Abstract
Cisgender men partnered with transgender women are an understudied and hard to engage population in HIV prevention efforts. Relationship stigma -the anticipation of negative treatment based on having a relationship with a member of a stigmatized group -has been linked to adverse health behaviors, but it remains unclear whether different sources of relationship stigma (i.e., family, friends, and the general public) are associated with HIV risk behaviors and whether these associations may vary by men’s sexual identities (e.g., gay, bisexual, heterosexual). The current study examined associations between relationship stigma and HIV risk behaviors, and whether these associations were moderated by sexual identity. We recruited a convenience sample of 185 cisgender men in primary partnerships with transgender women to participate in a one-time survey. Gay-identified men reported greater levels of relationship stigma from the general public compared to heterosexual-identified men. In multivariable models, higher levels of relationship stigma from the public were associated with increased odds of engaging in drug use prior to having condomless sex and receiving an STI diagnosis in the last 30 days. There were significant interaction effects such that higher levels of relationship stigma from the public were associated with both indicators of HIV risk for gay-identified men but not for heterosexual-identified men. Findings support the importance of HIV prevention approaches accounting for relationship stigma from the general public and the diverse sexual identities of men partnered with transgender women when seeking to increase linkage to and engagement in HIV prevention services, including biomedical prevention strategies.
Keywords: HIV prevention, stigma, sexual identity, sexual risk behavior, gay men
Introduction
Transgender (‘trans’) women (individuals with a feminine and/or female gender identity who were assigned male at birth) are disproportionately affected by HIV. Compared with cisgender (non-transgender) peers, evidence suggests that trans women have the highest rates of new HIV diagnoses by gender (2.1%, compared to 1.2% among cisgender men and 0.4% among cisgender women) (Baral et al., 2013). Like other groups, the risk for acquiring sexually transmitted infections (STIs), including HIV among trans women is particularly high in the context of primary partnerships with cisgender male partners (Melendez & Pinto, 2007; Nemoto, Operario, Keatley, & Villegas, 2004; Nemoto, Operario, Keatley, Han, & Soma, 2004; Operario, Nemoto, Iwamoto, & Moore, 2011a, 2011b; Reisner et al., 2009). Recent years have seen advances in biomedical prevention strategies, such as treatment as prevention (TasP) and pre-exposure prophylaxis (PrEP), as a means of eliminating HIV transmission and acquistion. However, there is a continued need to attend to the social, relational, and behavioral factors underlying HIV risk in order to fully maximize the potential of biomedical HIV prevention strategies. For example, drug use has been associated with an increased risk of engaging in condomless sex and HIV/STI transmission (Boone, Cook, & Wilson, 2013; Yu, Wall, Chiasson, & Hirshfield, 2015) and may undermine HIV treatment adherence (Closson, Mitty, Malone, Mayer, & Mimiaga, 2016; Kalichman et al., 2015). There are also concerns that the use of biomedical prevention strategies may increase the acquisition and transmission of other STIs (Marrazzo, Dombrowski, & Mayer, 2018). Although there have been limited HIV prevention research efforts with cisgender men in primary partnerships with trans women, the few existing studies have found high HIV and STI prevalence, inconsistent condom use with their primary and outside partners, drug use prior to engaging in sex, and low linkage and engagement with HIV prevention and care services (Operario et al., 2011a, 2011b).
While there has been increased attention towards developing tailored HIV/STI programs to increase the uptake and use of biomedical prevention strategies for men who have sex with men (MSM), men who have sex with cisgender women (MSW), and men who have sex with men and cisgender women (MSMW), there have been limited efforts focused on men who have sex or partner with trans women. Importantly, cisgender men who partner with trans women challenge common assumptions in conventional categorical distinctions which rely solely on sexual identity or behaviors that are often are used in HIV/STI prevention research and programming (Operario, Burton, Underhill, & Sevelius, 2008). Cisgender men partnered with trans women have diverse sexual identities that do not easily map on to behavioral categories often used in public health frameworks, such as MSM, MSW, or MSMW (Operario et al., 2008). The sexual identities that these men choose to identify with - e.g., as heterosexual, gay, bisexual or “other” - might have important implications for health behaviors and accessing health promotion resources. A recent qualitative study found that cisgender men in partnerships with trans women did not want to be linked to or engage in HIV prevention programs that were designed for sexual and gender minority communities (Reisner, Menino, Leung, & Gamarel, in press). Although there have been strides to provide supportive norms surrounding same-gender sexual behavior as part of cultural compentency, intersectional approaches to guide health promotion efforts (Kapilashrami & Hankivsky, 2018) are needed to understand the ways in which drivers of HIV risk may be differentially experienced by men of diverse sexual identities.
Stigma as a Determinent of HIV Risk
In accordance with the Gender Minority Stress Model, people who do not conform to societal norms regarding gender roles and identities are vulnerable to stigma, which can have deleterious effects on emotions, cognitions, and health behaviors (Hendricks & Testa, 2012). Trans women and their cisgender male partners experience extreme stigma and social oppression (Bradford, Reisner, Honnold, & Xavier, 2013; Poteat, German, & Kerrigan, 2013). The Gender Minority Stress Model has been applied to trans women and their cisgender male partners, illustrating that both partners may anticipate negative treatment due to their relationship status, which results in relationship stigma (Gamarel, Reisner, Laurenceau, Nemoto, & Operario, 2014). That is, the societal stigma targeted towards trans women may result in the anticipation by cisgender men of negative treatment from the general public, families, and friends about their relationship with a member of a stigmatized group. This form of relationship stigma has been associated with reduced relationship satisfaction and greater depressive symptoms among cisgender men partnered with trans women (Gamarel et al., 2014).
Stigma towards trans people can occur at multiple levels and from varied sources, which can have differential consequences for trans individuals and their partners (White Hughto, Reisner, & Pachankis, 2015). Building on theoretical and empirical advances in relationship science (Lehmiller & Agnew, 2006; Rosenthal & Starks, 2015), relationship stigma from different sources (e.g., family, friends, general public) may have different consequences for the individual’s health and wellbeing. For example, studies have found that relationship stigma from one’s more proximal social network (i.e., friends and family) was a stronger predictor of adverse relationship outcomes compared to more distal sources (i.e., general public) (Lehmiller & Agnew, 2006; Rosenthal & Starks, 2015).
Importantly, studies with cisgender men partnered with trans women have not teased apart various sources of relationship stigma and their association with HIV risk. The diversity of cisgender men’s sexual identities (Operario et al., 2008) and notable barriers to linking and engaging these men in HIV/STI prevention programs and services (Reisner et al., in press) necessitates further investigation into whether sources of relationship stigma are differentially associated with HIV risk and whether these associations vary by an individual’s sexual identity.
The Current Study
The goal of this study was to build on and extend research on the connections between relationship stigma and HIV risk among cisgender men partnered with trans women. We aimed to disentangle whether there were differences in men’s reports of relationship stigma from varied sources (i.e., from family, friends, or the general public) and examine whether an individual’s sexual identity moderated the associations between different sources of relationship stigma and two indicators of HIV risk: drug use prior to engaging in condomless sex in the last 30 days and any self-reported STI diagnoses in the last 12 months. We also aimed to further understand the unique pathway between relationship stigma and these two indicators of HIV risk after statistically adjusting for well-known correlates of relationship stigma and HIV risk. Specifically, individuals younger in age, in shorter relationships, and those who are HIV- negative or unknown status may engage in higher HIV risk behaviors (Gamarel et al., 2015; Operario et al., 2011a, 2011b). Furthermore, men living in poverty, with a history of incarceration history may experience greater levels of stigma (Gamarel et al., 2015).
Methods
Participants
Participants were 185 cisgender men in primary partnerships with transgender women (Operario et al., 2011a). Participants were recruited in the San Francisco Bay Area of California using purposive sampling methods by identifying a range of community spaces and venues where trans women and cisgender male partners of trans women congregate (e.g., community-based organizations, bars, and nightclubs) and posting flyers. Participants called to learn more about the study and were screened for eligibility criteria. Eligible participants were scheduled for an in-person one-time survey at the research center or a conveniently located confidential space at a community-based organization.
To be eligible, cisgender men must have reported that they were in a primary intimate partnership with a transgender woman for at least 3 months, defined as a “partner to whom you feel committed above anyone else and with whom you have had a sexual relationship.” In addition, all participants were: (1) at least 18 years old; (2) living or working in the San Francisco Bay Area; (3) English or Spanish speaking; and (4) able to provide informed consent. Data for this analysis were collected between November 2008 and November 2010.
Procedures
Surveys were administered to participants using audio computer-assisted self-interview (ACASI) technology. Survey items were translated into Spanish, but Spanish version surveys were administered on paper; 5 monolingual Spanish participants completed the Spanish survey. Surveys took approximately 1 hour to complete, and participants received $50 reimbursement and a brochure with a list of local community organizations addressing transgender issues. Procedures were approved by the Institutional Review Boards (IRB) at the Public Health Institute, Oakland, University of California, San Francisco, and University of Oxford, Oxford, United Kingdom.
Measures
Sexual Identity.
Participants were asked to report their sexual orientation identity with response options l=Straight/Heterosexual, 2=Gay/Homosexual, 3=Bisexual, 4=Asexual, 5=Other, 6=Unsure/Questioning, and 7=Refuse to Answer. None of the participants selected “Refuse to Answer.” Due to the small number of participants who endorsed Asexual (n = 6), Unsure/Questioning (n = 7) and Other (n = 10), we collapsed these participants into one category. Those who indicated “Other” did not provide a write-in response for their sexual identity.
Sociodemographics.
Participants reported their age (in years), race and ethnicity, HIV serostatus (positive or negative/unknown), housing status (categorized as homeless or unstable housing versus own apartment or house). Participants self-reported their monthly income (1=$0 to $249; 2=$250 to $499; 3=$500 to 749; 4=$750 to $999; 5=$1,000 to $1,499; 6=$1,500 to $1,999; 7=$2,000 to $3,999; 8=$4,000 or more). Approximately 61% (n = 112) reported that they earned less $500 per month; therefore, financial hardship was categorized as greater than or equal to $500 a month versus $499 or less a month. Participants also provided the duration of the primary relationship (in months).
Relationship Stigma.
Participants completed the relationship stigma scale that assesses the anticipation of rejection due to being in a relationship with a trans woman from family, friends, and the general public. The psychometric properties of the relationship stigma scale have been reported previously and demonstrated good internal reliability (α = 0.82) (Gamarel et al., 2014). Response options ranged from 0 = “Never” to 4 = “Always.” For these items, participants reported how often they felt relationship stigma from friends (e.g., “How often do you have difficulty introducing your partner to friends?”), from family (e.g., “How often do you feel uncomfortable spending time with your partner with your family?), and the general public (e.g., “How often do you feel uncomfortable holding hands with your partner in public”?). We summed each of the three subscales, such that higher scores indicate greater relationship stigma (α=0.72 3-items friends, α=0.78 3-items family, α=0.82 3-items public, 9 items total).
HIV Risk.
Participants were asked about two indicators of HIV risk. First, participants were asked to self-report whether they had used any drugs (e.g., crack, cocaine, amphetamines, heroine, marijuana, opioids, hallucinogens, sedatives) prior to engaging in condomless anal or vaginal sex in the last 30 days with their primary or outside partner (i.e., l=any drug use prior to sex versus 0=no drug use prior to sex). Second, participants were asked to self-report whether they had been diagnosed with syphilis, gonorrhea, chlamydia, herpes, genital warts, or urethritis in the past 12 months. We created a binary variable such that l=any STI diagnosis in the past 12 months versus 0=no STI diagnosis in the past 12 months.
Statistical Analyses
Descriptive statistics were obtained for all variables included in the analyses, including the distribution of scale scores. After testing for normality with the Shapiro-Wilk test, we conducted bivariate analyses to examine differences in each of the study variables by sexual identity using Analysis of Variance (ANOVA) and chi-square tests. Differences between continuous variables were foliowed-up with Tukey’s tests. Next, we examined bivariate correlations between stigma from friends, stigma from family, stigma from the general public, and each indicator of HIV risk. Stigma from friends was not significantly associated with either indicator of HIV risk and there were no significant differences by sexual identity. Therefore, we next fit two separate multivariable logistic regression models to examine whether stigma from family or the general public was associated with each indicator of HIV risk, over and above covariates. We then fit separate models to examine whether the associations between stigma from family or the general public and each indicator of HIV risk behavior was moderated by sexual identity, over and above covariates. Finally, significant moderation effects (i.e., as demonstrated by a significant interaction effect between general public stigma and sexual identity) were plotted and examined by means of simple slope tests, using the range of the stigma variable from one standard deviation below and above the mean as outlined by Aiken and West (1991).
Results
Sample Characteristics
In total, 46% (n = 85) self-identified as heterosexual, 25% (n = 46) as gay, 12% (n = 22) as bisexual. Additionally, 17% (n = 32) of the men identified as a different (“other”) sexual identity, such as asexual or unsure/questioning. The majority of the sample (83.8%) self-identified as a member of a racial/ethnic minority group (22.7% Black; 18.4% Latino; 21.6% Asian; and 21.1% Mixed/Other). More than half of the sample reported living in poverty-earning less than $500 a month (60.5%), unstable housing (52.4%), and a history of incarceration in their lifetime (52.4%). Over one-third of the men self-reported an HIV-positive serostatus. The average age of participants was 37.69 (SD = 11.47) and mean length of relationship was 38.28 months (SD = 51.69).
Bivariate Comparisons by Sexual Identity
As shown in Table 1, a greater proportion of individuals who identified as gay (67.4%) and “other” (78.1%) reported earning less than $500 per month compared to heterosexual (50.6%) and bisexual men (59.1%), χ2(3)=8.59, p<0.05. Gay-identified men reported significantly higher relationship stigma from the general public (M= 1.14, SD = 0.69) compared to heterosexually-identified men (M= 0.81, SD = 0.84), F(3, 184)=3.53, p<0.05. Additionally, gay-identified (M= 2.34, SD = 1.65) and bisexually-identified (M= 2.50, SD = 1.00) reported significantly higher stigma from family compared to heterosexual-identified men (M=1.85, SD = 1.10), F(3, 184)=2.58, p< 0.05. There were no significant differences in either indicator of HIV risk by sexual identity.
Table 1.
Sample Characteristics By Sexual Identity (n=185)
| Total Sample |
Heterosexual | Gay | Bisexual | Other | Bivariate Test | |
|---|---|---|---|---|---|---|
| N=185 | n=85 | n=46 | n=22 | n=32 | ||
| N (%) | N (%) | N (%) | N (%) | N (%) | ||
| Race/Ethnicity | n.s. | |||||
| Asian | 40 (21.6) | 20 (23.5) | 10 (21.7) | 4 (18.2) | 6 (18.8) | |
| Black | 42 (22.7) | 18 (21.2) | 12 (26.1) | 5 (22.7) | 7 (21.9) | |
| Latino | 34 (18.4) | 14 (16.5) | 8 (17.4) | 2 (9.1) | 10 (31.3) | |
| White | 30 (16.2) | 13 (15.3) | 7 (15.2) | 7 (31.8) | 3 (9.4) | |
| Mixed/Other | 39 (21.1) | 20 (23.5) | 9 (19.6) | 4 (18.2) | 6 (18.8) | |
| Poverty (Less $500) | 112 (60.5) | 43 (50.6) | 31 (67.4) | 13 (59.1) | 25 (78.1) | χ2(3)=8.59* |
| Unstably Housed | 97 (52.4) | 38 (44.7) | 28 (60.9) | 11 (50.0) | 20 (62.5) | n.s. |
| Incarceration History | 97 (52.4) | 44 (51.8) | 28 (60.9) | 13 (59.1) | 12 (37.5) | n.s. |
| HIV Status | n.s. | |||||
| HIV-positive | 73 (39.5) | 30 (35.3) | 23 (50.0) | 11 (50.0) | 9 (28.1) | |
| HIV-negative | 112 (60.5) | 55 (64.7) | 23 (50.0) | 11 (50.0) | 23 (71.9) | |
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | ||
| Age in Years | 37.69 (11.47) | 36.95 (12.03) | 38.28 (11.70) | 41.41 (8.28) | 36.25 (11.40) | n.s. |
| Relationship Length in Months | 38.28 (51.69) | 34.62 (41.28) | 36.74 (47.13) | 44.32 (54.04) | 46.08 (76.89) | |
| Stigma from Public | 0.99 (0.68) | 0.81 (0.84)a | 1.14 (0.69)b | 0.96 (0.63) | 1.18 (0.75) | F(3, 184)=3.53* |
| Stigma from Family | 2.10(1.24) | 1.85 (1.10)a | 2.34 (1.65)b | 2.50 (1.00)b | 2.17 (0.94) | F (3, 184)=2.58* |
| Stigma from Friends | 2.12 (0.97) | 1.93 (0.88) | 2.31 (1.30) | 2.38 (0.63) | 2.15 (0.79) | n.s. |
| N (%) | N (%) | N (%) | N (%) | N (%) | ||
| Any Drug Use Prior to Sex, Last 30 Days | 80 (43.2) | 34 (40.0) | 24 (52.2) | 8 (36.4) | 14 (43.8) | n.s. |
| Any STI Diagnosis, Last 12 Months | 52 (28.1) | 21 (24.7) | 14 (30.4) | 8 (36.3) | 9 (28.1) | n.s. |
Note: Means having different subscripts differ from each other significantly at the p<0.05 level by Tukey comparison.
p<0.05
Bivariate Associations between Stigma and HIV Risk
Table 2 shows the bivariate correlations between each of the stigma subscales and indicates of HIV risk behavior. Stigma from the general public was positively correlated with stigma from family (r = 0.23, p<0.05), stigma from friends (r = 0.35, p<0.01), reporting drug use before condomless sex in the past 30 days (r = 0.17, p<0.05), and self-reporting any STI diagnosis in the past 12 months (r = 0.27, p<0.01). Stigma from family was positively associated with stigma from friends (r = 0.45, p<0.05), reporting drug use before condomless sex in the past 30 days (r = 0.15, p<0.05), and self-reporting any STI diagnosis in the past 12 months (r = 0.18, p<0.05). There was also a positive correlation between reporting drug use before condomless sex in the past 30 days and self-reporting any STI diagnosis in the past 12 months (r = 0.23, p<0.05). There were no significant bivariate associations between stigma from the general public and either indicator of HIV risk behavior.
Table 2.
Bivariate Correlations Between Stigma and HIV Risk Indicators (n=185)
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. Stigma from Public | -- | ||||
| 2. Stigma from Family | 0.23** | -- | |||
| 3. Stigma from Friends | 0.35** | 0.45** | -- | ||
| 4. Any Drug Use Prior to Sex, Last 30 Days | 0.17* | 0.15* | 0.10 | -- | |
| 5. Any STI Diagnosis, Last 12 Months | 0.27** | 0.18* | 0.07 | .23** | -- |
Note:
p<0.01;
p<0.05
Impact of Sexual Identity in the Association between Stigma and HIV Risk
Table 3 presents the multivariable logistic regression examining the associations between sexual identities, stigma, and the interactions between sexual identities and stigma from two different sources (i.e., family or general public) on engaging in drug use prior to engaging in condomless anal or vaginal sex with a primary or outside partner in the past 30 days. As shown in Model 3a, gay-identified men had an increased odds in engaging in drug use before condomless sex compared to heterosexual men (aOR = 1.70, 1.27, 95% Cl: 1.27, 3.98). Greater levels of relationship stigma from the general public was associated with an increased odds of engaging drug use before condomless sex (aOR = 1.41, 95% Cl: 0.81, 2.45). Model 3b illustrates the multivariable models with the interaction terms. As show in Model 3b, there was a significant interaction between sexual identity (i.e., gay compared to heterosexual) and relationship stigma from the general public on drug use before condomless sex (aOR= 3.42, 95% Cl: 1.73, 5.95). Figure 1 presents the significant interaction illustrating that greater levels of relationship stigma from the general public were associated with an increased odds of drug use prior to condomless sex in the last 30 days for gay-identified men (aOR = 2.03, 95% Cl: 1.52, 3.41), but not for heterosexual-identified men (aOR = 1.95, 95% Cl: 0.30, 2.20).
Table 3.
Multivariable Model Examining Associations between Sexual Identity, Stigma, and Drug Use Prior to Sex in the Last 30 Days Among Cisgender Men Partnered With Transgender Women (n=185)
| Model 3a | Model 3b | |||
|---|---|---|---|---|
| AOR | 95% Cl | AOR | 95% Cl | |
| Sexual Identitya | ||||
| Gay | 1.70 | 1.27, 3.98* | 1.45 | 1.22, 9.43* |
| Bisexual | 1.08 | 0.10, 1.70 | 2.32 | 0.07, 6.23 |
| Other Sexual Identity | 1.00 | 0.03, 3.72 | 1.12 | 0.04, 3.68 |
| Unstable Housing | 1.39 | 0.29. 6.69 | .73 | 0.35, 1.52 |
| History of Incarceration | 3.01 | 0.51,7.79 | 1.95 | 0.91,4.17 |
| Age in Years | 0.98 | 0.91, 1.05 | .97 | 0.94, 1.01 |
| Poverty | 2.61 | 0.52,3.01 | .82 | 0.39, 1.76 |
| Relationship Length | 1.00 | 0.98, 1.02 | 1.00 | 0.99, 1.01 |
| Stigma from Public | 1.67 | 1.49, 2.71* | 1.95 | 1.39, 2.34* |
| Stigma from Family | 1.41 | 0.81, 2.45 | 1.42 | 0.88, 2.29 |
| Public Stigma x Gay | -- | -- | 3.42 | 1.73, 5.95* |
| Public Stigma x Bisexual | -- | -- | 2.89 | 0.43, 9.58 |
| Public Stigma x Other | -- | -- | 2.06 | 0.48, 8.90 |
| Family Stigma x Gay | -- | -- | 0.51 | 0.30, 1.95 |
| Family Stigma x Bisexual | -- | -- | .473 | 0.13, 1.75 |
| Family Stigma x Other | -- | -- | .657 | 0.21, 2.08 |
Note:
Referent=Heterosexual; AOR = Adjusted Odds Ratio; 95% Cl = 95% Confidence Interval
p<0.05
Figure 1.
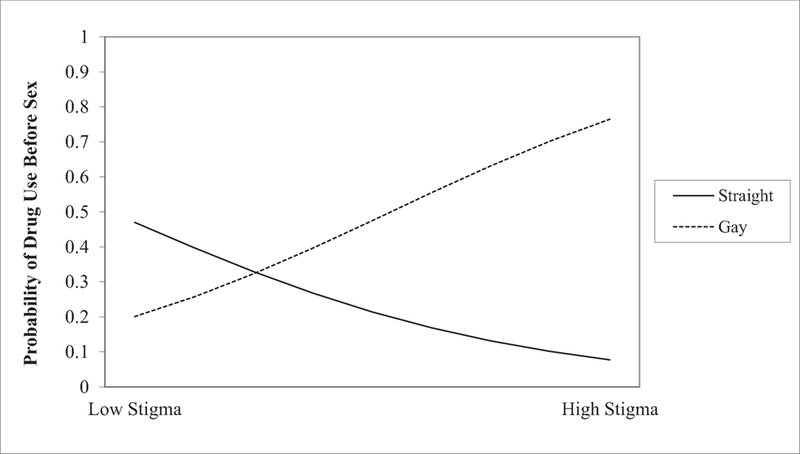
The Moderating Role of Sexual Identity in the Association of Relationship Stigma and Drug Use Prior to Sex in the Last 30 Days
Table 4 presents the multivariable logistic regression examining the associations between sexual identities and relationship stigma on self-reporting any STI diagnosis in the past 12 months, as well as the interactions between sexual identities and relationship stigma from the three different sources on this outcome. As shown in Model 4a, self-identifying as gay was associated with increased odds of reporting any STI diagnosis (aOR= 1.51, 95% Cl: 1.07, 3.95). Reporting unstable housing (aOR = 2.31, 95% Cl: 1.01, 5.27) and having a history of incarceration (aOR = 2.56, 95% Cl: 1.07, 6.14) were each associated with increased odds of reporting any STI diagnosis. Additionally, greater levels of relationship stigma from the general public were associated with increased odd of self-reporting any STI diagnosis (aOR = 2.00, 95% Cl: 1.09, 3.67). Model 4b presents the multivariable model with the interaction terms. There was a significant interaction between self-identifying as gay compared to heterosexual and relationship stigma from the general public on STI diagnosis (aOR= 4.88, 95% Cl: 2.08, 9.55). Figure 2 presents the significant interaction illustrating that the association between greater levels of relationship stigma from the general public were associated with increased odds of self-reporting an STI diagnosis for gay-identified men (aOR= 3.41, 95% Cl: 2.01, 5.05), but not for heterosexual-identified men (aOR= 1.95, 95% Cl: 0.12, 2.04).
Table 4.
Multivariable Model Examining Associations between Sexual Identity, Stigma, and Any STI diagnosis in Past 12 Months Among Cisgender Men Partnered With Transgender Women (n=185)
| Model 4a | Model 4b | |||
|---|---|---|---|---|
| AOR | 95% Cl | AOR | 95% Cl | |
| Sexual Identity | ||||
| Gaya | 1.51 | 1.07, 3.95* | 1.22 | 1.02, 2.20* |
| Bisexual | 1.82 | 0.55, 6.01 | .61 | 0.01, 8.01 |
| Other Sexual Identity | 1.43 | 0.16, 2.18 | 1.64 | 0.07, 3.00 |
| Unstable Housing | 2.31 | 1.01, 5.27* | 1.98 | 0.38,2.52 |
| History of Incarceration | 2.56 | 1.07, 6.14* | 1.93 | 0.34, 2.55 |
| Age in Years | 1.01 | 0.97, 1.04 | 1.02 | 0.98, 1.07 |
| Poverty | 1.00 | 0.43, 2.35 | .64 | 0.23, 1.81 |
| Relationship length in Months | 0.99 | 0.98, 1.00 | 1.00 | 0.99, 1.01 |
| Stigma from the Public | 2.00 | 1.09, 3.67* | 1.54 | 1.12, 2.38* |
| Stigma from Family | 1.02 | 0.73, 1.42 | .76 | 0.38, 1.51 |
| Public Stigma x Gay | -- | -- | 4.88 | 2.08, 9.55* |
| Public Stigma x Bisexual | -- | -- | 8.22 | 0.85,9.54 |
| Public Stigma x Other | -- | -- | .89 | 0.08, 9.78 |
| Family Stigma x Gay | -- | -- | 2.34 | 0.87, 6.26 |
| Family Stigma x Bisexual | -- | -- | .88 | 0.22, 3.59 |
| Family Stigma x Other | -- | -- | .83 | 0.21,3.37 |
Note:
Reference = Heterosexual
AOR = Adjusted Odds Ratio
95% Cl = 95% Confidence Interval
Figure 2.
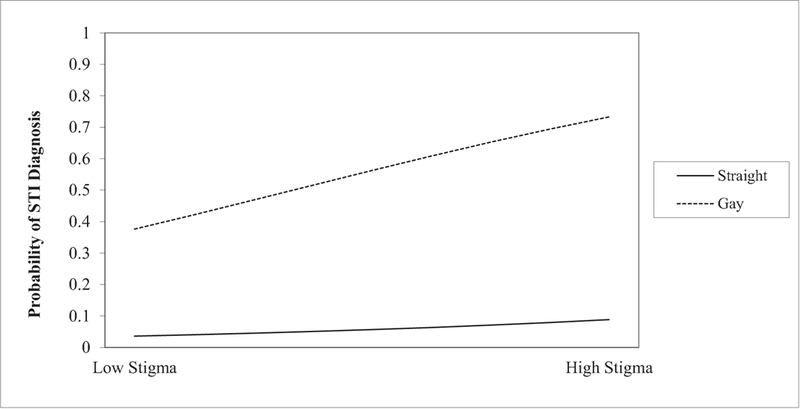
Sexual Identity and Stigma on STI diagnosis in the Past 12 Months
Discussion
Findings from this study further demonstrate the importance of considering relationship stigma from the general public and highlight the complexity in sexual identities and HIV risk factors for cisgender men partnered with trans women (Operario et al., 2008). Study findings suggest the need for nuanced HIV/STI prevention programs and services for these men to amplify the benefits of biomedical prevention strategies. No differences were observed among men of different sexual identities and likelihood of reporting either indicator of HIV risk. However, findings revealed differences by which stigma might produce differential associations with HIV-related risk behaviors for gay-identified men compared with heterosexual-identified men. For gay-identified men, experiencing higher levels of relationship stigma from the general public was associated with higher likelihood of reporting drug use prior to engaging in condomless sex in the past 30 days and having been diagnosed with an STI within the past year. For heterosexual men, relationship stigma from the general public was not significantly associated with likelihood of reporting drug use prior to engaging in condomless sex in the past 30 days and having been diagnosed with an STI within the past year.
Contrary to prior research (Lehmiller & Agnew, 2006; Rosenthal & Starks, 2015), more distal sources of relationship stigma were associated with higher likelihood of reporting both indicators of HIV risk for gay-identified men. Although gay-identified men had significantly higher reports of relationship stigma from both family and the general public compared to heterosexual-identified men, relationship stigma from family was not associated with either indicator of HIV risk in multivariable models. The mechanisms of action that link relationship stigma from the general public and HIV risk are unclear based on the analyses reported here. Qualitative research has illustrated that cisgender men partnered with trans women often feel “isolated” and “alone” due to their stigmatized relationship, and report a consistent fear of violence from others when walking down the streets with their trans women partners (Reisner, Gamarel, Coffey-Esquivel, Drucker, & Mimiaga, 2015). It is plausible that an individual’s relationship with a trans woman may be more intentionally concealed from family and friends, which might mitigate the anticipated forms of proximal stigma for these men. In addition, men might subjectively perceive less of an imminent threat of physical violence from friends and family compared to the risks from the general public, due to their relationship with a trans woman. Stigma deriving from more distal sources - e.g., in general community locations - might be unpredictable and less controllable for cisgender men partnered with trans women.
Notably, gay-identified men who reported high levels of relationship stigma from the general public had an increased odds of reporting HIV risk outcomes, compared with their heterosexual-identified peers. Given the pervasiveness of stigma directed toward trans people (White Hughto et al., 2015), it is plausible that gay-identified men may anticipate or perceive general public stigma deriving from both gay and heterosexual communities as a result of their relationship with a trans woman. As such, gay-identified men may use drugs to cope with stigma, which may reduce inhibitions and decision-making surrounding condom use (Feinstein, Moran, Newcomb, & Mustanski, 2018). Moreover, gay-identified men partnered with trans women may also avoid HIV/STI prevention services due to the real or anticipated fears of stigma from healthcare providers if they were to disclose their partner’s transgender identity.
Our findings regarding greater risk vulnerability among gay-identified male partners of trans women may be also interpreted within discourses of power and privilege. It is possible that heterosexual-identified men may benefit from heterosexual privilege within their partnerships. Heterosexual-identified men may not perceive or be attuned to stigma within their immediate social contexts, particularly in the milieu of cisgender male privilege. It may also be that gay-identified men have a heightened awareness of stigma (i.e., hypervigilance) due to their prior experiences with heterosexism, which leads them to anticipate rejection and mistreatment (e.g., transphobia) due to being partnered with a trans woman (Pachankis, Goldfriend, & Ramrattan, 2008; Quinn & Chaudoir, 2009). Sexual identity is also a concealable stigma; however, a gay- identified man who is partnered with a trans woman may no longer be able to conceal their sexual identity depending on whether their partner “passes” and a concealable stigma may become visible to the general public (Pachankis, 2007). Future research is needed to better understand the ways in which internalized heterosexism and transphobia may interact and contribute to HIV risk.
Cisgender men partnered with trans women have been difficult to identify and engage in HIV/STI prevention services (Reisner et al., 2015). Although the bivariate correlations between relationship stigma and HIV risk were small, our findings suggest that relationship stigma from the general public may be one barrier to reaching some of these men. Although there has been some success in engaging these men in couples-based HIV intervention efforts (Operario et al., 2016), these intervention efforts predated biomedical prevention strategies. Additionally, whereas research with cisgender sexual minority men and trans women has shown the health-protective effects of relationship quality, recent research with cisgender male partners of trans women suggests that relationship quality may not offset the negative health effects of stigma in this group (Gamarel, Sevelius, Reisner et al, 2018). Furthermore, men partnered with trans women may not be interested in engaging in couples-based HIV prevention interventions (Reisner et al., in press). Thus, the effectiveness of biomedical prevention strategies such as PrEP or TasP may require novel approaches for men partnered with trans women. Specifically, research is needed to identify other potential drivers of HIV risk among men partnered with trans women, such as mental health problems. Additionally, our current study findings illustrate the necessity of moving beyond category-based behavioral approaches to HIV prevention, including the use of terminology previously used to describe these men (e.g., men who have sex with trans women, MSTW).
The strong associations between public stigma and health outcomes specifically among gay-identified men point to a concentrated risk context. For these men, engaging in sexual partnerships with trans women might challenge common understandings about sexual orientation and static (versus fluid) patterns of sexual attraction. Indeed, many HIV prevention and intervention efforts are constructed on static, category-based assumptions of sexual orientation, and these men are frequently considered as outliers (Operario et al., 2008). Healthcare and social service providers working with men partnered with trans women should not make assumptions about an individual’s sexual identity or partner’s gender identity. That is, gay-identified men may be fearful of discussing their sexual history with providers who lack cultural humility training in transgender health. It may also be important to consider the ways in which relationship stigma from the general public, as well as other forms of stigma (e.g., racism, heteronormativity), may manifest itself as a barrier to engagement in HIV prevention strategies. Although relationship stigma from family and friends was not associated with HIV risk behaviors in multivariable models, the manifestation of transphobia within families and friends may produce stress and isolation. Prior research has illustrated that men may be concerned that HIV testing counselors might share their personal information regarding being in a relationship with a trans woman, which might be particularly troubling in close knit neighborhoods (Reisner et al., in press). Furthermore, men may experience overt forms of discrimination or anticipate rejection in HIV testing and prevention services. Group interventions may provide support for men partners with trans women, which can be used to assist men in discussing and understanding transphobia and helping them access prevention and other behavioral health services. Future research would also benefit from examining the acceptability and utility of mobile health interventions, such as home testing. Finally, substance use programs may be a viable way to help men partnered with trans women address perceptions of relationship stigma from the general public and link them to HIV prevention services.
Limitations
Several limitations must be noted when interpreting our study findings. First, this study relies on self-report data, which may be subject to social desirability. For example, there may be underreporting of STI diagnoses and future research is warranted to replicate these findings to verify these associations with biomedically-verified STI outcomes. Given the small number of participants who engaged in condomless sex with primary or casual partners by different partner HIV statuses, we collapsed this into one variable, which may underestimate levels of risk. With advances in biomedical prevention strategies (e.g., PrEP and TasP), better risk assessments are needed to more accurately capture HIV risk behavior (Gamarel, Chakravarty, Neilands, et al (2018). Due to the cross-sectional study design, causal or temporal claims cannot be drawn. Given the small number of men who identified as asexual or unsure/questioning, we were unable to examine differences among these groups and combined these identities into a single group. Furthermore, there may have been low power to detect differences between men who identified as bisexual and other; therefore, the results must be interested with caution. Confidence intervals for some of the main findings were large, which possibly reflect sample size limitations or instable effect sizes related to these subgroup distinctions among cisgender men partnered with trans women. Future research with larger sample sizes and using more nuanced approaches to capturing sexual identities, as well as sexual attractions and behaviors, are warranted to better understand the diverse HIV/STI prevention needs of these men.
Additionally, our overarching research question was focused on understanding associations between relationship stigma, sexual identity, and HIV risk; however, cisgender men partnered with trans women are likely to have other salient social identities (e.g., race/ethnicity, class). We also did not include other forms of stigma, such as internalized stigma. Thus, future research guided by an intersectional framework is needed to understand how multiple social identities and varying forms of stigma are related to HIV risk in order to guide effective HIV/STI prevention programs. Moreover, participants were recruited from the San Francisco Bay Area where there have been tremendous strides in social and legal protections for trans women within the past few years and these data were collected between 2008 and 2010; therefore, these findings may not be generalizable to cisgender men partnered with trans women presently or other geographic locales.
Conclusions
Despite these limitations, this study provides a deeper look into the diversity of cisgender men partnered with trans women, a group that has been difficult to link and engage in HIV/STI prevention services. Echoing calls from over a decade ago (Operario et al., 2008; Young & Meyer, 2005), evolving biomedical HIV prevention strategies will only be effective if researchers and practitioners continue to disentangle sexual identity from sexual behavior and refrain from treating all groups as homogenous. HIV prevention research and programming must account for men’s structural, social, and relational context through ensuring cultural humility as part of health care and social service provider training in order to maximize the effectiveness of both behavioral and biomedical HIV prevention strategies, such as PrEP and TasP.
Acknowledgements:
This research was supported by grants from the National Institutes of Health (R01DA018621, R34MH093232; R01MH115765). The first author was also supported (in part) by research education grant (R25MH067127). We gratefully thank the men who participated in the study; staff members; and colleagues Mariko Iwamoto and Colleen Hoff for their valuable contributions to this project. We also thank Dr. Susannah Allison for her support of this work.
References
- Baral SD, Poteat T, Stromdahl S, Wirtz AL, Guadamuz TE, & Beyrer C. (2013). Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infectious Diseases, 13(3), 214–222. [DOI] [PubMed] [Google Scholar]
- Boone MR, Cook SH, & Wilson P. (2013). Substance use and sexual risk behavior in HIV-positive men who have sex with men: an episode-level analysis. AIDS and Behavior, 17(5), 1883–1887. [DOI] [PubMed] [Google Scholar]
- Bradford J, Reisner SL, Honnold JA, & Xavier J. (2013). Experiences of transgender-related discrimination and implications for health: results from the Virginia Transgender Health Initiative Study. American Journal of Public Health, 103(10), 1820–1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Closson EF, Mitty JA, Malone J, Mayer KH, & Mimiaga MJ (2016). Exploring strategies for PrEP adherence and dosing preferences in the context of sexualized recreational drug use among MSM: A qualitative study. AIDS Care, 30(2), 191–198. [DOI] [PubMed] [Google Scholar]
- Feinstein BA, Moran KO, Newcomb ME, & Mustanski B. (2018). Differences in HIV risk behaviors between self-identified gay and bisexual young men who are HIV-negative. Archives of Sexual Behavior, 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamarel KE, Chakravarty D, Neilands TB, Hoff CC, Lykens J, & Darbes LA (2018). Composite Risk for HIV: A new approach towards integrating biomedical and behavioral strategies in couples-based HIV prevention research. AIDS and Behavior, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamarel KE, Reisner SL, Darbes LA, Hoff CC, Chakravarty D, Nemoto T, & Operario D. (2015). Dyadic dynamics of HIV risk among transgender women and their primary male partners: The role of sexual agreement types and motivations. AIDS Care, 28(1), 104–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamarel KE, Reisner SL, Laurenceau J-P, Nemoto T, & Operario D. (2014). Gender minority stress, mental health, and relationship quality: A dyadic investigator of transgender women and their cisgender male partners. Journal of Family Psychology, 28(4), 437–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamarel KE, Sevelius JM, Reisner SL, Sutten Coats C., Nemoto T, & Operario D. (2018). Commitment, interpersonal stigma, and mental health in romatic relationships between transgender women and their cisgender male partners. Journal of Social and Personal Relationships, 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendricks ML, & Testa RJ (2012). A conceptual framework for clinical work with transgender and gender nonconforming clients: An adaptation of the Minority Stress Model. Professional Psychologicial Research Pr, 43(5), 460. [Google Scholar]
- Kalichman SC, Kalichman MO, Cherry C, Hoyt G, Washington C, Grebler T, … Welles B. (2015). Intentional medication non-adherence due to interactive toxicity beliefs among HIV-positive active drug users. Journal of Acquired Immune Deficiency Syndromes, 70(5), 503–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapilashrami A, & Hankivsky O. (2018). Intersectionality and why it matters to global health. Lancet, 391, 2589–2591. [DOI] [PubMed] [Google Scholar]
- Lehmiller JJ, & Agnew CR (2006). Marginalized relationships: The impact of social disapproval on relationship commitment. Personality and Social Psychology Bulletin, 32(1), 40–51. [DOI] [PubMed] [Google Scholar]
- Marrazzo JM, Dombrowski JC, & Mayer KH (2018). Sexually transmitted infections in the era of antiretroviral-based HIV prevention: Priorities for discovery research, implementation science, and community involvement. PLoSMedicine, 15(1), el 002485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melendez RM, & Pinto R. (2007). ‘It’s really a hard life’: love, gender and HIV risk among male-to-female transgender persons. Cultual Health & Sexuality, 9(3), 233–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemoto T, Operario D, Keatley J, & Villegas D. (2004). Social context of HIV risk behaviors among male-to-female transgender of colour. AIDS Care, 16(6), 724–735. [DOI] [PubMed] [Google Scholar]
- Nemoto T, Operario O, Keatley J, Han L, & Soma T. (2004). HIV risk behaviors among male-female transgender persons of color in San Francisco. American Journal of Public Health, 94(1), 1193–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Operario D, Burton J, Underhill K, & Sevelius J. (2008). Men who have sex with transgender women: challenges to category-based HIV prevention. AIDS and Behavior, 12(1), 18–26. [DOI] [PubMed] [Google Scholar]
- Operario D, Gamarel KE, Iwamoto M, Suzuki S, Suico S, Darbes LA, & Nemoto T. (2016). Couples-focused prevention program to reduce HIV risk among transgender women and their primary male partners: Feasibility and promise of the Couples HIV Intervention Program. AIDS and Behavior. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Operario D, Nemoto T, Iwamoto M, & Moore T. (2011a). Risk for HIV and unprotected sexual behavior in male primary partners of transgender women. Archives of Sexual Behavior, 40(6), 1255–1261. [DOI] [PubMed] [Google Scholar]
- Operario D, Nemoto T, Iwamoto M, & Moore T. (2011b). Unprotected sexual behavior and HIV risk in the context of primary partnerships for transgender women. AIDS and Behavior, 15(3), 674–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE (2007). The psychological implications of concealing a stigma: A cognitive-affective behavioral model. Psychological Bulletin, 133(2), 328–345. [DOI] [PubMed] [Google Scholar]
- Pachankis JE, Goldfriend JE, & Ramrattan ME (2008). Extension of the rejection sensitivity construct to the interpersonal functioning of gay men. Journal of Consulting and Clinical Psychology, 76(2), 306–317. [DOI] [PubMed] [Google Scholar]
- Poteat T, German D, & Kerrigan D. (2013). Managing uncertainty: a grounded theory of stigma in transgender health care encounters. Social Science & Medicine, 84, 22–29. [DOI] [PubMed] [Google Scholar]
- Quinn DM, & Chaudoir SR (2009). Living with a concealable stigmatized identity: The impact of anticipated stigma, centrality salience, and cultural stigma on psychological distress and health. Journal of Personality and Social Psychology, 97(4), 634–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Gamarel KE, Coffey-Esquivel J, Drucker M, & Mimiaga MJ (2015). Project LUST: Adapting Couples HIV Counseling and Testing (CHCT) for transgender women and their cisgender male sexual partners. Paper presented at the Harvard University CFAR Conference Presentation, Boston, MA. [Google Scholar]
- Reisner SL, Menino D, Leung K, & Gamarel KE (in press). “Unspoke Agreements”: Perceived acceptability of couples HIV testing and counseling (CHTC) among cisgender men with transgender women partners. AIDS and Behavior. [DOI] [PubMed] [Google Scholar]
- Reisner SL, Mimiaga MJ, Bland S, Mayer KH, Perkovich B, & Safren SA (2009). HIV risk and social networks among male-to-female transgender sex workers in Boston, Massachusetts. J Assoc Nurses AIDS Care, 20(5), 373–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal L, & Starks TJ (2015). Relationship stigma and relationship outcomes in interracial and same-sex relationships: Examination of sources and buffers. Journal of Family Psychology, 29(6), 818–830. [DOI] [PubMed] [Google Scholar]
- White Hughto JM, Reisner SL, & Pachankis JE (2015). Transgender stigma and health: A critical review of stigma determinants, mechanisms, and interventions. Social Science & Medicine, 147, 222–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young RM, & Meyer IH (2005). The trouble with “MSM” and “WSW”: Erasure of the sexual-minority person in public health discourse. American Journal of Public Health, 95, 1144–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu G, Wall MM, Chiasson MA, & Hirshfield S. (2015). Complex drug patterns and associated HIV transmission risk behaviors in an internet sample of U.S. men who have sex with men. Archives of Sexual Behavior, 44(2), 421–428. [DOI] [PMC free article] [PubMed] [Google Scholar]


