Abstract
Importance: Adults with intellectual and developmental disabilities (IDD) are twice as likely as their peers without disabilities to have had a physical exam in the past year; however, as a result of challenging behavior during office visits, they are significantly less likely to have received recommended health screenings. Challenging behaviors in clinical settings have been identified as a barrier to providing adequate care for this population.
Objective: This scoping review examined the within-session effects of multisensory environments (MSEs) on people with IDD to determine the clinical utility of MSEs for this population.
Data Sources: Studies published between January 1, 2000, and August 1, 2018, were identified using Summon and Google Scholar.
Study Selection: Studies were included in the review if they systematically collected and reported data on within-session effects of an MSE intervention on people with IDD.
Findings: Thirteen studies met criteria for this review: 4 with Level I evidence, 2 with Level II evidence, 3 with Level III evidence, and 4 with Level IV evidence. Studies examined the effects of MSEs on maladaptive behaviors, positive behaviors, distress and discomfort, activity and alertness states, and cost of care for people with IDD.
Conclusion and Relevance: Preliminary support was found for the use of MSEs in clinical settings to reduce anxiety and challenging behaviors in patients with IDD during clinical care. Further research is needed to determine the efficacy of MSEs for producing the effects described in this review.
What This Article Adds: The findings support the potential of MSEs as a tool that occupational therapy practitioners can use to support their clients with IDD who have sensory sensitivities in clinical settings. This article also highlights a multidisciplinary approach whereby medical providers and occupational therapy practitioners could work together in nontraditional ways to support this population.
Intellectual and developmental disabilities (IDD) are disorders that originate before adulthood and are characterized by lifelong impairments in intellectual, adaptive, or physical functioning (National Institutes of Health, 2010). Impairments in any area can range from mild to profound. People with IDD consistently experience poorer health status than the general population (Havercamp & Scott, 2015).
Even among people with IDD who regularly use health care services, disparities persist. Havercamp and Scott (2015) found that even though adults with IDD were twice as likely as their peers without disabilities to have had a physical exam in the past year, they were significantly less likely to have received the health screenings recommended for their age group. Challenging behavior during office visits has been identified as a barrier to providing adequate care for this population and may contribute to these disparities (Casamassimo et al., 2004; Hulland & Sigal, 2000; Tyler et al., 2010). Self-advocates, caregivers, and health care providers participating in focus groups and interviews in the greater Boston area felt that patients with challenging behaviors were automatically labeled as difficult and often went without routine health services or received them only under heavy sedation (Ward et al., 2010).
Some of the behaviors that make it difficult to provide health care to people with IDD may be brought on by the noxious sensory environment of clinical settings (e.g., bright lights, beeping machines, noisy waiting rooms) and procedures (e.g., pain, cold instruments, intrusive touch). Sensory processing difficulties are a well-documented feature of autism spectrum disorder (ASD; Baker et al., 2008; Tavassoli et al., 2014), and a study by Baranek et al. (2006) revealed that children with developmental disabilities displayed patterns of hyperresponsiveness to sensory stimuli similar to those of children with ASD. This increased sensitivity can generate disproportionate behavioral responses to stimuli that may not be bothersome to a typically developing child. The sensory experience of medical treatment, unpleasant for most, may become nearly intolerable for people with sensory hypersensitivity. The use of multisensory environments (MSEs) in clinical spaces may offer a means of minimizing the discomfort people with sensory sensitivities experience in these spaces and make it easier for them to receive appropriate medical care.
MSEs were first conceptualized in the 1970s by two Dutch therapists as an accessible, nondirective leisure activity for people with developmental disabilities (Hogg, Cavet, et al., 2001). MSEs vary in composition but are commonly dimly lit spaces that include elements such as mirror balls, bubble tubes, fiber-optic sprays, projectors with colorful rotating images, aromatic oils, relaxing music, a variety of comfortable seating, and padded floors (Chan et al., 2010; Koller et al., 2018; Lancioni et al., 2002). The result is gentle sensory stimulation that produces a calm and engrossing atmosphere.
Proposed benefits of MSEs include relaxation, pain management, improved attention, and a reduction in maladaptive behaviors (Ashby et al., 1995; Gómez et al., 2016; Hill et al., 2012; Poza et al., 2013; Schofield & Davis, 2000; Singh et al., 2004). Research on MSEs with people with IDD has focused on determining whether repeated exposure to an MSE can modify participants’ behavior over time. The generalization of behavior change (e.g., reduction in challenging behaviors) observed in an MSE to participants’ daily living environment has been an area of emphasis and has produced mixed results. Kaplan et al. (2006) reported reductions in the daily frequency of challenging behaviors of two of three participants receiving occupational therapy in an MSE room, whereas Chan et al. (2005) found no difference between MSEs and activity therapy in reducing challenging behaviors. Little interest has been shown in the effects that MSEs may have on people with IDD while they are in the MSE (i.e., within-session effects).
The initial intent of this review was to examine the use of MSEs in medical treatment, but the shortage of research in this area prompted us to investigate the within-session effects of MSEs instead. The rationale for this approach is that within-session effects could be replicated in an MSE in a clinical setting and potentially affect clinical care outcomes.
Method
We aimed to answer the following two research questions:
What are the within-session effects of MSEs on people with IDD?
What is the clinical utility of MSEs for people with IDD?
Because of the nature of the research questions and the high variability in the design of included studies, we did not perform a meta-analysis. Literature for this review was identified using the Summon search tool and Google Scholar. Summon is a web-scale discovery service that simultaneously searches multiple academic databases and library content. Additional literature was identified by mining bibliographies of articles that met the inclusion criteria and following “cited by” links on Google Scholar. The first author performed an initial search in February 2018 and an updated search in August 2018. Literature from January 1, 2000, to August 1, 2018, was included in this review. The following terms were used to search the title fields of potential studies: Snoezelen, multisensory room, multisensory environment, multisensory therapy, and sensory adapted environment. Because of the varied terminology used to refer to IDD (e.g., profound multiple disabilities, learning disabilities, mental retardation), as well as the many diagnoses meeting the criteria for developmental disability, we used no IDD-specific search terms.
To meet the inclusion criteria for this review, studies had to be published in English in a peer-reviewed academic journal and report within-session effects of an MSE on people with IDD. Studies met the IDD inclusion criteria if they stated in some form that participants had intellectual disabilities or a diagnosis that fit the National Institutes of Health’s (2010) definition of developmental disability: “a severe, long term disability that can affect cognitive ability, physical functioning, or both. These disabilities appear before age 22 and are likely to be life-long” (p. 1). Snoezelen is a term that is commonly used to refer to MSEs in the literature; however, it is the brand name of a specific manufacturer of multisensory equipment and is not the focus of this review. Studies met the criteria of using an MSE intervention if the environment was modified to provide gentle stimulation of multiple sensory systems, regardless of whether the equipment used to do so was manufactured by Snoezelen.
In addition, although there are no standard requirements for the composition of an MSE, we did not consider studies that used a single piece of equipment as having used an MSE intervention and excluded them from the review. Studies involving participants of all ages were included. Studies were excluded if they did not include participants with IDD, did not use an MSE intervention, or did not report within-session effects of the intervention on the participants with IDD. For example, several studies reported on behavior immediately after or between MSE sessions and were excluded from this review. Studies targeting people with cognitive impairments acquired in adulthood such as dementia and traumatic brain injury were also excluded, as were review articles and studies that did not systematically collect data (e.g., anecdotal data).
Articles were reviewed for inclusion in a stepwise fashion. First, all articles not published in English or in a peer-reviewed journal were removed. Second, the first and second authors (Breslin and Guerra) independently screened the abstracts of the remaining articles. Those that appeared to meet the inclusion criteria were reviewed in full. Third, the reviewers met and discussed their individual evaluations, and consensus was reached on all items. Articles identified in the search process for which full text was not available online were retrieved by interlibrary request from a local public university. Each included study was independently assessed by two reviewers and assigned to a level of evidence category. These categories are outlined in the American Occupational Therapy Association’s (2015) Guidelines for Systematic Reviews:
Level I: systematic reviews, meta-analyses, randomized controlled trials (RCTs)
Level II: two-group, nonrandomized studies (e.g., cohort, case–control)
Level III: one-group, nonrandomized (e.g., before and after, pretest–posttest)
Level IV: descriptive studies that include analysis of outcomes (single-subject, case series)
Level V: case reports and expert opinion that include narrative literature reviews and consensus statements.
Results
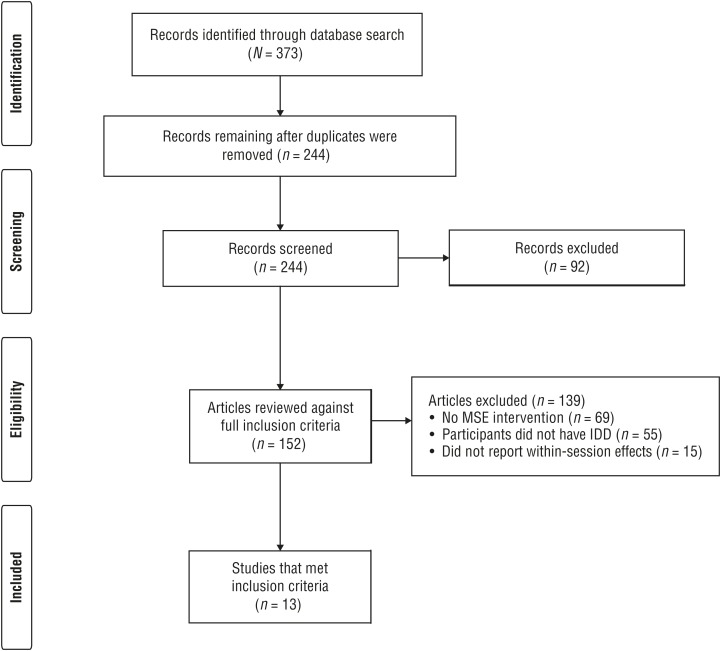
The initial search yielded 373 publications. After the removal of non-English (n = 16), non-peer-reviewed (n = 76), and duplicate (n = 129) publications, 152 abstracts were reviewed against the full inclusion criteria. Only 13 studies met the inclusion criteria for this review (Figure 1).
Figure 1.
Flow diagram for studies included in the systematic review.
Note. IDD = intellectual and developmental disabilities; MSE = multisensory environment.
Figure format from “Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement,” by D. Moher, A. Liberati, J. Tetzlaff, and D. G. Altman; PRISMA Group, 2009, PLoS Medicine, 6, e1000097. https://doi.org/10.1371/journal.pmed.1000097
Sample sizes ranged from 2 to 50 participants. Outcomes measured included maladaptive behaviors (e.g., aggression, stereotypy, self-injury; n = 6), positive behavior (e.g., communication, focus, engagement, cooperation; n = 8), distress and discomfort (n = 4), activity and alertness states (n = 2), and cost of care (n = 1). Many studies reported both within- and postsession effects of MSE intervention, but we consider only within-session effects in this review. Several studies reported on multiple outcomes and are discussed in more than one section of the Results. Six studies targeted adults with IDD, and 7 targeted children and adolescents with IDD. Studies primarily targeted participants with severe to profound IDD (n = 11). Three studies included participants with mild and moderate IDD, but none exclusively examined this population.
The MSE elements used across studies were similar. Music, slow-moving visual projections, bubble tubes, vibrating elements, and aromatic oils were the most commonly included items. Studies that took place in a residential setting tended to use olfactory stimulation more frequently than those that took place in a clinical setting, and deep-pressure stimulation was used only in clinical settings. See Table 1 at the end of this article for a brief overview of included studies.
Table 1.
Characteristics of the Studies Included in the Scoping Review
| Author/Year | Level of Evidence | Setting | Sample Size | Age Range, yr | IDD Characterization | MSE Elements Used | Outcomes Measured | Findings |
| Cermak et al. (2015) | I | Dental | 22 | 6–12 | ASD | Dimmed lighting, projected visual effects, rhythmic music, body-hugging wrap, weighted vest | Physiological distress, pain, sensory discomfort, cost-of-care estimates | Decreases in physiological distress, pain intensity, and sensory discomfort were seen in children with ASD and typically developing children. Cost-of-care measures produced mixed results. |
| Cuvo et al. (2001) | IV | Residential facility | 3 | 44–65 | Profound | Vibrating cushions, projected visual effects, lava lamp, bubble tube, aromatherapy oils, soft music, bean bags, rocking chair, various interactive objects | Stereotypic behaviors and engagement | In Experiment 1, all participants displayed lower stereotyped behaviors and higher engagement in MSE. In Experiment 2, all participants displayed lower stereotyped behavior and higher engagement in outdoor condition. |
| Fava & Strauss (2010) | II | Residential facility | 27 | 30–48 | Profound; 9 with co-occurring ASD | Vibrating cushions, projected visual effects, lava lamp, bubble tube, aromatherapy oils, bean bags, rocking chair, various textured objects | Disruptive and prosocial behaviors | Participants with ASD displayed decreased aggressive and stereotypic behavior in the MSE. Participants with profound IDD displayed lower stereotypy and increased social behavior and activity in the stimulus-preference MSE. |
| Hill et al. (2012) | IV | Residential facility | 2 | 14–18 | Severe with co-occurring ASD | Padded walls and floor, light, mirror balls, music, bubble tubes | Stereotypic behaviors and engagement | Both participants displayed lower stereotyped behaviors in MSE conditions. Engagement was higher in MSE than living room when matched for attention |
| Koller et al. (2018) | IV | Hospital | 5 | 6–17 | Unspecified | Fiber-optic spray, massage tube, bubble tube, music, projected visual effects | Physiological and behavioral changes | Overall, more positive behaviors were displayed in MSE conditions. Results for physiological changes were mixed. |
| Lindsay et al. (2001) | II | Residential facility | 8 | 23–62 | Profound | Dimmed lighting, bubble tubes, fiber-optics, colored lights, projected visual effects, soft music, aroma board, tactile wall, mirrors | Positive and negative communication | Results showed increased positive communication and decreased negative communication in MSE condition. |
| Potter et al. (2018) | III | Dental | 44 | 33–62a | Mild to profound | Dimmed lighting, projected visual effects, vibroacoustic speakers, rhythmic music, aromatic oil | Agitated behavior | Decreased duration and frequency of agitated behaviors were observed in the MSE condition. |
| Shapiro, Melmed, et al. (2009) | I | Dental | 16 | 6–11 | Moderate to severe | Dimmed lighting, projected visual effects, rhythmic music, body-hugging wrap, bass vibrator connected to chair | Anxious behaviors, physiological arousal, cooperation during treatment | Decreased duration and magnitude of anxious behaviors, decreased physiological arousal, and increased cooperation were observed in MSE conditions. No effect was seen on the number of anxious behaviors. |
| Shapiro, Sgan-Cohen, et al. (2009) | I | Dental | 16 | 6–11 | Moderate to severe | Dimmed lighting, projected visual effects, rhythmic music, body-hugging wrap, bass vibrator connected to chair | Anxious behaviors and relaxation | Decreased duration of anxious behaviors and increased relaxation were observed for both groups in MSE condition. |
| Singh et al. (2004) | I | Residential facility | 45 | 22–57 | Severe to profound with co-occurring mental health diagnosis | Fiber-optics, laser light show, disco balls, nature sound generator, soft music, aromatherapy, scented markers, vibrating massagers, interactive light panels, mirrors, rockers | Aggression and self-injury | Results showed decreased aggression and self-injury in MSE condition. |
| Thompson (2011) | III | School | 50 | 6–17 | Severe to profound | Unspecified | Focus, self-injury, relaxation, happiness, engagement | Results showed increased sustained focus, decreased self-injurious behaviors, and increased total relaxation during the MSE intervention. |
| Tunson & Candler (2010) | IV | Nursing facility | 3 | 3–10 | Severe | Light effects, bubble tube, music, aroma | Behavior states | Two participants showed no change in behavior states; 1 participant showed a decrease in self-directed behavior. |
| Vlaskamp et al. (2003) | III | Residential facility | 19 | 18–41 | Profound | Observations occurred at multiple facilities; MSE elements were not specified | Activity level | Similar patterns of activity were observed in MSE and normal living environment. Interaction with materials was higher in MSE condition. |
Note. ASD = autism spectrum disorder; IDD = intellectual and developmental disabilities; MSE = multisensory environment.
Estimated from reported means and standard deviations because age range was not provided.
Maladaptive Behaviors
Six studies assessed the effect of MSEs on maladaptive behaviors (e.g., aggression, self-injury, stereotypy). All studies examining maladaptive behaviors used behavioral observations and targeted participants with severe to profound IDD. Five studies—1 with Level I evidence (Singh et al., 2004), 2 with Level II evidence (Fava & Strauss, 2010; Lindsay et al., 2001), and 2 with Level IV evidence (Cuvo et al., 2001; Hill et al., 2012)—took place in residential facilities and compared frequencies of maladaptive behaviors in MSE conditions with other therapies or leisure activities in adolescents and adults. One Level III study (Thompson, 2011) compared self-injurious behavior of children in regular classroom and MSE conditions. All studies used a permanent MSE space at the facility (see Table 1 for characteristics of the MSE) and reported reduced frequency of maladaptive behaviors in MSE conditions.
Positive Behaviors
Nine studies reported on the effects of MSEs on a range of positive behaviors. Two studies with Level I evidence reported increased cooperation among children during dental examination and treatment when multisensory equipment was used in the examination room compared with the regular dental environment (Cermak et al., 2015; Shapiro, Melmed et al., 2009). Four studies, 1 with Level II evidence (Fava & Strauss, 2010), 1 with Level III evidence (Vlaskamp et al., 2003), and 2 with Level IV evidence (Cuvo et al., 2001; Hill et al., 2012), used behavioral observations to compare levels of engagement and prosocial behaviors in MSEs with those in living rooms among adolescents and adults with severe and profound IDD at residential facilities. Three of these studies found more positive behaviors during MSE sessions, although only 1 study with Level IV evidence (Hill et al., 2012) controlled for the level of attention participants received in each condition. The fourth study did not find marked differences between MSE and normal living conditions but did see an increase in interaction with materials in the MSE condition (Vlaskamp et al., 2003). One Level III study found increased focus and engagement among children while in an MSE room compared with their regular classroom setting (Thompson, 2011). The authors of a study with Level IV evidence delivered MSE therapy at children’s bedside in a pediatric hospital and observed significantly more positive behaviors during MSE therapy than when participants watched a preferred TV program (Koller et al., 2018). The remaining study with Level II evidence found that MSE therapy increased positive communication behaviors among adults with severe IDD to a greater extent than hand massage and active therapy, but to a lesser extent than relaxation therapy (Lindsay et al., 2001).
Distress and Discomfort
All 4 studies examining the effect of MSEs on distress and discomfort were conducted in dental offices and compared routine dental care in a regular dental environment with the same care performed in an environment that had been modified to include multisensory equipment. Three studies with Level I evidence used a combination of behavioral observations and electrodermal activity measures to determine children’s discomfort during care and found decreased physiological distress and decreased duration and magnitude of distress behaviors (Cermak et al., 2015; Shapiro, Melmed et al., 2009; Shapiro, Sgan-Cohen et al., 2009). Two of these studies targeted children with moderate to severe IDD, and 1 targeted children with ASD (Cermak et al., 2015). One of these studies also reported reductions in self-reported pain in the MSE environment, but only half of the participants with ASD completed the ratings (Cermak et al., 2015). The fourth study likewise compared dental care in regular and MSE environments but targeted adults with mild to profound IDD (Potter et al., 2018). This Level III study used behavioral observations and found reductions in the frequency and duration of distressed behaviors in the MSE condition.
Activity and Alertness States
Two studies used behavioral observations to examine the effect of MSEs on activity and alertness states in people with severe IDD. One study with Level IV evidence took place in a pediatric nursing facility and found no change in behavior state among children in an MSE compared with their regular classroom environment (Tunson & Candler, 2010). The second study had Level III evidence and likewise reported similar levels of activity between living rooms and MSE rooms among adults at residential facilities (Vlaskamp et al., 2003).
Cost of Care
Only Cermak et al. (2015) provided cost-of-care comparisons between MSE and control conditions. This Level I study used length of dental cleaning and the number of hands required to restrain children during examination and cleaning to estimate cost of care and reported mixed results. Fewer hands were required to restrain children with ASD in the MSE dental environment, but the time required to complete the procedures increased. The authors suggested that the increased time may have indicated a more thorough cleaning.
Discussion
The current literature on the within-session effects of MSEs has reported a range of positive outcomes for people with IDD and emphasizes reduced distress, discomfort, and maladaptive behavior and increased engagement. These results support our hypothesis that people who experience sensory sensitivities and anxiety may benefit from MSEs in clinical settings. The research included in our review did not examine the mechanism of MSE effects. Multisensory stimulation may exhibit a calming effect on the central nervous system, as suggested by Poza et al. (2013), or it may simply serve as an intriguing distraction from unpleasant feelings and stimuli.
A notable difference between the use of MSEs in residential and school settings versus clinical settings is the opportunity for the person to move about, explore, and interact with the environment. In most studies set in residential facilities, MSE sessions were self-directed, and participants were free to choose equipment that suited their preferences. In clinical interventions, participants either were required to remain stationary for a procedure or were unable to move because of physical limitations. In either case, participants in clinical settings tended to be passive recipients of the sensory elements.
A benefit to the stationary nature of the clinical MSE is the ability to use weighted body-hugging wraps and weighted aprons for deep-pressure stimulation. Some research has reported that deep-pressure stimulation promotes relaxation in children and adults with IDD, suggesting that deep-pressure stimulation may serve an important function in a clinically based MSE (Edelson et al., 1999; Reynolds et al., 2015). In contrast to other commonly used forms of restraint and stabilization, the deep-pressure stimulation elements used in studies that met the inclusion criteria were well received by both participants and parents.
Multisensory Environments in Dental Care
Research has consistently shown that people with IDD experience large disparities in oral health compared with the general population (Anders & Davis, 2010; Anderson et al., 2013; Morgan et al., 2012). The resistive behaviors that can accompany sensory sensitivities and anxiety have been identified as a significant barrier in providing dental care to this population (Casamassimo et al., 2004). All 4 studies examining the use of MSEs in dental offices found that patients with IDD and ASD displayed decreased anxious behaviors and decreased phasic electrodermal activity, indicating greater relaxation during a standard dental exam and cleaning (Cermak et al., 2015; Shapiro, Melmed, et al., 2009; Shapiro, Sgan-Cohen, et al., 2009; Potter et al., 2018). In addition, both studies that measured cooperation during care reported greater cooperation in the MSE condition. Only 1 study (Cermak et al., 2015) measured the use of restraint and reported a decreased requirement for physical restraint in the MSE condition. Cermak et al. (2015) also suggested that the reduction in anxious and challenging behaviors may allow providers to complete more thorough examinations and cleanings. Although the evidence is preliminary, the results of this review support the utility of MSEs during dental care for patients with IDD who display anxious and challenging behaviors.
Several studies included in this review demonstrated the feasibility of implementing MSEs in dental practice. Specialty multisensory equipment is often expensive, but Cermak et al. (2015) demonstrated large treatment effect sizes for physiological distress and dentist-reported cooperation in children with ASD using only a CD player, projector, and weighted body-hugging wrap. These results suggest that the abundance of specialty equipment that characterizes the typical MSE may not be necessary to achieve the desired effect, making it less cost prohibitive to implement. Moreover, 2 dental MSE studies saw similar decreases in physiological and behavioral anxiety in typically developing children, indicating that MSE use in dental care may also be beneficial for the general population. In addition, implementing MSEs in clinical care would require minimal staff training. Adapting to working in the dim lighting of an MSE was the only adjustment reported in clinically based MSE interventions and was achieved by dental providers wearing headlamps that could be aimed directly into patients’ mouths.
Multisensory Environments in Medical Care
Little research exists on the use of MSEs in clinical care outside of dental practices. However, similar challenges to providing care have been identified in both settings. Research has shown that children with IDD experience greater anxiety related to medical examination and treatment than their peers who are developing typically, and increased anxiety has been linked to uncooperative behaviors (Evans et al., 2005; Gillis et al., 2009; Pascolo et al., 2018). A survey of nurses specializing in developmental disabilities by Tyler et al. (2010) identified lack of patient cooperation as the number one barrier to patients with IDD receiving recommended screenings. It is possible that the calming effect seen in dental MSEs could be replicated during routine medical care.
Limitations
Despite the overall positive reports on within-session effects of MSEs, we should note that these effects are not necessarily universal for people with IDD. Fava and Strauss (2010) reported that multiple participants expressed a clear dislike of the MSE. Thresholds for sensory stimulation can vary widely among people with IDD. Preference and tolerance for sensory input should be assessed before exposing a person to an MSE, regardless of setting. Various methods of preference assessment have been used with people with IDD (Virués-Ortega et al., 2014); however, Vlaskamp et al. (2003) noted that instruments for these assessments have yet to be developed and validated. Future research should include the development of sensory assessment tools that are feasible for use in clinical settings to systematically address patients’ sensory needs.
The current evidence for within-session effects of MSEs for people with IDD is promising, but preliminary. All of the studies included in this scoping review had small sample sizes, and few used adequate control conditions. Many studies conducted in residential settings did not control for room size, the number of people present, and the level of interaction with staff in MSE and control conditions. The majority of included studies relied exclusively on behavioral observations to measure outcomes. Behavioral observation is a common method used in research with people with IDD with limited communicative abilities (Hogg, Reeves, et al., 2001; Petry & Maes, 2006), but Koller et al. (2018) pointed out that coding behavior in a population with poor motor control can be ambiguous (e.g., a spasm vs. an intentional behavior). Moreover, coding behavior in MSE sessions precludes the possibility of blinding observers to study conditions, which may have introduced bias to the results.
Researchers have largely focused on the severe to profound classifications of IDD, making it difficult to determine the benefit of MSEs for people with a higher level of intellectual functioning. As shown in Figure 1, fewer than half of the studies that used an MSE intervention included participants with IDD. The majority of studies targeted adults with dementia; these studies were excluded. Of those studies that did include people with IDD, fewer than half examined within-session effects, and fewer still were conducted in a clinical setting.
Implications for Occupational Therapy Practice and Research
Occupational therapy practitioners who work with people with IDD are familiar with their sensory needs and are aware of many strategies available to assist with daily activities such as medical and dental appointments. The results of this review support the use of MSEs as one such strategy occupational therapy practitioners may use in supporting their clients with IDD. The results of this review have the following implications for occupational therapy practice and research:
Occupational therapy practitioners should work with clients and health care providers to identify and address sensory elements that contribute to anxiety or maladaptive behaviors in clinical settings.
MSE interventions should be flexible and allow for customization of the sensory experience to suit each clients’ individual needs.
Future research should examine the use of MSEs in clinical settings beyond dental practice for children and adults with a range of functional levels.
Conclusion
The results of this review provide preliminary support for the utility of MSEs in reducing anxiety and challenging behaviors during clinical care for people with IDD. There is not yet enough evidence to recommend the widespread adoption of MSEs in clinical settings. However, the results show promise and warrant further investigation. Future research should expand on the work done in dental settings to examine the utility of MSEs in other areas of medical practice.
Acknowledgments
This research was conducted at The Resource Exchange in Colorado Springs, Colorado.
Footnotes
Indicates articles included in the scoping review.
References
- American Occupational Therapy Association. (2015). Guidelines for systematic reviews. Retrieved from http://ajot.submit2aota.org/journals/ajot/forms/systematic_reviews.pdf
- Anders P. L., & Davis E. L. (2010). Oral health of patients with intellectual disabilities: A systematic review. Special Care in Dentistry, 30, 110–117. 10.1111/j.1754-4505.2010.00136.x [DOI] [PubMed] [Google Scholar]
- Anderson L. L., Humphries K., McDermott S., Marks B., Sisirak J., & Larson S. (2013). The state of the science of health and wellness for adults with intellectual and developmental disabilities. Intellectual and Developmental Disabilities, 51, 385–398. 10.1352/1934-9556-51.5.385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashby M., Lindsay W., Pitcaithly D., Broxholme S., & Geelen N. (1995). Snoezelen: Its effects on concentration and responsiveness in people with profound multiple handicaps. British Journal of Occupational Therapy, 58, 303–307. 10.1177/030802269505800711 [DOI] [Google Scholar]
- Baker A. E., Lane A., Angley M. T., & Young R. L. (2008). The relationship between sensory processing patterns and behavioural responsiveness in autistic disorder: A pilot study. Journal of Autism and Developmental Disorders, 38, 867–875. 10.1007/s10803-007-0459-0 [DOI] [PubMed] [Google Scholar]
- Baranek G. T., David F. J., Poe M. D., Stone W. L., & Watson L. R. (2006). Sensory Experiences Questionnaire: Discriminating sensory features in young children with autism, developmental delays, and typical development. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 47, 591–601. 10.1111/j.1469-7610.2005.01546.x [DOI] [PubMed] [Google Scholar]
- Casamassimo P. S., Seale N. S., & Ruehs K. (2004). General dentists’ perceptions of educational and treatment issues affecting access to care for children with special health care needs. Journal of Dental Education, 68, 23–28. [PubMed] [Google Scholar]
- *Cermak S. A., Stein Duker L. I., Williams M. E., Dawson M. E., Lane C. J., & Polido J. C. (2015). Sensory adapted dental environment to enhance oral care for children with autism spectrum disorders: A randomized controlled pilot study. Journal of Autism and Developmental Disorders, 45, 2876–2888. 10.1007/s10803-015-2450-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan S., Fung M. Y., Tong C. W., & Thompson D. (2005). The clinical effectiveness of a multisensory therapy on clients with developmental disability. Research in Developmental Disabilities, 26, 131–142. 10.1016/j.ridd.2004.02.002 [DOI] [PubMed] [Google Scholar]
- Chan S. W., Thompson D. R., Chau J. P., Tam W. W., Chiu I. W., & Lo S. H. (2010). The effects of multisensory therapy on behaviour of adult clients with developmental disabilities—A systematic review. International Journal of Nursing Studies, 47, 108–122. 10.1016/j.ijnurstu.2009.08.004 [DOI] [PubMed] [Google Scholar]
- *Cuvo A. J., May M. E., & Post T. M. (2001). Effects of living room, Snoezelen room, and outdoor activities on stereotypic behavior and engagement by adults with profound mental retardation. Research in Developmental Disabilities, 22, 183–204. 10.1016/S0891-4222(01)00067-1 [DOI] [PubMed] [Google Scholar]
- Edelson S. M., Edelson M. G., Kerr D. C., & Grandin T. (1999). Behavioral and physiological effects of deep pressure on children with autism: A pilot study evaluating the efficacy of Grandin’s Hug Machine. American Journal of Occupational Therapy, 53, 145–152. 10.5014/ajot.53.2.145 [DOI] [PubMed] [Google Scholar]
- Evans D. W., Canavera K., Kleinpeter F. L., Maccubbin E., & Taga K. (2005). The fears, phobias and anxieties of children with autism spectrum disorders and Down syndrome: Comparisons with developmentally and chronologically age matched children. Child Psychiatry and Human Development, 36, 3–26. 10.1007/s10578-004-3619-x [DOI] [PubMed] [Google Scholar]
- *Fava L., & Strauss K. (2010). Multi-sensory rooms: Comparing effects of the Snoezelen and the Stimulus Preference environment on the behavior of adults with profound mental retardation. Research in Developmental Disabilities, 31, 160–171. 10.1016/j.ridd.2009.08.006 [DOI] [PubMed] [Google Scholar]
- Gillis J., Hammond Natof T., Lockshin S., & Romanczyk R. (2009). Fear of routine physical exams in children with autism spectrum disorders: Prevalence and intervention effectiveness. Focus on Autism and Other Developmental Disabilities, 24, 156–168. 10.1177/1088357609338477 [DOI] [Google Scholar]
- Gómez C., Poza J., Gutiérrez M. T., Prada E., Mendoza N., & Hornero R. (2016). Characterization of EEG patterns in brain-injured subjects and controls after a Snoezelen® intervention. Computer Methods and Programs in Biomedicine, 136, 1–9. 10.1016/j.cmpb.2016.08.008 [DOI] [PubMed] [Google Scholar]
- Havercamp S. M., & Scott H. M. (2015). National health surveillance of adults with disabilities, adults with intellectual and developmental disabilities, and adults with no disabilities. Disability and Health Journal, 8, 165–172. 10.1016/j.dhjo.2014.11.002 [DOI] [PubMed] [Google Scholar]
- *Hill L., Trusler K., Furniss F., & Lancioni G. (2012). Effects of multisensory environments on stereotyped behaviours assessed as maintained by automatic reinforcement. Journal of Applied Research in Intellectual Disabilities, 25, 509–521. 10.1111/j.1468-3148.2012.00697.x [DOI] [PubMed] [Google Scholar]
- Hogg J., Cavet J., Lambe L., & Smeddle M. (2001). The use of “Snoezelen” as multisensory stimulation with people with intellectual disabilities: A review of the research. Research in Developmental Disabilities, 22, 353–372. 10.1016/S0891-4222(01)00077-4 [DOI] [PubMed] [Google Scholar]
- Hogg J., Reeves D., Roberts J., & Mudford O. C. (2001). Consistency, context and confidence in judgements of affective communication in adults with profound intellectual and multiple disabilities. Journal of Intellectual Disability Research, 45, 18–29. 10.1111/j.1365-2788.2001.00289.x [DOI] [PubMed] [Google Scholar]
- Hulland S., & Sigal M. J. (2000). Hospital-based dental care for persons with disabilities: A study of patient selection criteria. Special Care in Dentistry, 20, 131–138. 10.1111/j.1754-4505.2000.tb01149.x [DOI] [PubMed] [Google Scholar]
- Kaplan H., Clopton M., Kaplan M., Messbauer L., & McPherson K. (2006). Snoezelen multi-sensory environments: Task engagement and generalization. Research in Developmental Disabilities, 27, 443–455. 10.1016/j.ridd.2005.05.007 [DOI] [PubMed] [Google Scholar]
- *Koller D., McPherson A. C., Lockwood I., Blain-Moraes S., & Nolan J. (2018). The impact of Snoezelen in pediatric complex continuing care: A pilot study. Journal of Pediatric Rehabilitation Medicine, 11, 31–41. 10.3233/PRM-150373 [DOI] [PubMed] [Google Scholar]
- Lancioni G. E., Cuvo A. J., & O’Reilly M. F. (2002). Snoezelen: An overview of research with people with developmental disabilities and dementia. Disability and Rehabilitation, 24, 175–184. 10.1080/09638280110074911 [DOI] [PubMed] [Google Scholar]
- *Lindsay W., Black E., & Broxholme S. (2001). Effects of four therapy procedures on communication in people with profound intellectual disabilities. Journal of Applied Research in Intellectual Disabilities, 14, 110–119. 10.1046/j.1468-3148.2001.00059.x [DOI] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., & Altman D. G.; PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6, e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan J. P., Minihan P. M., Stark P. C., Finkelman M. D., Yantsides K. E., Park A., . . . Must A. (2012). The oral health status of 4,732 adults with intellectual and developmental disabilities. Journal of the American Dental Association, 143, 838–846. 10.14219/jada.archive.2012.0288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health. (2010). Intellectual and developmental disabilities. Bethesda, MD: Author. Retrieved from https://report.nih.gov/nihfactsheets/Pdfs/IntellectualandDevelopmentalDisabilities(NICHD).pdf
- Pascolo P., Peri F., Montico M., Funaro M., Parrino R., Vanadia F., . . . Cozzi G. (2018). Needle-related pain and distress management during needle-related procedures in children with and without intellectual disability. European Journal of Pediatrics, 177, 1753–1760. 10.1007/s00431-018-3237-4 [DOI] [PubMed] [Google Scholar]
- Petry K., & Maes B. (2006). Identifying expressions of pleasure and displeasure by persons with profound and multiple disabilities. Journal of Intellectual and Developmental Disability, 31, 28–38. 10.1080/13668250500488678 [DOI] [PubMed] [Google Scholar]
- *Potter C., Wetzel J., & Learman K. (2018). Effect of sensory adaptations for routine dental care in individuals with intellectual and developmental disabilities: A preliminary study. Journal of Intellectual and Developmental Disability, 44, 305–314. 10.3109/13668250.2017.1409597 [DOI] [Google Scholar]
- Poza J., Gómez C., Gutiérrez M. T., Mendoza N., & Hornero R. (2013). Effects of a multi-sensory environment on brain-injured patients: Assessment of spectral patterns. Medical Engineering and Physics, 35, 365–375. 10.1016/j.medengphy.2012.06.001 [DOI] [PubMed] [Google Scholar]
- Reynolds S., Lane S., & Mullen B. (2015). Effects of deep pressure stimulation on physiological arousal. American Journal of Occupational Therapy, 69, 6903350010 10.5014/ajot.2015.015560 [DOI] [PubMed] [Google Scholar]
- Schofield P., & Davis B. (2000). Sensory stimulation (snoezelen) versus relaxation: a potential strategy for the management of chronic pain. Disability and Rehabilitation, 22, 675–682. 10.1080/096382800445470 [DOI] [PubMed] [Google Scholar]
- *Shapiro M., Melmed R. N., Sgan-Cohen H. D., & Parush S. (2009). Effect of sensory adaptation on anxiety of children with developmental disabilities: A new approach. Pediatric Dentistry, 31, 222–228. [PubMed] [Google Scholar]
- *Shapiro M., Sgan-Cohen H. D., Parush S., & Melmed R. N. (2009). Influence of adapted environment on the anxiety of medically treated children with developmental disability. Journal of Pediatrics, 154, 546–550. 10.1016/j.jpeds.2008.10.017 [DOI] [PubMed] [Google Scholar]
- *Singh N. N., Lancioni G. E., Winton A. S., Molina E. J., Sage M., Brown S., & Groeneweg J. (2004). Effects of Snoezelen room, activities of daily living skills training, and vocational skills training on aggression and self-injury by adults with mental retardation and mental illness. Research in Developmental Disabilities, 25, 285–293. 10.1016/j.ridd.2003.08.003 [DOI] [PubMed] [Google Scholar]
- Tavassoli T., Miller L. J., Schoen S. A., Nielsen D. M., & Baron-Cohen S. (2014). Sensory over-responsivity in adults with autism spectrum conditions. Autism, 18, 428–432. 10.1177/1362361313477246 [DOI] [PubMed] [Google Scholar]
- *Thompson C. (2011). Multi-sensory intervention observational research. International Journal of Special Education, 26, 202–214. [Google Scholar]
- *Tunson J., & Candler C. (2010). Behavioral states of children with severe disabilities in the multisensory environment. Physical and Occupational Therapy in Pediatrics, 30, 101–110. 10.3109/01942630903546651 [DOI] [PubMed] [Google Scholar]
- Tyler C., Zyzanski S., Panaite V., & Council L. (2010). Nursing perspectives on cancer screening in adults with intellectual and other developmental disabilities. Intellectual and Developmental Disabilities, 48, 271–277. 10.1352/1934-9556-48.4.271 [DOI] [PubMed] [Google Scholar]
- Virués-Ortega J., Pritchard K., Grant R. L., North S., Hurtado-Parrado C., Lee M. S., . . . Yu C. T. (2014). Clinical decision making and preference assessment for individuals with intellectual and developmental disabilities. American Journal on Intellectual and Developmental Disabilities, 119, 151–170. 10.1352/1944-7558-119.2.151 [DOI] [PubMed] [Google Scholar]
- *Vlaskamp C., de Geeter K., Huijsmans L., & Smit I. (2003). Passive activities: The effectiveness of multisensory environments on the level of activity of individuals with profound multiple disabilities. Journal of Applied Research in Intellectual Disabilities, 16, 135–143. 10.1046/j.1468-3148.2003.00156.x [DOI] [Google Scholar]
- Ward R. L., Nichols A. D., & Freedman R. I. (2010). Uncovering health care inequalities among adults with intellectual and developmental disabilities. Health and Social Work, 35, 280–290. 10.1093/hsw/35.4.280 [DOI] [PubMed] [Google Scholar]