Abstract
This case report presents an elderly male patient who on diagnosis with a large oropharyngeal tumour had no specific symptomatology apart from severe obstructive sleep apnoea. Histopathology revealed the tumour to be an adult rhabdomyoma, a rare but benign tumour arising from striated muscle cells. The tumour obstructed most of the oropharyngeal space and almost occluded the patient’s airway when lying in a supine position. The patient was deemed operable, and the tumour was excised in toto using a transoral robotic surgery system. On follow-up, the patient had a severe reduction of apnoeas/hypopnoeas and felt subjectively ‘reborn’. This is to our knowledge the first case where an adult rhabdomyoma is removed using a robot-assisted approach, thus presenting a new and viable option when considering removal of benign tumours of the pharynx leading to a very minor degree of morbidity for the patients.
Keywords: ear, nose and throat; sleep disorders (respiratory medicine); head and neck surgery; otolaryngology / ENT
Background
We report an interesting case of a man presenting with symptoms of severe obstructive sleep apnoea (OSA) and where the examination revealed a rare oropharyngeal tumour, which contributed significantly to the primary symptoms.
OSA is a disease affecting an increasingly large amount of individuals worldwide. Obstruction of the upper airway during sleep causes recurrent hypopnoeas and apnoeas, which in turn leads to microarousals and sleep disturbance. In addition to day time sleepiness, the condition is associated with a number of adverse long-term health effects including diabetes and cardiovascular disease.1 2 There are multiple contributing factors leading to OSA, of which excessive weight, age and a narrow upper airway are most common.3–5 Tumours in the upper airway are rarely the cause of OSA, with only few reported cases found throughout the published literature.
In this report, we present a rare cause of severe OSA: an adult rhabdomyoma (AR) in the base of tongue, causing semiocclusion of the oropharyngeal space.
Case presentation
The patient, an otherwise healthy 68-year-old man, first presented at his general practitioner due to night-time snoring, observed apnoeas and excessive daytime sleepiness. Symptoms were progressing throughout a period of 2–3 years. An estimated Epsworth scale degree of 16 points corresponded with a severe likelihood of having sleep apnoea. Blood biochemistry and ECG as well as vital parameters were all within normal ranges. The patient had a body mass index of 27.8, corresponding with slight overweight.
In previous years, the patient had been a heavy smoker, smoking 20–30 cigarettes a day for approximately 30 years ceasing at the age of 50 years. He had no excessive alcohol consumption at any point in life. Neither were there reports of unintended weight loss or excessive nightly sweats. On referral to the otorhinolarygological specialist, the patient also complained of fullness in the throat, however, denying dysphagia, wakeful respiratory problems or pain. No additional symptoms were reported by the patient. The initial examination revealed a large submucosal tumour protruding from the base of tongue on the right side, significantly reducing the pharyngeal space (figure 1). When the patient was in supine position, the tumour receded to cover the uppermost part of the hypopharynx as well as the laryngeal aditus. A sleep apnoea evaluation yielded an Apnea–Hypopnea Index (AHI) of 52.4 indicating severe sleep apnoea (52 apnoea or hypopnoea events per hour).
Figure 1.

Photo of the tumour from the primary clinical examination.
Investigations
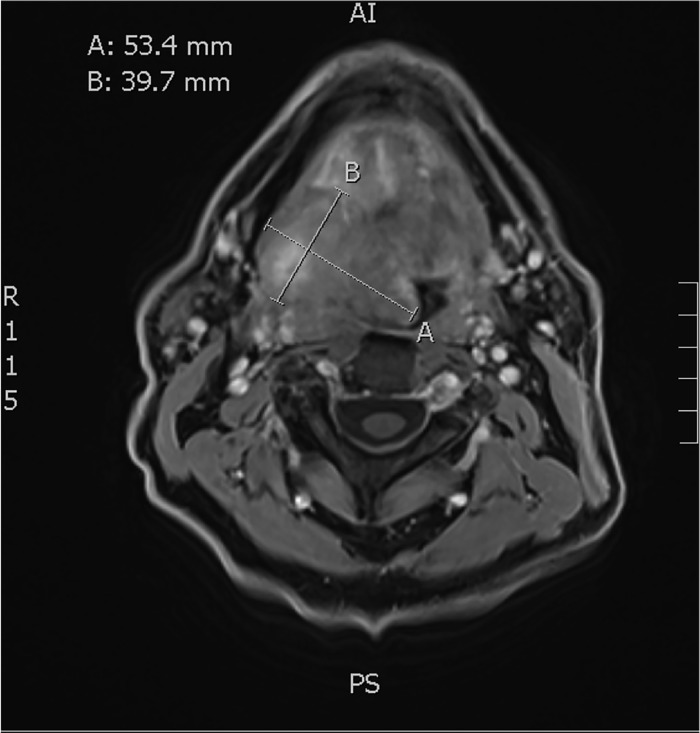
The patient was referred to a tertiary hospital for further evaluation of the oropharyngeal tumour, primarily to rule out malignancy. MRI of the neck revealed a large, inhomogeneous tumour in the base of tongue on the right side, extending into the ipsilateral tonsillar fossa, deep into the extrensic musculature of the tongue and significantly protruding into the oropharyngeal and hypopharyngeal space causing subtotal occlusion. The tumour was well demarcated, measuring 40×63×53 mm (figure 2). No signs of invasion or dissemination were found. Supplementary work-up including CT of the thorax and blood work revealed no associated pathology. Evaluation under anaesthesia including biopsy was performed. Due to not having a setup for drug-induced sleep endoscopy (DISE), this was not performed. Due to potential difficulty in securing an airway, safety measures regarding airway management were taken. Clinically, the tumour was found to involved the entire right half of the base of tongue, extending deep into the musculature and with significant protrusion into the pharyngeal space. It appeared soft and mobile, and the overlying mucosa was intact and appeared normal. Exposure of the oropharynx was good, and the patient was deemed operable and eligible for transoral robotic surgery (TORS) based on preoperative evaluation by a TORS surgeon.
Figure 2.
MRI from primary diagnosis. Coronal view. Tumour marked and measured.
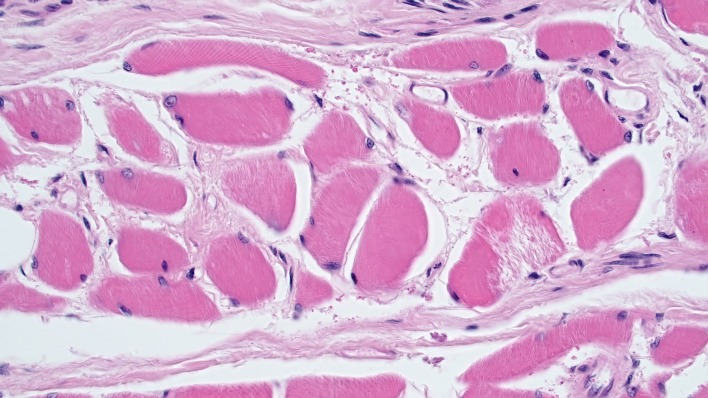
Histopathology based on biopsy of the tumour showed AR consisting of a homogenous collection of tightly packed, cross-sectioned, round striated muscle cells. All nuclei were round with coarse chromatin and slightly granulated cytoplasm. Surrounding the tumour was a thick fibrous capsule with no malignant infiltration in the surrounding tissues. The outermost layer was covered in well-defined non-keratinised epithelium (figure 3).
Figure 3.
Histopathology with H&E colouring showing striated muscle cells. No dysplasia of malignant infiltration.
Differential diagnosis
Although the clinical appearance of the tumour indicated a benign condition, the diagnostic work up was accelerated on order to quickly establish diagnosis and rule out cancer, that is, lymphoma, salivary gland tumour and squamous cell carcinoma.
Treatment
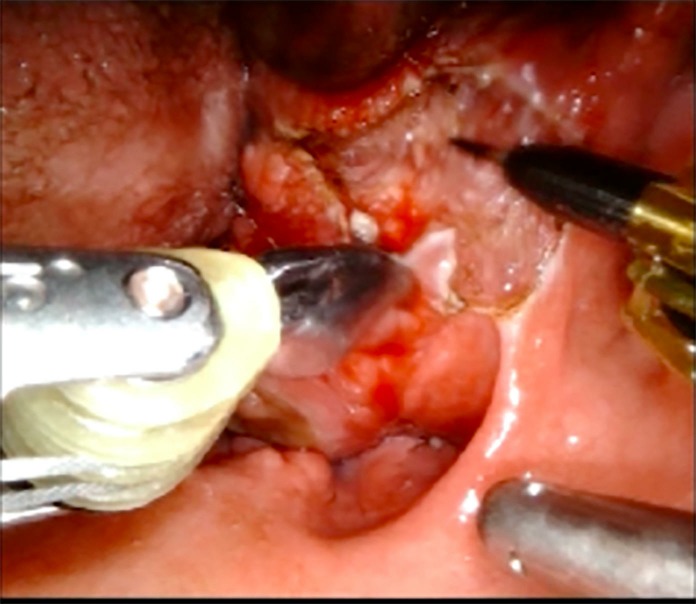
Definite treatment of AR is surgical. Thus, a surgical excision was planned. Despite the significant size of the tumour and its deep extension into the extrinsic musculature to the base of tongue, it was considered resectable by TORS, based on previous assessments. This would allow a minimal invasive approach without splitting the lip, tongue and mandible. A surgical robot, DaVinci Xi (Intuitive Surgical) was used. Endo-wrist instruments (Maryland and monopolar spatula) combined with a 30° dual endoscope and adequate access by a mouth gag (FK-WO-retractor) enabled good exposure and full manoeuvrability in the operative field. The tumour was excised with close but macroscopically adequate margins (figure 4). Only minor bleeding was encountered, and the lingual artery could be spared. The tumour was excised along with the right base of tongue and tonsillar fossa, and the wound left to heal by secondary intention. The patient could be extubated immediately following surgery and returned to the ward on the same day. On the third day postoperative, the patient was discharged. Swallowing ability was good, based on a functional evaluation of swallowing test, thus a nasogastric tube was not found necessary.
Figure 4.
Peroperative photo from TORS resection. Tumour partially resected. TORS, transoral robotic surgery.
Outcome and follow-up
The patient quickly returned to a normal oral diet having no complaints of dysphagia or aspiration. There were no postoperative complications. Sleep evaluations were performed 14 days and 2 months after surgery, showing a significant fall in AHI to 37.2. This led to CPAP (continuous positive airway pressure) treatment with good effect as airview showed no more obstructive apnoeas, but 12 central apnoeas that did not require treatment. Subjectively, the patient reported sleeping better than ever and the feeling of being ‘reborn’.
Transnasal endoscopy performed 1 month postoperatively showed full restitution with only minimal scarring, normal mobility of the base of tongue and practically normal anatomy.
Discussion
Rhabdomyomas are rare but histologically well described. Traditionally, they are divided into fetal type and adult type and further subdivided based on origin: cardiac and extracardiac. The extracardiac ARs are mostly present in the head and neck area; however, genital types also occur.6–9
Using the PubMed database, a search was conducted using MeSH words ‘Rhabdomyoma’ AND ‘Head and Neck Neoplasms’, which yielded 251 results. Of these, 67 articles were ruled out as ‘not relevant’ (ie, fetal type rhabdomyoma, rhabdomyomas located in another species) and 88 articles were unavailable for full text due to either age or solely published in a non-English language journal. Based on the remaining articles, the majority being case reports, AR is described in relation to the larynx, pharynx, oral cavity and different levels of the neck. However, AR evolving from the tongue/tongue base is definitively a rarity. There are only a few publications presenting AR in the pharyngeal region and associated with OSA. Farboud et al reported on a case of OSA caused by AR in the supraglottic larynx. The tumour could not be completely removed and was thus debulked by transoral laser surgery, which would imply a significant risk of recurrence of symptoms.10 11 Boysen et al 11 reported a case of AR in the anterior tongue, which was treated by external debridement. Cuesta Gil et al 12 reported a simular case to ours in 2000, namely an AR at the base of tongue causing dysphagia and OSA. The tumour was, however, removed using a midline tongue split. This procedure, although effective, is associated with significant discomfort, delayed healing and longterm morbidity. Apart from TORS, another relatively novel approach is transoral ablation. This is also considered less invasive than traditional open surgery. A case using this approach was reported by Karaman et al 13 in 2009, treating an AR of the tonsillar fossa measuring 9×5×3 cm.
Thus, the surgical approach using TORS in treating this kind of airway obstructing tumour represents a modern and minimally invasive approach but additionally also shows a lot of promise in the future treatment of OSA in general.14
A limitation in this study is the lack of a performed DISE study on the patient. Since DICE represents a promising but still somewhat debated way of targeting specific surgical procedures, it would have been a valuable addition in the examination of the patient as he then could have been evaluated using standard NOHL and VOTE scoring systems.15 Unfortunately, a DISE set-up was not available at the hospital at the point of diagnosis and treatment.
This is, to our knowledge, the first reported case of AR localised at the base of tongue fully removed in toto using TORS with verified considerable effect on a patients OSA.
Learning points.
Transoral robotic surgery is a viable surgical option and may, if available, be preferential to transoral manual surgical approaches when dealing with benign tumours in the oro/hypopharynx.
Thorough clinical examination is important in all patients with obstructive sleep apnoea, as the underlying cause is not always obvious.
Adult rhabdomyoma is a rare but benign tumour and should be considered in patients with relatively asymptomatic exophytic tumours in the head and neck area.
Careful planning of anaesthetic procedure is important in patients with severe and very severe obstructive sleep apnoea regardless of the cause.
Acknowledgments
The authors would like to acknowledge the doctors Steen Bærentzen og Mette Bak Brogaard from the Department of Pathology at Aarhus University hospital for providing the histopathological diagnosis and images.
Footnotes
Contributors: All registered authors contributed significantly in the production of this case report. All authors have approved the submitted draft. The corresponding author HJM has written and finalised the main text including learning objectives. JB was the primary examining clinician and in-hospital director of sleep medicine. PO did the initial direct laryngoscopy and biopsy and contributed to the transoral robotic surgery (TORS) operability assessment as well as obtained the patient consent. TK is the in-hospital primary TORS surgeon, finalised the operability assessment and facilitated the resection of the tumour as well as contributed with the TORS specific details in the 'treatment' section of the article.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Reutrakul S, Mokhlesi B. Obstructive sleep apnea and diabetes: a state of the art review. Chest 2017;152:1070–86. 10.1016/j.chest.2017.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Maeder MT, Schoch OD, Rickli H. A clinical approach to obstructive sleep apnea as a risk factor for cardiovascular disease. Vasc Health Risk Manag 2016;12:85–103. 10.2147/VHRM.S74703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Guilleminault C, Sullivan SS, Huang Y-S. Sleep-Disordered breathing, orofacial growth, and prevention of obstructive sleep apnea. Sleep Med Clin 2019;14:13–20. 10.1016/j.jsmc.2018.11.002 [DOI] [PubMed] [Google Scholar]
- 4. Tham KW, Lee PC, Lim CH. Weight management in obstructive sleep apnea: medical and surgical options. Sleep Med Clin 2019;14:143–53. 10.1016/j.jsmc.2018.10.002 [DOI] [PubMed] [Google Scholar]
- 5. Semelka M, Wilson J, Floyd R. Diagnosis and treatment of obstructive sleep apnea in adults. Am Fam Physician 2016;94:355–60. [PubMed] [Google Scholar]
- 6. Winther LK. Rhabdomyoma of the hypopharynx and larynx. Report of two cases and a review of the literature. J Laryngol Otol 1976;90:1041–51. 10.1017/s0022215100083092 [DOI] [PubMed] [Google Scholar]
- 7. Tanner NS, Carter RL, Clifford P. Pharyngeal rhabdomyoma: an unusual presentation. J Laryngol Otol 1978;92:1029–36. 10.1017/S002221510008645X [DOI] [PubMed] [Google Scholar]
- 8. Wyatt RB, Schochet SS, McCormick WF. Rhabdomyoma. light and electron microscopic study of a case with intranuclear inclusions. Arch Otolaryngol 1970;92:32–9. 10.1001/archotol.1970.04310010058006 [DOI] [PubMed] [Google Scholar]
- 9. Willis J, Abdul-Karim FW, di Sant'Agnese PA. Extracardiac rhabdomyomas. Semin Diagn Pathol 1994;11:15–25. [PubMed] [Google Scholar]
- 10. Farboud A, Pratap R, Helquist H, et al. An unusual cause of obstructive sleep apnoea. J Laryngol Otol 2009;123:e22 10.1017/S0022215109990910 [DOI] [PubMed] [Google Scholar]
- 11. Boysen M, Scott H, Hovig T, et al. Rhabdomyoma of the tongue. Report of a case with light microscopic, ultrastructural and immunohistochemical observations. J Laryngol Otol 1988;102:1185–8. 10.1017/s0022215100107674 [DOI] [PubMed] [Google Scholar]
- 12. Cuesta Gil M, Fernández-Alba Luengo J, Navarro Vila C. Rhabdomyoma of the base of the tongue. A case report. Int J Oral Maxillofac Surg 2000;29:136–7. [PubMed] [Google Scholar]
- 13. Karaman E, Saritzali G, Ozcora E. Rhabdomyoma of the tonsillar fossa. J Craniofac Surg 2009;20:1207–9. 10.1097/SCS.0b013e3181acdd48 [DOI] [PubMed] [Google Scholar]
- 14. Vicini C, Montevecchi F. Transoral robotic surgery for obstructive sleep apnea: past, present, and future. Sleep Med Clin 2019;14:67–72. 10.1016/j.jsmc.2018.10.008 [DOI] [PubMed] [Google Scholar]
- 15. Meraj TS, Muenz DG, Glazer TA, et al. Does drug-induced sleep endoscopy predict surgical success in transoral robotic multilevel surgery in obstructive sleep apnea? Laryngoscope 2017;127:971–6. 10.1002/lary.26255 [DOI] [PubMed] [Google Scholar]