requirements Section VI. https://www.acgme.org/What-We-Do/Accreditation/Common-Program-Requirements/Summary-of-Proposed-Changes-to-ACGME-Common-Program-Requirements-Section-VI. Accessed July 28, 2018.
- 28.Golub JS, Weiss PS, Ramesh AK, Ossoff RH, Johns MM III. Burnout in residents of otolaryngology-head and neck surgery: a national inquiry into the health of residency training. Acad Med. 2007;82(6):596-601. doi: 10.1097/ACM.0b013e3180556825 [DOI] [PubMed] [Google Scholar]
- 29.West CP, Dyrbye LN, Satele DV, Sloan JA, Shanafelt TD. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. 2012;27(11):1445-1452. doi: 10.1007/s11606-012-2015-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.West CP, Dyrbye LN, Sloan JA, Shanafelt TD. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med. 2009;24(12):1318-1321. doi: 10.1007/s11606-009-1129-z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Baseline and Week 32 Mini-Z Responses
eFigure 1. Use of Weekly Nonclinical Time by Residents
eFigure 2. Flowchart of Resident Participation in Weekly Intervention While on Intervention Phase