Abstract
Purpose
To report a case of a woman who had Ehlers Danlos syndrome who developed a bullous retinal detachment.
Observations
A 33-year-old Caucasian woman presented with 1-day history of floaters and photopsia. Patient had extensive scleral ectasia. Scleral buckle could not be performed due the severity of the ectasia. Patient had a vitrectomy and subsequently had multiple re-detachments with sclera ruptures during the retinal detachment repairs. Patient required a 360-degree scleral patch graft to prevent scleral ruptures during the vitrectomy. Patient has a stable flat report 7 months post-op with vision of 1/60.
Conclusions and importance
This is the first case report of a patient requiring a 360-degree scleral patch graft. This option should be considered to assist in preventing scleral ruptures, intraoperatively and post operatively in patient who have an increased risk of scleral rupture, such as patients with connective tissue disorders.
Keywords: Ehlers Danlos syndrome, EDS, Retinal detachment, Scleral ectasia, Scleral patch graft, Scleral rupture
1. Introduction
Ehlers Danlos syndrome (EDS) is a hereditary connective tissue disorder caused by defective collagen synthesis with variable clinical manifestations affecting primarily the skin, ligaments, joints, blood vessels and internal organs.1 It is known that EDS has a prevalence of 1:5000.1 Collagen proteins make up the extracellular matrix providing the structure to broadly all tissues and organs in the body.2 Ocular complications associated with Ehlers syndrome include epicanthal folds, blue sclera, retinal detachment, ectopia lentis, glaucoma and angioid streaks.3
To date, there has being no reports of a patient requiring a 360-degree scleral patch graft in order to assist in retinal reattachment in a patient. Scleral patch grafts are performed primarily for iatrogenic surgical complications.4,5 Various types of tissue have been used for sclera graft including live tissue known as auto scleral flaps, allograft material such as lyophilized donor scleral material, an autologous grafting with fascia lata or periostium and cadaveric tissue known as cadaveric sclera grafts.6, 7, 8
2. Case presentation
A 33-year-old Caucasian woman presented to the emergency department with a 1-day history of floaters in her right eye. The patient was a known Ehlers Danlos syndrome patient, type 6A. The patient was a high myope, −14 diopters in both eyes. Visual acuity on presentation was hand movements in her right eye and 6/9 with correction in the left eye. Fundus examination showed superior temporal macula on bullous retinal detachment with mild vitreous haemorrhage.
Initially, it was decided a scleral buckle and cryotherapy was the best form of treatment for the patient. This primary procedure was decided against and pneumatic retinopexy with 20% SF6 gas was performed, after discovering extensive scleral ectasia which was worse in the superotemporal quadrant on examination in the operating theatre. During the pneumatic retinopexy procedure, a spontaneous scleral perforation occurred in the superior temporal quadrant, on gentle manipulation in the operating room. Tissue glue with 7/0 vicryl was used to repair the fragile sclera. After the pneumatic retinopexy, cryotherapy was used to seal the round holes in the superotemporal retina which were difficult to identify due to the background pale appearance of retina and the choroid. Five days later the patient presented with macula off retinal detachment. Donor sclera was ordered and the patient underwent elective scleral graft, 20-gauge(G) vitrectomy, cryotherapy and SF6 20% gas under general anaesthetic. 25G sutureless vitrectomy was attempted at first but due to repeated breakdown of the scleral entry wound, the surgery was converted to 20G vitrectomy. Donor scleral graft was sutured to the patient's sclera 360° with 7-0 vicryl mixed with 9-0 nylon sutures up to muscle insertions 4–5mm from the limbus, shown in Fig. 1. Posteriorly the donor scleral graft was left without suturing, due to extreme thinning of the sclera and posteriorly it was glued. Tissue glue was used during this first vitrectomy which was later found to have caused some blanching of the patient's sclera in that localized area without serious consequences. Vitreous syneresis and posterior vitreous detachment was observed during this vitrectomy. The donor scleral shell was trimmed anteriorly and along the course of four recti to leave room for the movements of the recti muscles. The extensive scleral ectasia in all quadrants of the globe, shown in Fig. 2., lead to an inability to clearly identify the retinal breaks.
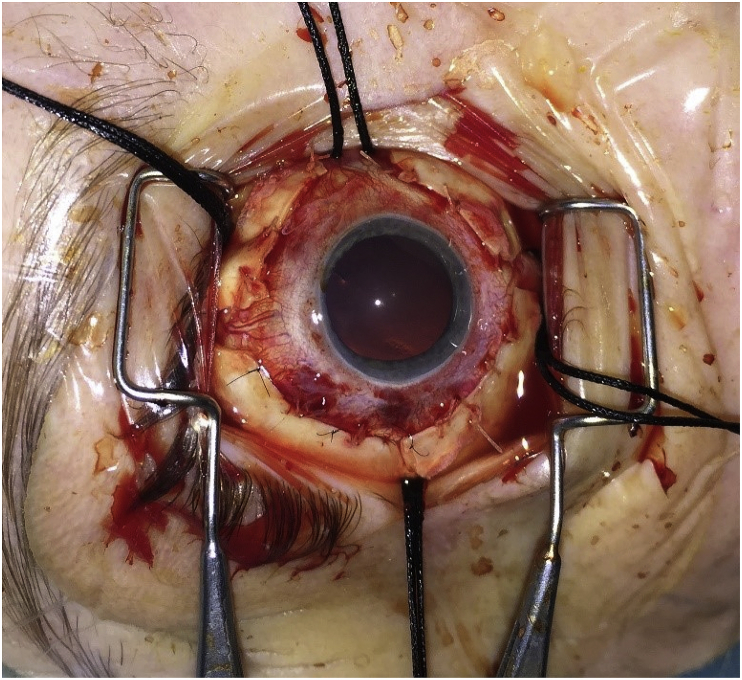
Fig. 1.
This post-operative picture shows the 360 scleral patch grafts supporting the sclera between the recti muscles. The graft was attached posteriorly to cover the equator with tissue glue.
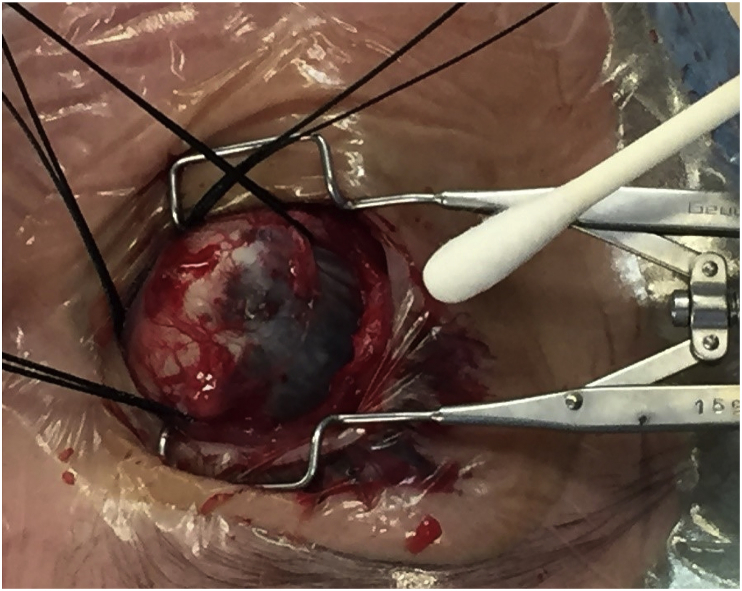
Fig. 2.
This intraoperative picture shows the extent of sclera ectasia.
The patient had a recurrence of retinal detachment inferiorly one-month post operatively. The patient was also found to have scleral thinning at the previous vitrectomy port sites just anterior to the edge of donor scleral graft. Operative findings were new retinal breaks inferiorly with grade 2 proliferative vitreoretinopathy (PVR) inferotemporal and nasally. A further donor scleral patch graft was planned and the donor scleral graft was sutured along the limbus and to the previous donor scleral graft, along with a 20G vitrectomy, endolaser, and silicone oil placement. The procedure was complicated with repeat breakdown of wounds for the scleral ports underneath the donor scleral graft. The patient remained stable in the immediate post-operative period. However, the patient was found to have further recurrence of retinal detachment six weeks later. The woman's visual acuity was 1/60 unaided improved to 6/36 with pin hole in the right eye.
Further surgery was performed including removal of silicone oil, 20G vitrectomy, lens aspiration, intraocular lens insertion, membrane peel, nasal and inferior 120-degree retinectomy, endolaser, donor scleral graft repair and reinsertion of silicone oil under general anaesthetic. The patient did well following the procedure and the oil was left in situ for 18-month when it was removed. The patient is now 7 months post removal of silicone oil and the patient has vision of 1/60. The retina was flat and shown in Fig. 3.
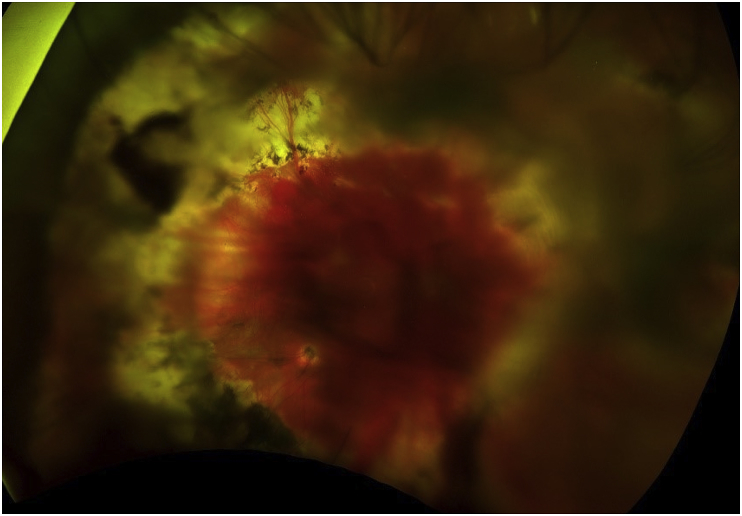
Fig. 3.
This is an image of the right fundus. The poor quality was due to the posterior capsule opacification. This patient was reluctant for laser to correct this.
In our case we had to use scleral graft in all quadrants due to extensive scleral ectasia and recurrent breakdown of sclerotomies. The donor sclera was sutured to slightly healthier looking host sclera, 4mm from the limbus all around. Dexamethasone and chloramphenicol eye drops were used to help with post -op inflammation and to decrease the risk of infection. This was a very difficult case due to a hypopigmented fundus (see Fig. 4), repeated breakdown of sclera resulting in cheese wiring and extension of scleral wounds.
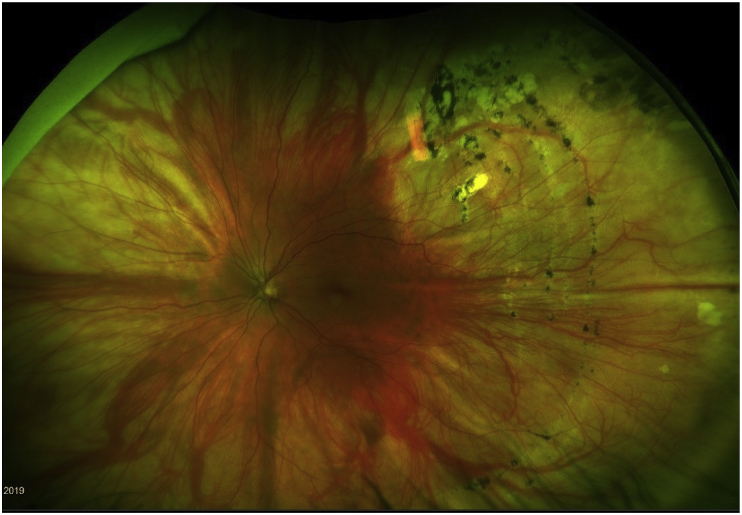
Fig. 4.
This is image of the left fundus. .
3. Discussion
Rupture of sclera is a less common but more serious complication of retinal detachment surgery and is associated with unfavourable anatomic and visual outcomes. The initial globe integrity can be restored by suturing the ruptured site or by placement of a patch graft or a silicone explant over the lacerated area.9 Tissue glue may be used to facilitate the restoration of the globe. Difficulty reattaching the retina and the high risk of PVR developing postoperatively compromise the final outcomes in these patients. Tabandeh H. et al. reports that the retina was successfully attached in 50% of the patients who had scleral rupture develop during the retinal detachment surgery compared with 97% of the eyes that did not have scleral rupture.10 Visual outcomes were similarly compromised.
Patients who develop a retinal detachment with EDS are known to have poor visual prognosis given the abnormalities in collagen concerning membranes adjacent with the retina.3 Given the rarity of the condition there are very few reported cases of retinal detachment repair requiring scleral grafts. Meticulous and thorough examination of the sclera should be evaluated prior to undertaking any intervention to determine which procedure would be the best management for the patient, be it a vitrectomy, pneumatic retinopexy or scleral buckle.
This case report gives a viable option for a patient who may have a severe degree of scleral ectasia, where a scleral buckle would not be an option due to the fear of rupture of the scleral and the inability to suture the band to the sclera. A sutureless vitrectomy(25G) may be difficult to be performed due to leakage of the sclerotomies during the vitrectomy.
4. Conclusion
Ehlers Danlos is a rare but important disease that can present to ophthalmologists. When surgical intervention is required on these individuals great care should be taken to examine the sclera in detail and a scleral patch graft should be considered when planning vitreoretinal surgery.
Patient consent
Consent to publish this case report has been obtained from the patient in writing.
Funding
No funding or grant support.
Conflicts of interest
The following authors have no financial disclosures: (S.W., Z.I.)
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Acknowledgements
None.
References
- 1.Mao J.-R., Bristow J. The Ehlers-Danlos syndrome: on beyond collagens. J Clin Investig. 2001;107(9):1063–1069. doi: 10.1172/JCI12881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ricard-Blum S. The collagen family. Cold Spring Harbor Perspect Biol .3(1):a004978-a. [DOI] [PMC free article] [PubMed]
- 3.Beighton P. Serious ophthalmological complications in the Ehlers-Danlos syndrome. Br J Ophthalmol. 1970;54(4):263–268. doi: 10.1136/bjo.54.4.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hodge C., Sutton G., Devasahayam R. The use of donor scleral patch in ophthalmic surgery. Cell Tissue Bank. 2017;18(1):119–128. doi: 10.1007/s10561-016-9603-4. [DOI] [PubMed] [Google Scholar]
- 5.Alkharashi M., Dagi A.F., Dagi L.R. Pericardial patch graft repair of severe localized scleral thinning encountered during strabismus surgery. J Am Assoc Pediatr Ophthalmol Strabismus. 2017;21(2) doi: 10.1016/j.jaapos.2017.03.010. 156-.e1. [DOI] [PubMed] [Google Scholar]
- 6.Chechelnitsky M., Mannis M.J., Chu T.G. Scleromalacia after retinal detachment surgery. Am J Ophthalmol. 1995;119(6):803–804. doi: 10.1016/s0002-9394(14)72792-8. [DOI] [PubMed] [Google Scholar]
- 7.Mauriello J.A., Jr., Pokorny K. Use of split-thickness dermal grafts to repair corneal and scleral defects--a study of 10 patients. Br J Ophthalmol. 1993;77(6):327–331. doi: 10.1136/bjo.77.6.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barman M., Finger P.T., Milman T. Scleral patch grafts in the management of uveal and ocular surface tumors. Ophthalmology. 2012;119(12):2631–2636. doi: 10.1016/j.ophtha.2012.06.024. [DOI] [PubMed] [Google Scholar]
- 9.Bodanowitz S., Hesse L., Postgens H., Kroll P. [Retinal detachment in Ehlers-Danlos syndrome. Treatment by pars plana vitrectomy] Der Ophthalmologe : Z Dtsch Ophthalmol Ges. 1997;94(9):634–637. doi: 10.1007/s003470050173. [DOI] [PubMed] [Google Scholar]
- 10.Tabandeh H., Flaxel C., Sullivan P.M., Leaver P.K., Flynn H.W., Jr., Schiffman J. Scleral rupture during retinal detachment surgery: risk factors, management options, and outcomes. Ophthalmology. 2000;107(5):848–852. doi: 10.1016/s0161-6420(00)00033-6. [DOI] [PubMed] [Google Scholar]