Abstract
Problem:
Researchers have prioritized understanding and differentiating the pathophysiologic mechanisms to improve precision in diagnosis and individualization of care, however the experiences of women with labor dystocia have been underexamined
Background:
Management of labor dystocia has been identified as an opportunity for reducing the rate of unnecessary cesarean births and the associated risks to women and their infants. This meta-synthesis explores women’s experiences of labor dystocia to enrich the discussion of care practices and contextualize discussions of shared decision making in what is most meaningful to women.
Questions:
How does prolonged labor influence women’s experience of birth and motherhood? What are women’s experiences with decision-making about labor augmentation during prolonged labor?
Methods:
Sandelowski and Barroso’s meta-synthesis approach was used to analyze primary qualitative studies of women’s experiences of labor dystocia. Through inductive thematic synthesis and reciprocal translation, themes identified in qualitative research, quotations, and coded meaning units were aggregated and interpreted into derived categories and themes.
Findings:
Fourteen qualitative studies were analyzed. Women experienced labor dystocia as a transition from healthy labor to abnormal labor requiring medical support consistent with Transition Theory by Meleis. Six new categories and thirty themes were identified. Each category and theme reflects a distinct component of the experience of labor dystocia.
Discussion/Conclusion:
There is wide variation in the way women experience labor dystocia. Facilitation of the transition from healthy labor to labor dystocia can be supported by a fluid, adaptable method of caring for women in the face of uncertainty and loss of choice.
Keywords: labor dystocia, augmentation, childbirth, qualitative methods, meta-synthesis
Introduction
Recent strategies to improve care of women with prolonged labor have emphasized understanding the underlying pathophysiology, however few researchers have explored the ways that women experience prolonged labor and the care they receive related to it. While deeper understanding of the pathophysiology may lead to the development of innovative care strategies, understanding what is meaningful to women within the experience creates the frame and context that are required to develop a holistic and family-centered plan of care. Meta-synthesis is a systematic approach to synthesizing and reconceptualizing primary qualitative data that we used to “enrich and enlarge” what is known about women’s experiences of labor dystocia beyond what is described in individual qualitative studies1.
Labor dystocia, the medical term for an abnormally slow rate of cervical dilation, is the most common indication for cesarean birth (CB) performed during active labor2. Reducing the CB rate is a public health priority aimed at controlling health care costs and limiting the exposure of women and their infants to possible surgical complications and adverse outcomes in future pregnancies3–5. A variety of methods have been proposed and implemented to reduce CB, yet the rate in the United States remains above the Healthy People 2020 target of 23.9% among low-risk women5,6. Accurate diagnosis of labor dystocia and judicious use of CB for this diagnosis have been proposed by the American College of Obstetricians and Gynecologists and the Society for Maternal and Fetal Medicine as one of the cornerstones of efforts to safely reduce the CB rate3. Oxytocin augmentation of labor is the most common management technique for labor dystocia; however, in randomized controlled trials, oxytocin augmentation has not been shown to reduce the rate of CB or improve outcomes for women and their infants7. Furthermore, oxytocin augmentation is commonly used without proper diagnosis of labor dystocia8,9.
In qualitative and quantitative research, unplanned CB due to labor dystocia is associated with negative birth experiences and difficulties in the transition to motherhood. In a survey of 829 women with spontaneous labor two months after birth, two thirds of women with labor dystocia reported negative experiences of labor and birth that had significant effects on their experience of motherhood10.
Caring for women with prolonged labor is an everyday experience for maternity care providers, however understanding labor dystocia through a qualitative approach reframes the usual discussion of labor management. Qualitative research studies specific phenomenon as situated in unique and particular lived experiences of people. Meta-synthesis is a rigorous approach to reanalyzing qualitative research that can yield insights beyond those found in each single study. It allows for expanded understanding of a phenomenon, confirmation of interpretations, and revelation of new interpretations thus providing novel understandings11–13. The purpose of this study is to explore women’s experiences of prolonged labor through meta-synthesis of the extant qualitative research. The research questions are: How does prolonged labor influence women’s experience of birth and motherhood? What are women’s experiences with decision-making about labor augmentation during prolonged labor?
Methods
A team-based qualitative meta-synthesis was conducted drawing on a well-established toolbox of inductive, deductive, and abductive (that is reasoning and theorizing) strategies. The strategy was reported in accordance with international standards14 and consisted of the following phases. 1. Structured research question and search strategy; 2. Data immersion through quality appraisal15; 3. Thematic synthesis16; and 4. Reciprocal translation11. The Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ) statement informed and framed our methodology14. All included studies were approved by the international review or ethics boards at the researchers’ respective institutions.
Data Sources and Search Strategy
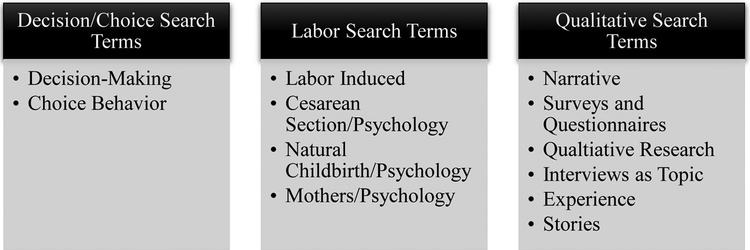
Five databases including PubMed (National Library of Medicine), CINAHL (EBSCO), and PsychINFO (Ovid) were searched using a combination of relevant terms (Figure 1). No date restrictions were applied as older articles may provide insight into changes in the context of care for prolonged labor over time. The database searches were supplemented by hand searching and reviewing the references of relevant studies.
Figure 1:
Search Terms: The search strategy consisted of searching databases using combined search phrases using at least one term in each column.
The Pubmed search was as follows:
1. (decision making) OR (choice behavior) OR (“Decision Making”[Mesh]) OR (“Choice Behavior”[Mesh])
2. (labor indue*) OR (Cesarean) OR (natural birth) OR (“Labor, Induced”[MeSH]) OR (“Cesarean Section/psychology”[MeSH]) OR (“Natural Childbirth/psychology”[MeSH]) OR (“Mothers/psychology”[MeSH])
3. (narrative) OR (“Surveys and Questionnaires”[Mesh]) OR (“Interviews as Topic”[MeSH Terms]) OR (experiences) OR (stories)
4. #1 AND #2 AND #3
Study Selection
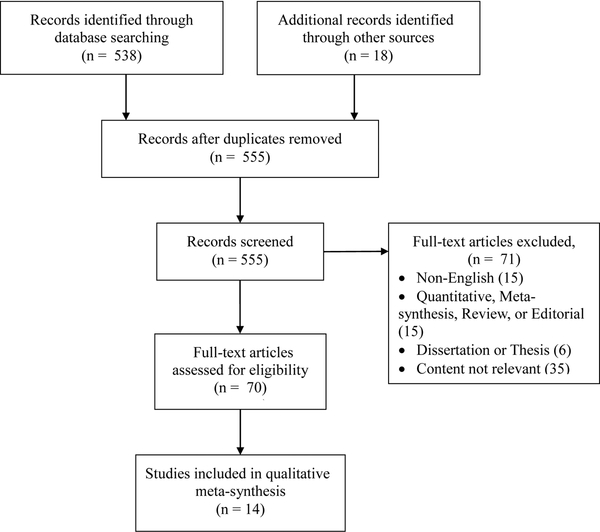
First, duplicates and articles not in English were excluded. The abstract and/or full text of each remaining study was reviewed by the first author, and the article was retained if the inclusion criteria were met: (1) qualitative research, (2) described women’s experiences with prolonged labor, and (3) conducted in the developed world. Articles were excluded if they were (1) quantitative or mixed methods, (2) editorial, review articles, or dissertation theses, (3) not written in English, or (4) focused on the experiences of providers or support persons. Quantitative and mixed methods studies were excluded as these approaches rely on assumptions that lead to a potential loss of contextual detail provided in the qualitative mono-method approach and allowing for richer insight within each study. The process of article selection is summarized in Figure 2.
Figure 2:
PRTSMA Diagram of Article Selection. Adapted from Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Iterns for Systematic Reviews and Meta-Analyses: The PRTSMA Statement. PLoS Med 6(7): e1000097. doi:110.1371/journal.pmed1000097
Data immersion and Quality Appraisal
Each study was read and evaluated separately by the first three authors of our team using the Letts quality appraisal tool, a comprehensive guide for evaluating the rigor of qualitative research for meta-synthesis15. The Letts tool consists of 17 elements including: purpose, background/literature review, study design, sampling, data collection and analysis, overall rigor, and conclusions/implications15. We compared our appraisals and made note of deficiencies in the methods of the reviewed studies; however we recognized that deficient texts still provided important insights, in many cases from marginalized voices13.
Thematic synthesis and reciprocal translation
We used an iterative process to analyze the complete text of the included studies through close reading and interpretation of the raw data to derive themes using thematic synthesis and reciprocal translation12,16. Thematic synthesis provides a novel interpretation of findings to go beyond mere aggregation11–13.
The team immersed themselves in the data by reading and re-reading each article noting the gestalt of the study, important quotations from the data, authors’ interpretations, and the identified themes. Using an inductive approach, the first three authors of our team independently identified meaningful units, assigned a code to each, and developed categories based on patterns emerging across studies16. Meaningful units were identified using a hierarchical strategy based on their relevance to the two research questions regarding the women’s experience of prolonged labor and decision-making about care during prolonged labor. We used reciprocal translation to list in vivo themes and then analyzed the full list abductively for similarities, differences, explanations and emerging patterns12,13. In vivo themes are those that were identified by the researchers within the included studies.
After reviewing the initial three articles, we recognized elements of the Transition Theory by Meleis that emerged from our data17. We incorporated Transition Theory as a theoretical framework for further analyzing the emerging data and used the concepts and relations from Transition Theory to guide the deductive process of reframing the integrated interpretation of the data13. Our own constructed categories and subthemes were developed based on the codes, in vivo themes, authors’ interpretations, and quotations from the included studies13,18,19. Our constructed themes were supported by the full text which contextualizes participant quotes.
Transition theory is a middle-range nursing theory that describes the process of transitions in health and illness. Transition theory consists of six interrelated components (types and patterns of transitions, properties of transition experiences, facilitating & inhibiting conditions, process indicators, outcome indicators, and nursing therapeutics) each with numerus sub-themes:
- Nature of Transitions
- Types: Developmental, Situational, Health/Illness, Organizational
- Patterns: Single, Multiple, Sequential, Simultaneous, Related, Unrelated
- Properties: Awareness, Engagement, Change and Difference, Transition Time Span, Critical Points and Events
- Transition Conditions: Facilitators & Inhibitors
- Personal: Meanings, Cultural beliefs & attitudes, Socioeconomic Status, Preparation & Knowledge
- Community
- Society
- Patterns of Response
- Process Indicators: Feeling Connected, Interacting, Location and Being Situated, Developing Confidence and Coping
- Outcome Indicators: Mastery, Fluid Integrative Identities
Nursing Therapeutics
Results
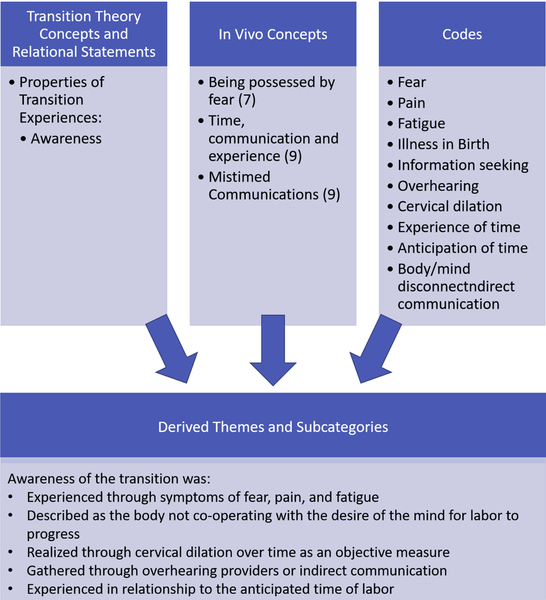
Fourteen articles met inclusion criteria. In aggregate, interviews from 233 women across 7 countries (Australia, England, Ireland, Canada, the United States, Sweden, and Switzerland) were included. The designs of the included studies varied including exploratory descriptive, descriptive qualitative, grounded theory, feminist critical, narrative, interpretive phenomenological, constant comparative, and participatory action. The methods consisted mostly of in-depth interviews that were either semi-structured or open; one research group conducted focus groups. Table 1 (supplemental material) provides characteristics of the included studies. The framework of Transition Theory provided a structure for identifying the components of the experience of transition into abnormal labor and articulating the relationships between components. The concepts and relational statements of Transition Theory contributed to the development of six derived themes with 3–7 subthemes each. An example of the process of synthesizing the concepts of the Transition Theory, in vivo themes, and our own codes is provided in Figure 3. Several components of the Transition Theory were found to be particularly relevant to understanding women’s experiences of prolonged labor including recognizing multiple, related transitions occurring simultaneously, the role of personal, community, and social conditions in the development of expectations, the importance of awareness of the transition as a critical event, loss of choice as a fundamental change affecting the transition, and positive and negative indicators of coping as key process indicators.
Figure 3:
Example of the derivation of themes and subcategories from Transition Theory, In Vivo Themes (those named in the articles), and Codes.
Prolonged labor was experienced as a transition from health, well-being, and the expectation of a natural birth to distress, illness, and the reality of a medical delivery. The process of this transition unfolded consistently with Transition Theory through expectations developed prenatally, marked by the woman becoming aware of the transition and a loss of previously available choice. Coping with the transition varies among women, but several indicators were identified that support positive or negative coping.
1. Transition from anticipated natural birth to medical delivery
Women experience prolonged labor as a transition from anticipated natural birth to medical delivery. Most of the participants desired and/or planned for as natural a birth as possible and received intervention due to prolonged labor.
I have had this basic attitude that it should all be natural[laughs]. I didn’t want any intervention. I had the opinion that this was something the body would manage in its own way and in the best way. There is a reason for the body to do as it does, so I said “No thanks” [to the drip] in the beginning - - - - - She asks me 3 or 4 times and eventually I agreed and it was a good decision20.
This transition was superimposed on the transition to motherhood, whichwas disrupted by prolonged labor21–24. Nystedt et al. and Armstrong and Kenyon interpreted the transition as entering the “sick role” characterized by extreme suffering24,25
‘Then I thought I was going to die, I was in so much pain. My labour pains were incredibly strong’. For many women, the transition was complicated by the necessity to transfer care locations or providers from home or birth center to the hospital and from midwifery care to obstetric care and a deviation from their birth plan23,24,26.
2. Expectations for labor and birth.
Many of the researchers discussed the ways that women developed expectations for labor and birth and emphasized the importance of these expectations in the experience of prolonged labor. Expectations were developed through the development of knowledge, preparation for labor, and birth planning21,22,25,27,28. Education and birth planning were emphasized by providers prenatally and by the health care system as a whole which assumes that women will be active, informed consumers making choices about the kinds of birth they have and taking responsibility for making plans.
I wanted to have a birth experience that I had planned so for me to be informed meant being involved in the decisions about the birth I wanted…28.
Expectations were framed by stories from family, friends and the media27,29. Fear of pain and the unknown dominated some women’s preparation for labor and birth22. For some women, particularly those who were socially disadvantaged, prenatal information was inadequate for participating in decision-making during labor23,27,28. Expectations for labor were rarely realized especially for first time mothers22,30.
And the worst thing is that I thought I was prepared. Like I really did. I had, you know, read up and read books, and taken the prenatal classes and surrounded myself with people that I hoped would help21.
3. Awareness of the transition.
Women became aware of the abnormality of their labor through symptoms of fear, pain, and fatigue20,24,25,30. Some researchers and participants described a disconnect between the body and mind with a perception that the body was not co-operating with the desire of the mind for labor to progress20,25.
I felt that I had forgotten that I was having a baby. For a long time, I actually forgot what I was doing there. I was so consumed in the end by the pain or by what was even going on, by everything… At that point, I was so tired too…22.
Some researchers stated that women realized their prolonged labor through their provider’s report of change in cervical dilation over time which served as an objective rather than subjective measure20,26,31. Women spoke positively about objective communication about progress in cervical dilation that allowed for clarity in framing the experience of prolonged labor and recognizing the need for additional care20,31.
We got to eight centimetres ok and they examined me again and part of the cervix wasn’t dilating further although most of it was but part of it wasn’t and so they said ‘ok, we’ll give it another couple of hours’, so we gave it another couple of hours and then examined again, it was still the same25.
At times, women became aware of prolonged labor by gathering information through overhearing providers or indirect communication20,31.
I was just waiting. And I, but I kind of knew. They were worried about the baby’s heart rate and this is me again sussing out what is going on from listening to their conversations… I realize I was gathering a whole lot of information from what people were saying that wasn’t being directed tome31.
Prolonged labor was experienced in relationship to the anticipated time of labor31.
I remember my mom, she had gone 40 hours with her first, with my brother, and this was 32, something like that. And I had said, “Can’t I go 8 more hours?” And he looked at me and he said, “Well, you’re only at 3 [centimeters dilatation], do you really think 8 more hours is going to do any-thing?” And I said, “Oh, okay, I guess not.” He made me feel like the patient, unknowing, that I didn’t have anything, I just felt like it was out of my hands32.
4. Loss of choice.
Loss of choice was experienced as a change from focusing on birth preferences to decisions being driven by clinical necessity20,24,25,33. This change was the essence of the experience of decision-making during prolonged labor. It was described in the in vivo themes: “coping with diminishing choice”25, “there came a point at which choice receded”25, “dialectical birth process”20, and “balancing natural and medical delivery”24).
I did feel that I had control over what was going on, what was happening, up until the point where they said we’ve got to get baby out and, at that point, I just thought ‘well whatever these guys think they need to do now’25.
For some women the loss of choice was related to being caught up in the physical experience of pain and fatigue in labor20,33. Some women described a lack of choice related to perceived increases in risk, especially a threat to the health of the baby21,23,25–28,30. Some researchers critiqued the lack of choice on a theoretical level, arguing that oxytocin augmentation is not the only management option for labor dystocia, while others presented augmentation of labor as a medical necessity.
You can only have so much [choice], I mean I cannot refuse a c-section because [of] the risk of my life and my baby’s life25.
Some women described being excluded from the process of decision-making, which was often associated with dissatisfaction with care provided21,23,25,28,29. Dependency on trusted care providers was identified in most of the papers and was primarily described as a positive experience especially in the presence of extreme pain and fear21,24–26,29.
I felt that I needed help to survive it all, that I couldn’t make it myself and that was what made me feel vulnerable, I think. Then I allowed myself to accept that I needed someone to help me with this24.
Several researchers questioned the fundamental concept of choice in labor21,25,27,30. One described the process of informed consent as tokenistic and disruptive to women who were suffering from pain, exhaustion, and the effects of pain medications25. Happel-Parkins and Azim interpreted choices as false dilemmas in which the provider offered an alternative, but unacceptable choice, as a rhetorical strategy to manipulate women into accepting augmentation27. These false dilemmas were often framed as exaggerated risks to the health of the baby27. Malacrida and Boulton21 contextualized choice within the conflicting frameworks of medicalized delivery and natural birth claiming that both perspectives disciplined the body, inserting a concept of choice where there is in fact no ability to exert one’s will.
5. Indicators of positive coping with the process of transition.
Positive coping with the process of the transition was closely linked with feeling connected to partners, families, and other support persons20,26,27,31. Coping relied heavily on feeling safe and valued through positive interactions of caring by providers20,23,24,28,30. VandeVusse found that women expressed more positive emotions, such as feeling confident, appreciative, and honored, when decision-making was increasingly shared32.
I had read a lot on my own and we discussed many things during labour so I had great confidence in the midwife and I never had any reason to question or comment on the intervention made by the midwife. I sensed that she knew what she was doing. I was in good hands and saw no reason to ask for alternatives29.
One indicator of positive coping and reconciliation was the acceptance of the necessity of medical intervention and the relief provided by treatment20,24,25,31,32. There was variation in the way that women wanted to engage in decision making including the desire to be very involved, wanting to be informed but relying on trusted providers to make decisions, and withdrawing completely from participation20,26,29,32. Women frequently reported relief in giving birth to a healthy baby21,29,33. Coping was indicated by high levels of satisfaction with the experience21,29,32. Having support in reconciling expectations and the actual experience supported coping20–22.
6. Indicators of negative coping.
Dissatisfaction and difficulty reconciling was often related to negative interactions with care providers, especially when women felt excluded from decision-making21,23,24,27,31. VandeVusse found that when decision-making was contested, women were more likely to feel devalued, angry, punished, and unsettled32. This was accentuated in socially disadvantaged women who reported feeling “silenced into conforming” by providers who were unavailable or who were perceived as judging the women23. Self-blame for the outcome was described as a factor that inhibited reconciliation21.
That’s always the question, right? Would this have happened that way if I had been able to do this, this and this differently, right? Maybe if I hadn’t had to lay in bed so much [due to fetal monitoring] and could have moved around … Lots of questions like that21.
Responsibility for the outcome of birth was described as a consequence of an emphasis on choice and education in preparing for birth21. Poor coping and reconciliation were associated with low satisfaction with the birth experience21,29,32. Some women experienced trauma in prolonged labor10,22,25,27.
Discussion
The experience of labor dystocia was characterized by a process of transition that women went through from natural birth to medical delivery. It was influenced by awareness, expectations, and positive and negative coping to reconciliation. Across the qualitative studies, “loss of choice” emerges as one of the core experiences of prolonged labor. Much of the distress identified by women hinges upon this loss, which was alternatively characterized in the included studies with the in vivo themes: loss of control24, loss of the role of patient/consumer and adoption of the sick role21, and loss of mind/body coordination20. Loss of choice can be a natural result of fatigue, pain, and the overwhelming physiologic shifts of labor, but it can also be constructed or exacerbated by the care environment.
A tempting response to the distress caused by interrupted autonomy would be to focus interventions on removing the contingencies that result in loss of choice. Indeed, many of the researchers situated their studies in care environments that idealized patient choice in this way. Women were encouraged to educate themselves prenatally and to develop birth plans as a means of enacting control during labor. However, even within this paradigm, several researchers described a disconnect between prenatal providers who encouraged birth planning and intrapartum providers who ignored or ridiculed the documents and plans once the “realities” of labor were at hand21. For women, this disconnect resulted, at best, in experiencing prenatal planning as tokenistic or meaningless, and worse, in a sense of guilt or failure when their bodies failed to conform to what their well-informed minds has planned.
It is possible to conceive of an alternative paradigm for care during prolonged labor in which walking with women rather than patient autonomy is emphasized. Such “walking with” consists of participation in practices such as attention, communication, and accompaniment34. These practices disrupt the somewhat fictional paradigm of a choice-driven birth experience and re-orient the relationship between women and their providers toward one of shared attention toward the mind/body dyad34. Rather than representing labor and birth as a consumer experience, the preparation for and process of labor and birth become a practice in orientation to the inherent pain, loss of control, temporary loss of synchronicity of body and mind, and contingencies along the fluid continuum of health and disease34.
We resist formulaic take-home points from this analysis; accompaniment cannot be distilled into “steps” or checklists. The fluidity and inherently random nature of labor makes it ill-suited to rigid pre-planning. Instead, providers may turn towards ways of caring for women throughout the embodied experience of pregnancy, labor, and birth that emphasize attention and accompaniment.
Strengths and Limitations
Our findings are strengthened by our rigorous methodology that was informed by current standards for qualitative synthesis12,14,18. All four components of trustworthiness (credibility, transferability, dependability, and confirmability) were addressed thoroughly15,35. Credibility was established through triangulation with existing theories, expert knowledge, and consistency among the included studies. Our large sample size from seven different countries contributes to transferability of the findings. We developed an audit trail to demonstrate dependability through meeting notes and the reciprocal translation table (Supplemental Material, Table 2). Confirmability, the neutral stance of the authors, was developed through reflective processes and the diverse team that contributed to critical evaluation of content and methods. Our team included members with little preconceived ideas about the content who took a neutral stance to the analysis as well as clinical experts who provided depth to the analysis and rich contextualization of the themes.
Our metasynthesis was restricted by limitations and deficiencies of the included studies. Most of the researchers assumed that augmentation of labor was necessary to “manage” prolonged labor. This assumption is understandable given that augmentation is ubiquitous. However, given the evidence that oxytocin augmentation is ineffective to prevent CBs, an understanding of the experience of prolonged labor separated from augmentation and the pervasive medical care environment would aid in the reimagining of labor care. Researchers of the included studies emphasized the understanding of individual women’s experiences in small, homogenous samples. None of the researchers suggested generalizing findings across populations. Generally, minority women of lower socio-economic-educational backgrounds were underrepresented. The small sample of each study was mitigated somewhat by synthesizing the findings across studies to improve transferability of findings.
Conclusion
In our meta-synthesis, we described the wide range of experiences of women with prolonged labor. In addition to gaining appreciation for the most common experiences, we also found that a small number of women suffer very significantly from labor dystocia and describe a complete withdrawal from the experience. This response is typical of a reaction to trauma and suggests that labor dystocia may be traumatic for some women. Future research is needed to target this extreme response in order to identify ways of preventing, recognizing, and supporting healing of birth trauma related to labor dystocia.
Differences within the experience of prolonged labor highlight the importance of individualizing care rather than relying on one-size-fits-all guidelines. Differences in experience may reflect differences in the underlying pathophysiology and support future research to understand different classifications of prolonged labor. Within the questionable background of widespread oxytocin augmentation, our findings detail what is meaningful to women to guide future research in developing evidence for caring for women with prolonged labor and should inform providers to rethink care of women both in preparing for and coping with labor with an emphasis on the fluid, dynamic and variable nature of labor.
Supplementary Material
Table 1. Description of Reviewed Studies
Table 2. Reciprocal Translation Table
Significance
Labor dystocia is the most common reason for cesarean birth during active labor and innovation in care for women with prolonged labor is essential for reducing the rate of unnecessary cesarean births.
What is Already Known
Researchers are currently refining the diagnosis and management of labor dystocia from a physiologic perspective to target different pathophysiologic causes of labor dystocia.
What this Paper Adds
A thorough description of the varied experiences of women with prolonged labor to contextualize care strategies in what is most meaningful to women. Loss of choice emerged as a core experience of prolonged labor. Care strategies emphasizing accompanying women through the unknowns of labor and birth may be more effective than those merely focusing on patient autonomy.
Acknowledgements and Disclosures
Contributors include Lilian Hoffecker, a health sciences librarian who supported our literature search, Dr. Nancy Lowe who provided writing assistance and editorial support, and Dr. Mark Kissler who provided proofreading and writing assistance. There has been no funding support for this project and there are no disclosures.
Funding Acknowledgement: Research reported in this abstract was supported by National Institute of Nursing Research of the National Institutes of Health under award number FN31NR018582–01. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Ethical Statement
Not applicable in this qualitative metasynthesis.
References
- 1.Thorne S Metasynthetic Madness: What Kind of Monster Have We Created? Qual Health Res 2017; 27(1): 3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang J, Troendle J, Reddy UM, et al. Contemporary cesarean delivery practice in the United States. American Journal of Obstetrics & Gynecology 2010; 203(4): 326 e1–e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Caughey AB, Cahill AG, Guise JM, Rouse DJ. Safe prevention of the primary cesarean delivery. American Journal of Obstetrics and Gynecology 2014; 210(3): 179–93. [DOI] [PubMed] [Google Scholar]
- 4.Main E, Morton C, Hopkins D, Giuliani G, Melsop K, Gould J. Cesarean deliveries, outcomes, and opportunities for change in California: Toward a public agenda for maternity care safety and quality. California White Paper 2011. [Google Scholar]
- 5.Martin J, Hamilton B, Osterman M, SC C, TJ M. National Vital Statistic Reports: Births Final Data for 2015. National Vital Statistics Reports 2017; 66(1): 1–70. [PubMed] [Google Scholar]
- 6.Office of Disease Prevention and Health Promotion. Healthy people 2020: Maternal infant and child health. 2017.
- 7.Bugg GJ, Siddiqui F, Thornton JG. Oxytocin versus no treatment or delayed treatment for slow progress in the first stage of spontaneous labour. Cochrane Database of Systematic Reviews 2013; (6): CD007123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neal JL, Lowe NK, Patrick TE, Cabbage LA, Corwin EJ. What is the slowest-yet-normal cervical dilation rate among nulliparous women with spontaneous labor onset? J Obstet Gynecol Neonatal Nurs 2010; 39(4): 361–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neal JL, Lowe NK, Phillippi JC, et al. Likelihood of cesarean delivery after applying leading active labor diagnostic guidelines. Birth 2017; 44(2): 128–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nystedt A, Högberg U, Lundman B. Women’s experiences of becoming a mother after prolonged labour. Journal of advanced nursing 2008; 63(3): 250–8. [DOI] [PubMed] [Google Scholar]
- 11.Noblit GW, Hare RD. Meta-Ethnography: Synthesizing the Qualitative Studies: Sage University Publications; 1988. [Google Scholar]
- 12.Thorne S, Jensen L, Kearney MH, Noblit G, Sandelowski M. Qualitative metasynthesis: reflections on methodological orientation and ideological agenda. Qualitative health research 2004; 14(10): 1342–65. [DOI] [PubMed] [Google Scholar]
- 13.Sandelowski M, Barroso J. Toward a metasynthesis of qualitative findings on motherhood in HIV-positive women. Research in nursing & health 2003; 26(2): 153–70. [DOI] [PubMed] [Google Scholar]
- 14.Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol 2012; 12: 181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Letts I, Wilkins S, Law M, Stewart D, Bosch J, Westmorland M. Guidelines for Critical Review Form: Qualitative Studies (Version 2.0). 2007.
- 16.Thomas DR. A general inductive approach for analyzing qualitative evaluation data. American journal of evaluation 2006; 27(2): 237–46. [Google Scholar]
- 17.Meleis AI, Sawyer LM, Im E-O, Hilfinger Messias DK, Schumacher K. Experiencing Transitions: An Emerging Middle-Range Theory. Advances in Nursing Science 2000; 23(1): 12–28. [DOI] [PubMed] [Google Scholar]
- 18.Goins RT, Jones J, Schure M, et al. Older adults’ perceptions of mobility: a metasynthesis of qualitative studies. The Gerontologist 2014; 55(6): 929–42. [DOI] [PubMed] [Google Scholar]
- 19.Messer LH, Johnson R, Driscoll KA, Jones J. Best friend or spy: a qualitative meta-synthesis on the impact of continuous glucose monitoring on life with Type 1 diabetes. Diabet Med 2018; 35(4): 409–18. [DOI] [PubMed] [Google Scholar]
- 20.Kjaergaard H, Foldgast AM, Dykes A-K. Experiences of non-progressive and augmented labour among nulliparous women: a qualitative interview study in a Grounded Theory approach. BMC pregnancy and childbirth 2007; 7(1): 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Malacrida C, Boulton T. The best laid plans? Women’s choices, expectations and experiences in childbirth. Health: 2014; 18(1): 41–59. [DOI] [PubMed] [Google Scholar]
- 22.Dahlen HG, Barclay L, Homer CS. ‘Reacting to the unknown’: experiencing the first birth at home or in hospital in Australia. Midwifery 2010; 26(4): 415–23. [DOI] [PubMed] [Google Scholar]
- 23.Ebert L, Bellchambers H, Ferguson A, Browne J. Socially disadvantaged women’s views of barriers to feeling safe to engage in decision-making in maternity care. Women and Birth 2014; 27(2): 132–7. [DOI] [PubMed] [Google Scholar]
- 24.Nystedt A, Hogberg U, Lundman B. Some Swedish women’s experiences of prolonged labour. Midwifery 2006; 22(1): 56–65. [DOI] [PubMed] [Google Scholar]
- 25.Armstrong N, Kenyon S. When choice becomes limited: Women’s experiences of delay in labour. Health: 2017; 21(2): 223–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meyer Y, Frank F, Muntwyler FS, Fleming V, Pehlke-Milde J. Decision-making in Swiss home-like childbirth: A grounded theory study. Women and Birth 2017; 30(6): e272–e80. [DOI] [PubMed] [Google Scholar]
- 27.Happel-Parkins A, Azim KA. At pains to consent: A narrative inquiry into women’s attempts of natural childbirth. Women and Birth 2016; 29(4): 310–20. [DOI] [PubMed] [Google Scholar]
- 28.O’Brien D, Butler MM, Casey M. A participatory action research study exploring women’s understandings of the concept of informed choice during pregnancy and childbirth in Ireland. Midwifery 2017; 46: 1–7. [DOI] [PubMed] [Google Scholar]
- 29.Blix-Lindström S, Christensson K, Johansson E. Women’s satisfaction with decision-making related to augmentation of labour. Midwifery 2004; 20(1): 104–12. [DOI] [PubMed] [Google Scholar]
- 30.Hauck Y, Fenwick J, Downie J, Butt J. The influence of childbirth expectations on Western Australian women’s perceptions of their birth experience. Midwifery 2007; 23(3): 235–47. [DOI] [PubMed] [Google Scholar]
- 31.Maher J Progressing through labour and delivery: Birth time and women’s experiences Women’s Studies International Forum; 2008: Elsevier; 2008. p. 129–37. [Google Scholar]
- 32.VandeVusse L Decision making in analyses of women’s birth stories. Birth 1999; 26(1): 43–50. [DOI] [PubMed] [Google Scholar]
- 33.Carlton T, Callister LC, Stoneman E. Decision making in laboring women: ethical issues for perinatal nurses. J Perinat Neonatal Nurs 2005; 19(2): 145–54. [DOI] [PubMed] [Google Scholar]
- 34.Mol A The Logic of Care: Health and the Problem of Patient Choice. New York, NY: Routledge; 2008. [Google Scholar]
- 35.Guba EG, Lincoln YS. Fourth generation evaluation: Sage; 1989. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table 1. Description of Reviewed Studies
Table 2. Reciprocal Translation Table