Abstract
Encephaloceles are one form of neural tube defect and are associated with partial absence of skull bone fusion, with an incidence of 1–4 cases for every 10 000 live births. We report the case of a neonate born at term, with an antenatal diagnosis of occipital encephalocele, which was successfully managed with excision and formation of a reverse visor scalp flap on day 2 of life.
Surgery was performed in a single stage, involving a multidisciplinary approach between neurosurgery and plastic surgery teams, with wider management involving neonatal intensive care, paediatric, obstetric and anaesthetic teams.
The patient had no early postoperative complications, and we use this case report to demonstrate that a reverse visor scalp flap is a good option to cover full-thickness defects in patients with encephaloceles.
Furthermore, we advocate early repair and a multidisciplinary approach to minimise the morbidity associated with occipital encephaloceles.
Keywords: neurosurgery, plastic and reconstructive surgery, paediatric surgery
Background
Encephaloceles are rare birth defects associated with partial absence of skull bone fusion, resulting in a gap through which cranial contents can protrude.1 They constitute one form of neural tube defects, with the other two being spina bifida and anencephaly.2 The incidence of encephaloceles has been reported as 1–4 cases for every 10 000 live births, with occipital being the most common site (75% of cases).3 Frontoethmoidal (13%–15%), parietal (10%–12%) and sphenoidal are the sites that follow, respectively.3 Anterior encephalocele is particularly prevalent in Southeast Asia, whereas occipital encephalocele is commonly found in the Western world.4 5
Encephaloceles are associated with considerable morbidity and mortality; occipital encephaloceles having the worst prognosis despite preoperative and postoperative interventions.6 Early excision and repair are recommended as it greatly reduces the well-known complications including cerebrospinal fluid (CSF) leak and reduced IQ level.7
Here we report the case of a neonate born at term with an occipital encephalocele diagnosed antenatally, and successfully managed by excision and formation of a reverse visor scalp flap at day 2 of age.
Case presentation
This is the case of a neonate, born at term (38+6 weeks gestation), with a large occipital encephalocele. This was first diagnosed at 17 weeks gestation, by antenatal ultrasound (US). This early anomaly US was offered, as the mother’s obstetric history included a termination of pregnancy at 21 weeks gestation due to fetal unilateral renal agenesis, dysplastic kidney and anhydramnios.
The US showed a large occipital encephalocele with echogenic content, suggesting possible herniation of neural tissue. Discussion was had regarding the prognosis of encephaloceles; the mother was advised that the size of the defect and severity of brain tissue herniation could lead to significant mental and physical disability. As encephaloceles can be associated with chromosomal abnormalities (eg, trisomy 13 or 18) and genetic syndromes (eg, Meckel Gruber syndrome), the option of invasive testing was offered. However, as amniocentesis carries a 1 in 100 risk of miscarriage, the mother declined this and committed to the pregnancy without invasive testing.
Further antenatal scans were conducted throughout the remainder of the mother’s pregnancy. This included fetal MRI at 30 weeks (see figure 1) confirming the encephalocele. A plan was therefore made for the mother to attend hospital at 38 weeks gestation, for an elective Caesarean section and repair of the encephalocele.
Figure 1.

Fetal MRI brain at 30 weeks gestation.
Although initially planned as a Caesarean section, the baby was born at 38 weeks gestation via vaginal delivery with no immediate perinatal problems. Wet gauze and a cling film wrap were used to cover the encephalocele.
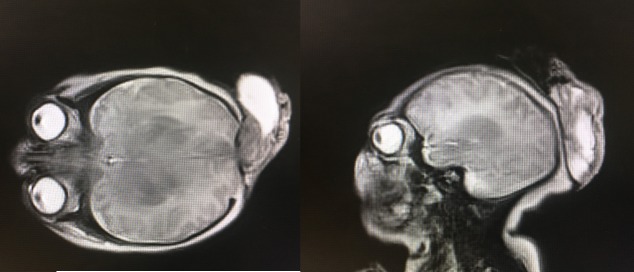
The baby was admitted to neonatal intensive care unit (NICU) as planned, for close monitoring. Repeat MRI head was performed the following morning (see figure 2) to aid preoperative planning. This showed the known occipital encephalocele, microcephaly, bilateral frontal areas of cystic change and multiple cortical malformations. She was subsequently prepared for theatre that afternoon.
Figure 2.
(A) MRI brain at 2 days old (axial view) (B) MRI brain at 2 days old (sagittal view).
Investigations
17 weeks gestation—US.
21 weeks gestation—fetal echocardiogram.
29 weeks gestation—US.
30 weeks gestation—MRI.
Day 2 of life—MRI.
Treatment
At day 2 of life, the patient underwent repair of the occipital encephalocele, measuring 7 cm in diameter.
The neurosurgical team performed the initial part of the procedure. The skin defect was excised from the edges and the dural plane identified from the periphery to the centre of the lesion. The encephalocoele pedicle was found and coagulated, and the encephalocoele excised using bipolar and cutting. A dural patch was applied on top of the dural defect and sutured watertight. Subgaleal dissection was then performed, preserving the pericranium.
The plastic surgery team undertook the second part of the procedure. The 7-cm defect was too small for a simple local flap and therefore a larger local flap was needed. For this reason, the decision was made to form a reverse visor flap. An anterior linear skin incision was initially made to facilitate the formation of the flap. A reverse visor flap was subsequently formed, based on the lateral blood supply of the scalp from both sides (ie, the superficial lateral temporal vessels). The flap was therefore raised keeping the lateral sides attached, with movement of the flap like that of a bucket handle. Both encephalocoele skin defect and the anterior flap defect were brought together with interrupted 3–0 undyed Vicryl (dissolvable) sutures. Interrupted 3–0 Vicryl Rapide (fast dissolving) sutures were used for skin closure. Tissue was recruited in from the temples to aid secondary (donor site) defect closure, which then allowed tissue to be recruited in centrally using the flap to close the primary defect.
The patient returned to NICU post-operatively for ongoing monitoring and was successfully extubated within 24 hours.
Outcome and follow-up
Postoperatively, the baby was kept nil-by-mouth and on intravenous fluids. The next day, a nasogastric (NG) tube was inserted and NG feed was initiated gradually, until she was ready for oral intake.
Due to suspected contamination with meconium following birth, she received 5 days of benzylpenicillin and gentamycin, and 10 days intravenous cefotaxime post encephalocele repair. Blood cultures however revealed no growth. Blood results also showed improvement in inflammatory markers from day 1 of birth to day 1 post-operation (white blood cells 24.55–11.57, neutrophils 17.6–3.55).
The patient spent 3 days in NICU, 1 day in the high dependency unit and 7 days in the neonatal special care unit. She made a good postoperative recovery and after 1 week she was feeding well, active and moving limbs, with normal cranial and peripheral nervous system examinations. Microcephaly was again noted with an occipito-frontal circumference (OFC) of 31 cm. It was advised the baby would likely encounter visual and cognitive challenges later in life.
Genetic testing was performed by array comparative genomic hybridisation analysis of DNA. This showed no significant imbalance and the results were consistent with a normal female chromosome complement.
She was deemed fit for discharge on day 11 of life.
At 3 weeks of age, the patient was seen in the plastic surgery outpatient department. She was reported to be well, with both the encephalocele repair site and the donor site healing well. A small area of scab was noted in the centre of the donor incision, but this was expected to heal over the next week. The mother was advised to bathe the baby normally, moisturise any areas of the wound not yet fully healed and to lay her in any position with enough padding underneath to protect the wound lines.
At 4 weeks of age, she was reviewed by paediatric ophthalmology. Visual evoked potentials suggested probable bilateral post-retinal visual pathway dysfunction but there were no other concerns.
At 2 months of age, she was seen by the neurosurgery team. On assessment, the wound was healing well. Microencephaly was ongoing and OFC was measured at 35.5 cm at birth. On examination, she was moving all four limbs, although slightly hypertonic with sudden jerk movements. Shortly afterwards, she was diagnosed with epilepsy, following a generalised tonic-clonic seizure). Electroencephalography was normal but levetiracetam 35 mg once daily was commenced.
At 4 months of age, she experienced further seizures and levetiracetam was titrated over the next 2 weeks to 125 mg twice daily. At this age, audiology review also demonstrated reduced hearing and the requirement for bilateral hearing aids.
Discussion
The European Surveillance of Congenital Anomalies has reported 484 cases of encephaloceles in Europe from 2013 to 2017; 32% live births, 2% deaths in utero and 66% pregnancies terminated.8 These figures are not insignificant, illustrating the importance of early diagnosis and treatment planning, including sensitive discussion with parents about further management and potential termination of pregnancy.
Although previously considered disorders of neurulation involving anterior neural tube closure, encephaloceles are now viewed as a result of abnormal separation of neural and surface ectoderm, following neural tube closure around the fourth week of the antenatal period.9 Herniation of intracranial contents through the calvarial defect ensues. The herniated contents are non-functioning in most cases, as a result of pathological processes such as calcification, necrosis and gliosis.9 Some of these abnormalities can be identified before birth on fetal MRI, showing involvement of the brainstem, cerebral vessels and white matter pathways.10
Several prognostic factors have been identified that influence outcome in occipital encephaloceles, including the size of the sac, hydrocephaly, contents of the neural tissue and the presence of infection.6 The single most important factor influencing survival has been reported as the absence of brain tissue within the sac.3 These factors can also help determine the degree of cerebral dysfunction, considering that brain tissue not extending into the encephalocele may also be distorted and functionally impaired.9 This, in turn, can guide surgical planning and timing of surgery.
The antenatal diagnosis of encephalocele commonly occurs through US at planned antenatal checks. Recently however, other methods of assessment have been proposed. The use of 3-dimensional US has been suggested to provide additional illustration of the abnormality and to detect fetal encephalocele earlier than traditional 2-dimensional US.11 In addition, amniotic fluid alpha-fetoprotein has been shown to be a reliable yet non-specific marker of open neural tube defects prior to the 26th week of gestation and may be a useful tool in specific cases.12
The treatment aim of encephaloceles is surgical closure of the defect soon after birth.3 Ramdurg et al described a case series of 20 patients, 3 of which presented with rupture of the encephalocele; 1 died due to shock preoperatively and 1 succumbed to meningitis and septic shock post repair.2 The other 17 patients had no immediate surgical mortality; however, 4 of them were complicated by a CSF leak (subsequently improved with conservative management) and 4 were complicated by hydrocephalus (requiring a shunt).2 The authors recommended early surgical repair of the encephalocele to prevent the complications of rupture, neurological deficits and tethering.2 Rehman et al described their case series of 50 patients: preoperative complications of CSF leakage (18%), sac rupture (4%), haemorrhage (2%), hydrocephalus (34%) and seizures (15%). These authors also recommended repair at an early age to reduce morbidity.7
Raja et al meanwhile published a case series of 25 cases and recommended elective surgery where possible, giving patients time to gain weight and the surgeons time to determine the best possible techniques.3
With regard to the technique of scalp wound closure, options for closure of full-thickness scalp defects include skin grafting, local fasciocutaneous flaps and dermal matrices.13 The visor flap is a relatively novel approach to full-thickness defect closure and is a bipedicled advancement flap with a triangular posterior extension.13 Hwang et al presented a case series of 7 patients who underwent wound closure using this novel approach, achieving total complete healing of the recipient site in all patients.13 The authors cited reduced donor site morbidity and avoidance of microsurgical reconstruction as the main advantages of using this method.13
On follow-up of the patient reported in this case study, the surgical repair remained closed and the donor site was healing well, showing the reverse visor scalp flap to be a safe and effective technique.
Furthermore, an expedient multidisciplinary approach was vital to ensure the best possible outcome. Obstetric, neonatal intensive care, anaesthetic, neurosurgery and plastic surgery teams were all heavily involved in the care of our patient. Velho et al also emphasises this need for a multidisciplinary approach in a case series of 54 patients.14 Close multidisciplinary follow-up after surgery is vital and helps improve the quality of life for this cohort postoperatively.15
In conclusion occipital encephalocele is a condition associated with significant morbidity and mortality. Most authors advocate early surgical management of encephaloceles, as exposed cranial contents are an infection risk and are thus a constant threat to life. Multiple options exist for closure of full-thickness scalp defects. Our case report describes a case of occipital encephalocele in a neonate, which was repaired on day 2 of life using a reverse visor scalp flap, without any early postoperative complications. We use this case report to demonstrate that a reverse visor scalp flap may be a good option to cover full-thickness defects in patients with encephaloceles. Furthermore, we advocate a multidisciplinary approach in the management of these patients.
Learning points.
Timely management of patients with encephalocele is vital to reduce morbidity and mortality, as exposed cranial contents are an infection risk and are thus a constant threat to life.
A reverse visor scalp flap may be a good option to cover full-thickness scalp defects, as demonstrated in this case.
A multidisciplinary approach is crucial to the successful management of a patient with encephalocele, both in the perioperative and postoperative period.
Acknowledgments
Many thanks to Cristina Bleil, consultant neurosurgeon, King’s College Hospital London, for reviewing the article.
Footnotes
Contributors: ET researched the case, wrote up the case report, reviewed and edited the article and submitted report. SM conducted the literature review, reviewed and edited the article. NM obtained patient consent, reviewed and edited the article. NC helped to plan the report, reviewed and edited the article.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Parental/guardian consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Fernando J. Synonyms of Encephalocele [Internet]. National Organisation for rare disorders, 2003: 1–6. https://rarediseases.org/rare-diseases/encephalocele/ [Google Scholar]
- 2. Ramdurg SR, Sukanya M, Maitra J. Pediatric encephaloceles: a series of 20 cases over a period of 3 years. J Pediatr Neurosci 2015;10:317–20. 10.4103/1817-1745.174462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Raja RA, Qureshi AA, Memon AR, et al. Pattern of encephaloceles: a case series. J Ayub Med Coll Abbottabad 2008;20:125–8. [PubMed] [Google Scholar]
- 4. Mahapatra AK, Agrawal D. Anterior encephaloceles: a series of 103 cases over 32 years. J Clin Neurosci 2006;13:536–9. 10.1016/j.jocn.2005.05.016 [DOI] [PubMed] [Google Scholar]
- 5. Hoving EW. Nasal encephaloceles. Childs Nerv Syst 2000;16:702–6. 10.1007/s003810000339 [DOI] [PubMed] [Google Scholar]
- 6. Kıymaz N, Yılmaz N, Demir I, et al. Prognostic factors in patients with occipital encephalocele. Pediatr Neurosurg 2010;46:6–11. 10.1159/000314051 [DOI] [PubMed] [Google Scholar]
- 7. Rehman L, Farooq G, Bukhari I. Neurosurgical interventions for occipital encephalocele. Asian J Neurosurg 2018;13:233–7. 10.4103/1793-5482.228549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. EUROCAT EUROCAT Prevalence Data Tables: Encephalocele (per 10,000 births) for the following registries: All Registries, from 2013 - 2017 [Internet] (European surveillance of congenital anomalies), 2017. Available: http://www.eurocat-network.eu/prevdata/resultsPdf.aspx?title=A5&allanom=false&allregf=true&allrega=true&anomalies=5&winx=1416&winy=800
- 9. Crean P, Hicks E. A Practice of Anesthesia for Infants and Children [Internet]. 4th edn Saunders, 2009. https://www.sciencedirect.com/topics/medicine-and-dentistry/encephalocele [Google Scholar]
- 10. Kasprian GJ, Paldino MJ, Mehollin-Ray AR, et al. Prenatal imaging of occipital encephaloceles. Fetal Diagn Ther 2015;37:241–8. 10.1159/000366159 [DOI] [PubMed] [Google Scholar]
- 11. Liao S-L, Tsai P-Y, Cheng Y-C, et al. Prenatal diagnosis of fetal encephalocele using three-dimensional ultrasound. J Med Ultrasound 2012;20:150–4. 10.1016/j.jmu.2012.07.005 [DOI] [Google Scholar]
- 12. Weiss RR, Macri JN, Elligers K, et al. Amniotic fluid alpha-fetoprotein as a marker in prenatal diagnosis of neural tube defects. Obstet Gynecol 1976;47:148–51. [PubMed] [Google Scholar]
- 13. Hwang L, Ford N-K, Spitz J, et al. The Visor flap: a novel design for scalp wound closure. J Craniofac Surg 2017;28:e146–8. 10.1097/SCS.0000000000003332 [DOI] [PubMed] [Google Scholar]
- 14. Velho V, Naik H, Survashe P, et al. Management strategies of cranial encephaloceles: a neurosurgical challenge. Asian J Neurosurg 2019;14:718–24. 10.4103/ajns.AJNS_139_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ugras M, Kavak O, et al. New born children with encephalocele. J Neurol Neurosci 2016;7:1–4. 10.21767/2171-6625.100073 [DOI] [Google Scholar]