Abstract
Purpose
The aim of this study was to devise a grassroots-level strategy for identification and management of middle ear disorders in a community-based program for individuals with cleft lip and palate in 2 rural districts in the state of Tamil Nadu in South India.
Method
Community workers underwent training to conduct video otoscopy using the ENTraview device. Community workers conducted video otoscopy on 160 individuals with cleft lip and palate between 3 and 35 years old in the community. Middle ear conditions were identified using store-and-forward telepractice. Diagnostic telehearing evaluation was conducted using synchronous pure tone audiometry and tympanometry for those who were identified with tympanic membrane (TM) and/or middle ear diseases (MEDs). A review of data collected over a 13-month period was carried out to assess coverage and follow-up intervention rates.
Results
The program was successful in achieving 80% coverage for identification of TM and MEDs within 13 months of program implementation. TM and/or MEDs were identified in 26% (82/320 ears) of those who underwent video otoscopy. Telehearing evaluations were completed on 42 ears of individuals with TM and/or MEDs; 52% (22/42 ears) of these individuals had a minimal, mild, or moderate degree of hearing loss. Regarding follow-up for intervention, 78% qualified for surgical intervention, and 31% qualified for medication.
Conclusions
This grassroots-level telemedicine approach was successful in achieving better coverage, and store-and-forward telepractice helped in providing remote diagnosis and recommendation by otolaryngologists to all individuals with TM/MEDs in the rural community. The follow-up for otological intervention significantly improved from that achieved in the previous years.
In an attempt to provide comprehensive services for individuals with cleft lip and palate (CLP) in a rural community, a community-based model was implemented in two districts, Thiruvannamalai (year 2005) and Cuddalore (year 2011) in the state of Tamil Nadu in South India. The World Health Organization initiated community-based rehabilitation after the Declaration of Alma-Ata in 1978 (World Health Organization, 1978) and further emphasized and promoted this model in 2004 (World Health Organization, 2004) as a strategy to provide equal access to health care and rehabilitation, and social inclusion of people with disabilities. One of the key goals of community-based rehabilitation is in building capacity, empowering and mobilizing people with disabilities and their families.
Our purpose was to create a grassroots-level program to identify individuals with CLP and provide comprehensive services, including surgical correction, speech and language assessment/therapy, hearing screening/assessment, and dental and orthodontic services. The project covers an area of 3,800 square miles and is located 100–130 miles from the tertiary care hospital at Chennai from where services were provided. Currently, there are 564 registered beneficiaries of the program; the beneficiaries are from 3 months to 35 years old.
Eight community workers are employed in this program to identify individuals with CLP and mobilize follow-up to the tertiary care hospital or at monthly camps 1 that were conducted in the rural community, as required. The community workers are central to this program as they are the connecting link between the beneficiary and the health care provider at the tertiary care hospital. In this program, all surgical corrections (plastic surgery, orthodontic, and dental) were provided at the tertiary care hospital, and other services (speech and language assessment/therapy, hearing screening/assessment, preventive dentistry, and orthodontic follow-up) were provided either at the tertiary care hospital or at the monthly camps in the rural community. The absence of a speech-language pathologist workforce in rural communities and the pertinent need for consistent intervention for the correction of speech errors led to the initiation of a community-worker–led model (Sell, Nagarajan, Wickenden, Howard, & Lohmander, 2011) of correction of error consonants.
It is known that individuals with CLP are susceptible to middle ear diseases (MEDs; Flynn, Möller, Jönsson, & Lohmander, 2009; Sheahan, Miller, Sheahan, Earley, & Blayney, 2003; Shprintzen, Siegel-Sadewitz, Amato, & Goldberg, 1985). In Western countries, the presence of MEDs among individuals with CLP was reported to be 75% (n = 22; Flynn et al., 2009), 79% (n = 110; Goldman, Martinez, & Ganzel, 1993), 97% (n = 50; Dhillon, 1988), and 100% (N = 50; Paradise, Bluestone, & Felder, 1969). Among Asian countries, Chen et al. (2012) found 72% among 319 individuals with CLP to have otitis media with effusion in Taiwan, and Ungkanont, Boonyabut, Komoltri, Tanphaichitr, and Vathanophas (2018) found that all 95 individuals with cleft had at least one episode of otitis media with effusion in Thailand. In India, 67% of 60 individuals with cleft lip and/or palate were reported to have MEDs (Gautam, Sharma, Prakash, Kumar, & Taneja, 2011).
Recurrent MEDs increase the risk of permanent hearing loss among these individuals (Flynn et al., 2009). Among children with cleft palate, ear and hearing disorders were found to be most prevalent between 4 and 6 years old, but these problems persisted for many years after this (Sheahan et al., 2003). Therefore, MEDs require early identification and intervention. Despite the overall success of the community-based program described above in providing comprehensive services to individuals with CLP, ear and hearing health care could not be well integrated.
A review of data on ear and hearing services in our community-based program showed that, during the initial 4 years of the program, 55% of beneficiaries with CLP in the two rural districts underwent pure tone audiometry screening and/or tympanometry screening. These screenings were conducted both at camps and during visits to the tertiary care hospital. However, only 0.2% of the beneficiaries received intervention for ear diseases. Subsequently, camp-based hearing screening was discontinued because of unavailability of equipment, hence screenings were conducted only at the tertiary care hospital. This resulted in a further reduction in coverage (12%–20%) for pure tone audiometry screening, and only 3.5% among those screened followed up for otolaryngology evaluation at the tertiary care hospital. Follow-up for intervention was recorded only for those who were recommended surgery. Surgeries performed at the tertiary care hospital Sri Ramachandra Medical Centre (SRMC) in Chennai city or at any other public or private hospitals were documented. Between 2005 and 2011, two individuals with MEDs received ventilation tubes (grommets) bilaterally, and seven individuals received unilateral grommets. Tympanoplasty was performed on four individuals. All those who underwent surgeries were under 19 years old. No surgeries were performed between 2012 and 2016 because of a lack of systematic audiologic surveillance. Compliance for medication and follow-up compliance postmedication were not documented (Sri Ramachandra Medical College–Transforming Faces [SRMC-TF] annual report 2006–2015).
Because, over the years, camp-based hearing screening was discontinued, red flags for further investigations were based on parent complaint/observation, patient history, and reported symptoms. Patients were referred to otolaryngology at the nearby hospital or to a tertiary care hospital at Chennai for middle ear evaluation and treatment. Hence, there was a need to adapt and modify the existing model to promote better ear and hearing health at the community level.
Given the success of several m-health, e-health, and telemedicine programs, it was felt that such an approach could be adopted to achieve greater coverage and follow-up. Outcomes of some tele-audiology programs support this hypothesis. For example, in Australia, Pearce, Ching, and Dillon (2009) revealed that the use of tele-audiology for the provision of hearing services to remote areas benefited the timelines of service provision and improved the coverage. In the United States, Dharmar et al. (2015) found reduction in loss during follow-up in a pediatric hearing screening program with introduction to tele-audiology diagnostic services. In India, Ramkumar et al. (2018) reported that integration of remote diagnostic assessments in a rural-community–based hearing screening program facilitated improved follow-up compliance. Parental perceptions regarding tele-audiology testing service were also reported to be positive in this community (Ramkumar et al., 2016).
Tele-audiology applications to assess middle ear status have primarily included video otoscopy (Biagio, Swanepoel, Adeyemo, Hall, & Vinck, 2013; Mandavia, Lapa, Smith, & Bhutta, 2018; Patricoski et al., 2003; Smith, Armfield, Wu, Brown, & Perry, 2012). Successful telepractice requires the able assistance of a facilitator at the patient end. Researchers in Australia and Africa have trained facilitators for store-and-forward video otoscopy to spread ear screening to rural and unreached populations and reported it to be feasible and effective (Biagio et al., 2013; Smith et al., 2012).
In 2016, with a surge in Internet penetration in remote rural areas in India (Internet and Mobile Association of India [IAMAI], 2016), a telemedicine approach was explored to improve speech, language, and hearing services. At first, home-based telespeech therapy provided by a speech-language pathologist was introduced to supplement community-worker–led correction of error consonants. In due course, a telemedicine approach for ear and hearing care was explored.
The aim of this study was to devise a grassroots-level strategy to identify individuals with MEDs in the rural community using a telemedicine approach. The specific objectives were to (a) identify middle ear conditions using store-and-forward video otoscopy devices among individuals with CLP in rural communities, (b) assess hearing status using synchronous pure tone audiometry and tympanometry for those identified with tympanic membrane (TM) and MEDs through asynchronous video otoscopy and provide telediagnostic confirmation of ear and hearing status, and (c) assess follow-up compliance for intervention.
Method
This study was approved by the institutional ethics committee of Sri Ramachandra Medical College and Research Institute (Deemed to be University), Porur, Chennai (IEC-NI/16/JAN/50/105).
Participants
This study included all individuals above 3 years old actively 2 seeking services through the community-based program for individuals with CLP (N = 201). Children younger than 3 years old (60 beneficiaries) could not be screened using the ENTraview device (Medtronic) as the speculum size was not suitable. These children were screened by audiologists at the camp site or during a hospital visit. The details of this manual otoscopy screening of younger children are not included as it is beyond the purview of this study. Consent was obtained from the parents before testing for children aged 18 years or below. As this study aimed at profiling the current status of middle ear function and hearing thresholds, no specific inclusion criteria related to age of palate repair were included.
Procedure
Community Worker Training
Eight community workers were trained and oriented to use the ENTraview video otoscopy device and to facilitate tele–pure tone audiometry and tympanometry. A 2-day modular training program was developed to be delivered in the local language, Tamil. The modules included orientation to the ear and middle ear disorders, the procedure to input demographic data and patient history using the mobile application, the procedure to carry out video otoscopy using the ENTraview, and a hands-on module.
Identification of Middle Ear Conditions
Community workers scheduled home visits in the community to perform store-and-forward (asynchronous) video otoscopy using the ENTraview device. This video otoscope is a Conformité Européene–certified production version (Medtronic, 2017) and uses a modified camera of a mobile phone with an 8-megapixel resolution. The device has an independent light source with options to adjust the brightness to ensure a clear image of the TM. The mobile phone works on Kitkat version 4.4, an Android operating system enabled with mobile Internet data using Subscriber Identification Module.
Community workers documented each patient's demographic details and ear and hearing history using the customized mobile application “Shruti,” which was available in the local language, Tamil (Medtronic, 2017). The community worker then captured the image of the TM and ear canal using the video otoscope. The obtained image, along with patient data and history, was then uploaded to the cloud using mobile data Internet. The audiologist viewed the images at the back-end (at the tertiary care hospital) using the Clickmedix platform. This platform has unlimited cloud storage and provides an interface for the audiologist to access the demographics details, patient history, and the images captured by the community worker in the rural community to provide appropriate recommendations. The audiologist periodically viewed the data and, when necessary, could export the data or share the patient data using the same platform in an encrypted format to the otolaryngologist for recommendations on appropriate management.
Those with impacted cerumen were recommended cerumen management (using Soliwax solution) based on the otolaryngologist's advice. The community worker repeated video otoscopy subsequently to ascertain the status of the middle ear. Those identified with MEDs by the otolaryngologist were recommended an appropriate medication or a surgical intervention. Because e-prescriptions are not legalized in India, prescriptions were mailed to the community workers, who hand-delivered them to the patients. The community workers subsequently followed up to repeat video otoscopy.
Hearing Assessment
Assessment of hearing was carried out for those who were identified with MEDs. Community workers scheduled home visits to complete the hearing assessment. If the beneficiary's home was remote and inaccessible, having poor Internet, testing was scheduled during the monthly multidisciplinary camps conducted at local nongovernmental organizations in villages.
The Sentiero PATH portable lightweight device (SOD100497), an integrated diagnostic audiometer and tympanometry, was used to conduct the hearing evaluation. The device interfaces with a laptop computer and data management software (MIRA; Path Medical, 2017), making it suitable for both synchronous and asynchronous telepractice. The audiologist at the tertiary care hospital conducted pure tone audiometry and tympanometry tests synchronously by remotely accessing the equipment at the rural community. Mobile hotspot-based 4G broadband Internet, with an average bandwidth of 0.40 mbps, was used at the patient end. Local area network–based Internet with an average bandwidth of 70 mbps was used at the hospital end. The community worker set up the equipment, established connectivity, and prepared the patient for testing.
In the case of pure tone audiometry testing, noise levels were measured in the test environment before each testing using a mobile application (BOSCH iNVH; Robert Bosch Engineers, 2018). Noise levels were ensured to be no more than 50 dBA before test commencement. Appropriate correction factors were applied by conducting listening checks on the community worker with normal hearing before testing. Testing was performed at octave frequencies from 500 Hz to 8 kHz for air-conduction thresholds and from 500 Hz to 4 kHz for bone-conduction thresholds. Air-conduction thresholds of 25 dB HL or less and bone-conduction thresholds of 15 dB HL or less were considered normal hearing thresholds.
Tympanometry was carried out using a 226-Hz probe tone at 85 dB SPL, with sweep pressure between −300 to +300 daPa. Tympanometry preceded pure tone audiometry testing. The community worker selected an appropriate ear tip and placed the probe in the individual's ear. The audiologist remotely assessed the accuracy of seal and initiated the testing.
The audiologist provided counseling via videoconferencing regarding hearing status and appropriate management options. The importance of follow-up was emphasized to ensure better compliance.
Analysis
This is an ongoing program; therefore, the interim data of a period of 13 months were reviewed to estimate the number of individuals with MEDs as well as follow-up for diagnosis and intervention.
Results
One hundred sixty individuals (105 males and 55 females) of the 201 active beneficiaries with CLP in the age range of 3–35 years underwent asynchronous video otoscopy. The type of cleft present among these individuals is mentioned in Table 1.
Table 1.
Summary of type of cleft.
| Type of cleft | N = 160 |
|---|---|
| Unilateral cleft lip and palate | 100 |
| Bilateral cleft lip and palate | 35 |
| Cleft palate | 23 a |
| Submucous cleft palate | 2 |
Three of 23 patients had syndromic craniofacial anomaly.
Identification of Middle Ear Conditions Using Store-and-Forward (Asynchronous) Video Otoscopy
Among the 160 individuals who underwent video otoscopy, 4% were between 3 and 6 years old, 64% were between 7 and 14 years old, and 32% were above 14 years old. The coverage for screening with store-and-forward video otoscopy achieved in this 13-month period was found to be 80% (160/201 individuals) and is significantly higher than what was achieved (55%) in a span of 4 years (2011–2015).
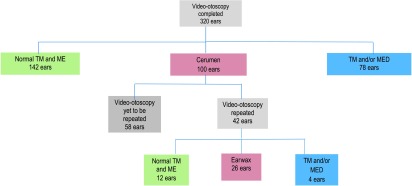
Figure 1 describes the outcome of video otoscopy earwise. TM and MEDs were identified in 78 ears during the initial video otoscopy. A significant proportion (100/320) of ears had cerumen impaction, because of which the TM could not be visualized. Cerumen management strategies were provided to these individuals. Video otoscopy was repeated on 42 ears after cerumen management, and four of these ears were also identified with TM/MEDs. Therefore, all 82 ears were identified with TM/MEDs.
Figure 1.
Outcome of video otoscopy. TM = tympanic membrane; ME = middle ear; MED = middle ear diseases.
Of the 82 ears with TM/MEDs, 52 ears were diagnosed with otitis media with effusion; 20 ears were diagnosed with TM abnormality including scarred TM, TM sclerosis, and hemotympanum; and 10 ears were diagnosed with TM perforation.
Assessment of Hearing Status Using Synchronous Pure Tone Audiometry and Tympanometry for Those Identified With TM and MEDs Using Asynchronous Video Otoscopy
Tele–pure tone audiometry and tympanometry evaluations were scheduled for those individuals with TM and/or MEDs. Evaluations were completed on 42 of 82 ears 3 with TM and/or MEDs. For the remaining ears, the community worker was unable to conduct home-based telehearing assessment because of logistic challenges. Such delays are inevitable because of difficulties in scheduling the visit at a mutually convenient time and because of the lack of a consistent power supply and poor mobile Internet coverage in several homes in the community. In such cases, individuals were asked to follow up at the monthly multidisciplinary camps conducted at local nongovernmental organizations in villages. However, follow-up compliance could not be achieved for these individuals within the study period.
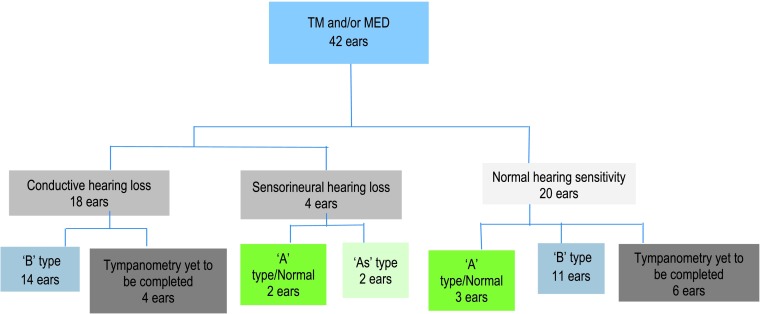
Figure 2 shows the details of test outcomes. Tympanometry could not be completed in 10 ears, when the community worker was unsuccessful in obtaining the accurate seal required to perform the measurement. Twenty-two of the 42 ears (52%) with TM and/or MEDs had hearing loss of either a minimal, mild, or moderate degree. Abnormal tympanograms (“B” type) were obtained in 14 of 22 ears (64%) with hearing loss and 11 of 20 ears (55%) with normal hearing sensitivity.
Figure 2.
Outcome of hearing assessment. TM = tympanic membrane; MED = middle ear diseases.
Assessment of Follow-Up Compliance for Intervention
Fifty-seven individuals (82 ears) with TM and MEDs received telediagnosis and recommendations from the otolaryngologist. Earlier, in the absence of the telemedicine approach, when screening was conducted at camps and individuals were to follow up at the tertiary care hospital or local clinic for diagnosis, the follow-up was found to be 3.5% (SRMC-TF annual report 2006–2015), but with the introduction of store-and-forward video otoscopy, 100% of those with MEDs received diagnosis and recommendation.
Follow-up compliance for recommended interventions was evaluated. Eleven individuals required only home remedies such as steam inhalation and were counseled regarding the same. Nine individuals were recommended surgical intervention, of whom three individuals underwent surgery with financial assistance from the program funding agency, four others are scheduled for surgery, and two individuals did not follow up for surgical intervention. Therefore, 78% (7/9) compliance was achieved for surgical intervention. Earlier, in 6 years (2005–2011), only 13 individuals had undergone surgical intervention (SRMC-TF annual report 2006–2015), whereas with the introduction of telediagnosis and recommendation by the otolaryngologist, seven individuals complied for surgery (three completed and four scheduled) within 13 months. This is a significant outcome for the program.
Thirty-five individuals were recommended medications and follow-up. Thirty-one percent of the individuals (11/35) followed advice, and video otoscopy was repeated to reassess middle ear status after medications. Middle ear condition had resolved, and TM was normal in seven individuals, whereas the TM could not be visualized because of the continued presence of cerumen in two individuals. Two individuals continued to have TM and/or MEDs (one individual with TM perforation and one individual with bulged TM) and were prescribed medications once again.
Challenges
Despite improved Internet penetration, not all localities in the rural community had adequate Internet connectivity for telepractice. Community workers had to locate a test environment near the patient's home with adequate Internet connectivity and bring the patient to this location for testing. To provide home-based telecorrection of error consonant and hearing evaluations, community workers sometimes traveled half a day to reach the location of the patient, thereby increasing the overall time involved in this method. At times, patients did not attend appointments despite prior scheduling by community workers. Such challenges increase the time taken to follow up with patients who are advised repeat video otoscopy. An Internet-enabled kiosk-based telepractice approach, operated by a community worker, may be explored to overcome some of the challenges encountered in home-based telepractice. Such kiosks, if placed in a space of a local nongovernmental organization, have the potential to serve the ear and hearing health care needs of not only individuals with CLP but also others living in these communities.
There were some technical challenges as well. For example, there was a learning curve observed in the skill of community workers in capturing images that were of good quality. The adjustment of light source was a challenge for the community workers initially, but they gained mastery by trial and error in due course.
Poor bandwidth resulted in time lag during pure tone audiometry testing and increased test time. Other researchers have approached the problem of poor bandwidth by adopting asynchronous screening with the help of nurses, health technicians, or audiology assistants. In this program, it was felt necessary to conduct both air-conduction and bone-conduction diagnostic testing in a synchronous fashion, as information on the air–bone gap is pertinent in the appropriate diagnosis of TM and/or MEDs.
To reduce the demand on the community workers in identifying the appropriate tip size for tympanometry, only four sizes of probe tips commonly used for the age group tested in this program were provided. However, the community workers had difficulty in obtaining the adequate seal required for measurement on some individuals (10 ears), because of which testing could not be completed.
Conclusion
In the 12 years of existence of this comprehensive community-based program for individuals with CLP, identification and management of TM and/or MEDs remained a challenge, until this grassroots-level strategy enabled with telemedicine was devised. The application of asynchronous video otoscopy at the community level increased coverage for the identification of MEDs and helped in providing remote diagnosis and recommendation by otolaryngologists to all individuals with TM/MEDs in the rural community. The follow-up for otological intervention significantly improved from that achieved in the previous years. On the basis of the initial success, this telemedicine approach for the identification and management of MEDs is now integrated to the larger program as a routine service delivery in these communities.
Acknowledgments
We thank Medtronic India Pvt. Ltd. for supporting this program with the ENTraview devices and Dr. (Maj) Prasanna Kumar, Otolaryngologist, Department of ENT-HNS, SRMC, Chennai, for providing remote diagnosis and recommendations. This study is a part of an ongoing project, “Comprehensive Management of Communication Disorders in Individuals With Cleft Lip and Palate,” supported by Transforming Faces, Canada. Portions of this article were presented at the 3rd International Internet & Audiology Meeting, Louisville, KY, July 2017, which was funded by National Institute on Deafness and Other Communication Disorders (NIDCD) Grant 1R13DC016547 and the Oticon Foundation.
Funding Statement
This study is a part of an ongoing project, “Comprehensive Management of Communication Disorders in Individuals With Cleft Lip and Palate,” supported by Transforming Faces, Canada. Portions of this article were presented at the 3rd International Internet & Audiology Meeting, Louisville, KY, July 2017, which was funded by National Institute on Deafness and Other Communication Disorders (NIDCD) Grant 1R13DC016547 and the Oticon Foundation.
Footnotes
Camp refers to a temporary location in the rural community, where a team of health care professionals provide consultation, recommendations, or appropriate interventions. In this project, camps were conducted on the premises of a public school or a community shelter or in a space provided by local nongovernmental organizations.
Among the 564 registered beneficiaries, 11 individuals are not alive, 260 individuals could not be contacted because of either relocation or noncompliance in seeking services, and 32 individuals were discharged from the program as their speech was normalized and they did not require additional services such as orthodontic correction.
Both ears were tested even if the individual had unilateral TM or MEDs. However, results are reported only for the ears with TM/MEDs.
References
- Biagio L., Swanepoel D. W., Adeyemo A., Hall J. W., & Vinck B. (2013). Asynchronous video-otoscopy with a telehealth facilitator. Telemedicine and E-Health, 19(4), 252–258. [DOI] [PubMed] [Google Scholar]
- Chen Y. W., Chen K. T., Chang P. H., Su J. L., Huang C. C., & Lee T.-J. (2012). Is otitis media with effusion almost always accompanying cleft palate in children?: The experience of 319 Asian patients. Laryngoscope, 122, 220–224. [DOI] [PubMed] [Google Scholar]
- Dharmar M., Simon A., Sadorra C., Friedland G., Sherwood J., Morrow H., … Marcin J. P. (2015). Reducing loss to follow-up with tele-audiology diagnostic evaluations. Telemedicine Journal and E-Health, 22(2). Epub ahead of print. https://doi.org/10.1089/tmj.2015.0001 [DOI] [PubMed] [Google Scholar]
- Dhillon R. S. (1988). The middle ear in cleft palate children pre and post palatal closure. Journal of the Royal Society of Medicine, 81(12), 710–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn T., Möller C., Jönsson R., & Lohmander A. (2009). The high prevalence of otitis media with effusion in children with cleft lip and palate as compared to children without clefts. International Journal of Pediatric Otorhinolaryngology, 73(10), 1441–1446. [DOI] [PubMed] [Google Scholar]
- Gautam P., Sharma R., Prakash A., Kumar S., & Taneja V. (2011). Assessment of middle ear function in patients with cleft palate treated under “Smile Train Project.” Indian Journal of Otology, 17(3), 105–108. https://doi.org/10.4103/0971-7749.91186 [Google Scholar]
- Goldman J. L., Martinez S. A., & Ganzel T. M. (1993). Eustachian tube dysfunction and its sequelae in patients with cleft palate. Southern Medical Journal, 86(11), 1236–1237. [DOI] [PubMed] [Google Scholar]
- IAMAI. (2016). Internet in India—2016: An IAMAI & KANTAR IMRB report. Retrieved from http://bestmediainfo.com/wp-content/uploads/2017/03/Internet-in-India-2016.pdf [Google Scholar]
- Mandavia R., Lapa T., Smith M., & Bhutta M. F. (2018). A cross-sectional evaluation of the validity of a smartphone otoscopy device in screening for ear disease in Nepal. Clinical Otolaryngology, 43(1), 31–38. [DOI] [PubMed] [Google Scholar]
- Medtronic. (2017). Shruti. Retrieved from http://www.medtronic.com/in-en/about/shruti.html
- Paradise J., Bluestone D., & Felder H. (1969). The universality of otitis media in 50 infants with cleft palate. Pediatrics, 44(1), 35–42. [PubMed] [Google Scholar]
- Path Medical. (2017). MIRA PC Software. Retrieved from https://pathme.de/support/#downloads
- Patricoski C., Kokesh J., Ferguson A. S., Koller K., Zwack G., Provost E., & Holck P. (2003). A comparison of in-person examination and video otoscope imaging for tympanostomy tube follow-up. Telemedicine Journal and E-Health, 9(4), 331–344. [DOI] [PubMed] [Google Scholar]
- Pearce W., Ching T. Y. C., & Dillon H. (2009). Brief communications hearing services using tele-audiology to remote areas. The Australian and New Zealand Journal of Audiology, 31(2), 96–100. [Google Scholar]
- Ramkumar V., John K. R., Selvakumar K., Vanaja C. S., Nagarajan R., & Hall J. W. (2018). Cost and outcome of a community-based paediatric hearing screening programme in rural India with application of tele-audiology for follow-up diagnostic hearing assessment. International Journal of Audiology, 57(6), 407–414. https://doi.org/10.1080/14992027.2018.1442592 [DOI] [PubMed] [Google Scholar]
- Ramkumar V., Selvakumar K., Vanaja C. S., Hall J. W., Nagarajan R., & Neethi J. (2016). Parents' perceptions of tele-audiological testing in a rural hearing screening program in South India. International Journal of Pediatric Otorhinolaryngology, 89, 60–66. https://doi.org/10.1016/j.ijporl.2016.07.028 [DOI] [PubMed] [Google Scholar]
- Robert Bosch Engineers. (2018). iNVH. Retrieved from https://appcenter.bosch.com/details/-/app/iNVH
- Sell D., Nagarajan R., Wickenden M., Howard S., & Lohmander A. (2011). Cleft palate speech in the majority world: Models of intervention and speech outcomes in diverse cultural and language contexts. In Howard S. & Lohmander A. (Eds.), Cleft palate speech: Assessment and intervention (pp. 105–121). Hoboken, NJ: Wiley-Blackwell. [Google Scholar]
- Sheahan P., Miller I., Sheahan J., Earley M., & Blayney A. (2003). Incidence and outcome of middle ear disease in cleft lip and/or cleft palate. International Journal of Pediatric Otorhinolaryngology, 67(7), 785–793. [DOI] [PubMed] [Google Scholar]
- Shprintzen R. J., Siegel-Sadewitz V. L., Amato J., & Goldberg R. B. (1985). Anomalies associated with cleft lip, cleft palate, or both. American Journal of Medical Genetics, 20(4), 585–595. [DOI] [PubMed] [Google Scholar]
- Smith A. C., Armfield N. R., Wu W., Brown C. A., & Perry C. (2012). A mobile telemedicine-enabled ear screening service for indigenous children in Queensland: Activity and outcomes in the first three years. Telemedicine and Telecare, 18, 485–489. [DOI] [PubMed] [Google Scholar]
- Ungkanont K., Boonyabut P., Komoltri C., Tanphaichitr A., & Vathanophas V. (2018). Surveillance of otitis media with effusion in Thai children with cleft palate: Cumulative incidence and outcome of the management. The Cleft Palate–Craniofacial Journal, 55(4), 590–595. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (1978). Alma Ata Declaration. Geneva, Switzerland: Author. [Google Scholar]
- World Health Organization. (2004). CBR: A strategy for rehabilitation, equalization of opportunities, poverty reduction and social inclusion of people with disabilities: Joint position paper/International Labour Organization, United Nations Educational, Scientific and Cultural Organization. Geneva, Switzerland: Author. [Google Scholar]