Abstract
An array of technology-based interventions has increasingly become available to support family caregivers, primarily focusing on health and well-being, social isolation, financial, and psychological support. More recently the emergence of new technologies such as mobile and cloud, robotics, connected sensors, virtual/augmented/mixed reality, voice, and the evermore ubiquitous tools supported by advanced data analytics, coupled with the integration of multiple technologies through platform solutions, have opened a new era of technology-enabled interventions that can empower and support family caregivers. This paper proposes a conceptual framework for identifying and addressing the challenges that may need to be overcome to effectively apply technology-enabled solutions for family caregivers. The paper identifies a number of challenges that either moderate or mediate the full use of technologies for the benefit of caregivers. The challenges include issues related to equity, inclusion, and access; ethical concerns related to privacy and security; political and regulatory factors affecting interoperability and lack of standards; inclusive/human-centric design and issues; and inherent economic and distribution channel difficulties. The paper concludes with a summary of research questions and issues that form a framework for global research priorities.
Keywords: Family caregiving, Technology-enabled, Innovation, Social isolation
By 2020, approximately 120 million older Americans will need care at home. According to the American Association of Retired Persons (AARP) the majority of caregivers—some 45 million—will be unpaid (compared to 5 million paid caregivers), and many will care for more than one aging family member (Caregivers & Technology, 2016; National Academies of Sciences, Engineering, and Medicine, 2016a). An array of technology-based interventions is now available to support caregivers, delivered through such platforms as mobile and cloud solutions, robotics, connected sensors—commonly referred to as “the Internet of Things” (IoT)—and the evermore ubiquitous tools supported by advanced data analytics (Bock et al., 2016; Demiris & Thompson, 2012; Le, Reeder, Chung, Thompson, & Demiris, 2014; Reeder et al., 2013). Although many of these interventions focus on the health and well-being of caregivers and connect them to sources of support (e.g., Health Vault, Ideal Life; Chi & Demiris, 2015), others aim to reduce the complexity of personal tasks and facilitate access to healthcare providers and other resource. Still another subset is designed to improve the safety, security, and well-being of care recipients (e.g., My Halo, Comfort Zone). The most prevalent technology-enabled interventions are those that expedite access to information and improve communication (e.g., Great Call; Lindeman & Menack, 2015).
Globally, there is an urgent need for enhanced capacity for home care and caregivers of older family members; many believe this need can be addressed, at least in part, through technology (Coughlin, 2006; Orlov, 2017). A recent National Academy of Sciences report suggested that technology might be useful for family caregivers in ways that are typical for the general population as well as some specific functions for the caregiving role (National Academies of Sciences, Engineering, and Medicine, 2016b). In the former category, this might include access to information published on the internet or engagement through social media or social networking sites to connect with others facing similar experiences. In the latter category, caregivers engage in a broad array of activities specific to the older adult care recipient. Such activities include medical and nursing tasks (e.g., medication and pain management, wound care), health monitoring, support for basic and instrumental activities of daily living, provision of emotional support and behavioral guidance, and coordination of care with the health and service sector (Feinberg, 2016). A 2017 report on global innovations for aging identified seven domains of technology-enabled care innovations that might be deployed to enable and empower caregiver in their performance of these activities. These domains include: caregiver platforms; caregiver support; care coordination; telehealth/diagnostics and digital care delivery; alternative therapeutics; transitions of care, housing and operations; and end-of-life planning (A Snapshot of Global Innovation in Aging and Senior Care, 2017).
The emerging literature on technology-enabled caregiving activities provides numerous examples of interventions (Czaja, 2016). One systematic review of telehealth and caregivers (65 papers) identified six categories of technology-delivered interventions: education, consultation, psychosocial/cognitive behavioral therapy (including problem solving training), data collection and monitoring, clinical care delivery, and social support (Chi & Demiris, 2015). These categories represent both the tasks/activities of caregiving and the maintenance and promotion of the wellness of the caregiver. Most of the studies used fairly common technologies like the telephone, video conferencing, web-based information, as well as telemetry/remote monitoring. Another systematic review highlighted health-related technology applications in smart homes to support the needs of older adults and the activities of caregiving. These applications included embedded sensors and monitors; computing and decision-making platforms; communication networks; and sensors and actuators (Majumder et al., 2017). Although these studies provide evidence of the array of potential technology-enabled interventions that are being developed for broad deployment, we lack a systematic review of their efficacy, utility and acceptability.
As society begins to benefit from the next era of technological innovation, it is imperative that we integrate what has been learned about technology solutions and the challenges to implementing them into emerging technology-enabled interventions for caregiving in order to set a course for future development and research (Marr, 2017). This paper addresses the future of technological solutions for family caregivers through a review of emerging technologies and their application to interventions, the identification of challenges to implementing technology-enabled solutions, the presentation of a framework for conceptualizing the moderators and mediators most likely associated with implementation of successful and accessible technology-enabled caregiving interventions, and a brief outline of the high-priority research and development activities that might be undertaken to enable implementation.
Emerging Technologies: Promising Directions for Family Caregivers
Many new technology solutions are emerging that will benefit family caregivers and their family members, including sensors (IoT), voice, assistive technologies, financial/cognitive technologies, and big data, among others. Driving these technologies is the rapidly expanding amount of data now available, increased computing power, and innovations in machine intelligence (artificial intelligence and machine learning). Several innovative technologies that can benefit family caregivers are highlighted below.
Enhanced Internet of Things and Technology Platforms
The introduction of more robust, interactive platforms that analyze data from multiple sources will reduce the complexity of health and social service coordination and care management. Better data will pave the way for greater use of predictive analytics, which in turn will lead to tailored services for caregivers and allow them to make more informed decisions with healthcare providers. For example, emerging platforms will permit the analysis of patterns in patient-generated data extracted from wearables and IoT connected devices, alerting the caregiver to changes in a care recipient’s health status, and automatically providing connection to appropriate resources and to members of the healthcare team (Anderson, 2018).
Voice
As low-cost, commercially available voice-enabled interfaces like Alexa, Google Home, and Siri—all of which are already integrated into our everyday lives—rapidly improve in their ability to understand, interpret, and even anticipate the needs of family caregivers, interventions could become considerably more effective. Often framed as “voice first,” this area includes understanding spoken requests and commands, offering alerts, answering questions, and prompting behavioral activity. These technologies involve the combination of a number of new processing and machine intelligence activities, including artificial intelligence (AI), natural language processing (NLP—the ability for computers to understand hand written and spoken human communication), and speech recognition are driving significant growth in adoption of voice technology across multiple dimensions. Speech recognition alone has been projected to be nearly ubiquitous in the near term, potentially penetrating up to 80% of mobile devices by 2020 (Orlov, 2019).
Remote Monitoring/Telehealth
The ability to manage—from a distance—care recipients’ health and well-being without leaving their homes has significantly reduced the burden on caregivers. Telehealth, coupled with remote monitoring and other technologies (e.g., virtual reality), will become an increasingly ubiquitous tool to help caregivers monitor and manage the health and well-being of care recipients over distance (Schulz et al., 2016). Likewise, no longer dependent on physical proximity to mental health professionals and support groups, caregivers will now be able to readily access the support they need from wherever they are, through such platforms as online forums, video conferencing, store and forward, virtual reality, and chatbots. With improved standards and methods, data collected through remote monitoring will provide a wealth of information for predictive and retrospective analytics, therein improving our ability to dramatically advance services. This will require the development of new measures and scales that can compare and contrast results of interventions for care recipients and caregivers across projects and interventions, paving the way for improved technology for geographically isolated caregivers (Dinesen, 2016; Mortenson et al., 2015). Although telehealth and remote monitoring have been available for several decades, states and insurers are finally changing regulations that will now allow for the expanded use of telehealth.
Mobility/Autonomous Vehicles
Autonomous vehicles, ride sharing, and drones are disrupting the way both caregivers and care recipients have access to the care and resources they need, or conversely, for resources to be more quickly and easily delivered to them, wherever they may be (Spahn, 2019). Technology is now expanding to include on-demand services, utilizing high levels of smartphone and internet support; customizing services for individuals while expanding services to all travelers; and supporting collaborative service models with real-time data capture, clearinghouse automation, and payment reconciliation functionality (Broderick, 2018).
Assistive Technologies
A number of emerging assistive technologies can be expected to have a significant effect on family caregivers (National Academies of Sciences, Engineering, and Medicine, 2019). Technology-enabled interventions that support functional limitations in vision, hearing, and mobility, offer one of the most robust opportunities to support the independence and autonomy care recipients, and subsequently their caregivers. Recent advances in smart phone technology (e.g., Microsoft) now embed significant software advances for persons with disabilities, such as built in screen readers, text capture, speech recognition, screen sizing, notification timing, speech command, seeing AI narration, and other functionalities. Smart glasses have the potential to help people with vision impairments to navigate while walking outdoors. Hearing devices, which are quickly becoming more intelligent and connected, are poised to proliferate through the advent of enhanced, low-cost, over-the-counter hearing solutions that will be permitted through the promulgation of forthcoming FDA guidelines (National Academies of Sciences, Engineering, and Medicine, 2016a).
Virtual/Augmented/Mixed Reality
Virtual reality and augmented reality are increasingly being used as platforms to help family caregivers receive the training necessary to address home emergencies and to perform the medical/nursing tasks that are often a central component of their duties, but for which they are often unprepared (Chambers, Connor, Diver, & McGonigle (2002); Collins, 2018). Virtual reality, augmented technologies, and mixed reality interventions and training platforms will not only enhance care for the care recipient, they will also improve the safety and well-being of the caregiver (e.g., Embodied Labs).
Financial Technologies
New technologies that remotely monitor financial accounts and transactions (e.g., EverSafe) are emerging as effective tools to enhance family caregiver financial transactions while protecting older adults (PCAST, 2016). Changes in financial capacity by older adults, whether it be knowledge, skills, or judgment, can lead to financial fraud or suboptimal decisions across financial tasks such as fee payments or credit card balance transfers, interactions that involve technology or can be identified via technology. Globally, banks and insurance companies are interested in technologies that can allow trusted parties, such as a family caregiver, to monitor financial accounts of older adults to identify impaired financial capacity or exploitation and to support family caregivers in managing financial activities.
Machine Intelligence—Artificial Intelligence and Machine Learning
Family caregivers need access to information, whether it is for healthcare, training, or support. The application of this information and related technology-enabled interventions is dependent upon data and data analytics. Access to information is undergoing transformative change with ever greater amounts of data, increased speed of data transmission, and the advent of innovative methods to analyze information. Due to these changes caregivers will be presented with previously unthought of options and resources to support their family members. Faster data transmission and emerging technology platforms will vastly improve caregivers’ access to information, help caregivers make better use of information, and improve methods for training and communication as is currently being applied in the broader work force (e.g., Care Journey; Nonnecke, Gummi, Crittenden, Lindeman, & Gillette (2018)). Advances in artificial intelligence/machine learning (AI/ML) algorithms, when combined with other innovations such as voice first, NLP, robotics, and ubiquitous sensors, will reshape caregivers’ relationships with their family members and interaction with each other, transforming the way caregivers find, share, and curate information (Chi et al., 2017). The greatest benefits of AI and ML are increased independence and safety for older adults through improved efficiency in care management and care coordination, leading to improved caregiving outcomes. AI and ML will support technology-enabled interventions that can anticipate and adjust to older adults’ abilities or needs in the moment, significantly reducing demands on family caregivers. Ultimately, machine intelligence and predictive analytics will lead to significant benefits for family caregivers, including improved communication with family members and providers, reduced social isolation and depression, and improved caregiver satisfaction (National Academies of Sciences, Engineering, and Medicine, 2019).
Challenges in Applying Technology Solutions
Compounding the rapid emergence of many new technologies are a number of social–cultural, ethical, and technical issues that influence the uptake and scalability of technologies for family caregivers, as presented below.
Equity, Inclusion, Access
It is imperative that older adult and caregiver-specific technologies are examined in relation to socio-cultural values and expectations so that they are not just appealing to a target population but also have the potential to make a difference (Bendere et al., 2014). Thanks to a variety of sociocultural factors and the digital divide, a significant number of older adults—including many family caregivers—do not have access to advanced technology. Only 27% of older adults with household incomes under $30,000 own smartphones, compared with 81% of their more affluent peers (Anderson & Perrin, 2017). Although the use of technology is increasing among older adults and their caregivers globally, the increase varies according to socioeconomic status, the type of technology, and cultural context (WHO, 2013).
There is a significant association between minority race/ethnic status, combined with low socioeconomic status, and a reduced likelihood of internet use for health information seeking among older adults (Yoon, Jang, Vaughan, & Garcia, 2018). Weitzman and colleagues have reported on the need to tailor a Spanish-language educational website intervention for U.S.-born Latino dementia caregivers so that it is culturally “attuned” and uses “plain language” (Weitzman, Neal, Chen, & Levkoff, 2008). Similarly, Chinese American dementia caregivers’ preferences for technology interventions are based on ease of installation and reliability as opposed to specific aspects of the technology design (Xiong, Astell, Mihailidis, & Colantonio, 2018). There are also significant cultural differences across generations which require that caregiver health technology interventions must fundamentally integrate in their design (Fox & Connolly, 2018). Likewise, further attention for technology design for Lesbian, Gay, Bisexual, Transgender, or Queer (LGBTQ) caregivers of older adults needs to be considered, given their historical marginalization in intervention design (Valenti & Katz, 2014).
Regardless of socioeconomic differences in older adults’ access to technology, there is the additional issue of wide variation in technology literacy among caregivers. Studies of both older adults and caregivers designed to better understand what types of technologies they want indicate that the most trustworthy source of technology recommendations is medical professionals, yet medical professionals report they are not up to date on the latest consumer technologies (National Academies of Sciences, Engineering, and Medicine, 2019).
Ethical Concerns/Privacy and Security
Ethical questions pose great challenges to the integration of technology in caregiving (Chung, Demiris & Thompson, 2016; Demiris & Towle, 2009). Who has permission to access health and personal information about an individual? How much information should individuals share with healthcare providers, and is their level of health and technical literacy adequate for consenting to share? Informed consent needs to be an ongoing process, not a single event, but how—and how often—does an individual with cognitive decline give informed consent? Potential conflicts can also arise when privacy preferences differ between a care recipient and the caregiver—for example, if one wants passive monitoring or video monitoring in the home but the other does not, who makes the ultimate decision? Concerns over protection of personal data, even with the increased use of security procedures such as blockchain, will become ever more paramount in an era of big data. In the future additional ethical issues that are difficult to even conceptualize today will most likely emerge—for example, the consequences of a care recipient’s emotional attachment to an AI caregiver.
Interoperability and Lack of Standards
The diversity of technological systems presents challenges. Without common standards, many devices, platforms, and systems remain point solutions lacking interoperability, thus limiting their usefulness (Majumder et al., 2017). Lag time in establishing relevant regulations—mirroring the lag time between innovation and published research—also stymies adoption and challenges business sustainability. Developing common standards and protocols will improve the interoperability of technologies and data sharing, resulting in more efficient and effective support for family caregivers and the conduct of comparative research.
Inclusive/Human-Centric Design
For myriad reasons—from lack of ready-made caregiver test groups and user panels to an underlying ageism that distances developers from their target audience—technology-enabled products are too often created in isolation from those who will use them. One major challenge ahead will be designing systems that focus on usability. Without the participation of caregivers and care recipients in the design process, many technologies either fail to serve the needs of their intended users, or they fail to be adopted. The limited knowledge of behavioral psychology related to caregivers’ perception and use of technology also hinders the development of effective interventions; understanding user experience and how individuals relate to technology remains crucial. Equally important is a greater appreciation of the influence of messaging on caregivers’ likelihood to adopt a new tool: why do some messages empower caregivers to grow comfortable with technology while others deter use. The application of universal design principals as promulgated in the development of assistive technologies supports broader accessibility of technology-enabled interventions to all family caregivers (National Academies of Sciences, Engineering, and Medicine, 2019).
Theoretical Framework for Assessing Technology-Enabled Solutions for Family Caregivers
There is ample opportunity for exploration and development of technologically enhanced solutions for family caregivers; however, we must have a conceptual framework that enables examination of the factors associated with the adoption of technologically enhanced solutions that yield positive care-recipient and caregiver outcomes. Environmental gerontology, which seeks to explain the interdependence of the person, their actions, and the role of the environment (physical, social, and ecological), offers a basis for such a framework (van Hoof et al., 2011; Lawton, Windley, & Byerts, 1982; Wahl & Weisman, 2003). Seminal scholarship in environmental gerontology differentiated three functions of the environment for older people: maintenance of consistency and familiarity, stimulation and the effects of departures from that consistency on behavior, and support as the potential to compensate for reduced or lost capability (Lawton et al., 1982). Building on this foundation of environmental gerontology, Carnemolla proposed the Human/Activity/Space/Technology (HAST) model as a way of analyzing these interdependencies and incorporating technology for aging in place (Carnemolla, 2018).
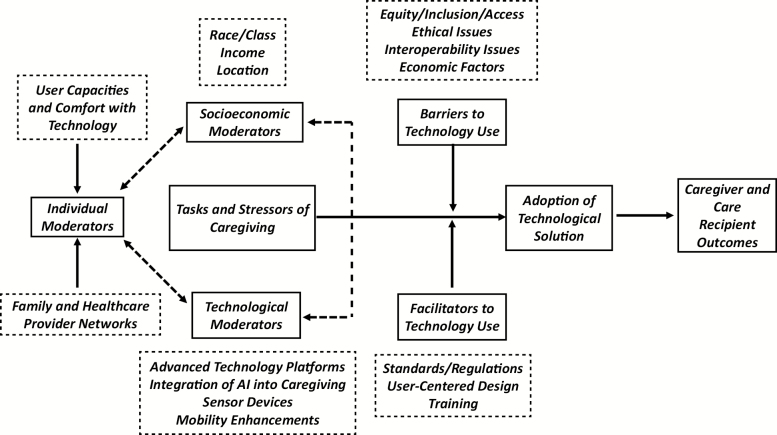
Focusing more on the factors that might contribute to adoption of technological solutions to caregiving challenges that might affect more distal outcomes of caregiver and care-recipient well-being, we are proposing a model of technology-enabled caregiving in the home (TECH). The model, represented in Figure 1, sorts the challenges identified above as either moderators or mediators of an adoption process that can affect outcomes for caregivers and care recipients. The figure is meant to provide a map for thinking about actions that might promote adoption of technology-enhanced caregiving solutions. It indicates, for example, that some kinds of moderators—like those having to do with user capacity or networks of care and support—may be susceptible to direct intervention. Programs of training can be provided to caregivers; healthcare system design can integrate the provision of remote consultation to distant care recipients and caregivers. Some moderators may be less (or not at all) amenable to alteration (e.g., social class or location) but appreciation for them could be incorporated into actions focused on other moderators (e.g., the design of advanced technology platforms or integration of AI into caregiving) in ways that acknowledge and provide work-arounds for the immutable moderators. The mediators in the framework, the barriers and facilitators to technology use, provide a focus on the ways in which intentionality in the design of technology and the crafting of policy can promote use and reduce or remove roadblocks to use. Incentivizing internet providers to extend access to rural areas, requiring interoperability as a condition for licensed use, ensuring the readability of operating instructions and providing readily accessible on-line training for the use of technological enhancements, or building data privacy conditions into on-going HIPAA training for clinicians are all ways in which the broader context of technology could be manipulated to promote access to caregiving-enhancement technologies.
Figure 1.
Technology-enabled caregiving in the home (TECH).
Priority Areas for Caregiver Technology Research and Development
Drawing from the range of technologies that are quickly becoming accessible to family caregivers and older adults and the array of challenges/issues that must be considered as we move into an era of ever more technology-driven caregiver support, the authors offer a research agenda to address caregiver technologies. The foundation for this agenda is the outcomes of the Research Priorities in Caregiving Summit: Advancing Family-Centered Care across the Trajectory of Illness. Held in March 2018, 50 thought leaders in family caregiving from across the country took part in a series of small- and large-group discussions to identify and prioritize caregiving research priorities, with a focus on issues related to technology, trajectory of illness, heterogeneity, and multicultural caregiving. The process and results of this summit are described in Harvath et al. (2020).
Grounded in the TECH framework we propose, the agenda poses a series of particular questions about caregiver needs and use (related to technology), strategies for strengthening the moderators and mediators of technology adoption, and methods for assessing the outcomes and effectiveness of technological solutions. Beyond these specific questions is the need to better understand the underlying mechanism of technology adoption and the broader to test and strengthen the TECH framework itself.
Thus, we propose a set of key research topics related to technology-enabled interventions with family caregivers for consideration by the international research community, according to the TECH framework (see Table 1). We believe these topics will reveal relevant, timely, and important knowledge to move this field forward.
Table 1.
Proposed Key Research Topics
| TECH component | Research topics |
|---|---|
| Moderators | |
| Individual moderators | • How can caregivers who perform complex medical and nursing tasks in the home have access to the necessary technologies and capacity (time, ability, training, and support) to successfully accomplish these tasks? • As machine learning methods and artificial intelligence technologies for caregivers emerge, what insights might emerge from these new data when combined with clinical and operational healthcare data that could inform precision medicine, predictions of outcomes, and personalized interventions? • What technologies, integrated with electronic health record and personal health record systems, are necessary and sufficient to accomplish shared decision making? |
| Socioeconomic moderators | • How does the digital divide affect caregivers of minority groups and underserved communities, and how can we design and disseminate technologies for equitable access? • How do technology tools like ride-sharing applications, smartphone and peer-to-peer payment systems, meal-prep, and grocery delivery services affect instrumental activities of daily living, and particularly the resource utilization of caregivers who are balancing cost and efficiency? |
| Technological moderators | • How can current models for technology adoption that take into account usefulness (for accomplishing the health/caregiving objective), usability (ease of use, intuitiveness), and the social and physical environment to map TECH and environmental gerontology theories and to generate testable models and measures for caregiver technology acceptance and use? • How might we utilize existing and commonly available collaboration technologies such as shared project coordination and document management systems, audio/video conferencing, instant messaging, to support intensive care coordination needs. • How might technology streamline the gathering of data, facilitate exchange of information among stakeholders, provide documentation of values and preferences, disseminate decisions that have been made to relevant stakeholders, and enable ongoing monitoring and evaluation of care plans? • What analytic methods and algorithms need to be developed to assure rigorously evaluated and trustworthy results to be built into interventions? |
| Mediators | |
| Barriers | • What specific concerns do caregivers have about data privacy and physical security of devices, beyond those of the general public and patients, and how can we design technology and policy infrastructure to assure privacy and security? |
| Facilitators | • What strategies should be employed to enable seamless interoperability and data sharing among diverse caregiver technologies? • How can human-centered design methods that seek to fully understand users’ needs and engage them in designing solutions be adapted and applied to generate innovative caregiver technologies and relevant interventions and guide the implementation of interventions that utilize these tools? • How can we assure communication networks are optimized such that caregiver technologies, as well as telemedicine and communication technologies, do not experience unacceptable performance and latency? |
| Measurement issues linked to technology | |
| Measurement issues | • What measures are relevant for evaluating caregiving outcomes linked to technology-enhanced caregiving?• How might we assess cost-effectiveness of technology-enabled caregiving interventions? |
Conclusion
The pace of innovation in technology is accelerating, and within a decade previously unimagined technologies will shape much of our experiences of living, aging, and caregiving (Orlov, 2017). Throughout history, technological advances have had unintended consequences on society. Automobiles improved access to jobs, healthcare, and services, yet the accompanying pollution has had a negative environmental impact. The internet has democratized access to information, but largely unchecked, social media and online programs can sometimes harm individuals, including family caregivers. Ultimately, researchers will need to balance the benefits and promises of new technologies with their unintended consequences and risks. How researchers keep pace with the speed of technology will be the one constant challenge in ensuring that research remains relevant to practice. However, in the long term, it is the very nature of technology’s rapid evolution that will increasingly make technology a crucial element in improving support for and the well-being of family caregivers.
Funding
This work was supported by a grant from the Gordon and Betty Moore Foundation (Grant Agreement #5968). This paper was published as part of a supplement sponsored and funded by the Gordon and Betty Moore Foundation.
Acknowledgment
The authors would like to acknowledge the funding from the Gordon and Betty Moore Foundation which established the Family Caregiving Institute at the Betty Irene Moore School of Nursing at University of California-Davis. The authors wish to acknowledge the contribution of Dr. Kenneth Hepburn in the design of the TECH conceptual framework and the assistance of Kristen Bettega and Liona Li in the technical editing of this manuscript.
Conflict of Interest
None reported.
References
- A snapshot of global innovation in aging and senior care (Rep.). (2017). Retrieved February 12, 2018, from Aging2.0 https://www.aging2.com/blog/report-a-snapshot-of-global-innovation-in-aging-and-senior-care/.
- Altman D., & Frist W. H (2015). Medicare and medicaid at 50 years: Perspectives of beneficiaries, health care professionals and institutions, and policy makers. Journal of the American Medical Association, 314, 384–395. doi:10.1001/jama.2015.7811 [DOI] [PubMed] [Google Scholar]
- Anderson N. (2018, February 4). Phone interview with D. Lindeman. [Google Scholar]
- Anderson M., & Perrin A (2017). Tech adoption climbs among older adults. Pew Research Center, 1–22. Retrieved March 3, 2018, from https://www.pewinternet.org/2017/05/17/tech-adoption-climbs-among-older-adults/ [Google Scholar]
- Bender M. S., Choi J., Arai S., Paul S. M., Gonzalez P., & Fukuoka Y (2014). Digital technology ownership, usage, and factors predicting downloading health apps among Caucasian, Filipino, Korean, and Latino Americans: The digital link to health survey. JMIR mHealth and uHealth, 2, e43. doi: 10.2196/mhealth.3710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bock C., Demiris G., Choi Y., Le T., Thompson H. J., Samuel A., & Huang D (2016). Engaging older adults in the visualization of sensor data facilitated by an open platform for connected devices. Technology and Health Care, 24, 541–50. doi:10.3233/THC-161150 [DOI] [PubMed] [Google Scholar]
- Broderick A. (2018). The future of mobility for older adults in rural areas. The future of mobility for older adults in rural areas. CITRIS and the Banatao Institute, UC Berkeley. Retrieved from ; http://www.advancingstates.org/sites/nasuad/files/180424_CITRIS_rural_mobility_paper_F.pdf [Google Scholar]
- Caregivers & Technology (Rep.). (2016, April). Retrieved February 12, 2018 from https://www.aarp.org/research/topics/care/info-2018/designing-technology-caregivers.html
- Carnemolla P. (2018). Ageing in place and the internet of things—How smart home technologies, the built environment and caregiving intersect. Visualization in Engineering, 6, 7. doi: 10.1186/s40327-018-0066-5 [Google Scholar]
- Chambers M., Connor S., Diver M., & McGonigle M (2002). Usability of multimedia technology to help caregivers prepare for a crisis. Telemedicine Journal & E-Health, 8, 343–347. doi: 10.1089/15305620260353234 [DOI] [PubMed] [Google Scholar]
- Chi N.-C., & Demiris G (2015). A systematic review of telehealth tools and interventions to support family caregivers. Journal of Telemedicine and Telecare, 21, 37–44. doi: 10.1177/1357633x14562734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi N.-C., Sparks O., Lin S. Y., Lazar A., Thompson H. J., & Demiris G (2017). Pilot testing a digital pet avatar for older adults. Geriatric Nursing, 38, 542–547. doi: 10.1016/j.gerinurse.2017.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung J., Demiris G., & Thompson H. J (2016). Ethical considerations regarding the use of smart home technologies for older adults: An integrative review. Annual Review of Nursing Research, 34, 155–181. doi: 10.1891/0739-6686.34.155 [DOI] [PubMed] [Google Scholar]
- Collins S. (2018, February 2). Phone interview with C. Gladstone and D. Lindeman. [Google Scholar]
- Coughlin J. & Lau X (2006). Cathedral builders wanted: Constructing a new vision of technology for old age. Public Policy and Aging Report, 16, 4–8. doi: 10.1093/ppar/16.1.4 [Google Scholar]
- Czaja S.J. (2018, March). Phone interview with C. Gladstone. [Google Scholar]
- Czaja S. J., Perdomo D., & Lee C. C (2016). The role of technology in supporting family caregivers. In Human aspects of IT for the aged population: Design for aging—2nd international conference, ITAP 2016 and held as part of HCI International 2016, Proceedings (Vol. 9754, pp. 178–185). [Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics) Vol. 9754)]. Springer Verlag. doi: 10.1007/978-3-319-39943-0_17 [Google Scholar]
- Demiris G. (2018, February 7). Phone interview with C. Gladstone and D. Lindeman. [Google Scholar]
- Demiris G., Doorenbos A. Z., & Towle C (2009). Ethical considerations regarding the use of technology for older adults. Research in Gerontological Nursing, 2, 128–136. doi: 10.3928/19404921-20090401-02 [DOI] [PubMed] [Google Scholar]
- Demiris G., & Thompson H. J (2012). Mobilizing older adults: Harnessing the potential of smart home technologies. Contribution of the IMIA working group on smart homes and ambient assisted living. Yearbook of Medical Informatics, 7:94–99. doi: 10.1055/s-0038-1639437. [PubMed] [Google Scholar]
- Dinesen B., et al. (2016). Personalized telehealth in the future: A global research Agenda. Journal Medical Internet Research, 18, e53. doi: 10.2196/jmir.5257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang M. L., Canham S. L., Battersby L., Sixsmith J., Wada M., & Sixsmith A (2018). Exploring privilege in the digital divide: Implications for theory, policy, and practice. Gerontologist, 59, e1–e15. doi: 10.1093/geront/gny037 [DOI] [PubMed] [Google Scholar]
- Feinberg L. F. (2016). The dual pressures of family caregiving and employment. Washington, DC: AARP Public Policy Institute.https://www.aarp.org/content/dam/aarp/ppi/2016-03/The-Dual-Pressures-off-Family-Caregiving-and-Employment.pdf. [Google Scholar]
- Feinberg L.F. (2018, February 1). Phone interview with C. Gladstone. [Google Scholar]
- Fox G., & Connolly R (2018). Mobile health technology adoption across generations: Narrowing the digital divide. Information Systems Journal, 28, 995–1019. doi: 10.1111/isj.12179. [Google Scholar]
- Gillette D. (2019, February 18). Phone interview with D. Lindeman. [Google Scholar]
- Harvath T.A., Mongoven J. M., Bidwell J. T., Cothran F. A., Sexson K. E., Mason D. J. & Buckwalter K (2020). Research priorities in family caregiving: Process and outcomes of a conference on family-centered care across the trajectory of serious illness. Gerontologist, 60(S1), S5–S13. doi: 10.1093/geront/gnz138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtzman J. (2018, February 8). Phone interview with C. Gladstone and D. Lindeman. [Google Scholar]
- van Hoof J., Kort H. S. M., Rutten P. G. S., & Duijnstee M. S. H (2011). Ageing-in-place with the use of ambient intelligence technology: Perspectives of older users. International Journal of Medical Informatics, 80, 310–331. doi: 10.1016/j.ijmedinf.2011.02.010 [DOI] [PubMed] [Google Scholar]
- Johnston S. (2018, January 1). Phone interview with C. Gladstone and D. Lindeman. [Google Scholar]
- Kontos E., Blake K. D., Chou W. Y. S., & Prestin A (2014). Predictors of eHealth usage: Insights on the digital divide from the health information national trends survey 2012. Journal of Medical Internet Research, 16, e172. doi: 10.2196/jmir.3117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar D., Hemmige V., Kallen M. A., Giordano T. P., & Arya M (2019). Mobile phones may not bridge the digital divide: A look at mobile phone literacy in an underserved patient population. Cureus, 11, e4104. doi: 10.7759/cureus.4104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latulippe K., Hamel C., & Giroux D (2017). Social health inequalities and eHealth: A literature review with qualitative synthesis of theoretical and empirical studies. Journal of Medical Internet Research, 19, e136. doi: 10.2196/jmir.6731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton M. P., Windley P. G., & Byerts T. O (1982). Aging and the environment: Theoretical approaches (No. 7). New York, NY: Springer Publications Company; ISBN: 9780826137609 [Google Scholar]
- Le T., Reeder B., Chung J., Thompson H., & Demiris G (2014). Design of smart home sensor visualizations for older adults. Technology and Health Care, 22, 657–66. doi: 10.3233/THC-140839 [DOI] [PubMed] [Google Scholar]
- Lindeman D., & Menack J (2015). Technologies that support aging in place. In Kress Cathy. (Ed.), Handbook of geriatric care management (4th ed.). Burlington, MA: Jones & Bartlett Learning. [Google Scholar]
- Majumder S., Aghayi E., Noferesti M., Memarzadeh-Tehran H., Mondal T., Pang Z., & Deen M (2017). Smart homes for elderly healthcare—Recent advances and research challenges. Sensors, 17, 2496. doi: 10.3390/s17112496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marr B. (2017, November 29). This is why blockchains will transform healthcare. Forbes.com.Retrieved March 1, 2018 from https://www.forbes.com/sites/bernardmarr/2017/11/29/this-is-why-blockchains-will-transform-healthcare/#59c272121ebe. [Google Scholar]
- Mortenson W., Demers L., Fuhrer M., Jutai J., Lenker J., & Deruyter F (2015). Development and preliminary evaluation of the caregiver assistive technology outcome measure. Journal of Rehabilitation Medicine, 47, 412–418. doi:10.2340/16501977-1952. [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2016a). Families caring for an aging America. National Academies Press; Retrieved from http://www.nationalacademies.org/hmd/Reports/2016/families-caring-for-an-aging-america.aspx [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2016b). Hearing health care for adults: Priorities for improving access and affordability Retrieved from http://nationalacademies.org/hmd/~/media/Files/Report%20Files/2016/Hearing/Hearing-Recs.pdf
- National Academies of Sciences, Engineering, and Medicine. (2019). Artificial intelligence applications for older adults and people with disabilities: Balancing safety and autonomy: Proceedings of a workshop—in brief. Washington, DC: The National Academies Press. doi: 10.17226/25427. [PubMed] [Google Scholar]
- National Alliance for Caregiving. (2009, December). Caregiving in the U.S. Washington, DC: AARP Research. doi: 10.26419/res.00062.001 [Google Scholar]
- National Alliance for Caregiving. (2015). Executive summary: Caregiving in the U.S. NAC and the AARP Public Policy Institute. Washington, DC: Greenwald & Associates. Retrieved from https://www.caregiving.org/wp-content/uploads/2015/05/2015_CaregivingintheUS_Executive-Summary-June-4_WEB.pdf [Google Scholar]
- Nonnecke B., Gummi M., Crittenden C., Lindeman D., Gillette D (2018). Putting AI to work: Technology and policy for enabling the workforce of the future.https://citrispolicylab.org/wp-content/uploads/2018/11/Putting-AI-To-Work_CITRIS_Sept-2018.pdf
- Orlov L. (2017). Tech-enabled home care: Rising worker scarcity, family expectations. Retrieved March 4, 2018, from Aging In Place Technology Watch: https://www.ageinplacetech.com/page/tech-enabled-home-care-rising-worker-scarcity-family-expectations
- Orlov L. (2019). Aging in place technology watch. Retrieved July 25, 2019, from https://www.ageinplacetech.com/blog/voice-health-and-well-being-launching-new-report-2020.
- President’s Council of Advisors in Science and Technology (PCAST). (2016). Independence, technology, and connection in older age.https://www.whitehouse.gov/blog/2016/03/15/supporting-active-and-connected-lives-more-americans-live-longer
- Reeder B., Meyer E., Lazar A., Chaudhuri S., Thompson H. J., & Demiris G (2013). Framing the evidence for health smart homes and home-based consumer health technologies as a public health intervention for independent aging: A systematic review. International Journal of Medical Informatics, 82, 565–579. doi:10.1016/j.ijmedinf.2013.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlesinger A., Edwards W. K., & Grinter R. E. (2017, May). Intersectional HCI: Engaging identity through gender, race, and class. In Proceedings of the 2017 CHI conference on human factors in computing systems (pp. 5412–5427). New York, NY: ACM. doi:10.1145/3025453.3025766 [Google Scholar]
- Schulz R., Beach S. R., Matthews J. T., Courtney K., De Vito Dabbs A., & Mecca L. P (2016). Caregivers’ willingness to pay for technologies to support caregiving. Gerontologist, 56, 817–829. doi:10.1093/geront/gnv033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spahn P. (2019). Older people need rides.https://www.nytimes.com/2019/08/16/health/uber-lyft-elderly.html
- Stephen R. (2018, January 2). Phone interview with C. Gladstone. [Google Scholar]
- Valenti K., & Katz A (2014). Needs and perceptions of LGBTQ caregivers: The challenges of services and support. Journal of Gay & Lesbian Social Services, 26, 70–90. doi: 10.1080/10538720.2013.865575 [Google Scholar]
- Wahl H. W., & Weisman G. D (2003). Environmental gerontology at the beginning of the new millennium: Reflections on its historical, empirical, and theoretical development. Gerontologist, 43, 616–627. doi: 10.1093/geront/43.5.616 [DOI] [PubMed] [Google Scholar]
- Weitzman P., Neal L., Chen H., & Levkoff S. E (2008). Designing a culturally attuned bilingual educational website for US Latino dementia caregivers. Ageing International, 32, 15–24. doi: 10.1007/s12126-008-9000-9 [Google Scholar]
- WHO. (2013). Summary report of the consultation on advancing technological innovation for older persons in Asia. 20–21 February 2013, Kobe, Japan. Retrieved July 28, 2019 https://extranet.who.int/kobe_centre/en/publications-details/238
- Xiong C., Astell A., Mihailidis A., & Colantonio A (2018). Needs and preferences for technology among Chinese family caregivers of persons with dementia: A pilot study. Journal of Rehabilitation and Assistive Technologies Engineering, 5. doi: 10.1177/2055668318775315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon H., Jang Y., Vaughan P. W., & Garcia M (2018). Older adults’ Internet use for health information: Digital divide by race/ethnicity and socioeconomic status. Journal of Applied Gerontology. Advance online publication. doi: 10.1177/0733464818770772 [DOI] [PubMed] [Google Scholar]