Abstract
Slipping rib syndrome is a commonly missed diagnosis of upper abdominal pain. It results from hypermobility of the anterior rib due to the disruption of the interchondral ligaments, most likely secondary to repetitive motions or some inciting event. The hypermobility leads to impingement of the intercostal nerves resulting in significant pain.
A 10-year-old adolescent male child was evaluated for 4 months of intermittent, left-sided, upper abdominal pain following a wrestling injury. His paediatrician referred him for further evaluation after a negative workup given the patient was still having intermittent bouts of short-lasting pain that would spontaneously resolve. Physical examination demonstrated a positive hooking manoeuvre with associated swelling and prominence over the lower left ribs.
In conclusion, a broad differential diagnosis, thorough clinical examination, and knowledge of slipping rib syndrome are important to appropriately diagnose and treat patients symptoms.
Keywords: slipping rib syndrome, pediatric, abdominal pain, chest pain, hooking maneuver, dynamic ultrasound
Background
Introduction
Slipping rib syndrome is caused by hypermobility of the anterior false ribs due to the disruption of the interchondral fibrous attachments. This disruption permits the costal cartilage tips to subluxate and impinge on the intercostal nerves passing along the undersurface of the adjacent rib, resulting in severe pain.1 Slipping rib syndrome is a rare cause of abdominal and/or lower chest pain that is often overlooked, underdiagnosed or misdiagnosed.
Majority of healthcare personnel are not aware of this diagnosis and therefore, patients end up undergoing years of debilitating pain, unnecessary testing and radiographic exposure. This paper reports a case of slipping rib syndrome in a 10-year-old male wrestler with the purpose of focusing on appropriate differential diagnosis and clinical examination to reach the correct diagnosis and management so that debilitating pain, unnecessary testing and anxiety can be avoided.
Case presentation
Case report
A 10-year-old active male child, with no known medical history, presents to the outpatient office accompanied by his parents for evaluation of left-sided upper abdominal pain. His paediatrician initially conducted an appropriate workup, including a negative X-ray, then referred the patient for further evaluation as he was still dealing with intermittent bouts of short-lasting severe pain. The patient reports that this problem had been going on for 4 months.
He reports the pain began as a result of a wrestling match in which he fell and his opponent landed onto his chest. He states having a sudden onset of pain at that time and described it as sharp and jabbing. The pain gradually settled down and he continued to wrestle the following day. Since then, the patient has had multiple intermittent episodes of a similar type of pain lasting up to 1 hour. He did not have any pain at the time of the office visit. He had a negative review of systems.
Physical examination revealed a well-developed well-nourished adolescent male child in no acute distress. His vital signs were within normal limits. The examination of his chest and abdomen were unremarkable, with the exception of a positive hook test on the left lower rib cage and associated swelling and prominence (figure 1). The positive hook test was demonstrated with both pain, and most importantly, movement of the cartilage against the adjacent cartilage. There was no tenderness over his rib cage and costal margins. Otherwise, his abdomen had no ecchymosis, tenderness or palpable masses. The use of a diagnostic dynamic ultrasound was discussed with parents, however, they declined and opted to pursue only if the pain persisted.
Figure 1.

Clinical image of patient abdomen with lower costal margins demarcated bilaterally. Swelling and prominence is noted on the left inferior costal margin.
Given the patient’s symptoms and physical examination findings, he was diagnosed with slipping rib syndrome. The patient and his parents were both educated on the pathophysiology of the disease. Reassurance of the benign nature of the disease was provided. Treatment was aimed at conservative management including activity modification, ice and non-steroidal anti-inflammatory drugs (NSAIDs). It was explained that if symptoms worsened or became a persistent issue, a referral for an intercostal nerve block would be recommended. As of the time of this writing, the patient has yet to follow-up.
Outcome and follow-up
Given a reassuring physical examination and diagnosis, the patient and his parents were relieved to know that surgery was not required. They opted to undergo conservative treatment including activity modification, ice and NSAIDs. Considering the patient is young and active in sports, they were notified of the possibility of recurrent symptoms secondary to trauma or an inciting event. As of the time of this writing, the patient has not suffered any recurrent episodes of slipping rib syndrome. He does continue to remain active and live a normal life. They will pursue conservative treatment modalities and follow-up if any issues arise.
Discussion
Slipping rib syndrome is an uncommon, but recognised, cause of recurrent lower chest or upper abdominal pain. Other names in the literature for this syndrome include rib tip syndrome, slipping rib cartilage syndrome, twelfth rib syndrome, clicking rib syndrome, painful rib syndrome, gliding ribs, displaced ribs, intercostal subluxation, traumatic intercostal neuritis, cyriax syndrome and nerve ripping.2
The pathophysiology of this syndrome is explained by the hypermobility of the false ribs. Unlike ribs 1 through 7 that attach directly to the sternum, the 8th, 9th and 10th ribs are indirectly attached via the adjacent cartilage (figure 2).3 Given this unique anatomy, there is increased mobility and greater susceptibility to trauma.
Figure 2.
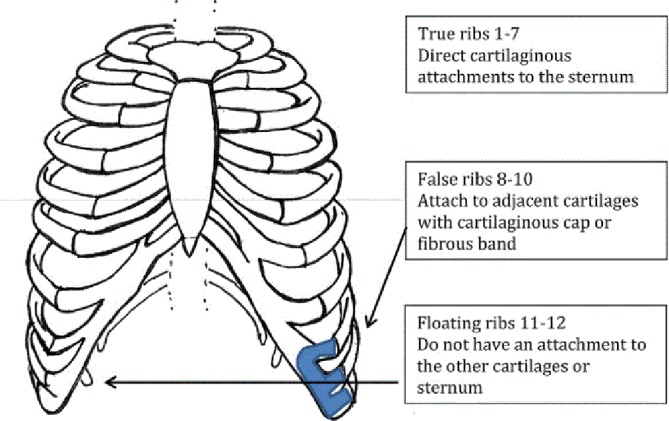
Rib chest wall anatomy.6
Additionally, each rib is attached by various ligaments including sternocostal (rib sternum), costochondral (rib cartilage) and costovertebral/costotransverse (rib vertebrae). When the rib intermittently slips out of place, these ligaments become stretched leading to an increased propensity of laxity and repetitive subluxation. This can manifest as periodic episodes of the lower chest/upper abdominal pain.3 The loose ribs may also impinge on the intercostal nerves, causing excruciating pain around the chest and into the back (figure 3).
Figure 3.
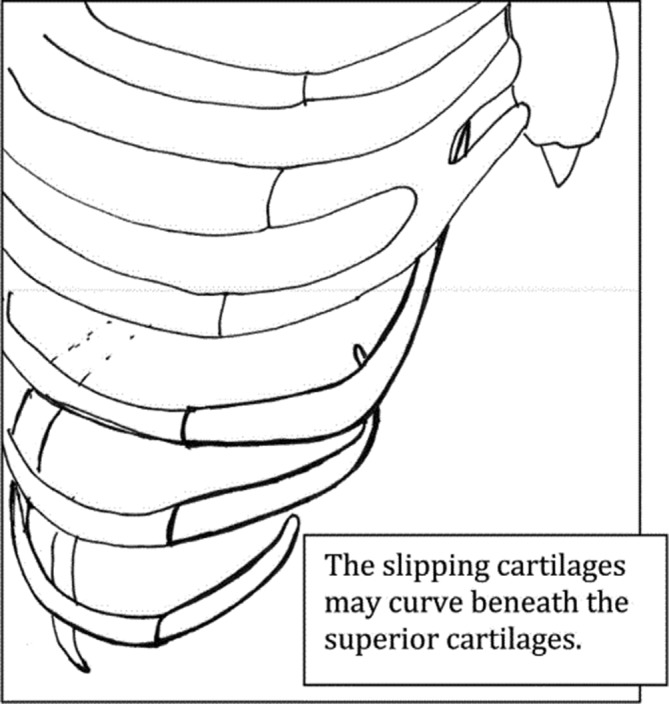
Image of right chest wall depicting slippage of the 8th, 9th and 10th costal cartilage.6
Slipping rib syndrome was first described by Cyriax, in 1919, as a non-visceral source of abdominal pain.4 5 Despite its awareness and publications in the literature today, it remains underdiagnosed or misdiagnosed by many medical professionals. The prevalence is believed to be 1% to 5%, however, this could be an underestimation.2
There are several reasons why this syndrome is commonly underdiagnosed or misdiagnosed. First, slipping rib syndrome is often a diagnosis of exclusion, therefore, many physicians conduct a prolonged workup with consequent waiting time. Second, slipping rib syndrome is not taught in clinical training. Consequently, physicians are inexperienced and unfamiliar with the diagnosis thus, they do not consider it a possible cause of pain. Third, physicians may tend to view these patients complaints as part of a psychological disorder. Fourth, there is a lack of an established algorithm to approach the diagnosis of unexplained abdominal or chest pain. Fifth, patients with slipping rib syndrome can present differently, making it difficult to pinpoint a classic presentation. Lastly, and most importantly, diagnostic testing is not commonly used to support the clinical findings.2 Although dynamic ultrasound allows for visualisation of the ribs slipping against each other, it is not often used and may not be readily available.6
As mentioned earlier, slipping rib syndrome is an elusive diagnosis. A list of differential diagnoses needs to be considered. The differential list for a patient with upper abdominal and lower chest pain may include cholecystitis, oesophagitis, gastric ulcer, hepatosplenic abnormalities, renal colic, pancreatitis, costochondritis, pleuritic chest pain, intercostal strain, oblique strain, rib fracture, costochondral dislocation, Tietze syndrome and slipping rib syndrome.1
Given the localisation and nature of the patient’s symptoms, the majority of intra-abdominal pathology was ruled out from our differential. The patient’s symptoms were initiated following a traumatic event during a wrestling match. There were no associated intra-abdominal symptoms such as nausea, vomiting, diarrhoea or constipation. Additionally, the symptoms were intermittent, only lasting approximately 1 hour in duration before returning to his normal state. Lastly, his physical examination was unremarkable except for reproducible pain and movement of the cartilage with the hooking manoeuvre. Our differential was now focused on musculoskeletal pathologies as a cause of the patient’s pain.
Considering that the patient’s pain was intermittent, occurring multiple times over the course of 4 months, it was believed that the cause could not have been a rib fracture, costochondral dislocation, intercostal strain or Tietze syndrome. Physical examination findings to support this include no tenderness to palpation over the ribs or costochondral junction. The patient only had a positive hook test which caused a reproducible pain and a palpable subluxation.
Due to the lack of knowledge and appropriate diagnostic methods, slipping rib syndrome has become difficult to properly diagnose. The first step involves a thorough history. History typically involves intermittent pain localised to the lower rib cage that is worse with particular movements. Given these are the typical symptoms, one should not ignore the diagnosis if a patient presents atypically. The exact aetiology of this syndrome is unknown, however, it is believed that overuse, trauma or some inciting event to the chest wall can precipitate the syndrome by disrupting the fibrous attachments of the ribs.
The best physical examination test for slipping rib syndrome was described in 1977 by Heinz and Zavala as the hooking manoeuvre.6 7 The physician places his fingers under the lower costal margin, on the side of concern. The physician then moves his hands anteriorly and superiorly (figure 4). A positive test reproduces the patient’s pain along with a palpatory subluxation. One can further confirm the diagnosis of slipping rib syndrome by administering an intercostal nerve block, which relieves the pain and prevents the reproduction of pain via the hooking manoeuvre.
Figure 4.

Hooking manoeuvre.3.
Management of slipping rib syndrome depends on the severity of the patients symptoms. All patients should be provided with reassurance and education of the benign syndrome. Often times, this provides enough satisfaction so that patients can cope with the pain knowing it is not serious or life-threatening. Patients with mild pain can follow conservative measures such as activity modification, ice packs and NSAIDs. Those with moderate pain can have an intercostal nerve block with local anesthetic±corticosteroid for relief of symptoms. Lastly, those with severe pain or refractory cases to conservative management can undergo surgical resection of the anterior rib and costal cartilage (figure 5).6 The outcomes of both conservative and surgical management have been shown to be favourable.8
Figure 5.
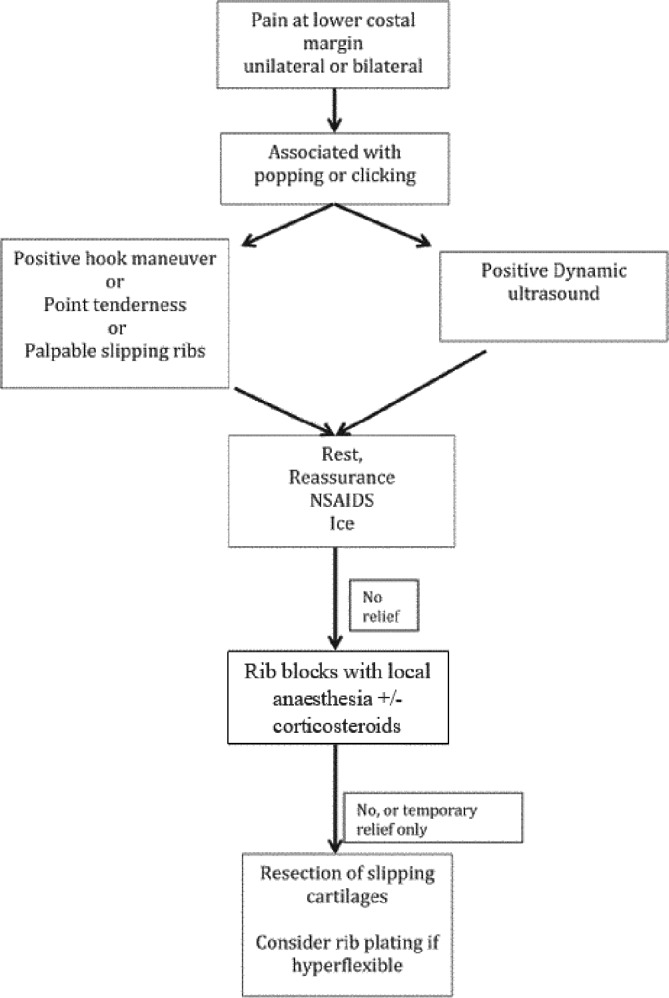
Algorithm for the evaluation, diagnosis and treatment of slipping rib syndrome.6 NSAID, non-steroidal anti-inflammatory drug.
Learning points.
Knowledge of slipping rib syndrome is important when assessing a patient with prolonged lower chest or upper abdominal pain of unknown cause.
As it is a commonly missed diagnosis of upper abdominal pain, many cases have been reported of patients suffering from pain and discomfort for months to years without an established diagnosis.
One should suspect slipping rib syndrome in a patient with intermittent lower chest or upper abdominal pain following an inciting event.
Adopting a robust method of assessing patients include history taking, clinical examinations and putting together a strong differential diagnosis which can significantly help with the investigation and management plan of their chief complaint.
Appropriately diagnosing this patient has led to avoidance of chronic complaints, unnecessary interventions, radiographic exposure and medication abuse.
Footnotes
Contributors: IC: design, revision and final approval; provided the basis of the patient’s information given he was the treating physician. QC: developed the paper with feedback and revisions from the primary author.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Parental/guardian consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. van Delft EAK, van Pul KM, Bloemers FW. The slipping rib syndrome: a case report. Int J Surg Case Rep 2016;23:23–4. 10.1016/j.ijscr.2016.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bolaños-Vergaray JJ, de la Gala García F, Obaya Rebollar JC, et al. Slipping Rib Syndrome as Persistent Abdominal and Chest Pain: A & A Case Reports 2015;5:167–8. [DOI] [PubMed] [Google Scholar]
- 3. Turcios NL. Slipping rib syndrome in an adolescent: an elusive diagnosis. Clin Pediatr 2013;52:879–81. 10.1177/0009922812469290 [DOI] [PubMed] [Google Scholar]
- 4. Saltzman DA, Schmitz ML, Smith SD, et al. The slipping rib syndrome in children. Paediatr Anaesth 2001;11:740–3. 10.1046/j.1460-9592.2001.00754.x [DOI] [PubMed] [Google Scholar]
- 5. Cyriax EF. On various conditions that may simulate the referred pains of visceral disease, and a consideration of these from the point of view of cause and effect. Practitioner 1919;102:314–22. [Google Scholar]
- 6. McMahon LE. Slipping rib syndrome: a review of evaluation, diagnosis and treatment. Semin Pediatr Surg 2018;27:183–8. 10.1053/j.sempedsurg.2018.05.009 [DOI] [PubMed] [Google Scholar]
- 7. Heinz GJ, Zavala DC. Slipping rib syndrome. JAMA 1977;237:794–5. 10.1001/jama.1977.03270350054023 [DOI] [PubMed] [Google Scholar]
- 8. Khan NAJ, Waseem S, Ullah S, et al. Slipping rib syndrome in a female adult with longstanding intractable upper abdominal pain. Case Rep Med 2018;2018:1–3. doi:0.1155/2018/7484560 [DOI] [PMC free article] [PubMed] [Google Scholar]


