Abstract
For many years, research from around the world has suggested that the neuroactive steroid (3α,5α)-3-hydroxypregnan-20-one (allopregnanolone or 3α,5α-THP) may have therapeutic potential for treatment of various symptoms of alcohol use disorders (AUDs). In this critical review, we systematically address all the evidence that supports such a suggestion, delineate the etiologies of AUDs that are addressed by treatment with allopregnanolone or its precursor pregnenolone, and the rationale for treatment of various components of the disease based on basic science and clinical evidence. This review presents a theoretical framework for understanding how endogenous steroids that regulate the effects of stress, alcohol and the innate immune system could play a key role in both the prevention and treatment of AUDs. We further discuss cautions and limitations of allopregnanolone or pregnenolone therapy with suggestions regarding the management of risk and the potential for helping millions who suffer from AUDs.
Introduction
The magnitude of the problem of alcohol addiction likely results from the plethora of signaling and neuronal pathways that are dysregulated in those who drink excessively and lose control over their drinking behavior. It is well established that various different neural systems are dysregulated by chronic ethanol exposure (Crews et al., 1996) and dysregulation of many structural aspects of brain and its circuits are apparent (Zahr and Pfefferbaum, 2017, Abrahao et al., 2017). How do we shift the balance in favor of recovery?
This review addresses the rationale for using the neuroactive steroid allopregnanolone or its precursor pregnenolone for treatment of alcohol addiction or alcohol use disorders (AUDs). This rationale addresses three major hypotheses of alcohol addiction and delineates how the neuroactive steroid allopregnanolone interrupts each of these paths to addiction. We will present the theories that ethanol addiction results from 1) the loss of central nervous system (CNS) inhibition due to adaptations in γ-aminobutyric acid type A (GABAA) receptor-mediated neurotransmission across brain, 2) excessive corticotropin releasing factor (CRF) signaling that dysregulates the hypothalamic-pituitary-adrenal (HPA) axis and extrahypothalamic CRF circuits across brain and 3) excessive pro-inflammatory neuroimmune signaling through Toll-like receptors (TLRs) in the innate immune system and the brain. Next, we will review the evidence that allopregnanolone or pregnenolone counteract these ethanol-induced adaptations to restore GABAergic inhibition, moderate CRF signaling across brain and inhibit TLR signaling in the innate immune system and brain. We argue that the endogenous neuroactive steroids may represent protective factors that prevent the development of alcohol addiction vulnerability and could be valuable therapeutics for AUDs. The pleiotropic actions of these neuroactive steroids provide an attractive strategy to simultaneously address multiple mechanisms of alcohol addiction in its treatment. In addition, this rationale summarizes evidence that neuroactive steroids moderate many of the co-occurring symptoms of alcohol addiction, including anxiety, depression, seizures, sleep disturbance, and pain, that likely contribute to the spiral of addiction to alcohol.
I. Alcohol addiction results from loss of GABAA receptor-mediated inhibition across the brain
Many laboratories have established that ethanol-induced adaptations in GABAA receptor plasticity are associated with the development of ethanol dependence in rodent models (for review, see (Grobin et al., 1998, Kumar et al., 2009, Olsen and Liang, 2017). Furthermore, there is congruent evidence for loss of GABAergic inhibition in post-mortem human brain of patients (mostly males or unspecified) with AUDs (Volkow et al., 1993, Mitsuyama et al., 1998, Behar et al., 1999, Lingford-Hughes et al., 2005, Dodd et al., 2006). The studies show that ethanol induces adaptations in both synaptic and extrasynaptic GABAA receptor expression and/or function in cortex, hippocampus, and central amygdala in various animal models of dependence. Overall, there is a loss of GABAergic inhibition, manifest by losses in both phasic and tonic inhibition, tolerance to ethanol, and cross-tolerance to benzodiazepines and other sedative hypnotics acting on GABAA receptors at the cellular level (Kumar et al., 2009, Bohnsack et al., 2018, Olsen and Liang, 2017). As a result of this growing body of evidence, we and others have proposed that ethanol addiction evolves in response to a loss of GABAergic inhibition across brain that results in an imbalance in excitatory and inhibitory signaling, leading to loss of control over neural firing in a plethora of circuits that regulate behavioral control of alcohol seeking and intake. Some examples of circuits that are over-activated in part due to loss of GABAA receptor-mediated inhibition include the medial prefrontal cortex (mPFC) – basolateral amygdala circuit (male C57 mice) (Pleil et al., 2015), the mPFC – central nucleus of the amygdala (CeA) circuit (male and female rats) (Hughes et al., 2019), intra-hippocampal circuits (male rats) (Liang et al., 2004), intra-amygdalar circuits (male rats and mice) (Herman and Roberto, 2016, Herman et al., 2016) and ventral tegmental area (VTA) circuits (mice, unspecified sex) (Arora et al., 2013). In addition, there is compelling evidence for ethanol-induced loss of tonic currents across brain. In the hippocampus, there is a decrease in basal tonic currents, as well as blunting of the enhancement in tonic currents induced by ethanol, gaboxadol (4,5,6,7-tetrahydroisoxazolo(5,4-c)pyridin-3-ol, THIP), or Ro15–4513 (male rats) (Liang et al., 2004, Liang et al., 2006). In cerebral cortical cultured neurons (from mixed sex rat pups), there is internalization of extrasynaptic α4βδ GABAA receptors that results in the loss of tonic inhibition as well as responses to THIP and ethanol (Carlson et al., 2016). In the central amygdala, there is a selective loss of tonic inhibition in the CRF1 receptor positive neurons that regulate neuronal output (male mice) (Herman et al., 2016). Since ethanol addiction results in the loss of both phasic and tonic inhibition in humans and animal models of addiction, therapeutics that restore GABA inhibition to normal levels may be beneficial for treatment during withdrawal periods where CNS excitation interferes with treatment, recovery and relapse prevention.
While benzodiazepines clearly enhance phasic GABAergic inhibition across brain, these compounds also promote the uncoupling and internalization of synaptic GABAA receptors (male rats, unspecified sex in mice) (Gallager et al., 1984, Tehrani and Barnes, 1997) and hence they promote the very mechanisms that lead to some of the ethanol-induced deficits in GABAergic inhibition. Indeed, the risk of benzodiazepine dependence is also a serious concern. Furthermore, benzodiazepines do not promote tonic inhibition or activate extrasynaptic GABAA receptors containing δ subunits (male mice) (Stell et al., 2003), so benzodiazepine therapy is unlikely to replace the loss of tonic inhibition following chronic ethanol exposure. Unfortunately, these considerations have not been incorporated into clinical practice and the continued use of benzodiazepines for alcohol withdrawal symptoms and detoxification may explain the relative ineffectiveness of this treatment with respect to the prevention of relapse (women and men) (Moos and Moos, 2006, Garbutt et al., 1999). We must do better in the treatment of alcohol withdrawal symptoms and detoxification.
a. Evidence that neuroactive steroids increase both phasic and tonic GABAA receptor-mediated inhibition
Neuroactive steroids that are 3α,5α-reduced derivatives of progesterone, deoxycorticosterone, dehydroepiandrosterone and testosterone, are endogenous positive modulators of all GABAA receptor subtypes (Puia et al., 1991, Kokate et al., 1994, Reddy and Rogawski, 2002, Belelli et al., 2002, Herd et al., 2007). Allopregnanolone and allotetrahydrodeoxycorticosterone (3α,5α-THDOC) exhibit high potency at most subtypes of recombinant GABAA receptors (Puia et al., 1990, Puia et al., 1993), although they are more potent at some extrasynaptic GABAA receptors containing the δ subunit (Belelli and Lambert, 2005, Carver and Reddy, 2013). For example, low concentrations of 3α,5α-THDOC, which have no effect on phasic conductance mediated by synaptic GABAA receptors, selectively enhance tonic currents mediated by δ subunit containing GABAA receptors in mouse dentate gyrus and cerebellar granule cells (Stell et al., 2003). Likewise, allopregnanolone and the synthetic neuroactive steroids SGE-516 and ganaxolone also increase tonic currents in dentate gyrus granule cells (LTK cells and male mice) (Modgil et al., 2017). Although the neuroactive steroid binding sites are located at the interface of the α and β subunits of synaptic receptors (Hosie et al., 2006), the δ subunit is thought to be responsible for the enhanced sensitivity to neuroactive steroids. In fact, δ subunit knockout mice have blunted tonic currents along with reduced sensitivity to neuroactive steroid modulation of GABAA receptors (unspecified or male mice) (Mihalek et al., 1999, Stell et al., 2003, Spigelman et al., 2003). Furthermore, α4 subunit knockout mice also display a loss of δ subunits and blunted tonic inhibition (unspecified sex) (Chandra et al., 2006), along with a reduced GABAergic potentiation by alphaxalone (male mice) (Liang et al., 2008).
Transient fluctuations in the levels of endogenous neuroactive steroids, which occur physiologically during the ovarian cycle or during pregnancy, alter GABAA receptor subunit expression and tonic currents in a way that parallels steroid concentrations. Thus, elevated allopregnanolone levels during the diestrus phase of the female mouse ovarian cycle (Maguire et al., 2005), or at gestational day 19 in pregnant female rats (Sanna et al., 2009) are associated with increased expression of δ subunit-containing GABAA receptors and subsequent enhancement in tonic inhibition. However, the in vivo regulation of extrasynaptic GABAA receptor expression and function by neuroactive steroids may be more complex, given that conditions associated with low allopregnanolone concentrations also enhance α4/δ-subunit containing GABAA receptors and associated tonic inhibition (males and females) (Serra et al., 2006, Shen et al., 2007, Carver et al., 2014, Locci et al., 2017).
b. Evidence that neuroactive steroids may restore deficits in GABA inhibition
Neuroactive steroids might represent a useful therapeutic approach to restore deficits in GABAergic inhibition, observed in patients with AUDs. This argument is supported by data from animal models of alcohol addiction and effects of neuroactive steroids in other conditions that involve the loss of inhibitory control in the CNS. Some examples are described.
i. Anxiolytic and antidepressant actions in animals and humans
Administration of allopregnanolone exerts anxiolytic-like and antidepressant-like effects in rodents (Crawley et al., 1986, Bitran et al., 1991, Khisti et al., 2000), which may be important for prevention and recovery from AUDs. Similar effects are reported in humans; specifically, intravenous infusion of Brexanolone, a proprietary formulation of allopregnanolone by Sage Therapeutics, exerts a rapid effect in counteracting postpartum anxiety and depression. Women with moderate to severe postpartum depression showed a quick improvement in agitation, anxiety and depressive symptoms following a 60-hour constant intravenous infusion of the drug, an effect that lasted more than a month (Kanes et al., 2017, Meltzer-Brody et al., 2018). Such rapid and long-lasting effects represent a major breakthrough for the treatment of depression. While it is unknown if the therapeutic effects of Brexanolone for postpartum depression are dependent on its GABAergic activity, this concept seems likely. Previous evidence has documented that GABA inhibition is compromised in patients with depression, since levels of GABA are reduced in plasma, cerebrospinal fluid and occipital cortex of depressed subjects, while GABAA receptors and physiological activity are also diminished in males and females (Sanacora and Saricicek, 2007, Croarkin et al., 2011). The recent studies with Brexanolone represent important clinical evidence supporting the idea that restoration of GABAergic inhibition may be therapeutic for depression, although other mechanisms are likely involved.
ii. Anticonvulsive effects in ethanol dependent rats
The GABAergic neuroactive steroids have potent anticonvulsant effects in several animal models (Reddy and Rogawski, 2012). Likewise, acute ethanol-induced elevations of allopregnanolone contribute to its anticonvulsant effects in male rats (VanDoren et al., 2000). By contrast, alcohol dependence reduces GABAergic inhibition across brain, including the sensitivity to GABA- and ethanol-induced anticonvulsant actions, thus leading to increased seizure susceptibility in male and female rats. In fact, allopregnanolone administration before seizure induction blocks the increased seizure susceptibility induced by ethanol withdrawal in male and female dependent rats and male mice, with female rats being more sensitive to the protective effect of neurosteroids (Devaud et al., 1995, Finn et al., 1995, Devaud et al., 1998). Chronic intermittent ethanol exposure, which causes a reduction in hippocampal allopregnanolone content, also decreases seizure threshold in male rats, an effect that is reversed by alphaxalone administration (Cagetti et al., 2004). In male rats ethanol dependence produces tolerance to ethanol and cross-tolerance to benzodiazepines and barbiturates, including the anticonvulsant effect of benzodiazepines (Devaud et al., 1996). However, ethanol-dependent male rats are sensitizedto the anticonvulsant effects of allopregnanolone and 3α,5α-THDOC, and their GABAA receptors also have enhanced sensitivity to the actions of neuroactive steroids (Devaud et al., 1996, Cagetti et al., 2004). Thus, GABAergic neuroactive steroids may be therapeutic during ethanol withdrawal, and their use may have advantages over benzodiazepine therapy since benzodiazepines exhibit cross-tolerance with ethanol.
iii. Effectiveness in status epilepticus
Status epilepticus is a neurological life-threatening condition characterized by continuous or recurring seizures with loss of consciousness for more than 30 minutes. Patients with this condition do not respond to the classical benzodiazepine therapy because seizures are likely to alter GABAA receptors subunit expression and trafficking (Rogawski et al., 2013) (mostly based on studies in males). In fact, preclinical studies in male rat models of status epilepticus showed that benzodiazepine sensitive synaptic GABAA receptors are internalized, causing a reduction in synaptic inhibition (Naylor et al., 2005), while benzodiazepine insensitive extrasynaptic α4/δ GABAA receptors do not internalize and are functional (Goodkin et al., 2008), thus representing a putative pharmacological target for status epilepticus. Given that GABAergic neuroactive steroids have potent anticonvulsant effects in several animal models (Devaud et al., 1995, Reddy and Rogawski, 2012), and potent modulatory actions at extrasynaptic GABAA receptors (Belelli and Lambert, 2005), they may be valuable therapeutic agents. Indeed, allopregnanolone and its synthetic 3β-methyl analog ganaxolone both proved effective in rodent (mostly males) models of treatment-resistant status epilepticus (Rogawski et al., 2013, Zolkowska et al., 2018). Furthermore, case reports,limited to two young girls and two young adult men, suggested that intravenous allopregnanolone may be therapeutic for status epilepticus in a number of individuals (Broomall et al., 2014, Vaitkevicius et al., 2017). However, a clinical trial (https://clinicaltrials.gov/ct2/show/study/NCT02477618) evaluating the efficacy of Brexanolone did not show any improvement for the treatment of super refractory status epilepticus in human patients, (https://investor.sagerx.com/news-releases/news-release-details/sage-therapeutics-reports-top-line-results-phase-3-status-trial), although its intravenous administration was well tolerated among adults and children (Vaitkevicius et al., 2017)https://clinicaltrials.gov/ct2/show/NCT02477618?term=NCT02477618&rank=1. Dosing of allopregnanolone and variations in metabolism among patients are issues that may have impacted the outcome of this study, since some patients clearly responded to the therapy.
iv. Potential effectiveness in sleep disturbances
Both synaptic and extrasynaptic GABAA receptors contribute to regulate sleep and wakefulness. Benzodiazepines, traditionally used to treat insomnia, typically act on synaptic α1-2-3-5βγ2 GABAA receptors mediating phasic inhibition. Benzodiazepines shorten latency to sleep and increase sleep continuity (Winsky-Sommerer, 2009). In addition, endogenous neuroactive steroids also exert sedative-hypnotic actions in male rats (Mendelson et al., 1987, Lancel et al., 1997), similar to other exogenous modulators (THIP) of extrasynaptic α4βδ GABAA receptors (Belelli and Lambert, 2005). Indeed, tonic inhibition mediated by α4βδ GABAA receptors in the thalamus and cortex, by adjusting the excitability of neuronal circuitries, plays an important role in modulating the magnitude and frequency of network oscillation characterizing waking and sleep (Winsky-Sommerer, 2009). Sleep disturbances are reported in AUDs, and alcohol’s action on GABAA receptors is thought to contribute to sleep loss and increased wakefulness (Koob and Colrain, 2019). Moreover, blunted neuroactive steroids responses to stress were associated with poor sleep quality in pregnant women (Crowley et al., 2016) and, given that alcoholics also show blunted HPA and neuroactive steroids responses to stress (Adinoff et al., 1990, Adinoff et al., 2005b, Adinoff et al., 2005c, Adinoff et al., 2005a, Porcu et al., 2008), these alterations might contribute to sleep dysregulation. Thus, administration of neuroactive steroids might ameliorate sleep quality in AUDs by restoring GABAergic tone.
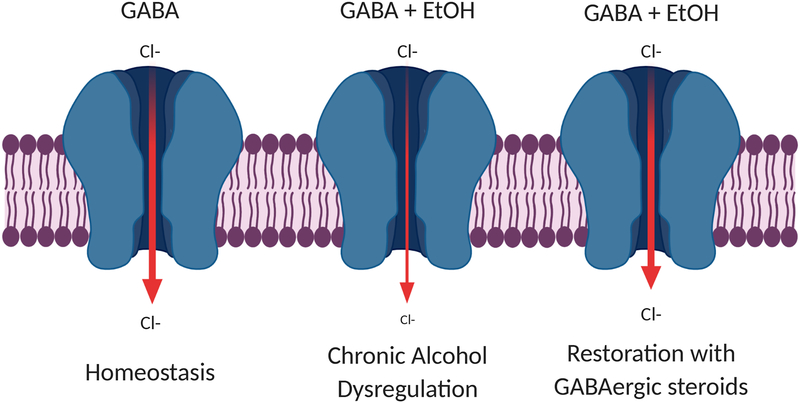
In summary, deficits in inhibitory transmission in the CNS are hallmarks of alcohol addiction and many of the definitive symptoms of AUDs. The neuroactive steroid allopregnanolone is capable of correcting deficits in inhibitory neurotransmission and has demonstrated clinical efficacy for treatment of anxiety, depression, seizures and sleep in both animal models and early human clinical trials. Figure 1 summarizes the theoretical basis of this argument. Importantly, allopregnanolone exhibited no evidence of toxicity or untoward effects in any study to date. The overlap and co-morbidity of these conditions in AUDs should not be ignored and based on these observations, the potential for allopregnanolone therapy warrants immediate consideration.
Figure 1. Schematic representation of GABAergic steroid restoration of GABAA receptor-mediated signaling dysregulation due to chronic alcohol exposure.
Chronic alcohol exposure causes a reduction of GABA-mediated signaling through loss of GABAA receptor expression and internalization. GABAergic steroids, such as allopregnanolone, restore homeostasis by increasing GABAA receptor-mediated inhibition through both synaptic and extrasynaptic receptors. Created using BioRender.com.
II. Alcohol addiction results from excessive CRF signaling
CRF signaling across the brain plays a major role in drug addiction, starting from the initial activation of the HPA axis through enhancement of hypothalamic CRF by acute administration of several drugs of abuse, to the subsequent phases of binge/intoxication, withdrawal, and relapse/reinstatement (Koob, 2013) that involves the extrahypothalamic CRF system in the extended amygdala (Zorrilla et al., 2014).
CRF is a 41 amino acid polypeptide widely distributed throughout the brain. The highest densities of CRF neurons are found in the paraventricular nucleus (PVN) of the hypothalamus, where CRF is the main effector of the response to stress mediated by HPA activation (male rats) (Rivier and Vale, 1983). CRF-positive cells are also abundant in extrahypothalamic structures of the extended amygdala, in particular the CeA, and the bed nucleus of the stria terminalis (BNST) (male mouse) (Peng et al., 2017), which mediate the behavioral and emotional response to stress (Schreiber and Gilpin, 2018). CRF binds to two types of Gs protein-coupled receptors, CRF receptor type 1 (CRFR1) and type 2 (CRFR2). CRFR1s are widely expressed throughout the brain and trigger the HPA response to stress as well as anxiogenic behavior. The role of CRFR2s, whom CRF binds with lower affinity, is less clear and may involve maintenance of homeostasis (Henckens et al., 2016).
In basal conditions, the CRF neurons are under the inhibitory influence of GABAergic interneurons located in the PVN (Cullinan et al., 2008) as well as in extrahypothalamic regions including BNST, VTA and nucleus accumbens (NAc). During acute stress, the main neurotransmitters released in PVN are norepinephrine and glutamate (Herman et al., 2002). However, chronic alcohol exposure, like chronic stress, disrupts the equilibrium between excitatory/inhibitory inputs, causing a decrease in inhibition and an increase in excitatory signals that results in hyperactivity of the HPA axis.
a. Evidence for exacerbation of CRF signaling across brain in ethanol dependence
Ethanol, like other drugs of abuse, activates the HPA response to stress during acute withdrawal via hypothalamic CRF and CRFR1 activation that results in elevated adrenocorticotropic hormone (ACTH) and corticosteroids; within hours it also activates the extrahypothalamic CRF response, with subsequent increased CRF release from the amygdala, which through CRFR1, increases GABA release in the CeA. Likewise, binge alcohol drinking also affects hypothalamic and extrahypothalamic CRF signaling in different ways depending on species, age and experimental procedures employed. Chronic alcohol exposure increases hypothalamic and extrahypothalamic CRF gene expression immediately after consumption. However, during withdrawal hypothalamic CRF and CRFR1 expression is reduced, with subsequent blunting of the HPA response, whereas extrahypothalamic CRF release is increased within the CeA and BNST (see (Agoglia and Herman, 2018, Roberto et al., 2017) and (Schreiber and Gilpin, 2018) for review). It has been hypothesized that upregulation of CRF signaling may contribute to negative affect during withdrawal that motivates escalation of alcohol drinking (Zorrilla et al., 2014).
The majority of these studies have been conducted in male rodents. However, preclinical studies demonstrated cellular and molecular sex differences in stress response systems, including CRFR1 coupling, signaling, and trafficking (reviewed in (Bangasser and Valentino, 2014, Oyola and Handa, 2017, Logrip et al., 2018)). Further studies are needed to determine sex differences in ethanol effects on CRF signaling.
CRF signaling also modulates the rewarding properties of alcohol and influences its consumption. A reduction in ethanol intake has been observed in CRF and CRFR1 knockout mice. Likewise, CRFR1 antagonists reduced binge-like ethanol drinking, drinking in dependent animals, as well as drinking in non-dependent animals that consume large amounts of alcohol. CRF signaling in the CeA has been thought to play a critical role in this effect, given that antagonism of CRFR1 in the CeA, but not BNST or NAc, reduced alcohol self-administration in dependent rats (Agoglia and Herman, 2018, Schreiber and Gilpin, 2018, Zorrilla et al., 2014).
A dysregulation of the extrahypothalamic CRF systems is hypothesized to play a role in the negative symptoms of withdrawal and subsequent relapse. In fact, the extrahypothalamic CRF signaling, activated by multiple withdrawal cycles, sensitizes the brain to such repeated cycles, thus contributing to negative emotional states (i.e. anxiety-like behavior) that trigger relapse and maintenance of drug taking (Zorrilla et al., 2014). In line with this interpretation, it has recently been shown that optogenetic inactivation of CRF neurons in the CeA reduced alcohol consumption and withdrawal symptoms in dependent male rats (de Guglielmo et al., 2019). CRFR1 are also involved in these processes; in fact, withdrawal-induced anxiety is absent in CRFR1 knockout mice or can be blocked by CRFR1 antagonists in alcohol dependent animals. Further, CRFR1 antagonists attenuate stress and cue-induced reinstatement of alcohol seeking behavior; the decrease in alcohol seeking behavior following stress is likely mediated by extrahypothalamic CRF, given that it is not influenced by adrenalectomy, while hypothalamic CRF may mediate cue-induced reinstatement because metyrapone, an inhibitor of glucocorticoid synthesis, mimics the reduction in reinstatement induced by CRFR1 antagonists (Schreiber and Gilpin, 2018).
Clinical studies also suggest that acute alcohol intoxication activates the HPA axis in healthy non-dependent subjects (Mendelson and Stein, 1966), but alcohol dependence leads to adaptations in the HPA/CRF signaling that result in a blunted cortisol and ACTH response to stress (Adinoff et al., 1990, Adinoff et al., 2005b, Adinoff et al., 2005c, Adinoff et al., 2005a). Further, such responses are accompanied by increased alcohol craving during stress in binge/heavy drinkers as well as in moderate social drinkers, and are predictive of higher risk for relapse after treatment (Breese et al., 2011, Sinha et al., 2011, Blaine et al., 2019), suggesting that CRF signaling represents a crucial therapeutic target for multiple aspects of AUDs. Furthermore, the loss of GABA inhibition in ethanol dependence likely contributes to the dysregulation of CRF signaling in AUDs.
Indeed, preclinical studies suggest that CRFR1 antagonists may have therapeutic utility in AUDs, to reduce symptoms of withdrawal and excessive alcohol drinking, as well as prevent relapse. However, clinical trials in humans have so far been unsuccessful. Thus, alternative ways to target CRF signaling in humans may be beneficial, and neuroactive steroids may represent one way to achieve this goal, given their modulatory action on HPA homeostasis (see below) and extrahypothalamic CRF levels (Balan et al., 2019a, Balan et al., 2019b).
b. Evidence that allopregnanolone reduces CRF signaling
Acute stress rapidly decreases the GABAergic transmission in male rats (Biggio et al., 2007), leading to HPA axis activation with subsequent release of corticosterone, as well as allopregnanolone (Purdy et al., 1991). The increase in allopregnanolone content, which occurs approximately 30 minutes after acute stress, is thought to represent a homeostatic mechanism to restore the GABAergic inhibition upon the PVN of the hypothalamus, thus shutting down HPA axis activity. Both corticosterone and allopregnanolone exert a negative feedback upon the hypothalamus and pituitary. Specifically, allopregnanolone counteracts the anxiety-like behavior induced by CRF administration, prevents the elevation of CRF gene expression induced by adrenalectomy and prevents the release of CRF from isolated hypothalamic explants (Patchev et al., 1994). Moreover, allopregnanolone or 3α,5α-THDOC administration before stress attenuates the stress-induced increase in ACTH and corticosterone (Patchev et al., 1996, Owens et al., 1992). In agreement, intracerebroventricular administration of allopregnanolone antiserum enhanced the corticosterone response to stress in prepubertal and adult male and female rats, without affecting its basal levels (Guo et al., 1995). Likewise, physiological levels of allopregnanolone (10 – 100 nM) inhibit CRF release from PVN neurons via a potentiation of GABAA receptors in electrophysiological recordings from neonatal male and female mice (Gunn et al., 2013, Gunn et al., 2015). In addition, systemic administration of allopregnanolone to adult male non-stressed rats increased hypothalamic CRF content as well as serum ACTH and corticosterone (Naert et al., 2007), supporting a regulatory role for this neuroactive steroid in HPA function, whereby allopregnanolone may increase hormone levels in basal conditions and decrease them in stress-induced perturbations to restore homeostasis. Systemic administration of pregnenolone, dehydroepiandrosterone and their sulfate metabolites also increased hypothalamic CRF and serum ACTH and corticosterone (Naert et al., 2007). All these effects were rapid and likely mediated by a direct action of neuroactive steroids on neurotransmission in the hypothalamus that regulate HPA axis activation.
c. Evidence that allopregnanolone may restore deficits precipitated by aberrant CRF signaling
Several lines of both clinical and basic science evidence suggest that neuroactive steroids may restore homeostasis in CRF signaling both at the hypothalamic and extrahypothalamic circuit levels. The anxiolytic effects of allopregnanolone are likely to be related to both hypothalamic and extrahypothalamic CRF levels since CRF circuits are tightly coupled to anxiety-like behaviors in rodents (vide supra). Some examples follow.
i. Antidepressant-like activity
Affective disorders, including major depression, postpartum depression, post-traumatic stress disorder (PTSD) and AUDs are characterized, among other features, by neuroendocrine alterations at the HPA axis level (Girdler and Klatzkin, 2007, Girdler et al., 2012, Schule et al., 2014, Rasmusson et al., 2017, Bixo et al., 1997, Baumeister et al., 2014, Adinoff et al., 2005b, Adinoff et al., 2005c). These alterations generally involve excessive baseline cortisol and suppression of the HPA axis response to stress. Considering the ability of allopregnanolone to regulate the HPA axis at the level of the hypothalamus, it is possible that restoration of HPA axis balance is an important component of treatment. Indeed, the remarkable clinical efficacy of Brexanolone in the treatment of postpartum depression may be related to this property of allopregnanolone. While further studies are needed to determine the mechanism(s) of the antidepressant actions of Brexanolone, the rapid and long-lasting efficacy following a short course of 60 hours of treatment suggests a type of reset that is consistent with normalization of HPA axis function.
Furthermore, although classical treatments for depression such as selective serotonin reuptake inhibitors require several weeks to produce therapeutic actions, increased neurosteroidogenesis is a likely mechanism involved in their therapeutic actions. Several studies have shown that administration of antidepressant drugs restores neuroactive steroid concentrations in both patients and rodents (Uzunov et al., 1996, Uzunova et al., 1998, Romeo et al., 1998, Marx et al., 2006, Schule et al., 2014). Indeed, serotonin reuptake inhibitors promote the conversion of 5α-dihydroprogesterone to allopregnanolone via a direct effect on the neurosteroidogenic enzyme 3α-hydroxysteroid dehydrogenase (Griffin and Mellon, 1999). Thus, neuroactive steroids may have great potential for the treatment of depression in general, and specifically depression associated with dysregulation of the HPA axis, a common feature in patients with AUDs.
ii. Neuroactive steroids deficits associated with HPA axis dysfunction in PTSD
PTSD patients show elevated CRF levels (Bremner et al., 1997), along with a dysregulated HPA axis function that leads to glucocorticoid hypersensitivity (Castro-Vale et al., 2016). In addition, concentrations of GABAergic neuroactive steroids are altered in PTSD patients: a reduction in cerebrospinal levels of allopregnanolone has been reported in premenopausal women and men, and such levels were negatively correlated with PTSD symptoms (Rasmusson et al., 2006, Rasmusson et al., 2017). Indeed, both preclinical and clinical evidence suggests a role for GABAergic neuroactive steroids in PTSD (Rasmusson et al., 2017). In agreement, clinical trials are ongoing (; ) to test the effectiveness of pregnenolone in targeting PTSD symptoms.
iii. Beneficial effects of neuroactive steroids against craving in humans with cocaine abuse disorders
Craving and compulsion are hallmark symptoms of AUDs and neuroactive steroids may be beneficial against such symptoms. Clinical evidence in both men and women with co-morbid cocaine and AUDs seeking treatment for cocaine dependence suggests that progesterone administration reduced cue and stress-induced cocaine craving as well as the cortisol response to stress and improved positive emotions (Fox et al., 2013, Milivojevic et al., 2016). Further, these subjects had decreased serum levels of progesterone, allopregnanolone and pregnenolone, that normalized after a 7-day treatment with exogenous progesterone (Milivojevic et al., 2016, Milivojevic et al., 2019). Interestingly, those subjects with higher allopregnanolone levels following progesterone treatment showed a normalization of basal and stress-induced cortisol levels, improved positive emotions and cognitive performance, and decreased cocaine craving as well as stress-induced cocaine craving. These results, albeit obtained in a small population, are very encouraging in supporting the therapeutic potential of neuroactive steroids in drug addiction, including AUDs.
iv. Allopregnanolone reversal of HPA axis dysregulation after social isolation
Social isolation from weaning to adulthood is a model of chronic stress and PTSD that markedly decreases brain and plasma allopregnanolone levels in rats and mice (Serra et al., 2000, Dong, 2001). A blunted HPA axis activity has been hypothesized to account for such decrease (Biggio et al., 2014). In agreement, socially isolated male rats also show a reduction in basal ACTH and corticosterone levels, and an impaired negative feedback regulation (Serra et al., 2005, Pisu et al., 2016, Boero et al., 2018). Importantly, administration of allopregnanolone either from the onset of social isolation, or following six weeks of isolation, prevents or normalizes the corticosterone response to the dexamethasone suppression test, as well as depression- and anxiety-like behavior in male rats (Evans et al., 2012). Since allopregnanolone normalizes the HPA axis and behavioral abnormalities after social isolation, it could have similar effects in other conditions that dysregulate the HPA axis and produce abnormal anxiety and depression.
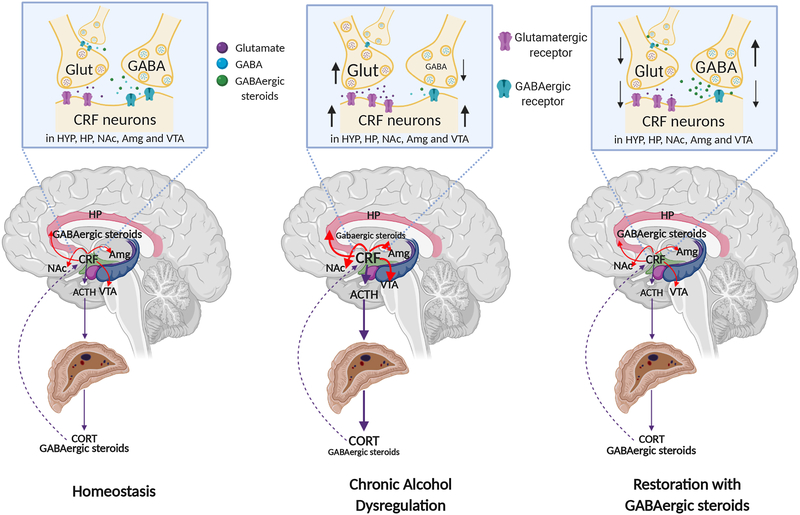
In summary, human depression and PTSD as well as drug craving each induce alterations in CRF and HPA axis function and each of these conditions is responsive to treatment with allopregnanolone, progesterone or pregnenolone. Figure 2 shows a schematic of the theoretical basis of this hypothesis. The similarities and high rates of co-morbidity of these conditions with AUDs should not be ignored and the beneficial effects of neuroactive steroids in these conditions support the rationale for the use of these neuroactive steroids in AUD treatment as well.
Figure 2. Restoration of CRF dysregulation in alcohol dependence by GABAergic steroids.
Chronic alcohol abuse decreases neuroactive steroids levels and increases CRF signaling, in both hypothalamic and extrahypothalamic circuits. The effects of ethanol on CRF signaling are enhanced by the reduction of GABAA receptor-mediated transmission and enhancement of glutamatergic transmission. GABAergic steroids can restore homeostasis by reinforcing GABAergic transmission and by directly decreasing CRF levels.
(HYP= hypothalamus; HP= hippocampus; NAc= nucleus accumbens; Amg= amygdala; VTA= ventral tegmental area; Glut= glutamatergic neuron; GABA= GABAergic neuron; ACTH= adrenocorticotropic hormone; CORT= cortisol/corticosterone; GABAergic steroids= neuroactive steroids positive modulators of GABAA receptors). Created using BioRender.com.
III. Alcohol addiction results from excessive pro-inflammatory neuroimmune signaling across brain
Neuroimmune signaling through TLRs is an important contributor to various inflammatory conditions, including AUDs (Crews et al., 2017a, He and Crews, 2008, Qin et al., 2008), other addictions (Lacagnina et al., 2017), depression (Bhattacharya et al., 2016, Dantzer et al., 2008), traumatic brain injury (He et al., 2004a) and epilepsy (Maroso et al., 2011). The innate immune cells in the brain, microglia, as well as neurons and other glial cells signal via TLRs to promote innate immune gene expression and produce pro-inflammatory cytokines and chemokines in a progressive and feed-forward fashion (Pavlov and Tracey, 2017), that is particularly long lasting in the brain (Crews et al., 2017a).
Several groups have suggested that excessive neuroimmune signaling in the brain drives alcohol addiction, based on studies in animal models in males and females as well as analysis of post-mortem brains of human alcoholics (male and female) (Crews et al., 2017a, Crews and Vetreno, 2016, Mayfield and Harris, 2017, Alfonso-Loeches et al., 2010, Aurelian and Balan, 2019). Indeed, alcohol activates multiple TLR signaling pathways in several brain regions (Leclercq et al., 2012, Pascual et al., 2015, Kane et al., 2014), enhances the microglial response to peripheral inflammation, and increases the expression of pro-inflammatory cytokines and chemokines (Crews et al., 2017a, Coleman et al., 2017, Coleman et al., 2018, Fernandez-Lizarbe et al., 2013) in neurons. Furthermore, alcohol alters the balance of pro- and anti-inflammatory cytokines thereby potentially contributing to increased risk or protection from AUDs (Aurelian and Balan, 2019, Qin et al., 2008).
a. Neuroimmune signaling across brain promotes excessive ethanol consumption
Previous studies have demonstrated that alcohol-preferring P rats (males or unspecified sex), which fulfill most of the criteria for an animal model of human alcohol abuse (Bell et al., 2006), have an innate neuronal TLR4/MCP-1 cytokine signal that is regulated by the α2 subunit protein of GABAA receptors (GABAA receptor-α2) located in the VTA, the CeA (Liu et al., 2011, June et al., 2015), and the NAc (Balan et al., 2018). This activated TLR4 signal is found in neurons from the alcohol-preferring P rats, but not the non-preferring NP rats and appears to induce the acquisition of binge drinking and impulsivity in the selectively bred P rats. Viral-mediated inhibition of either TLR4 or the GABAA receptor-α2 subunit protein inhibit binge drinking as well as impulsivity (June et al., 2015, Balan et al., 2018). TLR4 activation is sustained by CRF that increases TLR4 expression and TLR4 activation also enhances CRF expression. Neuronal activation of TLR4 in rat brain can induce the formation of either pro-inflammatory or anti-inflammatory cytokines and the balance of these pathways may determine if neuronal TLR4 activation leads to detrimental behavioral outcomes (Aurelian and Balan, 2019).
Other studies have demonstrated that TLR3, TLR4 and TLR7 activation by their respective agonists enhances ethanol consumption in rodent models (both sexes in mice; male rats) (Warden et al., 2019, Randall et al., 2019, Blednov et al., 2011). Activation of both TLR3 and TLR4 signaling can enhance ethanol consumption, but knockout of TLR4 has not consistently produced the expected decrease in consumption (for review see (Aurelian and Balan, 2019, Mayfield and Harris, 2017)). TLR4 coupling to TLR2 may be required for acquisition of ethanol dependence (Fernandez-Lizarbe et al., 2013) and studies of many other TLR pathways are needed. Moreover, bioinformatics analysis of the effects of excessive ethanol intake in an animal models of ethanol dependence and human alcoholics suggest that neuroimmune signaling is activated and may contribute to various aspects of alcohol addiction (Agrawal et al., 2014, Kapoor et al., 2019).
b. Evidence for ethanol-induced activation of TLR signaling
Ethanol increases the expression of TLR2, TLR3, TLR4, and TLR7 and members of the pathways activated by these pathogen-activated receptors (Crews et al., 2017b). TLR signaling initiates with complex formation and activation of myeloid differentiation response protein (MyD88)-dependent and independent pathways. These include transcription factors NFκB, cyclic AMP response element binding protein (CREB), activator protein-1 (AP-1), and interferon regulatory factor (IRF) that translocate to the nucleus and control expression of chemokines and cytokines. Ethanol activates the TLR-MyD88-NFκB pathways as well as the TLR3-regulated TRIF-pathway. Intermittent alcohol drinking during adolescence upregulates the expression of TLR4 in the adult hippocampus, TLR3 and TLR4 in the adult prefrontal cortex, and TLR1-TLR8 in the adult cerebellum of male rats (Breese and Knapp, 2016, Knapp et al., 2016, Harper et al., 2017), suggesting distinct immune activation and function at distinct brain sites. Production of pro-inflammatory cytokines appears to be involved in the altered brain activity associated with alcohol intoxication and dependence (Gruol, 2013). Indeed, neuroimmune signaling via the classic pro-inflammatory cytokines in brain appears to enhance glutamatergic transmission and reduce GABAergic transmission (Stellwagen et al., 2005, Pribiag and Stellwagen, 2013, Ferguson et al., 2008, Stuck et al., 2012) rather than produce other signs of inflammation such as swelling or macrophage infiltration. On the other hand, TLR7 signaling in brain appears to lead to ethanol-induced neurodegeneration, involving the production of high motility group box 1 (HMGB1) and the miRNA-let-7 (Coleman et al., 2017, Coleman et al., 2018).
c. Evidence that neuroactive steroids inhibit TLR signaling and the production of pro-inflammatory molecules
Recent investigations suggest that neuroactive steroids, pregnenolone and allopregnanolone inhibit TLR4 signaling in an immortalized macrophage cell line (RAW264.7) as well as innate TLR4 and CRF activation in VTA of alcohol preferring P male rats (Balan et al., 2019a). In the mouse macrophage cell line, the TLR4 agonist LPS increased all the canonical markers of TLR4 activation, as well as the transcription factor pNFκB, the pro-inflammatory endogenous TLR4 agonist HMGB1, the chemokine monocyte chemoattractant protein 1 (MCP-1) and the cytokine tumor necrosis factor-α (TNF-α). All of these effects were completely inhibited by both neuroactive steroids at 0.5 and 1.0 μM doses. Pregnenolone was more potent than allopregnanolone and this effect was independent of GABAA receptor activity as pregnenolone lacks this activity (Purdy et al., 1990) and was not converted to allopregnanolone in the cells. The mechanism of neuroactive steroid inhibition appears to involve blockade of TLR4/MD-2 protein interactions in RAW246.7 cells, as both neuroactive steroids blocked the co-immunoprecipitation of TLR4 with MD-2, a requisite step in the activation of the TLR4-MyD88-dependent signaling pathway. These data suggest a novel role for both pregnenolone and allopregnanolone to inhibit TLR4 signaling in the innate immune system (Balan et al., 2019a). Similar inhibition of TLR4 signaling by pregnenolone, progesterone and allopregnanolone were found via degradation of TLR2 and TLR4-associated proteins (Murugan et al., 2019).
In the P rat VTA, allopregnanolone administration reduced both CRF expression (30%) and innate TLR4 activation via TLR4 binding to the GABAA receptor α2 subunit protein (60%) and/or MyD88 (40%), measured by co-immunoprecipitation (Balan et al., 2019a). The data suggest that inhibition of pro-inflammatory neuroimmune signaling contributes to the protective effects of allopregnanolone in brain, apparently involving blockade of protein-protein interactions that initiate TLR4-dependent signaling. Other studies show that allopregnanolone and progesterone block TLR4 activation in animal models of ischemia and traumatic brain injury (He et al., 2004a, Sayeed and Stein, 2009). In light of the hypothesis that activation of inflammatory neuroimmune signaling underlies the development of alcohol addiction, the ability of allopregnanolone to inhibit TLR4 signaling in both macrophages and brain suggests that it may have therapeutic utility in the prevention or treatment of AUDs. Allopregnanolone may also impact other TLR pathways (Murugan et al., 2019, Sayeed and Stein, 2009), and this question also deserves further study.
d. Evidence that allopregnanolone and pregnenolone block feed-forward activation of neuroimmune signals.
Neuroactive steroids might represent a useful therapeutic approach to arrest detrimental neuroimmune signaling, observed in patients with AUDs. This argument is supported by data from animal models of alcohol addiction and effects of neuroactive steroids in other conditions that involve excessive neuroimmune activation in the CNS. Some examples are described.
i. Therapeutic effects in multiple neuroinflammatory diseases
The endogenous neuroactive steroids pregnenolone and allopregnanolone have protective activity in neurological and psychiatric conditions that involve pro-inflammatory signaling. Significantly, progesterone and/or allopregnanolone have shown efficacy in clinical studies of traumatic brain injury (Wright et al., 2007), co-morbid cocaine and AUD craving (Fox et al., 2013, Milivojevic et al., 2016) as well as postpartum depression (Kanes et al., 2017, Meltzer-Brody et al., 2018). Further, allopregnanolone has therapeutic activity in traumatic brain injury (He et al., 2004b), multiple sclerosis (Noorbakhsh et al., 2014, Schumacher et al., 2007), and Alzheimer’s disease (Brinton, 2013). This growing body of inflammatory conditions that respond to intervention with neuroactive steroids supports the idea that inhibition of neuroimmune signaling may be an important component of their actions.
Pain is considered a neuroinflammatory condition. AUDs are often associated with chronic pain, and the overlap of the neuronal circuits and neuromodulators involved in both conditions has been suggested to account for such comorbidity (Egli et al., 2012). Preclinical studies suggest that neuroactive steroids play an important role in both inflammatory and neuropathic pain. Intracerebroventricular administration of allopregnanolone has analgesic effects in naïve male rats (Kavaliers and Wiebe, 1987). Likewise, systemic and intrathecal administration of allopregnanolone, or its precursor progesterone, exerts anti-nociceptive properties in several models of neuropathic (see (Gonzalez et al., 2019) for review) and inflammatory pain (Ocvirk et al., 2008). Thus, administration of neuroactive steroids might be beneficial to ameliorate pain symptoms. Indeed, a recent clinical study in 92 veterans showed that pregnenolone administration for 4 weeks reduced chronic pain symptoms by 20% while the patients in the placebo control group reported a decrease in pain symptoms of 4% (https://www.ajmc.com/conferences/sobp-2018/new-drug-discoveries-aim-to-help-veterans-others-with-chronic-pain.). However, other evidence in humans linking neuroactive steroids to pain showed opposite effects: low serum allopregnanolone content was associated with either increased pain tolerance in healthy male and female volunteers (Mechlin et al., 2007), or increased self-reported pain symptoms in another study of male war veterans (Naylor et al., 2016). Therefore, allopregnanolone and pregnenolone should be further studied for inhibition of inflammatory signaling associated with pain.
ii. Therapeutic effects in postpartum depression – once again
Depression is increasingly linked to neuroinflammation or more specifically to the presence of pro-inflammatory markers in patients (Bhattacharya et al., 2016, Dantzer et al., 2008, Vichaya et al., 2019). Indeed, several studies show that inflammatory markers are elevated in women with postpartum depression (Corwin et al., 2008, Kendall-Tackett, 2007), suggesting that neuroimmune activation may contribute to symptoms of depression in these women. As presented in Sections I and II of this review, the remarkable, rapid and long-lasting antidepressant effect of Brexanolone infusion for postpartum depression may involve inhibitory effects on neuroinflammation as well as restoration of GABAergic inhibition and normalization of CRF signaling. The ability of allopregnanolone to inhibit the activation of TLR signaling in the innate immune system could reduce pro-inflammatory signaling that contributes to these therapeutic effects. While this idea remains speculative, there is substantial evidence for the opposing condition where elevation of inflammatory signaling is well known to promote depression in humans and depression-like behavior in animal models (Painsipp et al., 2011, Fu et al., 2010, Dantzer et al., 2011).
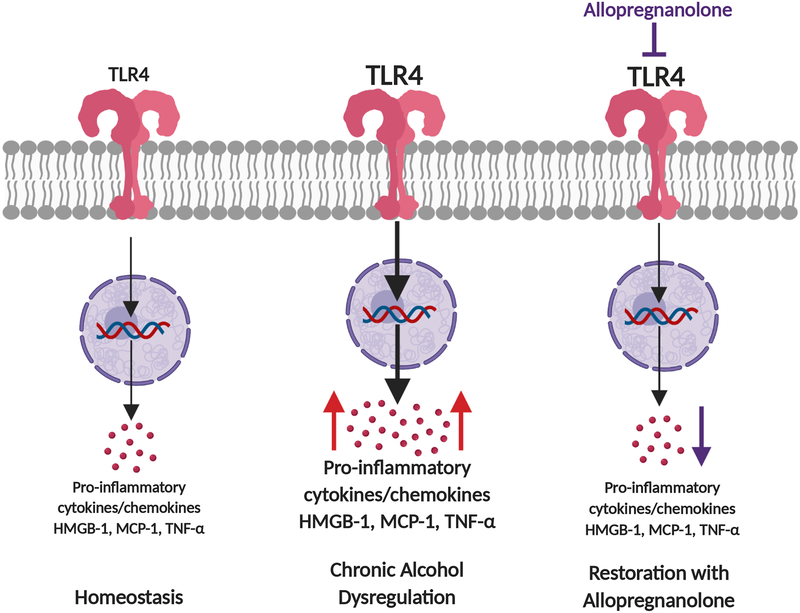
In summary, several lines of evidence suggest that ability of allopregnanolone and pregnenolone to inhibit TLR activation in the immune system and the brain may be linked to their therapeutic actions in neuropsychiatric conditions that involve inflammatory signaling. AUD represents a systemic disease that involves many organs which exhibit inflammation arising from the gut to the blood stream, then to the organs, including brain. The innate immune system plays a key role in this process and neuroactive steroids may be a critical factor that moderates the pathological effects of alcohol on inflammation that contribute to AUDs. Figure 3 illustrates the theoretical application of this idea.
Figure 3. Restoration of TLR pathway dysregulation due to chronic alcohol exposure.
TLR4 activation is increased by chronic alcohol abuse, causing the increase of pro-inflammatory cytokines/chemokines, such as HMGB-1, MCP-1 and TNF-α. Allopregnanolone restores homeostasis by blocking TLR4 activation to inhibit the production of the pro-inflammatory cytokines/chemokines MCP-1, HMGB-1 and TNF-α. Created using BioRender.com.
IV. Allopregnanolone and/or pregnenolone may protect individuals from developing alcohol addiction and may have therapeutic potential for treatment of AUDs
Neuroactive steroids might represent a useful therapeutic approach to restore deficits in GABAergic inhibition, dysregulation of CRF signaling and excessive neuroimmune activation that are apparent in patients with AUDs. This argument is supported by data from animal models of alcohol addiction and effects of neuroactive steroids in other conditions that involve the loss of inhibitory control in the CNS. Some examples are described.
a. Evidence that neuroactive steroids are dysregulated in alcohol addiction
Endogenous neuroactive steroid levels are altered by alcohol exposure, with effects that depend on length of exposure and that differ across species, sex and brain regions examined. Acute ethanol exposure at relatively high doses increases neuroactive steroids in rats, in some mouse strains, and in human adolescents admitted to the emergency room due to alcohol intoxication. By contrast, no changes or a decrease in allopregnanolone levels were observed in monkeys and in healthy subjects who consumed low (0.2 g/kg) or moderate (0.8 g/kg) ethanol doses (see (Morrow et al., 2006), (Porcu et al., 2010, Porcu et al., 2019), for review).
In contrast to effects of acute exposure, chronic ethanol consumption often depletes neuroactive steroid concentrations, but there are also species, sex and regional differences. Ethanol-dependent male, but not female rats, have decreased basal cerebrocortical and hippocampal allopregnanolone levels (Janis et al., 1998, Cagetti et al., 2004, Morrow et al., 2006), and there is a blunted elevation of cerebrocortical allopregnanolone, and of plasma and brain deoxycorticosterone levels in male rats following an acute ethanol challenge (Khisti et al., 2005, Morrow et al., 2006), suggesting tolerance to the ethanol-induced increase in neuroactive steroid levels. In mice, chronic alcohol exposure differentially affects GABAergic neuroactive steroids, depending on strain, sex, and brain regions examined (Finn et al., 2010, Porcu and Morrow, 2014, Snelling et al., 2014). Increased allopregnanolone levels were reported in whole brain from male, but not female, C57BL/6J mice, following voluntary ethanol consumption (Finn et al., 2010). By contrast, chronic intermittent ethanol exposure and subsequent withdrawal in male C57BL/6J mice decreased allopregnanolone immunoreactivity in the lateral amygdala and VTA (Maldonado-Devincci et al., 2014). Furthermore, repeated binge ethanol exposure in male and female C57BL/6J mice differentially alters NAc expression of steroidogenic acute regulatory protein and CRF signaling pathways (Finn et al., 2018), both implicated in promoting neurosteroidogenesis. In cynomolgus monkeys, serum allopregnanolone levels following prolonged voluntary ethanol self-administration in males show a depletion of allopregnanolone (Beattie et al., 2017). Moreover, allopregnanolone immunoreactivity in the lateral and basolateral amygdala was reduced following twelve-months of voluntary alcohol self-administration, the decrease was inversely related to daily ethanol intake, and more pronounced in heavy drinkers (Beattie et al., 2017). However, in the same subjects allopregnanolone immunoreactivity in the hippocampus was slightly enhanced (Beattie et al., 2018), suggesting that chronic alcohol may selectively dysregulate GABAergic neuroactive steroids across brain regions. Likewise, increased allopregnanolone immunoreactivity was reported in the VTA and substantia nigra pars medialis of male human alcoholics (Hasirci et al., 2017). Furthermore, the neuroactive steroid precursors pregnenolone and dehydroepiandrosterone were elevated in several limbic regions of alcohol-dependent male and female subjects (Karkkainen et al., 2016). Studies of both male and female subjects are lacking in many of the reports described here, therefore additional studies comparing results in both sexes are needed.
Nonetheless, it should be noted that both male and female human alcoholics have reduced circulating levels of progesterone, allopregnanolone and 3α,5α-THDOC during withdrawal, which normalized upon recovery (Hill et al., 2005, Romeo et al., 1996). Moreover, male alcohol-dependent subjects had a delayed deoxycorticosterone response to CRF challenge (Porcu et al., 2008), a likely consequence of the blunted HPA axis in response to chronic alcohol exposure (Porcu and Morrow, 2014). Overall, GABAergic neuroactive steroids appear dysregulated in AUDs; whether this dysregulation is pre-existent to, or is the consequence of, alcohol exposure is at present still unclear.
b. Neuroactive steroids reduce ethanol consumption in alcohol-preferring P rats
P rats exhibit innate activation of TLR4 signaling in the VTA, NAc and CeA that is not observed in NP rats or wild type Wistar rats (Liu et al., 2011, June et al., 2015, Balan et al., 2018). GABAergic neuroactive steroids affect ethanol consumption in P rats, but not in other rat and mouse strains (see Section V). Allopregnanolone reduced ethanol consumption in dependent alcohol-preferring P rats (Morrow et al., 2001). Likewise, administration of the neuroactive steroid precursor pregnenolone, or the endogenous (3β,5β-THP or epiallopregnanolone) or synthetic (3α,5β−20-oxo-pregnane-3-carboxylic acid) neuroactive steroids, also decreased ethanol self-administration in male alcohol-preferring P rats (O’Dell et al., 2005, Besheer et al., 2010), suggesting that neuroactive steroids may protect against excessive drinking in this selectively bred strain of rats. This hypothesis was further tested by enhancement of neuroactive steroid biosynthesis with over-expression of P450scc, the rate limiting enzyme in steroid synthesis. Recombinant adeno-associated serotype-2-vector-mediated over-expression of P450scc in the VTA of alcohol-preferring P male rats lead to a long-lasting decrease in ethanol reinforcement and consumption, and to a concomitant increase in allopregnanolone immunoreactivity in this area (Cook et al., 2014). Hence, targeted enhancement of allopregnanolone levels by its direct administration, administration of the steroid precursors or through increased expression of specific neurosteroidogenic enzymes may represent a useful therapeutic approach for AUDs.
c. Individual differences in allopregnanolone levels are related to ethanol consumption
Individual differences in vulnerability to alcoholism have a genetic component (Schuckit, 2009, Reilly et al., 2017), and studies in rodents suggested a shared genetic sensitivity to ethanol, anxiety and stress/HPA axis response (Boehm et al., 2002). We hypothesized that a similar relationship may exist for basal and ethanol-induced levels of GABAergic neuroactive steroids. In selected BXD male mouse strains, we found that basal cerebral cortical allopregnanolone levels across strains ranged between 1.8 and 3.7 ng/g (resulting in a 2-fold genetic variation), while following acute ethanol administration changes in allopregnanolone levels ranged between +4% and +63% (Porcu and Morrow, 2014). Moreover, http://www.genenetwork.org/both basal and ethanol-induced cerebral cortical allopregnanolone levels were negatively correlated with phenotypes of ethanol consumption; thus, those strains with increased allopregnanolone levels in response to acute ethanol consumed less alcohol. This preliminary finding, obtained in just a few strains, supports the hypothesis that neuroactive steroid responses to ethanol may predict excessive alcohol consumption (Morrow et al., 2006, Porcu and Morrow, 2014). We further identified significant genetic variation in serum levels of allopregnanolone, 3α,5α-THDOC, and their precursor pregnenolone in male and females from 19 BXD strains subjected to chronic intermittent ethanol exposure. Variation in neuroactive steroid levels was linked to several behavioral phenotypes of anxiety, previously determined in these strains, consistent with the fact that neuroactive steroids modulate anxiety-like behavior. Moreover, individual variation in allopregnanolone levels was negatively correlated to ethanol consumption in male and female, control and CIE-exposed strains; that is, those strains with lower allopregnanolone levels were the ones who consumed more alcohol. This effect was not observed for 3α,5α-THDOC or pregnenolone levels, thus it appears to be specific to allopregnanolone (Porcu et al., 2017).
V. Cautions and limitations of neuroactive steroid therapeutics for AUDs
Considering the plethora of evidence for neuroactive steroid actions that might serve to support the recovery from AUDs, it is surprising that human laboratory and clinical studies have not been conducted using neuroactive steroids or their precursors. Caution has prevailed due to the perception that GABAergic neuroactive steroids are comparable to benzodiazepines, despite the fact that the actions of neuroactive steroids are clearly distinct from benzodiazepines as described in Section 1. Even among researchers, however, there have been controversies regarding their risks and potential for use in human disease. One compelling issue has been the lack of data in females across many human and animal studies of the etiologies of AUDs. Emerging studies have revealed remarkable sex differences in human responses to drugs in many neuropsychiatric conditions (Rainville et al., 2018) and therefore, the lack of data in females may lead to misleading conclusions. Here we address the issues that are most compelling and propose a rational approach to the introduction of neuroactive steroid therapy for AUDs.
a. Neuroactive steroids may increase ethanol reinforcement, consumption and reinstatement of drinking in animal models
Neuroactive steroids influence ethanol reinforcement and consumption in rodents, and under certain conditions may increase, rather than suppress, drinking. For instance, while allopregnanolone decreased reinforcement and consumption in dependent alcohol-preferring P male rats, as described above, it increased ethanol-reinforced operant responding in non-dependent male Long-Evans rats (Janak et al., 1998). Likewise, ganaxolone at low doses (1 mg/kg) increased, while at high doses (30 mg/kg) decreased ethanol-reinforced responding in alcohol-preferring P male rats (Besheer et al., 2010). A similar biphasic effect of neuroactive steroids was reported in male C57BL/6J mice, where allopregnanolone administration at low doses (3.2 mg/kg) increases ethanol self-administration in a limited access paradigm, while at high doses (24 mg/kg) it decreases consumption in a two-bottle drinking paradigm (Ford et al., 2005). Similar results were observed with ganaxolone administration to mice (Ramaker et al., 2011, Ramaker et al., 2012). In the same strain, both allopregnanolone and ganaxolone also reinstate ethanol seeking behavior (Finn et al., 2010, Ramaker et al., 2014). Further, modulation of drinking behavior by allopregnanolone appears to be sex-dependent; in fact, female C57BL/6J mice are insensitive to allopregnanolone modulation of ethanol intake (Finn et al., 2010).
Taken together, these results suggest that neuroactive steroids may not be an effective treatment for AUD patients or may enhance consumption in some subjects. This conclusion presumes that our animal models of alcohol abuse are representative of effects in humans. We argue this idea is not supported by the literature in several cases where compounds that were highly effective in animal models of alcohol consumption (CRF antagonists / Varenicline) failed to prove effective in human disease (Shaham and de Wit, 2016, de Bejczy et al., 2015). Human studies with allopregnanolone, progesterone and pregnenolone will be needed to address this concern.
b. Neuroactive steroid interactions with ethanol may lead to untoward effects including allopregnanolone dependence and/or addiction
It is well known that GABAergic neuroactive steroids can interact with ethanol in ways that might be deleterious, such as when driving or operating machinery. Since AUDs are chronic and characterized by the loss of control of one’s behavior as well as the tendency to relapse, the concern over these potential interactions is understandable and might be fully justified. Alternatively, it is possible that AUD patients may have different responses to allopregnanolone and/or pregnenolone compared to average healthy subjects. This might occur since AUD patients are suffering from deficient GABAergic transmission, CRF regulation and inflammatory neuroimmune overactivity. In this case, the administration of the neuroactive steroids may normalize biological function and interactions with ethanol would not be unmanageable. In diabetes for example, the administration of insulin normalizes metabolic function rather than causing excess energy production that would be detrimental in normal healthy control subjects. In every clinical trial reported to date with allopregnanolone or pregnenolone for neuropsychiatric conditions, there were no serious adverse effects in the male or female patients (vide supra). Nonetheless, until we know more about neuroactive steroid effects in patients with AUDs, trials could be limited to intravenous infusions of allopregnanolone in a medically supervised setting, drug interactions could be tested in laboratory settings and oral treatments could be given for short periods to assess patient responses.
The rapid and long lasting antidepressant effect of Brexanolone in female patients with postpartum depression (Meltzer-Brody et al., 2018) suggests that allopregnanolone therapy might be useful during detoxification and might last up to a month or longer such that other treatments such as cognitive behavioral therapies could have a greater impact. Neuroactive steroid therapy might be considered like other anti-inflammatory therapies that are administered once monthly to control inflammatory conditions, such as the TNF-α antagonist, Remicade.
Other animal studies have suggested that progesterone withdrawal and therefore by analogy, withdrawal from allopregnanolone can lead to anxiety, GABAA receptor dysregulation and dysfunction (Costa et al., 1995, Smith et al., 1998, Moran and Smith, 1998, Moran et al., 1998). The data suggests a danger from rapid allopregnanolone withdrawal in human subjects as well. Again, this clinical concern has not borne out in any of the clinical studies conducted to date. Nonetheless, withdrawal signs should be monitored and prevented by gradual tapering if therapy is discontinued. However, therapy for chronic AUD may be life-long, as in the case of cardiovascular disease, diabetes and many other chronic conditions.
VI. Final conclusion
We have previously suggested that allopregnanolone may be a protective factor in normal healthy controls that helps to prevent the development of AUDs (Morrow, 2007). It is an endogenous factor that helps to maintain normal CNS inhibition, behavioral control, HPA axis homeostasis and prevents the activation of neuroimmune signaling through TLR4 receptors that initiate systemic inflammatory responses and excessive brain excitability. Both acute stress and acute ethanol exposure increase allopregnanolone levels in circulation along with endotoxin, and cortisol/corticosterone. The concurrent production of allopregnanolone may help to ensure the return to hypothalamic and extrahypothalamic CRF and HPA axis homeostasis and prevent the activation of TLR signaling and thus the production of pro-inflammatory molecules. This is a healthy response to alcohol and stress, and it may explain why most people can manage the stress of life and moderate alcohol consumption without issues.
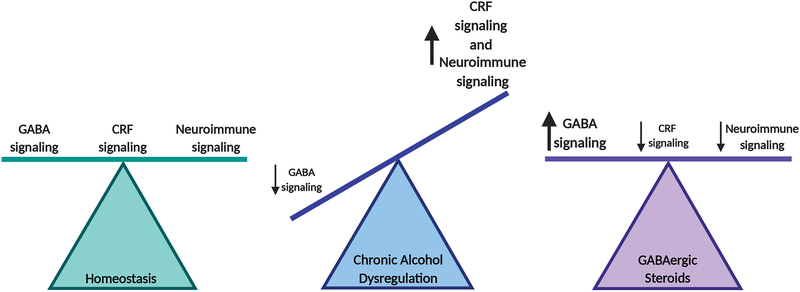
With chronic excessive stress or chronic ethanol administration or both situations, the neuroactive steroids are often depleted in serum and/or brain, HPA axis and CRF dysregulation ensue, GABAA receptor function is dysregulated and markers of neuroinflammation are found. In addition, there is tolerance to the effects of acute alcohol or stress challenge on the production of allopregnanolone. At this point, behavioral manifestations of alcohol dependence are prominent with anxiety, dysphoria and alcohol craving to relieve the symptoms of the adaptations caused by chronic exposure to stress and/or alcohol exposure. Binge levels of alcohol consumption exacerbates these effects and repeated withdrawals from ethanol also enhance the duration or severity of these adaptations (Olsen and Liang, 2017, Breese and Knapp, 2016). Figure 4 illustrates the hypothesis that allopregnanolone can restore homeostasis of GABA inhibition, CRF signaling, and neuroimmune activation following chronic ethanol exposure.
Figure 4. Theoretical framework of the dysregulation caused by chronic alcohol abuse and restoration of homeostasis by GABAergic neuroactive steroids.
Chronic alcohol exposure decreases GABAergic signaling while increasing CRF and neuroimmune signaling. Neuroactive steroids may restore homeostasis by increasing GABAA receptor-mediated inhibition, and decreasing CRF and deleterious neuroimmune signaling, all of which contribute to the etiology of AUDs. Created using BioRender.com.
Some people can overcome these adaptations and return to health, but many are not so fortunate. Here we propose that inadequate neuroactive steroid regulation of GABAergic function, CRF production and neuroimmune signaling contributes to the disorder and therefore, patients with AUDs would respond to treatment with allopregnanolone or its precursors in a favorable manner. Pregnenolone is a nutritional supplement that is available from many sources that manufacture under GMP guidelines including independent testing of purity. Progesterone is an FDA-approved compound for various conditions, that shows promise for reducing drug craving in men and women. Brexanolone is now FDA approved for the treatment of postpartum depression and could be tested for AUDs or prescribed under the appropriate conditions. Studies are warranted to investigate the clinical efficacy of these neurosteroids and to compare their respective effects in AUDs.
FUNDING AND DISCLOSURES:
This critical review was supported by the NIAAA-R01-AA024095 (ALM), and the UNC Bowles Center for Alcohol Studies.
A. L. Morrow has filed a worldwide patent on the use of allopregnanolone and pregnenolone as anti-inflammatory agents for inflammatory conditions.
References
- Abrahao KP, Salinas AG, Lovinger DM (2017) Alcohol and the Brain: Neuronal Molecular Targets, Synapses, and Circuits. Neuron 96:1223–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adinoff B, Junghanns K, Kiefer F, Krishnan-Sarin S (2005a) Suppression of the HPA axis stress-response: implications for relapse. Alcohol Clin Exp Res 29:1351–1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adinoff B, Krebaum SR, Chandler PA, Ye W, Brown MB, Williams MJ (2005b) Dissection of hypothalamic-pituitary-adrenal axis pathology in 1-month-abstinent alcohol-dependent men, part 1: adrenocortical and pituitary glucocorticoid responsiveness. Alcohol. Clin. Exp. Res 29:517–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adinoff B, Krebaum SR, Chandler PA, Ye W, Brown MB, Williams MJ (2005c) Dissection of hypothalamic-pituitary-adrenal axis pathology in 1-month-abstinent alcohol-dependent men, part 2: response to ovine corticotropin-releasing factor and naloxone. Alcohol. Clin. Exp. Res 29:528–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adinoff B, Martin PR, Bone GH, Eckardt MJ, Roehrich L, George DT, Moss HB, Eskay R, Linnoila M, Gold PW (1990) Hypothalamic-pituitary-adrenal axis functioning and cerebrospinal fluid corticotropin releasing hormone and corticotropin levels in alcoholics after recent and long-term abstinence. Arch. Gen. Psychiatry 47:325–330. [DOI] [PubMed] [Google Scholar]
- Agoglia AE, Herman MA (2018) The center of the emotional universe: Alcohol, stress, and CRF1 amygdala circuitry. Alcohol 72:61–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal RG, Owen JA, Levin PS, Hewetson A, Berman AE, Franklin SR, Hogue RJ, Chen Y, Walz C, Colvard BD, Nguyen J, Velasquez O, Al-Hasan Y, Blednov YA, Fowler AK, Syapin PJ, Bergeson SE (2014) Bioinformatics analyses reveal age-specific neuroimmune modulation as a target for treatment of high ethanol drinking. Alcohol Clin Exp Res 38:428–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfonso-Loeches S, Pascual-Lucas M, Blanco AM, Sanchez-Vera I, Guerri C (2010) Pivotal role of TLR4 receptors in alcohol-induced neuroinflammation and brain damage. J Neurosci 30:8285–8295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arora DS, Nimitvilai S, Teppen TL, McElvain MA, Sakharkar AJ, You C, Pandey SC, Brodie MS (2013) Hyposensitivity to gamma-aminobutyric acid in the ventral tegmental area during alcohol withdrawal: reversal by histone deacetylase inhibitors. Neuropsychopharmacology 38:1674–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aurelian L, Balan I (2019) GABAAR alpha2-activated neuroimmune signal controls binge drinking and impulsivity through regulation of the CCL2/CX3CL1 balance. Psychopharmacology (Berl) 236:3023–3043. [DOI] [PubMed] [Google Scholar]
- Balan I, Beattie MC, O’Buckley TK, Aurelian L, Morrow AL (2019a) Endogenous Neurosteroid (3⍺,5⍺)3-Hydroxypregnan-20-one Inhibits Toll-like-4 Receptor Activation and Pro-inflammatory Signaling in Macrophages and Brain. Sci Rep 9:1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balan I, O’Buckley TK, Schleicher R, Boero G, Aurelian LA, Morrow AL. The endogenous neurosteroid (3α,5α)3-hydroxypregnan-20-one (3α,5α-THP) inhibits pro-inflammatory toll-like receptor (TLR)-MyD88-dependent signaling in immune cells and brain online]. Program No. 675.04. 2019 Neuroscience Meeting Planner. Chicago, IL: Society for Neuroscience, 2019. Online. [Google Scholar]
- Balan I, Warnock KT, Puche A, Gondre-Lewis MC, Aurelian L (2018) Innately activated TLR4 signal in the nucleus accumbens is sustained by CRF amplification loop and regulates impulsivity. Brain Behav Immun 69:139–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bangasser DA, Valentino RJ (2014) Sex differences in stress-related psychiatric disorders: neurobiological perspectives. Front Neuroendocrinol 35:303–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumeister D, Lightman SL, Pariante CM (2014) The Interface of Stress and the HPA Axis in Behavioural Phenotypes of Mental Illness. Curr Top Behav Neurosci 18:13–24. [DOI] [PubMed] [Google Scholar]
- Beattie MC, Maldonado-Devincci AM, Porcu P, O’Buckley TK, Daunais JB, Grant KA, Morrow AL (2017) Voluntary ethanol consumption reduces GABAergic neuroactive steroid (3α,5α)3-hydroxypregnan-20-one (3α,5α-THP) in the amygdala of the cynomolgus monkey. Addict Biol 22:318–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beattie MC, Reguyal CS, Porcu P, Daunais JB, Grant KA, Morrow AL (2018) Neuroactive Steroid (3⍺,5⍺)3-hydroxypregnan-20-one (3⍺,5⍺-THP) and Pro-inflammatory Cytokine MCP-1 Levels in Hippocampus CA1 are Correlated with Voluntary Ethanol Consumption in Cynomolgus Monkey. Alcohol Clin Exp Res 42:12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behar KL, Rothman DL, Petersen KF, Hooten M, Delaney R, Petroff OAC, Shulman GI, Navarro V, Petrakis IL, Charney DS, Krystal JH (1999) Preliminary Evidence of Low Cortical GABA Levels in Localized1H-MR Spectra of Alcohol-Dependent and Hepatic Encephalopathy Patients. American Journal of Psychiatry 156:952–954. [DOI] [PubMed] [Google Scholar]
- Belelli D, Casula A, Ling A, Lambert JJ (2002) The influence of subunit composition on the interaction of neurosteroids with GABAA receptors. Neuropharmacology 43:651–661. [DOI] [PubMed] [Google Scholar]
- Belelli D, Lambert JJ (2005) Neurosteroids: endogenous regulators of the GABAA receptor. Nat Rev Neurosci 6:565–575. [DOI] [PubMed] [Google Scholar]
- Bell RL, Rodd ZA, Lumeng L, Murphy JM, McBride WJ (2006) The alcohol-preferring P rat and animal models of excessive alcohol drinking. Addict Biol 11:270–288. [DOI] [PubMed] [Google Scholar]
- Besheer J, Lindsay TG, O’Buckley TK, Hodge CW, Morrow AL (2010) Pregnenolone and ganaxolone reduce operant ethanol self-administration in alcohol-preferring P rats. Alcohol Clin Exp Res 34:2044–2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhattacharya A, Derecki NC, Lovenberg TW, Drevets WC (2016) Role of neuro-immunological factors in the pathophysiology of mood disorders. Psychopharmacology (Berl) 233:1623–1636. [DOI] [PubMed] [Google Scholar]
- Biggio G, Concas A, Follesa P, Sanna E, Serra M (2007) Stress, ethanol, and neuroactive steroids. Pharmacol Ther 116:140–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biggio G, Pisu MG, Biggio F, Serra M (2014) Allopregnanolone modulation of HPA axis function in the adult rat. Psychopharmacology (Berl) 231:3437–3444. [DOI] [PubMed] [Google Scholar]
- Bitran D, Hilvers RJ, Kellogg CK (1991) Anxiolytic effects of 3⍺-hydroxy-5⍺[ß]-pregnan-20-one: Endogenous metabolites of progesterone that are active at the GABAA receptor. Brain Res 561:157–161. [DOI] [PubMed] [Google Scholar]
- Bixo M, Andersson A, Winblad B, Purdy RH, Backstrom T (1997) Progesterone, 5⍺-pregnan-3,20-dione and 3⍺-hydroxy-5⍺-pregnane-20-one in specific regions of the human female brain in different endocrine states. Brain Res 764:173–178. [DOI] [PubMed] [Google Scholar]
- Blaine SK, Nautiyal N, Hart R, Guarnaccia JB, Sinha R (2019) Craving, cortisol and behavioral alcohol motivation responses to stress and alcohol cue contexts and discrete cues in binge and non-binge drinkers. Addict Biol 24:1096–1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blednov YA, Benavidez JM, Geil C, Perra S, Morikawa H, Harris RA (2011) Activation of inflammatory signaling by lipopolysaccharide produces a prolonged increase of voluntary alcohol intake in mice. Brain Behav Immun 25 Suppl 1:S92–S105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehm SL 2nd, Reed CL, McKinnon CS, Phillips TJ (2002) Shared genes influence sensitivity to the effects of ethanol on locomotor and anxiety-like behaviors, and the stress axis. Psychopharmacology (Berl) 161:54–63. [DOI] [PubMed] [Google Scholar]
- Boero G, Pisu MG, Biggio F, Muredda L, Carta G, Banni S, Paci E, Follesa P, Concas A, Porcu P, Serra M (2018) Impaired glucocorticoid-mediated HPA axis negative feedback induced by juvenile social isolation in male rats. Neuropharmacology 133:242–253. [DOI] [PubMed] [Google Scholar]
- Bohnsack JP, Hughes BA, O’Buckley TK, Edokpolor K, Besheer J, Morrow AL (2018) Histone deacetylases mediate GABAA receptor expression, physiology, and behavioral maladaptations in rat models of alcohol dependence. Neuropsychopharmacology 43:1518–1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breese GR, Knapp DJ (2016) Persistent adaptation by chronic alcohol is facilitated by neuroimmune activation linked to stress and CRF. Alcohol 52:9–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breese GR, Sinha R, Heilig M (2011) Chronic alcohol neuroadaptation and stress contribute to susceptibility for alcohol craving and relapse. Pharmacol Ther 129:149–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bremner JD, Licinio J, Darnell A, Krystal JH, Owens MJ, Southwick SM, Nemeroff CB, Charney DS (1997) Elevated CSF corticotropin-releasing factor concentrations in posttraumatic stress disorder. Am J Psychiatry 154:624–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brinton RD (2013) Neurosteroids as regenerative agents in the brain: therapeutic implications. Nat Rev Endocrinol 9:241–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broomall E, Natale JE, Grimason M, Goldstein J, Smith CM, Chang C, Kanes S, Rogawski MA, Wainwright MS (2014) Pediatric super-refractory status epilepticus treated with allopregnanolone. Ann Neurol 76:911–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cagetti E, Pinna G, Guidotti A, Baicy K, Olsen RW (2004) Chronic intermittent ethanol (CIE) administration in rats decreases levels of neurosteroids in hippocampus, accompanied by altered behavioral responses to neurosteroids and memory function. Neuropharmacology 46:570–579. [DOI] [PubMed] [Google Scholar]
- Carlson SL, Bohnsack JP, Patel V, Morrow AL (2016) Regulation of extrasynaptic GABAA alpha4 receptors by ethanol-induced protein kinase A, but not protein kinase C activation in cultured rat cerebral cortical neurons. J Pharmacol Exp Ther 356:148–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CM, Reddy DS (2013) Neurosteroid interactions with synaptic and extrasynaptic GABA(A) receptors: regulation of subunit plasticity, phasic and tonic inhibition, and neuronal network excitability. Psychopharmacology 230:151–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CM, Wu X, Gangisetty O, Reddy DS (2014) Perimenstrual-like hormonal regulation of extrasynaptic delta-containing GABAA receptors mediating tonic inhibition and neurosteroid sensitivity. J Neurosci 34:14181–14197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro-Vale I, van Rossum EF, Machado JC, Mota-Cardoso R, Carvalho D (2016) Genetics of glucocorticoid regulation and posttraumatic stress disorder--What do we know? Neurosci Biobehav Rev 63:143–157. [DOI] [PubMed] [Google Scholar]
- Chandra D, Jia F, Liang J, Peng Z, Suryanarayanan A, Werner DF, Spigelman I, Houser CR, Olsen RW, Harrison NL, Homanics GE (2006) GABAA receptor ⍺4 subunits mediate extrasynaptic inhibition in thalamus and dentate gyrus and the action of gaboxadol. Proc Natl Acad Sci U S A 103:15230–15235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman LG Jr., Zou J, Crews FT (2017) Microglial-derived miRNA let-7 and HMGB1 contribute to ethanol-induced neurotoxicity via TLR7. J Neuroinflammation 14:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman LG Jr., Zou J, Qin L, Crews FT (2018) HMGB1/IL-1beta complexes regulate neuroimmune responses in alcoholism. Brain Behav Immun 72:61–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook JB, Werner DF, Maldonado-Devincci AM, Leonard MN, Fisher KR, O’Buckley TK, Porcu P, McCown TJ, Besheer J, Hodge CW, Morrow AL (2014) Overexpression of the steroidogenic enzyme cytochrome P450 side chain cleavage in the ventral tegmental area increases 3alpha,5alpha-THP and reduces long-term operant ethanol self-administration. J Neurosci 34:5824–5834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corwin EJ, Johnston N, Pugh L (2008) Symptoms of postpartum depression associated with elevated levels of interleukin-1 beta during the first month postpartum. Biol Res Nurs 10:128–133. [DOI] [PubMed] [Google Scholar]
- Costa AM, Spence KT, Smith SS, ffRench-Mullen J (1995) Withdrawal from the endogenous steroid progesterone results in GABAA currents insensitive to benzodiazepine modulation in rat CA1 hippocampus. Journal of Neurophysiology 74:464–469. [DOI] [PubMed] [Google Scholar]
- Crawley JN, Glowa JR, Majewska MD, Paul SM (1986) Anxiolytic activity of an endogenous adrenal steroid. Brain Res 398:382–385. [DOI] [PubMed] [Google Scholar]
- Crews F, Morrow AL, Criswell H, Breese G (1996) Effects of Ethanol on Ion Channels, in International Review of Neurobiology, Vol 39, International Review of Neurobiology, Vol 39 (BRADLEY RJ, HARRIS RAeds), pp 283–367, Academic Press, New York. [DOI] [PubMed] [Google Scholar]
- Crews FT, Lawrimore CJ, Walter TJ, Coleman LG Jr. (2017a) The role of neuroimmune signaling in alcoholism. Neuropharmacology 122:56–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crews FT, Vetreno RP (2016) Mechanisms of neuroimmune gene induction in alcoholism. Psychopharmacology (Berl) 233:1543–1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crews FT, Walter TJ, Coleman LG Jr., Vetreno RP (2017b) Toll-like receptor signaling and stages of addiction. Psychopharmacology (Berl) 234:1483–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croarkin PE, Levinson AJ, Daskalakis ZJ (2011) Evidence for GABAergic inhibitory deficits in major depressive disorder. Neurosci Biobehav Rev 35:818–825. [DOI] [PubMed] [Google Scholar]
- Crowley SK, O’Buckley TK, Schiller CE, Stuebe A, Morrow AL, Girdler SS (2016) Blunted neuroactive steroid and HPA axis responses to stress are associated with reduced sleep quality and negative affect in pregnancy: a pilot study. Psychopharmacology (Berl) 233:1299–1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullinan WE, Ziegler DR, Herman JP (2008) Functional role of local GABAergic influences on the HPA axis. Brain Struct Funct 213:63–72. [DOI] [PubMed] [Google Scholar]
- Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW (2008) From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci 9:46–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dantzer R, O’Connor JC, Lawson MA, Kelley KW (2011) Inflammation-associated depression: from serotonin to kynurenine. Psychoneuroendocrinology 36:426–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bejczy A, Lof E, Walther L, Guterstam J, Hammarberg A, Asanovska G, Franck J, Isaksson A, Soderpalm B (2015) Varenicline for treatment of alcohol dependence: a randomized, placebo-controlled trial. Alcohol Clin Exp Res 39:2189–2199. [DOI] [PubMed] [Google Scholar]
- de Guglielmo G, Kallupi M, Pomrenze MB, Crawford E, Simpson S, Schweitzer P, Koob GF, Messing RO, George O (2019) Inactivation of a CRF-dependent amygdalofugal pathway reverses addiction-like behaviors in alcohol-dependent rats. Nat Commun 10:1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devaud LL, Fritschy J-M, Morrow AL (1998) Influence of gender on chronic ethanol-induced alternations of GABAA receptors in rats. Brain Res 796:222–230. [DOI] [PubMed] [Google Scholar]
- Devaud LL, Purdy RH, Finn DA, Morrow AL (1996) Sensitization of gamma-aminobutyric acidA receptors to neuroactive steroids in rats during ethanol withdrawal. J Pharmacol Exp Ther 278:510–517. [PubMed] [Google Scholar]
- Devaud LL, Purdy RH, Morrow AL (1995) The neurosteroid, 3α-hydroxy-5α-pregnan-20-one, protects against bicuculline-induced seizures during ethanol withdrawal in rats. Alcohol Clin Exp Res 19:350–355. [DOI] [PubMed] [Google Scholar]
- Dodd PR, Buckley ST, Eckert AL, Foley PF, Innes DJ (2006) Genes and gene expression in the brains of human alcoholics. Ann N Y Acad Sci 1074:104–115. [DOI] [PubMed] [Google Scholar]
- Dong E, Matsumoto K., Uzunova V., Sugaya I. Takahata H., Nomura H., Watanabe H., Costa E., Guidotti A., (2001) Brain 5-alpha-dihydroprogesterone and allopregnanolone synthesis in a mouse model of protracted social isolation. Proc Natl Acad Sci U S A 98:2849–2854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egli M, Koob GF, Edwards S (2012) Alcohol dependence as a chronic pain disorder. Neurosci Biobehav Rev 36:2179–2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans J, Sun Y, McGregor A, Connor B (2012) Allopregnanolone regulates neurogenesis and depressive/anxiety-like behaviour in a social isolation rodent model of chronic stress. Neuropharmacology 63:1315–1326. [DOI] [PubMed] [Google Scholar]
- Ferguson AR, Christensen RN, Gensel JC, Miller BA, Sun F, Beattie EC, Bresnahan JC, Beattie MS (2008) Cell death after spinal cord injury is exacerbated by rapid TNF alpha-induced trafficking of GluR2-lacking AMPARs to the plasma membrane. J Neurosci 28:11391–11400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez-Lizarbe S, Montesinos J, Guerri C (2013) Ethanol induces TLR4/TLR2 association, triggering an inflammatory response in microglial cells. J Neurochem 126:261–273. [DOI] [PubMed] [Google Scholar]
- Finn DA, Beckley EH, Kaufman KR, Ford MM (2010) Manipulation of GABAergic steroids: Sex differences in the effects on alcohol drinking- and withdrawal-related behaviors. Horm Behav 57:12–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finn DA, Hashimoto JG, Cozzoli DK, Helms ML, Nipper MA, Kaufman MN, Wiren KM, Guizzetti M (2018) Binge Ethanol Drinking Produces Sexually Divergent and Distinct Changes in Nucleus Accumbens Signaling Cascades and Pathways in Adult C57BL/6J Mice. Front Genet 9:325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finn DA, Roberts AJ, Crabbe JC (1995) Neuroactive steroid sensitivity in withdrawal seizure-prone and -resistant mice. Alcohol Clin Exp Res 18:410–415. [DOI] [PubMed] [Google Scholar]
- Ford MM, Nickel JD, Phillips TJ, Finn DA (2005) Neurosteroid modulators of GABAA receptors differentially modulate ethanol intake patterns in male C57BL/6J mice. Alcohol Clin Exp Res 29:1630–1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox HC, Sofuoglu M, Morgan PT, Tuit KL, Sinha R (2013) The effects of exogenous progesterone on drug craving and stress arousal in cocaine dependence: impact of gender and cue type. Psychoneuroendocrinology 38:1532–1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu X, Zunich SM, O’Connor JC, Kavelaars A, Dantzer R, Kelley KW (2010) Central administration of lipopolysaccharide induces depressive-like behavior in vivo and activates brain indoleamine 2,3 dioxygenase in murine organotypic hippocampal slice cultures. J Neuroinflammation 7:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallager DW, Lakoski JM, Gonsalves SF, Rauch SL (1984) Chronic benzodiazepine treatment decreases postsynaptic GABA sensitivity. Nature (Lond) 308:74–77. [DOI] [PubMed] [Google Scholar]
- Garbutt JC, West SL, Carey TS, Lohr KN, Crews FT (1999) Pharmacological treatment of ethanol dependence: a review of the evidence. JAMA 281:1318–1325. [DOI] [PubMed] [Google Scholar]
- Girdler SS, Klatzkin R (2007) Neurosteroids in the context of stress: implications for depressive disorders. Pharmacol. Ther 116:125–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girdler SS, Lindgren M, Porcu P, Rubinow DR, Johnson JL, Morrow AL (2012) A history of depression in women is associated with an altered GABAergic neuroactive steroid profile. Psychoneuroendocrinology 37:543–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez SL, Meyer L, Raggio MC, Taleb O, Coronel MF, Patte-Mensah C, Mensah-Nyagan AG (2019) Allopregnanolone and Progesterone in Experimental Neuropathic Pain: Former and New Insights with a Translational Perspective. Cell Mol Neurobiol 39:523–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodkin HP, Joshi S, Mtchedlishvili Z, Brar J, Kapur J (2008) Subunit-specific trafficking of GABA(A) receptors during status epilepticus. J Neurosci 28:2527–2538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin LD, Mellon SH (1999) Selective serotonin reuptake inhibitors directly alter activity of neurosteroidogenic enzymes. Proc Natl Acad Sci USA 96:13512–13517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grobin AC, Matthews DB, Devaud LL, Morrow AL (1998) The role of GABAA receptors in the acute and chronic effects of ethanol. Psychopharmacology 139:2–19. [DOI] [PubMed] [Google Scholar]
- Gruol DL (2013) Neuroimmune regulation of neurophysiology in the cerebellum. Cerebellum 12:307–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunn BG, Cunningham L, Cooper MA, Corteen NL, Seifi M, Swinny JD, Lambert JJ, Belelli D (2013) Dysfunctional astrocytic and synaptic regulation of hypothalamic glutamatergic transmission in a mouse model of early-life adversity: relevance to neurosteroids and programming of the stress response. J. Neurosci 33:19534–19554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunn BG, Cunningham L, Mitchell SG, Swinny JD, Lambert JJ, Belelli D (2015) GABAA receptor-acting neurosteroids: a role in the development and regulation of the stress response. Front Neuroendocrinol 36:28–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo A-L, Petraglia F, Criscuolo M, Ficarra G, Nappi RE, Palumbo MA, Trentini GP, Purdy RH, Genazzani AR (1995) Evidence for a role of neurosteroids in modulation of diurnal changes and acute stress-induced corticosterone secretion in rats. Gynecol.Endocrinol. 9:1–7. [DOI] [PubMed] [Google Scholar]
- Harper KM, Knapp DJ, Park MA, Breese GR (2017) Age-related differences in anxiety-like behavior and amygdalar CCL2 responsiveness to stress following alcohol withdrawal in male Wistar rats. Psychopharmacology (Berl) 234:79–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasirci AS, Maldonado-Devincci AM, Beattie MC, O’Buckley TK, Morrow AL (2017) Cellular GABAergic Neuroactive Steroid (3⍺,5⍺)-3-Hydroxy-Pregnan-20-One (3⍺,5⍺-THP) Immunostaining Levels Are Increased in the Ventral Tegmental Area of Human Alcohol Use Disorder Patients: A Postmortem Study. Alcohol Clin Exp Res 41:299–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He J, Crews FT (2008) Increased MCP-1 and microglia in various regions of the human alcoholic brain. Exp Neurol 210:349–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He J, Evans CO, Hoffman SW, Oyesiku NM, Stein DG (2004a) Progesterone and allopregnanolone reduce inflammatory cytokines after traumatic brain injury. Exp Neurol 189:404–412. [DOI] [PubMed] [Google Scholar]
- He J, Hoffman SW, Stein DG (2004b) Allopregnanolone, a progesterone metabolite, enhances behavioral recovery and decreases neuronal loss after traumatic brain injury. Restor Neurol Neurosci 22:19–31. [PubMed] [Google Scholar]
- Henckens MJ, Deussing JM, Chen A (2016) Region-specific roles of the corticotropin-releasing factor-urocortin system in stress. Nat Rev Neurosci 17:636–651. [DOI] [PubMed] [Google Scholar]
- Herd MB, Belelli D, Lambert JJ (2007) Neurosteroid modulation of synaptic and extrasynaptic GABAA receptors. Pharmacol Ther 116:20–34. [DOI] [PubMed] [Google Scholar]
- Herman JP, Tasker JG, Ziegler DR, Cullinan WE (2002) Local circuit regulation of paraventricular nucleus stress integration: glutamate-GABA connections. Pharmacol Biochem Behav 71:457–468. [DOI] [PubMed] [Google Scholar]
- Herman MA, Contet C, Roberto M (2016) A functional switch in tonic gaba currents alters the output of central amygdala corticotropin releasing factor receptor-1 neurons following chronic ethanol exposure. J Neurosci 36:10729–10741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman MA, Roberto M (2016) Cell-type-specific tonic GABA signaling in the rat central amygdala is selectively altered by acute and chronic ethanol. Addict Biol 21:72–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill M, Popov P, Havlikova H, Kancheva L, Vrbikova J, Meloun M, Kancheva R, Cibula D, Pouzar V, Cerny I, Starka L (2005) Reinstatement of serum pregnanolone isomers and progesterone during alcohol detoxification therapy in premenopausal women. Alcohol Clin Exp Res 29:1010–1017. [DOI] [PubMed] [Google Scholar]
- Hosie AM, Wilkins ME, da Silva HM, Smart TG (2006) Endogenous neurosteroids regulate GABAA receptors through two discrete transmembrane sites. Nature 444:486–489. [DOI] [PubMed] [Google Scholar]
- Hughes BA, Bohnsack JP, O’Buckley TK, Herman MA, Morrow AL (2019) Chronic Ethanol Exposure and Withdrawal Impairs Synaptic GABAA Receptor-Mediated Neurotransmission in Deep Layer Prefrontal Cortex. Alcohol Clin Exp Res 43:822–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janak PH, Redfern JEM, Samson HH (1998) The reinforcing effects of ethanol are altered by the endogenous neurosteroid, allopregnanolone. Alcohol Clin Exp Res 22:1106–1112. [PubMed] [Google Scholar]
- Janis GC, Devaud LL, Mitsuyama H, Morrow AL (1998) Effects of chronic ethanol consumption and withdrawal on the neuroactive steroid 3α-hydroxy-5α-pregnan-20-one in male and female rats. Alcohol Clin Exp Res 22:2055–2061. [PubMed] [Google Scholar]
- June HL, Liu J, Warnock KT, Bell KA, Balan I, Bollino D, Puche A, Aurelian L (2015) CRF-amplified neuronal TLR4/MCP-1 signaling regulates alcohol self-administration. Neuropsychopharmacology 40:1549–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane CJ, Phelan KD, Douglas JC, Wagoner G, Johnson JW, Xu J, Phelan PS, Drew PD (2014) Effects of ethanol on immune response in the brain: region-specific changes in adolescent versus adult mice. Alcohol Clin Exp Res 38:384–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanes S, Colquhoun H, Gunduz-Bruce H, Raines S, Arnold R, Schacterle A, Doherty J, Epperson CN, Deligiannidis KM, Riesenberg R, Hoffmann E, Rubinow D, Jonas J, Paul S, Meltzer-Brody S (2017) Brexanolone (SAGE-547 injection) in post-partum depression: a randomised controlled trial. Lancet 390:480–489. [DOI] [PubMed] [Google Scholar]
- Kapoor M, Wang JC, Farris SP, Liu Y, McClintick J, Gupta I, Meyers JL, Bertelsen S, Chao M, Nurnberger J, Tischfield J, Harari O, Zeran L, Hesselbrock V, Bauer L, Raj T, Porjesz B, Agrawal A, Foroud T, Edenberg HJ, Mayfield RD, Goate A (2019) Analysis of whole genome-transcriptomic organization in brain to identify genes associated with alcoholism. Transl Psychiatry 9:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karkkainen O, Hakkinen MR, Auriola S, Kautiainen H, Tiihonen J, Storvik M (2016) Increased steroid hormone dehydroepiandrosterone and pregnenolone levels in post-mortem brain samples of alcoholics. Alcohol 52:63–70. [DOI] [PubMed] [Google Scholar]
- Kavaliers M, Wiebe JP (1987) Analgesic effects of the progesterone metabolite, 3 alpha-hydroxy-5 alpha-pregnan-20-one, and possible modes of action in mice. Brain Res 415:393–398. [DOI] [PubMed] [Google Scholar]
- Kendall-Tackett K (2007) A new paradigm for depression in new mothers: the central role of inflammation and how breastfeeding and anti-inflammatory treatments protect maternal mental health. Int Breastfeed J 2:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khisti RT, Boyd KN, Kumar S, Morrow AL (2005) Systemic ethanol administration elevates deoxycorticosterone levels and chronic ethanol exposure attenuates this response. Brain Res 1049:104–111. [DOI] [PubMed] [Google Scholar]
- Khisti RT, Chopde CT, Jain SP (2000) Antidepressant-like effect of the neurosteroid 3a-hydroxy-5a-pregnan-20-one in mice forced swim test. Pharmacol Biochem Behav 67:137–143. [DOI] [PubMed] [Google Scholar]
- Knapp DJ, Harper KM, Whitman BA, Zimomra Z, Breese GR (2016) Stress and Withdrawal from Chronic Ethanol Induce Selective Changes in Neuroimmune mRNAs in Differing Brain Sites. Brain Sci 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kokate TG, Svensson BE, Rogawski MA (1994) Anticonvulsant activity of neurosteroids: Correlation with gamma-aminobutyric acid-evoked chloride current potentiation. J Pharmacol Exp Ther 270:1223–1229. [PubMed] [Google Scholar]
- Koob GF (2013) Theoretical frameworks and mechanistic aspects of alcohol addiction: alcohol addiction as a reward deficit disorder. Curr Top Behav Neurosci 13:3–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF, Colrain IM (2019) Alcohol use disorder and sleep disturbances: a feed-forward allostatic framework. Neuropsychopharmacology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar S, Porcu P, Werner DF, Matthews DB, Diaz-Granados JL, Helfand RS, Morrow AL (2009) The role of GABAA receptors in the acute and chronic effects of ethanol: a decade of progress. Psychopharmacology (Berl) 205:529–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacagnina MJ, Rivera PD, Bilbo SD (2017) Glial and Neuroimmune Mechanisms as Critical Modulators of Drug Use and Abuse. Neuropsychopharmacology 42:156–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancel M, Faulhaber J, Schiffelholz T, Romeo E, di Michele F, Holsboer F, Rupprecht R (1997) Allopregnanolone affects sleep in a benzodiazepine-like fashion. J Pharmacol Exp Ther 282:1213–1218. [PubMed] [Google Scholar]
- Leclercq S, Cani PD, Neyrinck AM, Starkel P, Jamar F, Mikolajczak M, Delzenne NM, de Timary P (2012) Role of intestinal permeability and inflammation in the biological and behavioral control of alcohol-dependent subjects. Brain Behav Immun 26:911–918. [DOI] [PubMed] [Google Scholar]
- Liang J, Cagetti E, Olsen RW, Spigelman I (2004) Altered pharmacology of synaptic and extrasynaptic GABAA receptors on CA1 hippocampal neurons is consistent with subunit changes in a model of alcohol withdrawal and dependence. J Pharmacol Exp Ther 310:1234–1245. [DOI] [PubMed] [Google Scholar]
- Liang J, Suryanarayanan A, Chandra D, Homanics GE, Olsen RW, Spigelman I (2008) Functional consequences of GABAA receptor α4 subunit deletion on synaptic and extrasynaptic currents in mouse dentate granule cells. Alcohol Clin Exp Res 32:19–26. [DOI] [PubMed] [Google Scholar]
- Liang J, Zhang N, Cagetti E, Houser CR, Olsen RW, Spigelman I (2006) Chronic intermittent ethanol-induced switch of ethanol actions from extrasynaptic to synaptic hippocampal GABAA receptors. J Neurosci 26:1749–1758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lingford-Hughes AR, Wilson SJ, Cunningham VJ, Feeney A, Stevenson B, Brooks DJ, Nutt DJ (2005) GABA-benzodiazepine receptor function in alcohol dependence: a combined 11C-flumazenil PET and pharmacodynamic study. Psychopharmacology (Berl) 180:595–606. [DOI] [PubMed] [Google Scholar]
- Liu J, Yang AR, Kelly T, Puche A, Esoga C, June HL Jr., Elnabawi A, Merchenthaler I, Sieghart W, June HL Sr., Aurelian L (2011) Binge alcohol drinking is associated with GABAA alpha2-regulated Toll-like receptor 4 (TLR4) expression in the central amygdala. Proc Natl Acad Sci U S A 108:4465–4470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locci A, Porcu P, Talani G, Santoru F, Berretti R, Giunti E, Licheri V, Sanna E, Concas A (2017) Neonatal estradiol exposure to female rats changes GABAA receptor expression and function, and spatial learning during adulthood. Horm Behav 87:35–46. [DOI] [PubMed] [Google Scholar]
- Logrip ML, Milivojevic V, Bertholomey ML, Torregrossa MM (2018) Sexual dimorphism in the neural impact of stress and alcohol. Alcohol 72:49–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maguire JL, Stell BM, Rafizadeh M, Mody I (2005) Ovarian cycle-linked changes in GABAA receptors mediating tonic inhibition alter seizure susceptibility and anxiety. Nat Neurosci 8:797–804. [DOI] [PubMed] [Google Scholar]
- Maldonado-Devincci AM, Cook JB, O’ Buckley TK, Morrow DH, McKinley RE, Lopez MF, Becker HC, Morrow AL (2014) Chronic intermittent ethanol exposure and withdrawal alters (3alpha,5alpha)-3-hydroxy-pregnan-20-one immunostaining in cortical and limbic brain regions of C57BL/6J mice. Alcohol Clin Exp Res 38:2561–2571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maroso M, Balosso S, Ravizza T, Liu J, Bianchi ME, Vezzani A (2011) Interleukin-1 type 1 receptor/Toll-like receptor signalling in epilepsy: the importance of IL-1beta and high-mobility group box 1. J Intern Med 270:319–326. [DOI] [PubMed] [Google Scholar]
- Marx CE, Shampine LJ, Khisti RT, Trost WT, Bradford DW, Grobin AC, Massing MW, Madison RD, Butterfield MI, Lieberman JA, Morrow AL (2006) Olanzapine and fluoxetine administration and coadministration increase rat hippocampal pregnenolone, allopregnanolone and peripheral deoxycorticosterone: implications for therapeutic actions. Pharmacol Biochem Behav 84:609–617. [DOI] [PubMed] [Google Scholar]
- Mayfield J, Harris RA (2017) The Neuroimmune Basis of Excessive Alcohol Consumption. Neuropsychopharmacology 42:376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mechlin B, Morrow AL, Maixner W, Girdler SS (2007) The relationship of allopregnanolone immunoreactivity and HPA-axis measures to experimental pain sensitivity: Evidence for ethnic differences. Pain 131:142–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer-Brody S, Colquhoun H, Riesenberg R, Epperson CN, Deligiannidis KM, Rubinow DR, Li H, Sankoh AJ, Clemson C, Schacterle A, Jonas J, Kanes S (2018) Brexanolone injection in post-partum depression: two multicentre, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet 392:1058–1070. [DOI] [PubMed] [Google Scholar]
- Mendelson JH, Stein S (1966) Serum Cortisol Levels in Alcoholic and Nonalcoholic Subjects During Experimentally Induced Ethanol Intoxication. Psychosomatic Medicine 28:616–626. [DOI] [PubMed] [Google Scholar]
- Mendelson WB, Martin JV, Perlis M, Wagner R, Majewska MD, Paul SM (1987) Sleep induction by an adrenal steroid in the rat. Psychopharmacology 93:226–229. [DOI] [PubMed] [Google Scholar]
- Mihalek RM, Banerjee PK, Korpi ER, Quinlan JJ, Firestone LL, Mi ZP, Lagenaur C, Tretter V, Sieghart W, Anagnostaras SG, Sage JR, Fanselow MS, Guidotti A, Spigelman I, Li Z, DeLorey TM, Olsen RW, Homanics GE (1999) Attenuated sensitivity to neuroactive steroids in γ-aminobutyrate type A receptor delta subunit knockout mice. Proc Natl Acad Sci U S A 96:12905–12910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milivojevic V, Covault J, Angarita GA, Siedlarz K, Sinha R (2019) Neuroactive steroid levels and cocaine use chronicity in men and women with cocaine use disorder receiving progesterone or placebo. Am J Addict 28:16–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milivojevic V, Fox HC, Sofuoglu M, Covault J, Sinha R (2016) Effects of progesterone stimulated allopregnanolone on craving and stress response in cocaine dependent men and women. Psychoneuroendocrinology 65:44–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitsuyama H, Little KY, Sieghart W, Devaud LL, Morrow AL (1998) GABAA receptor α1, α4 and ß3 subunit mRNA and protein expression in frontal cortex of human alcoholics. Alcohol Clin Exp Res 22(4):815–822. [PubMed] [Google Scholar]
- Modgil A, Parakala ML, Ackley MA, Doherty JJ, Moss SJ, Davies PA (2017) Endogenous and synthetic neuroactive steroids evoke sustained increases in the efficacy of GABAergic inhibition via a protein kinase C-dependent mechanism. Neuropharmacology 113:314–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH, Moos BS (2006) Rates and predictors of relapse after natural and treated remission from alcohol use disorders. Addiction 101:212–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran MH, Goldberg N, Smith SS (1998) Progesterone withdrawal II: Insensitivity to the sedative effects of a benzodiazepine. Brain Res 807:91–100. [DOI] [PubMed] [Google Scholar]
- Moran MH, Smith SS (1998) Progesterone withdrawal I: Pro-convulsant effects. Brain Res 807:84–90. [DOI] [PubMed] [Google Scholar]
- Morrow AL (2007) Recent developments in the significance and therapeutic relevance of neuroactive steroids - Introduction to the special issue. Pharmacol Ther 116:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrow AL, Porcu P, Boyd KN, Grant KA (2006) Hypothalamic-pituitary-adrenal axis modulation of GABAergic neuroactive steroids influences ethanol sensitivity and drinking behavior. Dialogues Clin Neurosci 8:463–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrow AL, VanDoren MJ, Penland SN, Matthews DB (2001) The role of GABAergic neuroactive steroids in ethanol action, tolerance and dependence. Brain Res Brain Res Rev 37:98–109. [DOI] [PubMed] [Google Scholar]
- Murugan S, Jakka P, Namani S, Mujumdar V, Radhakrishnan G (2019) The neurosteroid pregnenolone promotes degradation of key proteins in the innate immune signaling to suppress inflammation. J Biol Chem 294:4596–4607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naert G, Maurice T, Tapia-Arancibia L, Givalois L (2007) Neuroactive steroids modulate HPA axis activity and cerebral brain-derived neurotrophic factor (BDNF) protein levels in adult male rats. Psychoneuroendocrinology 32:1062–1078. [DOI] [PubMed] [Google Scholar]
- Naylor DE, Liu H, Wasterlain CG (2005) Trafficking of GABA(A) receptors, loss of inhibition, and a mechanism for pharmacoresistance in status epilepticus. J Neurosci 25:7724–7733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naylor JC, Kilts JD, Szabo ST, Dunn CE, Keefe FJ, Tupler LA, Shampine LJ, Morey RA, Strauss JL, Hamer RM, Wagner HR, Workgroup M, Marx CE (2016) Allopregnanolone Levels Are Inversely Associated with Self-Reported Pain Symptoms in U.S. Iraq and Afghanistan-Era Veterans: Implications for Biomarkers and Therapeutics. Pain Med 17:25–32. [DOI] [PubMed] [Google Scholar]
- Noorbakhsh F, Baker GB, Power C (2014) Allopregnanolone and neuroinflammation: a focus on multiple sclerosis. Front Cell Neurosci 8:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Dell LE, Purdy RH, Covey DF, Richardson HN, Roberto M, Koob GF (2005) Epipregnanolone and a novel synthetic neuroactive steroid reduce alcohol self-administration in rats. Pharmacol Biochem Behav 81:543–550. [DOI] [PubMed] [Google Scholar]
- Ocvirk R, Pearson Murphy BE, Franklin KB, Abbott FV (2008) Antinociceptive profile of ring A-reduced progesterone metabolites in the formalin test. Pain 138:402–409. [DOI] [PubMed] [Google Scholar]
- Olsen RW, Liang J (2017) Role of GABAA receptors in alcohol use disorders suggested by chronic intermittent ethanol (CIE) rodent model. Mol Brain 10:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens MJ, Ritchie JC, Nemeroff CB (1992) 5α-Pregnane-3α,21-diol-20-one (THDOC) attenuates mild stress-induced increases in plasma corticosterone via a non-glucocorticoid mechanism: comparison with alprazolam. Brain Res 573:353–355. [DOI] [PubMed] [Google Scholar]
- Oyola MG, Handa RJ (2017) Hypothalamic-pituitary-adrenal and hypothalamic-pituitary-gonadal axes: sex differences in regulation of stress responsivity. Stress 20:476–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Painsipp E, Kofer MJ, Sinner F, Holzer P (2011) Prolonged depression-like behavior caused by immune challenge: influence of mouse strain and social environment. PLoS One 6:e20719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascual M, Balino P, Aragon CM, Guerri C (2015) Cytokines and chemokines as biomarkers of ethanol-induced neuroinflammation and anxiety-related behavior: role of TLR4 and TLR2. Neuropharmacology 89:352–359. [DOI] [PubMed] [Google Scholar]
- Patchev VK, Holsboer F, Almeida OFX (1996) Neuroactive steroids and the behavioral and endocrine response to stress., in The Brain: Source and Target for Sex Steroid Hormones, The Brain: Source and Target for Sex Steroid Hormones. (GENAZZANI AR, PETRAGLIA F, PURDY RH eds), pp 93–102, The Parthenon Group, New York. [Google Scholar]
- Patchev VK, Shoaib M, Holsboer F, Almeida OFX (1994) The neurosteroid tetrahydroprogesterone counteracts corticotropin-releasing hormone-induced anxiety and alters the release and gene expression of corticotropin-releasing hormone in the rat hypothalamus. Neuroscience 62:265–271. [DOI] [PubMed] [Google Scholar]
- Pavlov VA, Tracey KJ (2017) Neural regulation of immunity: molecular mechanisms and clinical translation. Nat Neurosci 20:156–166. [DOI] [PubMed] [Google Scholar]
- Peng J, Long B, Yuan J, Peng X, Ni H, Li X, Gong H, Luo Q, Li A (2017) A Quantitative Analysis of the Distribution of CRH Neurons in Whole Mouse Brain. Front Neuroanat 11:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pisu MG, Garau A, Boero G, Biggio F, Pibiri V, Dore R, Locci V, Paci E, Porcu P, Serra M (2016) Sex differences in the outcome of juvenile social isolation on HPA axis function in rats. Neuroscience 320:172–182. [DOI] [PubMed] [Google Scholar]
- Pleil KE, Lowery-Gionta EG, Crowley NA, Li C, Marcinkiewcz CA, Rose JH, McCall NM, Maldonado-Devincci AM, Morrow AL, Jones SR, Kash TL (2015) Effects of chronic ethanol exposure on neuronal function in the prefrontal cortex and extended amygdala. Neuropharmacology 99:735–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porcu P, Concas A, Morrow AL (2019) Neuroactive steroids and ethanol exposure: Relevance to ethanol sensitivity and alcohol use disorders risk, in Neuroscience of Alcohol: Mechanisms and Treatment, Neuroscience of Alcohol: Mechanisms and Treatment (PREEDY VR ed, pp 405–415, Academic Press, Elsevier. [Google Scholar]
- Porcu P, Morrow AL (2014) Divergent neuroactive steroid responses to stress and ethanol in rat and mouse strains: relevance for human studies. Psychopharmacology (Berl) 231:3257–3272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porcu P, O’Buckley TK, Alward SE, Song SC, Grant KA, de Wit H, Morrow AL (2010) Differential effects of ethanol on serum GABAergic 3alpha,5alpha/3alpha,5beta neuroactive steroids in mice, rats, cynomolgus monkeys, and humans. Alcohol Clin Exp Res 34:432–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porcu P, O’Buckley TK, Lopez MF, Becker HC, Miles MF, Williams RW, Morrow AL (2017) Initial genetic dissection of serum neuroactive steroids following chronic intermittent ethanol across BXD mouse strains. Alcohol 58:107–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porcu P, O’Buckley TK, Morrow AL, Adinoff B (2008) Differential hypothalamic-pituitary-adrenal activation of the neuroactive steroids pregnenolone sulfate and deoxycorticosterone in healthy controls and alcohol-dependent subjects. Psychoneuroendocrinology 33:214–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pribiag H, Stellwagen D (2013) TNF-alpha downregulates inhibitory neurotransmission through protein phosphatase 1-dependent trafficking of GABA(A) receptors. J Neurosci 33:15879–15893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puia G, Ducic I, Vicini S, Costa E (1993) Does neurosteroid modulatory efficacy depend on GABAA receptor subunit composition? Receptors and Channels 1:135–142. [PubMed] [Google Scholar]
- Puia G, Santi M, Vicini S, Pritchett DB, Purdy RH, Paul SM, Seeburg PH, Costa E (1990) Neurosteroids act on recombinant human GABAA receptors. Neuron 4:759–765. [DOI] [PubMed] [Google Scholar]
- Puia G, Vicini S, Seeburg PH, Costa E (1991) Influence of recombinant GABAA receptor subunit composition on the action of allosteric modulators of GABA-gated Cl− currents. Mol Pharmacol 39:691–696. [PubMed] [Google Scholar]
- Purdy RH, Morrow AL, Blinn JR, Paul SM (1990) Synthesis, metabolism, and pharmacological activity of 3a-hydroxy steroids which potentiate GABA-receptor-mediated chloride ion uptake in rat cerebral cortical synaptoneurosomes. J Med Chem 33:1572–1581. [DOI] [PubMed] [Google Scholar]
- Purdy RH, Morrow AL, Moore PH Jr., Paul SM (1991) Stress-induced elevations of gamma-aminobutyric acid type A receptor-active steroids in the rat brain. Proc Natl Acad Sci U. S. A 88:4553–4557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin L, He J, Hanes RN, Pluzarev O, Hong JS, Crews FT (2008) Increased systemic and brain cytokine production and neuroinflammation by endotoxin following ethanol treatment. J Neuroinflammation 5:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rainville JR, Tsyglakova M, Hodes GE (2018) Deciphering sex differences in the immune system and depression. Front Neuroendocrinol 50:67–90. [DOI] [PubMed] [Google Scholar]
- Ramaker MJ, Ford MM, Fretwell AM, Finn DA (2011) Alteration of ethanol drinking in mice via modulation of the GABA(A) receptor with ganaxolone, finasteride, and gaboxadol. Alcohol Clin Exp Res 35:1994–2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaker MJ, Ford MM, Phillips TJ, Finn DA (2014) Differences in the reinstatement of ethanol seeking with ganaxolone and gaboxadol. Neuroscience 272:180–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaker MJ, Strong MN, Ford MM, Finn DA (2012) Effect of ganaxolone and THIP on operant and limited-access ethanol self-administration. Neuropharmacology 63:555–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randall PA, Vetreno RP, Makhijani VH, Crews FT, Besheer J (2019) The Toll-Like Receptor 3 Agonist Poly(I:C) Induces Rapid and Lasting Changes in Gene Expression Related to Glutamatergic Function and Increases Ethanol Self-Administration in Rats. Alcohol Clin Exp Res 43:48–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmusson AM, Marx CE, Pineles SL, Locci A, Scioli-Salter ER, Nillni YI, Liang JJ, Pinna G (2017) Neuroactive steroids and PTSD treatment. Neurosci Lett 649:156–163. [DOI] [PubMed] [Google Scholar]
- Rasmusson AM, Pinna G, Paliwal P, Weisman D, Gottschalk C, Charney D, Krystal J, Guidotti A (2006) Decreased cerebrospinal fluid allopregnanolone levels in women with posttraumatic stress disorder. Biol Psychiatry 60:704–713. [DOI] [PubMed] [Google Scholar]
- Reddy DS, Rogawski MA (2002) Stress-induced deoxycorticosterone-derived neurosteroids modulate GABAA receptor function and seizure susceptibility. J Neurosci 22:3795–3805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy DS, Rogawski MA (2012) Neurosteroids - Endogenous Regulators of Seizure Susceptibility and Role in the Treatment of Epilepsy, in Jasper’s Basic Mechanisms of the Epilepsies, Jasper’s Basic Mechanisms of the Epilepsies (NOEBELS JL, AVOLI M, ROGAWSKI MA, OLSEN RW, DELGADO-ESCUETA AV eds), Bethesda (MD). [Google Scholar]
- Reilly MT, Noronha A, Goldman D, Koob GF (2017) Genetic studies of alcohol dependence in the context of the addiction cycle. Neuropharmacology 122:3–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivier C, Vale W (1983) Modulation of stress-induced ACTH release by corticotropin-releasing factor, catecholamines and vasopressin. Nature 305:325–327. [DOI] [PubMed] [Google Scholar]
- Roberto M, Spierling SR, Kirson D, Zorrilla EP (2017) Corticotropin-Releasing Factor (CRF) and Addictive Behaviors. Int Rev Neurobiol 136:5–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogawski MA, Loya CM, Reddy K, Zolkowska D, Lossin C (2013) Neuroactive steroids for the treatment of status epilepticus. Epilepsia 54 Suppl 6:93–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romeo E, Brancati A, De Lorenzo A, Fucci P, Furnari C, Pompili E, Sasso GF, Spalletta G, Troisi A, Pasini A (1996) Marked decrease of plasma neuroactive steroids during alcohol withdrawal. Clin Neuropharmacol 19:366–369. [DOI] [PubMed] [Google Scholar]
- Romeo E, Ströhle A, Spalletta G, di Michele F, Hermann B, Holsboer F, Pasini A, Rupprecht R (1998) Effects of antidepressant treatment on neuroactive steroids in major depression. Am J Psychiatry 155:910–913. [DOI] [PubMed] [Google Scholar]
- Sanacora G, Saricicek A (2007) GABAergic contributions to the pathophysiology of depression and the mechanism of antidepressant action. CNS Neurol Disord Drug Targets 6:127–140. [DOI] [PubMed] [Google Scholar]
- Sanna E, Mostallino MC, Murru L, Carta M, Talani G, Zucca S, Mura ML, Maciocco E, Biggio G (2009) Changes in expression and function of extrasynaptic GABAA receptors in the rat hippocampus during pregnancy and after delivery. J Neurosci 29:1755–1765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayeed I, Stein DG (2009) Progesterone as a neuroprotective factor in traumatic and ischemic brain injury. Prog Brain Res 175:219–237. [DOI] [PubMed] [Google Scholar]
- Schreiber AL, Gilpin NW (2018) Corticotropin-Releasing Factor (CRF) Neurocircuitry and Neuropharmacology in Alcohol Drinking. Handb Exp Pharmacol 248:435–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuckit MA (2009) An overview of genetic influences in alcoholism. J Subst Abuse Treat 36:S5–14. [PubMed] [Google Scholar]
- Schule C, Nothdurfter C, Rupprecht R (2014) The role of allopregnanolone in depression and anxiety. Prog Neurobiol 113:79–87. [DOI] [PubMed] [Google Scholar]
- Schumacher M, Guennoun R, Stein DG, De Nicola AF (2007) Progesterone: therapeutic opportunities for neuroprotection and myelin repair. Pharmacol Ther 116:77–106. [DOI] [PubMed] [Google Scholar]
- Serra M, Mostallino MC, Talani G, Pisu MG, Carta M, Mura ML, Floris I, Maciocco E, Sanna E, Biggio G (2006) Social isolation-induced increase in α4 and d subunit gene expression is associated with a greater efficacy of ethanol on steroidogenesis and GABAA receptor function. J. Neurochem 98:122–133. [DOI] [PubMed] [Google Scholar]
- Serra M, Pisu MG, Floris I, Biggio G (2005) Social isolation-induced changes in the hypothalamic-pituitary-adrenal axis in the rat. Stress 8:259–264. [DOI] [PubMed] [Google Scholar]
- Serra M, Pisu MG, Littera M, Papi G, Sanna E, Tuveri F, Usala L, Purdy RH, Biggio G (2000) Social isolation-induced decreases in both the abundance of neuroactive steroids and GABAA receptor function in rat brain. J. Neurochem 75:732–740. [DOI] [PubMed] [Google Scholar]
- Shaham Y, de Wit H (2016) Lost in Translation: CRF1 Receptor Antagonists and Addiction Treatment. Neuropsychopharmacology 41:2795–2797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen H, Gong QH, Aoki C, Yuan M, Ruderman Y, Dattilo M, Williams K, Smith SS (2007) Reversal of neurosteroid effects at α4ß2d GABAA receptors triggers anxiety at puberty. Nat Neurosci 10:469–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, Fox HC, Hong KI, Hansen J, Tuit K, Kreek MJ (2011) Effects of adrenal sensitivity, stress- and cue-induced craving, and anxiety on subsequent alcohol relapse and treatment outcomes. Arch Gen Psychiatry 68:942–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SS, Gong QH, Hsu F-C, Markowitz RS, Ffrench-Mullen JMH, Li X (1998) GABAA receptor α4 subunit suppression prevents withdrawal properties of an endogenous steroid. Nature 392:926–930. [DOI] [PubMed] [Google Scholar]
- Snelling C, Tanchuck-Nipper MA, Ford MM, Jensen JP, Cozzoli DK, Ramaker MJ, Helms M, Crabbe JC, Rossi DJ, Finn DA (2014) Quantification of ten neuroactive steroids in plasma in Withdrawal Seizure-Prone and -Resistant mice during chronic ethanol withdrawal. Psychopharmacology (Berl) 231:3401–3414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spigelman I, Li Z, Liang J, Cagetti E, Samzadeh S, Mihalek RM, Homanics GE, Olsen RW (2003) Reduced inhibition and sensitivity to neurosteroids in hippocampus of mice lacking the GABA(A) receptor delta subunit. J Neurophysiol 90:903–910. [DOI] [PubMed] [Google Scholar]
- Stell BM, Brickley SG, Tang CY, Farrant M, Mody I (2003) Neuroactive steroids reduce neuronal excitability by selectively enhancing tonic inhibition mediated by d subunit-containing GABAA receptors. Proc Natl Acad Sci U S A 100:14439–14444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stellwagen D, Beattie EC, Seo JY, Malenka RC (2005) Differential regulation of AMPA receptor and GABA receptor trafficking by tumor necrosis factor-alpha. J Neurosci 25:3219–3228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuck ED, Christensen RN, Huie JR, Tovar CA, Miller BA, Nout YS, Bresnahan JC, Beattie MS, Ferguson AR (2012) Tumor necrosis factor alpha mediates GABA(A) receptor trafficking to the plasma membrane of spinal cord neurons in vivo. Neural Plast 2012:261345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tehrani MHJ, Barnes EM Jr., (1997) Sequestration of gamma-aminobutyric acidA receptors on clathrin-coated vesicles during chronic benzodiazepine administration in vivo. J Pharmacol Exp Ther 283:384–390. [PubMed] [Google Scholar]
- Uzunov DP, Cooper TB, Costa E, Guidotti A (1996) Fluoxetine-elicited changes in brain neurosteroid content measured by negative ion mass fragmentography. Proc Natl Acad Sci U S A 93:12599–12604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uzunova V, Sheline Y, Davis JM, Rasmusson A, Uzunov DP, Costa E, Guidotti A (1998) Increase in the cerebrospinal fluid content of neurosteroids in patients with unipolar major depression who are receiving fluoxetine or fluvoxamine. Proc Natl Acad Sci U S A 95:3239–3244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaitkevicius H, Husain AM, Rosenthal ES, Rosand J, Bobb W, Reddy K, Rogawski MA, Cole AJ (2017) First-in-man allopregnanolone use in super-refractory status epilepticus. Ann Clin Transl Neurol 4:411–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanDoren MJ, Matthews DB, Janis GC, Grobin AC, Devaud LL, Morrow AL (2000) Neuroactive steroid 3α-hydroxy-5α-pregnan-20-one modulates electrophysiological and behavioral actions of ethanol. J Neurosci 20:1982–1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vichaya EG, Laumet G, Christian DL, Grossberg AJ, Estrada DJ, Heijnen CJ, Kavelaars A, Dantzer R (2019) Motivational changes that develop in a mouse model of inflammation-induced depression are independent of indoleamine 2,3 dioxygenase. Neuropsychopharmacology 44:364–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Wang GJ, Hitzemann R, Fowler JS, Wolf AP, Pappas N, Biegon A, Dewey SL (1993) Decreased cerebral response to inhibitory neurotransmission in alcoholics. A J Psychiatry 150:417–422. [DOI] [PubMed] [Google Scholar]
- Warden AS, Azzam M, DaCosta A, Mason S, Blednov YA, Messing RO, Mayfield RD, Harris RA (2019) Toll-like receptor 3 activation increases voluntary alcohol intake in C57BL/6J male mice. Brain Behav Immun 77:55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winsky-Sommerer R (2009) Role of GABAA receptors in the physiology and pharmacology of sleep. Eur J Neurosci 29:1779–1794. [DOI] [PubMed] [Google Scholar]
- Wright DW, Kellermann AL, Hertzberg VS, Clark PL, Frankel M, Goldstein FC, Salomone JP, Dent LL, Harris OA, Ander DS, Lowery DW, Patel MM, Denson DD, Gordon AB, Wald MM, Gupta S, Hoffman SW, Stein DG (2007) ProTECT: a randomized clinical trial of progesterone for acute traumatic brain injury. Ann Emerg Med 49:391–402. [DOI] [PubMed] [Google Scholar]
- Zahr NM, Pfefferbaum A (2017) Alcohol’s Effects on the Brain: Neuroimaging Results in Humans and Animal Models. Alcohol Res 38:183–206. [PMC free article] [PubMed] [Google Scholar]
- Zolkowska D, Wu CY, Rogawski MA (2018) Intramuscular allopregnanolone and ganaxolone in a mouse model of treatment-resistant status epilepticus. Epilepsia 59 Suppl 2:220–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zorrilla EP, Logrip ML, Koob GF (2014) Corticotropin releasing factor: a key role in the neurobiology of addiction. Front Neuroendocrinol 35:234–244. [DOI] [PMC free article] [PubMed] [Google Scholar]