Abstract
Amyloidosis is the extracellular deposition of unique protein fibrils in different tissue organs. It is most commonly associated with B-cell malignancy such as multiple myeloma or Waldenstrom macroglobulinaemia. It involves the liver, heart, kidney, peripheral nerves and soft tissues. Liver however is affected, but clinically apparent disease is very rare. Hepatomegaly and mild elevation of alkaline phosphatase is the most common presentation in patients with liver involvement. Acute hepatic failure is a rare presentation with myeloma-induced amyloidosis. The diagnosis can be difficult requiring biopsy or sometimes special staining of the tissue. Management is still very challenging
Keywords: gastroenterology, liver disease, oncology
Background
Hepatic involvement is common in amyloidosis and occurs in myeloma-associated amyloidosis (primary amyloidosis) or amyloid-associated amyloidosis (secondary amyloidosis). Most common presentation is hepatomegaly, mild jaundice and mild-to-normal elevation of alkaline phosphatase. However, clinically significant involvement of liver is very rare. Portal hypertension, subcapsular haematoma and rupture of liver can also occur.1 2 Acute and subacute hepatic failure has been reported in myeloma-associated amyloidosis. Here, we have presented a case of amyloidosis that initially presented with mild elevation of liver function tests (LFTs) and subsequently, the patient developed acute hepatic failure. Acute/subacute hepatic failure associated with amyloidosis commonly presents in patients with multiple myeloma. Patient was diagnosed with amyloidosis on liver biopsy. Later, during hospitalisation patient developed multiorgan failure.
Case presentation
A 44 years old male was initially seen by primary care physician for complaints of persistent cough. Patient was treated with antibiotics for community-acquired pneumonia. His chest X-ray later revealed a large right-sided pleural effusion. The patient cough worsened and was referred to the hospital for further management. He had a thoracentesis done (2 L of fluid removed) and his symptoms improved. On fluid analysis patient had exudative effusion with lymphocytic infiltrates. His shortness of breath initially improved, but within few days his symptoms returned. Repeat chest X-ray revealed worsening left-sided pleural effusion. Patient cardiac echo was unremarkable. He was evaluated by cardiothoracic surgery team and recommended a right video-assisted thoracic surgery (VATS) with decortication and pleural biopsy. A right VATS with decortication was done. Pathology showed extensive caseating granulomas and tissue cultures came back positive for mycobacterium tuberculosis. Laboratory tests showed elevated LFTs with cholestatic pattern with bilirubin of 6, and alkaline phosphatase 300, alanine aminotransferase and aspartate aminotransferase increased to 80’s. The patient was started on levofloxacin, rifabutin and ethambutol due to less hepatotoxic profile and initial workup for deranged LFTs was negative. During hospitalisation patient’s LFTs kept on worsening. Ultrasound of abdomen showed patent splenic, mesenteric portal and hepatic veins with normal waveforms. Hepatomegaly with perihepatic ascites were noted. (figure 1) Medications were stopped and a liver biopsy was done. There was significant involvement of the liver by amyloidosis on pathology. (figure 2) Patient’s further work up included a bone marrow biopsy which revealed 30% to 40% cellularity, 5% to 10% plasma cells, amyloidosis (kappa type), normal cytogenetics consistent with multiple myeloma. (figures 3–5) Oncology team recommended to start chemotherapy with CyBorD (cyclophosphamide, bortezomib and dexamethasone) for multiple myeloma. Despite chemotherapy patient’s hepatic renal and cardiac functions were worsening over a period of weeks. Patient developed abdominal pain, moderate ascites and hypotension with elevated international normalised ratio (INR), bilirubin in the 30's and alkaline phosphatase in 1000’s. He was ultimately transferred to intensive care unit where he developed cardiac arrest and died due to multiorgan failure.
Figure 1.

Ultrasound of abdomen demonstrating normal flow in hepatic artery and perihepatic ascites (white arrow).
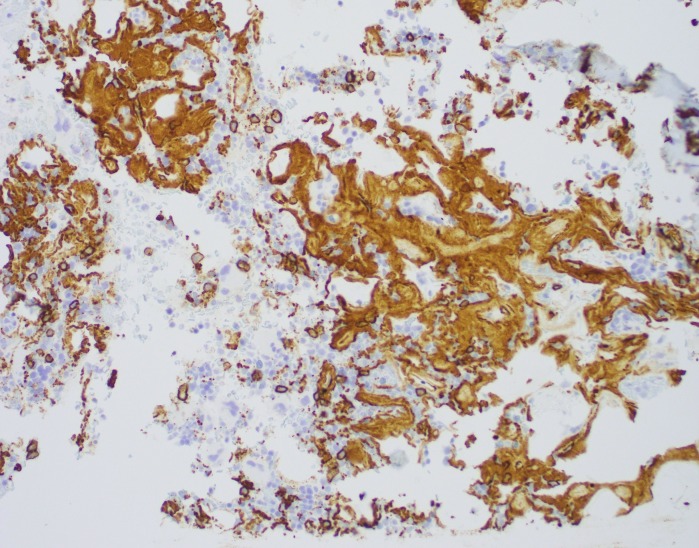
Figure 2.
Liver biopsy demonstrating diffuse sinusoidal amyloidosis (black arrow) - congophilic, extracellular, pale eosinophilic, hyaline, amorphous, acellular material.
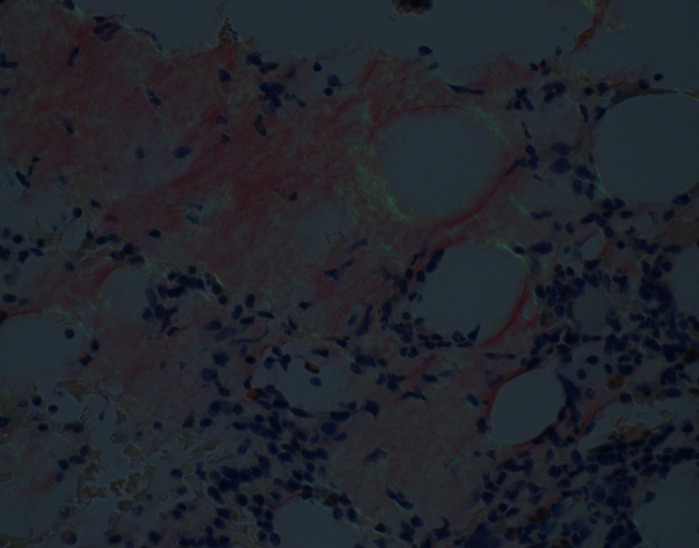
Figure 3.
Immunostain for CD-138 for palsma cells in bone marrow.
Figure 4.
Bone marrow biopsy - Congo red stain light micrograph with salmon pink staining for amyloid.
Figure 5.
Bone marrow biopsy- Congo red stain (polarised light micrograph) with apple green birefringence for amyloid.
Investigations
Complete blood count.
Complete metabolic panel.
Prothrombin time, INR.
Serum/urine electrophoresis and immunofixation for multiple myeloma.
Serum free light chain assay for multiple myeloma.
Ultrasound of abdomen with doppler: Patent splenic, mesenteric portal and hepatic veins with normal waveforms. Hepatomegaly with perihepatic ascites were noted. Normal anteroposterior diameter of the portal vein (figure 1).
Liver biopsy for amyloidosis: Diffuse hepatic sinusoidal amyloidosis with canalicular and hepatic cholestasis (figure 2).
Bone marrow biopsy for multiple myeloma (figures 3–5).
Differential diagnosis
Differential diagnosis we considered were hepatic tuberculosis, multiple myeloma-induced acute hepatic failure, hepatic amyloidosis, haemochromatosis, hepatitis, drug-induced hepatic failure, toxin-induced hepatic failure.
Treatment
Chemotherapy with CyBorD.
High dose melphalan and stem cell transplant.
Liver transplantation.
Stem cell transplant.
Outcome and follow-up
Due to multiple complications that includes hepatic failure and kidney failure, the patient was transferred to intensive care unit where he developed cardiac arrest and died.
Discussion
Amyloidosis is a condition of abnormal protein metabolism, characterised by extracellular deposition of amyloid fibrils in different tissues and organs. It can be classified based on chemical composition of amyloid fibrils and their predecessor protein type. The two main types of amyloidosis are (1) myeloma-associated (AL) amyloidosis or primary amyloidosis and (2) amyloid-associated (AA) amyloidosis or secondary amyloidosis. Myeloma-associated amyloidosis is most commonly associated with plasma cell dyscrasias and malignant B-cell type lymphoproliferative malignancies and is characterised by deposition of kappa or lambda light chains. It is due to this reason myeloma-associated amyloidosis is called as A ‘L’ amyloidosis. Amyloid-associated amyloidosis is characterised by deposition of amyloid A fibrils, which are produced from serum amyloid A precursor proteins. Serum amyloid A is a protein that is produced in response to inflammation or infection. Thus, chronic inflammatory conditions such as rheumatoid arthritis and chronic infections such as tuberculosis are the prime examples of secondary amyloidosis causing deposition of serum amyloid A over several years. Both types can be localised or systemic.3
Clinical manifestations of amyloidosis depend on the various organ involvement. Liver involvement is common, but it rarely presents as clinically significant disease and is not associated with liver dysfunction. The most common clinical presentation of hepatic involvement in amyloidosis is hepatomegaly, while the only chemical abnormality is elevation of alkaline phosphatase.4 Portal hypertension, cholestasis and subcapsular haematoma with subsequent hepatic rupture has also been reported in the patients with myeloma-associated amyloidosis.2 5 6 Hepatic failure is not a common consequence of amyloidosis however few, but well written cases have been reported with patients having acute to subacute hepatic failure in myeloma-associated amyloidosis.7–10 Liver involvement in any type of amyloidosis has been associated with worse prognosis as compared with patients without liver involvement. This association was explained by Lovat et al. Study included 180 patients with AL amyloidosis, 138 with AA amyloidosis, 99 with hereditary amyloid syndromes and 67 with dialysis-related (β2 microglobulin) amyloid. It was shown that 5-year survival in patients without hepatic involvement was better (72%) while patients with hepatic disease had 43% which indicated poor prognosis.11 If systemic disease is suspected patient should undergo evaluation of other organs such as kidney where it can present as acute renal failure. In heart it causes restrictive cardiomyopathy. Peripheral sensorimotor neuropathy along with autonomic neuropathy is also a common manifestation of AL amyloidosis. Macroglossia is also a prominent symptom of AL amyloidosis. Respiratory system, skin, joints are also involved.
Amyloidosis leading to hepatic failure has poor prognosis and many times present as diagnostic dilemma.12 13 Diagnosis of liver involvement by AL amyloidosis can be made with liver biopsy along with bone marrow examination. Biopsy via transjugular technique has been proposed to prevent major bleeding. Different histological patterns have been seen in patients with amyloidosis. Vascular pattern in which hepatic arteries and arterioles are involved and a sinusoidal pattern in which the space of Disse and hepatic sinusoids are involved.14 15 The amyloid looks acellular, pale and amorphous on regular H&E stain, while when stained with Congo red it shows green birefringence under polarisation.16
Patients with multiorgan involvement in amyloidosis, biopsies are not the initial mode of management. The first test in these patients would be serum immunofixation and an Ig free light chain assay for kappa and lambda immunoglobulin light chains. If immunofixation is positive, then abdominal fat pad aspirate or bone marrow biopsy. Patient with cardiac amyloidosis and echocardiogram showing cardiac changes should undergo pyrophosphate scan.17 The following algorithm is showing steps of diagnosing amyloidosis in different organs. (figure 6)
Figure 6.
Algorithm for diagnosis of multisystem amyloidosis.15
Various combinations of treatment have been tried for the management of primary amyloidosis with hepatic involvement. Girnius et al demonstrated improvement in hepatic disease in two-third of the patients that underwent high dose intravenous melphalan and autologous stem cell transplant.18 Another case demonstrated how sequential liver and stem cell transplant has been successful in disease remission in patients with hepatic failure secondary to amyloidosis.19 Bortezomib, a proteasome inhibitor is a potential agent for the targeted therapy. Two studies have demonstrated higher response rate and remission with CyBorD.20 21 However one case report showed poor response to CyBorD.12 Liver transplant in hepatic amyloidosis along with bortezomib and dexamethasone post-transplant showed favourable results. Patient was started 6 weeks post-transplant on bortezomib/dexamethasone and achieved remission after only one course.22 No recurrent disease was noted 22 months post-transplant.
Despite various studies about possible treatment there is still scarcity of literature regarding the successful treatment of patients with hepatic amyloidosis. Our patient presented developed acute hepatic failure. Biopsy of the liver and bone marrow was done which showed significant involvement of the liver and bone marrow by AL amyloidosis. Bone marrow biopsy demonstrated multiple myeloma. Patient was started on CyBorD. Unfortunately, patient had multiorgan failure and expired. This highlights the need for further investigations of potential therapeutic protocols for this devastating disease.
Learning points.
Although hepatic involvement is common in amyloidosis, acute/subacute hepatic failure can result in multiple myeloma-associated amyloidosis.
CyBorD(cyclophosphamide, bortezomib and dexamethasone) is the current treatment of choice for myeloma-associated hepatic amyloidosis, however further study should be done regarding therapeutic options.
Liver transplantation along with stem cell transplant has been proposed for isolated hepatic amyloidosis.
Footnotes
Twitter: @vakasullah
Contributors: MMK coordinated the data collection. MUR did the statistical analysis and wrote the manuscript. WU helped in reference arrangement and data mining. IH did the critical review. AH did the supervision and review.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Next of kin consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Serra L, Poppi MC, Criscuolo M, et al. Primary systemic amyloidosis with giant hepatomegaly and portal hypertension: a case report and a review of the literature. Ital J Gastroenterol 1993;25:435–8. [PubMed] [Google Scholar]
- 2. Bujanda L, Beguiristain A, Alberdi F, et al. Spontaneous rupture of the liver in amyloidosis. Am J Gastroenterol 1997;92:1385–6. [PubMed] [Google Scholar]
- 3. Merlini G, Bellotti V. Molecular mechanisms of amyloidosis. N Engl J Med 2003;349:583–96. 10.1056/NEJMra023144 [DOI] [PubMed] [Google Scholar]
- 4. Ebert EC, Nagar M. Gastrointestinal manifestations of amyloidosis. Am J Gastroenterol 2008;103:776–87. 10.1111/j.1572-0241.2007.01669.x [DOI] [PubMed] [Google Scholar]
- 5. Ünsal Ç., Paydaş S, Gönlüşen G. Cholestasis and renal failure in a patient with secondary amyloidosis. Ren Fail 2002;24:863–6. 10.1081/JDI-120015688 [DOI] [PubMed] [Google Scholar]
- 6. Bion E, Brenard R, Pariente EA, et al. Sinusoidal portal hypertension in hepatic amyloidosis. Gut 1991;32:227–30. 10.1136/gut.32.2.227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yamamoto T, Maeda N, Kawasaki H. Hepatic failure in a case of multiple myeloma-associated amyloidosis (k-AL). J Gastroenterol 1995;30:393–7. 10.1007/BF02347517 [DOI] [PubMed] [Google Scholar]
- 8. Oe Y, Nakaya I, Yahata M, et al. κ I light chain AL amyloidosis presenting with rapidly progressive renal and hepatic failure with unusual renal amyloid distribution. Clin Nephrol 2012;77:66–70. 10.5414/CN106804 [DOI] [PubMed] [Google Scholar]
- 9. Dohmen K, Nagano M, Iwakiri R, et al. A case of prominent hepatic cholestasis developing to hepatic failure in lambda-AL amyloidosis. Gastroenterol Jpn 1991;26:376–81. 10.1007/BF02781928 [DOI] [PubMed] [Google Scholar]
- 10. Ales NC, Daniels JT, Frizell ER, et al. Multiple myeloma-associated amyloidosis manifesting as fulminant hepatic failure. South Med J 2001;94:1036–9. [PubMed] [Google Scholar]
- 11. Lovat LB, Persey MR, Madhoo S, et al. The liver in systemic amyloidosis: insights from 123I serum amyloid P component scintigraphy in 484 patients. Gut 1998;42:727–34. 10.1136/gut.42.5.727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yim B, Kertowidjojo E, Zhang Y, et al. Poor outcomes in hepatic amyloidosis: a report of 2 cases. Case Rep Oncol Med 2016;2016:1–5. 10.1155/2016/7625940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Premkumar M, Rangegowda D, Vyas T, et al. Primary hepatic amyloidosis presenting as acute-on-chronic liver failure. ACG Case Reports Journal 2017;4:e22 10.14309/crj.2017.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cacciapuoti F. The role of echocardiography in the non-invasive diagnosis of cardiac amyloidosis. J Echocardiogr 2015;13:84–9. 10.1007/s12574-015-0249-1 [DOI] [PubMed] [Google Scholar]
- 15. Kiel PJ, Trueg AO, Ferguson M, et al. Disease-Free survival following high dose or standard dose therapy in patients with amyloidosis. Br J Haematol 2016;174:153–5. 10.1111/bjh.13656 [DOI] [PubMed] [Google Scholar]
- 16. Altraif I, Handoo FA, Alsaad KO, et al. Fatal subacute hepatic failure in a patient with AA-type amyloidosis: case report. Patholog Res Int 2010;2010:1–4. 10.4061/2010/648089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ye L, Shi H, Wu H-M, et al. Primarily isolated hepatic involvement of amyloidosis: a case report and overview. Medicine 2016;95:e5645 10.1097/MD.0000000000005645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Girnius S, Seldin DC, Skinner M, et al. Hepatic response after high-dose melphalan and stem cell transplantation in patients with al amyloidosis associated liver disease. Haematologica 2009;94:1029–32. 10.3324/haematol.2008.001925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kumar KS, Lefkowitch J, Russo MW, et al. Successful sequential liver and stem cell transplantation for hepatic failure due to primary al amyloidosis. Gastroenterology 2002;122:2026–31. 10.1053/gast.2002.33648 [DOI] [PubMed] [Google Scholar]
- 20. Mikhael JR, Schuster SR, Jimenez-Zepeda VH, et al. Cyclophosphamide-bortezomib-dexamethasone (CyBorD) produces rapid and complete hematologic response in patients with al amyloidosis. Blood 2012;119:4391–4. 10.1182/blood-2011-11-390930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Venner CP, Lane T, Foard D, et al. Cyclophosphamide, bortezomib, and dexamethasone therapy in al amyloidosis is associated with high clonal response rates and prolonged progression-free survival. Blood 2012;119:4387–90. 10.1182/blood-2011-10-388462 [DOI] [PubMed] [Google Scholar]
- 22. Nakano R, Ohira M, Ide K, et al. Treatment of hepatic amyloid light-chain amyloidosis with bortezomib and dexamethasone in a liver transplant patient. Hepatol Res 2015;45:E150–5. 10.1111/hepr.12462 [DOI] [PubMed] [Google Scholar]