Abstract
OBJECTIVES
The aim of this study was to evaluate the knowledge of physicians on influenza and pneumococcal vaccine.
MATERIALS AND METHODS
A questionnaire was administered to physicians working in Kyrenia University Hospital and Near East University School of Medicine.
RESULTS
There were 38 female (56.7%) and 29 male (43.3%) participants. The mean age was 39.3±12.5 years. There were 24 general practitioners (GP) and 43 specialists participating in the study. Influenza vaccine and its risk minimization for infection were well known among 92.5% of the participants. However, 76.1% of them mentioned that they had knowledge about the pneumococcal vaccine, and this ratio about its reducing the risk of infection was 73.1%. 83.7% of specialists and 79.2% of GP thought that adult vaccines were effective (p=0.6). The rate of influenza vaccination among specialists was higher than that of GP (67.4% vs. 41.7%, p=0.04). However, the rates of pneumococcal vaccination were low and similar in both groups (p=0.3). In both specialists and GP, the most common reason for not receiving the vaccine was the belief of not being in the risk group (p=0.9). The knowledge level of pneumococcal vaccination in GP was found to be statistically lower than in specialists (p<0.05).
CONCLUSION
Although influenza vaccine and its risk minimization for infection are well known among physicians, the pneumococcal vaccine is not well known. It is suggested that training about vaccination for both specialists and GP are important for preventive medicine.
Keywords: Influenza, knowledge, pneumococcus, physician, vaccination
INTRODUCTION
Influenza and pneumococcal infections are the leading causes of mortality and morbidity worldwide, particularly in older adults [1]. Every year, pneumococcal infections account for approximately 1.6 million deaths worldwide [2]. It is also known that pneumococcal infections are more prevalent during spikes in the incidence of influenza. Secondary bacterial pneumonia (mostly S. pneumonia) corresponds to approximately 50% of deaths during the flu season in the United States [2].
Although the effectiveness, safety, and efficacy of pneumococcal and influenza vaccines have been proven by many studies, vaccination coverage of high-risk adults even in developed countries, remains low [3–5]. Pneumococcal vaccination rates in elderly are as low as 31% in Germany. For influenza, the rate is approximately 37%, which is lower than the target of 75% given by the World Health Organization (WHO) [6].
Health care workers are also at high risk of both acquiring influenza and transmitting it to the patients and other medical staff. Vaccination is the best preventive intervention against influenza. Thus, immunization is recommended annually for all health care providers by the WHO, the CDC in the United States, and the national health authorities of most European countries [7]. A survey reporting influenza vaccination rates from 10 European countries during three consecutive flu seasons (from 2008 to 2011) among health care workers remained <35% [7]. A review including 14 studies from around the world found that one of the strongest predictors of vaccination is physician’s recommendation [8]. Because the vaccination coverage rates even among health care professionals remain low, the objective of this study was to understand the knowledge and attitudes of physicians about influenza and pneumococcal vaccines.
MATERIALS AND METHODS
The study was carried out in University of Kyrenia Dr. Suat Gunsel Hospital and Near East University, School of Medicine All the participants were physicians. A self-administered questionnaire was provided to all volunteer physicians between September 2017 and October 2017. Physicians included general practitioners (GP) and specialists (Infectious Disease, Pulmonary Disease, Internal Sciences, and Surgical Sciences). Approximately 100 physicians were contacted, and 67 of them responded to the questionnaire.
The questionnaire included demographic data (age, gender, employment duration) and 10 questions about influenza and pneumococcal vaccines. The knowledge on influenza and pneumococcal vaccines, the effect of vaccines on reducing the infection risk, vaccination rates among physicians, and reasons for refusing the vaccine were examined. The knowledge of vaccination was defined according to one question: “Do you have knowledge about the influenza/pneumococcal vaccine?” The questionnaire was prepared by specialists in pulmonary disease and infectious diseases, and it was not a validated questionnaire. All statements included in the questionnaire were either exactly right or wrong to decrease the inter-individual interpretation difference. Thus, the answers were classified as “yes,” “no,” or “no idea.” If the participants were sure about the answer they chose yes or no. But if they were not sure about the question, they chose no idea. For example,
I have heard about the name of the vaccine, and I know the efficacy. Yes.
I have not heard about the name of the vaccine, and I do not know the efficacy. No.
I have heard about the name of the vaccine, but I do not know about its effectiveness. No idea.
All participants were informed about the aim of the study, and they gave their written informed consent. The study was approved by the local ethical committee of the University of Kyrenia (22/08/2017; ref no. RY-2017–12).
Statistical Analysis
All statistical analyzes were performed using the IBM Statistical Package for the Social Sciences for Windows version 20.0 (IBM SPSS Corp.; Armonk, NY, USA). Continuous variables were expressed as the mean±standard deviation, and categorical variables were expressed as counts (percentage). Comparisons of categorical variables between the groups were performed using the chi-squared test. A two-sided p-value <0.05 was considered to be statistically significant.
RESULTS
A total of 67 physicians, 38 female (56.7%) and 29 males (43.3%), were enrolled. The mean age was 39.3±12.5 years. The mean age was higher in male than female physicians, and the difference was statistically significant (44.6±13.3 vs. 35.2±10.3 years, p=0.001). Two-thirds of the physicians had been working for at least 5 years.
Eighty-one percent of physicians stated that the adult vaccination was effective. There was no significant difference in gender regarding the opinion on the efficacy of adult vaccination (p=0.2). Influenza vaccine and its risk minimization for infection was well known among 92.5% of the physicians (Figure 1). However, 76.1% mentioned that they had knowledge about pneumococcal vaccine, and this ratio about its reducing of the risk of infection was 73.1% (Figure 2).
Figure 1.
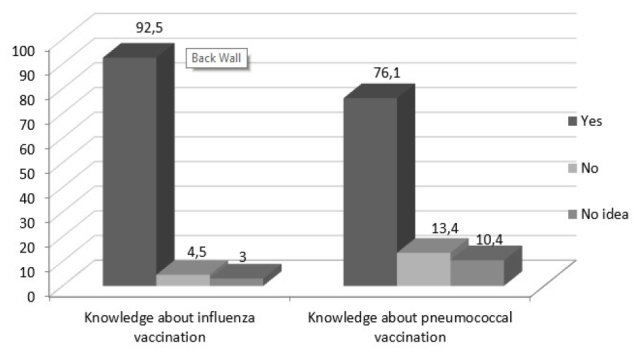
Do you have knowledge about influenza and pneumococcal vaccination? (%)
Figure 2.
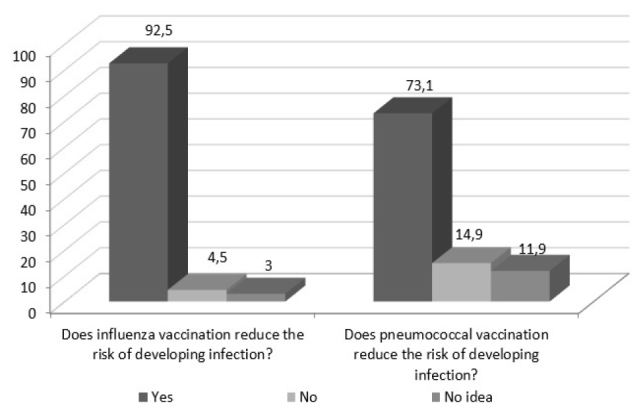
Do vaccinations reduce the risk of developing infections? (%)
Among the participating physicians, the rates of vaccination were 58% for influenza and 4.5% for pneumococcal vaccination. The rate of influenza vaccination was similar in both genders (63.2% vs. 51.7%, p=0.3). Only 3 (4.5%) of the cases had pneumococcal vaccination, and all were female. The ages of these physicians were 34, 30, and 31 years, respectively. One of them was a general surgeon, and others were GP. All of them stated that they had a pneumococcal vaccine with a doctor’s recommendation.
There were 24 (35.8%) GP and 43 (64.2%) specialists in the study. The distribution of the physicians according to working specialties is shown in Figure 3. Of them, 83.7% of specialists and 79.2% of GP thought that adult vaccines were effective (p=0.6). The rate of influenza vaccination among specialists was higher than that of GP (67.4% vs. 41.7%, p=0.04). However, the rates of pneumococcal vaccination were low and similar in both groups (p=0.3). All of the influenza-vaccinated specialists indicated that their colleague had recommended the vaccination, but the colleague recommendation was 70% in the GP, and the difference was statistically significant (p=0.009). Among vaccinated specialists and GP, the proportion of people who thought that vaccination was beneficial was found to be similar (72.4% vs. 70%, p=0.6).
Figure 3.
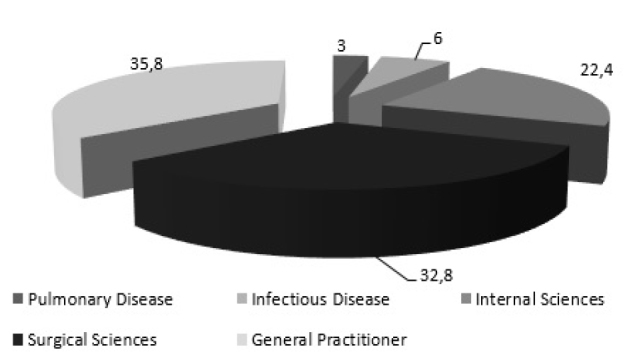
Distribution of physicians according to working specialties (%)
In both specialists and GP, the most common reason for not receiving the vaccine was the belief of not being in the risk group (p=0.9) (Figure 4). While the knowledge level on influenza vaccination was similar between practitioners and specialists, the knowledge level on pneumococcal vaccination in GP was found to be statistically lower than in specialists (p<0.05; Table 1).
Figure 4.
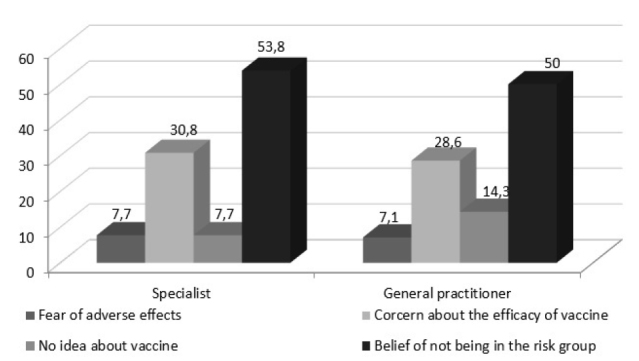
Reasons for not being vaccinated among specialists and general practitioners (%)
Table 1.
Knowledge level of specialists and general practitioners about influenza and pneumococcal vaccination
| Specialist | General practitioner | ||||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Yes | No | No idea | Yes | No | No idea | p | |
| Do you have information about influenza vaccination? n (%) | 40 (93%) | 1 (2.3%) | 2 (4.7%) | 22 (91.7%) | 2 (8.3%) | 0 | 0.3 |
| Does influenza vaccine reduce the risk of infection? n (%) | 40 (93%) | 2 (4.7%) | 1 (2.3%) | 22 (91.7%) | 1 (4.2%) | 1 (4.2%) | 0.9 |
| Do you have information about pneumococcal vaccination? n (%) | 37 (86%) | 4 (9.3%) | 2 (4.7%) | 14 (58.3%) | 5 (20.8%) | 5 (20.8%) | 0.03 |
| Does pneumococcal vaccine reduce the risk of infection? n (%) | 36 (83.7%) | 6 (14%) | 1 (2.3%) | 13 (54.2%) | 4 (16.7%) | 7 (29.2%) | 0.004 |
DISCUSSION
This study demonstrated that the knowledge level on influenza vaccination was similar between GP and specialists; however the knowledge level on pneumococcal vaccination in GP was found to be statistically lower than in specialists. Nearly 60% of the physicians had influenza vaccination. The rate of influenza vaccination among specialists was higher than that of GP. In addition, the rates of pneumococcal vaccination were low in both groups. The most common reason for refusing the vaccine was the belief of not being in the risk group.
Influenza leads to over 200,000 hospitalizations and 300–49,000 deaths annually in the United States [9,10]. It can cause severe illness and serious complications, such as secondary bacterial pneumonia [11,12]. Streptococcus pneumoniae is the most commonly isolated microorganism from adults with pneumonia and sepsis [13]. Failure of natural immunity leads to invasive pneumococcal infections. The highest rates of pneumococcal disease are observed in infants, the elderly, immune compromised patients, and patients with chronic respiratory disease [14]. Health care workers are also at increased risk for influenza, and vaccination is justified to protect them from occupational exposure and to prevent the spread of disease to susceptible patients [15].
Vaccination of high-risk patients against influenza and pneumococcal infections prevents disease-associated mortality and morbidity, and it is one of the key public health issues in most countries. Influenza vaccination is a fundamental tool for the prevention of influenza in health care settings, and its administration to health care workers is recommended in over 40 countries, including the United States of America and many countries of the European Union [16]. Furthermore, pneumococcal disease is a vaccine-preventable disease. The 23-valent pneumococcal polysaccharide vaccine and the 13-valent pneumococcal conjugate vaccine have been recommended for individuals at high risk of pneumococcal disease since 2003, including adults aged >65 years [14]. The Advisory Committee on Immunization Practice of the CDC recommends immunization schedules and updates them regularly. Although these recommendations are available to health care professionals, studies show that almost 50% of those do not rely on guidelines [17].
Studies suggest that additional control strategies for pneumococcal disease are needed particularly during the influenza season and pandemic outbreaks. This means that policymakers can potentially control two diseases that co-occur [2].
According to the CDC survey, approximately 20% of adults aged ≥65 years who received flu vaccine reported that they have never received a pneumococcal vaccination [18]. Many barriers to successful vaccination programs have been identified, including the fear of adverse effects, missed opportunities, and lack of awareness regarding the seriousness of those infections. The results of a study from Korea showed that the most important barrier to vaccination was that 75% of high-risk patients were not even aware that the vaccine existed. Second most common barrier was a negative attitude coming from clinicians. However, doctors’ advice was the most triggering factor that encouraged patients to get vaccination, similar to results of several studies [18].
Being both in the high-risk group and a potential motivator to receive flu vaccine, physicians play an important role in successful vaccination programs. Immunization rates of health care workers have changed over years and in various countries. The highest immunization rate among physicians (88.3%) with influenza vaccination was reported in Saudi Arabia [19]. In the 2005–2006 NICS study in Canada, the physician coverage of flu vaccine was close to that of elderly patients (physicians, 74.3%; patients, 69.9%) [5]. According to a survey from Turkey, physicians’ self-vaccination rate for influenza was approximately 41.2% [18]. Similarly, Maltezou et al. [15] reported a coverage level of 44% among physicians in their survey. This rate varied from 30% to 76.4% in Italy [16,20]. There are no significant data about the immunization of health care workers in Northern Cyprus. As a first study conducted in Northern Cyprus, to the best of our knowledge, the self-vaccination rate of all physicians was 58.2 % in our study. It was 67.4% for specialists and 41.7% for GP. These findings suggest that the priority should be given to GP training in the action plan.
The main reasons for refusing vaccination are the feeling of invulnerability to vaccination, belief of not being at risk, of being too young or in good health. Misconceptions about the vaccine efficacy, fear of needles, fear of adverse effects, and fear of contracting illness from the vaccine are significantly associated with noncompliance [21–23]. In the study by Haridi et al. [19], the main reasons for vaccination avoidance were the misconception that the vaccine causes influenza (38.5%) and concern about the vaccine efficacy (32.7%). In our study, the most common reason for refusing vaccination among the physicians was the belief of not being at risk (51.9%). Similar to Haridi et al. [19], there was a concern about the efficacy of vaccination in 30.8% of the specialists and 28.6% of GP. Data from the United States show that the flu vaccination rate increased from 47% to 96% where influenza vaccination is legally obligatory [21]. It is thought that stronger recommendations are needed to achieve a higher vaccination coverage against vaccine-preventable diseases. Furthermore, the barriers in front of the vaccination can be overcome with education and legal regulations.
In some studies, the vaccination rate was increased with longer working durations, and this can be explained with increased awareness. In our study, two-thirds of the physicians had been working for at least 5 years. There was no significant difference in the vaccination rates with respect to longer working durations. This might be explained by our relatively small study group.
The pneumococcal vaccination coverage rates were significantly low in our study. This was primarily due to the health care workers’ not being in the risk group for pneumococcal disease. In health care workers, influenza vaccination is indicated, although there are no recommendation about the pneumococcal vaccination in this population without comorbidities [24]. But the study also showed that the awareness of pneumococcal vaccination was lower than that of influenza. When compared to specialists, GP have similar attitudes about flu vaccination, but a lower information level on pneumococcal vaccination.
To the best of our knowledge, this is the first study evaluating the knowledge of physicians about influenza and pneumococcal vaccination in Cyprus. In addition, there are some limitations to the study. First, the study was carried out in only two hospitals, so the study population had a limited number. Second, it did not include all physicians working in Cyprus. Third, the questionnaire used in this study was prepared by authors, and it was not a validated questionnaire. Fourth, the questionnaire does not include questions about the medical history of the physicians, so it is not possible to evaluate the effect of the comorbidities on the vaccination rates.
This study shows that physicians still have doubts and lack awareness about influenza and pneumococcal vaccination. As the health care professionals are the key to successful community immunization programs, they must be well aware of the guidelines about it. Policymakers should consider setting up training programs about adult immunization that would cover all clinicians, particularly the GP in primary care.
Although influenza vaccine and the effect of vaccine in reducing the incidence of infection are well known among physicians, the pneumococcal vaccine is not. This is especially true for GP. It is suggested that the training about vaccination for both specialists and GP is important for preventive medicine.
MAIN POINTS.
Most of the physicians have knowledge gaps about both their occupational and certain patients’ risks for influenza and pneuomococcal infections.
General practitioners and specialists have differences betweeen the attitude and knowledge level about vaccination.
As physicians are the key to successful community immunization programmes, they should be well aware of the adult vaccination guidelines.
A particular attention has to be given to continuous training programmes on adult vaccination.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of the University of Kyrenia.
Informed Consent: Verbal informed consent was obtained from the physicians who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - E.Ü.E.; Design - E.Ü.E.; Supervision - F.Y.; Resources - S.B.Ö.; Data Collection and/or Processing - H.E.; Analysis and/or Interpretation - S.A.B.; Literature Search - Z.Ö.Y.; Writing Manuscript - E.Ü.E.; Critical Review - F.Y.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES
- 1.Ridda I, Lindley IR, Gao Z, et al. Differences in attitudes, beliefs and knowledge of hospital health care workers and community doctors to vaccination of older people. Vaccine. 2008;26:5633–40. doi: 10.1016/j.vaccine.2008.07.070. [DOI] [PubMed] [Google Scholar]
- 2.Gilchrist SA, Nanni A, Levine O. Benefits and Effectiveness of Administering Pneumococcal Polysaccharide Vaccine with Seasonal Influenza Vaccine: An Approach for Policymakers. Am J Public Health. 2012;102:596–605. doi: 10.2105/AJPH.2011.300512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Immunization Survey-Flu (NIS-Flu) and Behavioral Risk Factor Surveillance System (BRFSS) Flu Vaccination Coverage, United States, 2014–15 Influenza Season. [Accessed date: November 2015]. Available from: http://www.cdc.gov/flu/fluvaxview/coverage-1415estimates.htm.
- 4.Williams WW, Lu PJ, O’Halloran A, et al. Vaccination coverage among adults, excluding influenza vaccination-United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;64:95–102. [PMC free article] [PubMed] [Google Scholar]
- 5.Satman I, Akalin S, Cakir B, et al. The diaVAX Study Group. The effect of physicians’ awareness on influenza and pneumococcal vaccination rates and correlates of vaccination in patients with diabetes in Turkey: an epidemiological Study “diaVAX”. Hum Vaccin Immunother. 2013;9:2618–26. doi: 10.4161/hv.25826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klett-Tammen CJ, Krause G, von Lengerke T, Castell S. Advising vaccinations for the elderly: a cross-sectional survey on differences between general practitioners and physician assistants in Germany. BMC Fam Pract. 2016;17:98. doi: 10.1186/s12875-016-0502-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Durando P, Alicino C, Dini G, et al. Determinants of adherence to seasonal influenza vaccination among healthcare workers from an Italian region: results from a cross-sectional study. BMJ Open. 2016;6:e010779. doi: 10.1136/bmjopen-2015-010779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schneeberg A, Bettinger JA, McNeil S, et al. Knowledge, attitudes, beliefs and behaviours of older adults about pneumococcal immunization, a Public Health Agency of Canada/Canadian Institutes of Health Research Influenza Research Network (PCIRN) investigation. BMC Public Health. 2014;14:442. doi: 10.1186/1471-2458-14-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thompson WW, Weintraub E, Dhankhar P, et al. Estimates of US influenza-associated deaths made using four different methods. Influenza Other Respir Viruses. 2009;3:37–49. doi: 10.1111/j.1750-2659.2009.00073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thompson WW, Shay DK, Weintraub E, et al. Influenza-Associated Hospitalizations in the United States. JAMA. 2004;292:1333–40. doi: 10.1001/jama.292.11.1333. [DOI] [PubMed] [Google Scholar]
- 11.Fiore AE, Shay DK, Broder K, et al. Centers for Disease Control and Prevention (CDC) Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2009;58:1–52. [PubMed] [Google Scholar]
- 12.Brundage JF, Shanks GD. Deaths from bacterial pneumonia during 1918–19 influenza pandemic. Emerg Infect Dis. 2008;14:1193–9. doi: 10.3201/eid1408.071313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bryant KA, Stover B, Cain L, et al. Improving influenza immunization rates among healthcare workers caring for high-risk pediatric patients. Infect Control Hosp Epidemiol. 2004;25:912–7. doi: 10.1086/502319. [DOI] [PubMed] [Google Scholar]
- 14.Chalmers JD, Campling J, Dicker A, et al. A systematic review of the burden of vaccine preventable pneumococcal disease in UK adults. BMC Pulm Med. 2016;16:77. doi: 10.1186/s12890-016-0242-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maltezou HC, Poland GA. Vaccination policies for healthcare workers in Europe. Vaccine. 2014;32:4876–80. doi: 10.1016/j.vaccine.2013.10.046. [DOI] [PubMed] [Google Scholar]
- 16.Alicino C, Iudici R, Barberis I, et al. Influenza vaccination among healthcare workers in Italy. Hum Vaccin Immunother. 2015;11:95–100. doi: 10.4161/hv.34362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnson DR, Nichol KL, Lipczynski K. Barriers to adult immunization. Am J Med. 2008;21:S28–35. doi: 10.1016/j.amjmed.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 18.Song JY, Cheong HJ, Heo JY, et al. Outpatient-Based Pneumococcal Vaccine Campaign and Survey of Perceptions about Pneumococcal Vaccination in Patients and Doctors. Yonsei Med J. 2013;54:469–75. doi: 10.3349/ymj.2013.54.2.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haridi HK, Salman KA, Basaif EA, et al. Influenza vaccine uptake, determinants, motivators, and barriers of the vaccine receipt among healthcare workers in a tertiary care hospital in Saudi Arabia. J Hosp Infect. 2017;96:268–75. doi: 10.1016/j.jhin.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 20.Desiante F, Caputi G, Cipriani R, et al. Assessment of coverage and analysis of the determinants of adherence to influenza vaccination in the general practitioners of Taranto. Ann Ig. 2017;29:256–63. doi: 10.7416/ai.2017.2157. [DOI] [PubMed] [Google Scholar]
- 21.Çiftci F, Şen E, Demir N, et al. Beliefs, attitudes, and activities of healthcare personnel about influenza and pneumococcal vaccines. Hum Vaccin Immunother. 2018;14:111–7. doi: 10.1080/21645515.2017.1387703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nitsch-Osuch A, Brydak LB. Influenza vaccinations of health care personnel. Med Pr. 2013;64:119–29. doi: 10.13075/mp.5893/2013/0011. [DOI] [PubMed] [Google Scholar]
- 23.Millner VS, Eichold BH, Franks RD, et al. Influenza vaccination acceptance and refusal rates among health care personnel. South Med J. 2010;103:993–8. doi: 10.1097/SMJ.0b013e3181eda3d5. [DOI] [PubMed] [Google Scholar]
- 24.ACIP Adult Immunization Work Group; Bridges CB, Woods L, Coyne-Beasley T Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP) recommended immunization schedule for adults aged 19years and older--United States, 2013. MMWR Suppl. 2013;62:9–19. [PubMed] [Google Scholar]


