Abstract
Teen pregnancy and childbearing have declined over the past two decades to historic lows. The most recent declines have occurred during a time of coordinated national efforts focused on teen pregnancy. This article highlights a federal partnership to reduce teen pregnancy through the implementation of innovative, evidence-based approaches in affected communities, with a focus on reaching African-American and Latino/Hispanic youth. This initiative has the potential to transform the design and implementation of future teen pregnancy prevention efforts and provide a model that can be replicated in communities across the nation.
Keywords: Adolescent pregnancy, Unintended pregnancy, Sexual behavior, Primary prevention
There is a cause for celebration as teen pregnancy [1] and childbearing [2] in the United States have continued their declines over the past two decades to historic lows—57.4 pregnancies and 24.2 births per 1,000 female teens aged 15–19 years. This marked decline has resulted from the combined effect of more teens delaying sexual activity and for those who are sexually active, more using contraception, [3,4] especially methods that are highly effective [5]. The most recent declines have occurred during a remarkable time of coordinated national efforts focused on teen pregnancy, highlighted by the establishment of the federal Teen Pregnancy Prevention Program [6] introduced by President Obama in the appropriations bill for fiscal year 2010. This initiative represents the largest federal program ever directed at the behavioral, social, and public health issues associated with teen pregnancy prevention, and is the first to focus solely on interventions with evidence of effectiveness and testing new approaches and strategies, and has led to the establishment of the Office of Adolescent Health (OAH) [6]. As part of this new program, OAH partnered with CDC’s Division of Reproductive Health to test a set of innovative community-wide approaches to reduce teen pregnancies and births by involving more teens in evidence-based programs and improving linkages between prevention programs and clinical services.
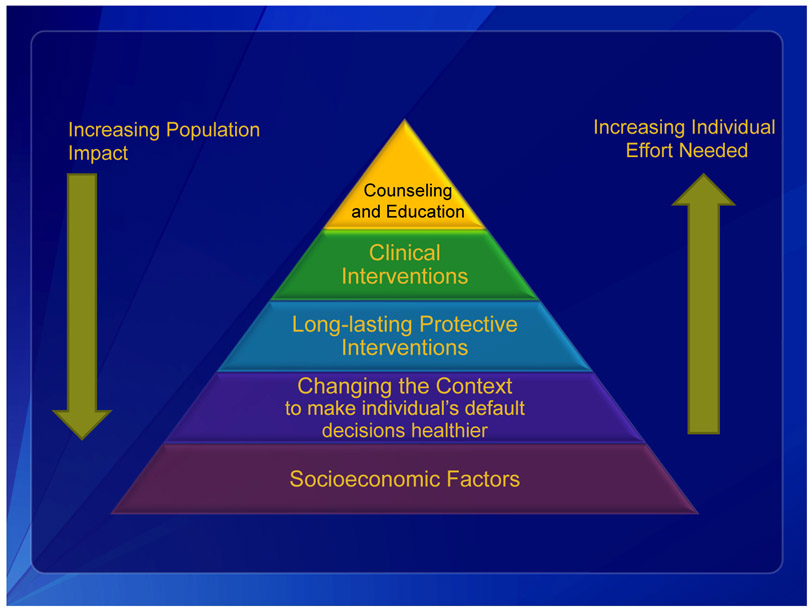
Aligning with federal efforts of the Teen Pregnancy Prevention Program, CDC also identified teen pregnancy as one of the agency’s six “Winnable Battles” for improving our nation’s health, i.e., a public health priority associated with known, effective strategies that have sufficient potential to make a large-scale impact on health [7]. A health impact pyramid adapted from the work of former CDC Director, Dr. Thomas Frieden, [8] (Figure 1) has served as the framework and foundation for the agency’s approach to addressing teen pregnancy by outlining changes needed in policy, program, clinical, and public health practices at the national, state, and community levels. The top tier of the pyramid, counseling and educational interventions, supports the use of evidence-based, medically accurate, and culturally and age-appropriate sexual health education (Figure 2). Such focused interventions are likely to be effective at changing individual behavior yet may not reach the entire population of teens at risk for pregnancy. The next level, strengthening clinical interventions, focuses on removing medical barriers to contraceptive use for teens and promoting the delivery of quality family planning services for all women, including adolescents. For example, evidence-based clinical guidance issued by CDC [9] affirms that the full range of contraceptive methods may be safely used by women of any reproductive age, including adolescents. Other guidance aims to reduce clinical barriers to providing contraceptive methods to clients [10] and improve the clinic environment for clients seeking contraceptive services, particularly adolescents [11]. In addition, provisions of the Affordable Care Act [12] remove cost barriers for women, including adolescents, by stipulating that 18 Food and Drug Administration–approved contraceptive methods must be covered with no copays, cost sharing, or deductibles. The third level, promoting long-lasting preventive interventions, aims to shift the use of contraception toward more effective methods by offering sexually active teens, including those who are already parents, the full range of Food and Drug Administration–approved methods, including long-acting reversible contraception (LARC), specifically intrauterine devices and contraceptive implants. LARC is safe and appropriate for teens, and major professional societies, including the American College of Obstetricians and Gynecologists and the American Academy of Pediatrics, [13,14] have endorsed LARC as a first-line contraceptive choice for teens. The fourth level involves changing the context to encourage healthy decisions, by promoting positive parent-child communication and addressing social norms toward teen sexual behavior and policies that promote access to effective contraception. The base level of the pyramid represents the need to address socioeconomic factors that contribute to teen pregnancy by promoting family and community engagement, educational achievement, and positive youth development. Compared with other teens, teen parents—particularly younger teen parents— [15,16] are far less likely to complete high school and obtain employment. Although all levels of the pyramid offer opportunities for impact, the interventions with the greatest potential to affect population-level health (i.e., reduction in teen pregnancy and birth) tend to be the most complex and are found at the base.
Figure 1.
The Health Impact Pyramid. Thomas R. Frieden. A Framework for Public Health Action: The Health Impact Pyramid. American Journal of Public Health: April 2010, Vol. 100, No. 4, pp. 590-595. 10.2105/AJPH.2009.185652.
Figure 2.
The Health Impact Pyramid as adapted to teen pregnancy prevention. Adapted from Thomas R. Frieden. A Framework for Public Health Action: The Health Impact Pyramid. American Journal of Public Health: April 2010, Vol. 100, No. 4, pp. 590-595. 10.2105/AJPH.2009.185652. LARC = long-acting reversible contraception; PYD = positive youth development.
The Teen Pregnancy Prevention Program (TPP) supports public and private entities to replicate evidence-based teen pregnancy prevention programs that have been proven effective through rigorous evaluation and to implement and evaluate innovative program models to reduce teen pregnancy [17]. The partnership between OAH and CDC evaluating community-wide approaches to teen pregnancy prevention (http://www.cdc.gov/TeenPregnancy/PreventTeenPreg.htm.) provides an opportunity to develop and test innovative models. Through this collaboration, five years of funding of up to $10 million annually was provided by OAH through the TPP program to support demonstration projects conducted by local health departments, community-based organizations, and state teen pregnancy prevention programs. These projects tested innovative, sustainable, and multicomponent initiatives in 10 communities that were most affected by teen pregnancy, with national partners funded by CDC providing tailored training and technical assistance for these projects.
Results of this partnership are highlighted in this special issue of the Journal of Adolescent Health, where we describe the implementation of these initiatives to reduce teen pregnancy and births, with a focus on reaching African-American and Latino/Hispanic youth aged 15–19 years. In collaboration with public and private partners who provide direct services and support to youth (e.g., health centers, schools, faith-based organizations, and youth-serving organizations), various articles describe the expertise and tools that communities need to prevent teen pregnancy and promote adolescent health. If proven effective, this effort has the potential to transform the design and implementation of teen pregnancy prevention efforts in the future and provide a model that can be replicated in communities across the nation.
In this issue, an overview of the community-wide initiative [18] is provided and lessons learned and how this approach advances the field of teen pregnancy prevention. This body of work includes the important role that capacity building plays in the successful implementation of evidenced-based interventions for youth at increased risk for teen pregnancy [19]. Efforts to improve the ability of health centers to implement evidence-based clinical practices and reproductive health services in a youth-friendly manner are described, [20] as are methods for monitoring implementation progress and rigorously evaluating the effectiveness of the community-wide initiatives [21]. In addition, grantees from five communities [22–26] describe their experiences on the frontline to help prevent teen pregnancy. These articles describe strategies used to successfully determine community readiness to implement community-wide initiatives [22], seek information from African-American and Latino youth on their reproductive health needs [23], educate stakeholders and mobilize the community in support of sexual health education [24], and link youth to reproductive health services [25,26].
In summary, the steps for reducing teen pregnancy implemented in the community-wide initiative build on the existing strengths of CDC, the OAH, and other federal partners and are designed in such a way to maximize nationwide impact. The lessons learned from these initiatives will enable communities to be better prepared to meet the needs of teens and have already served as a springboard to inform the Teen Pregnancy Prevention Replication efforts by OAH in its most recent announcement of new grants for fiscal years 2015–2019 [27]. We believe that these efforts will help further delay initiation of sexual intercourse, increase the availability and accessibility of effective methods of contraception, including LARC, to teens contemplating sexual activity, and ultimately contribute to reduced rates of teen pregnancy.
Footnotes
Conflicts of Interest: The authors declare no conflicts of interest to disclose.
Disclaimer: Publication of this article was supported by the Office of Adolescent Health. The opinions or views expressed in this supplement are those of the authors and do not necessarily represent the official position of the funder.
References
- [1].Kost K, Henshaw S. U.S. Teenage pregnancies, births and Abortions, 2010: National and state Trends by age, Race and Ethnicity. New York: Guttmacher Institute; 2014. Available at: http://www.guttmacher.org/pubs/USTPtrends10.pdf. Accessed July 27, 2015. [Google Scholar]
- [2].Hamilton BE, Martin JA, Osterman M, Curtin SC. Births: Preliminary data for 2014 National vital statistics reports. Hyattsville, MD: National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- [3].Tyler CP, Warner L, Kraft JM, et al. Sexual experience and contraceptive use among female teens-United States, 1995, 2002, and 2006-2010. MMWR Morb Mortal Wkly Rep 2012;61:297. [PubMed] [Google Scholar]
- [4].Santelli JS, Lindberg LD, Finer LB, Singh S. Explaining recent declines in adolescent pregnancy in the United States: The contribution of abstinence and improved contraceptive use. Am J Public Health 2007;97:150–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Romero LM, Pazol K, Warner L, et al. “Vital signs: Trends in use of long-acting reversible contraception among teens aged 15-19 years seeking contraceptive services–United States, 2005-2013”. MMWR Morb Mortal Wkly Rep 2015;64:363–9. [PMC free article] [PubMed] [Google Scholar]
- [6].Kappeler EM, Farb AF. Historical context for the creation of the Office of Adolescent Health and the teen pregnancy prevention program. J Adolesc Health 2014;54:S3–9. [DOI] [PubMed] [Google Scholar]
- [7].Centers for Disease Control and Prevention. Winnable Battles fact sheet. 2012. Available at: http://www.cdc.gov/winnablebattles/pdf/wb_fact_sheet_aug2012.pdf. Accessed January 26, 2017.
- [8].Frieden T A framework for public health action: The health impact pyramid. Am J Public Health 2010;100:590–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Centers for Disease Control and Prevention. U.S. medical eligibility criteria for contraceptive use 2010. MMWR Morb Mortal Wkly Rep 2010; 59(No. RR-4):1–86. [PubMed] [Google Scholar]
- [10].Centers for Disease Control and Prevention (CDC). “US selected practice recommendations for contraceptive use, 2013”. MMWR Recomm Rep 2013;62:1–64. [PubMed] [Google Scholar]
- [11].Gavin L, Moskosky S, Carter M, et al. Providing quality family planning services. MMWR Morb Mortal Wkly Rep 2014;63:1–54.24402465 [Google Scholar]
- [12].Coverage of Certain preventive services under the Affordable Care Act. Final Rules, 45 C.F.R. Parts 147 and 156. 2010. Available at: http://www.gpo.gov/fdsys/pkg/FR-2013-07-02/pdf/2013-15866.pdf. Accessed January 26, 2017.
- [13].American College of Obstetricians and Gynecologists. Adolescents and long-acting reversible contraception: Implants and intrauterine devices. Committee opinion no. 539. Obstet Gynecol 2012;120:983–8. [DOI] [PubMed] [Google Scholar]
- [14].American Academy of Pediatrics; Committee on Adolescence; Contraception for adolescents. Pediatrics 2014;134:e1244–56.25266430 [Google Scholar]
- [15].Perper K, Peterson K, Manlove J. Diploma attainment among teen mothers Fact sheet. Washington, DC: Child Trends; 2010. Available at: http://childtrends.org/?publications=diploma-attainment-among-teen-mothers. Accessed January 26, 2017. [Google Scholar]
- [16].Cox S, Pazol K, Warner L, et al. Vital signs: Births to teens aged 15–17 Years—United States, 1991–2012. MMWR Morb Mortal Wkly Rep 2014; 63:312–8. [PMC free article] [PubMed] [Google Scholar]
- [17].Farb AF, Margolis AL, Rice TM, Jensen JAG. Implementing evidence-based teen pregnancy prevention programs: Legislation to practice. J Adol Health 2014;54(3 Suppl.):S1–96. [Google Scholar]
- [18].Mueller T, Tevendale HD, Fuller TR, et al. Teen pregnancy prevention: Implementation of a multicomponent, community-wide approach. J Adolesc Health 2017;60:S9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].House LD, Tevendale HD, Martinez-Garcia G. Implementing evidence-based teen pregnancy-prevention interventions in a community-wide initiative: building capacity and reaching youth. J Adolesc Health 2017; 60:S18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Romero LM, Olaiya O, Hallum-Montes R, et al. Efforts to increase implementation of evidence-based clinical practices to improve adolescent-friendly reproductive health services. J Adolesc Health 2017;60:S30–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Tevendale HD, Condron DS, Garraza LG, et al. Practical approaches to evaluating progress and outcomes in community-wide teen pregnancy prevention initiatives. J Adolesc Health 2017;60:S63–8. [DOI] [PubMed] [Google Scholar]
- [22].Bhuiya N, House LD, Desmarais J, et al. Strategies to build readiness in community mobilization efforts for implementation in a multi-year teen pregnancy prevention initiative. J Adolesc Health 2017;60:S51–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Galloway CT, Duffy JL, Dixon RP. Exploring African-American and Latino teens’ perceptions of contraception and access to reproductive health care services. J Adolesc Health 2017;60:S57–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Plastino K, Quinlan J, Todd J, Tevendale HD. Stakeholder education and community mobilization garner support for sex education. J Adolesc Health 2017;60:S24–9. [DOI] [PubMed] [Google Scholar]
- [25].O’Uhuru DJ, Santiago V, Murray LE, et al. Bronx Teens Connection’s Clinic Linkage Model: connecting youth to quality sexual and reproductive health care. J Adolesc Health 2017;60:S38–44. [DOI] [PubMed] [Google Scholar]
- [26].Sotolongo J, House LD, Swanson S, Davis SEH. Integrated community strategies for linking youth to adolescent reproductive health services: a case study. J Adolesc Health 2017;60:S45–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Office of Adolescent Health. TPP Program Grantees (FY2015-2019). Available at: http://www.hhs.gov/ash/oah/oah-initiatives/tpp_program/cohorts-2015-2020.html. Accessed January 26, 2017.