Abstract
Importance: Despite advancements in stroke rehabilitation research, occupational therapy practitioners still face challenges with implementing research into routine practice. Although the development of evidence-based practices (EBPs) is one critical step along the knowledge translation continuum for the population of people with stroke, research is also needed to identify the most effective strategies for implementing EBPs with stroke survivors who are receiving occupational therapy services.
Objective: To synthesize research related to occupational therapy practitioners’ implementation of EBPs in adult stroke rehabilitation.
Data Sources: We searched four electronic databases—CINAHL, MEDLINE, PubMed, and Academic Search Complete—and the peer-reviewed journal Implementation Science to identify relevant research studies.
Study Selection and Data Collection: Studies that met the following inclusion criteria were included in the scoping review: published between January 2003 and January 2018, addressed the adult stroke population, and examined the implementation of occupational therapy interventions. Data were abstracted on the basis of recommendations from the seminal review framework established by Arksey and O’Malley (2005). Thematic analysis identified themes that emerged from the included studies.
Findings: Twenty-five articles satisfied our inclusion parameters. Our analyses yielded three overarching themes: barriers to implementation, facilitators of implementation, and implementation strategies. Implementation strategies often consisted of multimodal knowledge translation training programs.
Conclusion and Relevance: Although the stroke rehabilitation literature appears to have established the barriers to and facilitators of EBP implementation, greater attention to the identification of effective implementation strategies that promote the uptake of EBPs by occupational therapy practitioners is needed.
What This Article Adds: This article summarizes the contextual factors and effective strategies that may influence practitioners’ implementation of stroke research findings in real-world practice.
Stroke remains a leading cause of disability among adults in the United States (Benjamin et al., 2017), with impairments ranging from minor changes in sensation to devastating motor deficits. Despite advancements in stroke rehabilitation research, translation of research into practice remains an ongoing challenge for rehabilitation professionals, including occupational therapy practitioners (Bayley et al., 2012; Wressle & Samuelsson, 2014). Occupational therapy practitioners are often tasked with implementing evidence-based interventions that address a multitude of functional, postural, behavioral, cognitive, and motor impairments (American Occupational Therapy Association [AOTA], 2014). High-quality evidence supports a variety of interventions to improve upper limb function after stroke, including constraint-induced movement therapy (Corbetta et al., 2010; Wolf et al., 2006), mirror therapy (Thieme et al., 2013), and mental practice (Braun et al., 2013; Wang et al., 2011). Evidence-based stroke interventions should be incorporated into routine occupational therapy practice to decrease the effects of disability on and increase the quality of life of stroke survivors.
Implementation science scholars have continually acknowledged the 17-yr time lag between scientific health care discoveries and the adoption of only 14% of those discoveries into clinical practice (Balas & Boren, 2000; Green et al., 2009; Morris et al., 2011). Occupational therapy practitioners in stroke rehabilitation are not immune to this time lag, and purposeful efforts are needed to identify effective strategies to implement research into practice (Juckett et al., 2019). This article presents a scoping review designed to examine the determinants and strategies related to implementation of evidence-based stroke interventions in occupational therapy, and it provides recommendations for expediting implementation of scientific discoveries into clinical stroke rehabilitation.
Method
Our scoping review methodology was guided by the framework initially presented by Arksey and O’Malley (2005) and further expanded on by Levac et al. (2010). The decision to use a scoping review methodology was based on two key research objectives: (1) Summarize research related to occupational therapy practitioners’ implementation of evidence-based practices (EBPs) in adult stroke rehabilitation and (2) identify gaps in the literature pertaining to the implementation of EBPs in stroke rehabilitation. We structured our protocol using five steps: identifying research questions, identifying studies, selecting studies, extracting data, and summarizing the results (Arksey & O’Malley, 2005).
Step 1: Identifying Research Questions
Our overarching research question was as follows: To what extent are occupational therapy researchers implementing EBPs in stroke rehabilitation? We anticipated locating studies that addressed two content areas: (1) determinants that have promoted or impeded occupational therapy practitioners’ implementation of EBPs in stroke rehabilitation and (2) strategies that have been examined to encourage occupational therapy practitioners’ implementation of EBPs in stroke rehabilitation.
Step 2: Identifying Studies
To perform a comprehensive search of the available literature, we accessed the electronic databases CINAHL, MEDLINE, PubMed, and Academic Search Complete and the journal Implementation Science, a peer-reviewed journal committed to publishing implementation research studies that address an array of health care issues. We consulted with stroke rehabilitation and implementation science scholars to determine which key terms to use in our database and journal searches (Table 1). Articles were entered into the web-based scoping–systematic review program Covidence (Veritas Health Innovation, Melbourne, Victoria, Australia), before undergoing title and abstract review.
Table 1.
Summary of the Search Strategy
| Database and Peer-Reviewed Journal | Key Terminology |
| CINAHL | Occupational therapy |
| MEDLINE | Stroke |
| PubMed | Cerebrovascular accident |
| Academic Search Complete | Implementation |
| Implementation Science | Knowledge translation |
| Intervention | |
| Evidence-based practice | |
| Dissemination | |
| Research utilization |
Step 3: Selecting Studies
We applied our inclusion and exclusion criteria to all identified titles and abstracts to determine which articles should be advanced to the full-text review phase. Studies that explored the actual implementation of stroke EBPs were included. We narrowed our search further by applying the following inclusion criteria to all abstracts and articles:
Published in English
Published between January 2003 and January 2018
Addressed the adult stroke population (age 18 yr and older)
Primarily addressed occupational therapy interventions.
We chose to exclude review articles such as meta-analyses, systematic reviews, and integrative and narrative reviews. We also chose to exclude articles that focused solely on physical therapy practitioners, addressed implementation of assessments, examined implementation of caregiver training, or presented study protocols without actual results.
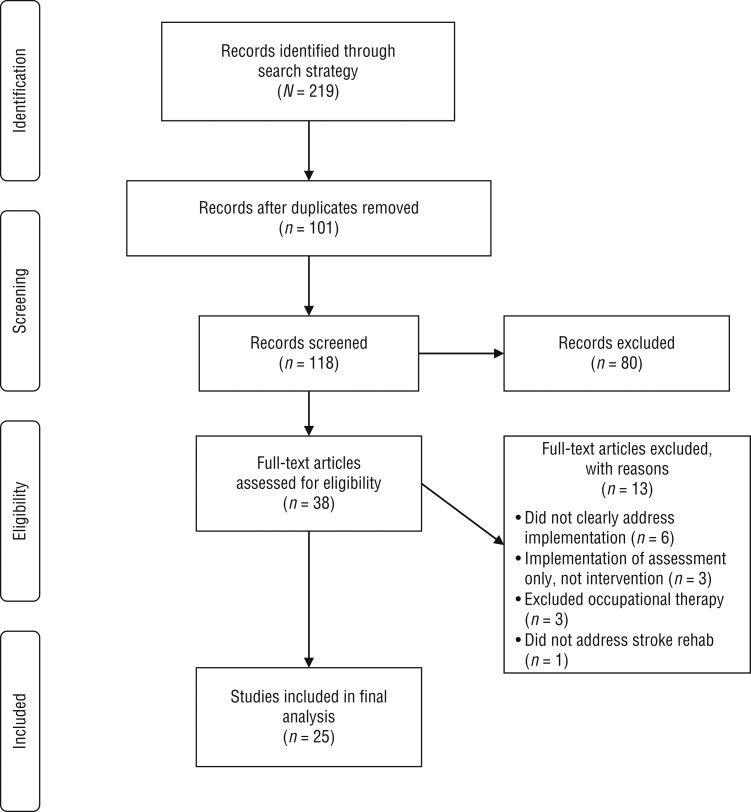
Two reviewers (LAJ and LRW) selected relevant articles, on the basis of the inclusion and exclusion criteria, to be included in the final review. The authors discussed conflicts and consulted with a third and fourth reviewer (JF and CEG) to achieve consensus on article inclusion. Of the original 118 references, 38 articles were obtained for full-text review, and 25 were ultimately included in the scoping review (Figure 1).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram of study selection process.
Note. Figure format from “Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement,” by D. Moher, A. Liberati, J. Tetzlaff, and D. G. Altman; PRISMA Group, 2009, PLoS Medicine, 6(6), e1000097. https://doi.org/10.1371/journal.pmed.1000097
Step 4: Data Extraction
After adapting Arksey and O’Malley’s (2005) data charting form (Table 2, at the end of this article), we abstracted pertinent information from each article using a descriptive–analytic method. We chose to use this method to provide readers with a broad understanding of each article, how implementation was examined, and the type of stroke intervention being implemented. As is inherent with scoping review methodologies, the data charting form was revised as needed throughout the data abstraction process to present the information in a cohesive and concise manner.
Table 2.
Characteristics of Articles Examining Occupational and Physical Therapy Practitioners’ Implementation of Stroke Rehabilitation EBPs
| Author/Year | Type of EBP | Implementation Approach | Methodology | Findings |
| Bayley et al. (2012) | Evidence-based recommendations for arm and leg rehabilitation after stroke | Local facilitators; workshop; consultation with KT experts; implementation toolkit | Qualitative; focus groups with practitioners | Barriers to implementation: decreased resources (staff, time, equipment, training); decreased communication among leadership |
| Connell, McMahon, Harris, et al. (2014) | GRASP designed to support higher exercise intensity in inpatient settings | N/A | Qualitative; interviews with practitioners |
|
| Connell, McMahon, Watkins, et al. (2014) | GRASP | N/A | Descriptive; cross-sectional survey | Facilitator of implementation of perceived value of GRASP |
| Doyle & Bennett (2014) | ULPSSI management | Workshop drawn from Adult Learning Theory and Theory of Planned Behavior | Single group pretest–posttest design | Implementation strategies: Workshop led to improved knowledge of, attitude toward, and confidence in capabilities with ULPSSI; also led to higher intended behaviors regarding ULPSSI |
| Gustafsson & McKenna (2003) | Practice related to support devices, PROM, Bobath techniques, and static positional stretches | N/A | Descriptive; cross-sectional survey | Barriers to implementation: inconsistent adherence to best practice recommendations; cost of recommendations |
| Korner-Bitensky et al. (2007) | Best practice utilization behaviors in rehabilitation | N/A | Descriptive; cross-sectional survey | Barriers to implementation: lack of resources (time and staff); lack of perceived value of EBP |
| Korner-Bitensky et al. (2008) | StrokEngine | N/A | Descriptive; cross-sectional | Facilitators of implementation: availability of resources (online) |
| Kristensen & Hounsgaard (2014) | General EBP for stroke rehab | Audit and feedback | Descriptive; chart audits | Implementation intervention: audits and feedback positively influenced use of EBPs |
| Kristensen et al. (2016) | General EBP for stroke rehab | N/A | Qualitative; field observations, interviews, focus groups |
|
| Levac et al. (2016a) | VR in stroke rehabilitation | Multimodal KT intervention including computer-based learning, hands-on learning sessions, experiential learning, email reminders; mentorship | Single group pretest–posttest design |
|
| Levac et al. (2016b) | Motor learning approach within VR | Multimodal KT intervention including self-paced e-learning, hands-on learning sessions, VR sessions with stroke survivors, didactic reminders | Single group pretest–posttest design | Implementation intervention: Multimodal KT intervention led to increased knowledge regarding motor learning and VR |
| Masterson-Algar et al. (2014) | A complex ADL intervention | N/A | Qualitative; semistructured interviews | Facilitators of implementation: building relationships among staff led to improved adherence to the intervention; being able to modify the physical environment also led to improved adherence |
| McCann et al. (2009) | Stroke performance indicators | Establishment of a stroke-specific hospital unit | Single group pretest–posttest design | Implementation intervention: Establishing a designated stroke unit led to increased compliance with performance indicators and enhanced stroke survivor outcomes |
| McCluskey et al. (2015) | Outdoor therapy sessions | Audit and feedback | Observational | Barriers to implementation: decreased adherence to conducting therapy sessions in the outdoor environment |
| McCluskey et al. (2016) | Outdoor mobility clinical guideline |
|
Experimental; cluster RCT | Implementation intervention: The multimodal KT intervention did not change community teams’ behavior in delivering outdoor mobility sessions with stroke survivors |
| McCluskey et al. (2013) | Multiple stroke guidelines | N/A | Qualitative; semistructured focus groups (6) and individual interviews (2) |
|
| McEwen et al. (2005) | General stroke EBP utilization | The Rehabilitation Education Program for Stroke was administered; it combined a self-directed online learning module with support from peer mentors, technical skill workshops, and organizational supports | Single group; pretest–posttest design | Implementation intervention: Multimodal KT intervention positively influenced the use of stroke rehabilitation practices |
| Munce et al. (2017) | Stroke clinical guidelines | N/A | Qualitative; semistructured focus groups |
|
| Petzold et al. (2012) | Poststroke USN | 7-hr in-person interactive workshop; 8-wk reinforcement period | Single group pretest–posttest design | Implementation intervention: A multimodal KT intervention can improve practitioners’ knowledge of how to manage poststroke USN |
| Petzold et al. (2014) | USN treatment | N/A | Qualitative; focus groups |
|
| Read & Levy (2006) | Stroke care pathways | Stroke care pathway implementation | Single group pretest–posttest design | Implementation intervention: Establishing stroke care pathways appears to improve the process of stroke care |
| Russell et al. (2018) | Cross-education, the practice of improving an untrained muscle through training of the same muscle on the opposite side of the body | N/A | Qualitative; focus groups | Facilitators of implementation: perceived value of intervention |
| Salbach et al. (2017) | 18 stroke rehab guidelines |
|
Experimental, cluster RCT | Implementation intervention: Of the 18 guidelines, the implementation of only 2 guidelines improved in the intervention group; in the control group, the implementation of 1 guideline improved |
| Schmid et al. (2008) | Stroke rehabilitation guidelines | N/A | Descriptive; cross-sectional survey | Barriers to implementation: lack of knowledge and skills regarding stroke guidelines |
| Scobbie et al. (2013) | Goal setting and action planning framework | N/A | Qualitative; interviews |
|
Note. ADL = activities of daily living; EBP = evidence-based practice; GRASP = Graded Repetitive Arm Supplementary Program; KT = knowledge translation; LOS = length of stay; N/A = not applicable; PROM = passive range of motion; RCT = randomized controlled trial; ULPSSI = upper limb poststroke sensory impairment; USN = unilateral spatial neglect; VR = virtual reality.
Step 5: Summarizing the Results
We established two processes to summarize our results: a descriptive numerical summary and a thematic analysis (Arksey & O’Malley, 2005; Levac et al., 2010). Our descriptive numerical summary highlighted details on the type and frequency of studies included, the EBPs being implemented, and the location where the study was conducted. We then used a thematic analysis approach to identify themes related to the implementation of stroke EBPs among practitioners. To guide our thematic analysis, we mapped our findings to the Consolidated Framework of Implementation Research (CFIR; Damschroder et al., 2009). Refer to Table 3 for a summary of the CFIR’s five domains and their respective constructs.
Table 3.
Constructs From the Consolidated Framework for Implementation Research
| Construct | Subconstructs |
| Intervention characteristics | Intervention source; evidence quality and strength; relative advantage; adaptability; trialability; complexity; design quality and packaging; cost |
| Outer setting | Patient needs and resources; cosmopolitanism; peer pressure; external policy and incentives |
| Inner setting | Structural characteristics; networks and communication; culture; implementation climate; tension for change; compatibility; relative priority; organizational incentives and rewards; goals and feedback; learning climate; readiness for implementation; leadership engagement; available resources; access to knowledge and information |
| Individual characteristics | Knowledge and beliefs; self-efficacy; individual stage of change; individual identification with organization; other personal attribute (e.g., values, motivation) |
| Implementation process | Planning; engaging; opinion leaders; formally appointed internal implementation leaders; champions; external change agents; executing; reflecting and evaluating |
Note. From “Fostering Implementation of Health Services Research Findings Into Practice: A Consolidated Framework for Advancing Implementation Science,” by L. J. Damschroder, D. C. Aron, R. E. Keith, S. R. Kirsh, J. A. Alexander, and J. C. Lowery, 2009. Implementation Science, 4, 50. Adapted from the original under the terms of the Creative Commons Attribution 2.0 Generic License (https://creativecommons.org/licenses/by/2.0). Retrieved from https://implementationscience.biomedcentral.com/articles/10.1186/1748-5908-4-50#rightslink
Results
Our review process yielded a total of 25 articles that aligned with our inclusion criteria. The majority of included articles used qualitative research methods (n = 9) to examine determinants that influenced occupational therapy practitioners’ implementation of EBPs in stroke rehabilitation. The remaining articles used quasi-experimental or pretest–posttest designs (n = 7), cross-sectional surveys (n = 5), cluster randomized controlled trials (RCTs; n = 2), or observational research designs (n = 2). Because of the large number of articles that assessed determinants that influence EBP implementation, we established two separate categories: barriers to effective implementation and facilitators of effective implementation. Because our scoping review was informed by the implementation science literature, we further classified our findings according to CFIR constructs: intervention characteristics, outer setting, inner setting, individual characteristics, and implementation process (Damschroder et al., 2009; see Table 3). Articles that examined actual strategies designed to increase the uptake of evidence into practice were compiled into their own category—implementation strategies.
Barriers to Effective Implementation
Intervention Characteristics.
Perhaps the most common barrier to effective EBP implementation was the high prevalence of inconsistent adherence to delivering the EBPs (e.g., interventions) as intended. This low rate of adherence, or fidelity, was identified through qualitative, observational, and cross-sectional survey data presented in several articles included in our review (Connell, McMahon, Harris, et al., 2014; Gustafsson & McKenna, 2003; Korner-Bitensky et al., 2007; Kristensen et al., 2016; Levac et al., 2016b; McCluskey et al., 2015; Scobbie et al., 2013). Related to this, the complexity of interventions served as an obstacle to their actual use in the rehabilitation setting, and interventions deemed inapplicable (Scobbie et al., 2013) or unadaptable (Kristensen et al., 2012; Levac et al., 2016b) were less likely to be implemented in clinical practice.
Inner Setting.
Several resource limitations impeded the extent to which occupational therapy practitioners implemented evidence in practice. Specifically, a lack of staff and EBP experts, increased costs associated with select EBPs, time constraints, logistical challenges, and inadequate equipment all had a negative impact on practitioners’ perceived ability to routinely implement EBPs (Bayley et al., 2012; Levac et al., 2016b; McCluskey et al., 2013; Petzold et al., 2014; Scobbie et al., 2013). Decreased interdisciplinary communication and inconsistent leadership engagement were also found to limit EBP adoption (Bayley et al., 2012; Munce et al., 2017).
Individual Characteristics.
A variety of extrapersonal factors influenced stroke rehabilitation practitioners’ ability to consistently implement quality EBPs. These factors included lack of knowledge that select interventions existed, decreased confidence in using new interventions, and difficulty forming new habits using novel interventions (Munce et al., 2017; Petzold et al., 2014; Schmid et al., 2008; Scobbie et al., 2013). Moreover, practitioners who did not have a favorable view of a particular EBP were less likely to implement that EBP in clinical practice, despite strong evidence supporting the benefits of the intervention (Munce et al., 2017).
Facilitators of Effective Implementation
Many of the same CFIR constructs identified as barriers to EBP implementation were also identified as facilitators of EBP implementation.
Inner Setting.
The availability of supporting resources played an integral role in enhancing the use of EBPs in stroke rehabilitation. Such resources included EBP experts (otherwise known as EBP champions), online support guides, and electronic education modules (Connell, McMahon, Harris, et al., 2014; Korner-Bitensky et al., 2007). In addition, relationship building among therapy stakeholders, clear support from management, and ongoing communication from organizational leadership all encouraged the use of EBPs, resulting in more consistent EBP implementation and more favorable opinions toward routinely adopting EBPs (Kristensen et al., 2012; Masterson‐Algar et al., 2014; Munce et al., 2017; Petzold et al., 2014).
Individual Characteristics.
The extent to which occupational therapy practitioners found value in a particular evidence-based intervention was the most common predictor of implementation (Connell, McMahon, Harris, et al., 2014; Connell, McMahon, Watkins, et al., 2014; Kristensen et al., 2012; Munce et al., 2017; Russell et al., 2018; Scobbie et al., 2013). Enthusiasm and support for a particular EBP promoted its adoption in the stroke rehabilitation setting. In addition, similar to how the lack of knowledge of current EBP recommendations impeded implementation, a strong working knowledge of available evidence-based interventions, along with their clinical application, enhanced EBP implementation (Munce et al., 2017; Petzold et al., 2014).
Outer Setting.
Although they identified no barriers in the outer setting construct of the CFIR, Levac et al. (2016b) found that patient preference had an impact on how often an evidence-based intervention was implemented. Occupational therapy practitioners were more likely to implement an evidence-based virtual reality intervention with patients who had previously demonstrated strong engagement and interest in the intervention.
Implementation Strategies
Although our scoping review identified several factors that influenced occupational therapy practitioners’ use of EBPs with the stroke population, we also sought to determine what implementation strategies, otherwise known as implementation interventions, have been used to promote the uptake of EBPs in clinical practice. Of the 25 articles, 10 (40%) examined one or more implementation strategies to increase EBP adoption. Multimodal knowledge translation strategies were those most often used and consisted of techniques such as in-person workshops, online modules, expert or mentor consultation, educational materials, and email reminders related to the targeted EBPs (Levac et al., 2016a, 2016b; McCluskey et al., 2016; McEwen et al., 2005; Petzold et al., 2012; Salbach et al., 2017). Multimodal knowledge translation strategies were found to increase practitioners’ knowledge and confidence in using stroke-related EBPs (Doyle & Bennett, 2014; Levac et al., 2016a, 2016b; Petzold et al., 2014), but they did not, with the exception of McEwen et al.’s (2005) knowledge translation program, consistently enhance the adoption of EBPs in the practice setting (McCluskey et al., 2016; Salbach et al., 2017). Audit and feedback strategies (Kristensen & Hounsgaard, 2014; McCann et al., 2009) and organizational initiatives designed to increase practice guideline adoption (McCann et al., 2009; Read & Levy, 2006) were successful techniques that had a positive impact on the integration of EBPs.
Discussion
The objective of this scoping review was to synthesize research related to occupational therapy practitioners’ implementation of EBPs in adult stroke rehabilitation. On the basis of our review, we were able to identify barriers to EBP use, facilitators of EBP use, and implementation strategies specifically intended to increase the adoption of EBPs with the population of people with stroke. By drawing from the implementation science literature, we mapped key barriers to and facilitators of EBP implementation to overarching constructs from the CFIR, a frequently referenced framework in implementation research.
We identified barriers to EBPs in stroke rehabilitation in three of the five CFIR constructs: intervention characteristics, inner setting, and individual characteristics. Common barriers that emerged throughout the scoping review process included the lack of resources to implement EBPs, lack of knowledge or awareness of EBPs, and varying adherence to EBP recommendations (i.e., lack of fidelity when administering evidence-based interventions in clinical practice). These barriers are consistent with the barriers to EBP implementation identified in existing allied health literature (Juckett & Robinson, 2018; Wressle & Samuelsson, 2014). Acknowledging barriers to EBP implementation is an important first step toward identifying effective strategies to enhance the uptake of research into practice.
Our coding and thematic analyses also found several facilitators of EBP use, all of which were mapped to the following three CFIR constructs: inner setting, individual characteristics, and outer setting. Of all facilitators identified, occupational therapy practitioners’ perceptions of the value of EBPs appeared to be the most consistent predictor of EBP implementation in clinical practice. This finding speaks to the importance of continuously incorporating research education into professional development from the student level all the way to the experienced occupational therapy practitioner level. Prior evidence has confirmed the notion that professionals with a positive opinion of EBPs are more likely to seek out and use EBPs with patients. Specifically, Jordan et al. (2016) found that recent nursing graduates (younger than age 40 yr) were more familiar with EBPs and, therefore, may be more likely to implement EBPs in practice. This finding may suggest the value of the EBP paradigm shift in academic programs because more recent graduates are more likely to receive training in EBPs in their curricula. Conversely, among occupational therapy practitioners, positive views of or recent exposure to EBPs has not necessarily led to greater implementation of EBPs with patients (Upton et al., 2014), although this is an area of study that requires further investigation.
Although our findings support common factors influencing implementation of EBPs with stroke survivors, recognition of these barriers and facilitators is merely one element of enhancing the adoption of EBPs. Greater emphasis on identifying effective strategies for increasing EBP implementation is imperative. Our scoping review commonly identified multimodal knowledge translation strategies that have been explored in research studies, yet the effectiveness of these specific strategies remains unclear, limiting their applicability to clinical practice. Notably, however, multimodal approaches have been found to be more effective than singular implementation strategies alone (i.e., one training session; Kirschner et al., 2017). Moreover, although we identified several studies that leveraged multimodal strategies to enhance EBP implementation (Doyle & Bennett, 2014; Levac et al., 2016a, 2016b; Petzold et al., 2014), applying these strategies in occupational therapy practice would be difficult because these authors did not provide adequate detail for replication. Implementation science scholars have encouraged clear descriptions of implementation strategies to enhance their replicability (Bunger et al., 2017; Proctor et al., 2013). Future research on the implementation of valid and reliable assessments (Lynch et al., 2016) for stroke survivors is also warranted because assessments inform the selection of appropriate EBPs.
Limitations
Although our findings make a valuable contribution to the implementation and knowledge translation research in occupational therapy, our study is not without limitations. As is standard with scoping reviews (Colquhoun et al., 2010), our methodology did not include a quality assessment of each included article, such as those conducted in systematic reviews. Our review methods were structured to include all study types, ranging from qualitative studies to RCTs, to examine the extent to which the implementation of stroke EBPs were included in the occupational therapy literature. Without quality assessments, our findings are not as generalizable to the occupational therapy profession but still provide insight that can guide future implementation research in stroke rehabilitation.
Practitioner perceptions examined in the included articles most often reflected the views of occupational therapists, not occupational therapy assistants. Although both groups of professionals work collaboratively, the EBP-related needs of occupational therapists may differ from the needs of occupational therapy assistants and warrant further research. Last, because implementation-related research is still an emerging area in occupational therapy, the articles we included did not investigate EBP implementation by occupational therapy practitioners exclusively. With these articles, we were unable to extract data that represented only occupational therapy practitioners; thus, our results may be less representative of the occupational therapy profession.
Implications for Occupational Therapy Practice
To make our findings most useful to occupational therapy, we have highlighted four key strategies that practitioners, supervisors, and administrators may consider embedding in their respective stroke rehabilitation settings:
Assess practitioners’ adherence to EBPs in the clinical setting. Practitioners’ ability to adhere to EBPs, as they are prescribed or intended, can vary on the basis of the availability of supportive resources, interest in or comfort with using EBPs in practice, and familiarity with the core components of EBPs. Identifying barriers to EBP adherence can be the first step in determining how to increase effective EBP use.
Consider assessing the value practitioners place on evidence-based interventions that are either currently used in practice or intended to become integrated into practice. Our review findings indicated that the greater value practitioners placed on research, the more likely they were to implement EBPs with their patients.
When planning to adopt one or more EBPs, consider using a multimodal knowledge translation program or combination of implementation strategies. For instance, instead of a 1-hr in-service on the use of functional electrical stimulation, structure the in-service to also include educational materials, electronic resources, and follow-up consultations to help practitioners solidify their understanding of how to apply the EBP in a real clinic scenario.
Use the EBP tools and resources available to AOTA members. Practitioners can access the Evidence-Based Practice & Research section of the AOTA website (https://www.aota.org/Practice/Researchers) and find practice-specific EBP resources, Critically Appraised Papers, a journal club toolkit, and a database of EBP resources. In addition, AOTA Occupational Therapy Practice Guidelines are available for purchase, including guidelines for adult stroke rehabilitation (Wolf & Nilsen, 2015). These resources are specifically geared toward occupational therapy practitioners and may assist in maximizing implementation of EBPs.
Conclusion
Implementation of research into practice is a complex process influenced by an array of individual and contextual determinants. Although recognition of these factors is important, the occupational therapy profession needs to expand on its examination of actual implementation strategies that have been shown to increase the adoption of EBPs with the stroke population. As stroke rehabilitation research becomes more robust, we encourage researchers to investigate implementation strategies to better facilitate translation into clinical practice. Collaborating with implementation scientists may help guide researchers toward an understanding of how to structure methodologies when designing implementation studies and when measuring implementation outcomes. Key implementation outcomes include acceptability, adoption, appropriateness, costs, feasibility, fidelity, penetration, and sustainability (Proctor et al., 2011). These outcomes can be assessed when examining the effectiveness of implementation strategies used to increase the uptake of EBPs with patients. Extensive examples of implementation strategies, also referred to as implementation interventions, can be found in Powell et al. (2012).
Although stroke mortality rates have decreased over the past 2 decades, the incidence of stroke-related disability continues to increase worldwide (Feigin et al., 2014). This trend demands that we establish effective, tangible solutions for narrowing the 17-yr research-to-practice gap. Although impressive advancements have been made in stroke rehabilitation research, it is essential that practitioners take these advancements to the next level by consistently integrating them into practice with stroke survivors. As practitioners continue to adhere to AOTA’s Vision 2025 of being a science-driven, evidence-based profession (AOTA, 2017), they must identify effective strategies for implementing evidence-based stroke rehabilitation practices to maximize performance levels of the stroke survivors they serve.
Footnotes
Indicates articles included in the scoping review.
References
- American Occupational Therapy Association. (2017). Vision 2025. American Journal of Occupational Therapy, 71, 7103420010 10.5014/ajot.2017.713002 [DOI] [PubMed] [Google Scholar]
- American Occupational Therapy Association. (2014). Occupational therapy practice framework: Domain and process (3rd ed.). American Journal of Occupational Therapy, 68(Suppl. 1), S1–S48. 10.5014/ajot.2014.682006 [DOI] [PubMed] [Google Scholar]
- Arksey H., & O’Malley L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8, 19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Balas E. A., & Boren S. A. (2000). Managing clinical knowledge for health care improvement. Yearbook of Medical Informatics, 2000, 65–70. [PubMed] [Google Scholar]
- *Bayley M. T., Hurdowar A., Richards C. L., Korner-Bitensky N., Wood-Dauphinee S., Eng J. J., . . . Graham I. D. (2012). Barriers to implementation of stroke rehabilitation evidence: Findings from a multi-site pilot project. Disability and Rehabilitation, 34, 1633–1638. 10.3109/09638288.2012.656790 [DOI] [PubMed] [Google Scholar]
- Benjamin E. J., Blaha M. J., Chiuve S. E., Cushman M., Das S. R., Deo R., . . . Muntner P.; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. (2017). Heart disease and stroke statistics—2017 update: A report from the American Heart Association. Circulation, 135, e146–e603. 10.1161/CIR.0000000000000485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun S., Kleynen M., van Heel T., Kruithof N., Wade D., & Beurskens A. (2013). The effects of mental practice in neurological rehabilitation: A systematic review and meta-analysis. Frontiers in Human Neuroscience, 7, 390 10.3389/fnhum.2013.00390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunger A. C., Powell B. J., Robertson H. A., MacDowell H., Birken S. A., & Shea C. (2017). Tracking implementation strategies: A description of a practical approach and early findings. Health Research Policy and Systems, 15, 15 10.1186/s12961-017-0175-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colquhoun H. L., Letts L. J., Law M. C., MacDermid J. C., & Missiuna C. A. (2010). A scoping review of the use of theory in studies of knowledge translation. Canadian Journal of Occupational Therapy, 77, 270–279. 10.2182/cjot.2010.77.5.3 [DOI] [PubMed] [Google Scholar]
- *Connell L. A., McMahon N. E., Harris J. E., Watkins C. L., & Eng J. J. (2014). A formative evaluation of the implementation of an upper limb stroke rehabilitation intervention in clinical practice: A qualitative interview study. Implementation Science, 9, 90 10.1186/s13012-014-0090-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Connell L. A., McMahon N. E., Watkins C. L., & Eng J. J. (2014). Therapists’ use of the Graded Repetitive Arm Supplementary Program (GRASP) intervention: A practice implementation survey study. Physical Therapy, 94, 632–643. 10.2522/ptj.20130240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbetta D., Sirtori V., Moja L., & Gatti R. (2010). Constraint-induced movement therapy in stroke patients: Systematic review and meta-analysis. European Journal of Physical and Rehabilitation Medicine, 46, 537–544. [PubMed] [Google Scholar]
- Damschroder L. J., Aron D. C., Keith R. E., Kirsh S. R., Alexander J. A., & Lowery J. C. (2009). Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science, 4, 50 10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Doyle S. D., & Bennett S. (2014). Feasibility and effect of a professional education workshop for occupational therapists’ management of upper-limb poststroke sensory impairment. American Journal of Occupational Therapy, 68, e74–e83. 10.5014/ajot.2014.009019 [DOI] [PubMed] [Google Scholar]
- Feigin V. L., Forouzanfar M. H., Krishnamurthi R., Mensah G. A., Connor M., Bennett D. A., . . . Murray C.; Global Burden of Diseases, Injuries, and Risk Factors Study 2010 and the GBD Stroke Experts Group. (2014). Global and regional burden of stroke during 1990-2010: Findings from the Global Burden of Disease Study 2010. Lancet, 383, 245–255. 10.1016/S0140-6736(13)61953-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green L. W., Ottoson J. M., García C., & Hiatt R. A. (2009). Diffusion theory and knowledge dissemination, utilization, and integration in public health. Annual Review of Public Health, 30, 151–174. 10.1146/annurev.publhealth.031308.100049 [DOI] [PubMed] [Google Scholar]
- *Gustafsson L., & McKenna K. (2003). Treatment approaches for clients with a stroke‐affected upper limb: Are we following evidence‐based practice? Australian Occupational Therapy Journal, 50, 205–215. 10.1046/j.1440-1630.2003.00395.x [DOI] [Google Scholar]
- Jordan P., Bowers C., & Morton D. (2016). Barriers to implementing evidence-based practice in a private intensive care unit in the Eastern Cape. Southern African Journal of Critical Care, 32, 50–54. 10.7196/SAJCC.2016.v32i2.253 [DOI] [Google Scholar]
- Juckett L. A., & Robinson M. L. (2018). Implementing evidence-based interventions with community-dwelling older adults: A scoping review. American Journal of Occupational Therapy, 72, 7204195010 10.5014/ajot.2018.031583 [DOI] [PubMed] [Google Scholar]
- Juckett L. A., Robinson M. L., & Wengerd L. R. (2019). Narrowing the gap: An implementation science research agenda for the occupational therapy profession. American Journal of Occupational Therapy, 73, 7305347010 10.5014/ajot.2019.033902 [DOI] [PubMed] [Google Scholar]
- Kirschner J., Waltz T., Powell B., Smith J., & Proctor E. (2017). Implementation strategies. In Brownson R., Colditz G., & Proctor E. (Eds.), Dissemination and implementation research in health: Translating science to practice (2nd ed., pp. 245–265). New York: Oxford University Press. [Google Scholar]
- *Korner-Bitensky N., Menon-Nair A., Thomas A., Boutin E., & Arafah A. M. (2007). Practice style traits: Do they help explain practice behaviours of stroke rehabilitation professionals? Journal of Rehabilitation Medicine, 39, 685–692. 10.2340/16501977-0106 [DOI] [PubMed] [Google Scholar]
- *Korner-Bitensky N., Roy M. A., Teasell R., Kloda L., Storr C., Asseraf-Pasin L., & Menon A. (2008). Creation and pilot testing of StrokEngine: A stroke rehabilitation intervention website for clinicians and families. Journal of Rehabilitation Medicine, 40, 329–333. 10.2340/16501977-0177 [DOI] [PubMed] [Google Scholar]
- Kristensen H. K., Borg T., & Hounsgaard L. (2012). Aspects affecting occupational therapists’ reasoning when implementing research-based evidence in stroke rehabilitation. Scandinavian Journal of Occupational Therapy, 19, 118–131. 10.3109/11038128.2011.556197 [DOI] [PubMed] [Google Scholar]
- *Kristensen H., & Hounsgaard L. (2014). Evaluating the impact of audits and feedback as methods for implementation of evidence in stroke rehabilitation. British Journal of Occupational Therapy, 77, 251–259. 10.4276/030802214X13990455043520 [DOI] [Google Scholar]
- *Kristensen H. K., Ytterberg C., Jones D. L., & Lund H. (2016). Research-based evidence in stroke rehabilitation: An investigation of its implementation by physiotherapists and occupational therapists. Disability and Rehabilitation, 38, 2564–2574. 10.3109/09638288.2016.1138550 [DOI] [PubMed] [Google Scholar]
- Levac D., Colquhoun H., & O’Brien K. K. (2010). Scoping studies: Advancing the methodology. Implementation Science, 5, 69 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Levac D. E., Glegg S. M., Sveistrup H., Colquhoun H., Miller P., Finestone H., . . . Velikonja D. (2016a). Promoting therapists’ use of motor learning strategies within virtual reality-based stroke rehabilitation. PLoS One, 11, e0168311 10.1371/journal.pone.0168311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Levac D., Glegg S. M., Sveistrup H., Colquhoun H., Miller P. A., Finestone H., . . . Velikonja D. (2016b). A knowledge translation intervention to enhance clinical application of a virtual reality system in stroke rehabilitation. BMC Health Services Research, 16, 557 10.1186/s12913-016-1807-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch E. A., Cadilhac D. A., Luker J. A., & Hillier S. L. (2016). Education-only versus a multifaceted intervention for improving assessment of rehabilitation needs after stroke: A cluster randomised trial. Implementation Science, 11, 120 10.1186/s13012-016-0487-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Masterson-Algar P., Burton C. R., Rycroft-Malone J., Sackley C. M., & Walker M. F. (2014). Towards a programme theory for fidelity in the evaluation of complex interventions. Journal of Evaluation in Clinical Practice, 20, 445–452. 10.1111/jep.12174 [DOI] [PubMed] [Google Scholar]
- *McCann L., Groot P., Charnley C., & Gardner A. (2009). Excellence in regional stroke care: An evaluation of the implementation of a stroke care unit in regional Australia. Australian Journal of Rural Health, 17, 273–278. 10.1111/j.1440-1584.2009.01098.x [DOI] [PubMed] [Google Scholar]
- *McCluskey A., Ada L., Kelly P. J., Middleton S., Goodall S., Grimshaw J. M., . . . Karageorge A. (2015). Compliance with Australian stroke guideline recommendations for outdoor mobility and transport training by post-inpatient rehabilitation services: An observational cohort study. BMC Health Services Research, 15, 296 10.1186/s12913-015-0952-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *McCluskey A., Ada L., Kelly P. J., Middleton S., Goodall S., Grimshaw J. M., . . . Karageorge A. (2016). A behavior change program to increase outings delivered during therapy to stroke survivors by community rehabilitation teams: The Out-and-About trial. International Journal of Stroke, 11, 425–437. 10.1177/1747493016632246 [DOI] [PubMed] [Google Scholar]
- *McCluskey A., Vratsistas-Curto A., & Schurr K. (2013). Barriers and enablers to implementing multiple stroke guideline recommendations: A qualitative study. BMC Health Services Research, 13, 323 10.1186/1472-6963-13-323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *McEwen S., Szurek K., Polatajko H. J., & Rappolt S. (2005). Rehabilitation education program for stroke (REPS): Learning and practice outcomes. Journal of Continuing Education in the Health Professions, 25, 105–115. 10.1002/chp.15 [DOI] [PubMed] [Google Scholar]
- Morris Z. S., Wooding S., & Grant J. (2011). The answer is 17 years, what is the question: Understanding time lags in translational research. Journal of the Royal Society of Medicine, 104, 510–520. 10.1258/jrsm.2011.110180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Munce S. E. P., Graham I. D., Salbach N. M., Jaglal S. B., Richards C. L., Eng J. J., . . . Bayley M. T. (2017). Perspectives of health care professionals on the facilitators and barriers to the implementation of a stroke rehabilitation guidelines cluster randomized controlled trial. BMC Health Services Research, 17, 440 10.1186/s12913-017-2389-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Petzold A., Korner-Bitensky N., Salbach N. M., Ahmed S., Menon A., & Ogourtsova T. (2012). Increasing knowledge of best practices for occupational therapists treating post-stroke unilateral spatial neglect: Results of a knowledge-translation intervention study. Journal of Rehabilitation Medicine, 44, 118–124. 10.2340/16501977-0910 [DOI] [PubMed] [Google Scholar]
- *Petzold A., Korner-Bitensky N., Salbach N. M., Ahmed S., Menon A., & Ogourtsova T. (2014). Determining the barriers and facilitators to adopting best practices in the management of poststroke unilateral spatial neglect: Results of a qualitative study. Topics in Stroke Rehabilitation, 21, 228–236. 10.1310/tsr2103-228 [DOI] [PubMed] [Google Scholar]
- Powell B. J., McMillen J. C., Proctor E. K., Carpenter C. R., Griffey R. T., Bunger A. C., . . . York J. L. (2012). A compilation of strategies for implementing clinical innovations in health and mental health. Medical Care Research and Review, 69, 123–157. 10.1177/1077558711430690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor E. K., Powell B. J., & McMillen J. C. (2013). Implementation strategies: Recommendations for specifying and reporting. Implementation Science, 8, 139 10.1186/1748-5908-8-139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor E., Silmere H., Raghavan R., Hovmand P., Aarons G., Bunger A., . . . Hensley M. (2011). Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health, 38, 65–76. 10.1007/s10488-010-0319-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Read S. J., & Levy J. (2006). Effects of care pathways on stroke care practices at regional hospitals. Internal Medicine Journal, 36, 638–642. 10.1111/j.1445-5994.2006.01147.x [DOI] [PubMed] [Google Scholar]
- *Russell W., Pritchard-Wiart L., & Manns P. J. (2018). Clinician perspectives on cross-education in stroke rehabilitation. Disability and Rehabilitation, 40, 2644–2649. 10.1080/09638288 [DOI] [PubMed] [Google Scholar]
- *Salbach N. M., Wood-Dauphinee S., Desrosiers J., Eng J. J., Graham I. D., Jaglal S. B., . . . Bayley M. T.; Stroke Canada Optimization of Rehabilitation By Evidence – Implementation Trial (SCORE-IT) Team. (2017). Facilitated interprofessional implementation of a physical rehabilitation guideline for stroke in inpatient settings: Process evaluation of a cluster randomized trial. Implementation Science, 12, 100 10.1186/s13012-017-0631-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Schmid A. A., Butterbaugh L., Egolf C., Richards V., & Williams L. (2008). Prevention of secondary stroke in VA: Role of occupational therapists and physical therapists. Journal of Rehabilitation Research and Development, 45, 1019–1026. 10.1682/JRRD.2007.10.0162 [DOI] [PubMed] [Google Scholar]
- *Scobbie L., McLean D., Dixon D., Duncan E., & Wyke S. (2013). Implementing a framework for goal setting in community based stroke rehabilitation: A process evaluation. BMC Health Services Research, 13, 190 10.1186/1472-6963-13-190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thieme H., Mehrholz J., Pohl M., Behrens J., & Dohle C. (2013). Mirror therapy for improving motor function after stroke. Stroke, 44, e1–e2. 10.1161/STROKEAHA.112.673087 [DOI] [PubMed] [Google Scholar]
- Upton D., Stephens D., Williams B., & Scurlock-Evans L. (2014). Occupational therapists’ attitudes, knowledge, and implementation of evidence-based practice: A systematic review of published research. British Journal of Occupational Therapy, 77, 24–38. 10.4276/030802214X13887685335544 [DOI] [Google Scholar]
- Wang P., Gou Y., Zhang J. M., Zhao L., Cui X. C., Liao W. J., & Yue G. H. (2011). Efficacy of mental practice on rehabilitation of hand function in patients with post-stroke: A systematic review. Chinese Journal of Evidence-Based Medicine, 11, 529–539. [Google Scholar]
- Wolf S. L., Winstein C. J., Miller J. P., Taub E., Uswatte G., Morris D., . . . Nichols-Larsen D.; EXCITE Investigators. (2006). Effect of constraint-induced movement therapy on upper extremity function 3 to 9 months after stroke: The EXCITE randomized clinical trial. JAMA, 296, 2095–2104. 10.1001/jama.296.17.2095 [DOI] [PubMed] [Google Scholar]
- Wolf T. J., & Nilsen D. M. (2015). Occupational therapy practice guidelines for adults with stroke. Bethesda, MD: AOTA Press. [Google Scholar]
- Wressle E., & Samuelsson K. (2014). High job demands and lack of time: A future challenge in occupational therapy. Scandinavian Journal of Occupational Therapy, 21, 421–428. 10.3109/11038128.2014.941929 [DOI] [PubMed] [Google Scholar]