CHWs were able to successfully deliver a culturally adapted version of the Diabetes Prevention Program to community members in an under-resourced setting in a middle-income country.
Keywords: Diabetes Prevention Program, Community health workers, Implementation, Global health
Abstract
Rates of cardiovascular disease and diabetes are rising in low- and middle-income countries (LMIC), but there is a dearth of research devoted to developing and evaluating chronic disease interventions in these settings, particularly in Africa. Lifestyle Africa is a novel, culturally adapted version of the Diabetes Prevention Program (DPP) being evaluated in an ongoing community-based cluster-randomized trial in an underresourced urban community in South Africa. The purpose of this study is to describe the adaptations and adaptation process used to develop the program and to report preliminary implementation findings from the first wave of groups (n = 11; 200 individuals) who participated in the intervention. The RE-AIM model and community advisory boards guided the adaptation process. The program was designed to be delivered by community health workers (CHWs) through video-assisted sessions and supplemented with text messages. Participants in the trial were overweight and obese members of existing chronic disease “support groups” served via CHWs. Implementation outcomes included completion of sessions, session attendance, fidelity of session delivery, and participant satisfaction. Results indicated that 10/11 intervention groups completed all 17 core sessions. Average attendance across all sessions and groups was 54% and the percentage who attended at least 75% of sessions across all groups was 35%. Fidelity monitoring indicated a mean of 84% of all required procedures were completed while overall communication skills were rated as “good" to “excellent”. These preliminary results support the feasibility of culturally adapting the DPP for delivery by CHWs in underresourced settings in LMIC.
Implications.
Practice: It is feasible for community health workers (CHWs) assisted by technology to deliver a culturally adapted lifestyle intervention in an underresourced community setting.
Policy: Policymakers should consider utilizing culturally adapted lifestyle interventions delivered by CHWs assisted with technology to address the chronic disease epidemic in low- and middle-income countries.
Research: Future research should be aimed at adapting and evaluating lifestyle interventions that can be delivered by CHWs in underresourced settings in low- and middle-income countries.
Introduction
Of the estimated 56.4 million global deaths in 2015, almost 40 million (70%) were attributed to noncommunicable diseases (NCDs), particularly cardiovascular diseases (CVDs) and diabetes mellitus (DM) [1]. The NCD epidemic is disproportionately affecting many low- and middle-income countries (LMIC) as they undergo “epidemiological transition” from a primary burden of infectious disease and undernutrition to NCDs and overnutrition [2].
Underlying these trends in LMIC are rising incomes and increased urbanization, which are associated with an increase in intake of fats, caloric sweeteners, animal source foods, and highly processed foods [3], as well as reductions in physical activity [4]. Despite the central role of diet and physical activity in the rising CVD epidemic, there is a dearth of research devoted to developing and evaluating NCD interventions in low- and middle-income settings, particularly in Africa. In high-income countries, considerable resources have been devoted to developing lifestyle interventions, such as the Diabetes Prevention Program (DPP) which has strong empirical support for improving the health of individuals with prediabetes and diabetes [5,6] and is being disseminated by the Centers for Disease Control (CDC) in the USA [7].
The DPP uses established behavioral principles in group sessions delivered by certified “lifestyle coaches” to encourage participants to engage in 150 min of moderate physical activity per week and to reduce body weight by 7% over 6 months. The DPP has also been adapted for several community settings within the USA [8,9].
Although the DPP has been successfully adapted for community settings in the USA, adaptation for widespread use in LMIC presents several challenges. LMIC are likely to lack sufficient trained public health professionals and not be able to afford their use at scale. The literacy and numeracy level assumed of DPP participants may not match the prevailing levels of literacy and numeracy in many LMIC communities. The environment may also not be conducive to being active or accessing affordable healthy food. Individuals may live in crowded informal (shack) settlements that lack reliable electricity, space, cold storage for fresh food, or safe places to exercise. Lastly, the role of cultural factors, such as norms and beliefs related to food preferences, food preparation, or body weight may be important. For example, in many African cultures, a larger body type may be associated with greater dignity and wealth [10].
In addition to barriers, there may be factors that can facilitate intervention delivery in LMIC. For example, CHWs are used in many LMIC countries to provide cost-effective community-based care; this provides opportunities to tap existing social support networks and a community-based health infrastructure [11]. In addition, there is widespread use of cell phones, which offers the opportunity to supplement interventions with a tailored text-message program (e.g., to reinforce or supplement program content and promote engagement), which can enhance behavior change intervention effectiveness [12].
In order to address the lack of proven lifestyle intervention programs suitable for underresourced settings in LMIC, our team has developed a novel adaptation of the DPP (“Lifestyle Africa”). The program is tailored to overweight and obese adults (regardless of disease status) in low-income, urban areas of sub-Saharan Africa and is being evaluated in an ongoing community-based cluster-randomized trial in South Africa [13]. The purpose of the present manuscript is to describe how the DPP was adapted for this setting, including the adaption process and adaptation elements, and to examine preliminary implementation outcomes based on the first wave of participants who received the intervention. Drawing on the RE-AIM model [14], implementation outcomes in this paper focus on outcomes related to reach (i.e., how well the program reached the targeted population) and implementation (i.e., the degree to which the program was implemented as intended), as well as participant satisfaction. These aspects of implementation are most amenable to evaluation at this stage of the trial.
Methods
Adaptations and adaptation process
The setting for the study is the area of Khayelitsha, a fast-growing urban township of Cape Town, South Africa. The residents of Khayelitsha are 99% Black African and 97% isiXhosa speaking [15]. Rates of poverty are very high, with unemployment estimated at 38% and 89% earning less than R6,400 (approximately 475 USD) per month. The majority of residents are migrants from rural areas. Education levels are low with 64% of adults not having completed high school [15]. There is a high prevalence of overweight and obesity [16].
Our community-based approach to adaptation began with formative research documenting the prevalence of chronic disease [16], examining perceptions about changes in lifestyle after migrating from a rural to an urban area [17], studying diet and food preparation habits [17,18], identifying barriers and facilitators to physical activity [19], and understanding cultural norms regarding body image [20]. Preliminary work included developing a training manual and pilot intervention program with CHWs [10,21].
Our formative work led to the development of a strong relationship with an NGO that provides chronic disease care using CHWs to community members diagnosed at local community clinics with CVD and/or diabetes. CHWs provide care to referred individuals by attending regular meetings of naturally occurring community “support groups” to deliver medications and monitor weight, blood pressure, and blood glucose. Support groups consist of approximately 10–50 individuals, mostly older nonworking women, who meet regularly in homes or community facilities for social support, health, or income-generating activities. Discussions with our NGO partner led to the recognition that, for CHWs to address lifestyle risk factors, a formal program or curriculum would be needed. As we considered the feasibility of utilizing the DPP for this purpose, we engaged in additional pilot work to develop and evaluate three sample intervention sessions based on the DPP. Success with the pilot sessions led to a plan to adapt and evaluate the entire DPP.
In addition to considering the five RE-AIM elements of intervention impact (i.e., Reach, Effectiveness, Adoption, Implementation, and Maintenance) [14], we formed two community advisory boards (CABs) and a panel of CHWs to assist with the adaptation process. CAB members included CHWs, community residents with DM and/or CVD, local experts in DM and CVD, and community leaders including a representative of the provincial department of health. The CABs provide input and assistance with all aspects of the project. Based on our formative work and review of the literature, several key adaptations were made to the DPP to increase reach, adoption, and effectiveness within the SA context:
Changing the mode of delivery from highly educated health professionals to video-based delivery facilitated by CHWs
Video support was chosen to reduce the extent to which CHWs needed to have lifestyle change content expertise or to be certified as DPP facilitators. A similar approach was used successfully with CHWs in the USA [9], although Lifestyle Africa extends the approach by using videos to guide the entire flow of each session and to deliver most of the informational content. The videos have an accompanying session guide that provides step-by-step instructions, including when to start and stop the video and the verbal prompts and questions to be used throughout. Videos are supplemented by handouts similar to those provided in the original DPP but adapted for the target community. CHWs are trained to facilitate discussion and guide participants in completing specific program tasks or exercises. Because CHWs deliver sessions in various community locations, portable miniprojectors are used. These are also easily concealed in a small bag, reducing crime risk.
Reducing the level of health literacy and numeracy needed to deliver and participate in the program
Health literacy and numeracy adaptations included significantly increasing information related to nutrition and exercise, including the physiology of diabetes and CVD and key concepts related to weight loss. Explanations of key concepts (e.g., calories, food groups, and energy balance) were simplified and contextualized using examples to fit with local cultural, habits, preferences, and environments. Similarly, numeracy demands were reduced as much as possible through simplification or elimination (e.g., a simplified color-coded guide of foods to choose or eat in moderation was provided as an alternative to calculating calories in a particular quantity of food). To facilitate the participant’s ability to attend to and absorb information, the video sessions included frequent pauses so that the information was delivered in “chunks” followed by discussion and questions. CHWs were given specific prompts to use during each pause to facilitate engagement. Attention was also paid to limiting the length of sessions to reduce the time burden. Lifestyle Africa consists of 17 rather than 16 sessions because one particularly long sessions was divided into two.
Modifying content to match the language and culture of the target community
Adaptations related to language and culture were considered essential for participants to understand the program and perceive the content to be relevant. Similar to the original DPP, role-model stories are used regularly throughout the program. For example, one of the characters is “Boniwe,” a 64 year old Xhosa woman who grew up in a rural area and moved to the city where her lifestyle changed and she developed high blood pressure. During the program, Boniwe is described in her efforts to make lifestyle changes (e.g., identifying her values and how they relate to being healthy and learning about the food groups and healthy eating). Sessions were drafted in English and reviewed by the research team with input from the CABs. Finalized session scripts were translated by bilingual (English and isiXhosa), bicultural team members and then reviewed and edited by other bilingual, bicultural team members. Visual elements of the videos and handouts (e.g., scenes of shops, homes, medical facilities, foods, utensils, and people) were based on still photographs taken by a local photographer in the community following a shot list provided by the video production company. Animation elements were based on the photographs as well as cultural norms related to colors and symbols (see Fig. 1). Animations were also used to explain complex concepts, such as diabetes, high blood pressure, and energy balance.
Fig 1 |.
Video animation and photographic scenes. Scenes depicting the target community and cultural norms such as food preferences.
Enhancing motivational elements of the program
Enhancement of the motivational elements of the program was considered important because participants were enrolled independent of baseline motivation for weight loss as is typical in most DPP studies. To this end, two additional motivational recruitment sessions were developed, which addressed the rising prevalence of diabetes and CVD, the physiology of diabetes and CVD, and the relevance of lifestyle change. The role-model story of Boniwe and her lifestyle before and after moving to the city from her rural homeland was introduced in these sessions. Motivation was also addressed during the core sessions through the use of Motivational Interviewing (MI) principles. The CHWs training curriculum included training in MI, including the MI “spirit” or philosophy (e.g., using an autonomy-supportive style rather than a directive style), core skills (e.g., using open-ended questions), and eliciting change talk (e.g., facilitating the values clarification exercise) [22]. Training in MI was conducted in isiXhosa by local research team members who were, in turn, trained by study team experts in MI (authors D.C., K.R., and L.T.). MI concepts were simplified and culturally appropriate examples used in training.
Capitalizing on the widespread use of cell phones to enhance the intervention with text messages tailored to support the intervention
With input from the CABs, a text-message system was developed and tailored to enhance program impact [23]. The message system was delivered on a dynamic schedule, with messages tailored to match progress through the adapted DPP (e.g., welcome messages at the outset and messages matching weekly content throughout the program). Broadly, messages were designed to reinforce session content, increase motivation, support implementation planning (e.g., “Stand for a period of time at home instead of sitting; this does not require much energy or time”), enhance self-efficacy, and provide positive affirmations.
Parent trial overview
The parent study is an ongoing two-arm parallel cluster-randomized control trial in which CHW teams and their associated support group(s) were randomly assigned to either an intervention or a delayed implementation control group, which continued with usual care. Support group members are enrolled in two waves 12 months apart. The present manuscript focuses on currently available implementation data and includes only intervention arm participants in the first wave who have received the Lifestyle Africa intervention and completed the first follow-up assessment that was conducted approximately 8 months after enrollment.
Recruitment and eligibility
Wave 1 participants were recruited during regular group meetings over approximately 2 months in February and March of 2018 by CHWs trained to deliver the two Lifestyle Africa recruitment sessions. At the second recruitment session, group members were invited to an eligibility screening and enrollment session held at or near their usual meeting place. Eligibility criteria were designed to increase external validity and enroll as many members as possible. Support group members with a body mass index (BMI) ≥25 kg/m2 were eligible to participate in the study, unless they were medically unstable, had a condition that interfered with assessment of weight or weight loss, or were unable to participate in the program. Exclusion criteria included: (a) elevated blood pressure of ≥160 mmHg (systolic) and/or ≥100 mmHg (diastolic); (b) elevated blood sugar (HbA1C > 11) [6]; (c) pregnant, breast feeding, or planning pregnancy within 2 years; (d) chronic use of an oral steroid medication; and/or (e) not planning to participate in the support group over the next 2 years; or (f) apparent intellectual disabilities that would prevent them from understanding the program. Informed consent was conducted prior to screening and those who were found to be eligible and completed baseline data collection were considered enrolled. Participants received a R150 (approximately $12 USD) gift voucher for completing the baseline screening and assessment.
Lifestyle Africa intervention
The Lifestyle Africa intervention consists of two recruitment and 17 core video-based sessions designed to be completed weekly or every other week if preferred by support group members. Core sessions are supplemented by up to 12 monthly, brief “post-core” sessions that do not utilize video. Consistent with the original DPP, the program includes a variety of evidence-based behavior change techniques (e.g., goal-setting, self-monitoring of weight, dietary intake, and physical activity) [24]. Each session has the same basic format: weigh-in; review and discussion of progress toward goal(s) from the prior session; delivery and discussion of new content; and goal setting (“action plans”) for the next session.
CHWs and CHW training
The CHWs delivering Lifestyle Africa were all currently providing care to support groups on behalf of our NGO partner. Each support group is served by two or more CHWs based on group size. CHWs had received basic training from their NGOs as part of their employment (e.g., in-home-based care, chronic disease management, and wellness). The requisite for their employment is basic reading, writing, and arithmetic skills sufficient to maintain attendance registers, medication logs, etc. For the Lifestyle Africa project, CHWs received an additional 5 and a half days of didactic training, including education on diabetes and diabetes management, behavior change principles, MI, group facilitation, projector use, logistics, and safety. MI training used adapted, jargon-free concepts and experiential learning activities and focused on the core skills of open-ended questions and reflective listening. The training to deliver the program sessions was conducted through eight additional weekly half-day experiential training sessions where they acted as program participants in an accelerated mock delivery of Lifestyle Africa. Over the course of the program, each CHW was required on a rotational basis to practice delivering key aspects of the program (e.g., conducting weigh-in, setting up the projector, and facilitating goal-setting exercise).
Measures
Reach
Indicators included the proportion of the number of individuals within support groups who were informed about the program that agreed to participate as well as individual-level session attendance. Although precise attendance numbers for the support groups were not available and varies over time as individuals join or discontinue attendance, we considered the denominator for reach to be all the individuals that were informed about the program at either of the two recruitment sessions that were held during regular group meetings. Attendance indexes were calculated with respect to attendance within each support group as groups are the primary unit of analysis. Indexes included the percent of enrolled participants within each group at each session, mean attendance within each group across all sessions, and the percent of participants within each group who received a high “dose” of the program, defined a priori as ≥75%.
Implementation
Implementation metrics were session completion and session fidelity on the part of the CHWs. Session completion was determined through completed attendance registers the CHW returned to the NGO. Confirmation of session completion was made by research staff either through direct observation of the sessions or through confirmation from support group managers who oversee events at the support groups.
Session fidelity was assessed by observing sessions using a checklist of required protocol elements and rating scales of facilitation quality. We aimed to observe the first 10 sessions for each group and then intermittently thereafter. The fidelity measure included nine protocol elements common to all sessions (e.g., set up the room correctly, completed weigh-in, and completed “opening facilitation”) and one to three session-specific protocol elements for each session (e.g., for Session 10: “demonstrated deep breathing and muscle relaxation exercises”). Completion of each element was rated as “yes”/”no” or “partially completed.” Fidelity to group facilitation and MI principles was assessed through adapted MI fidelity rating scales [25]. Items assessed the use of open questions, reflective listening, building confidence, expressing empathy and acceptance, sharing of power (i.e., conveying a sense of partnership and autonomy support), and avoiding confrontation. Group facilitation skills were assessed with seven items that assessed how well the CHW kept the conversation going, gave everyone a chance to speak, kept the group on track, kept the focus on the group members, allowed members to talk through their problems, responded to questions, kept the session interactive, and handled participant questions. One item was used to provide an overall rating of how well the CHW conducted the session. The response scale for all items was a 7-point Likert scale with three verbal anchors (1 = poor/never; 4 = good/often; 7 = excellent/always). In prior research using the instrument, a cutoff of 4 or higher was deemed to be an acceptable level of fidelity [26].
Participant satisfaction
Program satisfaction measures were completed by all participants as part of the interviewer-administered 8 month follow-up survey. Ten items included overall ease or difficulty of understanding the sessions (1 = very difficult; 4 = very easy), length of the sessions (1 = too short; 3 = too long), the number of sessions (1 = not enough; 3 = too much), overall helpfulness of each component of the program, including weigh-ins, videos, CHWs, group discussions, participant “notebooks” (i.e., book of handouts for all sessions), activity logs (i.e., logs for tracking minutes of exercise), “action plans” (i.e., goals that were set at the end of each session), and text messages (1 = not at all helpful; 4 = extremely helpful), how suitable the program is for other community residents to prevent or help with diabetes or heart disease (1 = not at all suitable; 3 = very suitable), and whether they would recommend that their family and friends participate in the program (yes/no).
Results
Participants were predominantly elderly (mean age 65; standard deviation [SD] 11.6), female (89%), and had low levels of education (mean years of education = 6.7; SD 3.5) and income (98% monthly household income was less than or equal to R6400 or approximately $500). The participants’ mean BMI was 34.4 (in the obese range). More than two-thirds had been prescribed medications for CVD and more than a quarter had been prescribed diabetes medications.
Reach
All 11 Wave 1 groups randomized to the intervention arm agreed to participate. Of 227 individuals who participated in any of the recruitment sessions conducted during usual group meetings, 200 (88%) came for screening and 134 (67% of those screened) were found to be eligible and enrolled. Reasons for exclusion (not mutually exclusive) were BMI <25 (n = 33), BP ≥160/100 (n = 23), HbA1c >11 (n = 11), planning to leave the group (n = 1), chronically taking a steroid medication (n = 1).
Session completion and attendance
Session completion was high, with 10 of 11 support groups holding all 17 core sessions (see Table 1). One support group did not complete one session and the attendance register was lost for Session 16, so the number of participants attending this session is not available. Mean attendance across all sessions for all groups was 54% (ranging from 44% to 81%). The mean percentage of participants that attended at least 75% of sessions across groups was 35% (ranging from 14% to 75%). Mean attendance across all groups varied by session from a low of 41% (Session 14) to a high of 71% (Session 1). Mean attendance decreased through Session 10 and then increased over the last three sessions.
Table 1 |.
Percentage of each group’s participants that attended each session
| Session | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | Mean |
| 1 | 93% | 93% | 67% | 53% | 80% | 33% | 53% | 60% | 80% | 47% | 47% | 53% | 40% | 27% | 20% | 47% | 80% | 57% |
| 2 | 67% | 53% | 66% | 100% | 93% | 80% | 67% | 53% | 53% | 53% | 53% | 53% | 33% | 87% | 47% | 67% | 40% | 63% |
| 3 | 50% | 63% | 63% | 38% | 38% | 50% | 50% | 63% | 50% | 38% | 38% | 63% | 50% | 38% | NC | C | 50% | 49% |
| 4 | 90% | 70% | 70% | 50% | 50% | 50% | 40% | 50% | 50% | 40% | 30% | 30% | 40% | 50% | 40% | 70% | 60% | 52% |
| 5 | 81% | 94% | 94% | 94% | 75% | 81% | 81% | 75% | 81% | 69% | 63% | 75% | 100% | 75% | 81% | 88% | 75% | 81% |
| 6 | 80% | 70% | 50% | 60% | 40% | 20% | 30% | 30% | 30% | 30% | 40% | 30% | 44% | 30% | 50% | 50% | 70% | 44% |
| 7 | 43% | 64% | 36% | 50% | 43% | 36% | 43% | 43% | 36% | 50% | 50% | 36% | 57% | 36% | 64% | 57% | 57% | 47% |
| 8 | 82% | 65% | 71% | 63% | 75% | 41% | 59% | 47% | 41% | 29% | 41% | 47% | 41% | 35% | 53% | 35% | 41% | 51% |
| 9 | 56% | 67% | 78% | 44% | 56% | 56% | 56% | 22% | 44% | 33% | 56% | 56% | 22% | 22% | 22% | 33% | 67% | 46% |
| 10 | 64% | 57% | 57% | 50% | 43% | 36% | 29% | 71% | 29% | 36% | 50% | 36% | 29% | 29% | 50% | 36% | 57% | 45% |
| 11 | 75% | 75% | 50% | 50% | 25% | 75% | 75% | 50% | 50% | 50% | 50% | 75% | 25% | 25% | 50% | 50% | 75% | 54% |
| Mean | 71% | 70% | 64% | 59% | 56% | 51% | 53% | 51% | 49% | 43% | 47% | 50% | 43% | 41% | 48% | 53% | 61% | 54% |
NC = Session not completed; C = Session completed but attendance data missing.
Fidelity
Of 186 sessions held, 131 (70%) were observed, with the first 10 sessions observed for 9 out of 11 groups and 7 out of the first 10 sessions observed for 2 groups. Mean completion rates (i.e., fully completed vs. partially or not completed) of protocol elements (e.g. set up the room appropriately and conduct the weigh-in) for each group ranged from 62% to 91% (mean = 84%), but all but one group was at 79% or higher. Mean group facilitation skills ranged from 4.8 to 6.2 (1 = poor/never; 7 = excellent/always), whereas mean MI skills ranged from 4.7 to 5.9 on a 7-point scale (1 = poor/never; 4 = good/often; 7 = excellent/always). The mean overall rating of the quality of the sessions by group ranged from 4.8 to 6.0 (1 = poor; 4 = good; 7 = excellent).
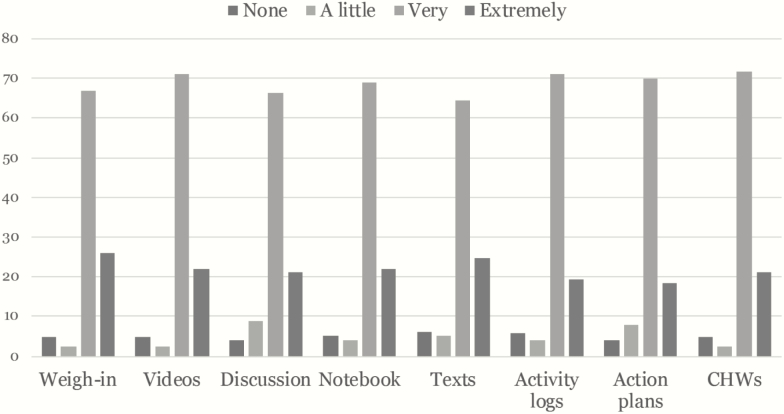
Satisfaction
Frequencies (percentages) of satisfaction ratings of the main components of the intervention are displayed in Fig. 2. Most participants (78%) rated the number of sessions as “just about right,” although substantially more of the remaining participants thought that there were too many rather than too few sessions (18% vs. 4%, respectively). Similarly, 80% of participants rated the length of sessions as “just about right,” although more participants thought sessions were too long rather than too short (16% vs. 4%, respectively). Most participants rated the sessions as “very easy” (53%) or “somewhat easy” (22%) to understand. Almost all participants rated the program as “very suitable” for other community residents and would recommend the program to family and friends (93% and 97%, respectively).
Fig 2 |.
Percent rating each category of perceived helpfulness by program component.
Discussion
The rise in NCDs in LMIC calls for innovative, context-specific interventions. Our novel adaptation of the DPP had excellent reach with respect to enrollment among the targeted community as all groups assigned to the intervention arm agreed to participate and a high proportion (88%) of group members attended the session for study screening and enrollment. Nearly 70% of screened participants met our BMI inclusion criterion, consistent with recent data about obesity prevalence in resource-limited settings [27].
Our preliminary implementation findings indicated that our delivery model is feasible. CHWs completed all 17 core sessions for all but one group which missed one session. This is notable because the intervention was delivered as naturalistically as possible. For example, there was no payment to any stakeholder (i.e., participants, NGO management, and CHWs) for the completion of sessions. CHWs were also not selected based on their abilities or skills but were the full cohort of currently employed CHWs. Resources in this environment are extremely limited compared to typical high-income country community settings (e.g., spaces to meet are limited in availability and size; furniture is limited and basic; spaces lack electricity or air-conditioning; and transportation is unreliable and costly for participants). Moreover, disruption of schedules is commonplace (e.g., due to community protests family events, such as illnesses or funerals, government pension collection days, criminal activity, power outages, and government policy changes).
These aspects of the environment affect the NGO management and supervisors, CHWs, and participants. One effect of the disruptive environment is that the completion of all 17 sessions took longer than anticipated, with most groups taking almost all of the 8 month period between the baseline and follow-up assessment to complete them. One concern that did not materialize was that projectors would breakdown, be lost or stolen, or make CHWs a target for being robbed. The risk of loss was reduced by removing projectors from the NGO office overnight while the building was unoccupied, but it was still notable that not a single projector had to be replaced.
Mean attendance exceeded 40% across all groups and, in 6 of the 11 groups, 30% or more attended more than 75% of sessions. While this is much lower than the percentage who elected to enroll in the program, participants received a small financial incentive for completing enrollment but no incentive for completing sessions. Futhermore, participants were not treatment seeking and were proactively recruited. Attendance in this study is lower than in a CHW delivered DPP program in North Carolina where attendance across all sessions was 79% [21]. However, in addition to being in a high-income country, participants in that study were relatively well educated and younger. Results from an analysis of the CDC’s National Diabetes Program, an effort to disseminate the DPP across the USA, revealed that less than 50% of participants attended 75% of the 16 core sessions [28]. Given the age of our participants and the resource-constrained environment, our observed attendance could be considered impressive.
We also noted a decline in attendance over time with somewhat of an increase toward the end. Anecdotally, it appeared that attendance declined due to winter weather. Attendance in this study was also likely bolstered by the fact that participants were recruited from, and sessions were held at, support groups where they regularly met. The implementation of the intervention through an existing community-based system of care and existing social networks was intentional, but our attendance results may not generalize outside of similar structures.
CHW’s were able to deliver the program with a reasonably high degree of fidelity. Full completion of basic protocol elements was, for all but one group, around 80% or higher. During training, one of the most challenging aspects for CHWs was learning to use the projectors (e.g., CHWs were challenged by the complex menu system for launching the video file). In practice, the CHWs had little difficulty after the initial sessions. More striking were our findings regarding CHWs group facilitation. Although subjective and based on ratings by different research team members, our MI fidelity measure has been successfully used in prior trials, including one in which blind, independent coding confirmed fidelity [26]. Mean ratings for the groups were around 5 or higher (i.e., between 4 = good/often and 7 = excellent/always). The training was limited to a few days, yet with the support of the videos and sessions scripts and handouts, CHWs were able to conduct sessions that meaningfully engaged participants in the program content. Our emphasis in training on MI principles led to CHWs communicating a reasonable degree of empathy, autonomy support, and avoidance of confrontation during the sessions. As noted above, CHWs could not be selected or replaced based on performance. The fidelity ratings across groups may have been enhanced because CHWs worked in teams (usually pairs), allowing them to support each other. Success with communication skills is potentially important because this has been identified as an important gap in research on the training of CHWs [29].
Participant satisfaction ratings provided additional support for the implementation model. All of the program components were rated as helpful with little difference between them, and there was broad satisfaction with the number and length of sessions. Participants also generally felt that the sessions were understandable and overwhelmingly indicated that they would recommend the program to others. In spite of these positive ratings, the minority responses also suggested that the program could be improved by reducing the number and length of sessions and making sessions easier to understand. For example, greater use of experiential learning (e.g., cooking and tasting) may be more effective than didactic videos. On the other hand, experiential learning may be logistically more difficult to implement. Also encouraging was the finding that a very high proportion of participants rated the program as suitable for the community. This is essential given that culturally appropriate interventions have been shown to be more effective (e.g., [30]).
Taken as a whole, this study provides encouraging results supporting the feasibility of adapting the DPP for underresourced settings in low- and middle-income settings. Other diabetes prevention programs have been implemented and evaluated in low- and middle-income countries, including those using elements of peer support models and/or text messaging (e.g., [31,32]). However, this study targeted a deeply underresourced community and contributes a new version of the CDC’s DPP using CHWs and video to deliver the intervention.
Limitations of the study include the reach of the program being to predominantly elderly females because of the nature of the preexisting groups. Other dissemination avenues are necessary to broaden the program’s impact. For example, in the USA, efforts have been made to disseminate the DPP via churches [8]. The findings are also based only on the first wave of participants from one NGO. Completion by the second wave may highlight NGO-related factors that affect implementation outcomes. Our findings are based on a single NGO working in a particular context and setting and may not necessarily generalize to all NGO’s and settings.
Despite these limitations, the study provides encouragement for the feasibility of adapting the DPP for delivery by CHWs in underresourced settings in low- and middle-income countries. The global chronic disease epidemic demands continued efforts to develop culturally appropriate intervention tools for underresourced communities in low- and middle-income countries.
Funding: This study was funded by the National Heart, Lung, and Blood Institute (R01 HL126099). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, And Blood Institute or the National Institutes of Health.
Compliance with Ethical Standards
Conflicts of Interest: Authors D.C., K.G., L.P.T., and K.R. occasionally conduct Motivational Interviewing training. T.P., K.F., J.M.S., E.A.H., S.S., M.Z.V., E.V.L., M.H., K.M., and R.S. declare that they have no conflicts of interest.
Authors’ Contributions: D.C., T.P., L.P.T., K.G., and K.R. contributed to overall study conception and design including the adaptation process. D.C., T.P., L.P.T., K.R., M.Z.V., E.V.L., and S.S. contributed to the design of the overall intervention. D.C., E.A.H., K.R., K.G., J.M.S., T.P., and L.P.T. helped to design measures and outcomes. JMS, DC, KG, and KR contributed to design of the text message component. D.C., K.R., K.G., and L.P.T. contributed to the Motivational Interviewing content and training. D.C., L.P.T., T.P., S.S., M.H., and K.M. contributed to data acquisition. D.C., S.S., and R.S. contributed to data analysis. D.C. drafted the manuscript and all others contributed to revising it critically for important intellectual content.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethical approval was obtained from the University of Cape Town and Children’s Mercy.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
References
- 1. World Health Organization. Global Health Estimates 2015: Deaths by Cause, Age, Sex, by Country and by Region 2016. https://www.who.int/healthinfo/global_burden_disease/estimates_regional_2000_2015/en/. Accessibility verified Sept 30, 2019. [Google Scholar]
- 2. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006; 3(11):2011–2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Popkin BM. The nutrition transition in the developing world. Dev Policy Rev. 2003;21(5-6):581–597. [Google Scholar]
- 4. Kruger HS, Venter CS, Vorster HH; THUSA Study . Physical inactivity as a risk factor for cardiovascular disease in communities undergoing rural to urban transition: The THUSA study. Cardiovasc J S Afr. 2003;14(1):16–23, quiz 23, 28. [PubMed] [Google Scholar]
- 5. Knowler WC, Barrett-Connor E, Fowler SE, et al. ; Diabetes Prevention Program Research Group . Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Look AHEAD Research Group, Pi-Sunyer X, Blackburn G, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Diabetes Care. 2007;30(6):1374–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. DPP Research Group. National Diabetes Prevention Program https://www.cdc.gov/diabetes/prevention/index.html. Accessibility verified Sept 30, 2019. [Google Scholar]
- 8. Boltri JM, Davis-Smith M, Okosun IS, Seale JP, Foster B. Translation of the National Institutes of Health diabetes prevention program in African American churches. J Natl Med Assoc. 2011;103(3):194–202. [DOI] [PubMed] [Google Scholar]
- 9. Katula JA, Vitolins MZ, Rosenberger EL, et al. One-year results of a community-based translation of the diabetes prevention program: Healthy-living partnerships to prevent diabetes (HELP PD) Project. Diabetes Care. 2011;34(7):1451–1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Puoane T, Bradley H, Hughes G. Community intervention for the emerging epidemic of non-communicable diseases. South Afr J Clin Nutr. 2006;19(2):56–62. [Google Scholar]
- 11. Bangdiwala SI, Fonn S, Okoye O, Tollman S. Workforce resources for health in developing countries. Public Health Rev. 2010;32(1):296–318. [Google Scholar]
- 12. Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev. 2010;32(1):56–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Catley D, Puoane T, Tsolekile L, et al. Adapting the diabetes prevention program for low and middle-income countries: Protocol for a cluster randomised trial to evaluate “Lifestyle Africa”. BMJ Open. 2019;9(11):e031400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: The RE-AIM framework. Am J Public Health. 1999;89(9):1322–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Statistics South Africa (Stats SA). Census 2011 Statistical Release 2012. https://www.statssa.gov.za/publications/P03014/P030142011.pdf. Accessibility verified Sept 30, 2019. [Google Scholar]
- 16. Malhotra R, Hoyo C, Østbye T, et al. Determinants of obesity in an urban township of South Africa. South Afr J Clin Nutr. 2008;21(4):315–320. [Google Scholar]
- 17. Stern R, Puoane T, Tsolekile L. An exploration into the determinants of noncommunicable diseases among rural-to-urban migrants in periurban South Africa. Prev Chronic Dis. 2010;7(6):A131. [PMC free article] [PubMed] [Google Scholar]
- 18. Bradley HA, Puoane T. Prevention of hypertension and diabetes in an urban setting in South Africa: Participatory action research with community health workers. Ethn Dis. 2007;17(1):49–54. [PubMed] [Google Scholar]
- 19. Puoane T, Matwa P, Bradley H, Hughes G. Socio-cultural factors influencing food consumption patterns in the black African population in an urban township in South Africa. 2011. http://search.ebscohost.com.proxy.library.umkc.edu/login.aspx?direct=true&db=edsoai&AN=edsoai.ocn845021749&site=eds-live&scope=site. Accessibility verified Sept 30, 2019. [Google Scholar]
- 20. Puoane T, Fourie JM, Shapiro M, Rosling L, Tshaka NC, Oelofse A. “Big is beautiful”—An exploration with urban black community health workers in a South African township. South Afr J Clin Nutr. 2005;18(1):6–15. [Google Scholar]
- 21. Puoane TR, Tsolekile L, Igumbor EU, Fourie JM. Experiences in developing and implementing health clubs to reduce hypertension risk among adults in a South African population in transition. Int J Hypertens. 2012;2012:913960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Miller WR, Rollnick S.. Motivational Interviewing. 3rd ed New York, NY: Helping People Change; 2012. [Google Scholar]
- 23. Heron KE, Smyth JM. Ecological momentary interventions: Incorporating mobile technology into psychosocial and health behaviour treatments. Br J Health Psychol. 2010;15(Pt 1):1–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Venditti EM, Kramer MK. Necessary components for lifestyle modification interventions to reduce diabetes risk. Curr Diab Rep. 2012;12(2):138–146. [DOI] [PubMed] [Google Scholar]
- 25. McMaster F, Resnicow K. Validation of the one pass measure for motivational interviewing competence. Patient Educ Couns. 2015;98(4):499–505. [DOI] [PubMed] [Google Scholar]
- 26. Catley D, Goggin K, Harris KJ, et al. A randomized trial of motivational interviewing: Cessation induction among smokers with low desire to quit. Am J Prev Med. 2016;50(5):573–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ford ND, Patel SA, Narayan KM. Obesity in low- and middle-income countries: Burden, drivers, and emerging challenges. Annu Rev Public Health. 2017;38(1):145–164. [DOI] [PubMed] [Google Scholar]
- 28. Ely EK, Gruss SM, Luman ET, et al. A national effort to prevent type 2 diabetes: Participant-level evaluation of CDC’s national diabetes prevention program. Diabetes Care. 2017;40(10):1331–1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jackson EJ, Parks CP. Recruitment and training issues from selected lay health advisor programs among African Americans: A 20-year perspective. Health Educ Behav. 1997;24(4):418–431. [DOI] [PubMed] [Google Scholar]
- 30. Creamer J, Attridge M, Ramsden M, Cannings-John R, Hawthorne K. Culturally appropriate health education for Type 2 diabetes in ethnic minority groups: An updated Cochrane Review of randomized controlled trials. Diabet Med. 2016;33(2):169–183. [DOI] [PubMed] [Google Scholar]
- 31. Sathish T, Williams ED, Pasricha N, et al. Cluster randomised controlled trial of a peer-led lifestyle intervention program: Study protocol for the Kerala diabetes prevention program. BMC Public Health. 2013;13(1):1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ramachandran A, Snehalatha C, Ram J, et al. Effectiveness of mobile phone messaging in prevention of type 2 diabetes by lifestyle modification in men in India: A prospective, parallel-group, randomised controlled trial. Lancet Diabetes Endocrinol. 2013;1(3):191–198. [DOI] [PubMed] [Google Scholar]