Abstract
Purpose
To report a case of refractory open angle glaucoma (POAG) in an osteogenesis imperfecta patient who was successfully treated with combination microinvasive glaucoma surgery: combined kahook blade goniotomy and ciliary sulcus suprachoroidal microtube insertion.
Observation
A 57-year-old woman with a history of osteoporosis, breast cancer, osteogenesis imperfecta, with uncontrolled POAG in right more than left. Anterior segment examination revealed thin blue sclera, the optic nerve examination revealed glaucomatous cupping with cup to disc ration of 0.9 in right and 0.7 in left. Her IOP on six (6) medications was 26 mmHg in the right eye. After discussion of the risks and benefits, she agreed to undergo combined kahook blade goniotomy and ciliary sulcus suprachoroidal microtube insertion surgery to lower her intraocular pressure. Her IOP at 6 months follow up was 13 in the right eye and a decrease number of medications from six (6) to three.
Conclusion and importance
Patients with OI have homogenously thinner sclera and conjunctiva which pose a challenge to traditional subconjunctival surgical methods. Combined kahook blade goniotomy and ciliary sulcus suprachoroidal microtube insertion surgery are bleb sparing operations that enhances aqueous outflow to the aqueous veins and supraciliary space to lower intraocular pressure.
Keywords: Combined microinvasive surgery, Osteogenesis imperfecta, Refractory open angle glaucoma, Glaucoma, Kahook blade goniotomy, Suprachoroidal microtube
Highlights
-
•
Combined microinvasive surgery.
-
•
Osteogenesis imperfecta.
-
•
Refractory open angle glaucoma.
-
•
Glaucoma, kahook blade goniotomy.
-
•
Suprachoroidal microtube.
1. Introduction
Osteogenesis imperfercta (OI) is a rare autosomally inherited connective tissue disease characterized by bone fractures, deafness, blue sclera and thin corneas. The most common ocular findings include glaucoma, myopia, decreased ocular rigidity, keratoconus, corneal opacity, small corneal diameter and congenital Bowman's layer agenesis. Patients with OI have homogenously thinner corneas and sclera.1 In a cohort study of 23 kids with OI, the central corneal thickness (CCT) was significantly lower compared to age-matched controls (459.5 ± 24.6; control group 543.6 ± 21.4 p < 0.001).2 A defect in COL1A1 is known to be associated with different forms of glaucoma in patients with OI. Although a detailed genotype-phenotype correlation has not been established, it is known that patient's with COL1A1 mutations develop glaucoma early with and without signs of OI.3
Glaucoma is the second leading cause of blindness globally affecting about 64.3 million people.4 Glaucoma is a progressive optic neuropathy with management mostly aimed at reducing the intraocular pressure (IOP). IOP reduction can be achieved via medications, laser techniques and surgery. Increasing rates of patient non-compliance to ocular anti-hypertensives,5 has led most glaucoma specialist to the use earlier microinvasive glaucoma surgery (MIGS). MIGS have been reported to have high safety profiles. A four year outcome of combined MIGS, two iStent (Trabecular stents) and one iStent Supra (suprachoroidal stent) and post-operative prostaglandin in refractory glaucoma showed significant reduction in IOP and decrease number of medications.6 The istent supra MIGS is a nice bleb sparing glaucoma procedure however, it is not commercially available and in the US the istent can be injected only at the time of cataract surgery. Literature on glaucoma surgery in patients with osteogenesis imperfecta and glaucoma is rare.
We present a rare and unique case of a 57-year-old woman with OI and uncontrolled moderate POAG who underwent Kahook blade Goniotomy7,8 and intra-scleral- ciliary sulcus suprachoroidal microtube9 shunt tube insertion to lower IOP.
2. Case
A 57-year-old woman with a history of osteoporosis, breast cancer in remission status post left mastectomy (2010), osteogenesis imperfecta, and pseudophakia status post cataract surgery and selective laser trabeculoplasty in both eyes presented with uncontrolled primary open angle glaucoma (POAG) in right more than the left for second opinion. Patient reported no drug allergies and no significant family medical history. She is a lifetime non-smoker and a social drinker. Her ocular medications included: brimonidine/timolol (0.2%/0.5%) twice a day in both eyes, bimatoprost 0.01% at bedtime in both eyes, brinzolamide 1% in the right eye twice a day and once a day in the left eye, phospholine iodide 1.25% right eye once a day and acetazolamide 500mg once a day. Other medications included duloxetine Hcl 20mg per day, alendronate 70mg per week, calcium1200mg per day and Vit D3 2000 IU per day.
Her best corrected visual acuity was 20/25 in both eyes. External exam was significant for pupils with 2mm + afferent pupillary defect (APD) in the right eye. Slit lamp exam revealed scleral thinning with bluish hue in both eyes. There was corneal thinning on pachymetry (410 μm right eye, 409μm left eye) with 1+ guttata on right cornea and 2+ left corneal guttata. The iris was normal, and the anterior chamber was deep and quiet in both eyes. Patient had clear posterior capsules and well positioned intraocular lens (PCIOL) implants in both eyes. Gonioscopy revealed Schaeffer grade IV open angles with 1–2+trabecular meshwork pigment. The anterior chamber was deep and quiet. The intraocular pressures were 26 mmHg in the right eye and 14 mmHg in the left eye. Optic nerve examination revealed a cup to disc ratio of 0.9 in the right eye with superior notching of the neuroretinal rim and a cup to disc ratio in the left eye of 0.7. The retina and macula were flat with no hemorrhages, pigmentary changes or edema bilaterally. The retinal vessels were normal. The retina periphery was flat with no detachments and/or holes. Visual field examination revealed inferior loss near fixation in the right eye with a VFI of 65% and a full visual field in the let eye with VFI of 99%.
After discussion of the risks and benefits, the patient decided to undergo combined kahook blade goniotomy and ciliary sulcus-suprachoroidal glaucoma microtube insertion in the right eye to lower the intraocular pressure.
2.1. Surgical devices
The Kahook Dual Blade (KDB; New World Medical, CA, USA) is a single-use ophthalmic knife designed to perform goniotomy. KDB is used to produce a single incision in the trabecular meshwork behind Schwalbe's line. Goniotomy using KDB has been described elsewhere.8,10
A sterile medical grade silicone microtube (Tube extender, New World Medical) was surgically placed to drain aqueous from the posterior chamber ciliary sulcus of the eye to the suprachoroidal space (SCS).9 The sterile medical grade silicone tube (Tube extender, New World Medical) can be cut to any size length (7–10 mm) depending on the size of the eye and length of insertion into the ciliary sulcus and SCS. The tubing has a 300 mm internal tube diameter and 600 mm external diameter.
2.2. Surgical procedure
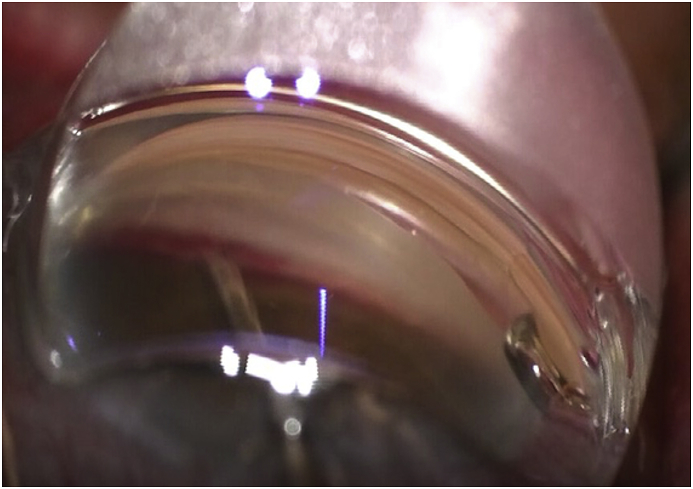
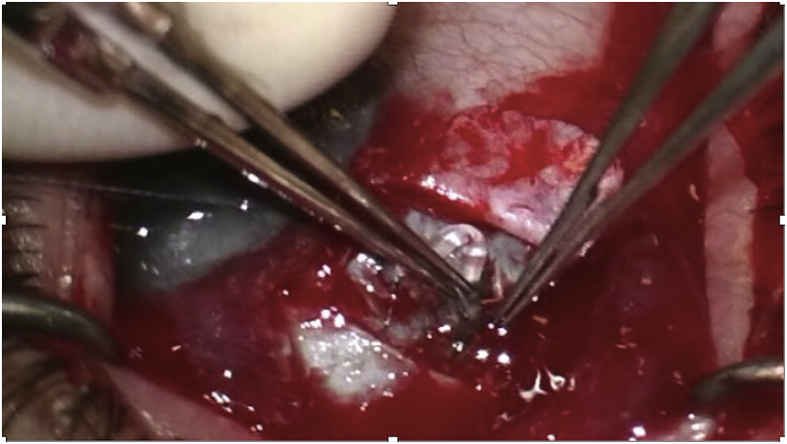
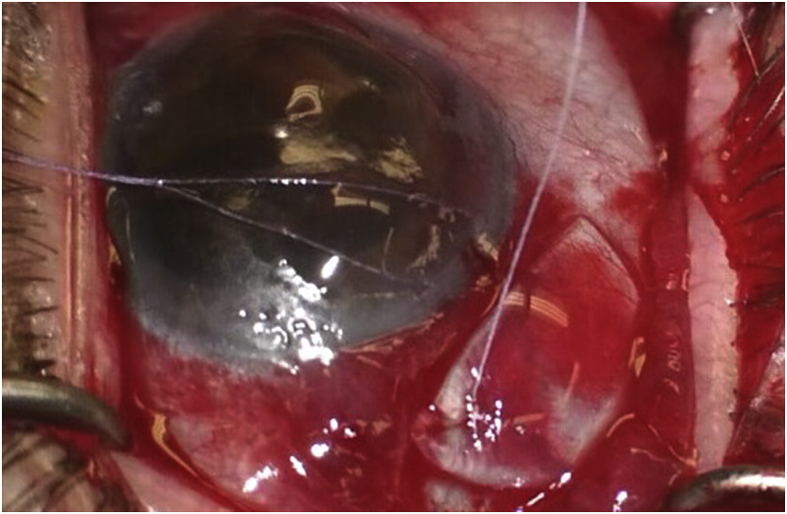
Informed consent was obtained and witnessed. The options of glaucoma surgery procedures were discussed with the patient. The benefits and risks were discussed in detail, including the risk of complete sight loss. The patients agreed to the risks and benefits of the procedure. The patient was taken to the operating room and attached to the usual monitoring devices by an anesthesiologist. The eye was prepped and draped in a sterile fashion for ophthalmic procedure. The patient received a retrobulbar block with a mixture of 2% lidocaine and 0.75% marcaine by anesthesia. A lid speculum was placed in the eye. A 15 blade was used to make a paracentesis. Viscoelastic was placed in the anterior chamber. A 2mm keratome was used to make a self-sealing incision in the clear cornea temporally. The patient's head was tilted 45 degrees away from the surgeon, and the microscope was tilted approximately 45 degrees towards the surgeon in a suitable position to visualize the trabecular meshwork with a direct goniolens (Katena). The Kahook blade was inserted via the clear corneal temporal incision and was then used to perform a 4-clock hour goniotomy (Fig. 1). Blood reflux was noted into the angle. The patient's head and the microscope were restored to the normal position. A 10-0 nylon suture was used to close the corneal wound. Serrated conjunctival forceps and Wescott scissors were used to perform an inferotemporal conjunctival peritomy. Hemostasis was maintained with wet-field cautery. A supplemental block of a mixture of 2% lidocaine and 0.75% marcaine was given. 0.12 forceps and crescent blade were used to make a 4 mm × 4 mm partial thickness scleral flap inferotemporally. 0.12 forceps and 15 blade was used to make a paracentesis site superiorly. Viscoelastic was used to make the anterior chamber deep and create a space within the inferotemporal ciliary sulcus. A 23-gauge needle was used to make an incision 2 mm from the limbus inferotemporally into the ciliary sulcus. The tube extender was cut with a 45-degree bevel. The tube was inserted into the inferotemporal ciliary sulcus with the bevel facing the intraocular lens. A 10-0 nylon suture was used to secure the tube to the sclera. 0.12 forceps and a crescent blade was used to make an incision at the base of the scleral flap into the suprachoroidal space approximately 6mm from the limbus. The silicone tubing was cut and inserted into the suprachoroidal space (Fig. 2). The scleral flap was closed with three interrupted 8-0 vicryl sutures. A corneal patch (Visiongraft) was sutured over the scleral flap and tube (Fig. 3). The conjunctiva was closed with two interrupted 8-0 running locking sutures. Intracameral Vigamox was given. A subconjunctival Kenalog was given. The patient tolerated the procedure without any complications and was taken to the recovery room in a stable condition.
Fig. 1.
Kahook goniotomy in right eye.
Fig. 2.
Microtube being inserted into the suprachoroidal space.
Fig. 3.
Corneal patch being placed over tube and sclera.
2.3. Results
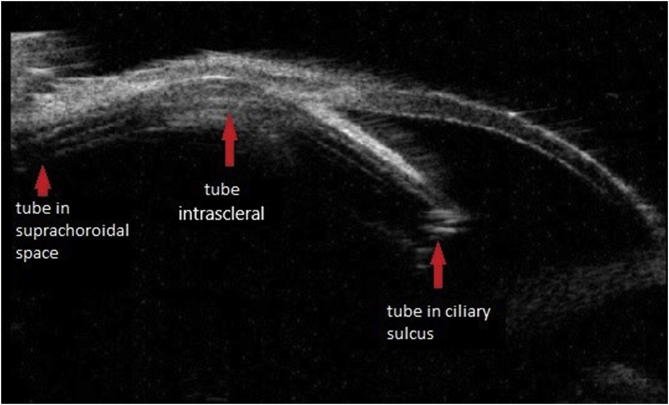
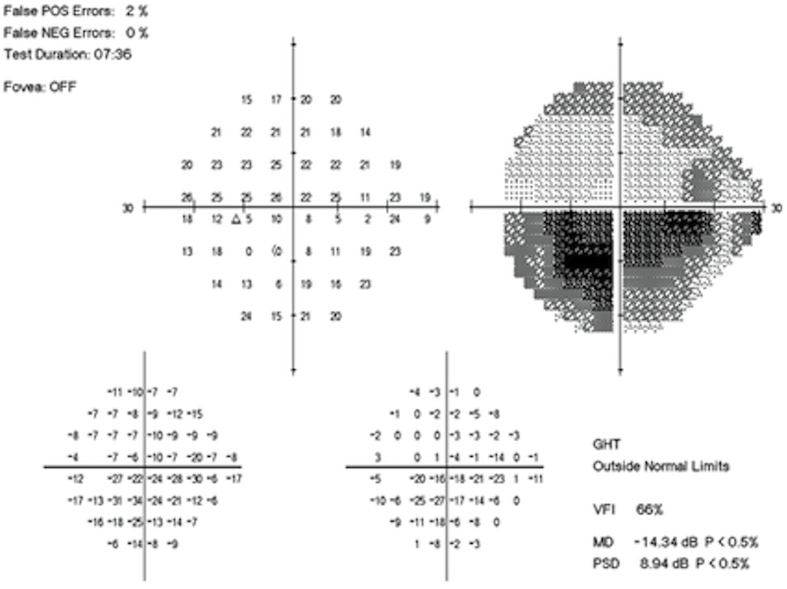
Post operatively the average IOP of the right eye over 6 months was 12.5 mmHg (ranging from 10 to 16 mmHg) on brimonidine/timolol (0.2%/0.5%) one drop in both eyes twice a day and brinzolamide 1% in both eyes twice a day. This represented 50% drop in intraocular pressure (IOP of 13 at the 6 months follow up visit). There was also a decrease in medications from six (6) to three (3) at 6 months. The microtube was well positioned in the ciliary sulcus (Fig. 4). The intrascleral portion was well positioned and was covered by the corneal patch to the suprachoroidal space. (Fig. 5). Ultrasound biomicroscopy (UBM) showed tube in the ciliary sulcus, intraciliary and suprachoroidal space (Fig. 6). Her best corrected visual acuity (BCVA) was 20/20 in the right eye. VFI performed 6 months after the procedure showed a stable VFI of 66% in the right eye (Fig. 7) and 99% in the left eye and mean deviation of −14.34 OD and −5.66 OS. Her best corrected visual acuity (BCVA) was 20/20 in the right eye.
Fig. 4.
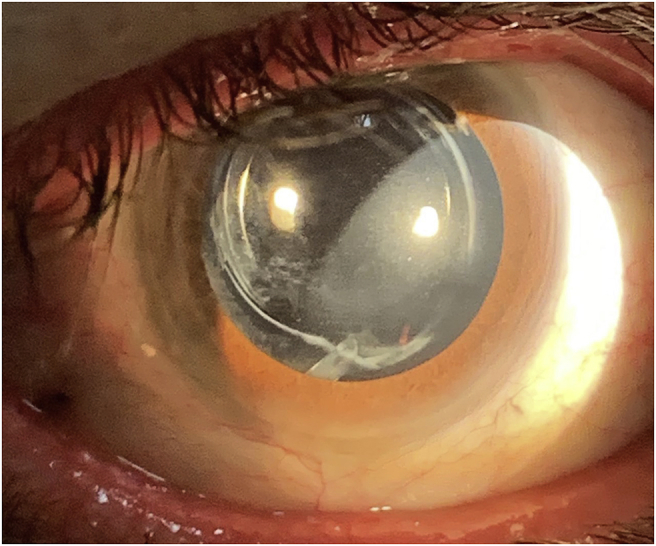
Microtube in ciliary sulcus.
Fig. 5.
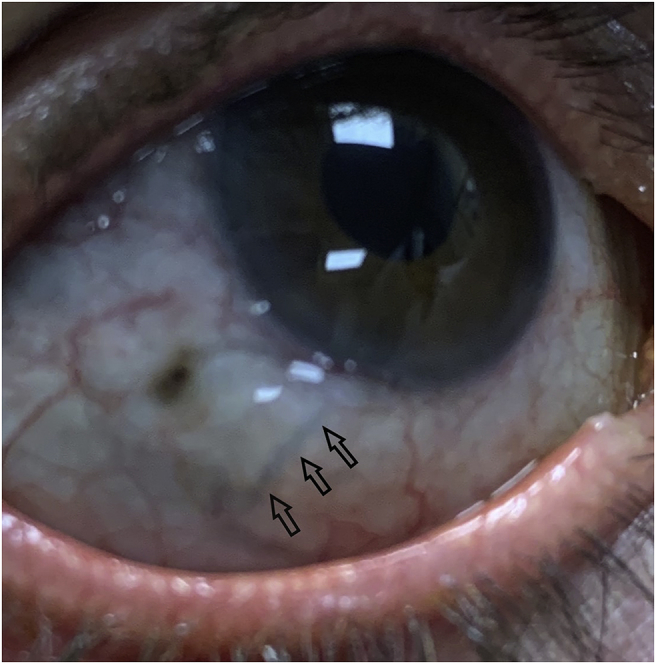
Blue thin sclera in OI with SC tube and arrows pointing to corneal patch. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Fig. 6.
UBM after SCS microtube insertion.
Fig. 7.
VFT at 6months right eye.
3. Discussion
This patient was successfully treated with a novel combined microinvasive glaucoma surgical technique of Kahook blade goniotomy and ciliary sulcus suprachoroidal microtube. Bothe techniques have been described individually by Greenwood et (Goniotomy using kahook blade) and Laroche et al. (Intra-Scleral Ciliary Sulcus Suprachoroidal Microtube).8,9 This is the first report of both of these procedures combined. The procedure is not only affordable but has high safety profile with no bleb formation comparable to other micro stent glaucoma surgeries. Our patient tolerated the procedure well with decreased IOP and reduced number of ocular hypertensive medications. IOP dropped from 26 to 13 (50% decrease) in 6 months and the number of medications decreased from six (6) to three (3) (50% decrease) post-surgery. The visual field has remained stable (VFI 66% from 65% on presentation).
The advent of MIGS has provided a better treatment option albeit its minimal safety concern in patients with primary open angle glaucoma.11 In patients with mild to moderate glaucoma, goniotomy has been described in literature to aid aqueous humor egress to collector channels. It has been an effective technique to reduce the intraocular pressure as well as the number of ocular antihypertensive medications. Combined microinvasive glaucoma surgery in osteogenesis imperfecta may have a better safety profile than traditional trabeculectomy. However, there is special considerations and risks assessment due to their phenotypic thin sclera. In this population, glaucoma usually presents early1 and the risks of vision loss can be exacerbated due to their earlier presentation. It therefore is imperative that surgeons take into account the long-term efficacy of the procedure(s) as wells as their safety profile and the need for aggressive control of elevated IOPs. Trabeculotomy presents a life long risk of endophthalmitis hence the need to avoid if possible in this population.
Ciliary sulcus suprachoroidal microtube surgery has been previously described by Laroche et al. in which the CS-SCS tube drained the aqueous from the anterior chamber to the suprachoroidal space and into the scleral veins resulting in IOP reduction in four (4) patients with minimal complications.9 They reported this bleb-less procedure had less corneal edema compared to patients who have undergone Cypass since the tube is not in anterior chamber and positioned in the ciliary sulcus. The gold standard glaucoma surgery, trabeculectomy, comes with complications such as hyphema, anterior chamber flattening, hypotonic maculopathy and choroidal detachment.12 These complications can be self-resolving or require secondary procedures. This patient underwent a combined kahook blade goniotomy with CS-SCS microtube tube insertion, that has a similar safety profiles compared to other MIGS and was able to obtain similar IOP in the low teens similar to trabeculectomy with reduction in the number of ocular hypertensive medications.
The rationale for the combination MIGS was to achieve lower IOPs using techniques that target different aqueous drainage sites. Our patient had undergone selective laser trabeculoplasty (SLT) in both eyes and we decided against trabeculectomy due to its safety concerns. By combining two bleb-less MIGS, we hoped to accomplish a lower IOP which individual MIGS cannot while keeping the safety profiles of each MIGS. Although literature is sparse on benefits of combination MIGS, Ferguson et al. demonstrated its efficacy by comparing patients who underwent trabecular microbypass stent, (iStent; Glaukos), cataract surgery and electro photocoagulation (ECP) with patients who underwent iStent and cataract surgery without ECP. The group that received ECP in addition had IOP reduction of 7.14 mmHg in 12 months without additional complications compared to 4.48 mmHg in the patients who did not undergo ECP.13 During the six month follow up, our patient had 50% reduction in IOP on three medications attesting to the efficacy of combined MIGS in refractory glaucoma.
The goniotomy and suprachoroidal microtube shunt procedure can also be performed with at 23 gauge cystotome and less expensive sterile silicone tubing in resource poor areas. In our patient, the scleral patch was reinforced to prevent extrusion of the microtube due to the thin sclera. This however is not necessary in patients with normal sclera. The tube was visualized behind the iris and inside the anterior chamber (Fig. 5). Patient's IOP decreased from 26 mmHg on six medications to 13 mmHg on three (3) medications during the 6-month period. The CS-SCS tube was able to drain aqueous from the anterior chamber to the suprachoroidal space.
4. Conclusion
In summary, we describe the use of kahook blade goniotomy and ciliary sulcus suprachoroidal microtube shunt surgical techniques in pseudophakic OI patient with thin corneas. This combined MIGS method can safely reduce IOP and decrease the number of medications without a bleb while stabilizing the visual field.
Limitations of this case study includes the need to see longer term success and further evaluation in a greater number of patients.
Patient consent
The patient consented to publication of this case in writing.
Funding
No funding or grant support.
Disclosures
DL. - Ivantis, Aerie, Bauch and Lomb.
GN. - No disclosures.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
Acknowledgements
The staff at Advance Eye Care of New York for their support
References
- 1.Magalhaes O.A., Rohenkohl H.C., de Souza L.T., Schuler-Faccini L., Felix T.M. Collagen I defect corneal profiles in osteogenesis imperfecta. Cornea. 2018;37(12):1561–1565. doi: 10.1097/ICO.0000000000001764. [DOI] [PubMed] [Google Scholar]
- 2.Evereklioglu C., Madenci E., Bayazit Y.A., Yilmaz K., Balat A., Bekir N.A. Central corneal thickness is lower in osteogenesis imperfecta and negatively correlates with the presence of blue sclera. Ophthalmic Physiol Optic. 2002;22(6):511–515. doi: 10.1046/j.1475-1313.2002.00062.x. [DOI] [PubMed] [Google Scholar]
- 3.Mauri L., Uebe S., Sticht H. Expanding the clinical spectrum of COL1A1 mutations in different forms of glaucoma. Orphanet J Rare Dis. 2016;11(1):108. doi: 10.1186/s13023-016-0495-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Resnikoff S., Pascolini D., Etya'ale D. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82(11):844–851. [PMC free article] [PubMed] [Google Scholar]
- 5.Okeke C.O., Quigley H.A., Jampel H.D. Adherence with topical glaucoma medication monitored electronically the Travatan Dosing Aid study. Ophthalmology. 2009;116(2):191–199. doi: 10.1016/j.ophtha.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 6.Myers J.S., Masood I., Hornbeak D.M. Prospective evaluation of two iStent((R)) trabecular stents, one iStent supra((R)) suprachoroidal stent, and postoperative prostaglandin in refractory glaucoma: 4-year outcomes. Adv Ther. 2018;35(3):395–407. doi: 10.1007/s12325-018-0666-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berdahl J.P., Gallardo M.J., ElMallah M.K. Six-month outcomes of goniotomy performed with the kahook dual blade as a stand-alone glaucoma procedure. Adv Ther. 2018;35(11):2093–2102. doi: 10.1007/s12325-018-0803-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Greenwood M.D., Seibold L.K., Radcliffe N.M. Goniotomy with a single-use dual blade: short-term results. J Cataract Refract Surg. 2017;43(9):1197–1201. doi: 10.1016/j.jcrs.2017.06.046. [DOI] [PubMed] [Google Scholar]
- 9.Laroche D., Anugo D., Ng C., Ishikawa H. Intra-scleral ciliary sulcus suprachoroidal microtube: making supraciliary glaucoma surgery affordable. J Natl Med Assoc. 2019;111(4):427–435. doi: 10.1016/j.jnma.2019.02.003. [DOI] [PubMed] [Google Scholar]
- 10.Sieck E.G., Capitena Young C.E., Epstein R.S. Refractive outcomes among glaucoma patients undergoing phacoemulsification cataract extraction with and without Kahook Dual Blade goniotomy. Eye Vis (Lond). 2019;6:28. doi: 10.1186/s40662-019-0153-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salimi A., Lapointe J., Harasymowycz P. One-year outcomes of second-generation trabecular micro-bypass stents (iStent inject) implantation with cataract surgery in different glaucoma subtypes and severities. Ophthalmol Ther. 2019;8(4):563–575. doi: 10.1007/s40123-019-00214-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arimura S., Miyake S., Iwasaki K. Randomised clinical trial for postoperative complications after ex-PRESS implantation versus trabeculectomy with 2-year follow-up. Sci Rep. 2018;8(1):16168. doi: 10.1038/s41598-018-34627-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferguson T.J., Swan R., Sudhagoni R., Berdahl J.P. Microbypass stent implantation with cataract extraction and endocyclophotocoagulation versus microbypass stent with cataract extraction for glaucoma. J Cataract Refract Surg. 2017;43(3):377–382. doi: 10.1016/j.jcrs.2016.12.020. [DOI] [PubMed] [Google Scholar]