Abstract
Purpose
to assess the resumption of physical activity after knee replacement.
Methods
retrospective study.
Results
118 patients were included in the final analysis. A resumption of >93% of the activities performed before surgery was observed. Logistic regression analysis did not show any significant associations between postoperatory activity and epidemiological and clinical variables except the function perceived by the patient.
Conclusions
the resumption of physical activity and sport is a paramount expectation for active patients. A clearer definition of physical activity and sports realistically achievable after a knee prosthesis is necessary but not yet fully available.
Keywords: Knee replacement, Arthroplasty, Return to sport, Physical activity, Health, Active lifestyle
1. Introduction
Gonarthrosis is a major cause of disability in adults. Pain-related physical deconditioning results in reduced fatigue resistance, aerobic capacity, muscle strength, and increased weight. An increased gonarthrosis prevalence has been recently predicted.1
There is a global concern about obesity and epidemic overweight, which are positively associated with sedentary lifestyles and negatively with regular physical activity. Patients with gonarthrosis do not perform the recommended levels of physical activity.2
Increased life expectancy and overweight/obesity percentage was associated with a high rate of prosthetic knee surgery. Successful surgical intervention, associated with pain relief and recovered joint function, in addition to wellbeing and cardiovascular risk reduction, has been achieved in several geographic settings.3 The long-term implant survival, the relative young age of the surgically treated patients, and the international recommendations on active lifestyles have raised the question on the potential resumption of a physical activity (i.e., type, frequency, and intensity). Concerns of the orthopedic surgeons are related to the increased wear of the components4,5 (function of the use and not of the time) joint instability, and periprosthetic fractures.
Usually the surgeon's advice to the patients is to resume a low-to-intermediate-impact physical activity,1 and to avoid high-impact sports, but these recommendations are mainly based on experts opinions from surveys, mainly focusing on prosthetic knee wear without an in-dept analysis on the adherence to international guidelines for health-enhancing physical activity and without considering enough the importance of a physically active lifestyle that improves mood, cardiovascular and metabolic condition, muscular strength, bone quality, balance and coordination of the patient.6,7
Since there are no precise guidelines about the topic,1 we strongly encourage the patients to resume a regular low-impact physical activity, allowing the return to intermediate-impact physical activity only to experienced practitioners, and discouraging high-impact physical activity.
The main aim of this study was to assess the resumption of physical activity in patients who underwent a knee arthroplasty, and to assay patient's compliance with surgeon's advice regarding the return to sport.
2. Materials and methods
A retrospective study was carried out on patients who underwent knee replacement between January 2014 and December 2017 in the Orthopedic Unit of the University of Sassari, Italy. Recruitment was consecutive.
Surgical interventions were performed by three senior surgeons, who performed total knee arthroplasty using a medial parapatellar retinacular approach. All patients followed a standardised rehabilitation protocol with early postoperatory mobilization and weight bearing as tolerated with crutches until wound healing (for a total duration of 2–4 weeks). Patient-, implant-, and surgery-related characteristics were collected through an ad hoc questionnaire, including implant survival, pre- and post-operative types of physical activity. Patients’ characteristics were the following: age, gender, height, weight, BMI, age of intervention, affected side, and comorbidities. Implant characteristics referred to the type of prosthesis were: unicompartmental (UKA) or total (TKA) knee prosthesis, posterior stabilized (PS), cruciate retaining (CR), and constrained non hinged (CNH) design. Types of physical activity and sports were categorized in three groups based on the level of impact on the knee joint according to Vail et al.8
The survey was conducted by telephone using a questionnaire developed by the authors. Questions were organized into three paragraphs: 1) patients’ characteristics and type of arthroplasty (age, height, weight, age of intervention, affected side, previous diseases or surgeries); 2) pre-operative physical activity (period of preoperative inactivity, type of activity, time between diagnosis and intervention); 3) postoperative physical activity (time to return to physical activities, type of activity, intensity and frequency compared to preoperative, reason for failure to resume the previous activity). Two years of inactivity before surgery was considered the threshold to classify a patient as active at the time of surgery, and to define physical activity after surgery as a resumption rather than a new beginning. The primary outcome was the resumption of physical activity after knee arthroplasty. The secondary outcomes were: 1) time after the surgery needed to resume physical activity; 2) relationship between resumption of activity after surgery and epidemiological and clinical variables.
2.1. Statistical analysis
An ad hoc electronic form was used to collect demographic, epidemiological, and clinical variables. Qualitative variables were described with absolute and relative (percentage) frequencies, whereas quantitative variables were summarized with means (standard deviations, SD) or medians (interquartile ranges, IQR) in case of parametric and non-parametric distribution, respectively. In-between group comparisons of quantitative variables were performed with the Student t-test and the Mann-Whitney for parametric and non-parametric variables, respectively. Logistic regression analyses were carried out to assess the relationship between post-operatory activity and epidemiological and clinical variables. The statistical software STATA version 15 (StatsCorp, TX) was used to perform all statistical computations.
3. Results
A total of 125 patients were recruited. However, 7 cases were excluded for the following reasons: death not related to the intervention (n = 1), patients not found or not available for the survey (n = 6). A total of 118 patients with 122 knee arthroplasties were included in the final analysis. The median (IQR) age was 73 (67–77) years, and females were more prevalent (71.3%) with a mean (SD) BMI of 29.1 (4.7) kg/m2; TKA PS was the most frequent type of implant (108, 88.5%), followed by TKA CNH (6, 4.9%), UKA (5, 4.1%), and TKA CR (3, 2.5%). More than 93% of the patients reported ≥1 regular physical activity or sport up to 2 years before surgery with a median (IQR) pre-operatory inactivity of 7 (5–12) months. Low-impact activities were the most frequently performed during the pre- (87.7%) and post-operatory (86.9%) period.
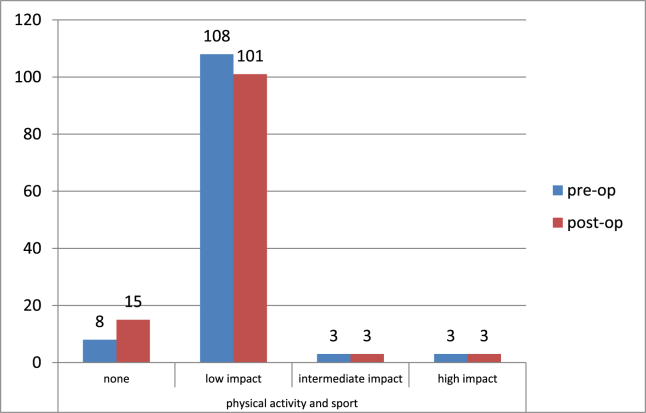
More than 87% of patients reported practicing physical activities or sport after surgery; a resumption of more than 93% of the activities performed before surgery was observed: 110 patients regularly performed a total of 123 physical-sports activities before surgery (with an average of 1.1 sports per active patient) and 103 patients (107 knee prosthesis) resumed 115 physical-sports activities after surgery (with an average of 1.1 activities per patient) (Graph 1, Table 1). Median (IQR) time to resumption of activity was of 4 (3–6) months. Patients reported a subjective function improved in 84 out of 122 prosthesis (68.9%), unchanged in 30/122 (24.6%) and worsened in 8/122 (6.6%).
Graph 1.
Number of patients who performed physical activity in the pre- and post-operative period divided by level of impact on the joint (none = no physical activity).
Table 1.
Physical activities pre- and post-surgery (*: resumption of physical activities).
| Activity | Pre-op | Post-op | % RPA * | RPA time (months) | Mean age (years) |
|---|---|---|---|---|---|
| Calisthenics | 2 | 2 | (100%) | 5,0 | 49 |
| Swimming | 7 | 4 | (57%) | 6,0 | 64 |
| Walking | 92 | 87 | (95%) | 3,9 | 73 |
| Stationary cycling | 0 | 1 | (>100%) | 2,0 | 63 |
| Water aerobics | 4 | 3 | (75%) | 4,3 | 70,5 |
| Cycling | 4 | 4 | (100%) | 4,3 | 75,5 |
| Bowls | 5 | 5 | (100%) | 3,8 | 73,8 |
| Tot. Low-Impact | 114 | 106 | (93%) | 4,8 | 72,1 |
| Free weight lifting | 1 | 1 | (100%) | 2,0 | 67 |
| Hunting | 3 | 3 | (100%) | 7,0 | 71,6 |
| Hiking | 2 | 2 | (100%) | 3,0 | 70,5 |
| Tot. Intermediate-Impact | 6 | 6 | (100%) | 4 | 70,5 |
| Motocross | 1 | 1 | (100%) | 2,0 | 70 |
| Running | 1 | 1 | (100%) | 5,0 | 74 |
| Soccer | 1 | 1 | (100%) | 5,0 | 74 |
| Tot. High-Impact | 3 | 3 | (100%) | 4 | 72,6 |
| Tot. | 123 | 115 | (93%) | 4 | 71,3 |
Eight patients did not perform any physical activities before surgery: 4 of them started a regular physical practice after surgery despite major comorbidities (2 rheumatoid arthritis, 1 fibromyalgia, 1 bilateral prosthesis); among the 4 who maintained an inactive lifestyle, 2 patients had a painful prosthesis (a75 years old woman with history of revision for tubercular gonilitis, and a 69 years old woman with a prosthetic failure awaiting revision, opposite knee and hip prosthesis and obesity) and 2 had sedentary habits without any limiting conditions.
Eleven patients, active before surgery, did not restarted a regular physical activity (all implanted with a TKA with a PS design: 5 complained of a painful knee prosthesis, whereas the other 6 showed chronic comorbidities) (Table 2).
Table 2.
Comorbidities, complications, and subjective function perceived by patients who failed to resume pre-operatory activity.
| Type of prosthesis | Pre-op activity | Post-op activity | Comorbidities and complications | Pts subjective function |
|---|---|---|---|---|
| TKA PS | Walking | NO | breast cancer, deep vein thrombosis, pulmonary embolism | improved |
| TKA PS | Walking | NO | chronic cardiorespiratory disease | unchanged/not known |
| TKA PS | Walking | NO | deep vein thrombosis, pulmonary embolism | unchanged/not known |
| TKA PS | Walking | NO | painful knee prosthesis | unchanged/not known |
| TKA PS | Walking | NO | painful knee prosthesis | unchanged/not known |
| TKA PS | Walking | NO | painful knee prosthesis | unchanged/not known |
| TKA PS | Walking | NO | opposite knee and hip arthrosis | worsened |
| TKA PS | Walking | NO | opposite knee arthrosis | worsened |
| TKA PS | Swimming | NO | painful knee prosthesis | worsened |
| TKA PS | Walking | NO | painful knee prosthesis | worsened |
| TKA PS | Walking | NO | prosthetic failure, diabete mellitus, polyneuropathy | worsened |
More than 50% of patients (62/118) reported no significant comorbidities, the remaining patients complained of ≥1 comorbidities or complications. Twenty-three patients had ≥1 joints requiring another prosthesis (including 3 patients with rheumatoid arthritis), 12 patients had ≥1 joints successfully treated with an arthroplasty, 6 complained about chronic painful knee prosthesis, 7 reported a chronic cardiorespiratory disease, 8 diabetes mellitus (1 of which complicated by polyneuropathy); other less frequently reported conditions were deep venous thrombosis complicated by pulmonary embolism (2 cases), early aseptic loosening of the tibial components that required a revision surgery (2 cases), severe low back pain (2 cases), knee joint tuberculosis (1 case), depression (1), fibromyalgia (1), severe osteoporosis (1 case).
Logistic regression analysis aimed to assess the relationship between postoperatory activity and epidemiological and clinical variables (age, sex, BMI, type of prosthesis, comorbidities, pre-operatory type of activity, duration of pre-operatory inactivity within the two year threshold, patients subjective function) did not show any statistically significant associations with the only exception of subjective function perceived by the patient (Table 3).
Table 3.
Relationship between post-operatory activity and epidemiological and clinical variables.
| Variables | OR (95% CI) | p-value |
|---|---|---|
| Age, years | 0.9 (0.9–1.0) | 0.11 |
| Males | 2.9 (0.6–13.6) | 0.18 |
| BMI, kg/cm2 | 1.0 (0.9–1.1) | 0.99 |
| Comorbidities | 4.8 (1.0–23.6) | 0.06 |
| Pre-operatory level of impact | 1.0 (0.2–3.9) | 0.95 |
| Pre-operatory inactivity, months | 1.0 (0.9–1.0) | 0.24 |
| Patients subjective function improvement | 48.4 (6.1–387.2) | <0.0001 |
4. Discussion
A regular physical activity after a knee replacement requires the motivation to be active, as well as being active before surgery. Huch et al.9 found that 94% of the patients were active during their lifetime, but only 36% were active immediately before surgery; then, the rate of resumption depended on pre-operative activity percentage considered (36 and respectively 81%). We considered active only those who performed regular physical activity up to at least two years before the intervention (realistic time between the occurrence of limiting symptoms and surgical intervention). One patient was considered pre-operatively inactive because he reported an inactivity period >2 years (36 months); in this case, the post-intervention activity was not considered a resumption.
WHO defines physical activity as “any bodily movement produced by skeletal muscles that requires energy expenditure - including activities undertaken while working, playing, carrying out household chores, travelling, and engaging in recreational pursuits”.2 We refer to physical activity including sport (a subcategory, inter alia, characterized by the goal of achieving results in competitions at all levels10) because significant health-related benefits are found in both activities and because in the scientific literature sport activities do not always show competitive features (e.g., walking, tai chi, hiking).
The type of activity could influence bearing surface wear, risk of aseptic loosening, and even more catastrophic events, such as periprosthetic fractures.1,8 In accordance with Vail et al., physical activities were assessed in relation with the potential impact on knee joint considering repetitiveness and magnitude of the stresses and risk of violent trauma. A systematic review and meta-analysis1 showed that resumption of physical activity is more likely for lower impact activities: 93–94%, 64–100%, 35–43% returning to low, intermediate, and high impact sports, respectively after TKA and UKA. Conversely to the conclusions emerged from Witjes's meta-analysis we did not observe significant differences in the resumption of physical and sports activity with reference to the level of impact and the type of prosthesis, but this result could be due to the sample size, and more in detail to the small number of participants in non-low impact activities and with non-TKA PS implants. In our series more than 87% of patients reported practicing physical activities or sport after surgery. This value corresponds to a resumption of physical activity in over 93% of patients, considering that only 110 patients (four of which with bilateral knee prosthesis) were engaged in ≥1 regular physical activity before surgery. A resumption of more than 93% of the activities performed before surgery was also observed.
A previous study found that the mean number of sports per patient decreased from 1.8 to 1.4 after TKA,11 in our series we did not observe such a reduction in mean number of sport activities per patients: 110 patients regularly performed a total of 123 physical-sports activities before surgery (with an average of 1.1 sports per active patient) and 103 patients (107 knee prosthesis) resumed 115 physical-sports activities after surgery (with an average of 1.1 activities per patient) but we cannot deduce if there has been a reduction in the intensity and frequency of the practice since this was not one of the assessed outcomes. Angerson et al.12 reported gender, age and BMI as possible confounding factors in return to sport after TKA. Chatterji et al.11 observed that men were significantly more sport oriented than women both pre and postoperative; Wylde et al.13 Huch 9and Keeney14 reported a more frequent resumption of sport activity for men than for women; in agreement with Naal et al.15 we did not find any significant influence of sex in resumption of sport activities.
Huch reported a negative influence of age in a large selected population under the age of 76 years, in our population, median age was 73 (IQR 67–77; range 26–89) years, and in agreement with Wylde et al. age did not show any significant influence in resumption of activity. Naal and Keeney reported a negative influence of BMI and resumption of activity after UKA and TKA respectively; in our series more than 70% of the patients were either overweight or obese but logistic regression analysis did not show any statistically significant associations between resumption of postoperatory activity and BMI. Angerson et al. and Huch et al. mentioned complication and co-morbidities as possible confounders, Bradbury et al.16 showed a negative influence of comorbidities on the return to sport after TKA, our data analysis showed no significant correlation between comorbidities and resumption of sport after surgery despite almost half (47%) of the patients complained of ≥1 comorbidities or complications. A clear definition of the time of assessment of the preoperative sport has a significant effect on RPA percentage as shown by Huch, instead the duration of inactivity within two years of the intervention did not significantly affect the resumption of sporting activity in our series. In this study the subjective function perceived by the patient and the resumption of physical activities were statistically strongly associated.
5. Conclusions
The characteristics of the population and of the prosthesis, thanks to medical progress and constant development of new models and biomaterials, are changing. Even if the majority of patients who undergo a knee arthroplasty is old and resumes a low-impact physical activity, we have to consider that life expectancy has increased, and there are more and more elderly active patients with greater functional needs, as well as young patients who want to resume intermediate and high-impact activities. Nowadays the average opinion for most surgeons is that activities involving frequent jumping and landing and high impact as well as twisting movements have to be strongly discouraged, while a return to a low-impact sport activity is allowed, but the attention tends to be confined to the mechanical functioning of the prosthesis to avoid its mechanical failure without globally considering the patient's health and expectations. It is clear that for those who were active before surgery, the return to physical activity and sport is an important expectation, a need, especially in young and active patients, who tend to be much more exigent.
The need for prosthetic revision, with all the risks associated with the procedure, must be reduced, but the benefits of physical activity, when appropriately and mindfully practiced, have a broad effect on health condition, improving cardiovascular and metabolic condition, bone quality, muscular strength, balance and coordination, hence helping the patient to decrease the risk of falling and periprosthetic fractures, to slow down the bone density reduction, and to better face a possible revision surgery.
The aim of the studies upon patients who resume physical activity after UKA and TKA should be to clearly define the real level of physical activity achievable after the arthroplasty, what are the patient characteristics influencing the resumption of physical activity, the physical activities associated factors for short-term implant failure (in order to set guidelines to avoid it), and to understand what is the type, intensity and frequency of physical activity that provides the maximum health benefit without reducing the longevity of the different types of prosthesis. In order to give the patients truthful and precise answers about the type and amount of sports activities they can resume, further studies are needed. Continuous follow-up studies upon physical activity and sport is essential, and studying patients involved in high-impact activities is a powerful tool to set new recommendations.
Author contributions
Francesco Pisanu: Conceptualization, Methodology, Writing - Original Draft , Review & Editing.
Matteo Andreozzi: Investigation.
Federico Costagli: Investigation, Data Curation.
Laura Saderi: Formal analysis.
Giovanni Sotgiu: Formal analysis.
Andrea Fabio Manunta: Supervision.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Contributor Information
Francesco Pisanu, Email: pisanuf@gmail.com, francesco.pisanu@aousassari.it.
Matteo Andreozzi, Email: matteo.andreozziscience@gmail.com.
Federico Costagli, Email: federico.costagli@h-ju.ch.
Gianfilipo Caggiari, Email: gianfilippocaggiari@gmail.com.
Laura Saderi, Email: lsaderi@uniss.it.
Giovanni Sotgiu, Email: giovanni.sotgiu@aousassari.it, gsotgiu@uniss.it.
Andrea Fabio Manunta, Email: andreafabio.manunta@aousassari.it.
References
- 1.Witjes S., Gouttebarge V., Kuijer P.P., van Geenen R.C., Poolman R.W., Kerkhoffs G.M. Return to sports and physical activity after total and unicondylar knee arthroplasty: a systematic review and meta-analysis. Sports Med. 2016;46(2):269–292. doi: 10.1007/s40279-015-0421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Global Recommendations on Physical Activity for Health. World Health Organization; 2010. [PubMed] [Google Scholar]
- 3.Ethgen O., Bruyère O., Richy F., Dardennes C., Reginster J.Y. Health-related quality of life in total hip and total knee arthroplasty. J Bone Joint Surg Am. 2004;86(5):963–974. doi: 10.2106/00004623-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Manunta A.F., Zedde P., Pisanu F., Marras F. Sports-related changes of the synovial membrane. Joints. 2015;13(2):181–187. 4. [PMC free article] [PubMed] [Google Scholar]
- 5.Pisanu F., Doria C., Andreozzi M. Pleomorphic clinical spectrum of metallosis in total hip arthroplasty. Int Orthop. 2019;43(1):85–96. doi: 10.1007/s00264-018-4176-4. [DOI] [PubMed] [Google Scholar]
- 6.Warburton D.E., Gledhill N., Quinney A. Musculoskeletal fitness and health. Can J Appl Physiol. 2001;26(2):217–237. doi: 10.1139/h01-013. [DOI] [PubMed] [Google Scholar]
- 7.Warbuton D.E., Gledhill N., Quinney A. The effects of changes in musculoskeletal fitness and health. Can J Appl Physiol. 2001;26(2):161–216. doi: 10.1139/h01-012. [DOI] [PubMed] [Google Scholar]
- 8.Vail T.P., Mallon W.J. Athletic activities after joint arthroplasty. Sports Med Arthrosc Rev. 1996;4:298–305. [Google Scholar]
- 9.Huch K., Müller K.A., Stürmer T., Brenner H., Puhl W., Günther K.P. Sports activities 5 years after total knee or hip arthroplasty: the Ulm Osteoarthritis Study. Ann Rheum Dis. 2005;64:1715–1720. doi: 10.1136/ard.2004.033266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Council of Europe Committee of Ministers European Sports Charter, article 2.
- 11.Chatterji U., Ashworth M.J., Lewis P.L., Dobson P.J. Effect of total knee arthroplasty on recreational and sporting activity. ANZ J Surg. 2005;75(6):405–408. doi: 10.1111/j.1445-2197.2005.03400.x. [DOI] [PubMed] [Google Scholar]
- 12.Argenson J.N., Parratte S., Ashour A., Komistek R.D., Scuderi G.R. Patient-reported outcome correlates with knee function after a single-design mobile bearing TKA. Clin Orthop Relat Res. 2008;466(11):2669–2676. doi: 10.1007/s11999-008-0418-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wylde V., Blom A., Dieppe P., Hewlett S., Learmonth I. Return to sport after joint replacement. J Bone Joint Surg Br. 2008;90(7):920–923. doi: 10.1302/0301-620X.90B7.20614. [DOI] [PubMed] [Google Scholar]
- 14.Keeney J.A.1, Nunley R.M., Wright R.W., Barrack R.L., Clohisy J.C. Are younger patients undergoing TKAs appropriately characterized as active? Clin Orthop Relat Res. 2014;472(4):1210–1216. doi: 10.1007/s11999-013-3376-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naal F.D.1, Fischer M., Preuss A. Return to sports and recreational activity after unicompartmental knee arthroplasty. Am J Sports Med. 2007;35(10):1688–1695. doi: 10.1177/0363546507303562. [DOI] [PubMed] [Google Scholar]
- 16.Bradbury N., Borton D., Spoo G., Cross M.J. Participation in sports after total knee replacement. Am J Sports Med. 1998;26(4):530–535. doi: 10.1177/03635465980260041001. [DOI] [PubMed] [Google Scholar]