Abstract
A majority of emerging infectious diseases are of zoonotic origin. Metagenomic Next-Generation Sequencing (mNGS) has been employed to identify uncommon and novel infectious etiologies and characterize virus diversity in human, animal, and environmental samples. Here, we systematically reviewed studies that performed viral mNGS in common livestock (cattle, small ruminants, poultry, and pigs). We identified 2481 records and 120 records were ultimately included after a first and second screening. Pigs were the most frequently studied livestock and the virus diversity found in samples from poultry was the highest. Known animal viruses, zoonotic viruses, and novel viruses were reported in available literature, demonstrating the capacity of mNGS to identify both known and novel viruses. However, the coverage of metagenomic studies was patchy, with few data on the virome of small ruminants and respiratory virome of studied livestock. Essential metadata such as age of livestock and farm types were rarely mentioned in available literature, and only 10.8% of the datasets were publicly available. Developing a deeper understanding of livestock virome is crucial for detection of potential zoonotic and animal pathogens and One Health preparedness. Metagenomic studies can provide this background but only when combined with essential metadata and following the “FAIR” (Findable, Accessible, Interoperable, and Reusable) data principles.
Keywords: virome, livestock, deep sequencing, animal reservoir, zoonosis, one health, viral metagenomics, NGS, emerging infectious diseases, high-throughput sequencing
1. Introduction
Emerging infectious diseases (EIDs) are responsible for a substantial burden of mortality and morbidity globally, and a majority of EIDs (60.3%) are caused by zoonotic pathogens [1,2,3]. In the past decades, high impact outbreaks have occurred with introductions from wildlife and livestock reservoirs, respectively, exemplified by the wildlife-borne outbreaks of Severe Acute Respiratory Syndrome (SARS) [4], Nipah disease [5,6], and Lassa fever [7], and outbreaks resulting from contact with livestock animals, such as Middle East Respiratory Syndrome [MERS] [8], avian influenza [9], Rift Valley fever [10], and swine influenza [11,12]. Livestock animals that live in close proximity to humans can facilitate transmission of infectious diseases through the wildlife-livestock-human interface [3].
Intensification of livestock farming is widely practiced in support of increasing food demand due to human population growth. This, in turn, facilitates disease transmissions within herds and between livestock and humans by increasing livestock population and density [3]. Therefore, the potential emergence of zoonoses from livestock population should not be underestimated [13,14]. In 2003, there was an outbreak of a highly pathogenic avian influenza A subtype H7N7 in humans linked to multiple commercial poultry farms in the Netherlands [15]. Two years later, another highly pathogenic avian influenza A H5N1 virus emerged in Asia in 2005, probably as a result of frequent mixing between flocks and wild birds, suggesting that pre-existing biosecurity measurements could not keep up with the rate of livestock intensification [16]. In 2007–2010, a large-scale Q fever outbreak was reported in the Netherlands, affecting more than 3500 human cases and resulting in a huge economic loss [17,18]. A steep increase in the number of goat farms most likely was the driver for the increased prevalence of Coxiella burnetii infections, with animal abortion waves that had gone unnoticed. The policy of voluntary reporting abortion outbreaks to the Animal Health Service hindered the timely detection of the circulation of Q fever, and therefore early interventions. These examples indicate that zoonotic risks in the livestock industry should be carefully managed and adapted to livestock intensification. The One Health approach has been coined for advocating collaboration between multiple stakeholders including veterinarians, clinicians, epidemiologists, virologists, microbiologists, ecologists, and policy makers to prevent and control EIDs through the human-animal-environment interface [19]. Surveillance of livestock and the surrounding environment is a hallmark of early detection but is currently targeted to known risks.
Advances in Next-Generation Sequencing (NGS) technologies and rapid development of bioinformatics and computational tools offer new opportunities for EID surveillance in quality and in scale. Particularly, metagenomic NGS (mNGS) allows unbiased detection of all microbes and viruses in a sample, showing potential for timely detection of rare or novel infectious etiologies, as well as for surveillance of foodborne and waterborne viruses [20,21,22,23,24,25,26]. However, the use of mNGS as a potential surveillance tool requires a deeper understanding of what is “normal” diversity in humans [27], as well as wildlife [28,29] and farm animals [30]. Characterizing species-specific metagenomes could potentially be used to provide a surveillance baseline for early detection and for tracking of movements of pathogens across different hosts, and has been promoted by projects like the global virome project [31]. However, for such applications, detailed background is needed regarding coverage, representativeness, and biases in the study designs. Here, we conduct a systematic review to identify available literature that performed viral mNGS in common farm animals including cattle, small ruminants (goats and sheep), poultry, and pigs. We reviewed the data and metadata availability and quality of these studies. We further summarized reported viromes of common farm animals in order to translate these efforts as background virus diversity profiles of common farm animals to guide preparedness of diseases at the livestock-human interface.
2. Materials and Methods
2.1. Search Strategy and Selection Criteria
To provide an overview of studies that performed viral mNGS in common livestock including cattle, small ruminants (goats and sheep), poultry, and pigs, we performed a systematic review in five electronic databases (Embase, Medline, Cochrane Central, Web of Science, and Google Scholar) on 21 February 2019 using search terms such as “metagenomic,” “farm animals,” “livestock,” “virome,” and “high-throughput sequencing.” The detailed search strategy is described in the Supplementary Materials. All identified references were imported to Mendeley (available at https://www.mendeley.com/). Duplicated references were removed.
Titles and abstracts of all unique references were screened by two independent reviewers (K.T.T.K. and D.F.N.). After first screening, full texts of remaining articles were assessed for eligibility. Articles that were not written in English were excluded. We also excluded conference abstracts and articles that did not report any original data (i.e., review papers, editorial, and commentaries). Only studies that performed viral metagenomic sequencing in specimens from farm animals were included. We included studies that focused on cattle, small ruminants (goats and sheep), poultry, and pigs. The flow of the systematic review was adapted from the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [32].
2.2. Data Extraction and Analysis
We extracted the following information from each included study: first author, journal name, year of publication, type of farm animals, breed type, health condition of the animals, age of the animals, sampling date, sample size, specimen type, farm type, location of the farm, geographical reference of the farm, virus detected, virus family detected, nucleic acid extraction method, sequencing platform, Sequence Read Archive (SRA)/European Nucleotide Archive (ENA)/GenBank record (if any), and rationale of the study.
Data cleaning, stratification, analysis, and visualization was performed using R packages [33] (dplyr [34], ggplot2 [35], reshape2 [36], and stringr [37]). Information on host range and taxonomy of different virus families was adapted from ViralZone [38] and International Committee Taxonomy of Viruses [39]. The host range of different virus families were stratified into seven groups: vertebrate virus, invertebrate virus, bacteriophage, plant virus, other virus not classified into the first four categories (e.g., mycovirus and archaeal virus etc.), virus with multiple hosts, and unclassified virus/virus with unknown host(s). Geographical origins of included studies were stratified according to World Health Organization (WHO) regions: Africa region, the Americas, Eastern Mediterranean region, European region, South-East Asia region, and the Western Pacific region. Health conditions of farm animals were stratified into four major groups: healthy, gastrointestinal signs, respiratory signs, and other clinical signs. The category “other clinical signs” refers to any clinical signs that could not be classified into the first three categories and unspecified health conditions. Studies were stratified into seven arbitrary types based on their primary findings: virome study (i.e., papers that focused on studying the virus diversity of the animals), genetic characterization, mNGS as a diagnostic tool, mNGS as a diagnostic tool and virome study, virus discovery (i.e., papers that primarily focused on discovery of novel viruses), methodology papers, and others. Sequencing platforms were stratified into four main sequencing platforms: 454 pyrosequencing (Roche), Illumina, Ion Torrent (Thermo Fisher), and Oxford Nanopore Technologies. Sample sizes were stratified into six arbitrary groups: less than 10, 11–50, 51–100, 101–500, 501–1500, and unspecified sample size. Nucleic acid extraction strategies were stratified into four groups: column-based, solvent-based (e.g., chloroform and TRIzol [Thermo Fisher]), magnetic bead-based, and other/multiple types of extraction methods.
3. Results
3.1. Overall Descriptions of All Studies
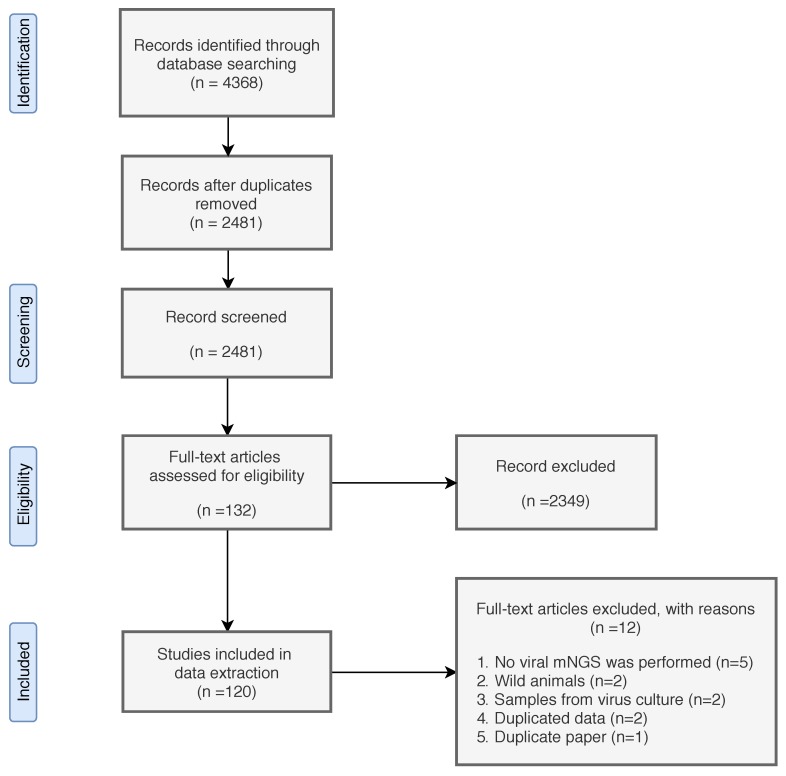
A total of 4368 records were identified (Figure 1). After record deduplication, we performed the first screening with 2481 included records. After first screening, 2349 records were excluded for the following reasons: no mNGS was performed, studied animals were wild animals or were not cattle, small ruminants (goat and sheep), poultry, and/or pigs, records were not written in English, records did not contain original findings, or records were conference abstracts. Full text of 132 remaining records were assessed for eligibility, and 120 records were included for data extraction (Supplementary Materials).
Figure 1.
Flow chart of systematic review. The procedures were adapted from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
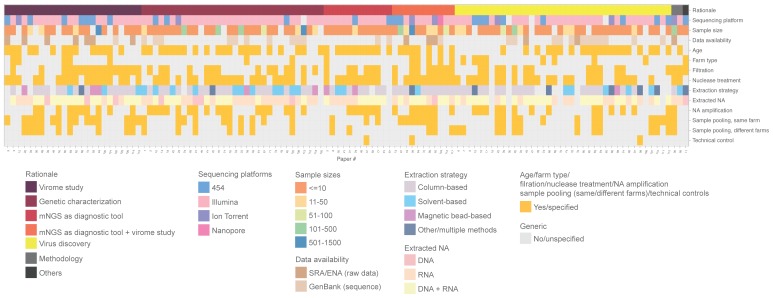
In terms of metadata availability, only one-fifth of the included studies specified farm types and nearly 40% of the studies did not mention the age of the farm animals (Figure 2). Twenty-eight percent and 40% of studies pooled specimens between farms and within farms together for sequencing, respectively. More than 95% of the studies did not specify whether there were technical controls for validating the sequencing results. For data availability, only 10.8% (N = 13) provided raw sequencing data in the public repository, either the SRA or ENA. There is no distinct pattern when comparing metadata and data availability in studies with different study rationales.
Figure 2.
An overview of study design and data (and metadata) availability of 120 included publications. Each column represents one paper, and numbers refer to the list of references (Supplementary Materials). Rows describe data fields extracted from the papers as follows (from top to bottom): study rationale, sequencing platforms, sample sizes, availability of sequencing data in public repository, availability of animal age description, availability of farm type description, indication of whether filtration was performed, indication of whether nuclease treatment was performed during sample preparation, nucleic acid extraction strategy, type of nucleic acid extracted, indication of whether nucleic acid amplification was performed, indication of whether sample pooling was performed in same/different farms, and mention of technical controls for validating sequencing results. Categories and color codes for each data field are indicated in the figure legend. Gray boxes indicate that the technique was not performed, or the information was not specified. mNGS = metagenomic Next-Generation Sequencing. SRA = Sequence Read Archive. ENA = European Nucleotide Archive. NA = nucleic acid.
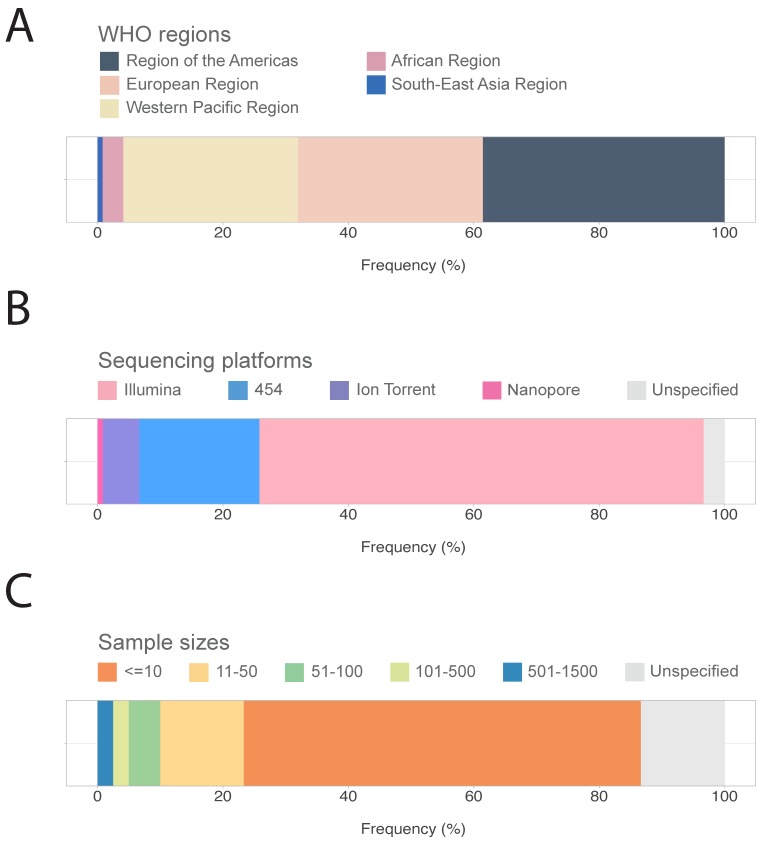
Geographically, most studies were carried out in three out of six WHO regions: the Americas (38.3%, N = 46), followed by European region (29.2%, N = 35), and the Western Pacific region (28.3%, N = 34) (Figure 3A). There were four studies in the African region (3.3%) and one study in the South-East Asia region (0.8%), and we did not identify publications from the Eastern Mediterranean region.
Figure 3.
(A) Geographical origin of included studies stratified by World Health Organization (WHO) regions. (B) An overview of sequencing platforms. (C) An overview of sample sizes.
For sequencing platform, the majority of the studies (70.9%, N = 85) performed NGS with Illumina sequencing platform, followed by 454 pyrosequencing (19.2%, N = 23), and Ion Torrent sequencing (5.8%, N = 7). (Figure 2 and Figure 3B). Only one study sequenced with the Nanopore platform (0.8%). Four studies (3.3%) did not specify which sequencing platforms were used [40,41,42,43]. The earliest included study was published in 2009. 454 pyrosequencing was the most popular platform during 2009–2013, gradually replaced by Illumina starting from 2014 (Supplementary Materials Figure S1).
In terms of viral enrichment strategies, we found that half of the included studies performed filtration steps, majority (68.3%, N = 82) performed nuclease treatment, and 45.8% (N = 55) studies performed DNA/RNA amplification steps (Figure 2). Almost half of the studies (N = 58) extracted both DNA and RNA and around one-third of the studies extracted RNA only (N = 44). For extraction strategies, majority used the column-based method (N = 62), followed by the solvent-based method (19.2%, N = 23), and the magnetic bead-based method (6.7%, N = 8).
Over 75% of studies had a sample size of less than a 100 (Figure 2 and Figure 3C). Six studies (5%) and three studies (2.5%) had a sample size of 101–500 and 501–1500, respectively. Of note, the majority of the studies (63.3%, N = 76) had a sample size range <= 10. Sixteen studies (13.3%) did not report sample size.
3.2. Farm Animals, Health Conditions, and Specimen Types
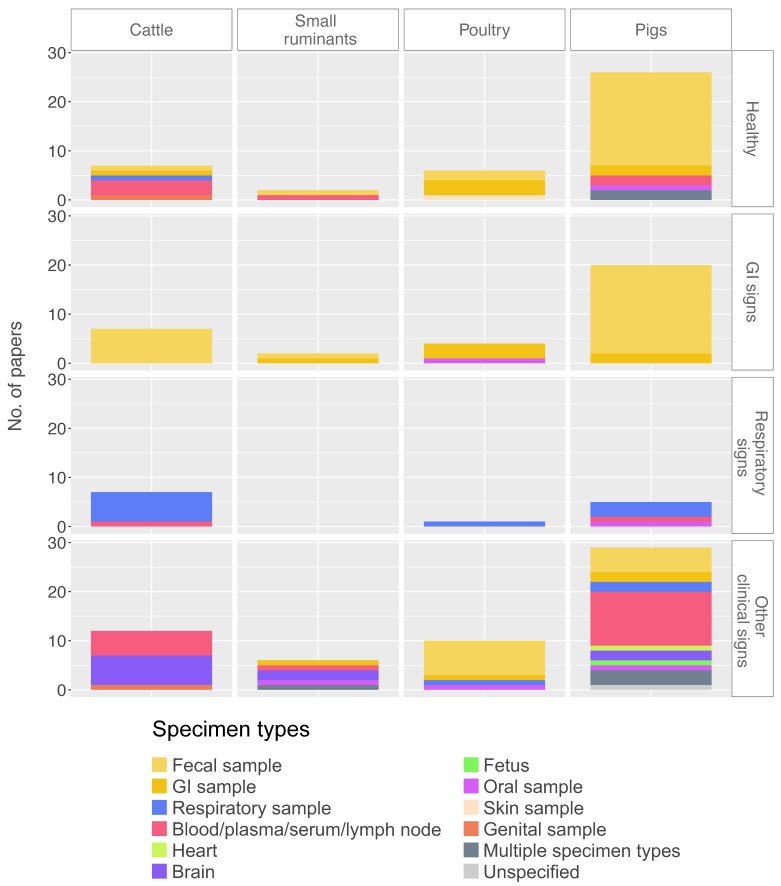
Pigs were the most frequently studied animals (N = 64) among all four types of farm animals in the available literature, followed by cattle (N = 29), poultry (N = 19), and small ruminants (goats and sheep) (N = 9). Only one study provided data on more than one type of farm animals.
Most studies involving pigs and poultry included healthy animals (N = 26 for pigs and N = 6 for poultry). For cattle, there were seven studies each for healthy animals, animals with respiratory signs, and animals with gastrointestinal signs. For small ruminants, there were two studies each for healthy animals and animals with gastrointestinal signs; there was no mNGS study available for small ruminants that had respiratory signs.
Furthermore, we looked into specimens collected for the four major health conditions. For healthy farm animals, specimen types were slightly skewed towards gastrointestinal samples, particularly in pigs (81%) and poultry (83%) (Figure 4). Specimen type diversity was highest in both cattle and pigs (N = 5), followed by poultry (N = 3), and small ruminants (N = 2). For respiratory samples, there was only one study with healthy cattle [44], whereas no studies in healthy pigs, poultry, and small ruminants were identified (Figure 4). For symptomatic animals, the sampling strategy reflected the clinical signs (i.e., gastrointestinal sample for gastrointestinal signs, respiratory samples for respiratory signs) (Figure 4).
Figure 4.
Types of specimens tested in different farm animals by number of papers, stratified by reported health conditions. Categories per variable are color-coded as shown in the legend. GI = gastrointestinal. A version of Y-axis as frequency (%) can be found in Supplementary Materials Figure S2.
3.3. Virus Diversity in Different Farm Animals
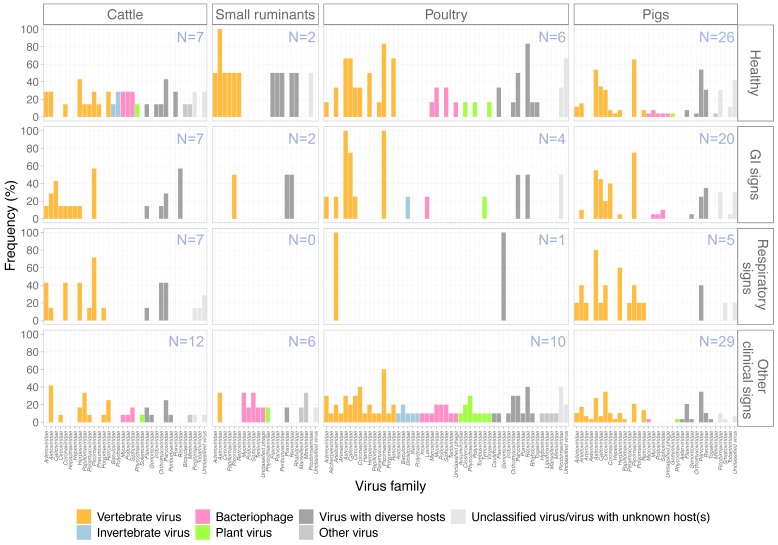
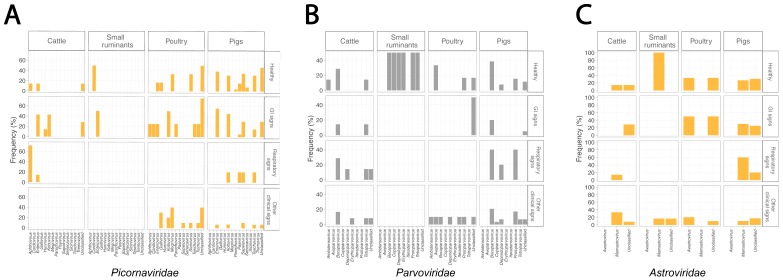
The greatest diversity of viruses was observed in samples from poultry, with 49 virus families reported in the available literature, followed by cattle with viruses found from 33 families and pigs with 32 families (Figure 5). In comparison, only 20 virus families were reported in studies involving small ruminants. Fifteen vertebrate virus families were reported in both pigs and poultry, followed by cattle (N = 14) and small ruminants (N = 6). Apart from vertebrate viruses, bacteriophages and plant viruses were found in all four types of livestock while invertebrate viruses were only detected in cattle and poultry. Bacteriophage belonging to families Myoviridae, Podoviridae, and Siphoviridae were detected in all four livestock types. Interestingly, the diversity of plant viruses was identified highest in poultry with seven plant virus families detected (compared to two each for pigs and cattle, and one for small ruminants). Overall, Picornaviridae, Parvoviridae, and Astroviridae were among the three most frequently found virus families identified. There was no distinguishable pattern when comparing genera of the above-listed three most abundantly found virus families in the four major health conditions (Figure 6). Enterovirus, bocaparvovirus, and dependoparvovirus were reported in all four livestock types (Figure 6). Viruses within the Astroviridae family were host species-specific as avastrovirus and mamastrovirus were only found in poultry and mammals, respectively (Figure 6C).
Figure 5.
An overview of virus families found in different farm animals in included studies, stratified by reported health conditions. The bars are color-coded by host range of the viruses as shown in the figure legend. GI = gastrointestinal. Y axis shows proportion of studies that found the viruses specified.
Figure 6.
Frequencies of virus genera of top three most abundant virus families stratified by health conditions. (A) Picornaviridae. (B) Parvoviridae. (C) Astroviridae. Color code is based on host range and adapted from Figure 5.
Reoviridae and Caliciviridae were frequently reported in studies of healthy poultry (83% and 66%, respectively) and poultry with gastrointestinal (GI) signs (50% and 75%, respectively). Herpesviridae were reported in 60% of studies of pigs with respiratory signs. In general, the reported virome of healthy farm animals and farm animals with clinical signs were somewhat similar. A diverse range of known animal viruses (listed in Table 1) and newly recognized viruses (listed in Table 2) were reported in mNGS studies. Notably, some viruses that are known to have zoonotic potential were reported in available mNGS studies including hepatitis E viruses in gastrointestinal samples of pigs [45,46] and cattle [47] and Influenza A viruses in respiratory samples of poultry [25] and pigs [46].
Table 1.
Examples of known animal viruses reported in available metagenomic Next-Generation (mNGS) studies.
| Farm Animal Type | Known Animal Viruses Found by mNGS Studies | References |
|---|---|---|
| Cattle | Bovine adenovirus | [44,48,49,50] |
| Bovine coronavirus | [44,50,51,52] | |
| Bovine papillomavirus | [53,54] | |
| Bovine parvovirus | [44,48,50,52,53,54,55,56] | |
| Bovine respiratory syncytial virus | [44] | |
| Bovine rhinitis A virus | [44,48,49] | |
| Bovine rhinitis B virus | [44,48,49,52,57] | |
| Bovine viral diarrhoea virus | [44,47] | |
| Enterovirus | [44,47,50,58] | |
| Hepatitis E virus | [47] | |
| Herpesvirus | [44,48,50,52,54,58] | |
| Influenza D virus | [48,59] | |
| Kobuvirus | [47] | |
| Norovirus | [58,60] | |
| Rotavirus | [47,58,61] | |
| Small ruminants | Enterovirus | [62] |
| Orf virus | [63,64] | |
| Rotavirus | [64,65] | |
| Poultry | Avastrovirus | [66,67,68,69,70] |
| Aveparvovirus | [69] | |
| Chicken anaemia virus | [68] | |
| Gallivirus | [70,71] | |
| Gammacoronavirus | [69,70] | |
| Influenza A virus | [25] | |
| Megrivirus | [69,70,71,72,73] | |
| Rotavirus | [67,70,72,74] | |
| Sicinivirus | [71,72] | |
| Tremovirus | [68,70] | |
| Pigs | African swine fever virus | [75] |
| Bocaparvovirus | [24,51,76,77,78,79,80,81] | |
| Enterovirus | [46,76,77,78,82,83,84,85,86,87,88,89,90,91,92,93] | |
| Hepatitis E virus | [45,46] | |
| Influenza A virus | [46] | |
| Kobuvirus | [46,76,77,78,79,80,84,87,88,91,92,94,95] | |
| Porcine adenovirus | [46,94] | |
| Porcine circovirus | [24,30,46,79,94,95,96,97,98] | |
| Porcine cytomegalovirus | [94,95,99] | |
| Porcine epidemic diarrhea virus | [46,79,84,88,92,100] | |
| Porcine reproductive and respiratory syndrome virus | [95,101,102] | |
| Porcine respiratory coronavirus | [46] | |
| Rotavirus | [24,80,82,83,84,87,90,92,100,103,104,105,106] | |
| Sapelovirus | [30,76,77,78,79,80,82,84,87,88,90,92,93,94] | |
| Sapovirus | [30,76,77,78,84,87,88,90,92,93,107] | |
| Torque teno virus | [24,30,46,79,94,95,108] |
Table 2.
Examples of novel viruses found in farm animals by available mNGS studies.
| Farm Animal Type | Novel Viruses Found by mNGS Studies | References |
|---|---|---|
| Cattle | Astrovirus | [109] |
| CRESS-DNA virus | [50] | |
| Hepacivirus | [110] | |
| Nidovirus | [52] | |
| Papillomavirus | [111] | |
| Parvovirus | [112] | |
| Picornavirus | [113] | |
| Orthobunyavirus | [114] | |
| Rotavirus | [115] | |
| Small ruminants | Astrovirus | [116,117] |
| Poultry | Coronavirus | [118] |
| Picobirnavirus | [42,119] | |
| Picornavirus | [120,121] | |
| Pigs | Astrovirus | [122,123] |
| Bocavirus/Bocavirus-like | [98,122,124] | |
| Bufavirus | [125] | |
| Circovirus/Circovirus-like | [40,104,126] | |
| Enterovirus/Enterovirus-like | [85,89,92,93] | |
| Immunodeficiency-associated stool virus | [127] | |
| Ljungan-like viruses | [122] | |
| Parvovirus | [128,129] | |
| Porcine stool-associated circular virus | [82] | |
| Posavirus | [100] | |
| Pestivirus | [41,130] | |
| Picornavirus | [131] | |
| Picornavirales | [132] | |
| Teschovirus/Teschovirus-like | [90] |
4. Discussion
The rapid and extensive development of NGS has opened up more opportunities to advance understanding in infectious disease diagnostics, surveillance, and transmission [133]. One of the key NGS applications is the primer-independent, agnostic (i.e., without prior knowledge) viral metagenomics to characterize all viruses present in the samples, and also allow the discovery of novel or uncommon infectious etiologies [134,135]. In this review, we summarize previous studies that performed viral mNGS in common farm animals including cattle, small ruminants, poultry, and pigs in an effort to provide background virus diversity profiles of these farm animals. Information systematically summarized from this review will help to guide the design of future studies employing mNGS for surveillance as well as preparedness for detection of diseases at the livestock-human interface.
The majority of available farm animal viral mNGS literature studied pigs, which may be explained by the emergence and global spread of swine viruses such as porcine epidemic diarrhea virus [136] and African Swine Fever virus [137] in the recent decade. Indeed, these viruses were reported in our included studies [75,88]. Other mNGS studies also found hepatitis E viruses in pigs, known to be zoonotic. In addition to these known animal viruses, a wide range of other viruses have been described in different livestock by using mNGS, highlighting the potential for using mNGS to identify not only viruses that affect the animals, but also zoonotic and novel viruses.
Although the global population of goats and sheep exceeds that of pigs [138], only nine mNGS studies of samples from small ruminants were identified in our review and hence it is not surprising that reported virus diversity of small ruminants was the lowest when compared to other common farm animals. Even though zoonoses from small ruminants such as chlamydiosis are thought to be transmitted via direct contact, the example of Q fever has shown the potential for spread by inhalation of contaminated aerosol [139]. The largest Dutch Q-fever outbreak in 2007–2010 with more than 3500 cases certainly indicated that zoonotic risk from small ruminants should not be underestimated [18], and in line with the predominance of viruses as causes of emerging disease outbreaks, studies are needed to characterize the virome of small ruminants and its possible relationship to the health and disease of exposed humans.
The viromes of farm animals in health and disease in the reviewed mNGS studies were relatively comparable. It could be that some infections were subclinical, for instance, porcine noroviruses and rotaviruses have been found in asymptomatic pigs as well as diarrheic pigs [140,141]. Also, as the major clinical syndromes can be caused by a range of pathogens, it is unlikely that a single predominant virus would be found in diseased animals, unless it would be a highly prevalent disease cause. This highlights the challenge in incorporating complex viral metagenomic data in disease association studies. In addition, disease association studies require deeper taxonomic annotation of virus sequences to the level of genus and species, which can be challenging with short read data provided by the most commonly used sequencing platforms, although sequence assembly methods have been improved considerably [142].
We showed that Picornaviridae, Parvoviridae, and Astroviridae were among the most commonly identified virus families in common farm animals. Therefore, although sample sizes were relatively small, these virus families may be signature viruses to indicate livestock exposure. For instance, Avastrovirus, an avian virus, so far has only been reported in poultry sample metagenomes. Multiple signature viruses would be required to set up a viral fingerprint profile for each livestock type, as one genetic marker may not be sensitive and/or specific enough. In our studies, we aim to identify stable signatures to allow tracking the flow of viruses between different livestock, humans, and the surrounding environment.
There are limitations in our review dataset of the available farm animal mNGS studies. Reporting bias might be introduced with different study objectives and research interests, the use of different algorithms for metagenomic analysis, reference databases [143], and different sample preparation strategies (e.g., presence/absence of nuclease treatment, filtration and random amplification, different sizes of filters used, and centrifugation strategies) [144]. Some studies performed pooling among samples from different farms. This practice is cost-effective for a resource-limited setting, however viruses with low abundance may be diluted and missed. About 90% of studies did not provide raw sequencing data on SRA or ENA which hampers cross-study comparison and future large-scale reanalysis and interpretation. This is crucial, as it has been shown that outputs from metagenomic workflows are not directly comparable with the use of different algorithms and reference databases. Data sharing is also warranted for successful pathogen surveillance and outbreak detection [145,146] and our review shows that there is much to be gained in the field of metagenomics. It was difficult to compare virome composition of farm animals from different farm types and of different ages in available studies. Over 80% and 40% of available studies did not specify farm type and age of farm animals. We observed that metadata availability is consistently lacking in available literature regardless of different study types. Our review shows that the current state of the art is far from providing such information as the minimal metadata that is needed to select datasets for analysis is rarely provided with published reports. In the longer term, a better understanding of the association between farm types and virome composition of farm animals would guide farm management practices for reducing risks from zoonoses. In the meantime, it is important to benchmark metagenomic tools and reference databases [147,148] and assess epidemic potential of pathogens for more accurate zoonoses prediction and detection [149].
Available viral mNGS studies of healthy farm animals primarily focused on fecal virome, probably because fecal samples of farm animals are a non-invasive sample and are readily available to be collected. However, one must notice that recently EIDs are like MERS, such as the avian and swine influenza, and are mostly respiratory related, although viral shedding of MERS coronavirus was also reported in camel and human stools and some MERS patients also experienced diarrhea [150]. Nonetheless, viral mNGS studies of respiratory samples of farm animals are substantially overlooked and underreported.
To our best knowledge, this is the first systematic review that summarizes available literature that performed viral mNGS in farm animal samples. These aforementioned limitations of the reviewed dataset may hinder the reusability of the published metagenomic data. An incredible amount of metagenomics data is being generated these days as we speak, given reduced costs of sequencing and increased availability of NGS platforms. Therefore, timing is perfect to take one step further to implement good data management practices referred as the “FAIR” (Findable, Accessible, Interoperable, and Reusable) data principles [151]. In brief, data should be properly indexed and easy to find and assess. Data should also be described with rich and well-defined metadata that can be interpreted by humans and computers. By making metagenomic data “FAIR”, reusability of the data can be optimized so the data can be combined into meta-analysis settings. Minimum datasets for the sharing of pathogen genomic data have already been established through the global microbial identifier project [152]. We propose to always include breed types, age of the animals, and farm types in the minimal metadata set to allow determination of viral fingerprints of different farm animals. More “FAIR” metagenomic data of farm animals would be favorable for future large-scale farm animal virome characterization analysis that can guide zoonotic outbreak preparedness.
This review provides an overview of available literature that performed viral mNGS in common livestock including cattle, small ruminants, poultry, and pigs. We summarized virus diversity of these farm animals reported in available literature and reviewed their study designs. This is a good starting point for identifying species signatures for porcine, bovine, and poultry fecal viromes, but major gaps in the data of the virus diversity of small ruminants exist. Given the lack and inconsistency of data and metadata availability in available literature, it is important to apply the “FAIR” data principles in future farm animal mNGS studies or any other related studies for enhancing data reusability. In the longer term, developing a better understanding of farm animal virome is crucial for detection of potential zoonotic pathogens, zoonotic outbreak response, and preparedness [153], as well as the preparedness to combat livestock diseases.
Acknowledgments
We thank Gerdien de Jonge from Erasmus MC medical library for technical assistance during the systematic literature search.
Supplementary Materials
Supplementary materials are available at https://www.mdpi.com/1999-4915/12/1/107/s1.
Author Contributions
K.T.T.K. and M.P.G.K. conceived the study. K.T.T.K. conducted the systematic review, analyzed and visualized data, and drafted the manuscript. K.T.T.K. and D.F.N. performed literature screening and revised the manuscript. M.V.T.P. advised on data analysis and revised the manuscript. M.P.G.K. supervised the study, revised the manuscript, and acquired the funding. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by ZonMW TOP project 91217040. D.F.N. and M.P.G.K. are supported by the European Union’s Horizon 2020 research and innovation programme (COMPARE, Grant Agreement No. 643476). M.V.T.P. is supported by Marie Sklodowska-Curie Individual Fellowship, funded by European Union’s Horizon 2020 research and innovation programme (Grant Agreement No. 799417).
Conflicts of Interest
All authors declare no conflicts of interest.
References
- 1.Jones K.E., Patel N.G., Levy M.A., Storeygard A., Balk D., Gittleman J.L., Daszak P. Global trends in emerging infectious diseases. Nature. 2008;451:990–993. doi: 10.1038/nature06536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wolfe N.D., Dunavan C.P., Diamond J. Origins of major human infectious diseases. Nature. 2007;447:279–283. doi: 10.1038/nature05775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones B.A., Grace D., Kock R., Alonso S., Rushton J., Said M.Y., McKeever D., Mutua F., Young J., McDermott J., et al. Zoonosis emergence linked to agricultural intensification and environmental change. Proc. Natl. Acad. Sci. USA. 2013;110:8399–8404. doi: 10.1073/pnas.1208059110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guan Y., Zheng B.J., He Y.Q., Liu X.L., Zhuang Z.X., Cheung C.L., Luo S.W., Li P.H., Zhang L.J., Guan Y.J., et al. Isolation and characterization of viruses related to the SARS coronavirus from animals in Southern China. Science. 2003;302:276–278. doi: 10.1126/science.1087139. [DOI] [PubMed] [Google Scholar]
- 5.Hsu V.P., Hossain M.J., Parashar U.D., Ali M.M., Ksiazek T.G., Kuzmin I., Niezgoda M., Rupprecht C., Bresee J., Breiman R.F. Nipah virus encephalitis reemergence, Bangladesh. Emerg. Infect. Dis. 2004;10:2082–2087. doi: 10.3201/eid1012.040701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chatterjee P. Nipah virus outbreak in India. Lancet. 2018;391:2200. doi: 10.1016/S0140-6736(18)31252-2. [DOI] [PubMed] [Google Scholar]
- 7.Roberts L. Nigeria hit by unprecedented Lassa fever outbreak. Science. 2018;359:1201–1202. doi: 10.1126/science.359.6381.1201. [DOI] [PubMed] [Google Scholar]
- 8.Azhar E.I., El-Kafrawy S.A., Farraj S.A., Hassan A.M., Al-Saeed M.S., Hashem A.M., Madani T.A. Evidence for camel-to-human transmission of MERS coronavirus. N. Engl. J. Med. 2014;370:2499–2505. doi: 10.1056/NEJMoa1401505. [DOI] [PubMed] [Google Scholar]
- 9.Lam T.T.Y., Zhou B., Wang J., Chai Y., Shen Y., Chen X., Ma C., Hong W., Chen Y., Zhang Y., et al. Dissemination, divergence and establishment of H7N9 influenza viruses in China. Nature. 2015;522:102–105. doi: 10.1038/nature14348. [DOI] [PubMed] [Google Scholar]
- 10.Tambo E., Olalubi O.A., Sacko M. Rift valley fever epidemic in Niger near border with Mali. Lancet Infect. Dis. 2016;16:1319–1320. doi: 10.1016/S1473-3099(16)30477-7. [DOI] [PubMed] [Google Scholar]
- 11.Fraaij P.L.A., Wildschut E.D., Houmes R.J., Swaan C.M., Hoebe C.J., de Jonge H.C.C., Tolsma P., de Kleer I., Pas S.D., Oude Munnink B.B., et al. Severe acute respiratory infection caused by swine influenza virus in a child necessitating extracorporeal membrane oxygenation (ECMO), The Netherlands, October 2016. Eurosurveillance. 2016;21:8–10. doi: 10.2807/1560-7917.ES.2016.21.48.30416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith G.J.D., Vijaykrishna D., Bahl J., Lycett S.J., Worobey M., Pybus O.G., Ma S.K., Cheung C.L., Raghwani J., Bhatt S., et al. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza a epidemic. Nature. 2009;459:1122–1125. doi: 10.1038/nature08182. [DOI] [PubMed] [Google Scholar]
- 13.Coker R., Rushton J., Mounier-Jack S., Karimuribo E., Lutumba P., Kambarage D., Pfeiffer D.U., Stärk K., Rweyemamu M. Towards a conceptual framework to support one-health research for policy on emerging zoonoses. Lancet Infect. Dis. 2011;11:326–331. doi: 10.1016/S1473-3099(10)70312-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Castillo-Chavez C., Curtiss R., Daszak P., Levin S.A., Patterson-Lomba O., Perrings C., Poste G., Towers S. Beyond Ebola: Lessons to mitigate future pandemics. Lancet Glob. Health. 2015;3:e354–e355. doi: 10.1016/S2214-109X(15)00068-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koopmans M., Wilbrink B., Conyn M., Natrop G., Van Der Nat H., Vennema H., Meijer A., Van Steenbergen J., Fouchier R., Osterhaus A., et al. Transmission of H7N7 avian influenza A virus to human beings during a large outbreak in commercial poultry farms in the Netherlands. Lancet. 2004;363:587–593. doi: 10.1016/S0140-6736(04)15589-X. [DOI] [PubMed] [Google Scholar]
- 16.Sims L.D., Domenech J., Benigno C., Kahn S., Kamata A., Lubroth J., Martin V., Roeder P. Origin and evolution of highly pathogenic H5N1 avian influenza in Asia. Vet. Rec. 2005;157:159–164. doi: 10.1136/vr.157.6.159. [DOI] [PubMed] [Google Scholar]
- 17.Van der Hoek W., Dijkstra F., Schimmer B., Schneeberger P.M., Vellema P., Wijkmans C., ter Schegget R., Hackert V., van Duynhoven Y. Q fever in the Netherlands: An update on the epidemiology and control measures. Eurosurveillance. 2010;15:15. [PubMed] [Google Scholar]
- 18.Schimmer B., Dijkstra F., Vellema P., Schneeberger P.M., Hackert V., ter Schegget R., Wijkmans C., van Duynhoven Y., van der Hoek W. Sustained intensive transmission of Q fever in the south of the Netherlands, 2009. Eurosurveillance. 2009;14:19210. doi: 10.2807/ese.14.19.19210-en. [DOI] [PubMed] [Google Scholar]
- 19.Destoumieux-Garzón D., Mavingui P., Boetsch G., Boissier J., Darriet F., Duboz P., Fritsch C., Giraudoux P., Le Roux F., Morand S., et al. The one health concept: 10 years old and a long road ahead. Front. Vet. Sci. 2018;5:14. doi: 10.3389/fvets.2018.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Quan P.L., Wagner T.A., Briese T., Torgerson T.R., Hornig M., Tashmukhamedova A., Firth C., Palacios G., Baisre-de-Leon A., Paddock C.D., et al. Astrovirus encephalitis in boy with X-linked agammaglobulinemia. Emerg. Infect. Dis. 2010;16:918–925. doi: 10.3201/eid1606.091536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Naccache S.N., Peggs K.S., Mattes F.M., Phadke R., Garson J.A., Grant P., Samayoa E., Federman S., Miller S., Lunn M.P., et al. Diagnosis of neuroinvasive astrovirus infection in an immunocompromised adult with encephalitis by unbiased next-generation sequencing. Clin. Infect. Dis. 2015;60:919–923. doi: 10.1093/cid/ciu912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chiu C.Y., Coffey L.L., Murkey J., Symmes K., Sample H.A., Wilson M.R., Naccache S.N., Arevalo S., Somasekar S., Federman S., et al. Diagnosis of fatal human case of St. Louis encephalitis virus infection by metagenomic sequencing, California. 2016. Emerg. Infect. Dis. 2017;23:1694–1698. doi: 10.3201/eid2310.161986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Briese T., Paweska J.T., McMullan L.K., Hutchison S.K., Street C., Palacios G., Khristova M.L., Weyer J., Swanepoel R., Egholm M., et al. Genetic detection and characterization of Lujo virus, a new hemorrhagic fever-associated arenavirus from southern Africa. PLoS Pathog. 2009;5:e1000455. doi: 10.1371/journal.ppat.1000455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blomström A.L., Fossum C., Wallgren P., Berg M. Viral metagenomic analysis displays the Co-infection situation in healthy and PMWS affected pigs. PLoS ONE. 2016;11:e0166863. doi: 10.1371/journal.pone.0166863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yu X., Jin T., Cui Y., Pu X., Li J., Xu J., Liu G., Jia H., Liu D., Song S., et al. Influenza H7N9 and H9N2 Viruses: Coexistence in Poultry Linked to Human H7N9 Infection and Genome Characteristics. J. Virol. 2014;88:3423–3431. doi: 10.1128/JVI.02059-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nieuwenhuijse D.F., Koopmans M.P.G. Metagenomic sequencing for surveillance of food-and waterborne viral diseases. Front. Microbiol. 2017;8:69. doi: 10.3389/fmicb.2017.00230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yinda C.K., Vanhulle E., Conceição-Neto N., Beller L., Deboutte W., Shi C., Ghogomu S.M., Maes P., Van Ranst M., Matthijnssens J. Gut Virome Analysis of Cameroonians Reveals High Diversity of Enteric Viruses, Including Potential Interspecies Transmitted Viruses. mSphere. 2019;4:e00585-18. doi: 10.1128/mSphere.00585-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Phan T.G., Kapusinszky B., Wang C., Rose R.K., Lipton H.L., Delwart E.L. The fecal viral flora of wild rodents. PLoS Pathog. 2011;7:e1002218. doi: 10.1371/journal.ppat.1002218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zheng X.Y., Qiu M., Guan W.J., Li J.M., Chen S.W., Cheng M.J., Huo S.T., Chen Z., Wu Y., Jiang L.N., et al. Viral metagenomics of six bat species in close contact with humans in southern China. Arch. Virol. 2018;163:73–88. doi: 10.1007/s00705-017-3570-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Blomström A.L., Ye X., Fossum C., Wallgren P., Berg M. Characterisation of the virome of tonsils from conventional pigs and from specific pathogen-free pigs. Viruses. 2018;10:382. doi: 10.3390/v10070382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carroll D., Daszak P., Wolfe N.D., Gao G.F., Morel C.M., Morzaria S., Pablos-Méndez A., Tomori O., Mazet J.A.K. The Global Virome Project. Science. 2018;359:872–874. doi: 10.1126/science.aap7463. [DOI] [PubMed] [Google Scholar]
- 32.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P.A., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Team, R.C. R: A Language and Environment for Statistical Computing. [(accessed on 5 December 2019)]; Available online: https://www.r-project.org/
- 34.Wickham H., François R., Henry L., Müller K. dplyr: A Grammar of Data Manipulation. [(accessed on 5 December 2019)]; Available online: https://cran.r-project.org/package=dplyr.
- 35.Wickham H. Ggplot2: Elegant Graphics for Data Analysis. Springer; New York, NY, USA: 2016. [Google Scholar]
- 36.Wickham H. Reshaping data with the reshape package. J. Stat. Softw. 2007;21:1–20. doi: 10.18637/jss.v021.i12. [DOI] [Google Scholar]
- 37.Wickham H. Stringr: Simple, Consistent Wrappers for Common String Operations. [(accessed on 5 December 2019)]; Available online: https://CRAN.R-project.org/package=stringr.
- 38.Hulo C., De Castro E., Masson P., Bougueleret L., Bairoch A., Xenarios I., Le Mercier P. ViralZone: A knowledge resource to understand virus diversity. Nucleic Acids Res. 2011;39:D576–D582. doi: 10.1093/nar/gkq901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lefkowitz E.J., Dempsey D.M., Hendrickson R.C., Orton R.J., Siddell S.G., Smith D.B. Virus taxonomy: The database of the International Committee on Taxonomy of Viruses (ICTV) Nucleic Acids Res. 2017;46:D708–D717. doi: 10.1093/nar/gkx932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cheung A.K., Ng T.F.F., Lager K.M., Alt D.P., Delwart E.L., Pogranichniy R.M. Unique circovirus-like genome detected in pig feces. Genome Announc. 2014;2:e00251-14. doi: 10.1128/genomeA.00251-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hause B.M., Collin E.A., Peddireddi L., Yuan F., Chen Z., Hesse R.A., Gauger P.C., Clement T., Fang Y., Anderson G. Discovery of a novel putative atypical porcine pestivirus in pigs in the USA. J. Gen. Virol. 2015;96:2994–2998. doi: 10.1099/jgv.0.000251. [DOI] [PubMed] [Google Scholar]
- 42.Pankovics P., Boros Á., Nemes C., Kapusinszky B., Delwart E., Reuter G. Molecular characterization of a novel picobirnavirus in a chicken. Arch. Virol. 2018;163:3455–3458. doi: 10.1007/s00705-018-4012-6. [DOI] [PubMed] [Google Scholar]
- 43.Yang C., Wang L., Shen H., Zheng Y., Bade S.A., Gauger P.C., Chen Q., Zhang J., Guo B., Yoon K.J., et al. Detection and genetic characterization of porcine pegivirus in pigs in the United States. Transbound. Emerg. Dis. 2018;65:618–626. doi: 10.1111/tbed.12844. [DOI] [PubMed] [Google Scholar]
- 44.Mitra N., Cernicchiaro N., Torres S., Li F., Hause B.M. Metagenomic characterization of the virome associated with bovine respiratory disease in feedlot cattle identified novel viruses and suggests an etiologic role for influenza D virus. J. Gen. Virol. 2016;97:1771–1784. doi: 10.1099/jgv.0.000492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Grierson S.S., McGowan S., Cook C., Steinbach F., Choudhury B. Molecular and in vitro characterisation of hepatitis E virus from UK pigs. Virology. 2019;527:116–121. doi: 10.1016/j.virol.2018.10.018. [DOI] [PubMed] [Google Scholar]
- 46.Hause B.M., Duff J.W., Scheidt A., Anderson G. Virus detection using metagenomic sequencing of swine nasal and rectal swabs. J. Swine Health Prod. 2016;24:304–308. [Google Scholar]
- 47.Chen X., Zhang B., Yue H., Wang Y., Zhou F., Zhang Q., Tang C. A novel astrovirus species in the gut of yaks with diarrhoea in the Qinghai-Tibetan plateau, 2013. J. Gen. Virol. 2015;96:3672–3680. doi: 10.1099/jgv.0.000303. [DOI] [PubMed] [Google Scholar]
- 48.Ng T.F.F., Kondov N.O., Deng X., Van Eenennaam A., Neibergs H.L., Delwart E. A Metagenomics and Case-Control Study To Identify Viruses Associated with Bovine Respiratory Disease. J. Virol. 2015;89:5340–5349. doi: 10.1128/JVI.00064-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hause B.M., Collin E.A., Anderson J., Hesse R.A., Anderson G. Bovine rhinitis viruses are common in U.S. cattle with bovine respiratory disease. PLoS ONE. 2015;10:e0121998. doi: 10.1371/journal.pone.0121998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Guo Z., He Q., Tang C., Zhang B., Yue H. Identification and genomic characterization of a novel CRESS DNA virus from a calf with severe hemorrhagic enteritis in China. Virus Res. 2018;255:141–146. doi: 10.1016/j.virusres.2018.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dumarest M., Muth E., Cheval J., Gratigny M., Hébert C., Gagnieur L., Eloit M. Viral diversity in swine intestinal mucus used for the manufacture of heparin as analyzed by high-throughput sequencing. Biologicals. 2015;43:31–36. doi: 10.1016/j.biologicals.2014.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tokarz R., Sameroff S., Hesse R.A., Hause B.M., Desai A., Jain K., Ian Lipkin W. Discovery of a novel nidovirus in cattle with respiratory disease. J. Gen. Virol. 2015;96:2188–2193. doi: 10.1099/vir.0.000166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang H., Li S., Mahmood A., Yang S., Wang X., Shen Q., Shan T., Deng X., Li J., Hua X., et al. Plasma virome of cattle from forest region revealed diverse small circular ssDNA viral genomes. Virol. J. 2018;15:11. doi: 10.1186/s12985-018-0923-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ling Y., Zhang X., Qi G., Yang S., Jingjiao L., Shen Q., Wang X., Cui L., Hua X., Deng X., et al. Viral metagenomics reveals significant viruses in the genital tract of apparently healthy dairy cows. Arch. Virol. 2019;164:1059–1067. doi: 10.1007/s00705-019-04158-4. [DOI] [PubMed] [Google Scholar]
- 55.Cibulski S.P., Teixeira T.F., dos Santos H.F., de Sales Lima F.E., Scheffer C.M., Varela A.P.M., de Lima D.A., Schmidt C., Silveira F., de Almeida L.L., et al. Ungulate copiparvovirus 1 (bovine parvovirus 2): Characterization of a new genotype and associated viremia in different bovine age groups. Virus Genes. 2016;52:134–137. doi: 10.1007/s11262-015-1266-x. [DOI] [PubMed] [Google Scholar]
- 56.Sadeghi M., Kapusinszky B., Yugo D.M., Phan T.G., Deng X., Kanevsky I., Opriessnig T., Woolums A.R., Hurley D.J., Meng X.J., et al. Virome of US bovine calf serum. Biologicals. 2017;46:64–67. doi: 10.1016/j.biologicals.2016.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Blomström A.L., Oma V., Khatri M., Hansen H.H., Stokstad M., Berg M., Myrmel M. Genome sequence of a bovine rhinitis B virus identified in cattle in Sweden. Genome Announc. 2017;5:e00172-17. doi: 10.1128/genomeA.00172-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nagai M., Omatsu T., Aoki H., Otomaru K., Uto T., Koizumi M., Minami-Fukuda F., Takai H., Murakami T., Masuda T., et al. Full genome analysis of bovine astrovirus from fecal samples of cattle in Japan: Identification of possible interspecies transmission of bovine astrovirus. Arch. Virol. 2015;160:2491–2501. doi: 10.1007/s00705-015-2543-7. [DOI] [PubMed] [Google Scholar]
- 59.Mekata H., Yamamoto M., Hamabe S., Tanaka H., Omatsu T., Mizutani T., Hause B.M., Okabayashi T. Molecular epidemiological survey and phylogenetic analysis of bovine influenza D virus in Japan. Transbound. Emerg. Dis. 2018;65:e355–e360. doi: 10.1111/tbed.12765. [DOI] [PubMed] [Google Scholar]
- 60.Ferragut F., Vega C.G., Mauroy A., Conceição-Neto N., Zeller M., Heylen E., Uriarte E.L., Bilbao G., Bok M., Matthijnssens J., et al. Molecular detection of bovine Noroviruses in Argentinean dairy calves: Circulation of a tentative new genotype. Infect. Genet. Evol. 2016;40:144–150. doi: 10.1016/j.meegid.2016.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hayashi-Miyamoto M., Murakami T., Minami-Fukuda F., Tsuchiaka S., Kishimoto M., Sano K., Naoi Y., Asano K., Ichimaru T., Haga K., et al. Diversity in VP3, NSP3, and NSP4 of rotavirus B detected from Japanese cattle. Infect. Genet. Evol. 2017;49:97–103. doi: 10.1016/j.meegid.2017.01.003. [DOI] [PubMed] [Google Scholar]
- 62.Omatsu T., Tsuchiaka S., Hirata T., Shiroma Y., Okazaki S., Katayama Y., Oba M., Nishiura N., Sassa Y., Furuya T., et al. Detection of enterovirus genome sequence from diarrheal feces of goat. Virus Genes. 2014;48:550–552. doi: 10.1007/s11262-014-1057-9. [DOI] [PubMed] [Google Scholar]
- 63.Maganga G.D., Relmy A., Bakkali-Kassimi L., Ngoubangoye B., Tsoumbou T., Bouchier C., N’Dilimabaka N., Leroy E.M., Zientara S., Berthet N. Molecular characterization of Orf virus in goats in Gabon, Central Africa. Virol. J. 2016;13:79. doi: 10.1186/s12985-016-0535-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chen F., Knutson T.P., Ciarlet M., Sturos M., Marthaler D.G. Complete genome characterization of a rotavirus B (RVB) strain identified in alpine goat kids with enteritis reveals inter-species transmission with RVB bovine strains. J. Gen. Virol. 2018;99:457–463. doi: 10.1099/jgv.0.001022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yang L.E., Zhao Z., Hou G., Zhang C., Liu J., Xu L., Li W., Tan Z., Tu C., He B. Genomes and seroprevalence of severe fever with thrombocytopenia syndrome virus and Nairobi sheep disease virus in Haemaphysalis longicornis ticks and goats in Hubei, China. Virology. 2019;529:234–245. doi: 10.1016/j.virol.2019.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Day J.M., Ballard L.L., Duke M.V., Scheffler B.E., Zsak L. Metagenomic analysis of the turkey gut RNA virus community. Virol. J. 2010;7:313. doi: 10.1186/1743-422X-7-313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shah J.D., Baller J., Zhang Y., Silverstein K., Xing Z., Cardona C.J. Comparison of tissue sample processing methods for harvesting the viral metagenome and a snapshot of the RNA viral community in a turkey gut. J. Virol. Methods. 2014;209:15–24. doi: 10.1016/j.jviromet.2014.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kim H.R., Yoon S.J., Lee H.S., Kwon Y.K. Identification of a picornavirus from chickens with transmissible viral proventriculitis using metagenomic analysis. Arch. Virol. 2015;160:701–709. doi: 10.1007/s00705-014-2325-7. [DOI] [PubMed] [Google Scholar]
- 69.Devaney R., Trudgett J., Trudgett A., Meharg C., Smyth V. A metagenomic comparison of endemic viruses from broiler chickens with runting-stunting syndrome and from normal birds. Avian Pathol. 2016;45:616–629. doi: 10.1080/03079457.2016.1193123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Qiu Y., Chen J.M., Wang T., Hou G.Y., Zhuang Q.Y., Wu R., Wang K.C. Detection of viromes of RNA viruses using the next generation sequencing libraries prepared by three methods. Virus Res. 2017;237:22–26. doi: 10.1016/j.virusres.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lima D.A., Cibulski S.P., Tochetto C., Varela A.P.M., Finkler F., Teixeira T.F., Loiko M.R., Cerva C., Junqueira D.M., Mayer F.Q., et al. The intestinal virome of malabsorption syndrome-affected and unaffected broilers through shotgun metagenomics. Virus Res. 2019;261:9–20. doi: 10.1016/j.virusres.2018.12.005. [DOI] [PubMed] [Google Scholar]
- 72.Lima D.A., Cibulski S.P., Finkler F., Teixeira T.F., Varela A.P.M., Cerva C., Loiko M.R., Scheffer C.M., Dos Santos H.F., Mayer F.Q., et al. Faecal virome of healthy chickens reveals a large diversity of the eukaryote viral community, including novel circular ssDNA viruses. J. Gen. Virol. 2017;98:690–703. doi: 10.1099/jgv.0.000711. [DOI] [PubMed] [Google Scholar]
- 73.Boros A., Pankovics P., Knowles N.J., Nemes C., Delwart E., Reuter G. Comparative Complete Genome Analysis of Chicken and Turkey Megriviruses (Family Picornaviridae): Long 3 Untranslated Regions with a Potential Second Open Reading Frame and Evidence for Possible Recombination. J. Virol. 2014;88:6434–6443. doi: 10.1128/JVI.03807-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Day J.M., Zsak L. Investigating Turkey Enteric Picornavirus and Its Association with Enteric Disease in Poults. Avian Dis. 2015;59:138–142. doi: 10.1637/10940-092414-RegR. [DOI] [PubMed] [Google Scholar]
- 75.Farlow J., Donduashvili M., Kokhreidze M., Kotorashvili A., Vepkhvadze N.G., Kotaria N., Gulbani A. Intra-epidemic genome variation in highly pathogenic African swine fever virus (ASFV) from the country of Georgia. Virol. J. 2018;15:190. doi: 10.1186/s12985-018-1099-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shan T., Li L., Simmonds P., Wang C., Moeser A., Delwart E. The Fecal Virome of Pigs on a High-Density Farm. J. Virol. 2011;85:11697–11708. doi: 10.1128/JVI.05217-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lager K.M., Ng T.F., Bayles D.O., Alt D.P., Delwart E.L., Cheung A.K. Diversity of viruses detected by deep sequencing in pigs from a common background. J. Vet. Diagn. Investig. 2012;24:1177–1179. doi: 10.1177/1040638712463212. [DOI] [PubMed] [Google Scholar]
- 78.Sachsenröder J., Twardziok S.O., Scheuch M., Johne R. The general composition of the faecal virome of pigs depends on age, but not on feeding with a probiotic bacterium. PLoS ONE. 2014;9:e88888. doi: 10.1371/journal.pone.0088888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhang B., Tang C., Yue H., Ren Y., Song Z. Viral metagenomics analysis demonstrates the diversity of viral flora in piglet diarrhoeic faeces in China. J. Gen. Virol. 2014;95:1603–1611. doi: 10.1099/vir.0.063743-0. [DOI] [PubMed] [Google Scholar]
- 80.Amimo J.O., El Zowalaty M.E., Githae D., Wamalwa M., Djikeng A., Nasrallah G.K. Metagenomic analysis demonstrates the diversity of the fecal virome in asymptomatic pigs in East Africa. Arch. Virol. 2016;161:887–897. doi: 10.1007/s00705-016-2819-6. [DOI] [PubMed] [Google Scholar]
- 81.Hargitai R., Pankovics P., Kertész A.M., Bíró H., Boros Á., Phan T.G., Delwart E., Reuter G. Detection and genetic characterization of a novel parvovirus distantly related to human bufavirus in domestic pigs. Arch. Virol. 2016;161:1033–1037. doi: 10.1007/s00705-015-2732-4. [DOI] [PubMed] [Google Scholar]
- 82.Cheung A.K., Ng T.F., Lager K.M., Bayles D.O., Alt D.P., Delwart E.L., Pogranichniy R.M., Kehrli M.E. A divergent clade of circular single-stranded DNA viruses from pig feces. Arch. Virol. 2013;158:2157–2162. doi: 10.1007/s00705-013-1701-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Theuns S., Conceição-Neto N., Zeller M., Heylen E., Roukaerts I.D.M., Desmarets L.M.B., Van Ranst M., Nauwynck H.J., Matthijnssens J. Characterization of a genetically heterogeneous porcine rotavirus C, and other viruses present in the fecal virome of a non-diarrheic Belgian piglet. Infect. Genet. Evol. 2016;43:135–145. doi: 10.1016/j.meegid.2016.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Akagami M., Ito M., Niira K., Kuroda M., Masuda T., Haga K., Tsuchiaka S., Naoi Y., Kishimoto M., Sano K., et al. Complete genome analysis of porcine kobuviruses from the feces of pigs in Japan. Virus Genes. 2017;53:593–602. doi: 10.1007/s11262-017-1464-9. [DOI] [PubMed] [Google Scholar]
- 85.Conceição-Neto N., Theuns S., Cui T., Zeller M., Yinda C.K., Christiaens I., Heylen E., Van Ranst M., Carpentier S., Nauwynck H.J., et al. Identification of an enterovirus recombinant with a torovirus-like gene insertion during a diarrhea outbreak in fattening pigs. Virus Evol. 2017;3:vex024. doi: 10.1093/ve/vex024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Knutson T.P., Velayudhan B.T., Marthaler D.G. A porcine enterovirus G associated with enteric disease contains a novel papain-like cysteine protease. J. Gen. Virol. 2017;98:1305–1310. doi: 10.1099/jgv.0.000799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kuroda M., Masuda T., Ito M., Naoi Y., Doan Y.H., Haga K., Tsuchiaka S., Kishimoto M., Sano K., Omatsu T., et al. Genetic diversity and intergenogroup recombination events of sapoviruses detected from feces of pigs in Japan. Infect. Genet. Evol. 2017;55:209–217. doi: 10.1016/j.meegid.2017.09.013. [DOI] [PubMed] [Google Scholar]
- 88.Chen Q., Wang L., Zheng Y., Zhang J., Guo B., Yoon K.J., Gauger P.C., Harmon K.M., Main R.G., Li G. Metagenomic analysis of the RNA fraction of the fecal virome indicates high diversity in pigs infected by porcine endemic diarrhea virus in the United States. Virol. J. 2018;15:95. doi: 10.1186/s12985-018-1001-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Masuda T., Sunaga F., Naoi Y., Ito M., Takagi H., Katayama Y., Omatsu T., Oba M., Sakaguchi S., Furuya T., et al. Whole genome analysis of a novel picornavirus related to the Enterovirus/Sapelovirus supergroup from porcine feces in Japan. Virus Res. 2018;257:68–73. doi: 10.1016/j.virusres.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 90.Oba M., Naoi Y., Ito M., Masuda T., Katayama Y., Sakaguchi S., Omatsu T., Furuya T., Yamasato H., Sunaga F., et al. Metagenomic identification and sequence analysis of a Teschovirus A-related virus in porcine feces in Japan, 2014–2016. Infect. Genet. Evol. 2018;66:210–216. doi: 10.1016/j.meegid.2018.10.004. [DOI] [PubMed] [Google Scholar]
- 91.Theuns S., Vanmechelen B., Bernaert Q., Deboutte W., Vandenhole M., Beller L., Matthijnssens J., Maes P., Nauwynck H.J. Nanopore sequencing as a revolutionary diagnostic tool for porcine viral enteric disease complexes identifies porcine kobuvirus as an important enteric virus. Sci. Rep. 2018;8:9830. doi: 10.1038/s41598-018-28180-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Tsuchiaka S., Naoi Y., Imai R., Masuda T., Ito M., Akagami M., Ouchi Y., Ishii K., Sakaguchi S., Omatsu T., et al. Genetic diversity and recombination of enterovirus G strains in Japanese pigs: High prevalence of strains carrying a papain-like cysteine protease sequence in the enterovirus G population. PLoS ONE. 2018;13:e0190819. doi: 10.1371/journal.pone.0190819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wang Y., Zhang W., Liu Z., Fu X., Yuan J., Zhao J., Lin Y., Shen Q., Wang X., Deng X., et al. Full-length and defective enterovirus G genomes with distinct torovirus protease insertions are highly prevalent on a Chinese pig farm. Arch. Virol. 2018;163:2471–2476. doi: 10.1007/s00705-018-3875-x. [DOI] [PubMed] [Google Scholar]
- 94.Hause B.M., Padmanabhan A., Pedersen K., Gidlewski T. Feral swine virome is dominated by single-stranded DNA viruses and contains a novel Orthopneumovirus which circulates both in feral and domestic swine. J. Gen. Virol. 2016;97:2090–2095. doi: 10.1099/jgv.0.000554. [DOI] [PubMed] [Google Scholar]
- 95.Qin S., Ruan W., Yue H., Tang C., Zhou K., Zhang B. Viral communities associated with porcine respiratory disease complex in intensive commercial farms in Sichuan province, China. Sci. Rep. 2018;8:13341. doi: 10.1038/s41598-018-31554-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zheng S., Wu X., Zhang L., Xin C., Liu Y., Shi J., Peng Z., Xu S., Fu F., Yu J., et al. The occurrence of porcine circovirus 3 without clinical infection signs in Shandong Province. Transbound. Emerg. Dis. 2017;64:1337–1341. doi: 10.1111/tbed.12667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Tochetto C., Lima D.A., Varela A.P.M., Loiko M.R., Paim W.P., Scheffer C.M., Herpich J.I., Cerva C., Schmitd C., Cibulski S.P., et al. Full-Genome Sequence of Porcine Circovirus type 3 recovered from serum of sows with stillbirths in Brazil. Transbound. Emerg. Dis. 2018;65:5–9. doi: 10.1111/tbed.12735. [DOI] [PubMed] [Google Scholar]
- 98.Blomström A.L., Belák S., Fossum C., McKillen J., Allan G., Wallgren P., Berg M. Detection of a novel porcine boca-like virus in the background of porcine circovirus type 2 induced postweaning multisystemic wasting syndrome. Virus Res. 2009;146:125–129. doi: 10.1016/j.virusres.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 99.Hause B.M., Smith C., Bishop B., Stewart C., Simonson R. Complete genome sequence of a porcine polyomavirus from nasal swabs of pigs with respiratory disease. Genome Announc. 2018;6:e00344-18. doi: 10.1128/genomeA.00344-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sano K., Naoi Y., Kishimoto M., Masuda T., Tanabe H., Ito M., Niira K., Haga K., Asano K., Tsuchiaka S., et al. Identification of further diversity among posaviruses. Arch. Virol. 2016;161:3541–3548. doi: 10.1007/s00705-016-3048-8. [DOI] [PubMed] [Google Scholar]
- 101.Chen Z., Collin E., Peddireddi L., Clement T., Gauger P., Hause B.M. Genetic diversity in envelope genes of contemporary U.S. porcine reproductive and respiratory syndrome virus strains influences viral antigenicity. Res. Vet. Sci. 2017;115:432–441. doi: 10.1016/j.rvsc.2017.07.027. [DOI] [PubMed] [Google Scholar]
- 102.Zhang J., Zheng Y., Xia X.Q., Chen Q., Bade S.A., Yoon K.J., Harmon K.M., Gauger P.C., Main R.G., Li G. High-throughput whole genome sequencing of Porcine reproductive and respiratory syndrome virus from cell culture materials and clinical specimens using next-generation sequencing technology. J. Vet. Diagn. Investig. 2017;29:41–50. doi: 10.1177/1040638716673404. [DOI] [PubMed] [Google Scholar]
- 103.Niira K., Ito M., Masuda T., Saitou T., Abe T., Komoto S., Sato M., Yamasato H., Kishimoto M., Naoi Y., et al. Whole genome sequences of Japanese porcine species C rotaviruses reveal a high diversity of genotypes of individual genes and will contribute to a comprehensive, generally accepted classification system. Infect. Genet. Evol. 2016;44:106–113. doi: 10.1016/j.meegid.2016.06.041. [DOI] [PubMed] [Google Scholar]
- 104.Phan T.G., Giannitti F., Rossow S., Marthaler D., Knutson T., Li L., Deng X., Resende T., Vannucci F., Delwart E. Detection of a novel circovirus PCV3 in pigs with cardiac and multi-systemic inflammation. Virol. J. 2016;13:184. doi: 10.1186/s12985-016-0642-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Alekseev K.P., Penin A.A., Mukhin A.N., Khametova K.M., Grebennikova T.V., Yuzhakov A.G., Moskvina A.S., Musienko M.I., Raev S.A., Mishin A.M., et al. Genome characterization of a pathogenic porcine rotavirus B strain identified in Buryat republic, Russia in 2015. Pathogens. 2018;7:46. doi: 10.3390/pathogens7020046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Vidal A., Clilverd H., Cortey M., Martín-Valls G.E., Franzo G., Darwich L., Martín M., Mateu E. Full-genome characterization by deep sequencing of rotavirus A isolates from outbreaks of neonatal diarrhoea in pigs in Spain. Vet. Microbiol. 2018;227:12–19. doi: 10.1016/j.vetmic.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 107.Li J., Zhang W., Cui L., Shen Q., Hua X. Metagenomic identification, genetic characterization and genotyping of porcine sapoviruses. Infect. Genet. Evol. 2018;62:244–252. doi: 10.1016/j.meegid.2018.04.034. [DOI] [PubMed] [Google Scholar]
- 108.Masembe C., Michuki G., Onyango M., Rumberia C., Norling M., Bishop R.P., Djikeng A., Kemp S.J., Orth A., Skilton R.A., et al. Viral metagenomics demonstrates that domestic pigs are a potential reservoir for Ndumu virus. Virol. J. 2012;9:218. doi: 10.1186/1743-422X-9-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Schlottau K., Schulze C., Bilk S., Hanke D., Höper D., Beer M., Hoffmann B. Detection of a Novel Bovine Astrovirus in a Cow with Encephalitis. Transbound. Emerg. Dis. 2016;63:253–259. doi: 10.1111/tbed.12493. [DOI] [PubMed] [Google Scholar]
- 110.Baechlein C., Fischer N., Grundhoff A., Alawi M., Indenbirken D., Postel A., Baron A.L., Offinger J., Becker K., Beineke A., et al. Identification of a Novel Hepacivirus in Domestic Cattle from Germany. J. Virol. 2015;89:7007–7015. doi: 10.1128/JVI.00534-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bauermann F.V., Joshi L.R., Mohr K.A., Kutish G.F., Meier P., Chase C., Christopher-Hennings J., Diel D.G. A novel bovine papillomavirus type in the genus Dyokappapapillomavirus. Arch. Virol. 2017;162:3225–3228. doi: 10.1007/s00705-017-3443-9. [DOI] [PubMed] [Google Scholar]
- 112.De Souza W.M., Dennis T., Fumagalli M.J., Araujo J., Sabino-Santos G., Maia F.G.M., Acrani G.O., Carrasco A.D.O.T., Romeiro M.F., Modha S., et al. Novel parvoviruses from wild and domestic animals in Brazil provide new insights into parvovirus distribution and diversity. Viruses. 2018;10:143. doi: 10.3390/v10040143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Nagai M., Omatsu T., Aoki H., Kaku Y., Belsham G.J., Haga K., Naoi Y., Sano K., Umetsu M., Shiokawa M., et al. Identification and complete genome analysis of a novel bovine picornavirus in Japan. Virus Res. 2015;210:205–212. doi: 10.1016/j.virusres.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Hoffmann B., Scheuch M., Höper D., Jungblut R., Holsteg M., Schirrmeier H., Eschbaumer M., Goller K.V., Wernike K., Fischer M., et al. Novel orthobunyavirus in cattle, Europe, 2011. Emerg. Infect. Dis. 2012;18:469–472. doi: 10.3201/eid1803.111905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Masuda T., Nagai M., Yamasato H., Tsuchiaka S., Okazaki S., Katayama Y., Oba M., Nishiura N., Sassa Y., Omatsu T., et al. Identification of novel bovine group A rotavirus G15P[1 4] strain from epizootic diarrhea of adult cows by de novo sequencing using a next-generation sequencer. Vet. Microbiol. 2014;171:66–73. doi: 10.1016/j.vetmic.2014.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Reuter G., Pankovics P., Delwart E., Boros Á. Identification of a novel astrovirus in domestic sheep in Hungary. Arch. Virol. 2012;157:323–327. doi: 10.1007/s00705-011-1151-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Pfaff F., Schlottau K., Scholes S., Courtenay A., Hoffmann B., Höper D., Beer M. A novel astrovirus associated with encephalitis and ganglionitis in domestic sheep. Transbound. Emerg. Dis. 2017;64:677–682. doi: 10.1111/tbed.12623. [DOI] [PubMed] [Google Scholar]
- 118.Chen G.Q., Zhuang Q.Y., Wang K.C., Liu S., Shao J.Z., Jiang W.M., Hou G.Y., Li J.P., Yu J.M., Li Y.P., et al. Identification and Survey of a Novel Avian Coronavirus in Ducks. PLoS ONE. 2013;8:e72918. doi: 10.1371/journal.pone.0072918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Boros Á., Polgár B., Pankovics P., Fenyvesi H., Engelmann P., Phan T.G., Delwart E., Reuter G. Multiple divergent picobirnaviruses with functional prokaryotic Shine-Dalgarno ribosome binding sites present in cloacal sample of a diarrheic chicken. Virology. 2018;525:62–72. doi: 10.1016/j.virol.2018.09.008. [DOI] [PubMed] [Google Scholar]
- 120.Boros Á., Nemes C., Pankovics P., Kapusinszky B., Delwart E., Reuter G. Identification and complete genome characterization of a novel picornavirus in Turkey (Meleagris gallopavo) J. Gen. Virol. 2012;93:2171–2182. doi: 10.1099/vir.0.043224-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Boros Á., Nemes C., Pankovics P., Kapusinszky B., Delwart E., Reuter G. Genetic characterization of a novel picornavirus in turkeys (Meleagris gallopavo) distinct from turkey galliviruses and megriviruses and distantly related to the members of the genus Avihepatovirus. J. Gen. Virol. 2013;94:1496–1509. doi: 10.1099/vir.0.051797-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Yu J.M., Li J.S., Ao Y.Y., Duan Z.J. Detection of novel viruses in porcine fecal samples from China. Virol. J. 2013;10:39. doi: 10.1186/1743-422X-10-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Padmanabhan A., Hause B.M. Detection and characterization of a novel genotype of porcine astrovirus 4 from nasal swabs from pigs with acute respiratory disease. Arch. Virol. 2016;161:2575–2579. doi: 10.1007/s00705-016-2937-1. [DOI] [PubMed] [Google Scholar]
- 124.Yang W.Z., Yu J.M., Li J.S., Cheng W.X., Huang C.P., Duan Z.J. Genome characterization of a novel porcine bocavirus. Arch. Virol. 2012;157:2125–2132. doi: 10.1007/s00705-012-1407-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Liu L., Schwarz L., Ullman K., Ahola H., Qiu Y., Ma Z., Hennig-Pauka I. Identification of a novel bufavirus in domestic pigs by a viral metagenomic approach. J. Gen. Virol. 2016;97:1592–1596. doi: 10.1099/jgv.0.000476. [DOI] [PubMed] [Google Scholar]
- 126.Palinski R., Piñeyro P., Shang P., Yuan F., Guo R., Fang Y., Byers E., Hause B.M. A Novel Porcine Circovirus Distantly Related to Known Circoviruses Is Associated with Porcine Dermatitis and Nephropathy Syndrome and Reproductive Failure. J. Virol. 2017;91:e01879-16. doi: 10.1128/JVI.01879-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Oba M., Katayama Y., Tsuchiaka S., Omatsu T., Murata Y., Ohya K., Makino S., Nagai M., Mizutani T. Discovery of genome of an immunodeficiency-associated virus-like virus from pig feces in Japan. Jpn. J. Vet. Res. 2018;66:53–56. [Google Scholar]
- 128.Schirtzinger E.E., Suddith A.W., Hause B.M., Hesse R.A. First identification of porcine parvovirus 6 in North America by viral metagenomic sequencing of serum from pigs infected with porcine reproductive and respiratory syndrome virus. Virol. J. 2015;12:170. doi: 10.1186/s12985-015-0401-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Palinski R.M., Mitra N., Hause B.M. Discovery of a novel Parvovirinae virus, porcine parvovirus 7, by metagenomic sequencing of porcine rectal swabs. Virus Genes. 2016;52:564–567. doi: 10.1007/s11262-016-1322-1. [DOI] [PubMed] [Google Scholar]
- 130.Arruda B.L., Arruda P.H., Magstadt D.R., Schwartz K.J., Dohlman T., Schleining J.A., Patterson A.R., Visek C.A., Victoria J.G. Identification of a divergent lineage porcine pestivirus in nursing piglets with congenital tremors and reproduction of disease following experimental inoculation. PLoS ONE. 2016;11:e0150104. doi: 10.1371/journal.pone.0150104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Naoi Y., Kishimoto M., Masuda T., Ito M., Tsuchiaka S., Sano K., Yamasato H., Omatsu T., Aoki H., Furuya T., et al. Characterization and phylogenetic analysis of a novel picornavirus from swine feces in Japan. Arch. Virol. 2016;161:1685–1690. doi: 10.1007/s00705-016-2834-7. [DOI] [PubMed] [Google Scholar]
- 132.Hause B.M., Hesse R.A., Anderson G.A. Identification of a novel Picornavirales virus distantly related to posavirus in swine feces. Virus Genes. 2015;51:144–147. doi: 10.1007/s11262-015-1215-8. [DOI] [PubMed] [Google Scholar]
- 133.Cotten M., Koopmans M. Next-generation sequencing and norovirus. Future Virol. 2016;11:719–722. doi: 10.2217/fvl-2016-0099. [DOI] [PubMed] [Google Scholar]
- 134.Gu W., Miller S., Chiu C.Y. Clinical Metagenomic Next-Generation Sequencing for Pathogen Detection. Annu. Rev. Pathol. Mech. Dis. 2019;14:319–338. doi: 10.1146/annurev-pathmechdis-012418-012751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Day M.J., Breitschwerdt E., Cleaveland S., Karkare U., Khanna C., Kirpensteijn J., Kuiken T., Lappin M.R., McQuiston J., Mumford E., et al. Surveillance of zoonotic infectious disease transmitted by small companion animals. Emerg. Infect. Dis. 2012;18:e1. doi: 10.3201/eid1812.120664. [DOI] [Google Scholar]
- 136.Goede D., Morrison R.B. Production impact & time to stability in sow herds infected with porcine epidemic diarrhea virus (PEDV) Prev. Vet. Med. 2016;123:202–207. doi: 10.1016/j.prevetmed.2015.11.010. [DOI] [PubMed] [Google Scholar]
- 137.Gallardo M.C., Reoyo A.D.L.T., Fernández-Pinero J., Iglesias I., Muñoz M.J., Arias M.L. African swine fever: A global view of the current challenge. Porc. Health Manag. 2015;1:21. doi: 10.1186/s40813-015-0013-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.FAO Food and Agricultural Organization of the United Nations Statistical Database. [(accessed on 15 November 2019)]; Available online: http://www.fao.org/faostat/en/#home.
- 139.Ganter M. Zoonotic risks from small ruminants. Vet. Microbiol. 2015;181:53–65. doi: 10.1016/j.vetmic.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 140.Villabruna N., Koopmans M.P.G., de Graaf M. Animals as reservoir for human norovirus. Viruses. 2019;11:478. doi: 10.3390/v11050478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Vlasova A.N., Amimo J.O., Saif L.J. Porcine rotaviruses: Epidemiology, immune responses and control strategies. Viruses. 2017;9:48. doi: 10.3390/v9030048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Simmonds P. Methods for virus classification and the challenge of incorporating metagenomic sequence data. J. Gen. Virol. 2015;96:1193–1206. doi: 10.1099/vir.0.000016. [DOI] [PubMed] [Google Scholar]
- 143.Mande S.S., Mohammed M.H., Ghosh T.S. Classification of metagenomic sequences: Methods and challenges. Brief. Bioinform. 2012;13:669–681. doi: 10.1093/bib/bbs054. [DOI] [PubMed] [Google Scholar]
- 144.Conceição-Neto N., Zeller M., Lefrère H., De Bruyn P., Beller L., Deboutte W., Yinda C.K., Lavigne R., Maes P., Van Ranst M., et al. Modular approach to customise sample preparation procedures for viral metagenomics: A reproducible protocol for virome analysis. Sci. Rep. 2015;5:16532. doi: 10.1038/srep16532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Gardy J.L., Loman N.J. Towards a genomics-informed, real-time, global pathogen surveillance system. Nat. Rev. Genet. 2018;19:9–20. doi: 10.1038/nrg.2017.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Aarestrup F.M., Koopmans M.G. Sharing Data for Global Infectious Disease Surveillance and Outbreak Detection. Trends Microbiol. 2016;24:241–245. doi: 10.1016/j.tim.2016.01.009. [DOI] [PubMed] [Google Scholar]
- 147.Ye S.H., Siddle K.J., Park D.J., Sabeti P.C. Benchmarking Metagenomics Tools for Taxonomic Classification. Cell. 2019;178:779–794. doi: 10.1016/j.cell.2019.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Nooij S., Schmitz D., Vennema H., Kroneman A., Koopmans M.P.G. Overview of virus metagenomic classification methods and their biological applications. Front. Microbiol. 2018;9:749. doi: 10.3389/fmicb.2018.00749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Woolhouse M.E.J., Brierley L., McCaffery C., Lycett S. Assessing the epidemic potential of RNA and DNA viruses. Emerg. Infect. Dis. 2016;22:2037–2044. doi: 10.3201/eid2212.160123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Drosten C., Seilmaier M., Corman V.M., Hartmann W., Scheible G., Sack S., Guggemos W., Kallies R., Muth D., Junglen S., et al. Clinical features and virological analysis of a case of Middle East respiratory syndrome coronavirus infection. Lancet Infect. Dis. 2013;13:745–751. doi: 10.1016/S1473-3099(13)70154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Wilkinson M.D., Dumontier M., Aalbersberg I.J.J., Appleton G., Axton M., Baak A., Blomberg N., Boiten J.W., da Silva Santos L.B., Bourne P.E., et al. Comment: The FAIR Guiding Principles for scientific data management and stewardship. Sci. Data. 2016;3:160018. doi: 10.1038/sdata.2016.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Wielinga P.R., Hendriksen R.S., Aarestrup F.M., Lund O., Smits S.L., Koopmans M.P.G., Schlundt J. Applied Genomics of Foodborne Pathogens. Springer; Berlin, Germany: 2017. Global Microbial Identifier. [Google Scholar]
- 153.Temmam S., Davoust B., Berenger J.M., Raoult D., Desnues C. Viral metagenomics on animals as a tool for the detection of zoonoses prior to human infection? Int. J. Mol. Sci. 2014;15:10377–10397. doi: 10.3390/ijms150610377. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.