Abstract
Purpose
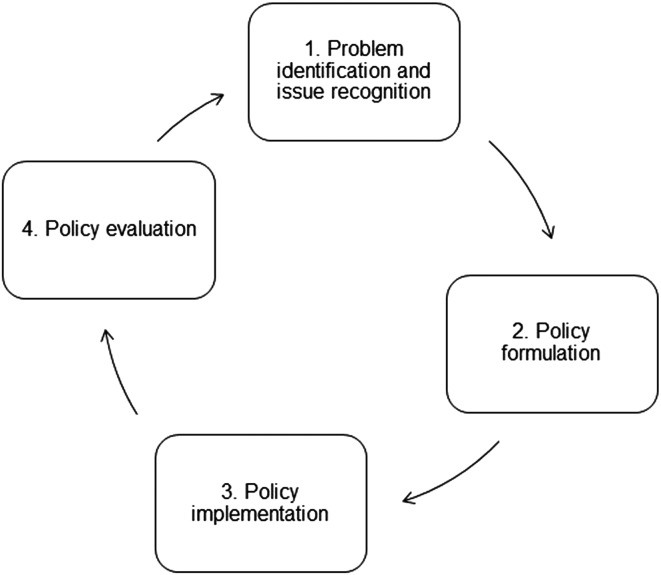
The scarcity of health care resources calls for their rational allocation, including within hearing health care. Policies define the course of action to reach specific goals such as optimal hearing health. The process of policy making can be divided into 4 steps: (a) problem identification and issue recognition, (b) policy formulation, (c) policy implementation, and (d) policy evaluation. Data and evidence, especially Big Data, can inform each of the steps of this process. Big Data can inform the macrolevel (policies that determine the general goals and actions), mesolevel (specific services and guidelines in organizations), and microlevel (clinical care) of hearing health care services. The research project EVOTION applies Big Data collection and analysis to form an evidence base for future hearing health care policies.
Method
The EVOTION research project collects heterogeneous data both from retrospective and prospective cohorts (clinical validation) of people with hearing impairment. Retrospective data from clinical repositories in the United Kingdom and Denmark will be combined. As part of a clinical validation, over 1,000 people with hearing impairment will receive smart EVOTION hearing aids and a mobile phone application from clinics located in the United Kingdom and Greece. These clients will also complete a battery of assessments, and a subsample will also receive a smartwatch including biosensors. Big Data analytics will identify associations between client characteristics, context, and hearing aid outcomes.
Results
The evidence EVOTION will generate is relevant especially for the first 2 steps of the policy-making process, namely, problem identification and issue recognition, as well as policy formulation. EVOTION will inform microlevel, mesolevel, and macrolevel of hearing health care services through evidence-informed policies, clinical guidelines, and clinical care.
Conclusion
In the future, Big Data can inform all steps of the hearing health policy-making process and all levels of hearing health care services.
Most clinicians and researchers working in audiology are likely to have heard about Big Data to support research evidence generation. However, they may not have been introduced to the application of Big Data for the advancement of health policy making and thus, hearing health care.
The future work of hearing care professionals will be the foundation for evidence-based decision-making processes in hearing health care. The use of Big Data analytics to generate evidence will drive new ways of delivering (hearing) health care and will influence day-to-day clinical practice. The purpose of the current article is to give clinicians and people working in the field of audiology an insight on how Big Data can create evidence supporting hearing health policy. It is meant as a comprehensive introduction to the concepts and language used in data-driven health care delivery and policy making.
EVOTION, a European Big Data project, is introduced to showcase the important elements of a Big Data platform that enables (a) the collection of heterogeneous data related to hearing impairment and (b) the performance of Big Data analytics.
State of the Art in Decision Making for Public Policies
The U.S. Senate passed the Food and Drug Administration Reauthorization Act of 2017, which includes the new Over-the-Counter Hearing Aid Act. This latter act makes hearing aids intended for adults with mild–moderate hearing impairment available over the counter without requiring prior medical evaluation or signing a waiver of that examination. By targeting deregulation, this act aims to increase accessibility to hearing aids without compromising the quality of hearing health care. This is an example of a hearing health care policy that resulted from extensive consultations, including those from the National Academies of Sciences, Engineering, and Medicine (2016). This raises some questions, namely, how this sociopolitical decision was made, as well as what data and evidence supported this decision. Further, how will the consequences of the act be monitored and evaluated against its aims, and most importantly, how will new ways of delivering (hearing) health care influence the future work of clinicians?
A policy is a course of action or a statement of goals, objectives, and means of activities, so health policies include the actions, decisions, and plans undertaken to achieve or maintain health care goals within a society (World Health Organization [WHO], 2017a).
The process that leads to new policies, whether within health care or within other spheres, is complex and highly political. Describing the steps involved makes plain the role of data and evidence throughout the process. Different models and theories abound in describing policy making. In this article, we use the “stages heuristic,” which breaks down the policy-making process, or lifecycle, into four steps (Sabatier & Jenkins-Smith, 1993):
Problem identification and issue recognition: the step in which public and political stakeholders identify an issue as worthy of attention and where it enters the policy agenda. To support this step, stakeholders usually map needs and gaps, available resources, and strengths, weaknesses, opportunities, and threats (analysis) of current and new policies.
Policy formulation: the step in which a policy is described, agreed upon, and disseminated. It includes communicating the aims, objectives, activities, and priorities of a policy and identifying the resources required for implementing this policy, elements that form the action plan.
Policy implementation: the step in which a policy is rolled out into practice. This includes execution of the action plan and monitoring the adherence of implementation activities to the original action plan. Although often overlooked, this step is crucial for policies to be applied as intended in practice, as local forces sometimes resist or modify new policies to suit other objectives.
Policy evaluation: The step in which the effect of the policy is measured. It covers both whether the policy achieved its original aims and objectives and whether the policy had any unintended consequences. This includes assessing the effects and outcomes of the policy. Based on the evaluation, adjustments to the current policy might be required, and this is why the process is described as a perpetual lifecycle.
Decision making in public policies is typically supported by various types of analyses (e.g., strengths, weaknesses, opportunities, and threats, cost-effectiveness, and cost–benefit analyses), the experience and expertise of the stakeholders involved, and the learnings acquired through monitoring and evaluation of previous policies (Jonassen, 2012). The process of policy making is traditionally based on guidelines, methodologies, templates, and extensive interaction and collaboration among stakeholders. These include local, regional, and national governmental institutions, authorities implementing policies, and nongovernmental stakeholders such as groups and organizations representing health care users and professionals.
For example, the stakeholders involved in Step 2 of the policy lifecycle, the “policy formulation” of the Over-the-Counter Hearing Aid Act, involved the President's Council of Advisors on Science and Technology and the National Academies of Science, Engineering, and Medicine. The legislation has received endorsements and criticism from different relevant stakeholders. The Hearing Loss Association of America and the Gerontological Society of America are in favor of the act as, in their opinion, it helps to reduce costs and increases consumer choice so that more Americans have access to affordable hearing aids.
Stakeholders representing health care professionals and interest groups, including the Hearing Industries Association, the American Academy of Audiology, and the International Hearing Society, have been more critical of the Over-the-Counter Hearing Aid Act. They raised concerns regarding the harm associated with direct-to-consumer hearing aid sales. One major concern is that, without qualified assessment from clinicians, patients lack an accurate understanding of the severity of their hearing impairment, which might result in ill-informed self-administered treatment of their hearing impairment (American Academy of Audiology, 2018; Hearing Review, 2017a, 2017b).
In the future, applying evidence from Big Data analytics to the policy-making process can reveal the impact of legislation such as the Over-the-Counter Hearing Aid Act based on robust data that allow for quick adjustments in all four steps in the policy lifecycle.
Call for Big Data Evidence in Health Policy Making
Big Data refers to extensive datasets, typically made of heterogeneous data types, collected retrospectively and/or prospectively in real time. Big Data computational analytics tools can reveal new patterns, trends, and associations that would be otherwise impossible to identify (Ullah et al., 2017).
Governments and international organizations recognize the potentials of Big Data. In the United States, the White House published recommendations to both seize the opportunities of Big Data while preserving intrinsic societal values such as privacy and equality (President's Council of Advisors on Science and Technology, 2014a, 2014b).
Big Data could also inform health policies and practices. The scarcity of health care resources calls for their rational allocation, and evidence can help improve cost-effectiveness. In health care, Big Data encompasses information from electronic health care records, client summaries, pharmaceutical data, test results, clinical trials, sensors, mobile apps, social media, well-being, behaviors, and socioeconomic indicators (European Commission, 2014). By combining all these data types, Big Data analysis can predict whether individuals will develop a particular disease and how they will respond to specific therapies. Taking this prediction one step further, Big Data can also prevent health conditions from occurring and can support public health interventions. Big Data can monitor the efficiency of health care systems and facilitate outcome-based reimbursement. The Journal of Biomedical and Health Informatics dedicated a special issue to “Big Data for Health” in 2015 where initiatives including Big Data analytics in health care were described. In summary, Big Data analytics in health is described as a source of innovation that improves the efficiency of policy making, care provision, and clinical decision making.
Still, few current public health policies are anchored in the solid evidence base that large sets of heterogeneous data can provide. Few publications have so far focused on applications of Big Data for health policy making. One exception is visual analytics tools, which have emerged to support public health decision making (Ola & Sedig, 2014). Advanced automated analysis combined with interactive visualization tools assist stakeholders in their assessment and policy formulation and their exploration of implications of hypothetical policy options. Examples of interactive visualization tools include the Midcourse Review (http://www.healthypeople.gov), with interactive features to gain insight on the progress made toward “Healthy People 2020” since they were published in 2010. These priorities for the health of the American population arose after wide stakeholder consultation and a similar process are now occurring for the identification of the latest health priorities and the formulation of “Healthy People” 2030.
Another visualization tool is Gapminder (2018) that Hans Gosling et al. developed. It makes comprehensive socioeconomic statistics more accessible and understandable. In 2006, Hans Gosling won recognition with his TED talk “The Best Statistics You Have Ever Seen” (Rosling, 2006). In practice, such visualization tools enable decision makers to create appealing illustrations, access and compare data, exclude irrelevant data, and investigate relationships and links between concepts, for example, environmental and health factors.
Most of the existing methods, techniques, and tools for evidence-informed policies provide simple guidelines to identify and incorporate evidence in health policy formulation (Canadian Foundation for Healthcare Improvement, 2014; Linstone & Turoff, 1975; National Collaborating Centre for Methods and Tools, 2009; WHO, 2015b, 2017b). Specifically, hearing health policies are the Action on Hearing Loss's framework for assessing hearing services (Action on Hearing Loss, 2013) and the WHO's situational analysis tool for hearing care (WHO, 2015a). Such guidelines suggest methods for formulating priorities and policies, for assessing health situations among the population, for evaluating health services, for using evidence, and for monitoring health policies.
Big Data Evidence Generation
The EVOTION Project: Supporting Evidence-Informed Decision Making in Policy With Big Data
Hearing impairment is a public health concern. It is the fifth leading cause of years lived with disability (Vos et al., 2015) and, due to its impact on social participation, has been described as one of the most significant modifiable risk factors for dementia (Livingston et al., 2017). The prevalence of hearing impairment is increasing globally, mostly because of an increase in life expectancy (WHO, 2012). In the United States, hearing impairment is expected to affect 15% of adults in 2020 and 22% of adults in 2060 (Goman, Reed, & Lin, 2017). The scarcity of health care resources calls for their rational allocation, especially as uptake and adherence to hearing health care services are currently suboptimal (Bainbridge & Wallhagen, 2014). The recent World Health Assembly Resolution on the Prevention of Deafness and Hearing Loss highlights the urgent need for evidence to underpin the policy-making process for ear and hearing care (WHO, 2017c).
The EVOTION research project seeks to facilitate evidence-informed policies regarding hearing impairment and its management, with a focus on problem identification and issue recognition, as well as policy formulation (Steps 1–2 in the process of policy making in Figure 1). The EVOTION platform includes several components: databases for heterogeneous data, a mobile phone application, a Big Data analytics platform, a simulation component, a decision support system, a public health policy decision-making model specification tool, and a social media analysis tool (Spanoudakis et al., 2017).
Figure 1.
The process of policy making, also known as the policy lifecycle, divided into four steps.
In the EVOTION project, Big Data analytic techniques investigate
hearing aid usage and its effectiveness for different types of individuals with hearing impairment,
temporary threshold shift episode occurrences for different types of individuals with hearing impairment and effectiveness of existing preventive measures (e.g., noise protection),
cognitive capabilities for different types of individuals with hearing impairment, and
correlations between different factors and comorbidities affecting hearing impairment and the overall well-being of people with hearing impairment.
As part of the EVOTION project, a clinical study will collect both retrospective static data from clinical repositories and prospective real-time data from clients. Retrospective data from clinical repositories in the United Kingdom and Denmark will be combined. As part of the clinical validation, over 1,000 people with hearing impairment will receive smart EVOTION hearing aids and a mobile phone application from clinics located in the United Kingdom and Greece. The hearing aids collect 21 time-stamped variables summarizing the sound environment and the client's usage of the volume control and the multiple hearing aid programs. These variables are sent wirelessly to the EVOTION mobile phone application every minute (Dritsakis et al., 2018). These clients also complete a battery of assessments, and a subsample will also receive a smartwatch including biosensors. Data types were chosen to elucidate the four patterns of interest as described above. These include environmental data (e.g., user location, noise), personal data (e.g., education, age, gender), and clinical data (e.g., smoking, family history, ototoxic medication), along with physiological, cognitive, and occupational data.
Table 1 of Dritsakis et al. (2018) provides an exhaustive list of all the data types that the EVOTION project collects. Big Data analytics will identify associations between client characteristics, context, and hearing aid outcomes, linking behavioral and physiological factors potentially affecting the effectiveness of hearing impairment management. A social media analysis tool also collects and analyzes opinions that clients and the public share on social networks regarding hearing impairment and its management without compromising privacy. Information available on social media, although available in the public domain, is nevertheless sensitive and not meant for collection and analysis without ethical consideration. Publicly available data must be recorded in either anonymized form or requires written consent from the data owner.
Table 1.
Technical challenges in Big Data acquisition, storage, management, and analysis, suggested mitigation paths, and supporting references.
| Challenge | Mitigation | Reference |
|---|---|---|
| Uncertain quality of data | Applying cleaning and editing techniques such as interactive, selective, automatic, and macroediting | Puts et al. (2015) |
| Inaccurate data | Predicting, detecting, and correcting inaccurate data in line with regulations regarding Big Data governance and management. Applying quick and automatic ways to monitor the quality of the data without the need to inspect the data in its most granular form to complement the decisions derived from Big Data | Håkonsson & Carroll (2016) and McFarland & McFarland (2015) |
| Potential and missing values that might affect the redundancy, reduction, and compression of data | Employing listwise or pairwise deleting, imputation, and illustration techniques to rectify this situation | Dong & Peng (2013) |
| Data storage at unprecedented rates and scales | Introducing a data lifecycle management procedure, as processing massive chunks of heterogeneous data within a limited time negatively affects the processing capabilities of Big Data analytical engines | M. Chen et al. (2014) |
| Data confidentiality | Effectively maintaining and analyzing large amounts of data without privacy errors are paramount. Preventing privacy breaches with internode and intranode parallelism and application-specific data processing | Yin & Zhao (2015) |
| Adaptability and scalability | Expanding Big Data analysis systems to support present and future datasets for more efficient policy decisions | M. Chen et al. (2014) |
Further, all people working with the data must protect it. Those responsible for the data and its handling must understand the ethics and accountability of social media data (Boyd & Crawford, 2012). EVOTION has an ethics board commissioned to monitor all potential ethical concerns and to provide advice on issues deriving from the use of personal data, for the benefit of the data owners, the general public, and the civil society.
The EVOTION platform includes databases and analytic tools to support the collection, storage, and processing of these datasets. The analyses, in turn, underpin a decision support system for stakeholders to identify, simulate, select, and monitor public health policies. The EVOTION decision support system models public health policy decisions to define, analyze, and address a wide range of hearing health issues. The decision support system supports stakeholders such as ministries, regulatory bodies, and nongovernmental organizations in formulating policies regarding hearing impairment (Katrakazas, Trenkova, Milas, Brdarić, & Koutsouris, 2017).
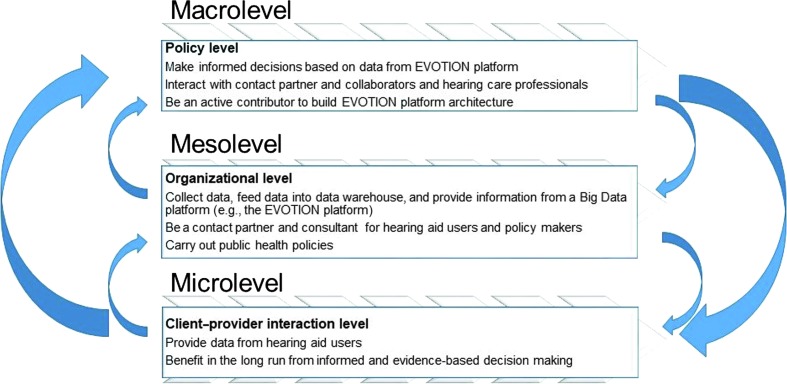
The ultimate objective of EVOTION is to enable and support a more holistic management of hearing impairment at the population level. To understand how this is done, it is relevant to look at how health care systems and their comprehensive networks are divided into three levels (WHO, 2002):
Macrolevel: policy level.
Mesolevel: organizational level.
Microlevel: client–provider interaction level.
Big Data can influence these three levels of health care services (Kuziemsky et al., 2014). For example, Big Data techniques and algorithms have organized and computed information to describe current trends in health policy at the macrolevel (Höchtl, Parycek, & Schöllhammer, 2016). Similarly, an analysis of a large dataset of hearing aid fittings and usage for subpopulations of people with hearing impairment has elucidated current clinical care at the microlevel (Timmer, Hickson, & Launer, 2017). Furthermore, as the three levels (macrolevel, mesolevel, and microlevel) interact, an action on a specific level will influence other levels. Figure 2 shows how the Big Data EVOTION project can lead to evidence-informed health care at the macrolevel, mesolevel, and microlevel.
Figure 2.
Evidence-informed health care at the macrolevel, mesolevel, and microlevel: the EVOTION research project as an example.
Making Sense of Data
Big Data Platforms and Their Potential Impact on Public Hearing Health Policy Making at the Macrolevel, Mesolevel, and Microlevel
The following section describes how Big Data platforms can support the transition of health policies into action at the macrolevel, mesolevel, and microlevel.
At the Macrolevel
The following describes how Big Data platforms can support the transition of health policies into action at the macrolevel.
Design of data-based regulatory policies to achieve better and more targeted impact on stakeholders and programs at the mesolevel and microlevel of hearing health care (Ong et al., 2014).
Political justification of public hearing health care programs that consider both audiology-specific factors and more general factors such as health inequalities (Asthana & Halliday, 2006).
Formulation of public hearing health care policies in line with economic (e.g., health care expenditure) and clinician evidence (e.g., clinicians' availability and competence skill set; Asthana & Halliday, 2006).
Creation of better supportive frames, for example, public hearing health care policy and funding schemes that specifically address national health information and research infrastructures (Caldwell & Mays, 2012).
Support of health programs for hearing impairment prevention, treatment, and rehabilitation to develop and maintain innovative and sustainable health systems (Jee & Kim, 2013).
Monitoring of hearing health care systems (Jee & Kim, 2013).
At the Mesolevel
The following describes how Big Data platforms can support the transition of health policies into action at the mesolevel.
Support for better and innovative health care delivery and services that improve client outcome through more accurate diagnoses and safer and more effective interventions (Kuziemsky et al., 2014).
Measurement of the impact of public health policies on health care delivery and services through targeted research (Brownson, Chriqui, & Stamatakis, 2009).
At the Microlevel
The following describes how Big Data platforms can support the transition of health policies into action at the microlevel.
Promotion of new ways of working and treatment paths that improve the effectiveness and efficiency of hearing health care services (Beaglehole & Bonita, 1998; Jee & Kim, 2013).
Benefit from the improved public hearing health policies leading to improved prevention, treatment, and rehabilitation measures for clients with hearing impairment (Heitmueller et al., 2014; Spanoudakis et al., 2017).
Challenges With Making Sense of Big Data
As described in the section above, the efficient and effective use of health data can lead to better public health decisions targeting hearing impairment prevention and management. However, to produce a complete picture of the issue, accurate sorting and preparation of data in accordance with regulations and requirements are needed (Thorpe & Gray, 2015). On this account, it is crucial to be aware of the challenges and limitations that Big Data analytics currently hold, for example, the challenge to automate the process of differentiating between structured versus unstructured data, representative versus unrepresentative data, and reliable versus unreliable sources (Stieb, Boot, & Turner, 2017). Challenges can be classified into three domains: technical, human, and political. Examples of challenges for each of these three domains are introduced below.
Technical Challenges
It can be difficult to draw data inferences due to missing data points, inaccurate or erroneous data, spurious correlations among data, and defective processes related to false correlations in the analysis algorithms. Large and constant data flows in the Big Data era can cause “big errors” in a Big Data ecosystem (Hoffman & Podgurski, 2013). Further, it remains hard to differentiate useful data from noise. In a health policy-making context, this can lead to wrong conclusions and ill-informed public health decisions. Although it is difficult to identify such erroneous decisions within hearing health care given that the usage of Big Data in this field is recent, this is a potential danger that all stakeholders must be aware of. Table 1 presents some of the technical challenges in Big Data acquisition, storage, management, and analysis and how these technical challenges can be mitigated.
Another current technical challenge is the fragmentation of health care data in information systems with incompatible formats (Raghupathi & Raghupathi, 2014). As a wide variety of datasets can be used as input to the Big Data analysis, legacy systems (older, superseded systems still in use) should be able to adapt and remap their relations with current data interoperability, heterogeneity, and existing standards (Höchtl et al., 2016). Interoperability allows stakeholders to employ data analytics to extract meaningful inferences from raw data (Ullah et al., 2017). Moreover, it is crucial to ensure efficient representation, access, and analysis of semistructured or unstructured data that are common in health care systems (C. L. P. Chen & Zhang, 2014). The technical challenges that heterogeneous datasets represent have been described in the hearing devices sector, where hearing aid and hearing implant manufacturers have suggested interoperability and standardization as mitigation paths (Laplante-Lévesque et al., 2016).
Human Challenges
Human-related challenges lie in the comprehension of different scenarios of data usage. The comprehension of data requires the cognitive ability of a human or systems to translate raw data into meaningful information, which subsequently allows sense-making processes and the translation of information into behaviors (Murdoch & Detsky, 2013).
As in all studies using data for evidence generation, one of the major challenges is to determine whether associations between variables are causal links between exposure and outcomes. Although Big Data ensures that associations are captured reliably, it does not ease the process of interpretation, distinguishing between causal and merely associated data points. On a macro level, this can lead to poor decision making and costly and ineffective policies.
Further, at a macrolevel, many policy makers are untrained to distinguish between good and bad data and may be prone to the influence of misused “facts” that interest groups present. In addition, scientific evidence may not carry as much weight as other types of evidence among policy makers, who operate on a different hierarchy of evidence than scientists. At a mesolevel, even if clinical guideline authors and clinicians had access to all the relevant data-supported information, sorting through that information to develop suitable clinical guidelines is exceedingly complex. Further, there are limitations due to missing retrospective data, to the abundance of nondigitized data, and to errors in collecting and cross-referencing extensive datasets, which can lead to incomplete information and conclusions (Johnson et al., 2016). At a microlevel, it is challenging to mitigate data sharing with third parties and the communication of data usage in transparent ways. This makes it hard for people with hearing impairment to assess how valuable their data are when pooled in Big Data analyses. Data ownership also comes with challenges, such as granting clients access to their data, allowing them to change, delete, share, or otherwise, further process their data. Clients must be able to port their data to different providers to take advantage of third-party applications that analyze their data and draw useful conclusions for personalized health care (European Data Protection Supervisor, 2015).
Political Challenges
At the microlevel–mesolevel of clinical care, evidence-based medicine, the application of research to clinical decision making (Sackett et al., 1996), has come a long way in anchoring practices in the highest level of scientific evidence. Yet, at the macrolevel, evidence-informed policy making has not seen the same uptake. For example, the Organization for Economic Co-operation and Development (2017) stated that “feeding high-quality evidence into policy making remains difficult, but is essential for improving public interventions. Governing better through evidence-informed policy making requires building capacity for the effective use and demand of evidence at all levels of government.” Health researchers and policy makers evolve in two separate worlds with different languages, values, rewards, and time horizons (Choi et al., 2005). As there is a problem both in the supply of relevant and timely evidence from researchers and the demand for this evidence from policy makers, experts call for linkages, networks, and close collaborations between policy makers, civil society, and researchers (International Network for the Availability of Scientific Publications, 2013).
High costs and the inability to effectively share health information across relevant stakeholders, organizations, health systems, and devices limit the power of Big Data analytics and their utilization (van Panhuis et al., 2014). Public health systems face the challenge to offer Big Data services and systems that secure people's rights to privacy and confidentiality. The aforementioned challenges and limitations need to be mitigated to support the successful use of Big Data analytics in policy making in health care.
Perspective: Applications of Big Data Evidence to Support Public Hearing Health Policies
Establishing Platforms Such as EVOTION as Standard Tools for Evidence-Informed Public Health Policies
The history of modern health care is often divided into three eras (Relman, 1988). First, the era of expansion (1940s–1960s) was characterized by the advent of policies supporting access to health care, rapid growth in hospitals facilities and clinicians, and raising expectations and demand from clients. Second, the era of cost containment (1960s–1980s) saw a backlash in expenditure due to the disproportionate increase in health care costs compared with general economic growth. Finally, the era of striving for improved assessment and accountability (1980s onward) is a result of the fact that health care costs continue to rise despite cost-cutting exercises. This present era focuses on effective and efficacious care, where the benefits of interventions outweigh their costs.
Going back to the example of the Food and Drug Administration Over-the-Counter Hearing Aid Act, how could Big Data support formulation of such future hearing health care policies? For example, as described above, the processes, content, and outcomes of policies could be anchored in the insights derived from large heterogeneous datasets such as the one that the EVOTION platform gathers and presents to stakeholders. Furthermore, the steps of implementation and evaluation could also be evidence-informed through large datasets that capture well the multiple dimensions of hearing health and its outcomes.
Implications for the Practicing Clinician
The EVOTION project aims to provide a platform to support public health policy making for hearing impairment. Decisions made about hearing impairment management at the macrolevel affect the services that clinicians provide to both people at risk of developing hearing impairment and to people with hearing impairment. Policies created at the macrolevel would influence the context in which clinicians practice at the microlevel. Such policies would potentially determine, for example, the clinical state of the client at presentation to the clinician, the stages and timeline of the clinical care pathway, or the structure and organization of rehabilitation services. However, the implications of EVOTION for the practicing clinician go beyond this. The EVOTION project uses novel strategies for collecting data about hearing impairment on a large scale. The analysis of this data will be directed toward the everyday challenges of the audiology clinic that all practicing clinicians face, with the goal of maximizing the benefit obtained from hearing interventions.
Currently available hearing aids can detect and classify different types of sound environments and manually or automatically switch between different settings to help the hearing difficulties of the clients who use them. Despite this ability, hearing aids only partially overcome the deficits associated with hearing impairment. As a consequence, hearing aid users sometimes visit their clinician several times for adjustments, and some eventually reject the hearing aids. Reasons for rejection include limited effectiveness in noisy environments due to poor sound quality and amplification of unwanted background noise.
It is well recognized that the factors that determine the experience of hearing impairment and success of rehabilitation are many and varied and extend far beyond the audiometric thresholds to include psychosocial, individual, and other health considerations.
The EVOTION project creates a platform to collect and analyze a large set of heterogeneous data and defines the interrelationships of multiple variables including hearing aid usage data and audiologic, physiological, cognitive, clinical, personal, behavioral, lifestyle, occupational, and environmental data. This is done through the standard clinical assessment process of interview and physical examination combined with real-time dynamic data of the participants obtained through the hearing aids linked to a smartphone application and physiological sensors as described above. The data is analyzed to identify specific factors that affect listening experience and are associated with hearing aid outcomes including usage.
Clinicians are provided with more detailed, personalized information on their clients, supporting them in their assessment of the client's overall hearing situation. For example, the EVOTION data will help clinicians to understand the factors determining the need for multiple clinic visits in some clients.
The real-time data collected by the hearing aids are also used by the EVOTION mobile phone application, which notifies the client by an alert about potentially hazardous noise exposure. The client then follows a simple decision aid via the application, thus allowing the early detection of potential noise-induced hearing impairment. Furthermore, the EVOTION project also includes auditory training delivered by the mobile phone application and hearing aid to the individual client, with the goal of improving auditory system function. The key elements of identification of outcome-related factors, knowledge of acoustic environments that clients experience, and customized hearing aids and auditory training will extend the scope of practicing clinicians.
Ultimately, Big Data evidence is expected to support clinicians to deliver person-centered care to improve outcomes for clients and increase the efficiency of resource usage at the microlevel, mesolevel, and macrolevel.
Potential of Big Data Evidence Beyond the EVOTION Project
Linking personal, proprietary, and government data to pursue health care objectives will maximize the benefits of Big Data. Increasing the amount of information available as open data and advancing data sharing will also add to these benefits, providing that the data formats are standardized and stored on interoperable platforms (Laplante-Lévesque et al., 2016). Clinical trial and other research data can provide an extended additional collective power of Big Data while addressing issues related to data ownership, privacy, and security (Stieb et al., 2017).
In the future, health care will become more data driven, and the ability to access, share, and optimize health care–related data will be even more critical to public health systems (Saboo, 2014). Therefore, platforms enabling the collection and analysis of Big Data will grow in availability and importance (Wehrens, 2014). Big Data such as those used in EVOTION are heterogeneous and collected both retrospectively and in real time. The EVOTION decision support system is developed together with local, regional, and national policy makers and advisors in the areas of health, as well as labor market and social policy, to promote more evidence-informed decision making, taking a coproduction approach.
Beyond EVOTION and extending to international health monitoring, accurately observing the need for hearing health care services and predicting, for example, which regions of the globe will have a higher prevalence of untreated hearing impairment in the future, can help clinicians target their prevention and management efforts (Ma, Wong Smith, Chu, & Taira Juarez, 2015). Such initiatives, deploying large screening studies to derive updated prevalence estimates of hearing impairment, are being run by, for example, the WHO, the International Centre for Evidence in Disability of the London School of Hygiene and Tropical Medicine, and the World Wide Hearing Foundation.
Further, Big Data uncovers inefficiencies in health systems and thereby reduces system costs (Raghupathi & Raghupathi, 2014). A better understanding of associations and patterns in health care delivery potentially improves care and the extraction of insights for improved and better informed decisions. Policy makers may critically appraise the current role of evidence in all steps of the policy-making process and develop guidelines for Big Data–informed health (Heitmueller et al., 2014).
Conclusion
This clinical focus article summarizes applications of Big Data for policy making in all four steps of the policy-making process and at all three levels of health care systems as applied to audiology and the hearing impaired population. EVOTION is presented as a concrete example of a research project and platform that can generate Big Data and, thereby, inform hearing health policies. Characteristics of EVOTION include a large dataset of heterogeneous data types chosen to elucidate patterns, a technology platform made of several components, close collaboration of policy makers in the project at all stages, and an interdisciplinary perspective to hearing health care. Keeping in mind that the policy lifecycle is an iterative process, the step of evaluation will identify new questions, problems, and issues that need addressing with improved policies, thereby starting a new policy cycle.
Big Data is not a universal remedy or a panacea for health care systems. Political, social, technical, and organizational challenges remain to transform raw data into insights. Mitigating those challenges carefully will help prevent costly and unintended negative consequences of Big Data, including ethically questionable practices. It is desired that stakeholders, including policy makers and clinicians, can translate Big Data evidence into sound hearing policies and clinical care.
Acknowledgments
This work is supported by the European Commission Horizon 2020 program (Grant 727521), awarded to the EVOTION consortium, which consists of 13 European Union organizations. The authors acknowledge the contribution of all EVOTION researchers to the project. Portions of this clinical focus article were presented at the 3rd International Internet & Audiology Meeting, Louisville, KY, July 2017, which was funded by National Institute on Deafness and Other Communication Disorders (NIDCD) Grant 1R13DC016547 and the Oticon Foundation.
Funding Statement
This work is supported by the European Commission Horizon 2020 program (Grant 727521), awarded to the EVOTION consortium, which consists of 13 European Union organizations. The authors acknowledge the contribution of all EVOTION researchers to the project. Portions of this clinical focus article were presented at the 3rd International Internet & Audiology Meeting, Louisville, KY, July 2017, which was funded by National Institute on Deafness and Other Communication Disorders (NIDCD) Grant 1R13DC016547 and the Oticon Foundation.
References
- Action on Hearing Loss. (2013). Evaluation framework for adult hearing services in England. Retrieved from http://www.actiononhearingloss.org.uk/-/media/ahl/documents/research-and-policy/reports/evaluation-framework-report.pdf
- American Academy of Audiology. (2018). The audiologist's guide to hearing aids, PSAP's hearables and OTC devices. Retrieved from https://www.audiology.org/over-counter-otc-hearing-aids
- Asthana S., & Halliday J. (2006). Developing an evidence base for policies and interventions to address health inequalities: The analysis of “Public Health Regimes.” The Milbank Quarterly, 84, 577–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bainbridge K. E., & Wallhagen M. I. (2014). Hearing loss in an aging American population: Extent, impact, and management. Annual Review of Public Health, 35, 139–152. [DOI] [PubMed] [Google Scholar]
- Beaglehole R., & Bonita R. (1998). Public health at the crossroads: Which way forward? The Lancet, 351, 590–592. [DOI] [PubMed] [Google Scholar]
- Boyd D., & Crawford K. (2012). Critical questions for big data: Provocations for a cultural, technological, and scholarly phenomenon. Information, Communication & Society, 15, 662–679. [Google Scholar]
- Brownson C. R., Chriqui F. A., & Stamatakis K. (2009). Understanding evidence-based public health policy. American Journal of Public Health, 99, 1576–1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell S., & Mays N. (2012). Studying policy implementation using a macro, meso and micro frame analysis: The case of the Collaboration for Leadership in Applied Health Research & Care (CLAHRC) programme nationally and in North West London. Health Research Policy and Systems, 10, 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Foundation for Healthcare Improvement. (2014). Accelerating healthcare improvement: Canadian Foundation for Healthcare Improvement’s Assessment Tool (CFHI Assessment Tool™ ). Retrieved from http://www.cfhi-fcass.ca/Libraries/Documents/Self-Assessment-Tool-2014-E.sflb.ashx
- Chen M., Mao S., Zhang Y., & Leung V. C. M. (2014). Big data: Related technologies, challenges and future prospects (pp. 81–89). Heidelberg, Germany: Springer. [Google Scholar]
- Chen C. L. P., & Zhang C.-Y. (2014). Data-intensive applications, challenges, techniques and technologies: A survey on big data. Information Sciences, 275, 314–347. [Google Scholar]
- Choi B. C., Pang T., Lin V., Puska P., Sherman G., Goddard M., … Clottey C. (2005). Can scientists and policy makers work together? Journal of Epidemiology and Community Health, 59, 632–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong Y., & Peng C.-Y. J. (2013). Principled missing data methods for researchers. SpringerPlus, 2(1), 222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dritsakis G., Kikidis D., Koloutsou N., Murdin L., Bibas A., Ploumidou K., … Bamiou D.-E. (2018). Clinical validation of a public health policy-making platform for hearing loss (EVOTION): Protocol for a big data study. British Medical Journal Open, 8(2), e020978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Commission. (2014). The use of big data in public health policy and research: Background information document. Retrieved from https://ec.europa.eu/health/sites/health/files/ehealth/docs/ev_20141118_co07b_en.pdf
- European Data Protection Supervisor. (2015). Meeting the challenges of big data: A call for transparency, user control, data protection by design and accountability. Retrieved from https://edps.europa.eu/sites/edp/files/publication/15-11-19_big_data_en.pdf
- Gapminder. (2018). Gapminder: Unveiling the beauty of statistics for a fact based world view. Retrieved from http://www.gapminder.org
- Goman A. M., Reed N. S., & Lin F. R. (2017). Addressing estimated hearing loss in adults in 2060. JAMA Otolaryngology–Head & Neck Surgery, 143, 733–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Håkonsson T., & Carroll T. (2016). Is there a dark side of big data—Point, counterpoint. Journal of Organization Design, 5, 5. [Google Scholar]
- Hearing Review. (2017a). IHS convention in Atlanta looks at OTC and new resources. Retrieved from http://www.hearingreview.com/2017/10/ihs-convention-atlanta-looks-otc-new-resources/
- Hearing Review. (2017b). President Trump signs OTC hearing aid legislation into law. Retrieved from http://www.hearingreview.com/2017/08/president-trump-signs-otc-hearing-aid-legislation-law/
- Heitmueller A., Henderson S., Warburton W., Elmagarmid A., Pentland A. S., & Darzi A. (2014). Developing public policy to advance the use of big data in health care. Health Affairs, 33, 1523–1530. [DOI] [PubMed] [Google Scholar]
- Höchtl J., Parycek P., & Schöllhammer R. (2016). Big data in the policy cycle: Policy decision making in the digital era. Journal of Organizational Computing and Electronic Commerce, 26, 147–169. [Google Scholar]
- Hoffman S., & Podgurski A. (2013). Big bad data: Law, public health, and biomedical databases. The Journal of Law, Medicine & Ethics, 41, 56–60. [DOI] [PubMed] [Google Scholar]
- International Network for the Availability of Scientific Publications. (2013). What is the evidence on evidence-informed policy-making? Lessons from the international conference on evidence-informed policy-making. Retrieved from http://www.inasp.info/uploads/filer_public/2013/04/22/what_is_the_evidence_on_eipm.pdf
- Jee K., & Kim G. (2013). Potentiality of big data in the medical sector: Focus on how to reshape the healthcare system. Healthcare Informatics Research, 19, 79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson A., Ghassemi M., Nemati S., Niehaus K., Clifton D., & Clifford G. (2016). Machine learning and decision support in critical care. Proceedings of the IEEE, 104, 444–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonassen D. H. (2012). Designing for decision making. Educational Technology Research and Development, 60, 341–359. [Google Scholar]
- Katrakazas P., Trenkova L., Milas J., Brdarić D., & Koutsouris D. (2017). The EVOTION decision support system: Utilizing it for public health policy-making in hearing loss. Studies in Health Technology and Informatics, 238, 88–91. [PubMed] [Google Scholar]
- Kuziemsky C. E., Monkman H., Petersen C., Weber J., Borycki E. M., Adams S., & Collins S. (2014). Big data in healthcare—Defining the digital persona through user contexts from the micro to the macro: Contribution of the IMIA organizational and social issues WG. Yearbook of Medical Informatics, 9, 82–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laplante-Lévesque A., Abrams H., Bülow M., Lunner T., Nelson J., Riis S. K., & Vanpoucke F. (2016). Hearing device manufacturers call for interoperability and standardization of Internet and audiology. American Journal of Audiology, 25, 260–263. [DOI] [PubMed] [Google Scholar]
- Linstone H. A., & Turoff M. (Eds.). (1975). The Delphi method: Techniques and applications (Vol. 29). Reading, MA: Addison-Wesley. [Google Scholar]
- Livingston G., Sommerlad A., Orgeta V., Costafreda S. G., Huntley J., Ames D., & Cooper C. (2017). Dementia prevention, intervention, and care. The Lancet, 390, 2673–2734. [DOI] [PubMed] [Google Scholar]
- Ma C., Wong Smith H., Chu C., & Taira Juarez D. (2015). Big data in pharmacy practice: Current use, challenges, and the future. Integrated Pharmacy Research and Practice, 4, 91–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarland D. A., & McFarland H. R. (2015). Big data and the danger of being precisely inaccurate. Big Data & Society, 2 https://doi.org/10.1177/2053951715602495 [Google Scholar]
- Murdoch T. B., & Detsky A. S. (2013). The inevitable application of big data to health care. Journal of the American Medical Association, 309, 1351–1352. [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2016). Hearing health care for adults: Priorities for improving access and affordability. Washington, DC: National Academies Press; Retrieved from http://www.nap.edu/catalog/23446/hearing-health-care-for-adults-priorities-for-improving-access-and [PubMed] [Google Scholar]
- National Collaborating Centre for Methods and Tools. (2009). Applicability and transferability of evidence tool (A&T Tool). National Collaborating Centre for Methods and Tools, Hamilton, McMaster University. Retrieved from http://www.nccmt.ca/resources/search/24
- Ola O., & Sedig K. (2014). The challenge of big data in public health: An opportunity for visual analytics. Online Journal of Public Health Informatics, 5, 223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong B., Morden A., Brooks L., Porcheret M., Edwards J., Sanders T., … Dziedzic K. (2014). Changing policy and practice: Making sense of national guidelines for osteoarthritis. Social Science & Medicine, 106, 101–109. [DOI] [PubMed] [Google Scholar]
- Organisation for Economic Co-operation and Development. (2017). Evidence-informed policy-making. Retrieved from http://www.oecd.org/gov/evidence-informed-policy-making.htm
- President's Council of Advisors on Science and Technology. (2014a). Big data: Seizing opportunities, preserving values. Washington, DC: Executive Office of the President. Report; Retrieved from https://obamawhitehouse.archives.gov/sites/default/files/docs/big_data_privacy_report_may_1_2014.pdf [Google Scholar]
- President's Council of Advisors on Science and Technology. (2014b). Big data and privacy: A technological perspective. Washington, DC: Executive Office of the President, President's Council of Advisors on Science and Technology; Retrieved from https://obamawhitehouse.archives.gov/sites/default/files/microsites/ostp/PCAST/pcast_big_data_and_privacy_-_may_2014.pdf [Google Scholar]
- Puts M., Daas P., & de Waal T. (2015). Finding errors in big data. Significance, 12, 26–29. [Google Scholar]
- Raghupathi W., & Raghupathi V. (2014). Big data analytics in healthcare: Promise and potential. Health Information Science and Systems, 2, 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Relman A. S. (1988). Assessment and accountability: The third revolution in medical care. New England Journal of Medicine, 319, 1220–1222. [DOI] [PubMed] [Google Scholar]
- Rosling H. (2006). The best stats you’ve ever seen [Video]. Retrieved from https://www.ted.com/talks/hans_rosling_shows_the_best_stats_you_ve_ever_seen?language=en
- Sabatier P. A., & Jenkins-Smith H. C. (1993). Policy change and learning: An advocacy coalition approach. Boulder, CO: Westview Press. [Google Scholar]
- Saboo A. (2014). Big data in healthcare: Using health IT innovation to accelerate value. FierceHealthcare. Retrieved from http://www.fiercehealthcare.com/healthcare/big-data-healthcare-using-health-it-innovation-to-accelerate-value
- Sackett D. L., Rosenberg W. M., Gray J. M., Haynes R. B., & Richardson W. S. (1996). Evidence based medicine: What it is and what it isn't. British Medical Journal, 312, 71–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spanoudakis G., Kikidis D., Bibas A., Katrakazas P., Koutsouris D., & Pontopidan N. H. (2017). Public health policy for management of hearing impairments based on big data analytics: EVOTION at genesis. Paper presented at the 17th IEEE International Bio-Informatics and Bio-Engineering Conference, October 23–25, 2017, Washington, DC Retrieved from http://openaccess.city.ac.uk/18205/1/BIBE_2017_paper_85.pdf [Google Scholar]
- Stieb D. M., Boot C. R., & Turner M. C. (2017). Promise and pitfalls in the application of big data to occupational and environmental health. BMC Public Health, 17, 372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorpe J., & Gray E. (2015). Big data and public health: Navigating privacy laws to maximize potential. Public Health Reports, 130, 171–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timmer B. H. B., Hickson L., & Launer S. (2017). Hearing aid use and mild hearing impairment: Learnings from big data. Journal of the American Academy of Audiology, 28, 731–741. [DOI] [PubMed] [Google Scholar]
- Ullah F., Habib M. A., Farhan M., Khalid S., Durrani M. Y., & Jabbar S. (2017). Semantic interoperability for big-data in heterogeneous IoT infrastructure for healthcare. Sustainable Cities and Society, 34, 90–96. [Google Scholar]
- van Panhuis W., Paul P., Emerson C., Grefenstette J., Wilder R., Herbst A., … Burke D. (2014). A systematic review of barriers to data sharing in public health. BMC Public Health, 14, 1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vos T., Barber R. M., Bell B., Bertozzi-Villa A., Biryukov S., Bolliger I., & Duan L. (2015). Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. The Lancet, 386, 743–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wehrens R. (2014). Beyond two communities—From research utilization and knowledge translation to co-production? Public Health, 128, 545–551. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2002). Innovative care for chronic conditions: Building blocks for actions: Global report. Retrieved from http://www.who.int/chp/knowledge/publications/iccc_ch2.pdf
- World Health Organization. (2012). Hearing loss in persons 65 years and older based on WHO global estimates on prevalence of hearing loss. Retrieved from http://www.who.int/pbd/deafness/news/GE_65years.pdf
- World Health Organization. (2015a). Ear and hearing care: Situation analysis tool. Retrieved from http://apps.who.int/iris/bitstream/10665/206141/1/9789241509954_eng.pdf
- World Health Organization. (2015b). Ear and hearing care: Planning and monitoring of national strategies—A manual. Retrieved from http://apps.who.int/iris/bitstream/10665/206138/1/9789241549479_eng.pdf
- World Health Organization. (2017a). Health policy. Retrieved from http://www.who.int/topics/health_policy/en/
- World Health Organization. (2017b). The health impact assessment procedure. Retrieved from http://www.who.int/hia/tools/process/en/index4.html
- World Health Organization. (2017c). World health assembly resolution on the prevention of deafness and hearing loss. Retrieved from http://apps.who.int/gb/ebwha/pdf_files/WHA70/A70_R13-en.pdf
- Yin J., & Zhao D. (2015). Data confidentiality challenges in big data applications. Paper presented at the IEEE International Conference on Big Data (Big Data 2015), Santa Clara, CA 2886–2888. Retrieved from http://ieeexplore.ieee.org/abstract/document/7364111 [Google Scholar]